Professional Documents
Culture Documents
Houseman Paed Note 2020 2
Uploaded by
BrendaJooYee0 ratings0% found this document useful (0 votes)
6 views1 pageThis document provides instructions for the care of a newborn baby referred from the labor room with tachypnea. Upon examination, the baby's vital signs and physical exam are documented. The plan outlines admitting the baby for observation, starting oxygen therapy and monitoring, and watching for signs of respiratory distress or inability to wean from oxygen. The baby is also to be kept nothing by mouth initially and have close monitoring of vital signs and feeding tolerance. The document also provides standardized care plans for various other potential newborn conditions.
Original Description:
Original Title
Houseman paed note 2020 2
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides instructions for the care of a newborn baby referred from the labor room with tachypnea. Upon examination, the baby's vital signs and physical exam are documented. The plan outlines admitting the baby for observation, starting oxygen therapy and monitoring, and watching for signs of respiratory distress or inability to wean from oxygen. The baby is also to be kept nothing by mouth initially and have close monitoring of vital signs and feeding tolerance. The document also provides standardized care plans for various other potential newborn conditions.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views1 pageHouseman Paed Note 2020 2
Uploaded by
BrendaJooYeeThis document provides instructions for the care of a newborn baby referred from the labor room with tachypnea. Upon examination, the baby's vital signs and physical exam are documented. The plan outlines admitting the baby for observation, starting oxygen therapy and monitoring, and watching for signs of respiratory distress or inability to wean from oxygen. The baby is also to be kept nothing by mouth initially and have close monitoring of vital signs and feeding tolerance. The document also provides standardized care plans for various other potential newborn conditions.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
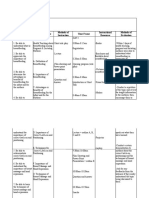
Paed referral in L/Room Normal __genitalia )B/L testes descended) Term low birth weight < 2kg
Inform MO if any tachypneic baby Anus: patent 1. Admit 6c
Spine: normal 2. For incubator care
For baby already born Hips: stable 3. Start feeding
Received referral from L/room for baby with tachypneic ______by O&G team No CTEV 4. W/o feeding intolerance and respiratory distress
Attended stat by me. Upon arrival ___am/pm, the baby was (condition of the baby with Moro complete, grasp reflex, suckling reflex 5. CBS at 4HOL and 4hourly
vital sign T, HR, SpO2 under RA/NPO2)
Plan: Term low birth weight 2-2.5kg
For standby (attend since birth) TTN: 1. Discharge to mother
Baby wa born vigorous with good cry, good respiratory effort and good muscle one with 1. Admit 6c 2. Start feeding
Apgar score of ___(1)___(5) 2. Put on NPO2 2l/Min 3. CBS at 4 HOL and 4 hourly for 24 hours
Put under radian warmer__(detailed) 3. Keep SpO2 >95 % % 4. If discharge, biweekly weighing at KK until BW>2.5kg, then weekly until BW>3kg
(condition of the baby, any respiratory distress) 4. Watch out for respiratory distress
??nasal flaring, ?grunting, ?tachypneic with RR of __ 5. If unable to wean off O2 by 6 HOL, for CXR Macrosomic baby 4-4.5kg
Recession, SpO2 under RA__, HR__, RR__ 6. Keep KBM with IVD D10% 1. Discharge to mother
The baby was put on neopuff: PEEP: 5 7. FBC and Blood C+S (if risk of sepsis)
Macrosomic baby >4.5kg
Maternal history Resolved TTN 1. Admit to 6C
Age: 1. Discharge to mother 2. CBS at 4 HOL and 4 hourly
Para: 2. Paed to review at 6 HOL and cm 3. Inform if CBS < 2.6 or symptomatic of hypoglycemia
MBG: 3. Encourage breast feeding
HIV/VDRL: 4. Watch out for respiratory distress Prematurity (<35 week or <2kg)
ANC: 1. Plot growth chart
1) Presenting complaint Risk of MAS if stable 2. Admit 6c for observation
2) Sure of date? LMP? EOD? 1. Discharge to mother 3. Keep NBM with IVD 10%
3) Significant antenatal scan 2. Paed to review at 6 HOL and cm 4. CBS at 4HOL and 4 hourly
4) Dexa scan 3. W/o s/sx of respiratory distress and sepsis 5. W/out for feeding intolerance
5) MgS04 (neuroprotection) 4. Encourage breast feeding
6) Past medical and surgical history 5. No need CBS monitoring Caput/ cephalohematoma
7) Significant pass obstetric history- early neonatal death/ Poor spacing/ History of 6. KIV discharge if well>24 hours 1. Allow disharge paed
miscarriages/ preterm deliveries 2. Breasfeeding
8) AFI & Droppler Risk of sepsis (PROM) if stable 3. Top up feeding
1. Discharge to mother 4. COH monitoring 4 hourly
Peripartum history: 2. Paed to review at 6 HOL and cm 5. Inform stat if caput increasing in size, jaundice and tender
1. ROM, duration of rupture, duration of second stage of labour 3. W/out s/sx of sepsis (fever/ tachycardia/tachypnea)
2. Medication in labour (e.g pethidine) 4. No need CBS monitoring SAH:
3. Maternal pyrexia? FBC? HVS C+S 5. Encourage breast feeding 1. Admit 6C
4. If PROM- covered? Doses? Last dose and time? Liquor colour 6. Trace mother’s HVS C+S 2. Start feeding
5. CTG abnormalities 3. Coagulation profile, KIV FFP
6. Cord round neck/ Placenta abruption Presumed sepsis 2nd to PROM/PPROM >18H (inadequately covered/ 4. COH monitoring hourly
7. Fetal distress (Cord blood gasses- Umbilical arterial and venous) chorioamnionitis) 5. Inform if COH increasing in size or hemodynamically unstable (tachycardia poor pulse
8. Placental Weight 1. Admit 6C volume, hypotension)
2. FBC and blood C+S
Baby history: 3. Start IV C penicillin and gentamycin Post resus care (PPV/ AS <6 at 5 min)
DOB: TOB: 4. Start IVD D10% for transportation 1. Admit 6c for observation
Gender: 5. Start feeding at ward 2. Start feeding
Mode of delivery/ gestation 6. W/out of sepsis (fever/ tachycardia/tachypnea) 3. W/O respiratory distress
Birth weight/ Length/ COH 7. Trace mother’s HVS C+S and placenta swab if taken 4. W/O feeding intolerance
Apgar score
GDM on d/c or s/c insulin
O/E: 1. Discharge to mother
Active on handling 2. Encourage breast feeding. To calculate how much feeding
Good tone, good PV, CRT <2sec 3. CBS at 4 HOL and 4 hourly
AFNT, no scalp swelling 4. Inform if CBS <2.6 or symptomatic of hypoglycemia
No ear/ eye abnormalities/ discharge 5. Paeds to review CM
No cleft palate/ lip palate
No dysmorphism
CVS: DRNM
Lungs: clear
Abdo:soft and non tender, hepatosplenomegaly
B/L femoral pulses felt
You might also like
- Paeds Code Pink CheatcodeDocument8 pagesPaeds Code Pink Cheatcodeafikah aimanNo ratings yet
- OBGYN TransDocument6 pagesOBGYN TransanonymousNo ratings yet
- OFFTAG QUESTION NEONATES by Fadhlin JamilDocument9 pagesOFFTAG QUESTION NEONATES by Fadhlin Jamiluzair muhdNo ratings yet
- Common ManagementDocument7 pagesCommon ManagementaslanNo ratings yet
- Labor Delivery NewbornDocument4 pagesLabor Delivery NewbornMello D. ConsulNo ratings yet
- Lecture-24 Twins PregnancyDocument30 pagesLecture-24 Twins PregnancyMadhu Sudhan PandeyaNo ratings yet
- 2 Delivery Room Rotation 3Document74 pages2 Delivery Room Rotation 3Jianne CaloNo ratings yet
- Shendi Obs OsceDocument35 pagesShendi Obs OsceYassin Jamal67% (3)
- High Risk Prenatal CareDocument4 pagesHigh Risk Prenatal CareKatherine Gayle GuiaNo ratings yet
- Maternal and Child Nursing Module 5Document4 pagesMaternal and Child Nursing Module 5Ezekiel John GarciaNo ratings yet
- Study ThisDocument30 pagesStudy ThisKamva DukadaNo ratings yet
- Cronology Event FarizDocument2 pagesCronology Event FarizsjamilmdfauzieNo ratings yet
- Flowchart 1 Immediate Management of An Asphyxiated NewbornDocument3 pagesFlowchart 1 Immediate Management of An Asphyxiated Newborndessy pratiwiNo ratings yet
- Multiple PregnancyDocument7 pagesMultiple PregnancyBiscuits and milkNo ratings yet
- Prenatal: Prepared byDocument94 pagesPrenatal: Prepared byHelenNo ratings yet
- Labor and Delivery Nursing Knowledge & Skills ChecklistDocument4 pagesLabor and Delivery Nursing Knowledge & Skills Checklistnorthweststaffing100% (4)
- Antenatal Fetal SurveillanceDocument115 pagesAntenatal Fetal SurveillanceNargis1000100% (1)
- Flowchart 1 Immediate Management of An AsphyxiatednewbornDocument3 pagesFlowchart 1 Immediate Management of An Asphyxiatednewborndessy pratiwiNo ratings yet
- PEDIA - 1st Sem Prelims FeedbackDocument3 pagesPEDIA - 1st Sem Prelims FeedbackEricNo ratings yet
- Care Plan Date: March 18, 2018 Student Name: Megan SeiferlingDocument1 pageCare Plan Date: March 18, 2018 Student Name: Megan SeiferlingMSNo ratings yet
- 1 High Risk Pregnancy Assessment and ManagementDocument48 pages1 High Risk Pregnancy Assessment and ManagementNeelofur Ibran Ali80% (5)
- Multiple GestationDocument4 pagesMultiple GestationCHRISNA AMMANG PASPASANNo ratings yet
- Changes During PregnancyDocument2 pagesChanges During PregnancyRalph Tama Mangacop BenitoNo ratings yet
- Multiple PregnancyDocument26 pagesMultiple PregnancyRaj PatelNo ratings yet
- General Guides To Daily Nicu Practice: Birth Weight (GM) Age To Start Feeding (Day)Document75 pagesGeneral Guides To Daily Nicu Practice: Birth Weight (GM) Age To Start Feeding (Day)Humayun NasserNo ratings yet
- Pre-Eclampsia and EclampsiaDocument19 pagesPre-Eclampsia and EclampsiaBiscuits and milkNo ratings yet
- Premature Rupture of Membranes (Prom)Document12 pagesPremature Rupture of Membranes (Prom)KABERA RENENo ratings yet
- Neonatal JaundiceDocument14 pagesNeonatal Jaundicewewewwe memeNo ratings yet
- MCN (Icons)Document7 pagesMCN (Icons)Angelica Charisse BuliganNo ratings yet
- History Clerking, Physical Examination of Obstetrics PatientsDocument9 pagesHistory Clerking, Physical Examination of Obstetrics PatientsCk Kma0% (1)
- M Questions 1Document351 pagesM Questions 1venture kulNo ratings yet
- DR Rot ReviewerDocument41 pagesDR Rot Reviewerwerismy daddyNo ratings yet
- Lecture-8 First Stage ManagementDocument10 pagesLecture-8 First Stage ManagementMadhu Sudhan PandeyaNo ratings yet
- Patient Admission Centre (Pac) (HRPZ Houseman Guide) : O&G HO Guide @thechayondeducationDocument25 pagesPatient Admission Centre (Pac) (HRPZ Houseman Guide) : O&G HO Guide @thechayondeducationNurulain HamzahNo ratings yet
- Obstetrics and Gynecology Intern HandbookDocument23 pagesObstetrics and Gynecology Intern HandbookMonna PaaktachaayNo ratings yet
- Gestational Conditions HandoutDocument17 pagesGestational Conditions HandoutFilamae Jayahr Caday100% (4)
- Maternal and Child NursingsDocument16 pagesMaternal and Child NursingsQueennie Hafsah K. PangandamanNo ratings yet
- MCN FinalsDocument13 pagesMCN FinalsMutya XDNo ratings yet
- Congenital HypothyroidismDocument16 pagesCongenital HypothyroidismEmily EresumaNo ratings yet
- ANC and BFDocument29 pagesANC and BFRose Anne Tusi BotinNo ratings yet
- SCNICU Starter PackDocument7 pagesSCNICU Starter PackALIF HAIQAL MOHD HUSSEINNo ratings yet
- Pedia S1Document22 pagesPedia S1betweenNo ratings yet
- History Taking: 1. DemographicsDocument12 pagesHistory Taking: 1. Demographicsanis jannahNo ratings yet
- Intrapartum Fetal Assessment Step 2Document3 pagesIntrapartum Fetal Assessment Step 2Andrew McGowanNo ratings yet
- Problems Related To Gestational Weight NotesDocument11 pagesProblems Related To Gestational Weight NotesODESSA GALOLONo ratings yet
- Gestational ConditionsDocument4 pagesGestational ConditionsHyacinth Mae Virtudazo RaganasNo ratings yet
- Abruptio Placenta Vs Placenta PreviaDocument1 pageAbruptio Placenta Vs Placenta PreviaMelcah Marie NacionalesNo ratings yet
- 4 - Poor FeedingDocument8 pages4 - Poor FeedingZeineddin EtkaidekNo ratings yet
- May 8-9Document5 pagesMay 8-9MineTagraNo ratings yet
- Fetal DistressDocument10 pagesFetal DistressLady Jane CaguladaNo ratings yet
- High Risk Pregnancy Assessment and ManagementDocument48 pagesHigh Risk Pregnancy Assessment and ManagementWilfredo PesanteNo ratings yet
- Fact Sheet MIN PDFDocument10 pagesFact Sheet MIN PDFDavid Underwood IINo ratings yet
- Transient Tachypneu of The Newborn: Supervisor: Dr. Nazardi Oyong Sp. ADocument57 pagesTransient Tachypneu of The Newborn: Supervisor: Dr. Nazardi Oyong Sp. AWella FadillahNo ratings yet
- Lecture-22 Prolonged PregnancyDocument24 pagesLecture-22 Prolonged PregnancyMadhu Sudhan PandeyaNo ratings yet
- Nicu ReportDocument66 pagesNicu ReportEr Shah Rukh QadriNo ratings yet
- MCN II AntepartumDocument28 pagesMCN II AntepartumJharaNo ratings yet
- Abnormal PuerperiumDocument23 pagesAbnormal PuerperiumLynee OlvianaNo ratings yet
- OBST 7010 Quiz 2 Review (Swan) : Week 2 - Antepartum CareDocument6 pagesOBST 7010 Quiz 2 Review (Swan) : Week 2 - Antepartum CareBridget MasonNo ratings yet
- Nursing Care of The High Risk NewbornDocument8 pagesNursing Care of The High Risk NewbornFebie GonzagaNo ratings yet
- Acute Flaccid Paralysis and Enteroviral InfectionsDocument15 pagesAcute Flaccid Paralysis and Enteroviral InfectionsBrendaJooYeeNo ratings yet
- MyPastest 3Document1 pageMyPastest 3BrendaJooYeeNo ratings yet
- Nausea and Vomiting Secondary To Hydronephrosis in Palliative PatientsDocument2 pagesNausea and Vomiting Secondary To Hydronephrosis in Palliative PatientsBrendaJooYeeNo ratings yet
- Conventional Phototherapy Level: Phototherapy & Exchange Transfusion Level For 35 Weeks Gestational Age, HRPB IpohDocument1 pageConventional Phototherapy Level: Phototherapy & Exchange Transfusion Level For 35 Weeks Gestational Age, HRPB IpohBrendaJooYeeNo ratings yet
- Tentative Quiz ProgrammeDocument1 pageTentative Quiz ProgrammeBrendaJooYeeNo ratings yet
- MyPastest 2Document1 pageMyPastest 2BrendaJooYeeNo ratings yet
- SLCC Anatomy CH 27: Urinary System: Study Online atDocument2 pagesSLCC Anatomy CH 27: Urinary System: Study Online atBrendaJooYeeNo ratings yet
- SLCC Anatomy CH 26-Digestive System: Study Online atDocument3 pagesSLCC Anatomy CH 26-Digestive System: Study Online atBrendaJooYeeNo ratings yet
- Quizlet CVSDocument2 pagesQuizlet CVSBrendaJooYeeNo ratings yet
- Quizlet Vessels and CirculationDocument2 pagesQuizlet Vessels and CirculationBrendaJooYee100% (2)
- Anatomy and Physiology - Chapter QuizDocument7 pagesAnatomy and Physiology - Chapter QuizBrendaJooYeeNo ratings yet
- Function: Voluntary and Involuntary Responses - AvivaDocument6 pagesFunction: Voluntary and Involuntary Responses - AvivaBrendaJooYeeNo ratings yet
- Multiple True False Past Year CompilationDocument9 pagesMultiple True False Past Year CompilationBrendaJooYeeNo ratings yet
- Excess Fluid VolumeDocument27 pagesExcess Fluid VolumeAdrian Ardamil100% (1)
- Formula FeedsDocument35 pagesFormula FeedsrandoNo ratings yet
- Date/Time Focus Data, Action, ResponseDocument3 pagesDate/Time Focus Data, Action, ResponseRoland Yuste100% (1)
- Postpartal Diabetes MellitusDocument7 pagesPostpartal Diabetes Mellitusnursereview100% (3)
- Nutrition During InfancyDocument4 pagesNutrition During InfancyMaryHope100% (1)
- Argument EssayDocument6 pagesArgument Essayapi-415388585No ratings yet
- Learning Objectives Content Outline Methods of Instruction Time Frame Instructional Resources Methods of EvaluationDocument3 pagesLearning Objectives Content Outline Methods of Instruction Time Frame Instructional Resources Methods of EvaluationteuuuuNo ratings yet
- Case Study - Full-Term BabyDocument32 pagesCase Study - Full-Term BabyMarron Jane GanoticeNo ratings yet
- Case Simulation in Pediatric Nursing Case Study 1Document4 pagesCase Simulation in Pediatric Nursing Case Study 1Cheska PalomaNo ratings yet
- Engorgement Post Partum: Merry C.ODocument12 pagesEngorgement Post Partum: Merry C.OmerycoNo ratings yet
- Tips For Triage NursesDocument4 pagesTips For Triage NursesCamille05No ratings yet
- Breastfeeding Benefits HandoutDocument4 pagesBreastfeeding Benefits Handoutapi-313912304No ratings yet
- Manual of Prototype Clinical Histories.: GeorgeDocument41 pagesManual of Prototype Clinical Histories.: Georgemacdominic22No ratings yet
- Child Care StandardsDocument44 pagesChild Care StandardsAnonymous UpWci5100% (1)
- Pari SynopsisDocument37 pagesPari SynopsisamitNo ratings yet
- Objectives:: Module On Basic NutritionDocument56 pagesObjectives:: Module On Basic NutritionMomhai Mhaimo100% (1)
- Pengaruh Pemberian Puding Daun Kelor (Moringa Oleifera) Terhadap Produksi Air Susu Ibu (ASI) Pada Ibu Menyusui Di Wilayah Kerja Puskesmas Kelurahan Cawang Jakarta TimurDocument8 pagesPengaruh Pemberian Puding Daun Kelor (Moringa Oleifera) Terhadap Produksi Air Susu Ibu (ASI) Pada Ibu Menyusui Di Wilayah Kerja Puskesmas Kelurahan Cawang Jakarta TimurAesthetic GirlNo ratings yet
- Postpartum Discharge InstructionsDocument7 pagesPostpartum Discharge InstructionsGilianne JimeneaNo ratings yet
- Pediatrics Case StudyDocument27 pagesPediatrics Case StudyPhelanCoy100% (1)
- Breastfeeding Techniques-Lesson PlanDocument12 pagesBreastfeeding Techniques-Lesson Planmonika makwanaNo ratings yet
- Ob ExamDocument8 pagesOb ExamRamones JokerNo ratings yet
- 2015-Hsc-Biology 15Document44 pages2015-Hsc-Biology 15Will NguyenNo ratings yet
- Spectra Baby USA Flange Guide 2022Document1 pageSpectra Baby USA Flange Guide 2022Celia MoonNo ratings yet
- KMC FinalDocument36 pagesKMC FinalGandimarei100% (2)
- GAD Plan Template With HAGADAGADocument54 pagesGAD Plan Template With HAGADAGAJenny NacuaNo ratings yet
- Demonstration ON Care of Newborn PhototherapyDocument28 pagesDemonstration ON Care of Newborn PhototherapyA J Fathima100% (1)
- 20050-Article Text-95231-1-10-20221219Document9 pages20050-Article Text-95231-1-10-20221219adindaNo ratings yet
- 10 - Nutrition During Infancy, Childhood and AdolescenceDocument45 pages10 - Nutrition During Infancy, Childhood and AdolescenceMaria Victoria A. PraxidesNo ratings yet
- Government College of Nursing:, Jodhpur (Raj.)Document7 pagesGovernment College of Nursing:, Jodhpur (Raj.)priyankaNo ratings yet
- Appendix B:: 2007-2008 NANDA-APPROVED Nursing DiagnosesDocument1 pageAppendix B:: 2007-2008 NANDA-APPROVED Nursing DiagnosesKim RamosNo ratings yet