Professional Documents
Culture Documents
Irritable Bowel Syndrome Prescribing Guidance
Uploaded by
tom8989Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Irritable Bowel Syndrome Prescribing Guidance
Uploaded by
tom8989Copyright:
Available Formats
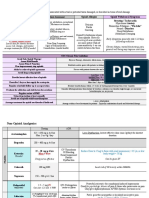
Treatment Options for Irritable Bowel Syndrome in Adults
Good communication, dietary and lifestyle advice: clear explanation and patient-centred discussion of IBS including:
• social/lifestyle factors: diet, exercise, sleep, and ingestion of caffeine, alcohol and other medication BDA IBS Food Fact Sheet
• psychological factors: presence of stress, anxiety, low mood and history of eating disorders
• biological factors: physiological abnormalities and medication side effects which are contributing to symptoms
1st Line Options 2nd Line Options
Antispasmodics - with dietary and lifestyle Antimotility Laxatives/soluble fibre
If laxatives, loperamide or
advice (Adjust to clinical response) (Adjust to clinical response)
antispasmodics have not helped,
consider tricyclic antidepressants as
1st Choice – Loperamide- licensed for Avoid lactulose, can worsen bloating 2nd Line.
1st Choice – hyoscine butylbromide 10mg to
20mg three times a day or peppermint oil symptomatic treatment of acute episodes of
The evidence for effectiveness of mebeverine or diarrhoea associated with IBS in adults.
Consider bulk forming laxatives,
alverine in IBS is weaker than for hyoscine increase dose gradually e.g. Fybogel® 1ST Choice – Tricyclic Antidepressants
butylbromide but may be better tolerated (TCA)
Caution: Colpermin® contains arachis oil Loperamide- dose of 4 mg initially, followed E.g. amitriptyline
Immediate release mebevrine is as effective as by 2 mg after every loose stool, up to a (Unlicensed indication)
Flatulence and bloating are the most
modified release and lower cost maximum of 12 mg per day, for diarrhoea-
common adverse effects of bulk-
predominant irritable bowel syndrome.
forming laxatives. They can usually be
Liquid preparation helpful to those
avoided or reduced by increasing the Start at a low dose e.g. 5mg to 10mg
Note: Antimuscarinics which reduce intestinal requiring low doses as they are very
dose of the laxative gradually every few amitriptyline, which should be taken
motility, such as hyoscine butylbromide and sensitive to the effects of loperamide
days until ONE or TWO soft formed once at night and reviewed regularly.
dicycloverine are poorly selective and are more Advise people to adjust the dose of
stools are produced every 1-2 days The dose may be increased but should
likely to cause antimuscarinic adverse effects (dry loperamide according to clinical response.
The aim is to produce a soft, well-formed not usually need to exceed 30 mg a day.
eyes and a dry mouth and can worsen
constipation) than direct-acting smooth muscle stool. An adequate fluid intake is important
relaxants or peppermint oil. to prevent intestinal obstruction. If TCAs have been shown to be
Dicycloverine is not recommended for Bulk-forming laxatives should not be ineffective, are contraindicated,
prescribing as it is poorly selective, more likely to Probiotics: if the patient wishes to try taken immediately before going to bed. or are not tolerated.
cause antimuscarinic adverse effects and there probiotics, advise them to choose and self-
are lower cost alternatives with relatively fewer purchase one brand and take the
adverse effects recommended dose for at least 4 weeks Consider adding or switching to
Macrogol compound oral powder 2nd Choice - Selective serotonin reuptake
Refer to the prescribing guidance on but discontinue if no benefit after 8 weeks
sachets or bisacodyl inhibitors (SSRIs) - Citalopram, fluoxetine,
anticholinergic drugs for advice on side effects
and paroxetine -unlicensed indication.
Patients with IBS-C (IBS with Constipation) that have failed a SIX month trial of at least two laxatives from different classes at
optimal/maximum tolerated doses may be suitable for a trial of linaclotide – refer to gastroenterology via CRS with a full laxative ▪ Citalopram: 10 mg to 20 mg daily.
history for the specialist to initiate a trial. ▪ Fluoxetine: 20 mg daily.
If beneficial, Specialist will recommend in writing to the GP to continue the prescribing ▪ Paroxetine: 10 mg to 20 mg daily
Produced by PMOT, WECCG and updated in collaboration with the Gastroenterology department at PAH Approved by MOPB December 2019, updated April 2022, review April 2025 or before if new guidance is published
You might also like
- The Presidential ScandalsDocument328 pagesThe Presidential ScandalsDr Nasser AfifyNo ratings yet
- A compilation of anabolic and nutritionnal supplementsFrom EverandA compilation of anabolic and nutritionnal supplementsRating: 5 out of 5 stars5/5 (1)
- Ebook Fulfilling Destiny As Demanded by GodDocument94 pagesEbook Fulfilling Destiny As Demanded by GodIfeanyi OmeiheakuNo ratings yet
- MetoclopramideDocument1 pageMetoclopramideIvanne Hisoler89% (27)
- Methyldopa Drug StudyDocument2 pagesMethyldopa Drug StudyBea Dela Cena100% (1)
- Drug StudyDocument21 pagesDrug StudyLeya ThaobunyuenNo ratings yet
- Chapter VIII Drug StudyDocument21 pagesChapter VIII Drug StudyDylan Angelo AndresNo ratings yet
- Icivics MontesquieuDocument3 pagesIcivics Montesquieuapi-32806152578% (9)
- Bago Project CharterDocument6 pagesBago Project CharterLarize BautistaNo ratings yet
- Midazolam Drug Study SaclotDocument1 pageMidazolam Drug Study SaclotMaybelle Cababat SaclotNo ratings yet
- Alien Cicatrix II (Part 02 of 03) - The CloningDocument4 pagesAlien Cicatrix II (Part 02 of 03) - The CloningC.O.M.A research -stopalienabduction-No ratings yet
- Financial Management - Risk and Return Assignment 2 - Abdullah Bin Amir - Section ADocument3 pagesFinancial Management - Risk and Return Assignment 2 - Abdullah Bin Amir - Section AAbdullah AmirNo ratings yet
- Chairperson 2012 Bar Examinations Committee: Bar Exam Question 2012 Martin S. Villarama, JRDocument73 pagesChairperson 2012 Bar Examinations Committee: Bar Exam Question 2012 Martin S. Villarama, JRsejinma0% (1)
- Midazolam Drug Study SaclotDocument1 pageMidazolam Drug Study SaclotMaybelle Cababat Saclot100% (1)
- Buscopan Drug StudyDocument3 pagesBuscopan Drug StudyMarc BantilanNo ratings yet
- Laxative Guidelines Nov 2013Document2 pagesLaxative Guidelines Nov 2013Purim KTshipNo ratings yet
- Drug StudyDocument3 pagesDrug StudyAlyssa Marie PepitoNo ratings yet
- Drug StudyDocument2 pagesDrug StudyAlyssa Marie PepitoNo ratings yet
- GI Topic SummaryDocument16 pagesGI Topic SummaryShingie MatemaNo ratings yet
- Drug Study AssignmentDocument1 pageDrug Study AssignmentDaniela Claire FranciscoNo ratings yet
- Drug Study AssignmentDocument1 pageDrug Study AssignmentDaniela Claire FranciscoNo ratings yet
- Drug NamesDocument7 pagesDrug Namestom10carandangNo ratings yet
- Laxative Treatment Guideline For AdultsDocument7 pagesLaxative Treatment Guideline For AdultsPurim KTshipNo ratings yet
- Appendix 12 Laxative Guidelines For AdultsDocument2 pagesAppendix 12 Laxative Guidelines For AdultsSha FiraNo ratings yet
- Drug Name Dosage, Route, Frequency Mechanis MOF Action Indications Contraindication S Adverse Effects Nursing ResponsibilitiesDocument4 pagesDrug Name Dosage, Route, Frequency Mechanis MOF Action Indications Contraindication S Adverse Effects Nursing ResponsibilitiesJonna Mae TurquezaNo ratings yet
- BRONCODILATADORESDocument6 pagesBRONCODILATADORESXiomara CardonaNo ratings yet
- Daat 07 I 2 P 144Document3 pagesDaat 07 I 2 P 144amit2352842No ratings yet
- Gerd HTP Bn3aDocument4 pagesGerd HTP Bn3aKristil ChavezNo ratings yet
- E.-Drug-Study-Report BevDocument2 pagesE.-Drug-Study-Report BevPatricia Jean FaeldoneaNo ratings yet
- Repitol: 105x148mm 105x148mmDocument1 pageRepitol: 105x148mm 105x148mmMohammad ImranNo ratings yet
- Durg Profile 6396Document7 pagesDurg Profile 6396MUHAMMAD ZOHAIBNo ratings yet
- Opioid-BenzosTapering FlowchartDocument1 pageOpioid-BenzosTapering FlowchartjuanchibarberoismNo ratings yet
- DiazepamDocument2 pagesDiazepamBIRIN, JEHAN KAYLE T.No ratings yet
- Drug Study 1 (Done)Document3 pagesDrug Study 1 (Done)Otaku MiyoNo ratings yet
- Primary Care Constipation Guidelines: Version 1.1 - December 2016Document5 pagesPrimary Care Constipation Guidelines: Version 1.1 - December 2016Budi WicaksonoNo ratings yet
- Drug Study 5Document4 pagesDrug Study 5Butts McgeeNo ratings yet
- Drug StudyDocument8 pagesDrug Studyzhapper2002No ratings yet
- Forcadilla - Drug Study orDocument31 pagesForcadilla - Drug Study orKeir Mrls ForcadillaNo ratings yet
- CaseStudy DengueDocument16 pagesCaseStudy DenguexxandraNo ratings yet
- Anxiolytic DrugDocument3 pagesAnxiolytic DrugAnna Mendiola-BasbasNo ratings yet
- Guia de ConstipacionDocument5 pagesGuia de ConstipacionWalter Barriga ManriqueNo ratings yet
- Chapter 12 GastrointestinalDocument11 pagesChapter 12 GastrointestinalRaju NiraulaNo ratings yet
- HTP - Substance Induced PsychosisDocument4 pagesHTP - Substance Induced PsychosisCarla Tongson MaravillaNo ratings yet
- Drug StudyDocument6 pagesDrug StudyLovelyNo ratings yet
- Drug Study: Drug Classificati ON Mechanism of Action Rationale Common Side Effects Nursing ConsiderationDocument5 pagesDrug Study: Drug Classificati ON Mechanism of Action Rationale Common Side Effects Nursing ConsiderationMaye ArugayNo ratings yet
- Common Medications Used in Paediatrics: AntipyreticsDocument7 pagesCommon Medications Used in Paediatrics: AntipyreticslukesqueNo ratings yet
- Observe Patient's 10 Rights of Medication AdministrationDocument2 pagesObserve Patient's 10 Rights of Medication AdministrationRyan Paul BalotNo ratings yet
- Risperidone (Aspidon OS)Document8 pagesRisperidone (Aspidon OS)Khristle DavidNo ratings yet
- Medical & Surgical Management in Cerebral PalsyDocument13 pagesMedical & Surgical Management in Cerebral PalsySahil SahniNo ratings yet
- Drug Study (Flagyl)Document3 pagesDrug Study (Flagyl)ELyssa Anne Maristelle DizonNo ratings yet
- Pharma Revision FileDocument21 pagesPharma Revision Filemaxwell amponsahNo ratings yet
- Pain - Opioids Combined PDFDocument26 pagesPain - Opioids Combined PDFJenna DantNo ratings yet
- Unit 4 - Emergency Drugs - Table FormDocument5 pagesUnit 4 - Emergency Drugs - Table FormTESORO Zeus DavidNo ratings yet
- Drug Study: Meclizine Is An Antagonist atDocument2 pagesDrug Study: Meclizine Is An Antagonist atJayson Ray AbellarNo ratings yet
- DexamethasoneDocument1 pageDexamethasoneACOB, Jamil C.No ratings yet
- Drug Study - FurosemideDocument2 pagesDrug Study - FurosemideryanNo ratings yet
- Psych Drug Study Xxx.Document5 pagesPsych Drug Study Xxx.Danica Kate GalleonNo ratings yet
- OSCE Common Drugs To Explain (Oscestop) - UnlockedDocument2 pagesOSCE Common Drugs To Explain (Oscestop) - Unlockedhannahkim55No ratings yet
- Suppositories Vaginal Suppositories: Dosage FormsDocument5 pagesSuppositories Vaginal Suppositories: Dosage FormsRye M. BirungNo ratings yet
- 2016 - OSEP ReviewerDocument4 pages2016 - OSEP ReviewerCRUZ Jill EraNo ratings yet
- DRUG. Clorphromazine and ClonazepamDocument3 pagesDRUG. Clorphromazine and ClonazepamEzron Kenneth DuranNo ratings yet
- SANGKULA Drug-Study-FormatDocument3 pagesSANGKULA Drug-Study-FormatAnonymous p0DPE1eNo ratings yet
- Medication Administration WorksheetDocument6 pagesMedication Administration WorksheetCheska CarrionNo ratings yet
- Antihistamines DSDocument2 pagesAntihistamines DSTamara Jael AspirasNo ratings yet
- Drug Study CNS StimulantsDocument10 pagesDrug Study CNS StimulantsJames Emman ClementeNo ratings yet
- V. Implementation Management A. MedicationsDocument3 pagesV. Implementation Management A. MedicationsSid Artemis FriasNo ratings yet
- Application Form SiloDocument8 pagesApplication Form Silotom8989No ratings yet
- Anal Fissure ChronicDocument17 pagesAnal Fissure Chronictom8989No ratings yet
- ASCIA Acute Management of Anaphylaxis Guidelines 2015Document4 pagesASCIA Acute Management of Anaphylaxis Guidelines 2015tom8989No ratings yet
- Lampiran 1 (Jadwal Penelitian)Document2 pagesLampiran 1 (Jadwal Penelitian)tom8989No ratings yet
- Reported Speech Rd1Document3 pagesReported Speech Rd1Jose ChavezNo ratings yet
- Whats New PDFDocument74 pagesWhats New PDFDe Raghu Veer KNo ratings yet
- Code of Conduct of Dabur Company - 1Document5 pagesCode of Conduct of Dabur Company - 1Disha KothariNo ratings yet
- Demonstration MethodDocument16 pagesDemonstration Methodfrankie aguirreNo ratings yet
- Research Design1 USED 6Document14 pagesResearch Design1 USED 6Joselle RuizNo ratings yet
- Current Technique in The Audiologic Evaluation of Infants: Todd B. Sauter, M.A., CCC-ADocument35 pagesCurrent Technique in The Audiologic Evaluation of Infants: Todd B. Sauter, M.A., CCC-AGoesti YudistiraNo ratings yet
- The Divine Liturgy Syro Malankara ChurchDocument4 pagesThe Divine Liturgy Syro Malankara ChurchGian Marco TallutoNo ratings yet
- Why We're Still Learning New Things About The JFK AssassinationDocument8 pagesWhy We're Still Learning New Things About The JFK AssassinationNolan SNo ratings yet
- Making Effective Pres. Academic Lit I. Weeks 4 5Document27 pagesMaking Effective Pres. Academic Lit I. Weeks 4 5irfanaNo ratings yet
- B.a.H Eco. 2nd Semester Mathematical Methods For Economics IIDocument3 pagesB.a.H Eco. 2nd Semester Mathematical Methods For Economics IINitinSharma100% (1)
- Compilation 2Document28 pagesCompilation 2Smit KhambholjaNo ratings yet
- (OCM) Chapter 1 Principles of ManagementDocument23 pages(OCM) Chapter 1 Principles of ManagementMehfooz PathanNo ratings yet
- Quiz Simple Present Simple For Elementary To Pre-IntermediateDocument2 pagesQuiz Simple Present Simple For Elementary To Pre-IntermediateLoreinNo ratings yet
- Maria Da Piedade Ferreira - Embodied Emotions - Observations and Experiments in Architecture and Corporeality - Chapter 11Document21 pagesMaria Da Piedade Ferreira - Embodied Emotions - Observations and Experiments in Architecture and Corporeality - Chapter 11Maria Da Piedade FerreiraNo ratings yet
- PracticeProbs (5 - 27 - 07) - CMOS Analog ICs PDFDocument70 pagesPracticeProbs (5 - 27 - 07) - CMOS Analog ICs PDFmyluvahanNo ratings yet
- Introduction To Financial Management: Topic 1Document85 pagesIntroduction To Financial Management: Topic 1靳雪娇No ratings yet
- Brief Orientation To Counseling 1st Edition Neukrug Test BankDocument25 pagesBrief Orientation To Counseling 1st Edition Neukrug Test BankStevenAdkinsyjmd100% (55)
- 3 Murex HIV Ag Ab CombinationDocument7 pages3 Murex HIV Ag Ab CombinationElias Dii Rivas GarvanNo ratings yet
- Firewatch in The History of Walking SimsDocument5 pagesFirewatch in The History of Walking SimsZarahbeth Claire G. ArcederaNo ratings yet
- Numerical Analysis: Prof. Dr. Süheyla ÇEHRELİDocument15 pagesNumerical Analysis: Prof. Dr. Süheyla ÇEHRELİEzgi GeyikNo ratings yet
- The University of Southern Mindanao VisionDocument9 pagesThe University of Southern Mindanao VisionNorhainie GuimbalananNo ratings yet
- How To Live A Healthy LifestyleDocument2 pagesHow To Live A Healthy LifestyleJocelynNo ratings yet
- SDS SheetDocument8 pagesSDS SheetΠΑΝΑΓΙΩΤΗΣΠΑΝΑΓΟΣNo ratings yet