Professional Documents
Culture Documents
12 Drugs Acting On The Cardiovascular System
Uploaded by
JAN CAMILLE LENONOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
12 Drugs Acting On The Cardiovascular System
Uploaded by
JAN CAMILLE LENONCopyright:
Available Formats
PHARMACOLOGY SEM 01 | CYC 02
LECTURE AUF-CON
NCM 0106 MODULE 12 & 13 – DRUGS ACTING ON THE CARDIOVASCULAR SYSTEM
OUTLINE
I Concept Review
A Cardiovascular System
B Congestive Heart Failure
II Drugs Acting on the CVS
A Cardiac Glycosides
B Antianginals
C Antidysrhythmics
CONCEPT REVIEW
CARDIOVASCULAR SYSTEM
● BLOOD VESSELS
PARTS ○ Arteries → Arterioles → Capillaries → Venules →
Veins
● HEART
○ Largest in lumen chena: veins
○ Shape of a blunt cone and size of clenched fist
○ Largest lumen in diameter: great veins
○ Composed mainly by myocardium (heart
○ Thicker wall: arteries
muscles)
○ A lot of medication have their effect on arteries
○ Covered externally by the pericardium, lined
specifically of the smooth muscle layer that is
internally by the endocardium
why the arteries are capable of performing
○ 4 Chambers: LA, LV, RA, RV
vasoconstriction and vasodilation that is not
● Atria: receiving chambers; delivers blood to
present in veins
the right and left ventricles
● BLOOD
● Ventricles: pumping chambers
○ Composed of plasma, erythrocytes, leukocytes
○ 4 Valves
and platelets
● Tricuspid and Mitral valves
○ Plasma: 90% water, 10% solutes
● Pulmonary and Aortic Semilunar valves
● FUNCTION: prevents backflow of blood
CONCEPTS
○ Perfused through the coronary arteries
● Supplies blood to the myocardium ● CONDUCTION OF ELECTRICAL IMPULSES
● Right Coronary Artery, Left Anterior ○ SA (sinoatrial) node
Descending Artery, Left Circumflex Artery ● Primary pacemaker
● BLOOD FLOW ● 60-80 bpms
○ Oxygen-rich blood: enters the heart from the ● Sets the mood; sets the heart into
lungs and goes out to the body contraction
○ Oxygen-poor blood: enters the heart from the ○ AV node (atrioventricular)
body and goes out to the lungs ● Secondary pacemaker
○ Superior (upper) and Inferior (lower) Vena ● 40-60 bpms
Cava → Right Atrium → Tricuspid valve → Right ○ Bundle of His (right and left bundle branches)
Ventricle → Pulmonary semilunar valves → ○ Purkinje Fibers
Pulmonary trunk → Pulmonary artery (lungs, ● Stimulates the heart to contract
carrying unoxygenated blood) → Pulmonary
veins → Left Atrium → Bicuspid valve → Left
● 📌 REMEMBER: AV node can act as the primary
pacemaker if the SA node is malfunctioning
Ventricle → Aortic semilunar valve → Aorta → ○ Assess for bradycardia since AV node delivers
rest of the body only 40–60 bpms, which is significantly lesser
than the SA node
NCM 0106| Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|1
MODULE 12 – DRUGS ACTING ON THE CARDIOVASCULAR SYSTEM
CONGESTIVE HEART FAILURE
● Heart failure is a condition where the heart can
not pump enough blood to match the body's
needs
WHAT HAPPENS?
● 1. Due to cardiac abnormalities or conditions that
place increase demand on the heart; heart
compensates →
● 2. Heart muscle weakens and enlarges
○ Loses its ability to pump blood to the lungs
and systemic circulation → left or right failure
● CONTROL OF BLOOD PRESSURE ● 3. Continuous increase, forceful contractions →
○ Arterial blood pressure: determined by ● 4. Compensatory mechanism fails → congestive
peripheral resistance and cardiac output heart failure → cardiac arrest (heart stops beating
○ High blood viscosity = high resistance if not treated)
○ Longer blood vessel = higher resistance
RIGHT-SIDED AND LEFT-SIDED HEART FAILURE
○ Blood vessel radius increases = lesser
resistance produced ● Right-Sided Heart Failure
○ Cardiac Output (CO) ○ Right atrium will return blood/fluid to the
● Volume of blood pumped by either systemic circulation
ventricles of the heart each minute ○ Mainly systemic S/Sx
● FORMULA: CO = HR x Stroke Volume ● Abdominal pain (masyadong maraming
(amount of blood ejected by the ventricle blood na nare-receive), fatigue, bloating,
every after heartbeat) nausea, dependent pitting edema, ankle
● Normal CO = 4-8 L/m edema, ascites, jaundice, hepatomegaly
○ Stroke Volume (SV) (enlargement of the liver), decreased urine
● Volume of blood pumped per ventricle output (lesser blood flow going to the
each time the heart contracts kidneys), increase central venous pressure
● Three Factors Affecting Stroke Volume (CVP; measures pressure in the right atrium
○ Preload: force exerted by blood against and nag-i-increase ito since maraming
the ventricles at the end of diastole blood sa RA), hypertension (maraming fluid
● Blood flow force that stretches sa circulation)
the ventricle ○ Ex. Peripheral edema
● Higher preload = higher cardiac ● Left-Sided Heart Failure
output ○ ANO’NG NANGYAYARI?: Naiipon ‘yung blood
○ Contractility: force of ventricular (from left atrium) sa left ventricle kasi ayaw na
contractions niyang mag-pump
● Higher preload and contractility = ● Since ayaw i-receive ng left
higher stroke volume atrium/ventricle ‘yung blood, nagpu-pool
○ Afterload: resistance to ventricular sila sa blood. Nalulunod ‘yung lungs sa
ejection of blood caused by opposing sobrang daming fluid.
pressures in the aorta and systemic ○ Mainly respiratory S/Sx
circulation ● Dyspnea, orthopnea, fatigue, restlessness,
● Afterload increases = crackles (due to .. hehe :ano raw),
decreased/weaker stroke volume peripheral cyanosis (oxygenated blood
● Left ventricle has to pump harder does not reach the periphery), dry
due to the presence of resistance non-productive cough (so much fluid in the
○ Heart Rate lungs), frothy blood tinged mucus
● Number of times the heart contracts each (nag-iipon ‘yung blood)
minute
NCM 0106 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|2
MODULE 12 – DRUGS ACTING ON THE CARDIOVASCULAR SYSTEM
○ Nursing Intervention: Do not place patient flat ● Decrease conduction of heart cells through
in bed, dapat orthopneic position propped with AV node
pillows ○ Increase stroke volume
● They will feel as if they’re drowning if placed ● Due to increased force of contraction
flat on the bed
○ Ex. Pulmonary edema DIGOXIN (LANOXIN)
STAGES OF HEART FAILURE (PUMP FAILURE) ● A secondary drug of choice for heart failure
● Indications: Heart Failure, Atrial Fibrillation (rapid
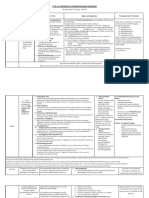
STAGE CHARACTERISTICS ACCORDING TO STAGE
beating)
High risk to heart failure without symptoms ● Route: PO and IV
A
of structural heart disease ● t ½: 36 hours (long half-life; given only once a day)
Some cardiac changes such as decreased ● Low protein binding power
ejection fraction of heart failure without ● 30% metabolized by the liver
symptoms ● 65% excreted by the kidneys unchanged
B
● Serum level for dysrhythmias: 0.8-2.0 ng/ml
Ejection fraction: how much is expelled from Serum level for heart failure: 0.5–1.0 ng/ml
●
the heart; 50-70% is normal
● Toxic level: >2-3 ng/ml
Structural heart disease with some ● PHARMACOKINETICS
symptoms of heart failure such as fatigue, ○ Contraindications
C
shortness of breath, edema, and decrease in ● Ventricular Fibrillation (fast AV node;
physical activity
hypokalemia)
Severe structural heart disease and marked ○ Side Effects
D
symptoms of heart failure even at rest ● N/V, diarrhea, abdominal pain, confusion,
weakness, blurred vision
DRUGS ACTING ON THE CVS ○ Adverse Reactions
● Bradycardia, cardiac dysrhythmias,
A. CARDIAC GLYCOSIDES Thrombocytopenia
Digitalis Glycosides ● Prior Nursing Intervention: read ECG
● Used since 1200 AD
● Naturally-occurring coming from purple and white DIGITALIS TOXICITY (CARDIOTOXICITY)
foxglove plants, which can be poisonous
● Signaled by emerging side effects
● MECHANISM: inhibits the Na-K pump that leads to
● Serum levels exceed 3 ng/ml
increased intracellular Na
● Elderly are more prone to develop toxicity
○ Leads to calcium influx that causes more
○ Because the elderly have degenerating
efficient cardiac muscle fiber contractions
excretory system, the liver ages, thus having
● INDICATIONS: Heart failure, correcting CHF, atrial
higher chances of not excreting excess level of
fibrillation and atrial flutter
digitalis
○ Atrial fibrillation is a type of cardiac
● S/Sx: Confusion, Irregular pulse, N/V, diarrhea, vision
dysrhythmia characterized by rapid and
changes, appetite loss
uncoordinated contractions of the atria
● Gastrointestinal distress: N/V, anorexia and/or
○ Atrial flutter is characterized by very rapid
diarrhea (earliest signs), salivation and abdominal
contractions (200–300 bpm)
pain
● FOUR EFFECTS OF DIGITALIS ON THE HEART
● Neurological effects: restlessness, irritability,
○ (+) Inotropic
headache, weakness, lethargy, drowsiness, and/or
● Influences the contraction; increases vigor
confusion, visual disturbances (blurred or colored
and force of contraction
vision, halo vision, amblyopia, and diplopia
● Increased CO
● Cardiac effects: cardiac dysrhythmias, bradycardia
○ (-) Chronotropic
and AV block
● Slows down the heart rate
● ANTIDOTES
● Addresses atrial fibrillation and/or flutter
○ Digoxin-Immune Fab (Ovine, Digifab, Digibind)
together with negative dromotropic action
● Bind with digitalis compound = excreted
○ (-) Dromotropic
together = lower digoxin level
● Slower conduction of signals from SA node
NCM 0106 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|3
MODULE 12 – DRUGS ACTING ON THE CARDIOVASCULAR SYSTEM
○ Phenytoin and Lidocaine are effective in ● Predictable
treating digoxin-toxicity-induced ventricular ● Occurs following physical exertion or stress
dysrhythmias ● Can be relieved by rest
● Controls only the symptoms brought about ○ Unstable Angina (Preinfarction)
by the toxicity but not correct the toxicity ● Unpredictable, may occur even at rest
● Occurs frequently over the course of a day
DIGOXIN DRUG INTERACTIONS with progressive severity
○ Variant (Prinzmetal, Vasospastic)
● (+) potent diuretics – digitalis toxicity ● Occurs during rest, worsens overtime
○ Potassium-wasting diuretics: Furosemide ● Typical pain is described as originating in the
(Lasix), Hydrochlorothiazide (Hydrodiuril) center of the chest, radiating to the left arm and
○ Furosemide and thiazides promote K loss neck
(hypokalemia) ● Decreased blood flow, decreased oxygen
● Normal potassium level: 3.5-5 mmol/L myocardium leading to pain lasting for a few
● Hypokalemia may intensify the minutes
concentration of digitalis ● S/sx: tightness, pressure in the center of the chest
○ Results in higher risk for patients to and pain radiating down the left arm, neck (severe
have digitalis toxicity because the AP)
digitalis bind at the same receptor site ○ Usually starts with epigastric pain
of potassium
○ Digoxin have stronger effect – it sapaws
the potassium
● (+) Cortisone preparations – digitalis toxicity
○ Promotes Na retention and K loss when taken
systematically
● (+) Antacids, bulk forming laxatives – decreased
digitalis absorption
NURSING RESPONSIBILITIES
● Obtain drug history
● Record baseline PR at the apical pulse for one full THREE TYPES OF ANTIANGINALS
minute; withhold drug if pulse is >60 bpm
○ Baka bumagal lalo since may negative ● MECHANISM: increase blood flow either by
chronotropic/dromotropic action = increasing oxygen supply or by decreasing oxygen
bradycardia demand by the myocardium
● Recommend potassium rich food sources as
permitted in diet NITRATES
○ We are preventing hypokalemia
● Developed in 1840s
● Monitor serum digoxin levels (NORMAL: 0.8–2
● First agent used to relieve angina
ng/ml); monitor I&O
● Act on smooth muscle and the blood vessels
● Space the time of medications
causing relaxation and dilation
● Instruct to report signs and symptoms of toxicity
○ Promotes generalized and coronary
vasodilation
B. ANTIANGINALS
● When nitrate is ingested and flows through
● Drugs used to treat Angina Pectoris the bloodstream, they enter the cells and
○ A condition of acute cardiac/chest pain caused smooth muscles located at the arteries and
by inadequate myocardial perfusion due to are converted to nitric oxide
either plaque formation or coronary artery ● They increase Cyclic Guanosine
spasms Monophosphate that causes the relaxation
● Could lead to Myocardial Infarction or a of the of smooth muscle layer of blood
heart attack vessels causing vasodilation
● THREE TYPES OF ANGINA PECTORIS
○ Stable Angina (Classic)
NCM 0106 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|4
MODULE 12 – DRUGS ACTING ON THE CARDIOVASCULAR SYSTEM
● Decreases preload and afterload = ○ Do not touch the medication portion
decreases workload of heart = reduces ● You might absorb the medication
myocardial oxygen demand systemically
● NITROGLYCERIN (NTG) ● Rotate sites: thighs and arms can be used
○ Most used nitrate ○ Do not repeatedly use one site only
○ Preparations: Sublingual (SL) tablets ● Avoid hairy areas (may shave to increase
(commonly used), ointment, transdermal patch absorption)
(kept for patient up to 8-12 hrs OD, usually in ● Do not apply on the chest in the vicinity of
anterior chest), extended release capsules, defibrillator-cardioverter paddle
aerosol sprays ● Avoid alcohol ingestion
● NTG SL → internal jugular vein → right ● Store bottle away from light
atrium ○ Might lose potency
○ Given in 3 doses, 5 minutes interval ● Burning and stinging sensation means the drug is
● PO is avoided because nitrates undergo potent
hepatic first pass (medications that ● Instruct client not to discontinue these drugs
undergoes hepatic first pass effect are without healthcare provider’s approval =
greatly metabolized before going to withdrawal symptoms may be severe
bloodstream); sa liver pa lang ubos na ● NON-PHARMACOLOGICAL WAYS
yung gamot ○ Avoid heavy meals, smoking, extremes weather
○ Side Effects: H/A (can be given changes, strenuous exercise, emotional upset
acetaminophen), postural hypotension, ● These might put extra workload in the heart
dizziness, weakness and faintness, myocardial and decrease oxygen
ischemia (rebound effect; lalala ‘yung ○ Moderate exercise, rest, relaxation techniques
condition), reflex tachycardia (compensatory ● Perform pain assessment
mechanism), and syncope because of ● Monitor blood pressure, report hypotension
vasodilating effect ● If NTG patch is about to be discontinued, taper
○ Drug Interactions down dose prior to discontinuation of drug
● (+) other vasodilators = risk for hypotension ○ If abruptly discontinued, nitrates can cause
greatly increases spasms
● (+) heparin = antagonized heparin effect ● Wear gloves when applying transdermal
when given NTG is given as an IV dose preparations
● Advise patient to refrain from doing activities
NURSING RESPONSIBILITIES requiring alertness as it can cause fainting
● Educate patient about orthostatic hypotension
● Monitor vital signs especially blood pressure
○ Monitor orthostatic hypotension BETA BLOCKERS
● Have client sit and lie down during
administration ● Blocks Beta receptors → decrease effects of
● Tolerance to nitrates may develop due to continued sympathetic NS → block release of catecholamines
increase in dosage and prolonged use (NE/Epi) → decrease HR and BP
● SUBLINGUAL ROUTE OF ADMINISTRATION ● Blocks Beta 1 and Beta 2 receptors
○ Offer sips of water before giving sublingual ● For classic angina (anti-angina) decrease HR,
nitroglycerin decrease myocardial contractility → decrease
● Dryness of the oral mucosa might affect the oxygen consumption → decrease pain of angina
absorption of the medication ● Decreases sympathetic nervous stimulation of
● DO NOT give after administration cardiac muscles
○ If chest pain persists after 3 doses of NTG SL, ● Decreased HR leads to decreased cardiac muscle
instruct client to do to nearest hospital oxygen demand which can reduce angina
● May be a sign of impending myocardial
infarction NON-SELECTIVE BETA BLOCKERS
● OINTMENT ROUTE OF ADMINISTRATION
○ Do not use finger, instead use gloves or tongue ● Blocks Beta 1 and 2 (decrease HR and
depressor bronchoconstriction)
● TRANSDERMAL PATCH ROUTE OF ADMINISTRATION
NCM 0106 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|5
MODULE 12 – DRUGS ACTING ON THE CARDIOVASCULAR SYSTEM
● Ex: Propranolol (Inderal), Nadolol (Cogard), Pindolol ○ Dysrhythmia (distured heart rhythm)
(Visken) ○ Arrhythmia (absence of rhythm)
● Contraindications: Asthma because of the
bronchoconstriction effect ELECTROCARDIOGRAM (ECG)
● S/E: bronchospasm, psychotic response,
impotence, bradycardia, hypotension
SELECTIVE BETA BLOCKERS (CARDIOSELECTIVE)
● Blocks Beta 1 (decreases HR)
● Ex: Atenolol (Tenormin), Metoprolol (Neobloc,
Lopressor)
● S/E: decrease HR (bradycardia), decrease BP
(hypotension)
CALCIUM CHANNEL BLOCKERS
● Also known as CCBs
● First introduced in 1982 for the treatment of stable
and variant angina, hypertension and certain
dysrhythmias
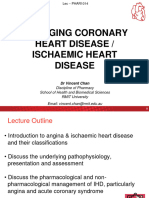
● Calcium ● P wave: atrial depolarization (contraction)
○ Increases myocardial contractions ● QRS wave: ventricular depolarization (contraction)
○ Increases workload of the heart ● T wave: ventricular repolarization (relaxation)
○ Increases oxygen need/consumption ● PQ interval: atrial repolarization (relaxation)
● Calcium Channel Blockers (blocks Ca)
○ Exert dilating effect on coronary arteries and 5 PHASES OF A HEARTBEAT
peripheral blood vessels by inhibiting calcium Travel of the cardiac action potential across the heart
→ coronary vasodilation and increase blood
PHASE EVENT
flow and lower BP
0 Rapid depolarization caused by Na influx
○ Negative inotropics and decreases afterload
which help decrease cardiac oxygen demands Initial repolarization which coincides with
1
Examples the termination of Na ions influx
●
○ “-dipine” (Amlodipine, Nifedipine, Nicardipine, 2 Plateau associated with the influx of Ca ions
Felodipine) Rapid repolarization caused by the influx of
3
○ Verapamil HCl, Diltiazem HCl K ions
● Routes: PO, IV 4 Resting membrane potential
● Common side effects: Hypotension (vasodilation),
Bradycardia, Dizziness, Headache
TYPES OF ANTIDYSRHYTHMIC DRUGS
C. ANTIARRHYTHMICS CLASS 1 - NA CHANNEL BLOCKERS – FAST
Antidysrhythmia
● Decreases Na ion influx which decreases
● Cardiac Dysrhythmia (Arrhythmia) conduction velocity and suppresses automaticity
○ Any deviation from the normal rate and pattern ● 1A
(normal sinus rhythm) of the heartbeat; ○ Slows conduction and prolong repolarization
bradycardia, tachycardia, irregular heart ○ Longer relaxation phase
rhythm ○ Ex: Quinidine, Procainamide
○ Often follow a myocardial infarction or as a ● 1B
result of hypoxia or hypercapnia ○ Slows conduction and shortens repolarization
○ Atrial dysrhythmia: prevent proper filling of ○ Faster relaxation phase
ventricles and decrease the CO by ⅓ ○ Ex: Lidocaine HCl
○ Ventricular dysrhythmia: – ● 1C
● NOTE: DYS- VS ARRHYTHMIA
NCM 0106 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|6
MODULE 12 – DRUGS ACTING ON THE CARDIOVASCULAR SYSTEM
○ Prolongs conduction with little effect on
repolarization
○ Given for fast arrhythmias
○ Ex: Propafenone
CLASS 2 - BETA BLOCKERS
● Block sympathetic activity
○ Leads to decreased contractility, BP, AV node
conduction, and enhance repolarization
○ Shortens cardiac action potential across the
heart
● Decreases conduction velocity, automaticity and
refractory time
● Ex: Propranolol (Inderal)
CLASS 3 - POTASSIUM CHANNEL BLOCKERS
● Drugs that prolong repolarization
● Prolong action potential and delay repolarization
and refractory period
● Increases the refractory period, and prolongs the
action potential duration
● Longer relaxation phase = lower HR
● Ex: Amiodarone HCl (Cordarone)
CLASS 4 - CA CHANNEL BLOCKERS
● Inhibit movement of calcium ions decreasing
excitability and contractility of the myocardium
● Most effective at the SA and AV nodes to reduce
rate of contraction
● Dilate coronary arteries and increase blood flow to
the myocardium
● A negative inotropic agent
● Ex: Verapamil (Calan), Diltiazem (Cardizem)
● SIDE EFFECTS
○ Cardiovascular depression, hypotension,
bradycardia, confusion, nausea and vomiting,
headache, dizziness
● NURSING RESPONSIBILITIES
○ Obtain baseline VS and ECG
● Hypotension and bradycardia
○ Perform objective pain assessment
● They may manifest chest pain
○ Monitor cardiac enzymes/markers
● Might indicate Myocardial infarction
○ Promote rest
REFERENCES
Synchronous Lecture: 15 Nov 2022 (CI: Ma’am Jennie
Junio)
Module: NCM 0106 - Module 12
NCM 0106 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|7
You might also like
- Neurological Examination PDFDocument6 pagesNeurological Examination PDFArif K BashaNo ratings yet
- Perioperative Nursing ManualDocument101 pagesPerioperative Nursing ManualGabrielle MagdaraogNo ratings yet
- Livro Acesso VenosoDocument302 pagesLivro Acesso VenosoDaniele MoraesNo ratings yet
- Webinar ACLSDocument52 pagesWebinar ACLSNurhasanahNo ratings yet
- Electrolytes (3607)Document11 pagesElectrolytes (3607)JennNo ratings yet
- Pharmacotherapy of Cardiac ArrhythmiasDocument68 pagesPharmacotherapy of Cardiac ArrhythmiasABREHAM BUKULONo ratings yet
- MCEM B CVS TachycardiaDocument12 pagesMCEM B CVS TachycardiaRajin MaahiNo ratings yet
- Anesthesia For Patients With Diabetes Mellitus - UpToDateDocument31 pagesAnesthesia For Patients With Diabetes Mellitus - UpToDateEduardoNo ratings yet
- Public Health CommunityDocument10 pagesPublic Health CommunityGummy BearsNo ratings yet
- Introduction To Nursing PharmacologyDocument97 pagesIntroduction To Nursing PharmacologyLiel TorresNo ratings yet
- DAILY ICU ROUNDSDocument59 pagesDAILY ICU ROUNDStuulipNo ratings yet
- LAB 4 - Additives and Order of DrawDocument2 pagesLAB 4 - Additives and Order of DrawJewel Jehd AlegriaNo ratings yet
- Nursing Flash CardsDocument5 pagesNursing Flash CardsJan Clarisse RamosNo ratings yet
- Renal Disorders GuideDocument62 pagesRenal Disorders GuideDardarConstantinoNo ratings yet
- Principles of Dialysis ModuleDocument9 pagesPrinciples of Dialysis ModuleCj MaravillaNo ratings yet
- Brochure The MS Disease Modifying MedicationsDocument16 pagesBrochure The MS Disease Modifying MedicationsBarath R BaskaranNo ratings yet
- PEDIATRIC ASSESSMENT OVERVIEWDocument2 pagesPEDIATRIC ASSESSMENT OVERVIEWAghnia Nafila100% (1)
- MS Eent (Nle)Document3 pagesMS Eent (Nle)Maginalyn CangasNo ratings yet
- I Summary Family MedicineDocument185 pagesI Summary Family MedicineModa ModyNo ratings yet
- Cardiac Arrythmias in The ED Menbeu Edited From AnaDocument106 pagesCardiac Arrythmias in The ED Menbeu Edited From AnaTemesgen Geleta100% (1)
- Pediatric NursingDocument146 pagesPediatric NursingJannele BernadasNo ratings yet
- Anatomy & Physiology Bootcamp NotesDocument51 pagesAnatomy & Physiology Bootcamp Notesgeorgia robinsonNo ratings yet
- Tipsy Avant ResumeDocument3 pagesTipsy Avant ResumeTIPSY ANTONYNo ratings yet
- PHARMACOLOGY CompilesDocument83 pagesPHARMACOLOGY Compilesjj alotintoNo ratings yet
- Drug Addiction: A Chronic Brain DiseaseDocument19 pagesDrug Addiction: A Chronic Brain Diseasetrigui amir100% (1)
- ICU One Pager EVD V11Document1 pageICU One Pager EVD V11Mohamed Mahmoud100% (1)
- Emergency NursingDocument29 pagesEmergency NursingLouise NicoleNo ratings yet
- Communicable Disease NursingDocument22 pagesCommunicable Disease NursingNur SanaaniNo ratings yet
- Fetal Heart TonesDocument1 pageFetal Heart TonesChristian Clyde N. JakosalemNo ratings yet
- Acute Critical Care Nursing HandoutDocument17 pagesAcute Critical Care Nursing HandoutRuby Ann DimayugaNo ratings yet
- (Macmillan Small Business Series) Paul Burns, Jim Dewhurst (Eds.) - Small Business and Entrepreneurship (1996, Macmillan Education UK)Document341 pages(Macmillan Small Business Series) Paul Burns, Jim Dewhurst (Eds.) - Small Business and Entrepreneurship (1996, Macmillan Education UK)K59 Dao Phuong MaiNo ratings yet
- Use of Restraint and Seclusion in The Emergency Department - Psychiatric TimesDocument10 pagesUse of Restraint and Seclusion in The Emergency Department - Psychiatric TimesKaren C. ManoodNo ratings yet
- Normal DIE CPP Calculations:: Increased Intracranial Pressure (Cerebral Perfusion Pressure)Document79 pagesNormal DIE CPP Calculations:: Increased Intracranial Pressure (Cerebral Perfusion Pressure)Nur SanaaniNo ratings yet
- Vascular Responses to PathogensFrom EverandVascular Responses to PathogensFelicity N.E. GavinsNo ratings yet
- Issue 26 - The Nurse Advocate - Hamad Medical Corporation - July 2016Document20 pagesIssue 26 - The Nurse Advocate - Hamad Medical Corporation - July 2016Brent ForemanNo ratings yet
- 03 Sympathomimetics-And-Blockers NCM206Document9 pages03 Sympathomimetics-And-Blockers NCM206julinka beyla yansonNo ratings yet
- ON-CALL ISSUES RESOLVEDDocument55 pagesON-CALL ISSUES RESOLVEDlatifaNo ratings yet
- Think Nursing! ReportDocument20 pagesThink Nursing! ReportRobert Fraser RNNo ratings yet
- ChemotherapeuticDocument22 pagesChemotherapeuticDino MicaNo ratings yet
- Cte #2: Matrix of Communicable DiseasesDocument7 pagesCte #2: Matrix of Communicable Diseasesjoannamae molagaNo ratings yet
- F&E For Elderly - ModuleDocument163 pagesF&E For Elderly - ModuleArihk NiladaNo ratings yet
- Nursing Care of Child With Thalassemia and LeukemiaDocument60 pagesNursing Care of Child With Thalassemia and LeukemiaJanicex FongNo ratings yet
- Assess client readiness for health changesDocument13 pagesAssess client readiness for health changesDarren VargasNo ratings yet
- Med Surge Skills Checklist Inna StreszDocument6 pagesMed Surge Skills Checklist Inna StreszPrecious Angelique MalacatNo ratings yet
- CARDIOVASCULAR NURSING: TISSUE PERFUSION AND VASCULAR DISORDERSDocument19 pagesCARDIOVASCULAR NURSING: TISSUE PERFUSION AND VASCULAR DISORDERSZayne Lucas Gabrielle TadiamonNo ratings yet
- IWT Sampling Bioassay Test Treatability StudyDocument44 pagesIWT Sampling Bioassay Test Treatability Studyharshu D100% (1)
- AssessmentDocument11 pagesAssessmentFarmisa MannanNo ratings yet
- Privacy and confidentiality overviewDocument22 pagesPrivacy and confidentiality overviewRayzl GacayanNo ratings yet
- UntitledמממDocument96 pagesUntitledמממAli Aborges Jr.No ratings yet
- Acute Stroke ProtocolDocument3 pagesAcute Stroke ProtocolKarissaNo ratings yet
- Survanta 25mg - ML Suspension - Summary of Product Characteristics (SMPC) - (Emc)Document7 pagesSurvanta 25mg - ML Suspension - Summary of Product Characteristics (SMPC) - (Emc)Mohadese hosseini zabetNo ratings yet
- AbbreviationDocument19 pagesAbbreviationJayson NatividadNo ratings yet
- Sirs & ModsDocument5 pagesSirs & Modsmarlou agananNo ratings yet
- AfibDocument2 pagesAfibhakdogNo ratings yet
- Data Collection Form - Pressure InjuryDocument3 pagesData Collection Form - Pressure InjuryErwin Dela GanaNo ratings yet
- Glucose TestingDocument5 pagesGlucose TestingMoira Julianne Serognas BrigoliNo ratings yet
- Nursing Care of Clients With Upper Airway or Respiratory DisordersDocument6 pagesNursing Care of Clients With Upper Airway or Respiratory DisordersLuna MarieNo ratings yet
- Pharmacology - Dosage Calculation GuideDocument20 pagesPharmacology - Dosage Calculation GuideKyla Avila TorrevillasNo ratings yet
- Pharmacology Text BookDocument431 pagesPharmacology Text BookSaba AmirNo ratings yet
- Sinus Bradycardia: I. Sinus Dysrhythmias Description ManagementDocument4 pagesSinus Bradycardia: I. Sinus Dysrhythmias Description ManagementMargueretti Delos ReyesNo ratings yet
- 07 Nursing Role in The Health of Ill Children and Their FamiliesDocument20 pages07 Nursing Role in The Health of Ill Children and Their FamiliesJAN CAMILLE LENONNo ratings yet
- 06.2 Care of Couples With Fertility ProblemsDocument9 pages06.2 Care of Couples With Fertility ProblemsJAN CAMILLE LENONNo ratings yet
- 06.1 High-Risk Postpartal ClientDocument22 pages06.1 High-Risk Postpartal ClientJAN CAMILLE LENONNo ratings yet
- 05.2 Problems of The PassageDocument5 pages05.2 Problems of The PassageJAN CAMILLE LENONNo ratings yet
- MCN REVIEW FOR MIDTERMSDocument5 pagesMCN REVIEW FOR MIDTERMSJAN CAMILLE LENONNo ratings yet
- 04 Third Trimester ConditionsDocument11 pages04 Third Trimester ConditionsJAN CAMILLE LENONNo ratings yet
- 05.3 Problems of The Power and Psyche PDFDocument12 pages05.3 Problems of The Power and Psyche PDFJAN CAMILLE LENONNo ratings yet
- 08 - LEC Family Nursing Care PlanDocument6 pages08 - LEC Family Nursing Care PlanJAN CAMILLE LENONNo ratings yet
- 03 Second Trimester ConditionsDocument7 pages03 Second Trimester ConditionsJAN CAMILLE LENONNo ratings yet
- Levels of clientele in community nursing and key Philippine health lawsDocument1 pageLevels of clientele in community nursing and key Philippine health lawsJAN CAMILLE LENONNo ratings yet
- 02 First Trimester ConditionsDocument12 pages02 First Trimester ConditionsJAN CAMILLE LENONNo ratings yet
- 16NBSHemoglobinDisorders IJNS2021Document13 pages16NBSHemoglobinDisorders IJNS2021JAN CAMILLE LENONNo ratings yet
- Care for high-risk pregnant women with diabetesDocument27 pagesCare for high-risk pregnant women with diabetesJAN CAMILLE LENONNo ratings yet
- Care of Mother and Child with Acute ProblemsDocument16 pagesCare of Mother and Child with Acute ProblemsJAN CAMILLE LENONNo ratings yet
- 06.1 High-Risk Postpartal ClientDocument22 pages06.1 High-Risk Postpartal ClientJAN CAMILLE LENONNo ratings yet
- Care for high-risk pregnant women with diabetesDocument27 pagesCare for high-risk pregnant women with diabetesJAN CAMILLE LENONNo ratings yet
- 01.1 High-Risk Prenatal ClientDocument18 pages01.1 High-Risk Prenatal ClientJAN CAMILLE LENONNo ratings yet
- 2518-Article Text-13816-1-10-20201215Document6 pages2518-Article Text-13816-1-10-20201215JAN CAMILLE LENONNo ratings yet
- Oia Keisha PDFDocument7 pagesOia Keisha PDFJAN CAMILLE LENONNo ratings yet
- Level 2 - Prelim Exam Guidelines 2023Document2 pagesLevel 2 - Prelim Exam Guidelines 2023JAN CAMILLE LENONNo ratings yet
- 05 - LEC The Family and Family HealthDocument5 pages05 - LEC The Family and Family HealthJAN CAMILLE LENONNo ratings yet
- 2554-Article Text-13960-1-10-20201220Document9 pages2554-Article Text-13960-1-10-20201220JAN CAMILLE LENONNo ratings yet
- Le3 Oia PDFDocument12 pagesLe3 Oia PDFJAN CAMILLE LENONNo ratings yet
- Requirements Level 2 OPDDocument5 pagesRequirements Level 2 OPDJAN CAMILLE LENONNo ratings yet
- 12 Drugs Acting On The Cardiovascular SystemDocument5 pages12 Drugs Acting On The Cardiovascular SystemJAN CAMILLE LENONNo ratings yet
- Maintaining Proper HygieneDocument10 pagesMaintaining Proper HygieneJAN CAMILLE LENONNo ratings yet
- 04-05 - LEC Intrapartal Care and The Labor PhenomenonDocument29 pages04-05 - LEC Intrapartal Care and The Labor PhenomenonJAN CAMILLE LENONNo ratings yet
- NCP Format 3Document3 pagesNCP Format 3JAN CAMILLE LENONNo ratings yet
- 07 - LEC Care of The NewbornDocument17 pages07 - LEC Care of The NewbornJAN CAMILLE LENONNo ratings yet
- Ischemic Heart DiseaseDocument56 pagesIschemic Heart DiseaseSMART PHARMACY By BRIJESHNo ratings yet
- UVA Family Medicine Qbank Answers PDFDocument101 pagesUVA Family Medicine Qbank Answers PDFjamesmgang100% (1)
- Pathology - Cardiovascular SystemDocument17 pagesPathology - Cardiovascular SystemNdegwa Jesse100% (2)
- Ignore The Awkward by Uffe RavnskovDocument91 pagesIgnore The Awkward by Uffe Ravnskov2361983100% (1)
- Heart Failure Nursing InterventionsDocument301 pagesHeart Failure Nursing Interventionsticoystephanie100% (2)
- Becker Et Al. - 1999 - Cardiotoxicity of The Antiproliferative Compound FDocument10 pagesBecker Et Al. - 1999 - Cardiotoxicity of The Antiproliferative Compound Faly alyNo ratings yet
- NPTE CArdio NotesDocument27 pagesNPTE CArdio NotesAubrey Vale SagunNo ratings yet
- Providing Prompt Medical Care for Major EmergenciesDocument78 pagesProviding Prompt Medical Care for Major EmergenciesGopala Hari100% (8)
- Resident Autopsy LogDocument5 pagesResident Autopsy LogrboumendjelNo ratings yet
- Cardiology and Medical MnemonicsDocument4 pagesCardiology and Medical MnemonicshawkreadNo ratings yet
- CHF Risk Factors in Type 2 DiabetesDocument6 pagesCHF Risk Factors in Type 2 DiabetesFini Riski Aulia SagalaNo ratings yet
- Wk5-Therapeutics of Heart Disease and Heart Attacks 2021Document75 pagesWk5-Therapeutics of Heart Disease and Heart Attacks 2021Khashayar MastooriNo ratings yet
- Paper " Part of Human Body and Health Problem HEART DISEASE"Document6 pagesPaper " Part of Human Body and Health Problem HEART DISEASE"ekklesia imbingNo ratings yet
- Medical Terminology Chapter 1 Practice QuestionsDocument30 pagesMedical Terminology Chapter 1 Practice Questionshtb495No ratings yet
- Atrial Fibrillation - Practice Essentials, Background, PathophysiologyDocument17 pagesAtrial Fibrillation - Practice Essentials, Background, PathophysiologyLorentina Den PanjaitanNo ratings yet
- Concept Map Worksheet Mary Richards Heart Failure Jasgou1752Document3 pagesConcept Map Worksheet Mary Richards Heart Failure Jasgou1752Jasmyn Rose100% (1)
- Experience of Health Professionals Around An Exorcism: A Case ReportDocument4 pagesExperience of Health Professionals Around An Exorcism: A Case ReportsorinfNo ratings yet
- Step 3 Form 3 CorrectedDocument41 pagesStep 3 Form 3 CorrectedSBG BPT100% (2)
- VVVVDocument5 pagesVVVVapi-634424915No ratings yet
- VELARDE-Pharmacology Notes Unit B-Cardiovascular System-2019Document19 pagesVELARDE-Pharmacology Notes Unit B-Cardiovascular System-2019j blNo ratings yet
- DepresijaDocument6 pagesDepresijaChristopher PhillipsNo ratings yet
- Sarawak Handbook of Medical Emergencies, 3rd EdDocument410 pagesSarawak Handbook of Medical Emergencies, 3rd EdKelvin SuNo ratings yet
- RocheCARDIACTroponinT 07007302190 V2 CAN ENDocument3 pagesRocheCARDIACTroponinT 07007302190 V2 CAN ENPrince KatariyaNo ratings yet
- Overview of Medical Care in Adults With Diabetes Mellitus - UpToDate PDFDocument47 pagesOverview of Medical Care in Adults With Diabetes Mellitus - UpToDate PDFIzamar RomeroNo ratings yet
- Expository Essay (English III)Document2 pagesExpository Essay (English III)Faiqa MalikNo ratings yet
- Oxford American Cardiology Library HypertensionDocument190 pagesOxford American Cardiology Library HypertensionWesker Albert100% (1)
- Chd. AmiDocument4 pagesChd. AmiDead shotNo ratings yet
- Asdui Jjasbd Uiwqbd Jsabdiuqw BJDocument78 pagesAsdui Jjasbd Uiwqbd Jsabdiuqw BJAndreas WongsoNo ratings yet
- Patient Safety and Patient Assessment in Pre-Hospital Care: A Study ProtocolDocument7 pagesPatient Safety and Patient Assessment in Pre-Hospital Care: A Study ProtocolDeby KurniawanNo ratings yet
- The CardiacDocument7 pagesThe CardiacCake ManNo ratings yet