Professional Documents
Culture Documents
J Yogaratnam 2013 Asia Piola PDF
Uploaded by
Camila RosenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
J Yogaratnam 2013 Asia Piola PDF
Uploaded by
Camila RosenCopyright:
Available Formats
East Asian Arch Psychiatry 2013;23:21-8 Review Article
Metabolic Complications of Schizophrenia
and Antipsychotic Medications — An Updated
Review
精神分裂症和抗精神病藥引發的代謝併發症:更新回顧
J Yogaratnam, N Biswas, R Vadivel, R Jacob
Abstract
Metabolic syndrome is a cluster of risk factors comprising obesity, dyslipidaemias, glucose intolerance,
insulin resistance (or hyperinsulinaemia), and hypertension, and is highly predictive of type 2 diabetes
mellitus and cardiovascular disease. The life expectancy of people with schizophrenia is reduced by 20%,
with 60% of the excess mortality due to physical illness. Schizophrenia itself may be a risk factor for
metabolic syndrome and there is also increasing concern that antipsychotic drugs, particularly second-
generation antipsychotics, have metabolic consequences that contribute to the risk. Various diagnostic
guidelines, updated facts with regard to epidemiology, pathophysiology, risk factors, and complications
of metabolic syndrome are discussed in this review. Moreover, the impact of various antipsychotics
on metabolic syndrome and their possible mechanisms are comprehensively reviewed. The authors
emphasise that, while many adults with schizophrenia receive little or no medical care, such care is
important given the risk of metabolic abnormalities associated not only with antipsychotic medications,
but also with schizophrenia in general.
Key words: Antipsychotic agents; Metabolic syndrome X; Metabolism; Schizophrenia
摘要
代謝綜合症是肥胖、血脂異常、葡萄糖耐受不良、胰島素抗性(或稱高胰島素血症)和高血壓
等的風險因素群,並且能高度預測二型糖尿病和心血管疾病。精神分裂症患者的壽命一般縮短
20%,而因身體疾病導致的額外死亡率也達到60%。精神分裂症本身也許是代謝綜合症的風險
因素,而抗精神病藥,尤其是第二代抗精神病藥對代謝功能的影響也漸受關注。本文回顧並討
論代謝綜合症各種診斷指南以及有關其流行病學、病理生理學以及風險因素和併發症的最新資
訊。本文也回顧各種抗精神病藥對代謝綜合症的影響和其可能機制。代謝異常的風險不僅與抗
精神病藥,且與精神分裂症相關。因此,在現行對成人精神分裂症患者相關護理不足甚至缺乏
的情況下,作者強調它的重要性。
關鍵詞:抗精神病藥、代謝綜合症、代謝、精神分裂症
Dr Jegan Yogaratnam, MBBS, MD, Institute of Mental Health / Woodbridge intolerance, insulin resistance (or hyperinsulinaemia), and
Hospital, Singapore.
Dr Neetesh Biswas, MBBS, Institute of Mental Health / Woodbridge Hospital,
hypertension, and is highly predictive of type 2 diabetes
Singapore. mellitus and cardiovascular disease.1 The mean age of
Dr Ramyadarshni Vadivel, MBBS, Institute of Mental Health / Woodbridge death is 61 years for patients with schizophrenia, which
Hospital, Singapore.
Dr Rajesh Jacob, MBBS, MD, Institute of Mental Health / Woodbridge Hospital,
is considerably younger than 76 years for the general
Singapore. population.2 Life expectancy in people with schizophrenia
is reduced by 20%,3 with 60% of the excess mortality due
Address for correspondence: Dr Jegan Yogaratnam, Woodbridge Hospital /
Institute of Mental Health, 10 Buangkok View, Singapore 539747.
to physical illness.4
Tel: (65) 6389 2000; Fax: (65) 6385 5900; email: jegany@gmail.com Schizophrenia itself may be a risk factor for metabolic
syndrome in addition to many other factors in patients
Submitted: 25 June 2012; Accepted: 10 September 2012
with schizophrenia, and there is also increasing concern
that antipsychotic drugs, particularly second-generation
Introduction antipsychotics (SGAs), have metabolic consequences that
contribute to the risk.5 The precise relationship between
Metabolic syndrome is a cluster of risk factors comprising antipsychotic drugs and metabolic syndrome remains
obesity (central and abdominal), dyslipidaemias, glucose uncertain, but it is clear that people with schizophrenia
© 2013 Hong Kong College of Psychiatrists 21
J Yogaratnam, N Biswas, R Vadivel, et al
treated with antipsychotic medications develop individual Americans, 22% of US adults, and 32% of Mexican
features of metabolic syndrome, and the syndrome itself, Americans17 estimated to have the condition. Additionally,
at a higher rate than the general population. Antipsychotic metabolic syndrome is considered an emerging epidemic in
polypharmacy, which is a common practice in many developing East-Asian countries, including China, Japan,
psychiatric settings, as compared with monotherapy, and Korea, where the prevalence ranged from 8 to 13% in
may be independently associated with increased risk of men and 2 to 18% in women depending on the population
pre-metabolic syndrome and higher rates of metabolic and definitions used.18 Even in many other countries
syndrome and lipid markers of insulin resistance, even worldwide, metabolic syndrome has been recognised as a
after adjusting for patients’ lifestyle characteristics.6,7 A highly prevalent health problem19 demanding attention and
recent study concluded that switching to monotherapy was intervention. The exact prevalence of metabolic syndrome
appropriate and reasonable as long as patients could return in patients with schizophrenia is unknown. Using baseline
to polypharmacy when necessary, and switching from a data from the Clinical Antipsychotic Trials of Intervention
higher- to a lower-risk agent or from polypharmacy to Effectiveness (CATIE) schizophrenia trial, the prevalence
monotherapy may facilitate metabolic improvement.8 of metabolic syndrome was 40.9% and 42.7% according
Many reviews have concluded that there is a need for to the NCEP and the American Heart Association /
active routine physical health screening of all individuals National Heart, Lung, and Blood Institute–derived criteria,
receiving treatment with antipsychotic drugs,9 which is in respectively.20
keeping with the recommendations of the National Institute
for Health and Clinical Excellence treatment guidelines Pathophysiology of Metabolic Syndrome
for schizophrenia. While many adults with schizophrenia
receive little or no medical care, such care is important, Metabolic syndrome is thought to be caused by adipose
given the risk of metabolic abnormalities associated not only tissue dysfunction and insulin resistance. Dysfunctional
with antipsychotic medications, but also with schizophrenia adipose tissue results in the release of proinflammatory
in general.10 cytokines such as tumour necrosis factor, adiponectin, leptin,
resistin, and plasminogen activator inhibitor, which play an
Diagnostic Guidelines for Metabolic Syndrome important role in the pathogenesis of obesity-related insulin
resistance, the primary mediator of metabolic syndrome.21
Guidelines for diagnosis of metabolic syndrome are listed
in Table 1.1,11-15 The most commonly used definitions Risk Factors for Metabolic Syndrome in
for metabolic syndrome are in keeping with the Adult Patients with Schizophrenia
Treatment Panel III (ATP III) of the National Cholesterol
Education Program (NCEP) definition and the adapted People with schizophrenia on average have a sedentary
ATP III recommendation proposed by the American Heart lifestyle involving lack of regular physical activity, poor food
Association which follows the International Diabetes intake, substance abuse, and high rates of smoking,22 which
Federation (IDF) guideline of lowering the threshold for increase their risk for development of metabolic syndrome
impaired fasting glucose to 5.56 mmol/L (100 mg/dL).11 in addition to the risk from antipsychotic medications.
An important difference between the NCEP / ATP III and These lifestyle factors are partly influenced by aspects of
the IDF definitions is that of the values for central obesity, the illness such as negative symptoms and vulnerability to
which are defined as > 102 cm for men and > 88 cm for stress. Moreover, earlier studies have shown an increased
women in the NCEP / ATP III definition, the IDF values are risk for people with schizophrenia to develop metabolic
comparatively lower at 94 cm and 80 cm, respectively, with abnormalities in the absence of antipsychotic medication,
a lower value of 80 cm for South-Asian men.16 and there are indications of an increased risk for diabetes in
first-degree relatives of patients with schizophrenia.23
Epidemiology of Metabolic Syndrome Other possibilities to explain these associations
in schizophrenia include stress and abnormalities of the
Metabolic syndrome is a burgeoning global problem, hypothalamic-pituitary-adrenal axis.24 A study showed that
with approximately 25% of adult Europeans and Latin people with schizoaffective disorder are more vulnerable
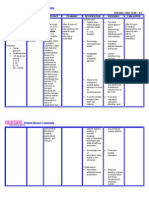
Table 1. Diagnostic guidelines for metabolic syndrome.
• American Heart Association / National Heart, Lung, and Blood Institute (2004)1
• International Diabetes Federation (2005)11
• World Health Organization (1998)12
• European Group for the Study of Insulin Resistance (1999)13
• American Diabetes Association (2003)14
• National Cholesterol Education Program Adult Treatment Panel III (2001)15
22 East Asian Arch Psychiatry 2013, Vol 23, No.1
Metabolic Complications of Schizophrenia and Antipsychotics
to metabolic syndrome than people with schizophrenia for dyslipidaemia and hypertension in the absence of type 2
unexplained reasons.25 diabetes mellitus) may be mechanistically linked to lower
academic and professional potential in adolescents, as lower
Complications of the Metabolic Syndrome cognitive performance and reduction in brain structural
integrity among adolescents with metabolic syndrome has
The complications of metabolic syndrome are broad. Table been documented in studies.32
226-30 shows that metabolic syndrome is a multisystem While there appears to be a dose-dependent
disorder involving the cardiovascular, hepatobiliary, and relationship between the dose of clozapine or olanzapine
central nervous / psychological systems. and metabolic complications, aripiprazole, quetiapine,
and ziprasidone do not show a causal relationship, and
Antipsychotics and Metabolic Syndrome risperidone has mixed results.33
Notwithstanding the therapeutic effectiveness of Antipsychotics and Weight Gain
antipsychotic drugs in many illnesses such as schizophrenia,
increased attention has turned to the possible deleterious Interestingly, an independent association between
side-effects of these agents. Metabolic derangements schizophrenia and physical illnesses that have a metabolic
associated with antipsychotic agents have been the focus signature, including obesity, has been proposed, with
of considerable interest and debate for many years. While several studies reporting significantly higher (p < 0.001)
metabolic syndrome affects all ages of patients who take prevalences of overweight (body mass index [BMI]
antipsychotic medications, children and adolescents ≥ 25 kg/m2) and obesity (BMI > 30 kg/m2) in patients with
receiving atypical antipsychotic medications are particularly psychotic disorders than in the general population.34 Drug-
vulnerable to these effects.31 Notably, obesity-associated naïve schizophrenia patients have also been found to have
metabolic disease short of type 2 diabetes mellitus (i.e. more than 3 times as much intra-abdominal fat (which
Table 2. Complications of metabolic syndrome.26-30
System Complication
Cardiovascular Coronary heart disease, atrial fibrillation,26 heart failure, aortic stenosis
Hepatobiliary Non-alcoholic fatty liver disease27
Central nervous system / psychological Ischaemic stroke, accelerated cognitive ageing, anger, depression, hostility28
Cancer Breast, colon, gall bladder, kidney, prostate gland, hepatocellular
carcinoma,29 and intrahepatic cholangiocarcinoma
Other Obstructive sleep apnoea, association with psoriasis30
Table 3. Relationship between second-generation antipsychotic medications and metabolic abnormalities.38
Drug Weight gain Risk for type 2 diabetes mellitus Worsening lipid profile
Clozapine +++ +++ +++
Olanzapine +++ +++ +++
Risperidone ++ ++ / + +
Quetiapine ++ ++ ++ / +
Aripiprazole* +/– +/– +
Ziprasidone* +/– + +
Amisulpride* +/– – –
Paliperidone* + + +
Asenapine* ++ / + + D
Iloperidone* ++ / + + D
Bifeprunox* +/– +/– D
Abbreviations: + = increased effect; – = no effect; D = discrepant results.
*
Newer drugs with limited long-term data.
East Asian Arch Psychiatry 2013, Vol 23, No.1 23
J Yogaratnam, N Biswas, R Vadivel, et al
is correlated with insulin resistance) as age- and BMI- with lower rates of weight gain. A genetic predisposition
matched control participants,35 supporting the independent for aberrant folate metabolism and hyperhomocysteinaemia
association between psychosis and weight gain. Additionally, and genetic markers, such as 5-hydroxytryptamine (5-HT)
weight gain typically occurs within the first 4 to 12 weeks 2C receptor and brain-derived neurotrophic factor, and
of treatment and may not reach a plateau.36 blockade of the serotonin receptor 5-HT2C have also been
While the prevalence of obesity in the medicated linked to risk for weight gain.43
schizophrenic population is currently estimated to range from
40 to 60% versus 30% of the general adult population, the Antipsychotics and Diabetes Mellitus
differences between typical and atypical agents with regard
to the risk for weight gain and disorders of carbohydrate and Additional studies have found the prevalence of both
lipid metabolism remain unclear, although weight gain and diabetes and obesity to be 2 to 4 times higher in people
carbohydrate and lipid metabolism disorders may be more with schizophrenia than in the general population, with
common in patients taking atypical agents.9 Several studies overall prevalence estimates for diabetes among patients
have supported the claim that treatment with atypical with schizophrenia ranging from 16 to 25%.44 Poor
antipsychotics was associated with more weight gain than outcomes for diabetes in patients with schizophrenia are
treatment with typical antipsychotics.37,38 due to the reasons that their high rates of smoking (up to
Of the typical antipsychotics, lower potency agents 75%) worsens the prognosis of diabetes and increases non-
(chlorpromazine and thioridazine) induce greater weight gain adherence to treatment for diabetes, which is estimated to
than higher potency drugs (fluphenazine and haloperidol). be about 50%.45 Most cases of new-onset type 2 diabetes
Typical antipsychotic-associated weight gain appears to caused by antipsychotic medications occur within the first
be comparable for oral and depot formulations of the same 6 months of treatment and are often, although not always,
drug.39 Of those atypical antipsychotics (SGAs), clozapine associated with significant weight gain or obesity. A family
and olanzapine appear to have the greatest propensity history of diabetes is also associated with an increased risk
to induce weight gain, quetiapine and risperidone have in this population.46
intermediate risk, followed by aripiprazole, ziprasidone, and A large population-based case-control study found
amisulpride which carry the least risk (Table 338). Weight the risk of diabetes associated with antipsychotic agents
gain associated with risperidone and quetiapine does appear to be quite variable.46 Olanzapine and risperidone had 4.2
to correlate with dose, and newer antipsychotics such as and 1.6 times the risk associated with conventional agents,
bifeprunox, asenapine, iloperidone, and paliperidone are and 5.8 and 2.2 times the risk associated with no treatment,
known to cause low weight gain.40 respectively. Several large retrospective population studies
The mechanism of antipsychotic-induced weight gain have found that olanzapine and clozapine are associated
is undetermined, but several neurotransmitter systems have with a significantly higher rate of diabetes than the other
been implicated (Table 441,42). Olanzapine, which has the agents, with a particular risk for younger patients.47
highest affinity for histaminic receptors, is associated with Quetiapine appears to be more likely than conventional
high rates of weight gain, while ziprasidone and aripiprazole, drugs to be associated with diabetes, but may ameliorate
with lower affinities for histamine receptors, are associated clozapine-related diabetes when given in conjunction with
Table 4. Mechanisms of metabolic complications of antipsychotic medications.41,42
Metabolic complication Possible mechanism
Weight gain • Histamine receptor blockade
• Blockade of the serotonin receptor 5-HT2C
• Aberrant folate metabolism and hyperhomocysteinaemia
• Genetic markers, such as 5-HT2C receptors
• Brain-derived neurotrophic factor levels
Diabetes mellitus / hyperlipidaemia • Weight gain
• Disruption of hypothalamic regulation of glucose serum levels
• Potent anticholinergic activity
• Hyperprolactinaemia
• Others:
o 5-HT2A / 5-HT2C antagonism
o Weight gain
o Leptin resistance
Abbreviation: 5-HT = 5-hydroxytryptamine.
24 East Asian Arch Psychiatry 2013, Vol 23, No.1
Metabolic Complications of Schizophrenia and Antipsychotics
clozapine.48 Data for aripiprazole and ziprasidone suggested Typical versus Atypical Antipsychotic
that neither drug alters glucose homeostasis. Aripiprazole Medications in Metabolic Syndrome
may even reverse diabetes caused by other drugs, although
ketoacidosis has been reported with aripiprazole.49 Although most of the emphasis on metabolic syndrome
Among the traditional neuroleptics, chlorpromazine and is aimed at SGAs, several studies have failed to detect
thioridazine50 are the agents most closely associated with differences in the prevalences of metabolic syndrome
diabetes mellitus, although the associations are weaker between patients taking SGAs and those taking conventional
than those with olanzapine or clozapine. The prevalence antipsychotic agents.59 It may be possible that the effects
of impaired glucose tolerance seems to be higher with of conventional antipsychotic agents on metabolic
aliphatic phenothiazines than with fluphenazine or symptoms have been underestimated. Support for this
haloperidol, although haloperidol has been reported to possibility comes from a study that compared olanzapine
increase insulin resistance and to be associated with higher and haloperidol in patients with first-episode psychosis — a
fasting glucose levels in obese women compared with group of patients who were comparatively free of previous
control participants.51 treatment and symptom chronicity.60 After 2 years, patients
Interestingly, some studies have suggested that first- taking olanzapine had gained a mean of 33.9 lb (15.4
generation antipsychotics are no different from SGAs in kg), and those taking haloperidol had gained 16.5 lb (7.5
their propensity to cause diabetes, whereas others have kg) —a considerable weight gain indicating that typical
suggested a modest, but statistically significant excess antipsychotic agents are associated with weight gain and
incidence of diabetes with SGAs.52 related metabolic abnormalities. A recent systematic review
A number of mechanisms for antipsychotic compared the metabolic effects among the different SGAs
medication–induced diabetes mellitus have been and showed that clozapine and olanzapine had the highest
suggested, although none has been proven with certainty incidences.61
(Table 441,42). While drug-induced weight gain has been
highly associated with diabetes, diabetes has occurred in Management Strategies for Metabolic
the absence of weight gain, and hypothalamic dopamine Syndrome
antagonism by antipsychotic medications or disruption
of hypothalamic regulation of glucose serum levels have The following strategies have been suggested for directly
been suggested, along with potent anticholinergic-induced caused adverse effects of antipsychotic agents on glucose–
inhibition of insulin secretion.53 Other mechanisms insulin homeostasis and lipid metabolism:
suggested include increased insulin resistance in peripheral 1. Patients with previously diagnosed diabetes mellitus
tissues caused by hyperprolactinaemia, 5-HT2A / 5-HT2C and / or hyperlipidaemia should be given conventional
antagonism, increased lipids, weight gain, and leptin antipsychotic agents or atypical agents such as
resistance.54 aripiprazole, which have no or few effects on glucose-
insulin homeostasis and lipid metabolism.62
Antipsychotics and Hyperlipidaemia 2. For patients who develop hyperinsulinaemia and /
or hyperlipidaemia during treatment with clozapine,
Phenothiazines are known to be associated with increased olanzapine, or structurally related agents, a change to
levels of triglycerides and low-density lipoprotein an antipsychotic drug with no or minimal capability
cholesterol and a decreased level of high-density to induce such adverse metabolic effects should be
lipoprotein cholesterol.55 Higher cholesterol levels have considered, or maintenance therapy with the lowest
been reported with chlorpromazine-treated patients than effective dose possible, together with regular follow-
those receiving haloperidol.56 The CATIE study showed up of metabolic parameters and appropriate treatment
that of the atypical antipsychotic agents, olanzapine and whenever necessary, is advised.62
quetiapine are associated with increases in total cholesterol 3. For patients who develop diabetes mellitus during
levels and triglyceride levels.56 Notably, risperidone and therapy with antipsychotic agents, a change to an
ziprasidone are associated with decreases in cholesterol and antipsychotic agent with no or little propensity to
triglyceride levels, and patients treated with clozapine have cause the condition is the first recommendation. For
triglyceride levels that are almost double those treated with patients taking clozapine, the lowest effective dose
typical antipsychotic agents.57 Aripiprazole and ziprasidone possible should be given, with clinical evaluation and
have minimal adverse effects on blood lipids and may determination of serum antipsychotic concentration,
even reverse dyslipidaemias associated with previous along with concomitant therapy for hyperlipidaemia /
antipsychotic use.58 hyperglycaemia.62
Although the exact mechanism of causation of
hyperlipidaemia is unknown, one or more of the mechanisms General Advice for Prevention of the
described above as causes for antipsychotic medication– Development of Metabolic Syndrome
induced diabetes mellitus (Table 338) may be involved in the
pathogenesis. 1. All patients who are going to start treatment with, or
East Asian Arch Psychiatry 2013, Vol 23, No.1 25
J Yogaratnam, N Biswas, R Vadivel, et al
are already using an antipsychotic drug with high or yearly. Patients prescribed clozapine, olanzapine,
intermediate propensity to induce weight gain should quetiapine, or phenothiazines should ideally have
undergo regular monitoring of weight and lifestyle their serum lipids measured every 3 months for the
modifications / therapy such as dietary adjustments, first year of treatment.
weight reduction, and physical training, if necessary. 4. Weight (including waist circumference and BMI, if
2. If such a patient gains a considerable amount of weight possible) should be measured at baseline, frequently
or has become overweight or obese already, a change for 3 months, and then yearly.
of the antipsychotic agent to a less weight-inducing
drug should be considered. Another possibility to Conclusion
decrease antipsychotic-induced weight gain may be
dose reduction. In the general population, controlled In summary, while many adults with schizophrenia
clinical trials have established modest efficacy receive little or no medical care, such care is important
for obesity drugs in combination with lifestyle given the risk of metabolic abnormalities and metabolic
therapy.63 Orlistat (a lipase inhibitor) and sibutramine syndrome associated with schizophrenia and with the
(a serotonin-dopamine-norepinephrine reuptake antipsychotic medications used to treat the condition. There
inhibitor) are the only drugs currently approved for is a need for active routine physical health screening of all
long-term weight loss. individuals receiving treatment with antipsychotic drugs.
3. Interventions to stop cigarette smoking and to reduce The implementation of such guidelines can substantially
physical inactivity are also of great importance in improve the health of patients with schizophrenia.
decreasing the risk of insulin resistance and type 2 However, adopting the guidelines in clinical practice can
diabetes mellitus in patients treated with antipsychotic be challenging.
agents.63
4. In order to further decrease the risk for development References
of insulin resistance and type 2 diabetes mellitus in
antipsychotic medication–treated patients, daytime 1. Grundy SM, Brewer HB Jr, Cleeman JI, Smith SC Jr, Lenfant C;
sedation caused by these drugs, leading to physical American Heart Association; National Heart, Lung, and Blood Institute.
inactivity, has to be recognised and handled properly.63 Definition of metabolic syndrome: Report of the National Heart, Lung,
and Blood Institute / American Heart Association conference on
5. Psychiatrists also have to be aware of those
scientific issues related to definition. Circulation 2004;109:433-8.
antipsychotic medication–treated patients who 2. Newman SC, Bland RC. Mortality in a cohort of patients with
are older, have a family history of type 2 diabetes schizophrenia: a record linkage study. Can J Psychiatry 1991;36:239-
mellitus, and / or are of an ethnic group with high 45.
genetic susceptibility to type 2 diabetes mellitus 3. Mazi-Kotwal N, Upadhyay B. Physical health in schizophrenia.
Cutting Edge Psychiatry in Practice 2011;1:74-7.
(e.g. American Indians, Mexican Americans, and
4. Barnes TR, Kerwin R. Mortality and sudden death in schizophrenia.
Hispanics) and, therefore, have an increased risk of In: Camm J, editor. Cardiovascular risk associated with schizophrenia
developing insulin resistance and type 2 diabetes and its treatment. London: Galliard Healthcare Communications;
mellitus.63 2003: 7-23.
5. Haddad PM. Antipsychotics and diabetes: review of non-prospective
Screening and Monitoring during the Use of data. Br J Psychiatry Suppl 2004;47:S80-6.
6. Reynolds GP, Kirk SL. Metabolic side effects of antipsychotic
Antipsychotic Medications drug treatment — pharmacological mechanisms. Pharmacol Ther
2010;125:169-79.
In view of the evidence for an increased prevalence of 7. Misawa F, Shimizu K, Fujii Y, Miyata R, Koshiishi F, Kobayashi M, et
metabolic syndrome in schizophrenia, individuals presenting al. Is antipsychotic polypharmacy associated with metabolic syndrome
with a first episode of psychosis should be screened using the even after adjustment for lifestyle effects? A cross-sectional study.
appropriate diagnostic criteria.15 According to the Maudsley BMC Psychiatry 2011;11:118.
8. Essock SM, Schooler NR, Stroup TS, McEvoy JP, Rojas I, Jackson C,
guidelines,40 metabolic parameters should be measured with et al. Effectiveness of switching from antipsychotic polypharmacy to
the frequency as described below: monotherapy. Am J Psychiatry 2011;168:702-8.
1. Plasma glucose (fasting blood sample, if possible) 9. Mackin P, Watkinson HM, Young AH. Prevalence of obesity, glucose
should be done at baseline, at 4 to 6 months, and then homeostasis disorders and metabolic syndrome in psychiatric patients
yearly. Ideally, all patients should have oral glucose taking typical or atypical antipsychotic drugs: a cross-sectional study.
Diabetologia 2005;48:215-21.
tolerance tests performed as this is the most sensitive 10. Hägg S, Joelsson L, Mjörndal T, Spigset O, Oja G, Dahlqvist R.
method of detection of diabetes mellitus. Fasting Prevalence of diabetes and impaired glucose tolerance in patients
plasma glucose tests are less sensitive but are still treated with clozapine compared with patients treated with conventional
recommended. depot neuroleptic medications. J Clin Psychiatry 1998;59:294-9.
2. Blood pressure should be measured at the baseline 11. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome — a new
world-wide definition. A Consensus Statement from the International
and frequently during dose titration. Diabetes Federation. Diabet Med 2006;23:469-80.
3. Fasting blood lipids (cholesterol and triglycerides) 12. Alberti KG, Zimmet PZ. Definition, diagnosis and classification
should be measured at baseline, at 3 months, and then of diabetes mellitus and its complications. Part 1: Diagnosis and
26 East Asian Arch Psychiatry 2013, Vol 23, No.1
Metabolic Complications of Schizophrenia and Antipsychotics
classification of diabetes mellitus, provisional report of a WHO review. J Clin Psychiatry 2009;70:1041-50.
commission. Diabet Med 1998;15:539-53. 34. Allison DB, Fontaine KR, Heo M, Mentore JL, Cappelleri JC, Chandler
13. Balkau B, Charles MA. Comment on the provisional report from LP, et al. The distribution of body mass index among individuals with
the WHO consultation. European Group for the Study of Insulin and without schizophrenia. J Clin Psychiatry 1999;60:215-20.
Resistance (EGIR). Diabet Med 1999;16:442-3. 35. Thakore JH, Mann JN, Vlahos I, Martin A, Reznek R. Increased
14. Bloomgarden ZT. American Diabetes Association Annual Meeting, visceral fat distribution in drug-naive and drug-free patients with
June 2003. Gastrointestinal and dietary aspects of diabetes. Diabetes schizophrenia. Int J Obes Relat Metab Disord 2002;26:137-41.
Care 2003;26:2941-6. 36. Tschoner A, Engl J, Laimer M, Kaser S, Rettenbacher M, Fleischhacker
15. Expert Panel on Detection, Evaluation, and Treatment of High Blood WW, et al. Metabolic side effects of antipsychotic medication. Int J
Cholesterol in Adults. Executive Summary of The Third Report of Clin Pract 2007;61:1356-70.
The National Cholesterol Education Program (NCEP) Expert Panel on 37. Allison DB, Casey DE. Antipsychotic-induced weight gain: a review
Detection, Evaluation, And Treatment of High Blood Cholesterol In of the literature. J Clin Psychiatry 2001;62 Suppl 7:S22-31.
Adults (Adult Treatment Panel III). JAMA 2001;285:2486-97. 38. McIntyre RS, Mancini DA, Basile VS. Mechanisms of antipsychotic-
16. Wildman RP, Gu D, Reynolds K, Duan X, He J. Appropriate body induced weight gain. J Clin Psychiatry 2001;62 Suppl 23:S23-9.
mass index and waist circumference cutoffs for categorization of 39. Llorente MD, Urrutia V. Diabetes, psychiatric disorders, and the
overweight and central adiposity among Chinese adults. Am J Clin metabolic effects of antipsychotic medications. Clin Diabetes
Nutr 2004;80:1129-36. 2006;24:18-24.
17. Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome 40. Taylor D, Paton C, Kerwin R. The Maudsley prescribing guidelines.
among US adults: findings from the third National Health and Nutrition 9th ed. London, Routledge; 2007.
Examination Survey. JAMA 2002;287:356-9. 41. Hasnain M, Fredrickson SK, Vieweg WV, Pandurangi AK. Metabolic
18. Hoang KC, Le TV, Wong ND. The metabolic syndrome in East Asians. syndrome associated with schizophrenia and atypical antipsychotics.
J Cardiometab Syndr 2007;2:276-82. Curr Diab Rep 2010;10:209-16.
19. Hu G, Lindström J, Jousilahti P, Peltonen M, Sjöberg L, Kaaja R, et al. 42. Clark NG. Consensus development conference on antipsychotic drugs
The increasing prevalence of metabolic syndrome among Finnish men and obesity and diabetes. Diabetes Care 2004;27:596-601.
and women over a decade. J Clin Endocrinol Metab 2008;93:832-6. 43. Zhang XY, Zhou DF, Wu GY, Cao LY, Tan YL, Haile CN, et al. BDNF
20. McEvoy JP, Meyer JM, Goff DC, Nasrallah HA, Davis SM, levels and genotype are associated with antipsychotic-induced weight
Sullivan L, et al. Prevalence of the metabolic syndrome in patients gain in patients with chronic schizophrenia. Neuropsychopharmacology
with schizophrenia: baseline results from the Clinical Antipsychotic 2008;33:2200-5.
Trials of Intervention Effectiveness (CATIE) schizophrenia trial and 44. Dixon L, Weiden P, Delahanty J, Goldberg R, Postrado L, Lucksted A,
comparison with national estimates from NHANES III. Schizophr Res et al. Prevalence and correlates of diabetes in national schizophrenia
2005;80:19-32. samples. Schizophr Bull 2000;26:903-12.
21. Goossens GH. The role of adipose tissue dysfunction in the 45. Perkins DO. Predictors of noncompliance in patients with
pathogenesis of obesity-related insulin resistance. Physiol Behav schizophrenia. J Clin Psychiatry 2002;63:1121-8.
2008;94:206-18. 46. Koro CE, Fedder DO, L’Italien GJ, Weiss SS, Magder LS, Kreyenbuhl
22. Scheen AJ, De Hert MA. Abnormal glucose metabolism in patients J, et al. Assessment of independent effect of olanzapine and risperidone
treated with antipsychotics. Diabetes Metab 2007;33:169-75. on risk of diabetes among patients with schizophrenia: population-
23. Kohen D. Diabetes mellitus and schizophrenia: historical perspective. based nested case-control study. BMJ 2002;325:243-7.
Br J Psychiatry Suppl 2004;47:S64-6. 47. Sernyak MJ, Leslie DL, Alarcon RD, Losonczy MF, Rosenheck R.
24. Grundy SM. Hypertriglyceridemia, insulin resistance, and the Association of diabetes mellitus with use of atypical neuroleptics in
metabolic syndrome. Am J Cardiol 1999;83:25F-29F. the treatment of schizophrenia. Am J Psychiatry 2002;159:561-6.
25. van Winkel R, van Os J, Celic I, Van Eyck D, Wampers M, Scheen A, 48. Reinstein MJ, Sirotovskaya LA, Jones LE, Mohan S, Chasanov
et al. Psychiatric diagnosis as an independent risk factor for metabolic MA. Effect of clozapine-quetiapine combination therapy on weight
disturbances: results from a comprehensive, naturalistic screening and glycaemic control: preliminary findings. Clin Drug Investig
program. J Clin Psychiatry 2008;69:1319-27. 1999;18:99-104.
26. Watanabe H, Tanabe N, Watanabe T, Darbar D, Roden DM, Sasaki S, 49. Campanella LM, Lartey R, Shih R. Severe hyperglycemic hyperosmolar
et al. Metabolic syndrome and risk of development of atrial fibrillation: nonketotic coma in a nondiabetic patient receiving aripiprazole. Am
the Niigata preventive medicine study. Circulation 2008;117:1255-60. Emerg Med 2009;53:264-6.
27. Kotronen A, Yki-Järvinen H. Fatty liver: a novel component of the 50. Baldessarini RJ, Lipinski JF. Toxicity and side-effects of antipsychotic,
metabolic syndrome. Arterioscler Thromb Vasc Biol 2008;28:27-38. antimanic, and antidepressant medications. Psychiatr Ann 1976;6:52-
28. Goldbacher EM, Matthews KA. Are psychological characteristics 68.
related to risk of the metabolic syndrome? A review of the literature. 51. Baptista T, Lacruz A, Angeles F, Silvera R, de Mendoza S, Mendoza
Ann Behav Med 2007;34:240-52. MT, et al. Endocrine and metabolic abnormalities involved in
29. Welzel TM, Graubard BI, Zeuzem S, El-Serag HB, Davila JA, obesity associated with typical antipsychotic drug administration.
McGlynn KA. Metabolic syndrome increases the risk of primary liver Pharmacopsychiatry 2001;34:223-31.
cancer in the United States: a study in the SEER-Medicare database. 52. Smith M, Hopkins D, Peveler RC, Holt RI, Woodward M, Ismail K.
Hepatology 2011;54:463-71. First- v. second-generation antipsychotics and risk for diabetes in
30. Gottlieb AB, Dann F, Menter A. Psoriasis and the metabolic syndrome. schizophrenia: systematic review and meta-analysis. Br J Psychiatry
J Drugs Dermatol 2008;7:563-72. 2008;192:406-11.
31. De Hert M, Dobbelaere M, Sheridan EM, Cohen D, Correll CU. 53. Johnson DE, Yamazaki H, Ward KM, Schmidt AW, Lebel WS,
Metabolic and endocrine adverse effects of second-generation Treadway JL, et al. Inhibitory effects of antipsychotics on carbachol-
antipsychotics in children and adolescents: a systematic review of enhanced insulin secretion from perifused rat islets: role of muscarinic
randomized, placebo controlled trials and guidelines for clinical antagonism in antipsychotic-induced diabetes and hyperglycemia.
practice. Eur Psychiatry 2011;26:144-58. Diabetes 2005;54:1552-8.
32. Yau PL, Castro MG, Tagani A, Tsui WH, Convit A. Obesity and 54. Buchholz S, Morrow AF, Coleman PL. Atypical antipsychotic-
metabolic syndrome and functional and structural brain impairments induced diabetes mellitus: an update on epidemiology and postulated
in adolescence. Pediatrics 2012;130:e856-64. mechanisms. Intern Med J 2008;38:602-6.
33. Simon V, van Winkel R, De Hert M. Are weight gain and metabolic 55. Sasaki J, Funakoshi M, Arakawa K. Lipids and apolipoproteins
side effects of atypical antipsychotics dose dependent? A literature in patients treated with major tranquilizers. Clin Pharmacol Ther
East Asian Arch Psychiatry 2013, Vol 23, No.1 27
J Yogaratnam, N Biswas, R Vadivel, et al
1985;37:684-7. 60. Zipursky RB, Gu H, Green AI, Perkins DO, Tohen MF, McEvoy JP, et
56. Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, al. Course and predictors of weight gain in people with first-episode
Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with psychosis treated with olanzapine or haloperidol. Br J Psychiatry
chronic schizophrenia. N Engl J Med 2005;353:1209-23. 2005;187:537-43.
57. Spivak B, Roitman S, Vered Y, Mester R, Graff E, Talmon Y, et 61. Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F,
al. Diminished suicidal and aggressive behavior, high plasma Lobos CA, et al. Head-to-head comparisons of metabolic side effects
norepinephrine levels, and serum triglyceride levels in chronic of second generation antipsychotics in the treatment of schizophrenia:
neuroleptic-resistant schizophrenic patients maintained on clozapine. a systematic review and meta-analysis. Schizophr Res 2010;123:225-
Clin Neuropharmacol 1998;21:245-50. 33.
58. De Hert M, Hanssens L, van Winkel R, Wampers M, Van Eyck D, 62. Melkersson KI, Dahl ML, Hulting AL. Guidelines for prevention
Scheen A, et al. A case series: evaluation of the metabolic safety of and treatment of adverse effects of antipsychotic drugs on glucose-
aripiprazole. Schizophr Bull 2007;33:823-30. insulin homeostasis and lipid metabolism. Psychopharmacology (Berl)
59. Cohn T, Prud’homme D, Streiner D, Kameh H, Remington G. 2004;175:1-6.
Characterizing coronary heart disease risk in chronic schizophrenia: 63. Li Z, Maglione M, Tu W, Mojica W, Arterburn D, Shugarman LR, et
high prevalence of the metabolic syndrome. Can J Psychiatry al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med
2004;49:753-60. 2005;142:532-46.
28 East Asian Arch Psychiatry 2013, Vol 23, No.1
You might also like
- PREVALENCE OF METABOLIC SYNDROME AMONG PATIENTS WITH SCHIZOPHRENIA FROM LONG CARE UNIT IN FORENSIC PSYCHIATRY PROGRAM: AN OBSERVATIONAL STUDYDocument6 pagesPREVALENCE OF METABOLIC SYNDROME AMONG PATIENTS WITH SCHIZOPHRENIA FROM LONG CARE UNIT IN FORENSIC PSYCHIATRY PROGRAM: AN OBSERVATIONAL STUDYJAVED ATHER SIDDIQUINo ratings yet
- SchizophreniaDocument10 pagesSchizophreniajhuNo ratings yet
- Suicide and Treatm EntDocument8 pagesSuicide and Treatm EntSourav DasNo ratings yet
- Metabolic Syndrome: A Psychiatric OutlookDocument5 pagesMetabolic Syndrome: A Psychiatric OutlookJAVED ATHER SIDDIQUINo ratings yet
- A Longitudinal Follow-Up Study of Anti-Depressant Drugs Causing Hepatotoxicity in Patients With Major Depressive DisordersDocument4 pagesA Longitudinal Follow-Up Study of Anti-Depressant Drugs Causing Hepatotoxicity in Patients With Major Depressive DisordersAbdul SamadNo ratings yet
- Schizophrenia: Medical Illness, Mortality, and Aging : INT'L. J. PSYCHIATRY IN MEDICINE, Vol. 41 (3) 245-251, 2011Document7 pagesSchizophrenia: Medical Illness, Mortality, and Aging : INT'L. J. PSYCHIATRY IN MEDICINE, Vol. 41 (3) 245-251, 2011Arum PratikaNo ratings yet
- Anorexia NervosaDocument9 pagesAnorexia NervosaDouglas SantosNo ratings yet
- Metabolic Syndrome: Learning ObjectivesDocument20 pagesMetabolic Syndrome: Learning Objectivesddeeb420% (1)
- Articulo 2Document16 pagesArticulo 2gregorioNo ratings yet
- Jurnal DR 56Document16 pagesJurnal DR 56taufik090214No ratings yet
- Diabetes and Mental HealthDocument3 pagesDiabetes and Mental HealthVENNA FADILLAHNo ratings yet
- Metabolomics To Study Psychotic Disorders and Their Metabolic ComorbiditiesDocument7 pagesMetabolomics To Study Psychotic Disorders and Their Metabolic Comorbiditiesjoseph psychayterNo ratings yet
- Metabolic Syndrome and StrokeDocument5 pagesMetabolic Syndrome and StrokeEmir SaricNo ratings yet
- Hypoglycemia - 2014 Morales N DoronDocument8 pagesHypoglycemia - 2014 Morales N DoronDian Eka RamadhaniNo ratings yet
- Metabolic Changes Associated With Antipsychotic Use: Joseph A. Lieberman, III, M.D., M.P.HDocument6 pagesMetabolic Changes Associated With Antipsychotic Use: Joseph A. Lieberman, III, M.D., M.P.HMerlintaNo ratings yet
- Geriatria Articulo EspecialDocument15 pagesGeriatria Articulo EspecialBonchita BellaNo ratings yet
- 2018 A Global Overview of Precision Medicine in Type 2 DiabetesDocument12 pages2018 A Global Overview of Precision Medicine in Type 2 Diabetesguanyulin01No ratings yet
- Nejm AnorexiaDocument9 pagesNejm AnorexiaRodrigo EstebanNo ratings yet
- 23 Rajeshkanna EtalDocument8 pages23 Rajeshkanna EtaleditorijmrhsNo ratings yet
- Systematic Review of Metabolic Syndrome Biomarkers: A Panel For Early Detection, Management, and Risk Stratification in The West Virginian PopulationDocument14 pagesSystematic Review of Metabolic Syndrome Biomarkers: A Panel For Early Detection, Management, and Risk Stratification in The West Virginian PopulationDany RamdhaniNo ratings yet
- Appi Ajp 2017 17040409Document2 pagesAppi Ajp 2017 17040409jhuNo ratings yet
- Metabolic Syndrome 2017 Diabetes Reversal by Plantbased Diet A Review Article Biswaroop Roy Chowdhury Indo Vietnam Medical BoardDocument2 pagesMetabolic Syndrome 2017 Diabetes Reversal by Plantbased Diet A Review Article Biswaroop Roy Chowdhury Indo Vietnam Medical Boardali shahidNo ratings yet
- Neuropatia DiabéticaDocument18 pagesNeuropatia DiabéticaGustavo PestanaNo ratings yet
- ADA Consenssus DM Eldery 2012Document15 pagesADA Consenssus DM Eldery 2012Jason CarterNo ratings yet
- Recent Research AnDocument9 pagesRecent Research AnloloasbNo ratings yet
- Emerging Therapeutic Options in The Management of Diabetes Recent Trends, Challenges and Future DirectionsDocument21 pagesEmerging Therapeutic Options in The Management of Diabetes Recent Trends, Challenges and Future DirectionsGabriela PachecoNo ratings yet
- HypoglicemiaDocument4 pagesHypoglicemiayeniNo ratings yet
- Reversibledementias: Milta O. LittleDocument26 pagesReversibledementias: Milta O. LittleLUCAS IGNACIO SANCHEZNo ratings yet
- Novel Di SeasDocument36 pagesNovel Di Seasfarishussein2023No ratings yet
- Pengaruh Hipoglikemia Pada Pasien Diabetes Melitus Tipe 2 Terhadap Kepatuhan Terapi Dan Kualitas HidupDocument8 pagesPengaruh Hipoglikemia Pada Pasien Diabetes Melitus Tipe 2 Terhadap Kepatuhan Terapi Dan Kualitas Hidupilma adilla syahidaNo ratings yet
- Effects of Hypoglycemia on Patients with Type 2 Diabetes Mellitus on Therapy Adherence and Quality of LifeDocument8 pagesEffects of Hypoglycemia on Patients with Type 2 Diabetes Mellitus on Therapy Adherence and Quality of Lifemail junkNo ratings yet
- Prediabetes: A Fundamental Text: Pathophysiology, Complications, Management & ReversalFrom EverandPrediabetes: A Fundamental Text: Pathophysiology, Complications, Management & ReversalNo ratings yet
- Advances in Lifestyle and Physical Health in SchizophreniaDocument8 pagesAdvances in Lifestyle and Physical Health in SchizophreniaKelvin TungNo ratings yet
- Metabolic Syndrome and Psychiatric Illness: Interactions, Pathophysiology, Assessment and TreatmentFrom EverandMetabolic Syndrome and Psychiatric Illness: Interactions, Pathophysiology, Assessment and TreatmentNo ratings yet
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionFrom EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNo ratings yet
- Prevalence and Major Risk Factors of Diabetic Retinopathy: A Cross-Sectional Study in EcuadorDocument5 pagesPrevalence and Major Risk Factors of Diabetic Retinopathy: A Cross-Sectional Study in EcuadorJorge Andres Talledo DelgadoNo ratings yet
- Diabetic Distress in Egyptian Elderly PatientsDocument11 pagesDiabetic Distress in Egyptian Elderly Patientsرقية ياسينNo ratings yet
- 10 1210@jc 2019-00198Document55 pages10 1210@jc 2019-00198Mădălina MitroiuNo ratings yet
- 2017 Antipsychotic-Associated Weight Gain Management Strategies and Impact On Treatment AdherenceDocument11 pages2017 Antipsychotic-Associated Weight Gain Management Strategies and Impact On Treatment AdherenceanonNo ratings yet
- nr4 004Document6 pagesnr4 004Loreta EpureNo ratings yet
- Casestudy JDDTDocument3 pagesCasestudy JDDTJulaiha QosimNo ratings yet
- McIntyre, CANMAT Comorbidity - Metabolic, Ann Clin Psyt 2012Document13 pagesMcIntyre, CANMAT Comorbidity - Metabolic, Ann Clin Psyt 2012JESUS FRANCISCO SANCHEZ PATRICIONo ratings yet
- Literature Review DiabetesDocument5 pagesLiterature Review Diabetesukefbfvkg100% (1)
- Deleterious Dozen DMT2Document18 pagesDeleterious Dozen DMT2cecilia zavala100% (1)
- DiabetesDocument352 pagesDiabetesbeltonNo ratings yet
- Neurobiology of Disease: ReviewDocument10 pagesNeurobiology of Disease: ReviewmarselyagNo ratings yet
- Influence of Psychopathology and Metabolic Parameters en Primeros Episodios PsicoticosDocument7 pagesInfluence of Psychopathology and Metabolic Parameters en Primeros Episodios PsicoticossiralkNo ratings yet
- Schizophrenia etiology, symptoms, treatmentDocument12 pagesSchizophrenia etiology, symptoms, treatmentmustafa566512345No ratings yet
- Differentiation of Diabetes by Pathophysiology, Natural History, and Prognosis PDFDocument15 pagesDifferentiation of Diabetes by Pathophysiology, Natural History, and Prognosis PDFHadi PrasetyoNo ratings yet
- Archgenpsychiatry 2011 2Document8 pagesArchgenpsychiatry 2011 2ruba azfr-aliNo ratings yet
- Diabetes AnnotatedDocument5 pagesDiabetes AnnotatedDavon Richard Walter Van-VeenNo ratings yet
- Metabolic Syndrome Program: How to Lose Weight, Beat Heart Disease, Stop Insulin Resistance and MoreFrom EverandMetabolic Syndrome Program: How to Lose Weight, Beat Heart Disease, Stop Insulin Resistance and MoreRating: 4.5 out of 5 stars4.5/5 (2)
- Best Practice & Research Clinical Endocrinology & MetabolismDocument11 pagesBest Practice & Research Clinical Endocrinology & MetabolismM Slamet RiyantoNo ratings yet
- Manu Et Al-2015-Acta Psychiatrica ScandinavicaDocument12 pagesManu Et Al-2015-Acta Psychiatrica ScandinavicamerianaNo ratings yet
- JAMA Intern Med 2021 Apr 1 181 (4) 520-521Document2 pagesJAMA Intern Med 2021 Apr 1 181 (4) 520-521Samuel SalazarNo ratings yet
- Heart Failure in Patients With Metabolic Syndrome XDocument12 pagesHeart Failure in Patients With Metabolic Syndrome XErwin SiahaanNo ratings yet
- Diabetes MellitusDocument43 pagesDiabetes MellitusRobi HSNo ratings yet
- Format PengkajianDocument8 pagesFormat PengkajianHandiniNo ratings yet
- Integrative Neuromuscular Medicine: Neuropathy and Neuropathic Pain: Consider The AlternativesDocument13 pagesIntegrative Neuromuscular Medicine: Neuropathy and Neuropathic Pain: Consider The AlternativesNawish SohailNo ratings yet
- Diabetes Treatment Literature ReviewDocument7 pagesDiabetes Treatment Literature Reviewafmzatvuipwdal100% (1)
- Orthodontic Treatment: Patient Information LeafletDocument2 pagesOrthodontic Treatment: Patient Information LeafletRakan KhtoomNo ratings yet
- CV DR Ari Sami Hussain NadhimDocument5 pagesCV DR Ari Sami Hussain NadhimAri SamiNo ratings yet
- Minimally Invasive Face-Lifting: S-Lift and S-Plus Lift RhytidectomiesDocument11 pagesMinimally Invasive Face-Lifting: S-Lift and S-Plus Lift RhytidectomiesAditi SharmaNo ratings yet
- Case Study: MargaretDocument2 pagesCase Study: MargaretmarielNo ratings yet
- OPERATING ROOM TEACHING PLANDocument7 pagesOPERATING ROOM TEACHING PLANjohnhenryv100% (2)
- DX Imaging 1 MT and FinalDocument24 pagesDX Imaging 1 MT and FinalRaymondNo ratings yet
- Rapid HIV Test Detects Antibodies in BloodDocument4 pagesRapid HIV Test Detects Antibodies in Bloodkbl27No ratings yet
- Nursing Care Plan Urinary Tract Infection (UTI)Document2 pagesNursing Care Plan Urinary Tract Infection (UTI)deric95% (97)
- U.S. Food & Drug: Administration 10903 New Hampshire Avenue Silver Spring, MD 20993Document14 pagesU.S. Food & Drug: Administration 10903 New Hampshire Avenue Silver Spring, MD 20993jonathan panganibanNo ratings yet
- Quality Assurance GuidelinesDocument28 pagesQuality Assurance Guidelinesmonir61No ratings yet
- Western Mindanao State University College of NursingDocument3 pagesWestern Mindanao State University College of NursingDarina Shumei MustaphaNo ratings yet
- Part-4 Pharmacological and Toxicological DataDocument10 pagesPart-4 Pharmacological and Toxicological DataShagorShagorNo ratings yet
- India's National Diabetes ProgrammeDocument9 pagesIndia's National Diabetes ProgrammeNaveenNo ratings yet
- Neonatal Hypoglycemia 2Document6 pagesNeonatal Hypoglycemia 2Lalo LanNo ratings yet
- Anti-Obesity MedicationsDocument33 pagesAnti-Obesity MedicationsJorge Luis Alva AlonsoNo ratings yet
- Werner & Ingbar’s The Thyroid 8th EditionDocument10 pagesWerner & Ingbar’s The Thyroid 8th Editionbyrock66No ratings yet
- Forensic PsychiatryDocument5 pagesForensic PsychiatrySheba Dan de WiseNo ratings yet
- 10 - Growth & Reproduction Exercise 4-1Document2 pages10 - Growth & Reproduction Exercise 4-1rhdoiuaNo ratings yet
- Sindrom AlagileDocument8 pagesSindrom AlagilewenyinriantoNo ratings yet
- Big Pharma's Worst NightmareDocument51 pagesBig Pharma's Worst NightmaredjoleNo ratings yet
- Care of The Older Adult Handouts PrelimsDocument7 pagesCare of The Older Adult Handouts PrelimsAmanda Joy TuizaNo ratings yet
- National Dengue Prevention Program OverviewDocument39 pagesNational Dengue Prevention Program OverviewkentNo ratings yet
- Simulation in Health Care Education: Perspectives in Biology and Medicine February 2008Document6 pagesSimulation in Health Care Education: Perspectives in Biology and Medicine February 2008Birendra MahatNo ratings yet
- Saran prasarana kepatuhan pada anemia aplastikDocument1 pageSaran prasarana kepatuhan pada anemia aplastikAlika Nigandiva41No ratings yet
- 2020 Vision Without Glasses PDFDocument340 pages2020 Vision Without Glasses PDFJacklynlim Lkc100% (3)
- 305.076.000 01 EN Bellavista Manual G6 PDFDocument162 pages305.076.000 01 EN Bellavista Manual G6 PDFanh khoa duongNo ratings yet
- Local AnestheticsDocument93 pagesLocal Anestheticsgeetika100% (1)
- Concise Review: Importance of Probiotics Yogurt For Human Health ImprovementDocument6 pagesConcise Review: Importance of Probiotics Yogurt For Human Health ImprovementIOSRjournalNo ratings yet
- Government College of Nursing:, Jodhpur (Raj.)Document43 pagesGovernment College of Nursing:, Jodhpur (Raj.)priyankaNo ratings yet
- Viruses: Serge Stroobandt and Roland StroobandtDocument3 pagesViruses: Serge Stroobandt and Roland StroobandtPuskesmas selongNo ratings yet