Professional Documents
Culture Documents
CNS Genetic Syndromes
Uploaded by
Ahmed H. Ali ElbestaweyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CNS Genetic Syndromes
Uploaded by
Ahmed H. Ali ElbestaweyCopyright:
Available Formats
Van den Veyver Ignatia B.
(Orcid ID: 0000-0002-0651-5924)
Prenatally diagnosed developmental abnormalities of the central nervous system and
genetic syndromes: a practical review.
Ignatia B. Van den Veyver, M.D.1
Affiliation: Department of Obstetrics and Gynecology, Baylor college of Medicine, Houston
TX
Running title: Prenatally diagnosed CNS defects and genetic syndromes.
1Corresponding author:
Ignatia B. Van den Veyver, M.D.
Department of Obstetrics and Gynecology
Baylor College of Medicine
Duncan Neurological Research Institute at Texas Children’s Hospital
1250 Moursund Street, Room DNRI 1025.14
Houston, TX 77030
Phone: (832) 824 8125
Fax: (832) 825 1271
email: iveyver@bcm.edu
Conflict of interest statement: No conflict of interest related to the contents of this
manuscript.
Funding: No grant support for this manuscript.
Word count: 6325
Table count: 2
Figure count: 3
What is already known about this topic?
Developmental brain abnormalities are complex, difficult to diagnose prenatally and
etiologically diverse
Genomic technologies such as chromosomal microarray (CMA) and genome
sequencing are rapidly expanding knowledge of genetic causes for brain abnormalities
What does this study add?
Review of how ultrasound and MRI benefit prenatal diagnosis of brain abnormalities
Review of detection rates by CMA and sequencing for different classes of brain
abnormalities
Highlights classes of genes typically associated with different brain abnormalities
Data availability statement: Research data not shared
This article has been accepted for publication and undergone full peer review but has not been
through the copyediting, typesetting, pagination and proofreading process which may lead to
differences between this version and the Version of Record. Please cite this article as doi:
10.1002/pd.5520
This article is protected by copyright. All rights reserved.
Abstract
Developmental brain abnormalities are complex and can be difficult to diagnose by prenatal
imaging because of the ongoing growth and development of the brain throughout pregnancy
and the resolution limitations of ultrasound, often requiring fetal magnetic resonance imaging
as an additional tool. As for all major structural congenital anomalies, amniocentesis with
chromosomal microarray and a karyotype is the first-line recommended test for the genetic
work-up of prenatally diagnosed central nervous system (CNS) abnormalities. Many CNS
defects, especially neuronal migration defects affecting the cerebral and cerebellar cortex, are
caused by single gene mutations in a large number of different genes. Early data suggest that
prenatal diagnostic exome sequencing for fetal CNS defects will have a high diagnostic yield,
but interpretation of sequencing results can be complex. Yet, a genetic diagnosis is important
for prognosis prediction and recurrence risk counseling. The evaluation and management of
such patients is best done in a multidisciplinary team approach. Here we review general
principles of the genetic work-up for fetuses with CNS defects and review categories of
genetic causes of prenatally diagnosed CNS phenotypes.
Key-words: fetal brain – prenatal ultrasound – prenatal magnetic resonance imaging (MRI) –
genetic syndrome – chromosomal microarray – single gene disorder – neuronal migration –
macrocephaly – microcephaly – posterior fossa – corpus callosum.
Acknowledgements: The author acknowledges the contributions of Dr. Magdalena Sanz
Cortes, Dr. Christopher Cassady, and Dr. Wesley Lee for ultrasound and MRI images used in
figures.
This article is protected by copyright. All rights reserved.
Introduction
Structural malformations of the brain have a prevalence at birth of 1-2:1,0001, or
potentially higher with newer imaging technologies2. Development and growth of the brain
and other parts of the central nervous system (CNS) is not completed until after birth. Major
brain structures are identifiable by the end of the first trimester3, allowing for early detection
of major abnormalities, such as acrania, exencephaly, anencephaly or holoprosencephaly3,4.
In contrast, defects of brain growth and differentiation are often not identified until later in
the pregnancy, mostly after 20-22 weeks, because the affected structures have not yet fully
developed before that stage5. These phenotypes also evolve throughout gestation and may not
be apparent until late second or early third trimester. Thus, prenatal diagnosis of CNS
abnormalities requires solid knowledge of CNS embryology and development and of the
limits of imaging at different gestational ages for accurate interpretation of findings on
screening prenatal ultrasound, dedicated fetal neurosonography, or fetal magnetic resonance
imaging (MRI). Although a detailed overview of CNS embryology, growth and
differentiation in perspective of prenatal imaging is beyond the scope of this review and can
be found elsewhere3,5,6, we will highlight relevant general concepts in the description of
specific categories of CNS abnormalities.
With the increasing use of new genomic technologies, including chromosomal
microarray (CMA)7-10 or next generation sequencing for gene-panel tests and whole genome
or exome sequencing (WES, WGS)11-16, new genes that cause syndromes and birth defects,
especially those involving the brain, are uncovered at an unprecedented pace17,18.
Thus, counseling about causes, associated syndromes, prediction of the prognosis for
neurodevelopment and function, seizures, and recurrence risk of structural brain
abnormalities is complex. Women with affected pregnancies are best cared for by a
multidisciplinary team (Table 1) with close communication between the primary prenatal
This article is protected by copyright. All rights reserved.
care providers, maternal-fetal medicine specialists, sonographers and radiologists, prenatal
and pediatric genetics professionals, neonatologists, pediatric neurologists and neurosurgeons
with expertise in fetal medicine, other subspecialists as needed, and social workers that
support the families. For the most severe defects with anticipated life-threatening
complications in the newborn, consultation with an experienced palliative care team (at our
institution referred to as the perinatal pediatric advanced care team or PPACT) helps guide
patients with decision making about neonatal management. Clinical prenatal geneticists and
genetic counselors play a crucial role in this multidisciplinary team. They guide the genetic
evaluation, direct the choice of the most appropriate genetic testing strategy, and counsel
prospective parents about possible or confirmed presence of a genetic syndrome in their fetus.
Genetic counselors also help families cope with uncertainty, prepare for poor prognosis,
connect with support groups, and inform about resources for early interventions and
treatments that improve life quality or outcomes.
In this review, we first provide a general overview of genetic etiologies and testing
strategies for prenatally identified developmental brain malformations. We then review
specific classes of CNS defects with their currently known most common genetic etiologies.
Because it is not possible to provide an all-encompassing overview that describes each
possible defect, we focus on broad categories and highlight the more commonly identified
conditions.
This article is protected by copyright. All rights reserved.
Detection of aneuploidies, copy number gains and losses, and single gene defects with
prenatally diagnosed structural CNS abnormalities
Numerical and structural chromosomal abnormalities
Trisomy 13 and trisomy 18 are the most common aneuploidies found when there are
structural brain abnormalities, but other aneuploidies and structural chromosomal
abnormalities also commonly present with CNS defects19. CMA is now a well-established
genetic diagnostic tool and is the recommended first-line genetic test for fetal structural
abnormalities. CMA identifies clinically significant copy number losses (deletions) or gains
(duplications) in 6-7% of pregnancies with fetal anomalies and a normal karyotype8,20. A
meta-analysis published in 2014 on over 3300 reported cases found a pooled prevalence of
pathogenic or likely pathogenic copy number variants (CNVs) of 6.8% overall and 6.2%
(35/563 cases) for CNS defects7. Shaffer et al reported in 2012 that CMA revealed a
significant finding in 8.6% of cases with CNS defects and that within that group, the highest
yield was when there were abnormalities in other organ systems (11%), in particular if there
were abnormalities of the posterior fossa and cerebellum (13.8%-19.6%), holoprosencephaly
(10.6%) or agenesis of the corpus callosum, while spinal abnormalities had the lowest
detection rate of 3.8%)9.
Single gene defects
Based on the above detection rates, women are best offered a diagnostic procedure
(most commonly an amniocentesis) with as recommended first-line test a CMA, to which
some add a karyotype to detect rare instances of balanced rearrangements or clarify the
cytogenetic origin of trisomies or location of copy number gains, as a first step to find a
genetic cause for fetal brain abnormalities identified by prenatal imaging. For certain specific
CNS defects, there is a high likelihood that a single gene defects are the underlying cause,
This article is protected by copyright. All rights reserved.
which may justify including a gene sequencing test early in the diagnostic work-up. This can
be a gene panel that contains from a few to hundreds of genes known to be associated with
specific categories of defects. These have the advantage of favorable cost and a lower
likelihood of detecting sequence variants of uncertain significance. The disadvantages are
that panel content may not be up to date with the newest disease gene discoveries because
they are typically developed based on information on disease genes for conditions that
present after birth and not optimized for prenatal presentations. A potentially more
successful strategy that we favor is genome-wide sequencing, such as diagnostic exome
sequencing, which has already shown benefit for prenatal cases with CNS abnormalities, but
full investigation of the clinical utility and their place in prenatal genetic testing is still
underway11,13,21-24.
Common prenatally diagnosed CNS defects
Choroid plexus cysts
Single or multiple choroid plexus cysts (CPCs) (Figure 1A) are present in 1-2% of all
pregnancies and among the most common findings on prenatal ultrasound of the brain in the
second trimester25. CPCs have been extensively studied because of their association with
aneuploidy, in particular trisomy 18. Although 40-50% of fetuses with trisomy 18 have
CPCs, they are not by themselves, without any other structural fetal anomalies, predictive of
trisomy 18 and can be present in many pregnancies with a normal outcome25-27. Other severe
syndromes with abnormal brain development can also present with CPCs, for example
Aicardi syndrome, but those typically have other identifiable CNS abnormalities28. Thus,
when isolated CPCs are found, counseling can be reassuring that the prognosis is favorable29.
It is helpful to include an explanation that CPCs form in non-neuronal tissues inside the
ventricles and are unlikely to impact future neurocognitive development.
This article is protected by copyright. All rights reserved.
Neural tube defects
Depending on geographic location, approximately 0.2 – 10:1000 infants are born with
neural tube defects (NTDs)30,31 (Figure 1B-E). Of the NTDs detectable during pregnancy
40% are anencephaly, 50% myelomeningocele (MMC; spina bifida), 3% craniorachischis,
and 7% encephalocele31. The majority of NTDs are of multifactorial etiology, with evidence
for a gene-environment interaction and their incidence is lowered by increasing folic acid
intake6,32,33. A subset of NTDs have a specific genetic etiology and can be a features of a
known genetic syndrome. Ten percent of myelomeningocele cases overall and 25% when
other structural anomalies are present have chromosomal abnormalities. In addition, 3.6% of
patients with spina bifida have a significant CNV detected by CMA and an estimated 1%
with myelomeningocele have a genetic syndrome. Chromosomal abnormalities are found in
0.6-5% of anencephaly cases and in 6.5% of encephalocele cases. About 25% of fetuses with
encephaloceles have extra-CNS structural abnormalities, in particular polydactyly and renal
abnormalities. This combination of findings is highly suggestive of a genetic syndrome, in
particular Meckel-Gruber syndrome and related disorders, caused by predominantly
autosomal recessive mutations in a growing number of genes, including MKS1, TMEM67,
TMEM216, RPGRIP1L, CEP290, CC2D2A, TCTN2 31,32. Obtaining a genetic diagnosis for
these is important for counseling about recurrence risk and diagnostic options for future
pregnancies.
Ventriculomegaly and hydrocephalus
Ventriculomegaly and hydrocephalus, affecting 0.4-1:1000 liveborns, are common
abnormalities detected on prenatal ultrasound34 (Figure 1F-H). Ventriculomegaly can be
primary, due to an inherent developmental abnormality, or secondary, resulting from
environmental insults, such as prenatal infections (e.g. cytomegalovirus). The developmental
This article is protected by copyright. All rights reserved.
prognosis depends on the size and symmetry of the ventricles and the presence of associated
abnormalities. Symmetrical ventriculomegaly has a higher incidence of associated
abnormalities (39% vs. 24%) than asymmetrical ventriculomegaly35. Ventriculomegaly can
be obstructive or non-obstructive and is divided into mild, moderate and severe, based on the
measurements of the lateral ventricle at the level of the antrum36,37. The risk for associated
CNS or non-CNS abnormalities is 10-40% with mild ventriculomegaly (10-12 mm) and 58-
78% with moderate (12.1 – 15 mm) and severe ventriculomegaly (>15 mm)37-39. Mild
ventriculomegaly in the second trimester is a well-known soft marker for Down syndrome
and an average of 2.7% of fetuses with isolated mild ventriculomegaly have chromosomal
abnormalities37. This increases to 14.2% with moderate and 17.4% with severe
ventriculomegaly38. Up to 7.6% of cases of ventriculomegaly with a normal karyotype have a
clinically significant CNV detected on CMA9.
The developmental prognosis for isolated ventriculomegaly is usually good, with no
neurological deficit in 78-100% of described cases, but studies on long-term outcomes
assessing for milder neurobehavioral problems are limited34,37,40,41. In severe obstructive
hydrocephalus, brain damage due to pressure affects prognosis, which can be difficult to
predict prenatally. When ventriculomegaly is a secondary sign of syndromes with
developmental abnormalities of neuronal migration (described below), the prognosis depends
on the underlying condition37.
Five to ten percent of male fetuses with nonsyndromic congenital hydrocephalus have
X-linked aqueductal stenosis due to mutations in the L1CAM gene in Xq28, the most
common genetic form of hydrocephalus (1:30,000)42. One recent study on 138 male fetuses
with severe hydrocephalus showed that 41% have mutations in L1CAM43; conversely, 90% of
males with L1CAM mutations have aqueductal stenosis. Adducted thumbs are present in >50-
88% and agenesis of the corpus callosum in 68%42,43. A distinct feature is pyramidal tract
This article is protected by copyright. All rights reserved.
hypoplasia42, which could be detectable on MRI tractography. Seven percent of L1CAM
mutations are de novo and the majority of affected males are simplex cases. In inherited
cases, >95% of carrier women are asymptomatic but they have a 50% chance of affected
male offspring.
Midline defects: Abnormalities of the corpus callosum and cavum septum pellucidum
Midline brain abnormalities are commonly diagnosed prenatally. Agenesis of the
corpus callosum (ACC) can be complete or partial and is found in up to 0.03-0.07% of
second trimester ultrasounds38,44 (Figure 1I-K). It affects 1.8/10,000 overall, but the
incidence of ACC is significantly higher in children with neurodevelopmental delay (2-3%)
and it is often part of a syndrome45-47. Prenatal diagnosis of ACC can be difficult and is often
delayed until after 20 weeks of gestation because the corpus callosum is not formed before
18-20 weeks46, but early signs, including absence of the cavum septum pellucidum, abnormal
course of the pericallosal artery and colpocephaly of the lateral ventricles can raise suspicion
for ACC44,46-48. When ACC is detected, it is important to search for other CNS and non-CNS
abnormalities. Isolated ACC has a favorable (although uncertain) prognosis with normal
intelligence but predisposition to learning and social deficits in 70-80% and
neurodevelopmental delay 20-30%, of which 12% is severe in some series49,50. Other CNS
abnormalities are present in ~50%-85% depending on the study, and extra-CNS abnormalities
are present in 65%47,49. When other abnormalities are present, there is a risk of 17% for
chromosomal abnormalities, but it is lower in isolated ACC. Furthermore, other CNS
abnormalities can be missed prenatally in up to 20% of cases44,49. The risk for significant
CNVs detected by CMA in a large postnatal series of patients with ACC is 7-9%, including
in “ACC-only” cases51. ACC is a component of one of >200 different genetic syndromes. It
has been associated with metabolic disorders such as pyruvate dehydrogenase or fumarase
This article is protected by copyright. All rights reserved.
deficiency, Smith–Lemli–Opitz syndrome, and several others. Some of the more common
syndromes with ACC (with causative genes listed in parentheses), are Aicardi syndrome
(unknown genetic etiology), Mowat-Wilson syndrome (ZEB2), acrocallosal syndrome
(KIF7), ATRX-related disorders (ATRX), Opitz G syndrome (MID1), L1-related disorders
including Mental retardation Adducted thumbs, Shuffling gait, Ataxia (MASA) and X-linked
hydrocephalus with aqueductal stenosis (L1CAM; see also above)45,47,52. Other causes can be
environmental, such as alcohol, other teratogen exposure, and congenital infections 45,52.
The cavum septum pellucidum (CSP) is visible as early as 15 weeks and should be
seen between 18 and 37 weeks, after which it begins to narrow5,53. Absent CSP is rare and
usually an early sign of other midline forebrain anomalies, such as holoprosencephaly and
ACC, but it can be a normal variant with good prognosis48,53-55. If the CSP is not seen by 18-
20 weeks’ gestation, further evaluation, including MRI, is indicated to search for other brain
abnormalities53 that may indicate the presence of a genetic syndrome. When frontal horns are
small, partial or complete ACC with or without other migrational abnormalities can be
present. When frontal horns are normal and there is a corpus callosum, it could indicate
septo-optic dysplasia (SOD), better referred to as hypoplastic optic nerve syndrome54,55. This
constellation of abnormalities includes hypoplastic optic nerve, which may require postnatal
ophthalmologic exam for confirmation, abnormalities of the hypothalamic-pituitary axis, and
in some, agenesis of the corpus callosum and schizencephaly53,54. Genetic abnormalities are
found in only 1% of cases, but mutations in HESX1, SOX1, SOX2 (with severe eye defects
and other anomalies), SOX3, OTOX2, and FGF8 have all been implicated56. The significance
of an enlarged (>10 mm) CSP is controversial, but it can be a sign of a CSP cyst and
associated with other findings, including chromosomal abnormalities5,54,57.
This article is protected by copyright. All rights reserved.
Midline defects: Holoprosencephaly
Holoprosencephaly (HPE) (Figure 1L,M) affects 1:250 conceptuses58,59, but is much
rarer (0.4-1.2/10,000) in live births because the majority of fetuses with HPE do not survive
the pregnancy52,60. The most severe form alobar HPE (40% of HPE) is associated with high
early lethality. The milder semi-lobar (43%) and lobar (17%) HPE as well as the rarer
interhemispheric and septo-preoptic variants are challenging to diagnose prenatally. Eighty
percent of fetuses with HPE have other anomalies, of which 80% are facial defects. Other
associated brain abnormalities include absent CSP, ACC, pituitary hypoplasia, neuronal
migration abnormalities and hydrocephalus56,59,61. The facial defects range from
hypotelorism, cleft lip and palate, single nostril, proboscis, to cyclopia and anophthalmia56,59.
Other extracranial abnormalities are present in 46% and depend on the etiology52. They
include urogenital anomalies (24%), postaxial polydactyly (8%), vertebral defects (5%), limb
reduction defects (4%), and transposition of great arteries (4%)59. HPE can be caused by
genetic or environmental factors. Environmental causes include teratogens, such as alcohol,
retinoic acids and maternal diabetes, which carries a 1% risk for HPE. Between 20-50% of
HPE are caused by chromosomal abnormalities56,60 of which 75% are trisomy 13 and others
include triploidy (20%) and trisomy 18 (1-2%)52. Trisomy 13 is the most likely differential
diagnosis when HPE is detected prenatally and other structural abnormalities are present52.
When the karyotype is normal, structural chromosomal abnormalities that can involve
multiple loci containing candidate genes for HPE are found in >10%9,62. In addition to
chromosomal abnormalities, genetic syndromes are the cause of 18-25% of HPE52,56, of
which 10% are related to abnormalities of cholesterol biosynthesis. The most common among
these is Smith-Lemli-Opitz syndrome (SLOS), a common autosomal recessive disease (birth
prevalence of 1:20,000-1:40,000) of variable severity, caused by mutations in DHCR7, the
gene that encodes 7-dehydrocholesterol reductase. Features of SLOS include fetal growth
This article is protected by copyright. All rights reserved.
restriction, microcephaly, occasionally HPE, cleft palate, cardiac defects, hypospadias or
ambiguous genitalia in males, 2-3 syndactyly of the toes, postaxial polydactyly, distinctive
facial features, and the potential for severe neurodevelopmental disability 63. Recently,
expanded carrier screening has revealed a higher carrier frequency for DHCR7 mutations
than previously ascertained, suggesting that there may be high early prenatal lethality of
affected fetuses64. Other syndromes associated with holoprosencephaly include Pallister-Hall
syndrome, Meckel syndrome, Rubinstein-Taybi syndrome, pseudotrisomy 13, and severe
presentations of 22q11.2 deletion syndrome52,56,61. Some forms of isolated HPE have been
linked to dominant mutations with reduced penetrance in single genes52. The most common
one is SHH, which is mutated in 40% of familial and <5% of sporadic cases. Others include
ZIC2, SIX3, and TGIF1, in 5%, 1.3% and 1.3% of familial cases respectively, and more rarely
GLI2, PTCH1, DISP1, FGF8, FOXH1, NODAL, TDGF1, GAS1, DLL1 and CDON56. The
clinical findings in familial cases can be subtle, such as a single incisor in apparently
unaffected family members. Thus, examining parents is helpful for recurrence risk
counseling. This phenotypic variability has led to a “multiple genetic hit” proposal with
digenic inheritance in some cases65.
Malformations of cortical development
Development of the cerebral cortex and cortical malformations.
New neurons of the developing cortex proliferate in the ventricular zone, then divide
asymmetrically and migrate in an inward-out pattern to populate the cortex where they
differentiate, form axons and dendrites, and establish patterned connections with other
neurons66. Malformations of cortical development can thus be classified as defects in
proliferation, migration or connectivity, based on which of those processes is (most)
affected66-68. Defects in proliferation and migration result in brain abnormalities that can be
This article is protected by copyright. All rights reserved.
visible prenatally, whereas connectivity defects primarily cause functional deficits resulting
in such conditions as intellectual disability, autism and epilepsies. Cortical malformations,
especially focal defects, such as heterotopia, polymicrogyria and focal cortical dysplasias are
often not visible until later in gestation, after the routine 20-week anatomy ultrasound, and
their diagnosis requires neurosonography and fetal MRI expertise. Typical imaging features
are abnormal (premature, delayed, absent, or wide) sulcation, thin or thickened irregular
hemispheres with abnormally developed and wide gyri, cortical clefts, or heterotopia which
present as nodular protrusions into the lateral ventricles or as intraparenchymal nodules68.
The genetics of cortical malformations is complex and mutations in multiple genes,
many of which are autosomal recessive, have been implicated. Although karyotype and CMA
are first-line diagnostic tests prenatally, a genetic diagnostic work-up by WES or WGS, may
be more successful in uncovering a genetic etiology. Genetic defects or insults that affect cell
proliferation will lead to reduced or excessive growth, causing microcephaly or
megalencephaly, respectively. Incomplete neuronal migration results in heterotopia and
classic (type 1) lissencephaly. Neuronal overmigration causes cobblestone cortical
malformation (cobblestone lissencephaly). Postmigrational defects that cause cortical
disorganization result in polymicrogyria and focal cortical dysplasias68. Malformations of
cortical development can also result from infectious, toxic or vascular insults, which are
beyond the scope of this review, but must be considered in the diagnostic work-up.
Disorders of proliferation – microcephaly
The developmental prognosis of congenital microcephaly (Figure 2A) is affected by
the presence of other associated intra- and extracranial abnormalities and negatively
correlates with the size of the brain. If the head circumference of -2SD, 10% have intellectual
disability and when it is -3SD, 50% have severe intellectual disability38. Microcephaly can be
secondary to environmental factors, including infections, such as cytomegalovirus and
This article is protected by copyright. All rights reserved.
Zikavirus, or maternal genetic conditions, such as uncontrolled maternal phenylketonuria69. A
detailed discussion of secondary microcephaly is beyond the scope of this review, but must
be considered in the diagnostic work-up. Genetic causes of microcephaly include
chromosomal abnormalities and pathogenic CNVs (present in 5.4%)9. A large number of
genes have been associated with isolated primary microcephalies (MCPH: microcephaly
primary hereditary), many of which encode proteins with essential roles in chromosomal
segregation, mitotic cell division, centrosome and kinetochore function. Others have a role in
DNA damage repair, DNA replication, and cilia function69-71. A distinct group of syndromic
disorders with microcephaly are the autosomal recessive microcephalic primordial
dwarfisms, which include Seckel syndrome caused by mutations in DNA damage response
genes ATR and ATRIP and centriole biogenesis genes. Another is Meier-Gorlin syndrome
caused by mutations in ORC1, ORC4, ORC6, and other genes that play a role in origin of
DNA replication. A third class of syndromes are the microcephalic osteodysplastic primordial
dwarfisms (MOPD)69-71. These conditions present prenatally with IUGR and microcephaly
out of proportion to fetal growth69-71. MOPD1 is caused by mutations in the non-coding RNA
gene RNU4ATAC, which codes for small nuclear RNA U4atac, a component of the minor
spliceosome. If exome sequencing is done for genetic work-up and this non-coding gene is
not included in the exome capture library, these mutations can be missed72. MOPD2 is caused
by mutations in PCNT, which encodes pericentrin, an essential component of the
pericentriolar material in the centrosome and essential for normal mitotic spindle formation.
The genetic etiology for MOPD3 is currently unknown.
Disorders of proliferation –megalencephaly
Megalencephaly (Figure 2B) or large brain can be primary or secondary73. Secondary
megalencephaly can be a sign of metabolic disorders that affect the brain, such as Canavan
This article is protected by copyright. All rights reserved.
disease, glutaric aciduria type I and lysosomal storage disorders. These are usually gradually
progressive postnatally and usually not detected by prenatal imaging73. Primary
megalencephaly results from a cellular defect that causes a more general overgrowth
syndrome or can result in overgrowth of only the brain, which can be generalized, confined to
a single hemisphere (hemimegalencephaly), or focal (focal cortical dysplasia)73. Activating
dominant or somatic mutations in genes that control two main pathways with important roles
in cell growth regulation, RAS-MAPK (RASopathies) and PI3K-AKT-mTOR, have been
implicated in these conditions73.
A common prenatal-onset syndromic form is Sotos syndrome74, which affects
1:14,000 live births and is primarily caused by fully penetrant autosomal dominant mutations
in NSD1, 95% of which are de novo with low (<1%) recurrence risk. Newborn infants have a
length that is >2SD above expected. They have a large broad forehead and dolichocephalic
head shape, which is ascertainable on prenatal ultrasound. Additional prenatally detectable
findings include ventriculomegaly, hypoplasia or agenesis of the corpus callosum,
megacisterna magna and cardiac (in 20%) and renal (in 15%) anomalies. Mild to severe
intellectual disability is common and 3% of individuals with Sotos syndrome develop tumors,
including sacrococcygeal teratoma. Weaver Syndrome or EZH2-related overgrowth with
intellectual disability75 is caused by heterozygous mutations in EZH2, and is associated with
prenatal-onset somatic and brain overgrowth with a variable range of other findings on
postnatal MRI, including ventriculomegaly, periventricular leukomalacia, cerebellar
hypoplasia, infarcts, and polymicrogyria with and without pachygyria. Other anomalies, such
as cardiac defects are rare. There is also an increased risk for tumors. Simpson-Golabi-
Behmel Syndrome (SGBS)76 is an X-linked condition caused by hemizygous mutations in
males in GPC3, which encodes glypican 3. SGBS is characterized by macrosomia of prenatal
onset and craniofacial features that include macrocephaly, coarseness, macroglossia, cleft lip
This article is protected by copyright. All rights reserved.
and palate, and bifid uvula. Affected males have mild to severe intellectual disability and can
have structural brain anomalies, a heart defect, diaphragmatic hernia, large kidneys with renal
dysplasia, cryptorchidism and hypospadias, gastrointestinal anomalies, skeletal anomalies
that include vertebral fusion, scoliosis, rib anomalies, and postaxial polydactyly. They are
also at increased risk for embryonal tumors. Other syndromes, caused by mutations in PTEN
include Bannayan-Riley-Ruvalcaba syndrome, Cowden, and PTEN-related Proteus (like)
syndrome. The more common form of Proteus syndrome is caused by heterozygous and
mosaic AKT1 mutations. Only Bannayan-Riley-Ruvalcaba syndrome is associated with
prenatal macrosomia and macrocephaly. All have a predisposition to tumors and hamartomas
and intellectual disability and there can be other anomalies
Segmental brain overgrowth phenotypes are associated with activating mutations in
genes that regulate the PI3K-AKT-mTOR signaling pathway73. Hemimegalencephaly and
megalencephaly with capillary malformation (MCAP) are caused by mosaic activating
PIK3CA mutations. Megalencephaly-Polymicrogyria- Polydactyly-Hydrocephalus (MPPH)
can be caused by mutations in PIK3R2, CCND2, or AKT3. Because these mutations are
mosaic, they can be challenging to detect prenatally as they may be present at only very low
levels in amniotic fluid. We have previous experience with a prenatal diagnosis of another
PIK3CA-related segmental overgrowth disorder (CLOVES syndrome), where a mosaic
mutation that was not detected on DNA prepared from amniocytes but became detectable
after cell culture. We hypothesized that this was the result of a proliferative advantage in
culture of the cells carrying the mutation77. Focal cortical dysplasias are another class of brain
malformations, with focal areas of dysplastic cortex abnormal gyri and sulci and caused by
somatic mutations that activate the mTOR pathway.
This article is protected by copyright. All rights reserved.
Disorders of neuronal migration
Defective neuronal migration can cause malformations of development of the cerebral
and cerebellar cortex. Many of the known genes mutated in these conditions encode
cytoskeletal proteins, tubulin subunits, and kinesins. These mutations produce diverse
conditions that can present with a combination of heterotopias, gyration abnormalities, other
CNS abnormalities and extracranial structural defects66-68. Early prenatal detection is
challenging because neuronal migration and cortical folding occurs in the late second and
third trimester of fetal development and because of the limitations of ultrasound. Fetal MRI
may be needed for full evaluation.
Disorders of incomplete migration: Heterotopias
The most common forms of heterotopias are periventricular heterotopias (PVH)
(Figure 2C) wherein neurons do not migrate out of the periventricular zone, and subcortical
band heterotopia (SBH) wherein migration is incomplete along the trajectory to the cerebral
cortex creating a bandlike layer of neurons within the white matter, referred to as “double
cortex”. A common form of PVH are Bilateral Periventricular Nodular Heterotopia (BPNH)
caused by mutations in FLNA in 49% of all cases, more specifically 100% of familial and
25% of sporadic cases. In this X-linked dominant condition, females are variably affected due
to mosaicism or X-inactivation patterns. Loss of function mutations in FLNA are prenatally
lethal in males, but there are surviving males with hypomorph and mosaic mutations. BPHN
is typically detected by MRI which reveals bilateral nearly contiguous PVH at the lateral
ventricular walls with an otherwise normal appearing cortex. The corpus callosum can be thin
and there can be posterior fossa and cerebellar abnormalities. It clinically manifests primarily
as a seizure disorder in affected girls and women, who have normal intelligence to borderline
intellectual disability and may have higher risk for cardiovascular disease78. A rarer recessive
This article is protected by copyright. All rights reserved.
form of BPNH is caused by mutations in ARFGEF2, which presents with associated
microcephaly and severe developmental delay and seizures66,68,78-80.
Subcortical band heterotopia is caused by heterozygous mutations in females in the X-
linked DCX gene, encoding doublecortin. Affected girls and women have focal or generalized
seizures and either normal intelligence, mild learning disability, or intellectual disability of
variable severity, depending on the severity of the mutation, X-inactivation, and mosaicism66-
68,81,82
. When women transmit the DCX mutation to males, it causes classic lissencephaly
(see below)82. Not all heterotopia are caused by these two genes and other genetic defects,
external exposures (such as ischemia or infections) must be considered.
Tuberous sclerosis
Tuberous sclerosis (TSC) should be considered if periventricular nodules are
identified on prenatal ultrasound 83. Prenatal intracranial features include cortical tubers in
70% and subependymal nodules in 90%, but the most prominent prenatal findings are single
or multiple cardiac rhabdomyomas. In contrast to CNS findings, these typically resolve after
birth, but their discovery should prompt detailed evaluation of the brain. TSC is highly
clinically variable: 80% of affected individual have seizures and 50% have
neurodevelopmental and behavioral impairment. Of individuals with clinical criteria for TS,
85% have autosomal dominant heterozygous mutations in either TSC1 (31%) or TSC2 (69%),
which is the more severe form. Two-thirds have de novo mutations, and one third are
familial. Germline (in 5%) and somatic mosaicism (in 1%) have both been reported in TSC.
Knowing whether germline mosaicism is present affects recurrence risk counseling.
This article is protected by copyright. All rights reserved.
Disorders of incomplete migration: Classic or type I lissencephaly
The term lissencephaly is derived from the Greek words “lissos” (smooth)
“enkephalos” (brain). It is divided in classic or type I lissencephaly and cobblestone or type II
lissencephaly (see below). Classical lissencephaly affects 1.2:100,000 births and is
characterized by a smooth thick disorganized 4-layer cortex and absence of deep sulci and
gyri, the result of neuronal undermigration, with absence of other major brain anomalies. It
can be divided in 6 grades from mild (grade 6) to complete agyria (grade 1)52,66,68,80,81. There
are three main genes for classic lissencephaly: the first is LIS1 (PAFAH1B1) in 17p13.3. Loss
of function of LIS1 causes Miller-Dieker syndrome (Figure 2D,E). This is often due to a
microdeletion, which is de novo in 80% and inherited from a parent with a balanced
translocation in 20%, but other LIS1 mutations have been found in isolated lissencephaly. A
second common cause of classic lissencephaly are mutations in DCX in Xq22.3 in males, of
whom 25% inherit the mutation from their mother and the remainder are caused by de novo
mutations66,80. Mutations in these two genes cause 76% of all lissencephaly52 and mutations
in TUBA1A cause an additional 4%52. Other findings associated with lissencephaly can
provide clues to the molecular etiology. Lissencephaly associated with microcephaly should
raise suspicion for TUBA1A mutations or other tubulinopathies (TUBB2B, TUBG1, etc).
Lissencephaly with cerebellar hypoplasia (LCH) presents with a spectrum of cerebellar
abnormalities from vermian hypoplasia, to underdevelopment or cerebellar agenesis and can
be caused by autosomal recessive TUBA1A (30% of cases) or RELN mutations. Other
variants include X-linked lissencephaly with ACC and ambiguous genitalia in males
(XLAG), caused by mutations in the ARX gene. Microlissencephaly is associated with a head
circumference of <3SD for developmental stage and can suggest a primordial dwarfism
(discussed above). Other more rarely implicated genes include VLDLR, CDK5, ACTB,
ACTG1, NDE1, DYNC1H1, KIF2A66,68,80,81.
This article is protected by copyright. All rights reserved.
Disorders of overmigration: Cobblestone cortical malformation or type II lissencephaly
Cobblestone cortical malformation (Figure 2F-H), now considered a better name than
type II lissencephaly, affects 1:100,000 births. These present with a more nodular cerebral
cortical surface caused by overmigration of neurons and glia. This phenotype is associated
with a very disorganized cortex with multiple coarse gyri and areas with no gyri, together
with other CNS abnormalities, including abnormal pons and kinked brain stem, cerebellar
abnormalities and callosal abnormalities. It most often results from mutations (the majority
autosomal recessive) in genes that are important for dystroglycan production and function,
resulting in a collection of congenital muscular dystrophies or “dystroglycanopathies”. The
most common ones are Walker-Warburg syndrome (WWS), muscle-eye-brain disease
(MEB), and Fukuyama congenital muscular dystrophies (FCMD). They have a uniformly
guarded prognosis for neurodevelopment and are differentiated by additional features that are
not all ascertainable on prenatal imaging. WWS is often associated with mortality in the first
year of life, while children with MEB may survive longer. Patients with WWS often have eye
abnormalities, cleft lip, renal dysplasia and sometimes hypoplastic genitalia. Congenital
contractures and akinesia or severe hypotonia can also be present66,68,81.
Postmigrational defects: disorders of cortical disorganization
Gyration abnormalities
Gyration abnormalities are postmigrational defects, which are not visible until later in
pregnancy and can be isolated or associated with other intra- and extracranial abnormalities.
They include polymicrogyria (PMG) (Figure 2I,J), agyria and pachygyria and constitute
20% of all malformations of cortical development. They can be difficult to see on prenatal
ultrasound and are best evaluated by MRI, performed in the late second or early third
trimester (after 20-22 weeks)52. Recent studies have suggested that an abnormal shape and
This article is protected by copyright. All rights reserved.
size of the sylvian fissure in early pregnancy can be an early sign of migration abnormalities
and indication for further imaging by ultrasound and MRI at a later gestational age 84,85. The
most common location is in the bilateral perisylvian region, but they can be unilateral, and
have an anterior-posterior or posterior-anterior gradient. The cortex in the abnormal gyri can
be unlayered with only 2 layers or layered with 4-6 layers. Schizencephaly is a subtype of
PMG that presents as a cleft in the cerebral cortex that connects the subarachnoid space to the
ventricles. It can have an open or closed lip and be unilateral or bilateral and is typically lined
by unlayered PMG66,68.
PMG can be sequelae of a non-genetic insult to the developing CNS by infections
(such as congenital CMV) or ischemia. Genetic causes include chromosomal abnormalities,
among which the 22q11.2 deletion, which is the most common prenatally detected
microdeletion and is well known for its association with cardiac anomalies but can
occasionally present with perisylvian PMG. Another common deletion syndrome with PMG
is the 1p36 deletion syndrome. The remainder of cases are caused by a variety of autosomal
dominant de novo, autosomal recessive and X-linked single gene mutations. Among these are
metabolic and lysosomal disorders, including Zellweger syndrome, neonatal
adrenoleukodystrophy, Pelizaeus-Merzbacher, glutaric aciduria type 2, maple syrup urine
disease and many others. Another class are collectively referred to as tubulinopathies (many
of which are de novo dominant)
For some conditions, such as Aicardi syndrome, the genetic cause is unknown, This condition
affects females only and is suspected when there are PMG, heterotopias and cysts, but it can
only be confirmed after birth by demonstration of the typical chorioretinal lacunae on
fundoscopic eye exam66,68,80,86.
This article is protected by copyright. All rights reserved.
Cerebellar and posterior fossa abnormalities
Prevalence and classification of cerebellar defects
Cerebellar abnormalities affect 1:5000 live births and are often associated with other
CNS and non-CNS anomalies. Overall, 20-100% of children with cerebellar abnormalities
have impaired neurological outcome, but the severity depends on the type of defect and the
degree by which the vermis and cerebellar hemispheres are affected. Types of posterior fossa
abnormalities include megacisterna magna, Dandy-Walker malformation, vermian agenesis,
rhombencephalosynapsis, pontocerebellar hypoplasia, cerebellar atrophy, posterior fossa
arachnoid cyst, and Blake’s pouch cyst (which indicates delayed closure of the vermis)87,88.
Although terms like Dandy-Walker Variant, Dandy-Walker Spectrum or Dandy-Walker
complex were previously used, it is now considered better to abandon these designations for
this more descriptive terminology87.
Mega-cisterna magna
Megacisterna magna (MCM) (Figure 3A,B), or a transverse measurement of the
posterior fossa >10 mm with normal appearing cerebellar vermis and hemispheres is the most
common prenatally diagnosed posterior fossa abnormality, comprising 40% of all findings in
the posterior fossa88,89. The neurodevelopmental outcome is normal in 86-100% of isolated
MCM cases88-90 with no increased risk for aneuploidy. Additional CNS abnormalities are
found on 12.6%, most commonly ventriculomegaly, and other anomalies are found in
16.6%90. Small series suggest that when MCM is associated with other CNS and non-CNS
defects, only 29% to two-thirds develop normally and one-third have cognitive, language and
motor delay and have an increased risk for chromosomal or other genetic abnormalities91.
This article is protected by copyright. All rights reserved.
Cerebellar hypoplasias
Vermian hypoplasia (Figure 3E) with intact cerebellar hemispheres is associated with
other anomalies in 70% of cases. When it is isolated, 77% are predicted to have normal
development, but 23% can have neurological abnormalities that include, gross and fine motor
disability, social and communication defects, behavioral abnormalities (15%) and hypotonia
(23%)87,88,92. Primary cerebellar hypoplasia is associated with chromosomal abnormality in
16.3% and 13.7% of those with a normal karyotype have a pathogenic copy number variant
by CMA87,88. Metabolic conditions including Smith-Lemli-Opitz syndrome, Molybdeen
deficiency, and adenoylsuccinase deficiency can be associated with cerebellar hypoplasia87.
Specific single gene disorders with cerebellar hypoplasia include Ritscher-Schinzel
Syndrome, caused by mutations in RTSC1/SPG8 (KIAA0196), RTSC2 (CCDC22), Joubert
spectrum disorders, which can be caused by mostly autosomal recessive mutations in
multiple genes and loci (see below). Other syndromes with cerebellar hypoplasia include
CHARGE Syndrome, associated with multiple other anomalies and caused by mutations in
CHD7, and acrocallosal syndrome caused by KIF7 mutations. When cerebellar hypoplasia is
associated with other brain malformations such as Dandy-Walker malformation,
rhombencephalosynapsis, pontocerebellar hypoplasia (often with cortical malformations), the
suspicion that it is part of a genetic syndrome should be high. Unilateral abnormalities are
more suggestive of cerebellar damage, for example by infection or ischemia, but can also be
caused by COL4A1 mutations or found in genetic syndromes such as PHACE syndrome, a
neurocutaneous syndrome characterized by posterior fossa brain malformations,
hemangiomas of the face (large or complex), arterial anomalies, cardiac anomalies, and eye
abnormalities. 87,88.
This article is protected by copyright. All rights reserved.
Dandy-Walker malformation
In Dandy walker malformation (DWM) (Figure 3C,D) there is complete or partial
agenesis of the cerebellar vermis, cystic dilation of 4th ventricle, and enlarged posterior fossa
with upward displacement of the tentorium87,88. Up to 86% of fetuses with DWM have other
abnormalities, of which 49% have other CNS anomalies. Development can be normal in up to
a third of prenatally detected DWM; in particular when the vermis is normally lobulated,
82%-90% have normal intelligence. However, with associated CNS or extra-CNS
malformations or absent or abnormal vermis lobulation, 50% will have neurological
abnormalities, 50% will have hypotonia, 42% will have cerebellar dysfunction and 5% will
show hemiparesis. Genetic abnormalities associated with Dandy-Walker include
chromosomal abnormalities in 16.3%50, as well as a variety of single gene mutations.
Joubert syndrome and related disorders
In this group of overlapping conditions, the cerebellar/posterior fossa abnormality is
characterized by an abnormally deep interpeduncular fossa, more horizontally oriented
enlarged superior cerebellar peduncles, and hypoplastic cerebellar vermis. This combination
of findings results in the diagnostic molar tooth sign which is easily recognizable with fetal
MRI, but can also be observed by high-resolution prenatal ultrasound imaging87,88 (Figure F-
H). Joubert syndrome-related disorders can have associated renal, hepatic, and eye
abnormalities and polydactyly. There is significant overlap with other conditions such as
Meckel-Gruber syndrome, hydrolethalus syndrome, nephronophthisis syndrome, acrocallosal
syndrome, Bardet-Biedl syndrome and orofacial digital (OFD) syndrome88. Joubert syndrome
and these overlapping conditions are associated with developmental delays, hypotonia,
breathing anomalies, ataxia, abnormal eye movement, and facial dysmorphia. Some, such as
Meckel-Gruber syndrome, are lethal due to the severity of the kidney abnormalities or other
This article is protected by copyright. All rights reserved.
defects. Collectively these conditions are caused by recessive mutations in more than 30
autosomal genes, as well as mutations in a few X-linked genes. Many of these have a role in
cilia function, leading to the term “ciliopathies”. Gene panel or exome testing yields a
molecular diagnosis in 62-94% of cases87,88,92-94.
Summary and conclusions
Structural abnormalities of the brain are complex with multiple genetic and non-
genetic etiologies and evaluation and management of women with affected pregnancies is
best done in a multidisciplinary team approach. Identifying the cause is essential for accurate
prognosis and recurrence risk counseling. In most cases, this requires a combination of high-
resolution neurosonography and prenatal MRI with expert interpretation of findings, and a
recognition that some features will not be apparent until later in gestation. Genetic testing
should be offered and include as first-line approach a chromosomal microarray analysis and
karyotype. Many structural brain abnormalities are caused by single-gene mutations.
Considering the large number of possible causative genes, exome sequencing is the strategy
most likely to yield a molecular diagnosis but is not yet widely available prenatally. Multi-
gene panels relevant to distinct phenotypes can also be considered in the diagnostic work-up
of these patients.
This article is protected by copyright. All rights reserved.
REFERENCES
1. Chitty LS, Pilu G. The challenge of imaging the fetal central nervous system: an aid
to prenatal diagnosis, management and prognosis. Prenat Diagn. 2009;29(4):301-302.
2. Di Mascio D, Sileo FG, Khalil A, et al. Systematic review and meta-analysis on the
role of prenatal magnetic resonance imaging in the era of fetal neurosonography: mild
and moderate ventriculomegaly. Ultrasound Obstet Gynecol. 2018; Dec 14. doi:
10.1002/uog.20197.
3. Blaas HG, Eik-Nes SH. Sonoembryology and early prenatal diagnosis of neural
anomalies. Prenat Diagn. 2009;29(4):312-325.
4. Blaas HG, Eik-Nes SH, Isaksen CV. The detection of spina bifida before 10
gestational weeks using two- and three-dimensional ultrasound. Ultrasound Obstet
Gynecol. 2000;16(1):25-29.
5. Monteagudo A, Timor-Tritsch IE. Normal sonographic development of the central
nervous system from the second trimester onwards using 2D, 3D and transvaginal
sonography. Prenat Diagn. 2009;29(4):326-339.
6. Greene ND, Copp AJ. Development of the vertebrate central nervous system:
formation of the neural tube. Prenat Diagn. 2009;29(4):303-311.
7. de Wit MC, Srebniak MI, Govaerts LC, Van Opstal D, Galjaard RJ, Go AT.
Additional value of prenatal genomic array testing in fetuses with isolated structural
ultrasound abnormalities and a normal karyotype: a systematic review of the
literature. Ultrasound Obstet Gynecol. 2014;43(2):139-146.
8. Wapner RJ, Martin CL, Levy B, et al. Chromosomal microarray versus karyotyping
for prenatal diagnosis. New Engl J Med. 2012;367(23):2175-2184.
9. Shaffer LG, Rosenfeld JA, Dabell MP, et al. Detection rates of clinically significant
genomic alterations by microarray analysis for specific anomalies detected by
ultrasound. Prenat Diagn. 2012;32(10):986-995.
10. Breman A, Pursley AN, Hixson P, et al. Prenatal chromosomal microarray analysis in
a diagnostic laboratory; experience with >1000 cases and review of the literature.
Prenat Diagn. 2012;32(4):351-361.
11. Normand EA, Braxton A, Nassef S, et al. Clinical exome sequencing for fetuses with
ultrasound abnormalities and a suspected Mendelian disorder. Genome Med.
2018;10(1):74.
12. Meng L, Pammi M, Saronwala A, et al. Use of Exome Sequencing for Infants in
Intensive Care Units: Ascertainment of Severe Single-Gene Disorders and Effect on
Medical Management. JAMA Pediatr. 2017:e173438.
13. Best S, Wou K, Vora N, Van den Veyver IB, Wapner R, Chitty LS. Promises, pitfalls
and practicalities of prenatal whole exome sequencing. Prenat Diagn. 2017;38(1):10-
19.
14. Van den Veyver IB. Recent advances in prenatal genetic screening and testing.
F1000Res. 2016;5:2591.
15. Yang Y, Muzny DM, Xia F, et al. Molecular Findings Among Patients Referred for
Clinical Whole-Exome Sequencing. JAMA. 2014;312(18):1870-1879.
16. Yang Y, Muzny DM, Reid JG, et al. Clinical whole-exome sequencing for the
diagnosis of mendelian disorders. New Engl J Med. 2013;369(16):1502-1511.
17. Mirzaa GM, Paciorkowski AR. Introduction: Brain malformations. Am J Med Genet
C Semin Med Genet. 2014;166C(2):117-123.
18. Wiszniewski W, Gawlinski P, Gambin T, et al. Comprehensive genomic analysis of
patients with disorders of cerebral cortical development. Eur J Hum Genet. 2018
Aug;26(8):1121-1131.
This article is protected by copyright. All rights reserved.
19. Adle-Biassette H, Golden JA, Harding B. Developmental and perinatal brain diseases.
Handb Clin Neurol. 2017;145:51-78.
20. Practice Bulletin No. 162 Summary: Prenatal Diagnostic Testing for Genetic
Disorders. Obstet Gynecol. 2016;127(5):976-978.
21. Joint Position Statement from the International Society for Prenatal Diagnosis (ISPD),
the Society for Maternal Fetal Medicine (SMFM), and the Perinatal Quality
Foundation (PQF) on the use of genome-wide sequencing for fetal diagnosis. Prenat
Diagn. 2018;38(1):6-9.
22. Talkowski ME, Rehm HL. Introduction of genomics into prenatal diagnostics. Lancet.
2019; 393(10173):719-721.
23. Petrovski S, Aggarwal V, Giordano JL, et al. Whole-exome sequencing in the
evaluation of fetal structural anomalies: a prospective cohort study. Lancet. 2019;
393(10173):758-767.
24. Lord J, McMullan DJ, Eberhardt RY, et al. Prenatal exome sequencing analysis in
fetal structural anomalies detected by ultrasonography (PAGE): a cohort study.
Lancet. 2019; 393(10173):747-757.
25. Rao R, Platt LD. Ultrasound screening: Status of markers and efficacy of screening
for structural abnormalities. Semin Perinatol. 2016;40(1):67-78.
26. Gupta JK, Khan KS, Thornton JG, Lilford RJ. Management of fetal choroid plexus
cysts. Br J Obstet Gynaecol. 1997;104(8):881-886.
27. Yoder PR, Sabbagha RE, Gross SJ, Zelop CM. The second-trimester fetus with
isolated choroid plexus cysts: a meta-analysis of risk of trisomies 18 and 21. Obstet
Gynecol. 1999;93(5 Pt 2):869-872.
28. Uchiyama CM, Carey CM, Cherny WB, et al. Choroid plexus papilloma and cysts in
the Aicardi syndrome: case reports. Pediatr Neurosurg. 1997;27(2):100-104.
29. DiPietro JA, Cristofalo EA, Voegtline KM, Crino J. Isolated prenatal choroid plexus
cysts do not affect child development. Prenat Diagn. 2011;31(8):745-749.
30. Cameron M, Moran P. Prenatal screening and diagnosis of neural tube defects. Prenat
Diagn. 2009;29(4):402-411.
31. Copp AJ, Stanier P, Greene ND. Neural tube defects: recent advances, unsolved
questions, and controversies. Lancet Neurol. 2013;12(8):799-810.
32. Avagliano L, Massa V, George TM, Qureshy S, Bulfamante GP, Finnell RH.
Overview on neural tube defects: From development to physical characteristics. Birth
Defects Res. 2018; Nov 12. doi: 10.1002/bdr2.1380.
33. Greene ND, Copp AJ. Neural tube defects. Annu Rev Neurosci. 2014;37:221-242.
34. Scelsa B, Rustico M, Righini A, et al. Mild ventriculomegaly from fetal consultation
to neurodevelopmental assessment: A single center experience and review of the
literature. Eur J Paediatr Neurol. 2018; 22(6):919-928.
35. Barzilay E, Bar-Yosef O, Dorembus S, Achiron R, Katorza E. Fetal Brain Anomalies
Associated with Ventriculomegaly or Asymmetry: An MRI-Based Study. AJNR Am J
Neuroradiol. 2017;38(2):371-375.
36. Ouahba J, Luton D, Vuillard E, et al. Prenatal isolated mild ventriculomegaly:
outcome in 167 cases. BJOG. 2006;113(9):1072-1079.
37. D'Addario V, Rossi AC. Neuroimaging of ventriculomegaly in the fetal period.
Seminars in fetal & neonatal medicine. 2012;17(6):310-318.
38. Mighell AS, Johnstone ED, Levene M. Post-natal investigations: management and
prognosis for fetuses with CNS anomalies identified in utero excluding neurosurgical
problems. Prenat Diagn. 2009;29(4):442-449.
This article is protected by copyright. All rights reserved.
39. Mehlhorn AJ, Morin CE, Wong-You-Cheong JJ, Contag SA. Mild fetal cerebral
ventriculomegaly: prevalence, characteristics, and utility of ancillary testing in cases
presenting to a tertiary referral center. Prenat Diagn. 2017;37(7):647-657.
40. Pagani G, Thilaganathan B, Prefumo F. Neurodevelopmental outcome in isolated
mild fetal ventriculomegaly: systematic review and meta-analysis. Ultrasound Obstet
Gynecol. 2014;44(3):254-260.
41. Perlman S, Bar-Yosef O, Jacobson JM, et al. Natural history of fetal isolated
ventriculomegaly: Comparison between pre- and post-natal imaging. J Matern Fetal
Neonatal Med. 2018;31(13):1762-1767.
42. Stumpel C, V Vos YJ. L1 Syndrome. 2004 Apr 28 [Updated 2015 Mar 5]. In: Adam
MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA):
University of Washington, Seattle; 1993-2019. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK1484/.
43. Adle-Biassette H, Saugier-Veber P, Fallet-Bianco C, et al. Neuropathological review
of 138 cases genetically tested for X-linked hydrocephalus: evidence for closely
related clinical entities of unknown molecular bases. Acta Neuropathol.
2013;126(3):427-442.
44. Vasudevan C, McKechnie L, Levene M. Long-term outcome of antenatally diagnosed
agenesis of corpus callosum and cerebellar malformations. Seminars in fetal &
neonatal medicine. 2012;17(5):295-300.
45. Palmer EE, Mowat D. Agenesis of the corpus callosum: a clinical approach to
diagnosis. Am J Med Genet C Semin Med Genet. 2014;166C(2):184-197.
46. Engels AC, Joyeux L, Brantner C, et al. Sonographic detection of central nervous
system defects in the first trimester of pregnancy. Prenat Diagn. 2016;36(3):266-273.
47. Leombroni M, Khalil A, Liberati M, D'Antonio F. Fetal midline anomalies: Diagnosis
and counselling Part 1: Corpus callosum anomalies. Eur J Paediatr Neurol. 2018;
22(6):951-962.
48. Malinger G, Lev D, Oren M, Lerman-Sagie T. Non-visualization of the cavum septi
pellucidi is not synonymous with agenesis of the corpus callosum. Ultrasound Obstet
Gynecol. 2012;40(2):165-170.
49. Mangione R, Fries N, Godard P, et al. Neurodevelopmental outcome following
prenatal diagnosis of an isolated anomaly of the corpus callosum. Ultrasound Obstet
Gynecol. 2011;37(3):290-295.
50. D'Antonio F, Pagani G, Familiari A, et al. Outcomes Associated With Isolated
Agenesis of the Corpus Callosum: A Meta-analysis. Pediatrics. 2016;138(3).
51. Sajan SA, Fernandez L, Nieh SE, et al. Both rare and de novo copy number variants
are prevalent in agenesis of the corpus callosum but not in cerebellar hypoplasia or
polymicrogyria. PLoS Genet. 2013;9(10):e1003823.
52. Huang J, Wah IY, Pooh RK, Choy KW. Molecular genetics in fetal neurology.
Seminars in fetal & neonatal medicine. 2012;17(6):341-346.
53. Sundarakumar DK, Farley SA, Smith CM, Maravilla KR, Dighe MK, Nixon JN.
Absent cavum septum pellucidum: a review with emphasis on associated commissural
abnormalities. Pediatr Radiol. 2015;45(7):950-964.
54. Nagaraj UD, Calvo-Garcia MA, Kline-Fath BM. Abnormalities Associated With the
Cavum Septi Pellucidi on Fetal MRI: What Radiologists Need to Know. AJR Am J
Roentgenol. 2018;210(5):989-997.
55. Pilliod RA, Pettersson DR, Gibson T, et al. Diagnostic accuracy and clinical outcomes
associated with prenatal diagnosis of fetal absent cavum septi pellucidi. Prenat Diagn.
2018;38(6):395-401.
This article is protected by copyright. All rights reserved.
56. Leombroni M, Khalil A, Liberati M, D'Antonio F. Fetal midline anomalies: Diagnosis
and counselling part 2: Septal anomalies. Eur J Paediatr Neurol. 2018; 22(6):963-
971.
57. Ho YK, Turley M, Marc-Aurele KL, et al. Enlarged Cavum Septi Pellucidi and
Vergae in the Fetus: A Cause for Concern. J Ultrasound Med. 2017;36(8):1657-1668.
58. Matsunaga E, Shiota K. Holoprosencephaly in human embryos: epidemiologic studies
of 150 cases. Teratology. 1977;16(3):261-272.
59. Orioli IM, Castilla EE. Epidemiology of holoprosencephaly: Prevalence and risk
factors. Am J Med Genet C Semin Med Genet. 2010;154C(1):13-21.
60. Solomon BD, Kruszka P, Muenke M. Holoprosencephaly flashcards: An updated
summary for the clinician. Am J Med Genet C Semin Med Genet. 2018;178(2):117-
121.
61. S Solomon BD, Gropman A, Muenke M. Holoprosencephaly Overview. 2000 Dec 27
[Updated 2013 Aug 29]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors.
GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-
2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1530/.
62. Rosenfeld JA, Ballif BC, Martin DM, et al. Clinical characterization of individuals
with deletions of genes in holoprosencephaly pathways by aCGH refines the
phenotypic spectrum of HPE. Hum Genet. 2010;127(4):421-440.
63. Nowaczyk MJM. Smith-Lemli-Opitz Syndrome. 1998 Nov 13 [Updated 2013 Jun
20]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews® [Internet].
Seattle (WA): University of Washington, Seattle; 1993-2019. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK1143/.
64. Lazarin GA, Haque IS, Evans EA, Goldberg JD. Smith-Lemli-Opitz syndrome carrier
frequency and estimates of in utero mortality rates. Prenat Diagn. 2017;37(4):350-
355.
65. Ming JE, Muenke M. Multiple hits during early embryonic development: digenic
diseases and holoprosencephaly. Am J Hum Genet. 2002;71(5):1017-1032.
66. Romero DM, Bahi-Buisson N, Francis F. Genetics and mechanisms leading to human
cortical malformations. Semin Cell Dev Biol. 2018;76:33-75.
67. Hu WF, Chahrour MH, Walsh CA. The diverse genetic landscape of
neurodevelopmental disorders. Annu Rev Genomics Hum Genet. 2014;15:195-213.
68. Lerman-Sagie T, Leibovitz Z. Malformations of Cortical Development: From
Postnatal to Fetal Imaging. Can J Neurol Sci. 2016;43(5):611-618.
69. Alcantara D, O'Driscoll M. Congenital microcephaly. Am J Med Genet C Semin Med
Genet. 2014;166C(2):124-139.
70. Duerinckx S, Abramowicz M. The genetics of congenitally small brains. Semin Cell
Dev Biol. 2018;76:76-85.
71. Jayaraman D, Bae BI, Walsh CA. The Genetics of Primary Microcephaly. Annu Rev
Genomics Hum Genet. 2018;19:177-200.
72. Wang Y, Wu X, Du L, et al. Identification of compound heterozygous variants in the
noncoding RNU4ATAC gene in a Chinese family with two successive foetuses with
severe microcephaly. Hum Genomics. 2018;12(1):3.
73. Mirzaa GM, Poduri A. Megalencephaly and hemimegalencephaly: breakthroughs in
molecular etiology. Am J Med Genet C Semin Med Genet. 2014;166C(2):156-172.
74. Tatton-Brown K, Cole TRP, Rahman N. Sotos Syndrome. 2004 Dec 17 [Updated
2015 Nov 19]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews
[Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK1479/.
This article is protected by copyright. All rights reserved.
75. Tatton-Brown K, Rahman N. EZH2-Related Overgrowth. 013 Jul 18 [Updated 2018
Aug 2]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews
[Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019. Available
from: https://www.ncbi.nlm.nih.gov/books/NBK148820/.
76. Sajorda BJ, Gonzalez-Gandolfi CX, Hathaway ER, Kalish JM. Simpson-Golabi-
Behmel Syndrome Type 1. I 2006 Dec 19 [Updated 2018 Nov 29]. In: Adam MP,
Ardinger HH, Pagon RA, et al., editors. GeneReviews [Internet]. Seattle (WA):
University of Washington, Seattle; 1993-2019. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK1219/.
77. Emrick LT, Murphy L, Shamshirsaz AA, et al. Prenatal diagnosis of CLOVES
syndrome confirmed by detection of a mosaic PIK3CA mutation in cultured
amniocytes. American journal of medical genetics Part A. 2014;164A(10):2633-2637.
78. Chen MH, Walsh CA. FLNA-Related Periventricular Nodular Heterotopia. 002 Oct 8
[Updated 2015 Sep 17]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors.
GeneReviews [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK1213/.
79. Deloison B, Sonigo P, Millischer-Bellaiche AE, et al. Prenatally diagnosed
periventricular nodular heterotopia: Further delineation of the imaging phenotype and
outcome. Eur J Med Genet. 2018;61(12):773-782.
80. Bahi-Buisson N, Guerrini R. Diffuse malformations of cortical development. Handb
Clin Neurol. 2013;111:653-665.
81. Fry AE, Cushion TD, Pilz DT. The genetics of lissencephaly. Am J Med Genet C
Semin Med Genet. 2014;166C(2):198-210.
82. Hehr U, Uyanik G, Aigner L, Couillard-Despres S, Winkler J. DCX-Related
Disorders. 2007 Oct 19 [Updated 2019 Feb 7]. In: Adam MP, Ardinger HH, Pagon
RA, et al., editors. GeneReviews [Internet]. Seattle (WA): University of Washington,
Seattle; 1993-2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1185/.
83. Northrup H, Koenig MK, Pearson DA, Au KS. Tuberous Sclerosis Complex. I 1999
Jul 13 [Updated 2018 Jul 12]. In: Adam MP, Ardinger HH, Pagon RA, et al., editors.
GeneReviews [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2019.
Available from: https://www.ncbi.nlm.nih.gov/books/NBK1220/.
84. Poon LC, Sahota D, Chaemsaithong P, et al. Transvaginal three-dimensional
assessment of Sylvian fissures at 18-30 weeks' gestation. Ultrasound Obstet Gynecol.
2018; Oct 31. doi: 10.1002/uog.20172.
85. Pooh RK, Machida M, Nakamura T, et al. Maldevelopment of Sylvian fissure as an
early sonographic sign of malformations of cortical development. Ultrasound Obstet
Gynecol. 2018; Oct 31. doi: 10.1002/uog.20171.
86. Stutterd CA, Leventer RJ. Polymicrogyria: a common and heterogeneous
malformation of cortical development. Am J Med Genet C Semin Med Genet.
2014;166C(2):227-239.
87. Poretti A, Boltshauser E, Doherty D. Cerebellar hypoplasia: differential diagnosis and
diagnostic approach. Am J Med Genet C Semin Med Genet. 2014;166C(2):211-226.
88. Lerman-Sagie T, Prayer D, Stocklein S, Malinger G. Fetal cerebellar disorders.
Handb Clin Neurol. 2018;155:3-23.
89. Massoud M, Guibaud L. Prenatal imaging of posterior fossa disorders. A review. Eur
J Paediatr Neurol. 2018; 22(6):972-988.
90. D'Antonio F, Khalil A, Garel C, et al. Systematic review and meta-analysis of isolated
posterior fossa malformations on prenatal ultrasound imaging (part 1): nomenclature,
diagnostic accuracy and associated anomalies. Ultrasound Obstet Gynecol.
2016;47(6):690-697.
This article is protected by copyright. All rights reserved.
91. Forzano F, Mansour S, Ierullo A, Homfray T, Thilaganathan B. Posterior fossa
malformation in fetuses: a report of 56 further cases and a review of the literature.
Prenat Diagn. 2007;27(6):495-501.
92. Bolduc ME, Limperopoulos C. Neurodevelopmental outcomes in children with
cerebellar malformations: a systematic review. Dev Med Child Neurol.
2009;51(4):256-267.
93. Vilboux T, Doherty DA, Glass IA, et al. Molecular genetic findings and clinical
correlations in 100 patients with Joubert syndrome and related disorders prospectively
evaluated at a single center. Genet Med. 2017;19(8):875-882.
94. Aldinger KA, Doherty D. The genetics of cerebellar malformations. Seminars in fetal
& neonatal medicine. 2016;21(5):321-332.
This article is protected by copyright. All rights reserved.
Table 1: Multidisciplinary team in the clinical work-up for pregnancies with prenatally
identified central nervous system abnormalities
Prenatal care provider
Sonographer
Maternal-fetal medicine specialist
Radiologist with expertise in prenatal ultrasound and fetal MRI
Prenatal and pediatric geneticist and/or genetic counselor
Neonatologist
Pediatric neurologist
Neurosurgeon
Other subspecialties (to address associated defects)
Perinatal Hospice team (PPACT: Perinatal Pediatric Advanced Care Team)
This article is protected by copyright. All rights reserved.
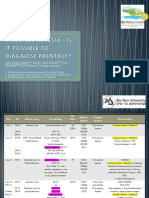
Table 2: Categories of central nervous system defects detectable on prenatal imaging
Common prenatally diagnosed central nervous system defects
Choroid plexus cysts
Neural tube defects
Ventriculomegaly and hydrocephalus
Midline defects
Abnormalities of the corpus callosum and cavum septum pellucidum
Holoprosencephaly
Malformations of cortical development
Disorders of proliferation – microcephaly
Disorders of proliferation – megalencephaly and hemimegalencephaly
Disorders of proliferation – focal cortical dysplasia
Disorders of neuronal migration
Incomplete migration: Heterotopias
Incomplete migration: Classic or type I lissencephaly
Overmigration: Cobblestone cortical malformation or type II lissencephaly
Postmigrational defects: disorders of cortical disorganization
Gyration abnormalities
Cerebellar and posterior fossa abnormalities
Mega-cisterna magna
Cerebellar hypoplasias
Dandy-Walker malformation
Joubert syndrome and related disorders
This article is protected by copyright. All rights reserved.
Figure 1: Commonly identified central nervous system abnormalities. (A) Second-
trimester ultrasound image of bilateral choroid plexus cysts (white arrows) in the lateral
ventricles. (B-E) Ultrasound images of neural tube defects: (B,C) Intracranial anomalies with
spina bifida at 17 weeks 1 day. (D) Myelomeningocele at 21 weeks 5 days. (E) Posterior
encephalocele. (F-H) Ventriculomegaly with aqueductal stenosis on ultrasound (F) and MRI
(G,H). (I-K) Agenesis of corpus callosum on ultrasound (I) and MRI (J,K). (L,M) Alobar
holoprosencephaly at 28 weeks 3 days on ultrasound (I) and MRI (J,K).
This article is protected by copyright. All rights reserved.
Figure 2: Malformations of cortical development. (A) Microcephaly at 25 weeks and 3
days. (B) Megalencephaly at 21 weeks. (C) Periventricular heterotopia at 21 weeks 5 days.
(D,E) Miller-Dieker syndrome lissencephaly at 32 weeks 1 day. (F-H) Cobblestone (type II)
lissencephaly at 25 weeks 5 days. (I-J) Polymicrogyria at 35 weeks 5 days. [All are MRI
images, except D and F].
This article is protected by copyright. All rights reserved.
Figure 3: Posterior fossa and cerebellar abnormalities. (A,B) Megacisterna magna at 32
weeks 4 days on ultrasound and MRI. (C,D) Dandy-Walker malformation at 34 weeks and 3
days (ultrasound and MRI) . (E) Vermian hypoplasia at 20 weeks 0 days (MRI). (F-H)
Joubert syndrome at 32 weeks and 1 day on ultrasound (F) and MRI (G,H). Red circle
indicates “molar tooth” sign.
This article is protected by copyright. All rights reserved.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Guidotti, Tee L - The Praeger Handbook of Occupational and Environmental Medicine 1-3 VOL-Praeger - ABC-CLIO (2010)Document1,703 pagesGuidotti, Tee L - The Praeger Handbook of Occupational and Environmental Medicine 1-3 VOL-Praeger - ABC-CLIO (2010)Ahmed H. Ali ElbestaweyNo ratings yet
- First Aid: 15 Minutes Presentation at Ald Ersgate CollegeDocument19 pagesFirst Aid: 15 Minutes Presentation at Ald Ersgate CollegeEmmanuel John Dela CruzNo ratings yet
- Nutrition Assessment 1Document22 pagesNutrition Assessment 1KHALEEL SALEHNo ratings yet
- Cancer and The New Biology of Water - Dr. Thomas Cowan MDDocument5 pagesCancer and The New Biology of Water - Dr. Thomas Cowan MDnufihyreNo ratings yet
- OSCE Checklist Dizziness History TakingDocument2 pagesOSCE Checklist Dizziness History TakingEe VoneNo ratings yet
- Screening For Preeclampsia Using Uterine Artery Doppler and Other BiomarkersDocument65 pagesScreening For Preeclampsia Using Uterine Artery Doppler and Other BiomarkersAhmed H. Ali ElbestaweyNo ratings yet
- Arab FellowShipDocument11 pagesArab FellowShipAhmed H. Ali ElbestaweyNo ratings yet
- EecDocument2 pagesEecAhmed H. Ali ElbestaweyNo ratings yet
- 2nd - Sreeja RajeshDocument1 page2nd - Sreeja RajeshAhmed H. Ali ElbestaweyNo ratings yet
- Uog12528-Fig-0002 - 10.1002/uog.12528 Chorionic BumpDocument1 pageUog12528-Fig-0002 - 10.1002/uog.12528 Chorionic BumpAhmed H. Ali ElbestaweyNo ratings yet
- Faculty AIUM2018Document1 pageFaculty AIUM2018Ahmed H. Ali ElbestaweyNo ratings yet
- Choanal Atresia For ISUOG-Jerusalem 2018Document10 pagesChoanal Atresia For ISUOG-Jerusalem 2018Ahmed H. Ali ElbestaweyNo ratings yet
- Advances Programme 2017Document2 pagesAdvances Programme 2017Ahmed H. Ali ElbestaweyNo ratings yet
- Detailed Program 28-11-18Document3 pagesDetailed Program 28-11-18Ahmed H. Ali ElbestaweyNo ratings yet
- Atretic Encephalocele, Tip of The IcebergDocument6 pagesAtretic Encephalocele, Tip of The IcebergAhmed H. Ali ElbestaweyNo ratings yet
- Cervical Recuperation Postpartum-US Conference-Jerusalem-Feb 2018Document23 pagesCervical Recuperation Postpartum-US Conference-Jerusalem-Feb 2018Ahmed H. Ali ElbestaweyNo ratings yet
- 2019 Chromosomal Microarray vs. NIPS Analysis of 5541 Low-Risk PregnanciesDocument6 pages2019 Chromosomal Microarray vs. NIPS Analysis of 5541 Low-Risk PregnanciesAhmed H. Ali ElbestaweyNo ratings yet
- At and Accuracy 2018 כנס החברה (1) Bardin PDFDocument22 pagesAt and Accuracy 2018 כנס החברה (1) Bardin PDFAhmed H. Ali ElbestaweyNo ratings yet
- Human Malformations - 10 - EarDocument45 pagesHuman Malformations - 10 - EarAhmed H. Ali ElbestaweyNo ratings yet
- 2nd Ha To NguyenDocument1 page2nd Ha To NguyenAhmed H. Ali ElbestaweyNo ratings yet
- Human Malformations - 13 - TongueDocument19 pagesHuman Malformations - 13 - TongueAhmed H. Ali ElbestaweyNo ratings yet
- Systematic Evaluation of Fetal Anatomy at 11-14 WeeksDocument36 pagesSystematic Evaluation of Fetal Anatomy at 11-14 WeeksAhmed H. Ali ElbestaweyNo ratings yet
- Human Malformations - 09 - EyeDocument29 pagesHuman Malformations - 09 - EyeAhmed H. Ali ElbestaweyNo ratings yet
- Human Malformations - 11 - NoseDocument17 pagesHuman Malformations - 11 - NoseAhmed H. Ali ElbestaweyNo ratings yet
- Human Malformations - 08 - Facial BonesDocument30 pagesHuman Malformations - 08 - Facial BonesAhmed H. Ali ElbestaweyNo ratings yet
- Human Malformations - 12 - LipsDocument13 pagesHuman Malformations - 12 - LipsAhmed H. Ali ElbestaweyNo ratings yet
- 1st Seema PatilDocument1 page1st Seema PatilAhmed H. Ali ElbestaweyNo ratings yet
- When A Patient's Request PushedDocument2 pagesWhen A Patient's Request PushedAhmed H. Ali ElbestaweyNo ratings yet
- Congenital Malformations 14 MicrognathiaDocument4 pagesCongenital Malformations 14 MicrognathiaAhmed H. Ali ElbestaweyNo ratings yet
- 43849-Article Text-41744-1-10-20090701Document4 pages43849-Article Text-41744-1-10-20090701Ahmed H. Ali ElbestaweyNo ratings yet
- Human Malformations - 07 - SkullDocument46 pagesHuman Malformations - 07 - SkullAhmed H. Ali ElbestaweyNo ratings yet
- Devi 2011Document2 pagesDevi 2011Ahmed H. Ali ElbestaweyNo ratings yet
- Dynamic Supervision Concerning A Dynamic SupervisionDocument7 pagesDynamic Supervision Concerning A Dynamic SupervisionAhmed H. Ali ElbestaweyNo ratings yet
- Patient Trust in The Physician: Relationship To Patient RequestsDocument8 pagesPatient Trust in The Physician: Relationship To Patient RequestsAhmed H. Ali ElbestaweyNo ratings yet
- SAFEMOB Final18673Document2 pagesSAFEMOB Final18673Muhammad FarisNo ratings yet
- Physical Examination RetdemDocument4 pagesPhysical Examination RetdemCharlize PareNo ratings yet
- Vitamin D SecretsDocument37 pagesVitamin D SecretsSaheedNo ratings yet
- Siti Nur Haliza - Farmasi 1B - Task 1Document6 pagesSiti Nur Haliza - Farmasi 1B - Task 1Gio ArgyandraNo ratings yet
- Epinephrine Vs Norepinephrine: Advanced Pharmacology Dr. Sana' Al Aqqad by Students: Ali Ghanem Ismael Bani MatarDocument15 pagesEpinephrine Vs Norepinephrine: Advanced Pharmacology Dr. Sana' Al Aqqad by Students: Ali Ghanem Ismael Bani MatarSabrina ShalhoutNo ratings yet
- Major ProjectDocument11 pagesMajor Projectapi-662080993No ratings yet
- Infections Caused by ECTOPARASITESDocument14 pagesInfections Caused by ECTOPARASITESSteven CullcayyNo ratings yet
- Neurocognitive DisordersDocument40 pagesNeurocognitive DisordersShahanaz ChoudhuryNo ratings yet
- Drug AddictionDocument22 pagesDrug AddictionLynton OrebNo ratings yet
- Chest Pain Questionnaire - Attending PhysicianDocument2 pagesChest Pain Questionnaire - Attending PhysicianVia B. BorrezNo ratings yet
- Atopic DermatitisDocument8 pagesAtopic DermatitisAndrés Adarve GarcíaNo ratings yet
- Sindrome Cardio-Renal NejmDocument13 pagesSindrome Cardio-Renal NejmNOTAS GINECONo ratings yet
- Yuyun CaseDocument11 pagesYuyun CaseFitra InfitarNo ratings yet
- Code Blue Group-Psychiatry History FormatDocument10 pagesCode Blue Group-Psychiatry History FormatsakariyeNo ratings yet
- 07 Sepsis - Dr. Sutrisno, M.Kes., SP - OG., Subsp. ONK.Document31 pages07 Sepsis - Dr. Sutrisno, M.Kes., SP - OG., Subsp. ONK.Syahid PutraNo ratings yet
- Oral Squamous Cell Carcinoma in Patients Twenty Years of Age orDocument6 pagesOral Squamous Cell Carcinoma in Patients Twenty Years of Age orSezen AltındişNo ratings yet
- DT 103 (First Aid)Document32 pagesDT 103 (First Aid)Andrea Nicole O. AzurinNo ratings yet
- Seronegative SpondyloarthropathiesDocument35 pagesSeronegative SpondyloarthropathiesAmjad SobehNo ratings yet
- Self Completion Medical History Form - PregnancyDocument4 pagesSelf Completion Medical History Form - PregnancymerjenNo ratings yet
- VomitingDocument29 pagesVomitinganusrisaranganNo ratings yet
- ATLS 1.0 Mar 2018Document65 pagesATLS 1.0 Mar 2018Mahfilza MayubNo ratings yet
- Chief Complaints: Sl. Medicine Name Dosage Freq. Duration InstructionsDocument4 pagesChief Complaints: Sl. Medicine Name Dosage Freq. Duration InstructionsBanshi Lal MaanNo ratings yet
- Stroke Training in TweeterDocument8 pagesStroke Training in TweeterShirsho ShreyanNo ratings yet
- Movement Disorders of The Mouth Review of The Common Phenomenologies 2022Document19 pagesMovement Disorders of The Mouth Review of The Common Phenomenologies 2022Gonçalo CabralNo ratings yet
- Anemia BrochureDocument1 pageAnemia BrochureMel MasculinoNo ratings yet
- Epidemiologi, Stadium, Dan Derajat Diferensiasi Kanker Kepala Dan LeherDocument7 pagesEpidemiologi, Stadium, Dan Derajat Diferensiasi Kanker Kepala Dan LeherKhumaira SantaNo ratings yet