Professional Documents
Culture Documents
04-05 - LEC Intrapartal Care and The Labor Phenomenon
Uploaded by
JAN CAMILLE LENONOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
04-05 - LEC Intrapartal Care and The Labor Phenomenon
Uploaded by
JAN CAMILLE LENONCopyright:
Available Formats
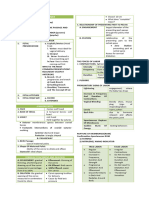
CARE OF MOTHER, CHILD, AND ADOLESCENT SEM 01 | CYC 01
LECTURE / WELL-CLIENTS AUF-CON
NCM 0107 MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
a. Poor
OUTLINE b. Moderate
I Intrapartal Care c. Good
A Normal Labor and Delivery d. Excellent
i Methods for Pain Management, Relaxation and
Birth Settings
II Labor 6. When the fetal presenting part is at the level of the
A Theories ischial spine, the station is:
B Components
i Passageway
a. 0
ii Passenger b. -1
· Fetal Presentation and Position c. +2
iii Power
d. +3
· Premonitory Signs of Pregnancy
· Signs of True Labor
· Rupture of the Membrane 7. Which of the following is the most common type of
iv Psyche fetal presentation?
C Stages of labor
i First a. Military
· Latent, Active, and Transition b. Brow
ii Second c. Face
iii Third
· Placental Separation and Expulsion d. Vertex
iv Fourth
8. All of the following are methods that can determine
fetal position, presentation, and lie, EXCEPT:
PRE-TEST a. Abdominal x-ray
b. Auscultation of fetal heart tones
1. Labor pains are perceived more quickly if anxiety is
c. Leopold’s maneuver
present.
d. Sonography
a. True
b. False
9. One of the premonitory signs of labor onset is slight
decrease in maternal weight 1 or 2 days before the
2. This component of labor refers to the fetal position:
onset of labor.
a. Psyche
a. True
b. Passageway
b. False
c. Passenger
d. Power
10. In the mechanisms of labor, which of the following
will follow after fetal descent?
3. The suture which joins the occipital bone and two
a. Internal rotation
parietal bones:
b. Flexion
a. Frontal
c. Extension
b. Sagittal
d. External rotation
c. Coronal
d. Lambdoid
11. Effacement is a characteristic referable to the:
a. widening of the cervical canal
4. This refers to the intersections of the cranial sutures:
b. shortening and thinning of the cervical
a. Mentum
canal
b. Fontanelle
c. thickening of the uterine wall
c. Molding
d. formation of a ridge dividing the uterus into
d. Attitude
two segments
5. When the fetus presents the smallest
12. The relation of the long axis of the fetus to the long
anteroposterior diameter because it puts the whole
axis of the mother is termed:
body into an ovoid shape, occupying the smallest
a. Station
space as possible, the fetal attitude is:
NCM 0107| Banaag, Cato, Diala, Mallari, Malonzo, Paras|1
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
b. Position 18. In a vertex presentation and an LOA position, the
c. Presentation fetal heart rate can usually be heard at the:
d. Attitude a. RLQ
e. Lie b. LLQ
c. RUQ
13. The primary aim of doing a perineal incision or d. LUQ
episiotomy is to:
a. prevent lacerations* 19. Voiding every 2–3 hrs is encouraged in a woman in
b. reduce duration of second stage of labor labor to:
c. prevent prolonged and severe stretching of I. Facilitate fetal descent
muscles supporting the bladder II. Lessen the weight of her abdomen
d. spare the infant's head from prolonged III. Avoid UTI
pressure and pushing against the rigid IV. Stimulate contractions
perineum a. 1 and 2
b. 1 and 3
14. Crowning is best defined as: c. 2 and 3
a. accommodation of the fetal head to the d. 3 and 4
pelvic shape
b. encirclement of the largest diameter of the 20. Which of the following is a characteristic of true
fetal head by the vulvar ring* labor pains?
c. enlargement of the fetal head a. lack of cervical effacement or dilatation
d. appearance of the fetal head at the vagina b. cessation of uterine contractions
c. irregular, generally confined to the abdomen
15. Signs of placental separation include the following; d. intensification of uterine contractions with
I. Uterus becomes elongated walking
II. Uterus rises to the level of the umbilicus
(Calkin’s sign) 21. The beginning of the second stage of labor can be
III. Sudden gush of blood from vagina recognized by the patient's desire to:
IV. Shortening of the cord a. blow during contractions
a. 1 and 2 b. tense up during contractions
b. 1 and 3 c. push during contractions
c. 2 and 3 d. pant during contractions
d. 3 and 4
22. The average length of time a primipara patient will
16. Which of the following describes the Shultz be in labor is approximately:
mechanism of placental separation? a. 18
I. Placenta separates first from its center b. 20
II. The shiny surfaces presents at vaginal c. 24
opening d. 14* (Multipara)
III. Placenta separates first at its edges
IV. The raw, red, irregular surface presents at the 23. When the placenta has been delivered, the first
vaginal opening thing the nurse should do is to:
a. 1 and 2 a. palpate the uterus if it is contracted
b. 2 and 3 b. administer oxytocic agents as ordered
c. 1 and 3 c. inspect the placenta for completeness of the
d. 3 and 4 cotyledon
d. estimate the blood loss to detect any
17. Which of the following is the most common position bleeding
of the fetus at birth?
a. right sacroposterior (RSP) 24. It is the relation of the fetal presenting part of a
b. left occiput anterior (LOA) specific quadrant of the woman's pelvis.
c. right mentum transverse (RMT) a. Station
d. right acromion dorsoanterior (RADA) b. Position
c. Presentation
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|2
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
d. Attitude ● 2. Impulses pass through a dense, interacting
network of cells in the spinal cord (substantia
25. It is the relation of the fetal presenting part to the gelatinosa)
level of the ischial spines. ● 3. A synapse occurs that returns the transmission
a. Lie to the peripheral site through motor nerve
b. Station ● 4. Impulse then continues in the spinal cord to
c. Presentation reach the hypothalamus and cortex of the brain
d. Position ● 5. Impulse is interpreted and perceived as pain
26. Stage of expulsion in labor PRINCIPLES
a. 1
b. 2 ● A woman needs to come into labor informed about
c. 3 what causes labor pain and prepared with
d. 4 breathing exercises to use to minimize pain during
contractions
27. Stage of dilatation in labor ● A woman experiences less pain if her abdomen is
a. 1 relaxed and the uterus is allowed to rise freely
b. 2 against the abdominal wall with contractions
c. 3 ● Using the gating control theory of pain perception:
d. 4 distraction techniques
28. Normal amount of blood loss during labor and METHODS FOR PAIN MANAGEMENT
delivery: A. GATE CONTROL MECHANISMS
a. 100 mL
b. 250–350 mL ● Involves halting an impulse at the level of the spinal
c. 600 mL cord so the impulse is never perceived at the brain
d. 1000 mL level as pain, a process similar to closing a gate
● Involves 3 techniques
29. It is the relation of the long axis of the fetus to the
long axis of the mother. CUTANEOUS STIMULATION
a. Presentation
b. Station ● Ability of the small nerve fibers at the injury site to
c. Position transmit pain impulses appears to decrease if the
d. Attitude large peripheral nerves next to the injury site are
e. Lie stimulated
● Examples
30. It is synonymous to crowning which is the ○ Rubbing an injured
encirclement of the largest diameter of the fetal part
head by the vulvar ring [station]. ○ Applying
a. +1 or +2 Transcutaneous
b. -1 or -2 Electrical Nerve
c. -3 or -4 Stimulation
d. +3 or +4 ○ Heat/cold compress
○ Effleurage: light abdominal massage
MODULE PROPER
DISTRACTION
NORMAL LABOR AND DELIVERY
PAIN PATHWAY ● If the cells of the brain stem that register an impulse
as pain are preoccupied with other stimuli, a pain
● 1. Endings of the small peripheral nerve fibers impulse will not register
detect a stimulus transmit to the cells in the dorsal ● Examples
horn of the spinal cord ○ Breathing techniques: increases oxygenation
– decreasing pain
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|3
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
○ Focusing/Imagery: sensate focus like ● Couple must be aware of these breathing exercises
photograph of her husband/children, a during prenatal care
graphic design, or something appealing to ● Ex: Unang Yakap
them
6 MAJOR CONCEPTS
REDUCTION OF ANXIETY
1. Labor should begin on its own, not induced
● Pain is perceived more quickly if anxiety is also 2. Woman should walk, move freely throughout the
present labor and change position
● Examples 3. Woman should bring loved one, friend for
○ Focusing/Imagery - sensate focus like continuous support
photography of her husband/children, a a. Woman should continuously receive support
graphic design, or something appealing to during labor
them b. DOULA: do not have any training in obstetrics
but hired to support the laboring mother
B. BRADLEY METHOD 4. Interventions that are not medically necessary
Partner-Coached should be avoided
a. No routine interventions such as IVF
● Developed by Robert Bradley
5. Women should be allowed to give birth in other
● Pregnancy is a joyful natural process and stresses
positions
importance of the husband
a. Allow woman to assume a non-supine position
● Pain is reduced by: abdominal breathing, walking
6. Mother and baby should be housed together
during labor
following birth
● Husband will coach the pregnant wife
C. PSYCHOSEXUAL METHOD RELAXATION TECHNIQUES
Sheila Kitzinger CONSCIOUS RELAXATION
● Stresses that pregnancy, labor and birth, and the Relax the body so the woman does not remain
●
early newborn period are important points in tense, have anxiety, unnecessary muscle strain and
woman’s life cycle fatigue during labor
● Program involves conscious relaxation and levels
of progressive breathing that encourages the CLEANSING BREATH
woman “to flow with” rather than struggle against
contractions of labor ● Woman breathes deeply and then exhale deeply
D. GRANTLY DICK-READ METHOD CONSCIOUSLY CONTROLLED
BREATHING
● Fear leads to tension and tension leads to pain
● Achieves relaxation and reduced pain in labor by LEVEL 1
using abdominal breathing during contractions
● Reduction/prevention of fear = no tension = no pain ● Slow chest breathing (comfortable but full
respirations 6-12 cpm)
E. LAMAZE METHOD ● Early labor
Ferdinand Lamaze
LEVEL 2
● Based on stimulus-response conditioning
○ To be effective, full concentration on ● Breathing lighter than level 1
breathing exercises during labor should be ● Rib cage expands lightly; the diaphragm barely
observed moves
● PSYCHOPROPHYLACTIC METHOD: preventing pain ● RR up to 40 cpm
during labor (prophylaxis) by the use of mind ● Good for contractions when cervical dilation is 4
(psyche) and 6 cm
● Teach the mother full concentration in breathing
exercises (mind over matter)
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|4
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
LEVEL 3 ALTERNATIVE METHODS OF BIRTH
● Breathing is shallow mostly at the sternum LEBOYER
● 50-70 cpm
● From a warm, fluid filled intrauterine environment to
● Keep the tip of the tongue against the roof of her
a noisy, air filled brightly lit birth room creates major
mouth
shock
● Cervical dilation 7 and 10 cm (full dilation)
● Birthing room is darkened so there is no sudden
contrast in light, keep pleasantly warm, soft music
LEVEL 4
is played, infant handled gently
● Uses “pant-blow pattern” ● Cord is cut late, placed in a warm-water bath
○ 3-4 quick breaths then a careful exhalation
○ “choo-choo” “hee-hee-hee-hoo” HYDROTHERAPY AND WATER BIRTH
● Reclining or sitting in warm water labor can be
LEVEL 5
soothing
● Chest panting is continuous, very shallow, 60 cpm ○ Feeling of weightlessness and relaxation can
Prevents pushing before dilation reduce discomforts
●
○ Ex: Labor in shower/spa tubs
TYPES OF BIRTH SETTING ● DIFFICULTIES
○ Water contaminated with feces, aspiration,
● Besides how to prepare for labor, choosing a birth maternal chilling
setting is another important decision that a couple ● HYDROTHERAPY is done during labor only
needs to make during pregnancy
UNASSISTED BIRTHING
HOSPITAL BIRTH
● Free birthing or couple birth = woman giving birth
● Labor, Birthing, Recovery, Postpartum room (LBRPs) without healthcare provider supervision
● Differs from home birthing
ALTERNATIVE BIRTHING ● Needs no medical supervision
CENTERS
THE LABOR PHENOMENON
● Lying-in clinics
● Wellness-oriented childbirth facilities designed to ● Normally begins when a fetus is sufficiently mature
remove childbirth from the acute care hospital to cope with extrauterine life yet not too large to
setting while providing enough medical resources cause mechanical difficulties in delivery
for emergency care should complication of birth ● A normal labor starts at 37-42 weeks AOG (term)
arises ○ However, the trigger that converts the
● Woman is encouraged to express her own needs random, painless Braxton-Hicks contractions
and wishes during labor, she can choose birth into strong, coordinated, productive labor
position, bring her own music or distraction objects contractions is unknown.
and partner can perform such as cutting the cord, ○ Preterm Labor: occurs earlier than 37 weeks
woman remains 4–24 hours after birth ● A series of events by which the uterine contractions
and abdominal pressure expel a fetus and
HOME BIRTH placenta from a woman’s body
● A series of continuous, progressive contractions of
● Allows for family integrity, puts the responsibility on the uterus which help the cervix to open (dilate)
the woman to prepare the house and take care of and to thin (efface), allowing the fetus to move
her infant after birth. through the birth canal
● Not allowed in the Philippines unless emergency Full cervical dilation is 10 cm in primigravida; 7-8
●
cm in multigravida
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|5
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
THEORIES OF LABOR ONSET COMPONENTS OF LABOR
Will the patient undergo NSD or CS?
UTERINE STRETCH
PASSAGEWAY
● Any hollow organ when stretched to capacity will Route of Travel
contract and empty because of the pressure on
● Route of the fetus to travel (maternal pelvis) from
nerve endings and increased irritability of the
the uterus through the cervix and vagina to the
uterine musculature
external perineum
○ Dadaanan ng baby para mapanganak siya
OXYTOCIN
○ Because these organs are contained inside
● Oxytocin is an effective stimulant of uterine the pelvis, the fetus must also pass between
contractions in late pregnancy and is commonly the pelvic ring.
used to induce labor ● A favorable type of pelvis is the gynecoid
● Fetus’ presenting part presses the cervix → Nipples ● Size of the maternal pelvis: diagonal conjugate (AP
are stimulated → Nerve impulses travel from nipple diameter of the transverse diameter outlet)
to the hypothalamus → stimulates posterior ○ Cephalopelvic disproportion: maternal pelvis
pituitary gland to produce oxytocin → causes is not enough to deliver the fetus vaginally
uterine contractions ● Ability of the cervix to dilate and efface
PELVIC INLET
● Top opening of the pelvis
● The part of the baby’s head which enters first
PELVIC OUTLET
● Where the baby’s head and body exits
● These dimensions need to be sized sufficiently to
allow the baby to maneuver comfortably through
the pelvis for birth
TAILBONE (SACRUM/COCCYX)
PROGESTERONE DEPRIVATION
● Needs to be sufficiently mobile to be gently pressed
● Progesterone inhibits uterine contraction back out of the way when the baby moves through
● Onset of labor in humans might result from
withdrawal of progesterone at a time of relative SYMPHYSIS PUBIS
estrogen dominance
● A cartilaginous joint in the front of the pelvis
PROSTAGLANDIN ● Needs to be properly mobile to help the pelvis flex
to allow the baby to pass through
● The relative progesterone deprivation and estrogen ● The relaxin hormone in the body helps both the
predominance set off production of corticosteroids tailbone and the symphysis pubis to become more
which act on lipid precursors to release arachidonic mobile to facilitate birth
acid, and in turn, increase the synthesis of
prostaglandins. PASSENGER
● Prostaglandins, like oxytocin, are known to Fetal Position
stimulate uterine contractions
● Checks if the fetus is of appropriate size and in an
advantageous position and presentation
AGING PLACENTA
● The baby needs to be positioned properly to make
● The decrease of nutrients and blood supply in the it through the pelvis
aging placenta causes uterine contractions ● FETAL HEAD
○ Body part that has the widest diameter
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|6
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
○ Occiput Anterior (OA): part of the head which FONTANELLES
is the optimal position and presenting part for
birth ● The intersections of the cranial sutures
● Pinakamaliit na part ng head na dapat ● ANTERIOR FONTANELLE
nakalagay sa pelvis ni mother ○ Diamond shape
● Chin should be touching the chest ○ Permits the growth of the brain by remaining
(well-flexed) unossified for 12 -18 months
● Babies can be born vaginally in a number of ● POSTERIOR FONTANELLE
positions ○ Triangular-shaped
○ Closes within 8-12 weeks/ 3-4 months
FETAL SKULL ○ Lies in the junction of the lambdoidal and
sagittal sutures
STRUCTURE
OTHER IMPORTANT LANDMARKS
CRANIUM
● MENTUM
● Uppermost proportion of the skull ○ The fetal chin
● 8 bones ● SINCIPUT
○ Frontal, Two Parietal, Occipital: the four ○ Anterior area known as brow
superior bones ● VERTEX
○ Sphenoid, Ethmoid, two temporal bones: lies ○ Area between the anterior and posterior
at the base of cranium fontanelles
● OCCIPUT
SUTURES ○ Area of the fetal skull occupied by the
occipital bone, beneath the posterior
● Membranous spaces between the cranial bones
fontanelle
● Allow for molding (overlapping of the bones)
○ Molding: changes in shape of the fetal skull
DIAMETERS
produced by the force of the uterine
contractions pressing the vertex against the
● The shape of the skull causes it to be wider in its
not-yet-dilated cervix
anteroposterior diameter than in its transverse
● SAGITTAL SUTURE LINE
diameter to fit the birth canal
○ Joins the two parietal bones of the skull
● Measurement: AP diameter of the skull is wider
● CORONAL SUTURE
than the transverse diameter
○ Joins the frontal bone and the two parietal
bones
TRANSVERSE
● LAMBDOID SUTURE
○ Joins the occipital bone and the two parietal ● Bi-parietal: 9.25 cm
bones ● Bitemporal: 8 cm
● FRONTAL/MITOTIC SUTURE
○ Joins the two frontal bones ANTEROPOSTERIOR
○ Becomes the anterior continuation of the
sagittal suture ● SUBOCCIPITOBREGMATIC
○ Narrowest diameter is from the inferior
aspect of the occiput to the center of the
anterior fontanelle (approximately 9.5 cm)
● OCCIPITOFRONTAL
○ Measured from the bridge of the nose to the
occipital prominence (approximately 12 cm)
● OCCIPITOMENTAL
○ Widest AP diameter measured from the chin
to the posterior fontanelle (approximately 13.
5 cm)
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|7
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
FACE PRESENTATION (Fig. D)
● Fetus is in poor flexion
● Back is arched
● Neck is extended
● Fetus is in complete extension
and presents a wide
(occipitomental) diameter
● This unusual position usually
presents too wide a skull diameter to the birth canal
FETAL PRESENTATION AND POSITION for vaginal birth
● May also reflect a neurologic abnormality in the
FETAL ATTITUDE fetus, causing spasticity
● Describes the degree of flexion a fetus assumes
FETAL LIE
during labor or the relationship of the fetal
presenting parts to each other
● The relationship of the cephalocaudal axis (spinal
column) of the fetus to the cephalocaudal axis of
GOOD ATTITUDE (well-flexed)
the woman
● The normal fetal position
● Advantageous for birth as it LONGITUDINAL LIE TRANSVERSE LIE
helps a fetus present the smallest Cephalocaudal axis of Cephalocaudal axis of the
anteroposterior diameter the fetus is parallel to fetus is at the right angles
● Complete flexion the woman’s spine to the woman’s spine
● Spinal column is bowed forward Fetus is in a vertical Fetus is in a horizontal
● The head is flexed forward so position position
much that the chin touches the Further classified as
sternum cephalic and breech
● The arms are flexed and folded on the chest
● The thighs are flexed onto the abdomen
● The calves are pressed against the posterior aspect
of the thighs
MILITARY POSITION (head is straight)
● LIE: longitudinal
● ATTITUDE: moderate flexion
● Chin is not touching the chest
but is in an alert
● Causes next-widest
FETAL PRESENTATION
anteroposterior diameter, the
● Determined by the fetal lie and by the body part of
occipital diameter to present to
the fetus that enters the maternal pelvis first
the birth canal
○ Combination of lie and attitude
● 12 cm; hard to deliver
● May be cephalic, breech, or shoulder
BROW AND FACE PRESENTATION (poor)
CEPHALIC PRESENTATION
● Most frequent presentation occurring as often as
BROW PRESENTATION (Fig. C) 95%
● The fetus is in partial extension
● Presents the brow of the head in VERTEX
the birth canal
● Most common type of presentation
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|8
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● Skull bones are capable of effective molding to PROBLEMS ENCOUNTERED
accommodate the cervix CAPUT SUCCEDANEUM: During labor, the area of the
● LIE: longitudinal fetal skull that comes in contact with the cervix often
● ATTITUDE: good (full flexion) becomes edematous from the continued pressure
● The fetal head is completely flexed onto the chest against it
● The smallest diameter of the fetal head ● Not all babies have this, nangyayari lang kapag
(suboccipitobregmatic) presents to the maternal hindi properly timed ‘yung pag-ire
pelvis ● Normal and the edema will subside
● The occiput is the presenting part
CEPHALHEMATOMA: Happens when blood is
MILITARY collected between the periosteum of the skull bone
and the skull bone itself; will subside after a few days
● Fetal head is neither flexed or extended (straight)
● The occipitofrontal diameter presents to the
maternal pelvis
● The sinciput is the presenting part
BROW
● The fetal head is partially extended
● The occipitomental diameter, the largest
anteroposterior diameter, is presented to the
maternal pelvis
BREECH PRESENTATION
FACE
COMPLETE
● The fetal head is hyperextended (complete
extension)
● Fetus has thighs tightly flexed on
● The face is the presenting part
the abdomen
● Both the buttocks and the tightly
flexed feet present to the cervix
● Good attitude and longitudinal lie
FRANK
● Attitude is moderate because the
hips are flexed but the knees are
extended to rest on the chest.
● Buttocks alone present to the
cervix
● Lies longitudinal and moderate
attitude
FOOTLING
● Neither the thighs nor lower legs are
flexed
● SINGLE FOOTLING: one foot is
present
● DOUBLE FOOTLING: both feet present
● Longitudinal lie, poor attitude
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|9
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
SHOULDER PRESENTATION LEVELS
Level of the ischial spine (synonymous
● In transverse lie, a fetus lies horizontally in the pelvis 0
with engagement)
so that the longest fetal axis is perpendicular to that
of the mother -1 to -4 Above the ischial spine (descending)
● Presenting part is -4 Floating
usually one of the +1 to +2 Below the ischial spine (engaged)
shoulders (acromion
Synonymous to crowning; encirclement
process), an iliac crest, a
+3 to +4 of the largest diameter of the fetal head
hand or an elbow by the vulvar ring; nakikita na ‘yung FPP
● Caused by relaxed
abdominal wall from
grand multiparity, allows
unsupported uterus to fall
forward, pelvic contraction where the horizontal is
greater than the vertical space, placenta previa
(low implantation of placenta; limit a fetus ability to
turn), external version (delivery: CS)
FETAL POSITION
● Relation of the fetal presenting part to a specific
quadrant of the woman’s pelvis (right
anterior/posterior and left anterior/posterior)
NOTATIONS TO DESCRIBE FETAL POSITION
ENGAGEMENT
● Right (R) or Left (L) side of the maternal pelvis
● Settling of the presenting part of the fetus far ● O, M, Sa, A (Occiput, Mentum, Sacrum, Acromion
enough to the pelvis to be at the level of the ischial Process)
spine ○ Landmark of the presenting part
○ In a vertex presentation, the occiput (O) is the
STATION chosen point.
○ In a face presentation, it is the chin (mentum
● The relationship of the presenting part of a fetus to [M]).
the level of the ischial spine ○ In a breech presentation, it is the sacrum (Sa).
○ The ischial spines can be palpated at about a ○ In a shoulder presentation, it is the scapula or
finger-length into the vagina (felt as bony the acromion process (A).
prominences) ● A, P, T (Anterior, Posterior, Transverse)
○ Depending on whether the landmark is in front,
back, or side of the pelvis
● Positions are indicated by an abbreviation of three
letters
○ FIRST LETTER: whether the landmark is pointing
to the mother’s right or left
○ MIDDLE LETTER: fetal landmark (O, M, Sa, A)
○ LAST LETTER: whether the landmark points A, P,
or T
● NOTE: Fetal positions left and right occiput posterior
need surgery
○ This position is associated with more frequent
induction and augmentation of labor,
chorioamnionitis, postpartum hemorrhage,
third and fourth degree perineal tears, wound
infection and endometritis
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|10
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● LOA is the most common and favorable fetal WHY IS IT IMPORTANT TO DETERMINE FETAL
position followed by ROA (born and delivered the PRESENTATION AND POSITION?
fastest) ● Determines the efficiency and duration of delivery
● Kapag occiput anterior, kita ang fetal back and ○ Positions other than the LOA and ROA might
spinal area extend the process of labor and put the
mother in pain because as the baby’s head
● Kapag occiput transverse, medyo naka-side
rotates, it presses on the mother’s sacral
naman si baby
nerve which would cause more discomfort
● Could put a fetus at risk due to proportional
● The triangular-shaped is the occiput while the
differences between fetus and pelvis
diamond-shaped is the anterior fontanel
● Membranes also are more apt to rupture early,
● Kapag hindi LOA or ROA, mas matagal ang
increasing possibility of infection
pag-ikot ng occiput papunta sa vaginal canal and
● Risk of fetal anoxia and meconium staining
mas matagal ang delivery
leading to respiratory distress at birth
○ NURSING RESPONSIBILITY: lay the mother in a
side-lying position or bring the knees and
WAYS TO DETERMINE FETAL POSITION,
hands towards the abdominal chest to
PRESENTATION, AND LIE
compress the abdomen and help with fetal
● Inspection and palpation (Leopold’s maneuver)
positioning
● Vaginal examination
● Sonography
● Auscultation of fetal heart tones
POWER
● The force supplied by the fundus of the uterus and
implemented by uterine contractions, which causes
cervical dilatation and then expulsion of the fetus
from the uterus
● After full dilatation of the cervix, the primary power
is supplemented by use of a secondary power
source, the abdominal muscles
● NURSING RESPONSIBILITY: Make sure that patients
understand that they should not bear down with
their abdominal muscles to push until the cervix is
fully dilated. Doing so impedes the primary force
and could cause fetal and cervical damage.
UTERINE CONTRACTIONS
● Braxton Hicks (False Labor)
○ The uterus begins to contract and relax
periodically as if it is rehearsing for labor
○ Usually mild but can be strong enough to be
mistaken for true labor
○ Usually irregular and are not painful, but they
do not cause cervical dilatation
● Comes from the uterine fundus and implemented
by uterine contractions, a process that causes
cervical dilatation and the expulsion of the fetus
from the uterus
○ Must be strong enough in order to cause
cervical dilatation so that it can aid in the
expulsion of fetus and placenta
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|11
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
○ Need to be at regular intervals, moving closer ● One to two days before the onset of labor because
together and increasing in strength throughout of decrease progesterone level and loss of appetite
the labor
○ Dapat mula sa fundus, then pababa 5. SOFTENING/RIPENING OF THE CERVIX
● In some patients, contractions appear to
originate in the lower uterine segment ● Butter-soft
rather than in the fundus. These are
reversed and ineffective and may actually SIGNS OF TRUE LABOR
cause tightening rather than dilatation of
the cervix. UTERINE CONTRACTIONS
● After dilatation of the cervix, the primary power is
supplemented by the use of abdominal muscles ● The surest sign that labor has begun is the initiation
of effective, productive, involuntary uterine
PREMONITORY SIGNS OF PREGNANCY contractions
1. LIGHTENING TRUE CONTRACTIONS
● Descent of the fetal presenting part into the pelvic ● Increment/Crescendo: increasing in the
inlet intensity/strength of the uterine contraction
● Happens 10-14 days before labor in primigravida ○ Kapag naka-contract ang uterus, constricted
and 1 day before labor in a multipara. din ang blood vessels na nagbibigay ng
● When the largest diameter of the presenting part nutrients sa placenta
passes the pelvic inlet, the head is said to be ● Apex/Acme: the peak of the uterine contraction;
"engaged." However, lightening is heralded by the hard uterus; dilation
following signs ● Decrement/Decrescendo: decrease in the strength
○ Relief of dyspnea/SOB/diaphragmatic pressure of the uterine contraction; paglambot at pag-relax
○ Relief of abdominal tightness ng uterus; refilling of blood
○ Increased frequency of voiding ○ Contraction should be decreased because of
○ Increased amount of vaginal discharges vasoconstriction
○ Increased lordosis as the fetus enters the pelvis ○ Rigid uterus: tuloy-tuloy na matigas ang uterus
and hindi nag-rerelax; need i-CS
📌
and falls forward
● Walking is more difficult and leg cramping ○ REMEMBER: Do not get the FHR if the uterus is
may increase contracted (pwedeng mababa or possible ring
○ Shooting leg pains (from the increased mataas ang HR because the baby is
pressure in the sciatic nerve) compensating for the lack of blood supply)
2. SUDDEN BURST OF MATERNAL ENERGY/ACTIVITY HOW TO GET THE DURATION
● Awaken full of energy epinephrine release initiated ● Place palm on the top of the patient’s abdomen
by decrease in progesterone produced by the ● Feel the contraction (start counting if hard)
placenta ● Stop counting (if abdomen softens)
● This is meant to prepare the body for the “labor”
ahead CHARACTERISTICS OF CONTRACTIONS
3. BRAXTON HICKS CONTRACTIONS (PRACTICE ● Frequency
CONTRACTIONS)
○ Timed from the beginning of one contraction to
● Happens in the last week or days before labor the beginning of the next
● False, painless, irregular, abdominal contractions ○ Contractions will be 3-5 times in every
and are relieved by walking 10-minute period
● Duration
4. SLIGHT DECREASE OF MATERNAL WEIGHT ○ Timed from moment the uterus first begins to
tighten/contract until it relaxes again
● Loss is about 2-3 lbs ○ 40-60 seconds duration
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|12
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● Interval ● Kinukuhang specimen during pap smear
○ Pagitan ng contraction ● Natatanggal once the cervix opens
○ From the end of the previous contraction to the ● Parang sipon na lumalabas three days
beginning of the next contraction before menstruation
● Intensity ● Need na dalhin sa hospital
○ Subjective
○ May be mild moderate or strong at its acme FALSE CONTRACTIONS
○ The interval decreases as the labor progresses
● Begin and remain irregular
INTENSITY OF UTERINE CONTRACTION ● Felt first abdominally and remain confined to the
abdomen, groin, or Braxton Hicks
● Mild ○ Hindi umaabot sa lower back
○ The uterine muscle becomes somewhat tense, ● Often disappear with ambulation and sleep
but can be indented with gentle pressure (tip of ● Do not increase in duration, frequency, or intensity
the nose) ● Do not achieve cervical dilatation
● Moderate ● Fetus is ballotable
○ The uterus becomes moderately firm and a
firmer pressure is needed to indent (forehead) UTERINE CHANGES
● Strong
○ Uterus becomes so firm that it has the feel of ● Duration of the contraction increases from 20-30
wood like hardness, and at the height of the secs to 60-90 secs
contraction, the uterus cannot be indented ● As labor contractions progress, the uterus is
when pressure is applied (wood) gradually differentiated into two distinct portions
● Distinguished by a ridge formed in the inner uterine
surface, the physiologic retraction ring by the
examiner’s finger
UPPER UTERINE SEGMENT (Fundus)
● Becomes thicker and active, preparing it to exert
the strength necessary to expel the fetus during
the expulsion phase
LOWER UTERINE SEGMENT
● Becomes thin walled, supple, and passive so that
the fetus can be pushed out of the uterus easily
TRUE CONTRACTIONS
CONTOUR OF THE UTERUS CHANGES
● Begin irregularly but become regular and
predictable ● From a round ovoid to a structure markedly
● Felt first in lower back and sweep around to the elongated in a vertical diameter rather than
abdomen in a wave horizontally
● Continue no matter the woman’s level of activity ● This lengthening serves to straighten the body of
● Increase in duration, frequency, and intensity with the fetus and place it in better alignment to the
movement cervix and pelvis
● Achieve cervical dilatation ● As the uterus contracts, round ligaments move
● Fetus usually engaged keeping the fundus forward, assisting the fetus in
○ Nakakapa na ‘yung presenting part during IE good alignment with the cervix
● There is bloody show (mucus + blood) ● Elongation of the uterus exerts pressure against the
○ Operculum: mucus plug, protective layer of the diaphragm
cervix ● Uterus is taking control of a woman’s body
● Most sperm cells and microorganisms get
trapped in the operculum
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|13
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
CERVICAL CHANGES RUPTURE OF THE MEMBRANE (BAG OF WATER)
EFFACEMENT ● Sudden gush or a scanty slow seeping of amniotic
fluid from the vagina
● Shortening and thinning of the cervical canal to ● The color of the amniotic fluid should always be
paper-thin edges to primiparas noted
● PRIMIPARAS: Effacement is accomplished before ○ Clear: contains vernix
dilatation begins ● At term, this is clear, almost colorless and
○ NURSING RESPONSIBILITY: Inform the patient contains white specks of vernix caseosa
of both effacement and dilatation following a ○ Green: contaminated with meconium (fetal
pelvic examination distress)
● MULTIPARAS: Dilatation may proceed before ○ Yellow: blood incompatibility
effacement is complete ○ Pink: bleeding
○ Effacement must occur by the end of
dilatation, however, before the fetus can be NURSING ACTIONS WITH RUPTURED MEMBRANE
safely pushed through the cervical canal;
otherwise, cervical tearing can result. ● Once membranes have ruptured, labor is inevitable,
● During labor, the longitudinal traction from the meaning to say that uterine contractions will occur
contracting uterus shortens the cervix so much that within the next 24 hours
the cervix virtually disappears ● INITIAL NURSING ACTIONS
○ Notify the physician.
○ Lie the patient to bed to ensure that the fetus is
not impinging on the cord.
○ Check the fetal heart rate to determine for fetal
distress. (Normal: 120-160 bpm)
○ If she feels that the loop of the cord coming out
from the vagina (umbilical cord prolapse)
● Position the woman in Trendelenburg
(lower the head of the bed) in order to
release pressure on the cord
DILATATION ● Apply sterile saline saturated gauze to
prevent drying of the cord, if needed
● Enlargement of the cervical canal from an opening
a few millimeters wide to one large enough PSYCHE
(approximately 10 cm.) to permit passage of the Psychological Outlook
fetus.
● WHY DOES DILATATION OCCUR? ● Psychological state or feelings a pregnant person
○ Uterine contractions gradually increase the brings into labor
diameter of the cervical canal lumen by ○ The woman’s psyche is preserved so afterward
pulling the cervix up over the presenting part labor can be viewed as a positive experience
of the fetus ○ If the mother is afraid, tense, stressed out,
○ Fluid-filled membranes push ahead of the angry, feels unsafe or unsupported, she will not
fetus and serve as an opening wedge likely do well during birth
● If they are ruptured, the presenting part ● GOOD EMOTIONAL STATE
will serve this same function, although ○ Helps mother to cope with the pain effectively
maybe not as effectively ○ Helps her tune in to her body
● SHOW ○ Helps guide her to her baby’s needs and allows
○ Blood-tinged mucus discharge from the the other 3 P's to sync up effectively
vagina because of pressure of the ○ A mom whose psyche is healthy, strong, and
descending fetal part on the cervical who has good support during labor, will have a
capillaries, causing their rupture. good birth.
○ Capillary blood mixes mucus when ○ Regardless of the medical interventions she
operculum is released may need, she will ride her labor to a birth
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|14
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
experience she will remember with a strong
heart and a peaceful mind
● NURSING RESPONSIBILITY A. FIRST STAGE (Dilatation)
○ Always coach and provide positive feedbacks
to the mother (responsibility of the assist) ● Begins with the initiation of true labor contractions
● Umiire kapag fully effaced and dilated and ends when the cervix is fully dilated (10cm)
lang. If relaxed ang uterus, mahihirapan and complete effacement (100%)
lang si mother
● Para maka-ire nang maayos si mother, LATENT/EARLY PHASE
itaas ang head part, instruct na i-dikdik
‘yung bottom niya sa bed (parang ● Begins at the
tumatae lang), and nakatingin sa tiyan onset of regularly
niya perceived uterine
● Effective ang pag-ire if lumalaki ang contractions and
butas ng anal area since nakalagay roon ends when rapid
ang pressure and dapat closed ang cervical dilatation
mouth begins
○ Direct the mother’s focus to the labor ● Lasts for 6 hours
for nullipara while
4.5 hours for multipara
STAGES OF LABOR
● WHAT HAPPENS DURING THIS PHASE?
○ Cervical effacement (stretching/thinning)
LENGTH OF LABOR
○ Minimal cervical dilatation (3 cm)
STAGE PRIMI MULTI ● A birthing parent who enters labor with a
1: Dilatation 12 1⁄2 hrs. 7 hrs. 20 mi “nonripe” cervix will probably have a longer
2: Expulsion 80 mins. 30 mins. than average latent phase
● Dilatation refers to enlargement/opening of
3: Placental Expulsion 10 mins. 10 mins.
the cervix
Total: 14 hrs. 8 hrs. ● CONTRACTIONS
○ Mild and short uterine contractions
● The 4th stage is included as the 1-4 hours after
○ INTERVAL: 10-20 mins apart
delivery (also considered critical)
○ DURATION: 20-40 secs
○ OVERALL AVERAGE TIME
● MANIFESTATIONS
● 18-20 hours: primipara
○ Low backaches (sign of true contractions;
● 12-14 hours: multipara
nagra-radiate na sa back)
○ Abdominal cramps
FALSE LABOR ○ Excited, alert, talkative, cooperative, and in
control
● Pain in the lower abdomen and groin
● NURSING RESPONSIBILITY: Encourage patients to
● Contractions do not increase in frequency, duration,
continue to walk about and make preparations for
and intensity; irregular
birth, such as doing last-minute packing for their
● No measurable progressive cervical change
stay at the hospital or birthing center, preparing
● Relieved by walking
older children for their departure and the upcoming
birth, or giving instructions to the person who will
TRUE LABOR
take care of them while they are away
● Pain in the lower back radiating to abdomen or ○ NONPHARMACOLOGIC MANAGEMENT:
from the fundus to the back aromatherapy, distraction, and accupressure
● Contractions increase in frequency, duration, and ○ NOTE: Analgesia can be given, but might
intensity prolong this phase when given too early in
○ Consistent regular rhythmic pattern labor
● Progressive cervical change ● Help with controlling breathing and walking
● Intensify with ambulation instead
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|15
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● MANIFESTATIONS
ACTIVE ○ Experience feeling of loss of control
○ Anxiety, panic, and irritability (giving birth is the
● Begins at 6 cm
mind’s focus; gusto na lang niya i-deliver)
● Lasts for 3 hours for
○ Intense discomfort may cause N/V
nullipara while 2
hours for multipara
NURSING DIAGNOSES RELATED TO LABOR
● TWO PERIODS:
○ Acceleration 1. POWERLESSNESS R/T DURATION OF LABOR
(4-5 cm)
○ Maximum slope (5-9 cm) ● They feel na wala na silang choice but to go into
● WHAT HAPPENS DURING THIS PHASE? labor
○ Complete effacement to more rapid cervical ● NURSING INTERVENTIONS
dilatation (4–7 cm) ○ Help empower women
○ Show (increased vaginal secretions) ● Ask each woman what will make her feel
○ Spontaneous rupture of the membranes may most comfortable
occur ● Breathing with contractions, change of
● CONTRACTIONS position, passive and quiet environment
○ INTERVAL: 3–5 mins apart (shouting and crying are inevitable, but try
○ DURATION: 40–60 secs to provide a quiet environment to help the
○ Stronger, longer, and begin to cause true mother gain control)
discomfort ○ Respect contraction time
● MANIFESTATIONS ● Allow the patient to finish breathing with
○ Realizing that labor is truly progressing makes contractions
this phase exciting and frightening ○ Promote change of positions
● MOST RAPID PACE: Average rate of 3.5 cm/hr in ● Either out of bed, kneeling, squatting,
nulliparas; 5–9 cm/hr in multiparas walking, sitting, ballroom dancing, swaying,
● NURSING RESPONSIBILITY: Encourage patients to be soaking in warm water
active participants in labor by keeping active and ● Active movement can shorten labor if it is
assuming whatever position is most comfortable not contraindicated
for them during this time, except flat on their back ○ Help with fetal alignment
● Squatting, all-fours position
TRANSITION ○ Promote voiding and provide bladder care
● Void every 2–4 hours during labor
● Peak of this phase can be identified by a slight ● Percussion of the bladder (dull and
slowing rate of cervical dilatation when 9 cm is resonant)
reached (baby is moving hence the slowing rate; ● If the mother is unable to void,
baka magkaroon ng precipitous labor) catheterization using French 12–14 is done
○ At 10 cm dilatation, an irresistible urge to push
2. RISK FOR INEFFECTIVE BREATHING PATTERN R/T
begins to occur
BREATHING EXERCISES
● Focus of the mother is entirely inward on the task of
birthing the baby ● HYPERVENTILATION
● WHAT HAPPENS DURING THIS PHASE? ○ Brought about by the deep exhalation, there is
○ Full effacement and dilatation (8–10 cm) too much loss of carbon dioxide leading to
○ If it has not previously occurred, show will occur respiratory alkalosis
as the last of the mucus plug from the cervix is ○ Respiratory Alkalosis: lightheaded, numbness
released at toes and fingertips, loss of consciousness
○ If the membranes have not previously ruptured, ○ Paper bag/cupped hands covering the mouth
they will usually rupture at full dilatation (10 cm) and the nose
● CONTRACTIONS ● When the mother inhales, hindi nawawala
○ Contractions reaches their peak of intensity ‘yung CO2, nare-rebreathe niya.
○ INTERVAL: 2–3 minutes ● The CO2 is now balanced
○ DURATION: 60–90 seconds
○ NOTE: Not to be mistaken for labor
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|16
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● Determined by the fetal lie and by the body part of
3. ANXIETY R/T STRESS OF LABOR the fetus that enters the maternal pelvis first
● Presenting part refers to the part of the fetus that
● Offer support
presents at the internal cervical os and may either
○ Respect and promote the support person
be the head, the buttocks, the shoulder, brow, chin,
(doula)
face or feet
● Hydrotherapy
● Cephalic, breech, and shoulder
○ Submerged in water while in labor
○ The feel/buoyancy of the water is relaxing for
4. FETAL ATTITUDE
the person in labor
4. RISK FOR FLUID VOLUME DEFICIT R/T PROLONGED ● Posture of a fetus during labor
LACK OF ORAL INTAKE AND DIAPHORESIS FROM THE ● FLEXION: Mammalian fetuses have a tendency to
EFFORT OF LABOR assume a fully flexed posture during development
and during parturition (also includes arms, legs,
● Glass of fluid every hour if permitted
and longitudinal posture)
● Offer ice chips, popsicles, and lollipops
○ Allows for the delivery of the head by its
● Isotonic sports drinks may be given to prevent
smallest bony diameter
dehydration, exhaustion, and uterine inertia
○ A loss of this flexed posture presents a
○ Isotonic dapat para hindi magkaroon ng
progressively larger fetal head to the bony
changes sa cell
pelvis for labor and delivery
● Lip balm to prevent cracking and drying of the lips
5. FETAL POSITION
NURSING CARE AND MANAGEMENT
● Relation of the fetal presenting part to a specific
HISTORY TAKING quadrant of the woman’s pelvis
● Review of the woman’s pregnancy, 6. STATION
(physical/psychological events) general health,
family medication information ● Relation of the fetal presenting part to the level of
● Confirm EDB/EDD, time when contractions began, the ischial spines
and amount/characteristics of any show
● Check for ROM if any, drug allergies, GPTPALM, and 7. ENGAGEMENT
birth plan
● Settling of the presenting part of a fetus far enough
to the pelvis to be at the level of the ischial spine
PHYSICAL ASSESSMENT
8. LOCATION OF FETAL HEART TONE IN RELATION TO
● Leopold’s maneuver and/or internal examination PRESENTATION
are done to determine the following:
● VERTEX: area of the fetal back (LLQ or RLQ)
1. EFFACEMENT, DILATATION, AND CONDITION OF THE ● BREECH: at or above the level of the umbilicus
MEMBRANES ● FACE: at the area of the fetal chest
● Average fetal heart rate is between 110 and 160 bpm
2. FETAL LIE
(can vary by 5–25 bpm)
● The fetal heart rate may change as your baby
● Relationship of the cephalocaudal axis (spinal
responds to conditions in your uterus
column) of the fetus to the cephalocaudal axis of
○ An abnormal fetal heart rate may mean that
the woman
your baby is not getting enough oxygen or that
● LONGITUDINAL LIE: cephalocaudal axis of the fetus
there are other problems
is parallel to the woman’s spine
● With every contraction, there will be a fetal
● TRANSVERSE LIE: cephalocaudal axis of the fetal
response (seen in the fetal heart rate)
spine is at the right angles to the woman’s spine
● WHAT CAN WE USE TO GET THE FHT?
○ Stethoscope and Doppler ultrasound
3. FETAL PRESENTATION
○ NOTE: Do not take the FHT once the uterus is
contracted as it will give you unreliable results.
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|17
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● You need to simultaneously get the fetal ● Do not artificially induce labor unless the fetus is in
heart tone and maternal pulse to distress
determine if the sound you are hearing ● Allow the patient to move freely during labor
comes from the baby and not from the ● DOULA: caring support person during labor
mother’s heartbeat (maternal souffle) ● No need to insert IV and other interventions
● Position of choice during labor
● Non-separation of mother and baby after birth
unless contraindicated
ADDITIONAL INTERVENTIONS
● RAPPORT: Provide privacy and assurance; establish
therapeutic relationship
● HYGIENE:
○ Bath for comfort and relaxation
○ Wipe front to back to prevent contamination
○ Perineal preparation
● Shaving depends on the patient or on
hospital protocol
● FOOD AND FLUIDS:
○ NPO, start IVF, and monitor input and output
FETAL HEART RATE AND UTERINE CONTRACTION ○ Avoid solid foods as these can cause:
RECORDS
● Digestion: delays labor
100–109 bpm; vagal
response from compression ● Full stomach: interferes with proper bearing
Moderate Bradycardia down
of fetal head; vagus nerve
stimulation = bradycardia ● Aspiration
Marked Bradycardia <100 bpm; hypoxia ● BLADDER: must be emptied every 2–3 hours
○ Distended bladder may retard fetal descent,
Moderate Tachycardia 161–180 bpm
urinary stasis can lead to UTI, full bladder can
>180 bpm; hypoxia, be traumatized during delivery
maternal fever, fetal ● BEARING DOWN: done only during true labor
Marked Tachycardia
arrhythmia, maternal contractions (cervix fully dilated and effaced) to
anemia or hypothyroidism
minimize maternal exhaustion and possible
lacerations
9. VITAL SIGNS ● SIM’S POSITION: encourage to change and assume
comfortable position
● Assess between contractions for comfort and
○ Favors anterior rotation of the head (allows
accuracy
faster delivery)
● DO NOT TAKE during contractions as the blood
○ Promotes relaxation between contractions
vessels are constricted.
○ Prevents supine hypotension syndrome
○ INACCURACY: Pwedeng mababa or possible
● MONITORING:
ring mataas ang HR because the baby is
○ UTERINE CONTRACTION: every hour during
compensating for the lack of blood supply
latent phase and every 30 mins during active
● Check for frequency, duration, and intensity of
phase
contractions
● Should not be taken during contractions
● Use the pain scale to identify if the labor is
● During uterine contractions, no blood goes
progressing
to the placenta. The blood is pooled in the
○ Pain should be escalating
peripheral blood vessels which results in
● Check the urine specimen for presence of protein
increased blood pressure
and glucose
○ VITAL SIGNS: BP and FHR taken every hour
during the latent phase and every 30 mins.
10. LABOR AS A NATURAL PROCESS
during the active phase
● Must be a joyful and memorable experience
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|18
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● FHR tends to decrease during a contraction ○ This is because pressure is no longer exerted on
because of the compression of the fetal their stomach as the fetus descends into the
head. pelvis
○ When the fetal head is compressed by ● Perspiration and Distention of Vessels
the contracting uterus, the vagus nerve ○ Caused by forceful pushing
is stimulated, thus causing ● The fetus begins descent and, as the fetal head
bradycardia. touches the internal perineum to begin internal
● Normal FHR: 120–160 bpm rotation, the perineum begins to bulge and appear
● DRUG ADMINISTRATION: tense
○ ANALGESICS: Demerol is usually given; acts to ○ The anus may become everted, and stool may
suppress the sensory portion of the cerebral be expelled
cortex ○ CROWNING: As the fetal head pushes against
● This way, the mother feels less pain the vaginal introitus, this opens and the fetal
○ ANESTHETICS: regional anesthesia is preferred scalp appears at the opening to the vagina and
over any other form as it does not enter enlarges from the size of a dime, to a quarter,
maternal circulation and therefore does not then a half-dollar.
retard labor contractions nor cause respiratory
depression in the newborn DECELERATION PHASE
● DANGER SIGNS: be aware of the danger signs of
labor and delivery (fetal/maternal distress) ● The progress of labor does not slow down
○ FETAL DISTRESS ● The final degree of cervical dilation is achieved and
● Tachycardia: >160 bpm the cervix retracts over the presenting part
● Bradycardia: <110 bpm
● Meconium: green-stained amniotic fluid FETAL DESCENT PHASE
● Fetal thrashing or hyperactivity due to the
● Fetus descent in the pelvic ring, being pushed
fetus struggling for more oxygen.
beyond the open cervix, perineum begins to bulge
● Fetal Acidosis: blood pH below 7.2
(labia), and vaginal introitus stretched apart
○ MATERNAL DISTRESS
● BP over 140/90 or falling BP (associated with
clinical signs of shock e.g. pallor, DFIERE: MECHANISMS OF LABOR
restlessness or apprehension, and
● Also known as the cardinal movements of labor
increased RR and PR)
● Passage of a fetus through the birth canal involves
● Hemorrhage: abnormal PR >100 bpm
a number of different position changes to keep the
● Inadequate/prolonged contractions
smallest diameter of the fetal head always
● Abnormal lower abdominal contour
presenting to the smallest diameter of the birth
● Oxygen deprivation/internal hemorrhage:
canal
increasing apprehension
● Only applicable to cephalic presentation
● TRANSFER: labor room to the delivery room when
● Engagement, descent, and flexion → IR → ER
cervix is dilated
(restitution) → extension → ER (shoulder rotation)
○ Multiparas: cervical dilatation of 7-9 cms
→ extension complete → expulsion
○ Primiparas: full dilation
B. SECOND STAGE (Expulsion/Fetal Delivery) DESCENT (D’RIERE)
● Time span from full dilatation and cervical ● Downward movement
effacement to birth of the infant of the biparietal
● A patient typically feels contractions change from diameter of the fetal
the characteristic crescendo–decrescendo pattern head within the pelvic
to an uncontrollable urge to push or bear down with inlet
each contraction as if to move their bowels ● Occurs because of
pressure on the fetus
● Momentary N/V by the uterine fundus
● FULL DESCENT
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|19
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
○ Occurs when the fetal head protrudes beyond EXTERNAL ROTATION
the dilated cervix and touches the posterior
vaginal floor ● RESTITUTION: Almost
● As the pressure of the fetal head presses on the immediately after the head
sacral nerves at the pelvic floor, the pregnant of the infant is born, the
person will experience the typical “pushing head rotates a final time
sensation,” which occurs with labor (from the anteroposterior
○ This pushing, which contracts the abdominal position it assumed to enter
muscles, aids descent the outlet) back to the
FLEXION diagonal or transverse
position of the early part of labor
● As descent is completed and the fetal head ● It would rotate 45 degrees to the left so that the
touches the pelvic floor, the head bends forward anterior shoulder is just below the pubic arch
onto the chest, causing the smallest
anteroposterior diameter (the ● SHOULDER ROTATION: The
suboccipitobregmatic diameter) to present to the after-coming shoulders are
birth canal brought into an
● Aided by abdominal muscle contraction during anteroposterior position, (best
pushing for entering the outlet)
● ATTITUDE: degree of flexion that the fetus assumed ● The anterior shoulder is
prior to delivery born first, assisted perhaps by
downward flexion of the
INTERNAL ROTATION infant’s head
● NOTE: Ask the mother not to push anymore but do
● During descent, the deep breathing
biparietal diameter of the fetal
skull was aligned to fit through EXPULSION
the wider anteroposterior
diameter of the pregnant ● End of the pelvic
person’s pelvis division of labor
● As the head flexes at the ● Once the shoulders are
end of descent, the occiput born, the rest of the baby is
rotates so the head is brought born easily and smoothly
into the outlet of the pelvis, or the anteroposterior because of its smaller size
diameter is now in the anteroposterior plane of the
pelvis
● This movement brings the shoulders into the
optimal position to enter the inlet, or puts the widest
diameter of the shoulders (a transverse one) in line
with the wide transverse diameter of the inlet
● SEQUENCE: occipitotransverse (LOT) → left
occipitoanterior (LOA) → occiput anterior (OA)
○ The occiput is now either superior to or just
below the symphysis pubis
EXTENSION
● As the occiput of the fetal head is born, the back of
the neck momentarily stops beneath the pubic
arch and acts as a pivot for the rest of the head ELECTRONIC FETAL MONITORING
● The head extends, and the foremost parts of the
head, the face and chin, are born
EXTERNAL FETAL MONITOR
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|20
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● Test used during pregnancy that is non-invasive,
easily applied, has less discomfort
○ Disadvantages: DOB, limited change of position
● Measures a baby's heart rate and the mother's
contractions
○ CONTRACTIONS: fundus of the mother
○ FHT: fetal back
● Uses instruments (electrodes) placed on the
mother's belly to make the measurements
● Results are viewed as graphs on a video screen
Upper grid is used for recording FHR and is vertically
scaled in bpm. The lower grid is for recording uterine
activity and is vertically scaled in mmHg
EXTERNAL UTERINE CONTRACTION MONITORING
TOCODYNAMOMETER
● Increased myometrial tension measured through
the abdominal wall
FLUCTUATIONS IN FHR
INTERNAL FETAL MONITOR
● Involves placing a electrode directly on the fetal
scalp through the cervix
● This test is performed to evaluate fetal heart rate
and variability between beats, especially in relation
to the uterine contractions of labor
● Invasive, 3cm dilation, ruptured membranes, more
discomfort
● For high risk labor; high chance of infection
ACCELERATIONS
● A short-term rise in the heart rate of at least 15
beats per minute, lasting at least 15 seconds
● Accelerations are normal and healthy. They tell the
doctor that the baby has an adequate oxygen
supply
● Non-periodic; increase in FHR; below 30 secs
● Caused by fetal movement, change in maternal
position, or analgesics
● BEFORE 32 WEEKS (PRETERM): 10 bpm; 10 seconds
● AFTER 32 WEEKS (8th month): 15 bpm; 15 seconds
EARLY DECELERATION [MIRRORING]
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|21
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● DECELERATION: ○ Occasional, consistent, gradually increase to
○ Temporary drops in the fetal heart rate repetitive
● Early decelerations are generally normal ● Due to uteroplacental insufficiency
and not concerning ○ Decrease blood flow impeding oxygen transfer
● Late and variable decelerations can to the fetus through the intervillous space
sometimes be a sign the baby isn’t doing during intense uterine contraction (hypoxemia)
well ● Supposedly by the end of the contraction,
○ Symmetrical; periodic lower in FHT magiging normal ulit kasi nare-reestablish
○ Caused by pressure on the fetal head during ‘yung blood flow
contractions, stimulating the vagus nerve which
causes parasympathetic stimulation
● Follows pattern of uterine contraction
○ Begins at the onset of contraction and end as
the contraction ends
○ Just prior to or early in contraction
● NURSING INTERVENTIONS:
○ Left-lateral position to supply oxygenation and
blood flow
○ IV and oxygen provision
● Inverse of contraction waveform ○ CS: late decelerations that occur along with
○ Waveform consistently uniform; inversely tachycardia and very little variability can mean
mirrors contraction that the baby is in fetal distress
○ Peak of contraction = decrease in FHR
● <100 bpm and returns to normal at the end PROLONGED DECELERATION
of the contraction
● Caused by pressure on the fetal head as it ● Decrease in FHR of 15 bpm or more and lasts longer
progresses down the birth canal from 2-3 minutes
● Increased intracranial pressure stimulates ● May be a sign of cord compression or maternal
vagus nerve which slows the heart rate hypotension
● Usually seen in active labor when dilatation 4–7 cm
○ Baby is descending through the birth canal VARIABLE DECELERATION
● If early labor tapos may early deceleration, baka
may cephalopelvic disproportion si mother (needs ● Decelerations at unpredictable times in relation to
to undergo CS) contractions
● Can be single or repetitive ● Due to umbilical cord compression, ROM, rupture
● NURSING INTERVENTIONS of BOW, or oligohydramnios (too little amniotic
○ No intervention is needed fluid)
○ Continuous monitoring of the baby ● Decreases amount of blood flow to the fetus
● Repetitive deceleration may indicate short cord or
LATE DECELERATION nuchal cord
● CS, forcep births or vacuum extraction is indicated
● OCCURS LATE IN CONTRACTION: delayed 30–40 ● Waveform variable, generally sharp drops and
seconds after the onset of contractions and returns
continued beyond end of contraction ● Abrupt with fetal insult: not related to contraction
○ Consistently after the midpoint of the ● Not usually within normal range
contraction ● Variable-single around midpoint or repetitive
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|22
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● NURSING INTERVENTIONS ○ Peak of contraction kapag matigas na ‘yung
○ Left-lateral position abdomen
○ Oxygen supplementation ● No Valsalva maneuver → impaired blood return
○ Knee-chest position ○ Increases maternal abdominal pressure and
puts increased workload on the heart
○ Mag-de-decrease ang uterus and placental
blood flow
● Prolonged descent is associated with
chorioamnionitis, increased CS, and urinary
incontinence
● Assume any comfortable position (align fetal
presenting part with cervix, increase pelvic
diameters, use fetal weight to help with descent)
● Breathe naturally, use blow-blow breathing pattern
to prevent pushing between contractions and have
an effective support person
○ Do not go against uterine contractions
● FOR EFFECTIVE 2ND STAGE PUSHING:
○ Effective support person
○ Wait to feel for urge to push
○ Semi-fowler’s position with legs raised against
NURSING CARE AND MANAGEMENT
abdomen, squatting, all-fours (allow gravity to
1. PREPARING THE PLACE OF BIRTH aid the effort)
○ Short or long/sustained pushes (comfortable
● Multipara: 7–8 cm dilation for the mother; push as if defecating)
● Primipara: crowning [10 cm] (quarter–half dollar) ○ No Valsalva
● Table with instruments (with cover) ○ Breathe out during a pushing effort
● Radiant heat warmer, equipment for resuscitation, ○ Multipara: pant breathe
eye care (ophthalmia neonatorum), and
identification 4. PERINEAL CLEANING AND MASSAGE
2. PROPER POSITIONING ON THE DELIVERY TABLE ● Massage the perineum
○ Done during internal examination
● Lithotomy: clear view of perineum, no slow fetal ○ Para hindi nabibigla ‘pag delivery na
descent, and no thrombophlebitis ● Use warmed antiseptic solution
● Alternative positions (lateral, Sim’s and dorsal ● Rinse the perineal area with sterile water and clean
recumbent), semi-sitting, squatting the vagina from inner to outer part; clean compress
○ Favored because of less tension on the with each stroke
perineum and results in fewer perineal tears
5. CARE OF THE EPISIOTOMY WOUND
3. BEARING DOWN TECHNIQUE
● Episiotomy is a surgical incision of the perineum
● Best time to encourage pushing contractions, the made to prevent tearing of the perineum and to
woman is asked to take two short breaths and bear release pressure on the fetal head during delivery
down the peak of the contraction ○ Bandage scissors is used to avoid causing
harm to the fetal head
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|23
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
○ No anesthesia is necessary during episiotomy 8. PROPER HANDLING OF THE NEWBORN
as the pressure of the fetal presenting part
against the perineum (crowning) is so intense ● Immediately after delivery, the newborn should be
that the nerve endings for pain are held below the level of the mother’s vulva so that
momentarily deadened, resulting in natural blood from the placenta can enter the infant’s body
anesthesia on the basis of gravity flow
● MEDIAN EPISIOTOMY: begun in the midline of the
perineum and directed toward the rectum 9. CUTTING OF THE CORD
○ Appear to heal more easily, cause less blood
● Postponed until pulsations have stopped as
loss, and result in less discomfort to a woman in
50–100ml of blood is flowing from the placenta to
the postpartum period.
the newborn at this time
● MEDIOLATERAL EPISIOTOMY: begun in the midline of
● DELAYED CUTTING (PHYSIOLOGIC CLAMPING)
the perineum but directed laterally away from the
○ Continue to pulsate for a few minutes after birth
rectum
○ Delayed cutting can prevent polycythemia and
○ Have the advantage over midline cuts in that, if
hyperbilirubinemia because of 50-100 mL of
tearing occurs beyond the incision, it will be
blood from placenta to fetus
away from the rectum with less danger of
● (+) Adequate RBCs and WBCs
complication from rectal mucosal tears.
○ Clamp the cord 8–10 inches from the infant's
6. BREATHING TECHNIQUES umbilicus with 2 hemostats then cut in the
middle of the hemostats (the partner may cut)
● As soon as the head crowns, the woman is ○ Check for 3 vessels
instructed not to push any longer as it can cause ● AVA: 2 arteries, 1 vein (larger diameter)
rapid expulsion of the fetus. Instead, she could be ● Wharton's jelly
advised to pant (rapid and shallow breathing)
10. INITIAL CONTACT
7. RITGEN’S MANEUVER
● If there is no complication after delivery,
● Support the perineum during crowning by applying maternal–infant bonding is initiated as soon as the
pressure with the palm against the rectum with a baby has been suctioned and provided warmth
sterile towel or sanitary pad ● The mother is informed of the baby’s sex and
○ Will not only prevent lacerations of the condition and allow her to hold onto her baby,
fourchette but will also bring the fetal chin maybe put to breast to suck, it can help contract
down the chest so that the smallest diameter of the uterus as well as the weight of the baby on her
the fetal head is the one presented at the birth abdomen
canal.
● The head should be pressed gently while it slowly C. THIRD STAGE (Placental Expulsion)
eases out to prevent rapid expulsion of the fetus
○ Could result to not only to lacerations, abruptio ● Begins with the birth of the infant and ends with the
placenta, and uterine inversion but also shock delivery of the placenta
because of sudden decrease in intra ● The placenta is a freely disc-like organ that is 15-20
abdominal pressure cm in diameter and 2.3 cm in thickness and weighs
● As soon as the head has been delivered, the nurse 500 grams at term
should insert two fingers into the vagina to feel for ○ A mature placenta has 16-30 separate
the presence of a cord looped around the neck. If it segments known as cotyledons
is loose, it should be slipped down the shoulder, be ● After the birth of the infant, the uterus can be
clamped twice an inch part and cut in between. palpated as a firm, round mass just below the level
● As the head rotates, give a gentle, steady of the umbilicus
downward push in order to deliver the anterior ● After a few minutes of rest, uterine contractions
shoulder and then a gentle, upward lift to deliver begin again, and the organ assumes a discoid
the posterior shoulder. shape
● While supporting the body’s head and neck, the rest ○ It retains this new shape until the placenta has
of the baby is delivered separated, approximately 5 minutes after the
● Time of delivery must be noted birth of the infant
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|24
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
PLACENTAL SEPARATION ○ NOTE: Pressure should never be applied to a
uterus in a non-contracted state because
● Occurs because of the disproportion between the doing so could cause the uterus to evert (turn
placenta and the contracting wall of the uterus that inside out), accompanied by massive
happens as the uterus contracts down on an hemorrhage
almost empty interior ● If the placenta does not deliver spontaneously, it
● Active bleeding on the maternal surface of the can be removed manually.
placenta begins with separation, which helps to ○ It needs to be inspected after delivery to be
separate the placenta still further by pushing it certain it is intact and part of it was not
away from its attachment site retained (which could prevent the uterus from
● As separation is completed, the placenta sinks to fully contracting and lead to postpartum
the lower uterine segment or the upper vagina hemorrhage)
● SIGNS THE PLACENTA IS READY TO BE DELIVERED:
○ There is lengthening of the umbilical cord NURSING CARE AND MANAGEMENT
○ A sudden gush of vaginal blood occurs
1. PLACENTAL DELIVERY AS THE MAIN FOCUS
○ The placenta is visible at the vaginal opening
○ Calkin’s Sign: the uterus contracts and feels ● Never hurry the delivery of the placenta by
firm round in shape and rising high at the level forcefully pulling out the cord or by vigorous fundal
of the umbilicus push as this can lead to uterine inversion
● SCHULTZ PRESENTATION ● Encourage the mother to push with contractions to
○ Placenta aid in placental expulsion
separates ● BRANDT ANDREWS MANEUVER: wind the cord
first at its around the clamp, then deliver the placenta by
center and rotating it so that no placental fragments are left
lastly at its inside the uterus
edges
○ Presents at 2. TAKE NOTE OF THE TIME OF PLACENTAL DELIVERY
the vaginal
opening ● Should be delivered within 20 minutes after the
with the delivery of the baby
fetal ○ If the placenta is not delivered within this time,
surface evident the doctor should be immediately notified as it
○ Shiny and glistening could be a sign of uterine atony, a condition
○ Fetal surface that could lead to death due to hemorrhage
● DUNCAN PRESENTATION
3. COMPLETENESS OF COTYLEDONS
○ Placenta separates first at its edges and slides
along the uterine surface ● Incomplete cotyledons means that some placental
○ Presents at the vagina with the maternal fragments may have been retained in the uterus.
surface evident ● This will prevent the uterus from contracting well
○ Looks raw, red, irregular, with the ridges or and, therefore, cause excessive bleeding.
cotyledons evident
○ Dirty Irregular maternal surface 4. DETERMINE DEGREE OF UTERINE CONTRACTION
● NOTE: 300–500 mL blood loss may occur as
placental separation occurs before the uterus ● If relaxed, boggy or non-contracted, the
contracts sufficiently to seal maternal capillaries immediate nursing actions are: a) massage the
fundus gently and properly and/or b) apply an ice
PLACENTAL EXPULSION or ice cap over the abdomen.
● NOTE: Massage muna ‘yung uterus bago notify
● Placenta delivers either by the natural yung physician
bearing-down effort of the birthing parent or the
Crede’s maneuver (gentle pressure on the 5. ADMINISTRATION OF OXYTOCIC AGENTS
contracted uterine fundus by the primary
healthcare provider) ● Administered as ordered to ensure uterine
contractions, thus preventing hemorrhage
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|25
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● Methergine (0.2 mg/mL) and Syntocinon/Oxytocin ● The normal amount of blood loss during labor and
(10 u/mL): more commonly-given oxytocics; given delivery is around 300–500 mL
intramuscularly ○ CS: 500-1000mL
● NOTE: Never administered oxytocics before ● Any amount exceeding 500 mL is considered
placental delivery, it may cause placental hemorrhage.
entrapment.
● Hypertension: common side effect of oxytocins 9. PERINEAL CARE
○ The nurse should, therefore, assess or monitor
● Provide comfort and perineal care, apply clean
the blood pressure of mothers who have
sanitary
received oxytocics
● Soiled napkins should be removed from front to
6. PERINEAL LACERATIONS back.
● Presence of bright red vaginal bleeding following 10. VITAL SIGNS
placental delivery and if the uterus is firm,
● Take vital signs every 15 minutes for the first hour
lacerations should be suspected
and palpate the uterine fundus for size, and
○ LACERATIONS: ragged edges which heal more
position.
slowly and therefore predispose the mother to
● Pulse may become rapid 80-90 min., respiration
infection
20-24/min. and BP slightly elevated due to the
● CLASSIFICATIONS
excitement of the mother and recent oxytocin
○ FIRST DEGREE: involve the vaginal mucous
administration.
membrane and the skin of the perineum to the
fourchette 11. TRANSFER BACK TO ROOM
○ SECOND DEGREE: vagina, perineal skin, fascia,
levator ani muscle, and perineal body ● Transfer back to room (recovery room if she had
○ THIRD DEGREE: entire perineum and external undergone anesthesia) and position flat on bed
sphincter of the rectum without pillows to prevent dizziness due to decrease
○ FOURTH DEGREE: entire perineum, rectal in intra-abdominal pressure
sphincter and some of the mucous membrane ● Marks the start of the fourth stage of labor
of the rectum
D. FOURTH STAGE (1–4 hours after delivery)
● The stage refers to the first one to four hours
immediately after delivery when the VS are quite
unstable.
○ As critical as the other three stages of labor
● CRITICAL CONDITION: possibility of uterine atony
○ May lead to bleeding
NURSING CARE AND MANAGEMENT
ASSESSMENT
7. EPISIORRHAPHY ● FUNDUS: palpate every 15 minutes during the the
first hour and every 30 minutes for the next hours
● Repair of episiotomy or lacerations ○ Palpate at the midline of the umbilicus
● Xylocaine: local anesthetic given in order to ○ Should feel firm
minimize pain during the procedure. ● BLADDER: checked every 2 hours during the 1st 8
● Vaginal Packing: done to maintain pressure on the hours and every 8 hours for 3 days
suture line and, therefore, prevent bleeding. The ○ Suspect full urinary bladder if fundus is not well
nurse should be aware that this packing is usually contracted and is shifted to the right
removed after 24-48 hours. ○ A full bladder prevents good contraction of the
uterus and may cause hemorrhage
8. ESTIMATE AMOUNT OF BLOOD LOSS
● VAGINAL DISCHARGE: checked every 15 minutes
and should be moderate
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|26
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
○ Saturated napkin every 30 minutes means ● Increased respiratory rate to respond to increased
excessive bleeding cardiovascular parameters
● BP AND PR: check every 15 minutes during the first ● Total oxygen needs increase 100% during the
hour and then every 30 minutes until stable second stage of labor
● PERINEUM: inspect every 8 hours for 3 days ● NURSING MANAGEMENT
○ Note that the episiorrhaphy should be clean ○ Monitor for any signs of hyperventilation
and intact ● If hyperventilation occurs, rebreathing into
a paper bag can be helpful
COMFORT MEASURES ○ If needed, use appropriately patterned
breathing exercises to regulate respiratory rate
● Perform perineal care gently and apply napkin
● Sabayan ang mother sa pag-inhale &
● Lower legs simultaneously from the stirrups and
exhale
position the patient flat on the bed
○ To prevent dizziness TEMPERATURE REGULATION
● Give the patient a soothing sponge bath then
change their linen and clothing ● Body temperature may increase up to 1°F
● Provide additional blankets ● Diaphoresis occurs with increased muscular
● Give them initial nourishment of coffee, tea, soup, or activity, accompanying evaporation to cool and
milk limit excessive warming
● Provide a quiet and restful environment ● NURSING MANAGEMENT
● Allow the patient to take enough rest and sleep in ○ Monitor for any signs of infection
order to regain energy ○ Offer cool washcloths for the patient’s forehead
for comfort if needed
RESPONSES TO LABOR
FLUID BALANCE
MATERNAL PHYSIOLOGIC EFFECTS
● Insensible water loss increases during labor due to
CARDIOVASCULAR SYSTEM diaphoresis and the increase in rate and depth of
respirations
● Cardiac output increases 40%–50% from prelabor ● NURSING MANAGEMENT
levels. ○ Encourage patients to sip fluid during labor the
● Blood loss at birth is 300–500 mL on average. same as they would if they were exercising to
● Blood pressure may rise with pain response and, keep hydrated
due to work of the system during contractions, by ○ If a patient is nauseated by labor, encourage
an average systolic rise of 15 mm Hg per sips of fluid, ice chips, or hard candy to supply
contraction. Epidural anesthesia may cause some extra fluid
hypotension.
● HEMATOPOIETIC SYSTEM/BLOOD: During labor, URINARY SYSTEM
WBCs increase to a level of 25,000–30,000
cells/mm3 compared to 5,000–10,000 cells/mm3 ● Pressure of the fetal head as it descends in the birth
(leukocytosis; response of stress and heavy canal against the anterior bladder reduces bladder
exertion) tone or the ability of the bladder to sense filling
● NURSING MANAGEMENT ● NURSING MANAGEMENT
○ Monitor closely for hemorrhage ○ Advise the mother to void every 2 hours to
○ Monitor for signs of pathology with hypertensive avoid overfilling/distention as this can decrease
episodes. postpartum bladder tone
○ If allowed, increase fluid intake. If not, start IV
MUSCULOSKELETAL SYSTEM
insertion
○ Ensure that patients are well hydrated prior to ● During pregnancy, relaxin is secreted from the
epidural administration. This usually involves an ovaries, causing the cartilage between joints to be
IV fluid bolus. more flexible.
○ Put the patient on upright or side-lying position ○ This allows the joints of the pelvis to be able to
open as much as 2 cm in labor to allow for fetal
RESPIRATORY SYSTEM passage
● NURSING MANAGEMENT
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|27
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
○ Monitor for appropriate mobility and be mindful FATIGUE
of fall risks
● By the time the date of birth approaches, a birthing
GASTROINTESTINAL SYSTEM parent is generally tired from the normal
discomforts of pregnancy and has not slept well for
● Blood shunts to life-sustaining organs causing the
the past month
GI system to become fairly inactive during labor
● Sleep hunger from this type of discomfort can
● Digestive and emptying time of the stomach
make it difficult for a person to perceive situations
becomes lengthened
clearly or to adjust rapidly to new situations
● Some patients experience a loose bowel movement
● It can make the process of labor loom as an
as contractions grow strong
overwhelming, unendurable experience unless the
● NURSING MANAGEMENT
patient has competent people to offer support,
○ Recommend small but high caloric intake of
reassurance, and comfort
snacks (chocolate bars, sports drink, yogurt)
FEAR
NEUROLOGIC AND SENSORY RESPONSE
● Being taken by surprise—labor moving faster or
● Increased pain and RR
slower than anticipated or contractions harder and
● NURSING MANAGEMENT
longer than they remember from a previous
○ Where pain registers is important in
pregnancy—can lead a patient to feel out of control
appreciating why epidural anesthesia is
and increase their level of pain
effective. For early labor, the anesthetic block
● This sense of lack of control combined with pain
needs to suppress the lower thoracic synapses;
may cause a patient to begin to worry for the infant
for birth, it needs to block sacral nerves.
and fear they will not meet their own behavioral
○ Discuss nonpharmacologic pain techniques if
expectations
the patient does not desire medication.
● Contractions last a certain length and reach a
certain intensity but always have a rest period in
MATERNAL PSYCHOLOGICAL EFFECTS
between, so patients can have a break from pain.
● Labor can lead to emotional distress because it is ● Fear of labor this way releases adrenaline, and
not only painful and fatiguing but it also represents adrenaline interferes with oxytocin release and so
the beginning of a major life change for a birthing can limit the effectiveness of uterine contractions
parent and partner ● NURSING INTERVENTION: Explain and repeat as
● NURSING MANAGEMENT necessary that labor is predictable but also
○ Offer expeditious care to the patient. variable
○ Continue to encourage the process of labor. FETAL PHYSIOLOGIC EFFECTS
○ Prior to birth, a birthing parent can investigate
the services of a doula. CARDIOVASCULAR SYSTEM
○ DOULA: an individual with specialized training
who provides physical, emotional, and ● HYPOXIA DURING A CONTRACTION
psychological support to laboring parents ○ As the arteries of the uterus become sharply
● Does not perform clinical tasks constricted, and the filling of cotyledons almost
● Their presence has been shown to reduce completely halts, the amount of nutrients,
the need for analgesia and anesthesia including oxygen, exchanged during this time is
requests, shorten labor times, and increase greatly reduced, causing a slight but
satisfaction with the birth experience inconsequential fetal hypoxia.
MATERNAL RESPONSES ● INCREASED BLOOD PRESSURE
○ Caused by increased intracranial pressure
PAIN raises blood pressure and keeps circulation
from falling below normal for the duration of a
● Cultural factors can strongly influence a patient’s contraction
experience and satisfaction with labor
● To make labor a positive experience, be prepared NEUROLOGIC SYSTEM
to adapt care to the patient’s specific needs
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|28
MODULE 04 & 05 – INTRAPARTAL CARE AND THE LABOR PHENOMENON
● Uterine contractions exert pressure on the fetal
head, so the same response that is involved with
any instance of increased intracranial pressure
occurs.
● FETAL HEART RATE
○ The fetal heart rate (FHR) decreases by as
much as five beats per minute during a
contraction, as soon as contraction strength
reaches 40 mm Hg; although not measurable,
fetal blood pressure also rises.
○ The decrease in FHR appears on a fetal heart
monitor as a normal or early deceleration
pattern.
INTEGUMENTARY SYSTEM
● The pressure involved in the birth process is often
reflected in minimal petechiae or ecchymotic areas
on a fetus (particularly the presenting part)
● There may also be edema of the presenting part
(caput succedaneum) from this pressure
MUSCULOSKELETAL SYSTEM
● The force of uterine contractions tends to push a
fetus into a position of full flexion or with the head
bent forward, which is the most advantageous
position for birth
RESPIRATORY SYSTEM
● The process of labor appears to aid in the
maturation of surfactant production by alveoli in
the fetal lung
● Both the pressure applied to the chest from
contractions and passage through the birth canal
help to clear the respiratory tract of lung fluid
○ For this reason, an infant born vaginally is
usually able to establish respirations more
easily than a fetus born by cesarean birth
REFERENCES
Synchronous Lecture: 07 & 17 Oct 2022 (CI: Dr. Angela
Gonzales/Ma’am Jennie Junio)
Module: NCM 0107 LEC Mod 04 and Mod 05
Presentation Deck: Module 04 Labor and Delivery
Book: Maternal and Child Health Nursing
NCM 0107 | Banaag, Cato, Diala, Mallari, Malonzo, Navarro, Paras|29
You might also like
- Tutorial 4.2Document4 pagesTutorial 4.2Rosa FinizioNo ratings yet
- General Surgery: Aiims MedeasyDocument19 pagesGeneral Surgery: Aiims Medeasyvk100% (2)
- OB 1.01 DystociaDocument9 pagesOB 1.01 DystociaRaquel Reyes100% (1)
- MED1 Samplex Rationale 9 - Breast ExaminationDocument4 pagesMED1 Samplex Rationale 9 - Breast ExaminationMartina GarciaNo ratings yet
- CELLULAR RESPIRATION Review WorksheetDocument8 pagesCELLULAR RESPIRATION Review WorksheetMhai MontanoNo ratings yet
- GynecologyDocument42 pagesGynecologyYa MaNo ratings yet
- MCN Exam 2 Study Guide - CompleteDocument87 pagesMCN Exam 2 Study Guide - CompleteColin MacKenzie100% (1)
- Angle of Anterior ChamberDocument55 pagesAngle of Anterior Chamberuttam prakashNo ratings yet
- General Characters and Classification of FungiDocument35 pagesGeneral Characters and Classification of Fungijeonkilovers100% (3)
- OB 1.01 DystociaDocument7 pagesOB 1.01 DystociaDan Paolo Diña SolayaoNo ratings yet
- Proprioception - The Sense WithinDocument8 pagesProprioception - The Sense WithinMi AniNo ratings yet
- Maternal Test Questions 2Document7 pagesMaternal Test Questions 2dhodejun lizhaldeNo ratings yet
- Nursing Aptitude Test ReviewerDocument15 pagesNursing Aptitude Test ReviewerAngelie De100% (19)
- Nursing Practice IIDocument9 pagesNursing Practice IITiffanny BesaNo ratings yet
- Ob Long TestDocument13 pagesOb Long TestLordson Gem P. IbonNo ratings yet
- Maternal & Newborn Nursing ExamDocument3 pagesMaternal & Newborn Nursing ExamPaul Jhon Vergara88% (25)
- MCN Lab Practice QuestionsDocument8 pagesMCN Lab Practice QuestionsTrishaNo ratings yet
- 05.1 Obstructed Labor and Problems of The PassengerDocument16 pages05.1 Obstructed Labor and Problems of The PassengerJAN CAMILLE LENONNo ratings yet
- Obstetrics Test 1Document3 pagesObstetrics Test 1Errold Joseph LahaganNo ratings yet
- Maternal Newborn Nursing ExamDocument3 pagesMaternal Newborn Nursing Examrevathidadam55555No ratings yet
- Post Test FinalDocument1 pagePost Test FinalRudelyn BarcelonaNo ratings yet
- قبالةDocument88 pagesقبالةMostafa MahmoudNo ratings yet
- Maternal Notes Part IDocument21 pagesMaternal Notes Part Iabbycruz012No ratings yet
- Normal Labour QuizDocument2 pagesNormal Labour QuizAsh_myNo ratings yet
- Obstetrics 2.04 Abnormal Labor - Dr. Tongco PDFDocument14 pagesObstetrics 2.04 Abnormal Labor - Dr. Tongco PDFPreeti Joan BuxaniNo ratings yet
- OBDocument6 pagesOBbsn_cathNo ratings yet
- Obstetric NursingDocument2 pagesObstetric NursingKaren Joyce Costales Magtanong100% (1)
- 2024 Ob MaterialsDocument11 pages2024 Ob MaterialsJoshelle AndradeNo ratings yet
- Post TestDocument1 pagePost TestRudelyn BarcelonaNo ratings yet
- MCN ReviewerDocument3 pagesMCN ReviewerJunghoon YangParkNo ratings yet
- IBQs & MCQsDocument58 pagesIBQs & MCQsskNo ratings yet
- Comprehensive Ob Recall 2014Document3 pagesComprehensive Ob Recall 2014Rem AlfelorNo ratings yet
- Gyneacology Midterm 10th SemesterDocument3 pagesGyneacology Midterm 10th SemesterSyeda MunazzaNo ratings yet
- Physiologic OB Samplex CollectionDocument6 pagesPhysiologic OB Samplex CollectionChelsea13WpNo ratings yet
- MCN ReviewerDocument3 pagesMCN ReviewerJunghoon YangParkNo ratings yet
- Mid 104 ReqDocument3 pagesMid 104 ReqErika Mae RevadiloNo ratings yet
- Human - Anatomy and Physiology 2Document2 pagesHuman - Anatomy and Physiology 2Hermann CHEMEUHINo ratings yet
- NCM109 Labor and DeliveryDocument4 pagesNCM109 Labor and DeliveryRussel Kate SulangNo ratings yet
- NUR195 ADocument14 pagesNUR195 AJemuel DalanaNo ratings yet
- Scribd OB 4Document5 pagesScribd OB 4Ralph Tama Mangacop BenitoNo ratings yet
- (Documen T Title) : (Document Subtitle)Document24 pages(Documen T Title) : (Document Subtitle)Gebretsadik GebregergisNo ratings yet
- (PED) FINAL EXAM CarepackageDocument27 pages(PED) FINAL EXAM CarepackageMonique BorresNo ratings yet
- OB Mod 4 Review QuestionsDocument26 pagesOB Mod 4 Review QuestionsMohit AnjanaNo ratings yet
- Ob Finals Williams SamplexDocument86 pagesOb Finals Williams SamplexJustine MembridoNo ratings yet
- Module 4 - Activity 1Document3 pagesModule 4 - Activity 1sanji vinsmokeNo ratings yet
- Ortho - Lec - 2 - Fracture Fracture Healing and DislocationDocument17 pagesOrtho - Lec - 2 - Fracture Fracture Healing and DislocationMira AurumtinNo ratings yet
- MCHN Quiz PrelimsDocument4 pagesMCHN Quiz PrelimsRastie MendozaNo ratings yet
- Rnpedia MCN Pnle NaDocument30 pagesRnpedia MCN Pnle NaFrances Sofia DuranNo ratings yet
- Day 4 WK 2Document8 pagesDay 4 WK 2Sanielle Karla Garcia LorenzoNo ratings yet
- Operation Vaginal Delivery Accomplish byDocument4 pagesOperation Vaginal Delivery Accomplish byMiguel Cuevas DolotNo ratings yet
- Sample Questions-PediaDocument7 pagesSample Questions-PediaALCANTARA ALYANNANo ratings yet
- (ANA) 4.01 Abdomen in General - Dr. ElevazoDocument22 pages(ANA) 4.01 Abdomen in General - Dr. ElevazopasambalyrradjohndarNo ratings yet
- Maternal and Child Health Nursing Practice Questions With RationaleDocument29 pagesMaternal and Child Health Nursing Practice Questions With RationaleGabrielle G. MaldoNo ratings yet
- JUWAK - Jassim - Module 2 MAT ALTDocument2 pagesJUWAK - Jassim - Module 2 MAT ALTJASSIM JUWAKNo ratings yet
- كامل نساءDocument213 pagesكامل نساءniemand da100% (1)
- MCN Practice Exam - For Academic Use. - MCN SET KDocument1 pageMCN Practice Exam - For Academic Use. - MCN SET KNicholeGarcesCisnerosNo ratings yet
- ExamsDocument14 pagesExamssharon chuaNo ratings yet
- MID101 Final ExaminationDocument10 pagesMID101 Final ExaminationAldrin Riel BoyanoNo ratings yet
- MCN Drill Answers No AnswerDocument8 pagesMCN Drill Answers No AnswerShane Zia FabrosNo ratings yet
- Book CBSE-Class-12-Biology-Reproductive-Health-Practice-QuestionsDocument9 pagesBook CBSE-Class-12-Biology-Reproductive-Health-Practice-QuestionsVikramNo ratings yet
- Long QuizDocument3 pagesLong QuizChristine CayosaNo ratings yet
- MCN MT1 RefresherDocument7 pagesMCN MT1 RefresherRogerQuxNo ratings yet
- Physiology of Man in SpaceFrom EverandPhysiology of Man in SpaceJ. H. U. BrownNo ratings yet
- 06.1 High-Risk Postpartal ClientDocument22 pages06.1 High-Risk Postpartal ClientJAN CAMILLE LENONNo ratings yet
- 08 - LEC Family Nursing Care PlanDocument6 pages08 - LEC Family Nursing Care PlanJAN CAMILLE LENONNo ratings yet
- RAs PDFDocument1 pageRAs PDFJAN CAMILLE LENONNo ratings yet
- 07 Nursing Role in The Health of Ill Children and Their FamiliesDocument20 pages07 Nursing Role in The Health of Ill Children and Their FamiliesJAN CAMILLE LENONNo ratings yet
- 06.2 Care of Couples With Fertility ProblemsDocument9 pages06.2 Care of Couples With Fertility ProblemsJAN CAMILLE LENONNo ratings yet
- MCN ReviewDocument5 pagesMCN ReviewJAN CAMILLE LENONNo ratings yet
- 05.2 Problems of The PassageDocument5 pages05.2 Problems of The PassageJAN CAMILLE LENONNo ratings yet
- 02 First Trimester ConditionsDocument12 pages02 First Trimester ConditionsJAN CAMILLE LENONNo ratings yet
- 03 Second Trimester ConditionsDocument7 pages03 Second Trimester ConditionsJAN CAMILLE LENONNo ratings yet
- 06.1 High-Risk Postpartal ClientDocument22 pages06.1 High-Risk Postpartal ClientJAN CAMILLE LENONNo ratings yet
- 2554-Article Text-13960-1-10-20201220Document9 pages2554-Article Text-13960-1-10-20201220JAN CAMILLE LENONNo ratings yet
- 05.3 Problems of The Power and Psyche PDFDocument12 pages05.3 Problems of The Power and Psyche PDFJAN CAMILLE LENONNo ratings yet
- 01.1 High-Risk Prenatal ClientDocument18 pages01.1 High-Risk Prenatal ClientJAN CAMILLE LENONNo ratings yet
- 04 Third Trimester ConditionsDocument11 pages04 Third Trimester ConditionsJAN CAMILLE LENONNo ratings yet
- 2518-Article Text-13816-1-10-20201215Document6 pages2518-Article Text-13816-1-10-20201215JAN CAMILLE LENONNo ratings yet
- Level 2 - Prelim Exam Guidelines 2023Document2 pagesLevel 2 - Prelim Exam Guidelines 2023JAN CAMILLE LENONNo ratings yet
- 01.2 Pregestational ConditionsDocument27 pages01.2 Pregestational ConditionsJAN CAMILLE LENONNo ratings yet
- Requirements Level 2 OPDDocument5 pagesRequirements Level 2 OPDJAN CAMILLE LENONNo ratings yet
- 16NBSHemoglobinDisorders IJNS2021Document13 pages16NBSHemoglobinDisorders IJNS2021JAN CAMILLE LENONNo ratings yet
- Le3 Oia PDFDocument12 pagesLe3 Oia PDFJAN CAMILLE LENONNo ratings yet
- Oia Keisha PDFDocument7 pagesOia Keisha PDFJAN CAMILLE LENONNo ratings yet
- NCP Format 3Document3 pagesNCP Format 3JAN CAMILLE LENONNo ratings yet
- 12 Drugs Acting On The Cardiovascular SystemDocument5 pages12 Drugs Acting On The Cardiovascular SystemJAN CAMILLE LENONNo ratings yet
- 12 Drugs Acting On The Cardiovascular SystemDocument7 pages12 Drugs Acting On The Cardiovascular SystemJAN CAMILLE LENONNo ratings yet
- 07 - LEC Care of The NewbornDocument17 pages07 - LEC Care of The NewbornJAN CAMILLE LENONNo ratings yet
- Max FdarDocument3 pagesMax FdarJAN CAMILLE LENONNo ratings yet
- 05 - LEC The Family and Family HealthDocument5 pages05 - LEC The Family and Family HealthJAN CAMILLE LENONNo ratings yet
- 06 - LEC Family Nursing ProcessDocument10 pages06 - LEC Family Nursing ProcessJAN CAMILLE LENONNo ratings yet
- Ebj JBL DRDocument7 pagesEbj JBL DRJAN CAMILLE LENONNo ratings yet
- Daftar Harga Pemeriksaan Radiologi Rsud Awet Muda NarmadaDocument4 pagesDaftar Harga Pemeriksaan Radiologi Rsud Awet Muda NarmadaRADIOLOGI RSHKNo ratings yet
- Cury and França (2020) Brain SciencesDocument10 pagesCury and França (2020) Brain SciencesCarina FrançaNo ratings yet
- Hemophagocytic Lymphohistiocytosis (HLH)Document15 pagesHemophagocytic Lymphohistiocytosis (HLH)Amira ElawadyNo ratings yet
- Biology 30Document6 pagesBiology 30Marah AlsurkhyNo ratings yet
- Theories in ENTDocument9 pagesTheories in ENTKamal MishraNo ratings yet
- Age Effect On Orthodontic TreatmentDocument8 pagesAge Effect On Orthodontic Treatment63127No ratings yet
- Edgcse Aap Sb6a Starch TestDocument2 pagesEdgcse Aap Sb6a Starch TestHana JuiceNo ratings yet
- Gas Exchange in Human Body Exam Paper Question O/lDocument31 pagesGas Exchange in Human Body Exam Paper Question O/lSANDARU AKASH GURUSINGHENo ratings yet
- Pearson Edexcel International Gcse 9 1 Business Student Book 1St Edition Rob Jones Full Chapter PDF ScribdDocument67 pagesPearson Edexcel International Gcse 9 1 Business Student Book 1St Edition Rob Jones Full Chapter PDF Scribdmisty.mellis432100% (7)
- Human Digestive SystemDocument2 pagesHuman Digestive SystemshabeshabNo ratings yet
- CKD Case AnalysisDocument25 pagesCKD Case Analysisしゃいな ふかみNo ratings yet
- Pediatric Case StudyDocument21 pagesPediatric Case StudyJobelle AcenaNo ratings yet
- Male Reproductive PhysiologyDocument50 pagesMale Reproductive PhysiologyJOSHI RAJUNo ratings yet
- Basic Understanding of PBPK: Principles & Connection To The Broader Scope of Systems PharmacologyDocument28 pagesBasic Understanding of PBPK: Principles & Connection To The Broader Scope of Systems PharmacologyBenni IskandarNo ratings yet
- T1 Condicion Fisica 4º EsoDocument6 pagesT1 Condicion Fisica 4º EsoMartín Benítez del HoyoNo ratings yet
- Lab Protocol - Cell Image LibraryDocument36 pagesLab Protocol - Cell Image LibraryElizabeth RussellNo ratings yet
- Hematology India: QuestionsDocument22 pagesHematology India: QuestionsSelim TarekNo ratings yet
- Anatomy of Mitral ValveDocument6 pagesAnatomy of Mitral ValvesrhubanbabuNo ratings yet
- THERAULAZ Task Partitioning in A Ponerine Ant, DESPRODocument9 pagesTHERAULAZ Task Partitioning in A Ponerine Ant, DESPROMARIA FERNANDA RONDONNo ratings yet
- ANPH Midterm NotesDocument44 pagesANPH Midterm NotesClaudine Jo B. TalabocNo ratings yet
- Rick - And.morty.s05e04.1080p.webrip.x264 Cakes (Eztv - Re)Document40 pagesRick - And.morty.s05e04.1080p.webrip.x264 Cakes (Eztv - Re)Tomás CMNo ratings yet
- U3 - 02 (Cat Anatomy) PDFDocument2 pagesU3 - 02 (Cat Anatomy) PDFliclisheNo ratings yet
- 1 s2.0 S1569199321019652 MainDocument1 page1 s2.0 S1569199321019652 MainAnita DewiNo ratings yet
- Study of Sleep, Wake Pattern in Healthy Individuals With Reference To Different MizajDocument4 pagesStudy of Sleep, Wake Pattern in Healthy Individuals With Reference To Different MizajyusufNo ratings yet