Professional Documents
Culture Documents
Bacteriology Reviewer: Bacteria Important Notes Tests Aerobic Gram-Positive (+) Cocci
Uploaded by
AJOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bacteriology Reviewer: Bacteria Important Notes Tests Aerobic Gram-Positive (+) Cocci
Uploaded by
AJCopyright:
Available Formats
1|Page
BACTERIOLOGY REVIEWER
Bacteria Important Notes Tests
Aerobic Gram-Positive(+) Cocci
• Catalase(+), In Clusters,
A. Staphylococcus • Cream/off-white colonies on
BA
• Normal Flora of anterior nares
• Coagulase(+), DNase (+)
• Skin and wound infection
• β- hemolytic on SBA
(folliculitis boils/Furuncles,
• Ferments Mannitol (+)
Carbuncles, impetigo)
(Yellow colonies on MSA)
• Food poisoning/Enterocolitis
• PYR and ornithine (-)
(caused by enterotoxin A-J, except
F) and Adult Joint Infections • Columbia Colistin-Nalidixic
Acid Agar (CNA)
• Toxic Shock Syndrome (caused by
1. S. aureus TSSToxin-1/enterotoxin F= phage • Phenylethyl Alcohol Agar
group I) (PEA)
• Scalded Skin Syndrome/Ritter’s • Vancomycin- antimicrobial
disease/Lyell’s syndrome (caused choice for MRSA (methicillin
by epidermolytic/Exfoliatin toxin= resistant S. aureus)
phage group II)
Note: (No Endotoxin- can only be
• Has Protein A on its cell wall
found on cell wall of gram
• Production of clumping factor,
Negative Bacteria)
hemolysin, and DNAse
• Most common CoNS
• Coagulase(-)
• Hospital-acquired UTI
2. S. epidermidis • Novobiocin (S)
• Surgical insertion of prosthetic
• Red colonies on MSA
devices (heart valves & CSF shunt)
• Coagulase(-)
• UTI among young sexually active
3. S. saprophyticus • Novobiocin (R)
females
• Red colonies on MSA
• Coagulase(-)
4. S. lugdunensis • Frequent cause of endocarditis • PYR (+)
• Ferments Mannitol (yellow)
• Coagulase(-), Tetrads
• Yellow and non hemolytic on
• NF of the skin and mucous
5. Micrococcus SBA
membranes
• Microdase/Modified Oxidase
(+)
• Obtain energy through fermentation
B. Streptococcus • Catalase(-), In Chains and Pairs
of sugars to Lactic acid
• Always considered pathogenic
• Strep throat (pharyngitis and
tonsillitis)
• β- hemolytic (due to
• Pyodermal infection (Impetigo, Streptolysin S)
1. S. pyogenes (Group A) Erysipelas, cellulitis)
• PYR/Taxo A(+)
• Streptococcal Toxic Shock
• Bacitracin(S)
Syndrome/STTS (caused by
erythrogenic toxin= rash seen in
Scarlet Fever)
Prepared by Jethro Rada Jr., RMT… puhon
2|Page
• Necrotizing Fasciitis (flesh-eating
disease)
• Otitis media, pneumonia
• Sequelae: Rheumatic Fever and
Post Streptococcal Acute
Glomerulonephritis (AGN)
• Early onset infection/Newborn • β- hemolytic
(pneumonia, meningitis, • CAMP(+) *B-Lysin from S.
sepsis/bacteremia) aureus (arrowhead hemolysis)
2. S. agalactiae (Group B)
• Immunocompromised (Endometritis • Hippurate Hydrolysis(+)
w/ wound infection, post-partum • PYR(-)
fever, endocarditis, pyelonephritis) • Bacitracin(R)
3. S. dysgalactiae subsp. equisimilis • Lancefield group C or G antigens
(Group C) • Resembles S. pyogenes diseases
• Isolation in blood cultures
indicates colon cancer
4. S. bovis/S. equines (Group D non- • a-hemolytic, nonhemolytic,
enterococcus) rarely β- hemolytic
• Endocarditis, UTIs, abscesses, • Bile Esculin(+)
wound infection, bacteremia • PYR/6.5% NaCl (-)
• a-hemolytic, nonhemolytic
5. Enterococcus (Group D) (most common), β- hemolytic
E. faecalis/E. faecium • Bile Esculin(+)
• PYR/6.5% NaCl (+)
• NF of URT (Upper Respiratory
• a-hemolytic Diplococci
Infection)
(Lancet or pullet shape)
• Lobar pneumonia (rusty brown
• Grows on SBA at 5-10% CO2 ,
6. S. pneumoniae sputum)- alcoholics and elderly
48 hrs (Mucoid, Umbilicated)
• Otitis media
• Optochin/Taxo P (S)
• Meningitis
• Bile Solubility (+)
• Important cause of CAP
• NF of the oral cavity, GI tract, URT
(common member) • a-hemolytic, nonhemolytic
• Major cause of subacute Bacterial • Optochin/Taxo P (R)
Endocarditis (SBE) in damaged • Bile Solubility (-)
7. Viridans streptococcus heart valves • Bile Esculin (-)
• Enter the blood through Dental • 6.5% NaCl/PYR (-)
procedures • Strep. anginosus/milleri-
• Abscesses, meningitis, empyema, Butterscotch/Caramel smell
wound infection
• Formerly known as Nutrionally
Variant Streptocci
• Vitamin B6 • PYR (+)
8. Abiotrophia and Granulicatella (Pyridoxal/Pyridoxamine) • 6.5% Nacl (-)
Dependent • Bile Esculin (-)
• CNS and opthalmic infections,
endocarditis
• PYR (+)
• Endocarditis, Lung and Brain
9. Gemella • Leucine Aminopeptidase/LAP
abscesses, meningitis, osteomyelitis
(+)
• PYR (-)
• Ventriculitis, osteomyelitis,
10. Leuconostoc • LAP (-)
postsurgical endophthalmitis
• Vancomycin resistant
Prepared by Jethro Rada Jr., RMT… puhon
3|Page
Aerobic Gram-Positive(+) Bacilli
Non Spore-Forming
A. Corynebacterium
• Picket fence/“Chinese
• Diphtheria (pseudomembrane at Letters”/Palisades/V and L
the back of the throat)
• Pleomorphic, nonmotile
• Found only in humans
• Elek Test/In vitro-
immunodiffusion (KL agar)
1. C. diphtheriae • Culture Media:
Tinsdale (Black colonies w/
Notes: Rhodococcus equi- former
brown halo), Cystine-
species of Corynebacterium and
Tellurite, Leoffler, Pai
Nocardia. Produce Pink colonies,
• Shick’s test
asaccharolytic
• Urease (-)
• Cause of nosocomial infection
2. C. jeikeium • Infection in Immunocompromised • Pyrazidamise (+)
Patients
3. C. urealyticum • UTIs • Rapid Urease (+)
• Causative agent of Erythrasma • Coral Red fluorescence under
4. C. minutissimum
(macular infection in DM) Wood’s lamp
• Urease (+), pleomorphic
5. C. ulcerans/pseudotuberculosis • Produce phospholipase D
• Brown halo on Tinsdale
• CAMP (+) /Arrowhead
• Spontaneous abortion • Tests mostly resembles S.
• Granulomatosis infantisepticum pyogenes but catalase (+)
• Meningitis • “Umbrella” Motility = @RT
B. Listeria monocytogenes
• Animal products (Deli meats, • Tumbling/“End-over, end”,
dairy products) motility = wet mount, Rocket
• Listeriosis • Cold enrichment
• Catalase (+), Neomycin (S)
• Occupational exposure
• Pleomorphic, nonmotile
• Domestic swine/slaughter houses
• H2S (+)
C. Erysipelothrix rhusiopathiae • Resistant to salting, pickling, and
• Catalase (-)
smoking
• Neomycin (R)
• Erysipeloid (cellulitis/skin lesions)
D. Arcanobacterium • Wound and tissue infections • Catalase (-), nonmotile
Spore-Forming
• Square ends
• Boxcar morphology
A. Bacillus • Frequent laboratory contaminant
• Lecithinase (+)
• Catalase (+)
• Anthrax (livestocks)
Forms:
a. Cutaneous- “Black • Medusa Head colonies
Eschar”/“Malignant pustule” • “Inverted Pine Tree” growth
1. B. anthracis b. Pulmonary- “Woolsorter’s • Bamboo rods
Disease”/Ragpickers Disease” • Nonhemolytic, nonmotile
c. Gastrointestinal- spore • String of Pearl test
ingestion
• Potential Bioterrorism Agent ∆
Prepared by Jethro Rada Jr., RMT… puhon
4|Page
• Food poisoning (Rice Products)
2. B. cereus • Oppostunistic wound, brain, bone, • β- hemolytic, motile
and eye infections
3. B. subtilis • Hay’s bacillus
Filamentous (Actinomycetes) • Petrichor (Post-Rain smell) • Morphology similar to fungi
A. Nocardia • Partially Acid-Fast
• Often form branched hyphae
1. N. asteroides • “Farmer’s Lung” (Pulmonary) • Sulfur granules, Catalase (+)
• Chalky/Velvety appearance
2. N. brasieliensis/N. caviae • Mycetomas (cutaneous) • Bread Crumbs
• “Paraffin Bait Technique”
• Similar to Nocardia
B. Actinomadura madurae/pelletieri • Mycetoma
• Cellubiose/Xylose (+)
• 3rd most common aerobic
C. Streptomyces griseus • ID done by reference lab
actinomycetes
Aerobic Gram-Negative(-) Diplococci
A. Neisseria • “Kidney Bean” morphology
• Gonorrhea (the clap) • Sensitive to Fatty Acids/Temp
• Males- Acute urethritis (prostatis • Culture:
& epididymitis) a. Required Enriched (CA)
• Females- Asymptomatic and Selective (TM, MTM,
(common), PID, ectopic pregnancy, ML,NYC, GC Lect) Media
1. N. gonorrhoeae
perihepatitis (Fitz-Hugh-Curtis) b. DO NOT GROW on BA
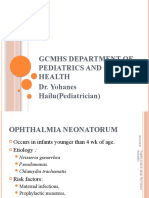
• Neonates- Opthalmia c. Capnophilic (grow on BA)
Neonatorum/conjunctivitis- • MALTOSE (-)
requires Erythromycin to treat Oxidase and Glucose (+)
• Contains Cytochrome Oxidase • DNase and Nitrate (-)
• Meningococcal meningitis/ • Culture: same with N.
meningococcemia (sepsis/blood) gonorrhoea but GROWS on
leading to DIC and “Waterhouse- both BA and CA
2. N. meningitidis Friderichsen syndrome” • Maltose (+), LACTOSE (-)
• Epidemic meningitis (CSF) and • Oxidase and Glucose (+)
meningococcal pneumonia • DNase and Nitrate (-)
(sputum)/Nasopharyngeal swab • N.lactimica – Lactose (+)
• Joints and bones infections
3. Kingella (coccobacilli) • Grow on BA, CA, and MTM
• Endocarditis
K. kingae • Can’t grow on MAC
• Member of HACEK (fastidious)
K. denitrificans/oralis • Reduce NITRATE (+)
• Isolated from throat and mouth
• NF of URT • DNase, Nitrate, Oxidase (+)
B. Moraxella cattarhalis
• Otits media, sinusitis, RT infection • Dark Purple (TMpPD)
Aerobic Gram-Negative(-) Bacilli • Asaccharolytic/ all carb test (-)
• Antigens (serogrouping) • Grows on MAC:
O (somatic)- cell wall; heat stable LF-pink, NLF- colorless
Enterobacteriaceae/Fermenting
K (envelope)- capsular; heat labile • “All Ferment Glucose,
H (flagellar)- flagellar; heat labile OXIDASE (-), Nitrite (+)”
Opportunistic Pathogen • Normal Flora of the GI tract • Most are Motile
A. Escherichia
• UTI, appendicitis, peritonitis, • Green Metallic Sheen on
1. E. coli
gallbladder infections, endocarditis, “EMB”, ß-hemolytic: SBA
Prepared by Jethro Rada Jr., RMT… puhon
5|Page
meningitis in newborn, • LF, TSI: A/AG, IMVC: + + - -
gastroenteritis, food poisoning • Pink/red colonies on MAC
• Stimulation of adenylate cyclase
• Community-acquired Cystitis 3. Enterotoxigenic (ETEC)-
Strains: “Traveler’s Diarrhea”/tropical
1. Enterohemorrhagic (EHEC)- climate/severe epidemic diarrhea
causes Hemorrhagic Colitis & 4. Enteroinvasive (EIEC)-
Hemolytic Uremic Syndrome bloody diarrhea with pus/
(HUS), bloody diarrhea with no dysentery, sereny test
pus, Shiga Toxin- serogroup (NONMOTILE)
O157:H7, does not grow on SMAC 5. Uropathogenic (UPEC)-
2. Enteropathogenic (EPEC)- most common cause of UTI
infantile/watery diarrhea and kidney infection
• Raw meat and milk
6. E. hermanii
• Wounds, spinal fluid • Yellow pigmented colonies
7. E. vulneris • Wounds
B. Klebsiella • K antigen- serogroup • NONMOTILE
• Lower respiratory tract infection • LF
• Wound infections, UTI, bacteremia • TSI= A/AG
1. K. pneumoniae
• Nosocomial outbreak • IMVC= - - + +
• K. pneumoniae – most commonly • Ornithine(-)
isolated
2. K. oxytoca • K. rhinoscleromatis/ozanae- • Indole (+)
rhinoscleroma/nasal infection
• Group 47 • Indole (+)
3. K. ornithinolytica/planticola
• Urine, RT, blood • Ornithine(+)
• Granuloma • Donovan bodies
4. K. (Calymmatobacterium)
Inguinale/Donovanosis- sexually • Does not gram stain and grow
granulomatis
transmitted on lab media (CA, others)
C. Enterobacter/Pantoea/Cronobacter • Occasional clinical isolates
• LF, TSI= A/A
• IMVC= - - + +
1. E. cloacae • Most common
• Arginine (+)
• Lysine (-)
• Arginine (-)
2. E. aerogenes • 2nd most common
• Lysine (+)
3. E. agglomerans • Septicemia, contaminated IV fluids
• Pathogen in neonates • Yellow-pigmented colonies
4. E. sakazakki/E. cowanii • Brain abscesses, respiratory and
wound infections
5. E. gergoviae/E. hormaechei • Blood, wounds, sputum • Rarely blood cultures (E. ger)
D. Citrobacter
• Late LF, TSI: K/AG, “H2S(+)”
• IMVC= - + - +
• Most common
1. C. freundii • Colonial morphology mistaken
• UTI, pneumonia
as Salmonella
• Lysine, Urease (-)
2. C. diversus • Nursery outbreaks • H2S (-)
3. C. amalonaticus • Found in feces
Prepared by Jethro Rada Jr., RMT… puhon
6|Page
• Produce pink to red pigment called • DNase, Lipase, Gelatinase (+)
E. Serratia
Prodigiosin at RT (22˚C) -unique
• Nosocomial outbreaks: burn units,
• LLF, TSI= K/AG or K/A
1. S. marcescens chemotherapy, nurseries
• IMVC: - - + +
• Most common clinical isolate
2. S. rubidaea/ liquefaciens • From human sources
• Isolated from respiratory tract (1) • Dirty, musty odor
3. S. odorifera
and blood and CSF (2) • Potato Odor
• Anatomical sites • LLF, Lysine, ONPG, KCN (+)
F. Hafnia alvei
• Originally from stool cultures • Delayed Citrate (+) reaction
• Non-Lactose Fermentor
• TSI= K/AG, “H2S (+)”
G. Proteus • Tribe Proteeae* • Phenylalanine/PDA, Lysine,
• “Burned Chocolate” odor/dried Tryptophan Deaminase (+)*
fish • “Swarming Colonies” on BA
• Urine, wound, ear infection • IMVC: (-) + v v
1. P. mirabilis
• Associated with Kidney Stones • Ornithine (+)
• Produce biofilms associated with • IMVC: (+) + - -
2. P. vulgaris catheters • Ornithine (-)
• Sucrose (+)
3. P. penneri • Newly recognized species
• NLF, TSI= K/AG
• Tribe Proteeae*
• Phenylalanine/PDA, Lysine,
H. Morganella morganii • UTI
Tryptophan Deaminase (+)*
• Nosocomial,post operative infection
• IMVC: + + - -
I. Providencia
• Tribe Proteeae* • NLF, TSI= K/A
1. P. rettgeri • Nosocomial outbreaks • Phenylalanine/PDA, Lysine,
2. P. stuartii • Urine Tryptophan Deaminase (+)*
• IMVC: + + - +
3. P. alcalifaciens
• Pathogen of fish and animals • NLF, TSI= K/AG, “H2S (+)”
J. Edwardsiella tarda
• Resembles Salmonella • IMVC: + + - -
Overt Pathogen
• Gastroenteritis • NLF, TSI= K/A, “H2S (+)”
• Many animal reservoir (Pet reptiles) • IMVC: - + - +
A. Salmonella (S. enterica/S. bongori)
• Undercooked poultry, eggs, dairy • Urease, PDA (-)
products, and contaminated water • Green with black center
• Typhoid fever (severe colonies on HE
salmonellosis/ “High Grave • For S. Thypi:
Serotypes: Fever”)- spread by Chronic carriers 1. Vi antigen– capsular; heat
• Rose Spots- 2nd week of fever labile. After heating- (+)
1. S. Typhi • Only human reservoir agglutination to D-grouping
• Cholecystectomy- removal of sera
gallbladder 2. Citrate (-)
• Paratyphoid fever 3. Only small amount of H2S
2. S. Paratyphi A, B, C unlike others
• Only human reservoir
• Most human infections in the U.S.
3. S. Thypimurium/Enteretidis
• Salmonella Bacteremia • Notes: O and H antigens-
serogrouping
4. S. Cholerasuis • Salmonella Bacteremia
Prepared by Jethro Rada Jr., RMT… puhon
7|Page
• Shigellosis • NLF/LLF, TSI= K/A
-Bacterial Dysentery • IMVC: - (+) - -
• Only human reservoir • Lysine decarb, Urease (-)
• Fecal-oral, food poisoning • NONMOTILE
B. Shigella
• Daycare centers/nursing home
outbreaks • Notes: O antigen-
• <50 bacteria= highly pathogenic serogrouping (No H because-
• Lost of Anal Wink Reflex in infant flagellar)
• Most virulent species • Mannitol (-)
• Enterotoxin- affects large intestine • ONPG (-)
1. S. dysenteriae (Serogroup A) • Neurotoxin- paralysis
• Complication: ileus, HUS, seizures • Notes: Produce Shiga Toxin-
• Mosts common in the Philippines HUS
• “Gay Bowel Syndrome” • Mannitol (+)
2. S. flexneri (Serogroup B)
• Mild diarrhea • ONPG (-)
• Mannitol (+)
3. S. boydii (Serogroup C) • Mild diarrhea
• ONPG (-)
• Late Lactose Fermentor *
• Mild diarrhea
4. S. sonnei (Serogroup D) • Mannitol (+)
• Most common in the U.S
• ONPG (+)
• Coccobacilli
C. Yersinia • Zoonotic
• Bipolar staining, “Safety pin”
• Plague
A. Forms: Bubonic/glandular (High
fever with painful lymph nodes-
buboes) and Pneumonic (blood stream • NONMOTILE at both 37˚C
and respiratory tract) and 25˚C
B. Three Pandemics:
• IMVC: - + - -
1. Y. pestis 1. Egypt => Europe
• Ornithine (-)
2. “Black Death”
3. Burma => world • TSI= K/A
Rats- hosts, natural reservoir • Urease (-)
Fleas (Xenopsylla cheopsis)-
vectors
• Potential Bioterrorism agent ∆
• CIN (cefsulodin-irgasan-
• Most commonly isolated novobiocin) medium
• Acute enteritis • YSA- CIN + Mannitol
• Mesenteric lymphadenitis/ • Cold enrichment
Enterocolitis (Appendicitis-like) • NONMOTILE at 37˚C
2. Y. enterocolitica • Arthritis, erthema nodosum • Motile at 25˚C*
• Pigs- natural reservoir • Late Lactose Fermentor but
• Household Pets TSI= A/A
• Contaminated water and meat • Sucrose (+)
• Can survive cold temperature • IMVC: v + - -
• Ornithine/ONPG (+)
• Rare cause of Mesenteric • NONMOTILE at 37˚C
lymphadenitis in children • Motile at 25˚C*
• Birds (turkey, geese, pegions) and • IMVC: - + - -
3. Y. pseudotuberculosis Rodents (guinea pigs)- natural • Urease (+)
reservoir • Other Enterobacteriaciae
• Pseudotubercles (caseous • Tatumella ptyseos-
swelling) NONMOTILE, PDA (+)
Prepared by Jethro Rada Jr., RMT… puhon
8|Page
Other Fermenting Bacteria • Indole and Oxidase (+)
• Curved g-rods/Comma-shaped
• Facultative anaerobe
• “Darting Motility” in Hanging
• Inhabitants of Aquatic Drop slide
Environment • String Test (+)
• 12 species (clinically significant) • Transport media: Cary-Blair
A. Vibrio
• HALOPHILIC- salt loving • Selective and differential
(Except V. cholerae and V. media: TCBS agar (thiosulfate
mimicus) citrate bile salt sucrose)
• Enrichment: Alkaline Peptone
Water (APW) w/ 1%NaCl
• Grows on 6% NaCl
• Cholera/Asiatic/Epidemic cholera
• Sucrose Fermenting
• Cholera toxin/choleragen-
enterotoxin • TCBS (Yellow)
• Ingestion of undercooked seafood,
contamindated water, ice cream
1. V. cholerae O1 Notes
• “Rice Water” Stools
• V.cholerae O139- new
• 3 Serotypes: Ogawa, Inaba,
serogroup from India (8th
Hikojima
cholera epidemic), cause severe
• 2 Biotypes: Classical (Bangladesh), diseases same with O1
El Tor (worldwide)
• Mild cholera-like illness
• Sucrose Fermenting
2. V. cholerae non-O1 • Lack the cholera toxin gene
• TCBS (Yellow)
• Cholecytitis, ear infection, cellulitis
• 2nd most common
• Non-Sucrose Fermenting
• Gastroenteritis/mild to moderate
• TCBS (Green)
cholera-like disease
3. V. parahaemolyticus • Kanagawa (+) in Wagatsuma
• Limited coastal/estuarine areas
agar (High-salt mannitol
• “Summer’s Diarrhea” in Japan
medium)
• Produce heat stable hemolysin
• 2nd most serious after cholera
• Cause Highly virulent Septicemia • “Lactose (+) vibrio”
4. V. vulnificus from ingestion of raw oysters • Non-Sucrose Fermenting
• Progressive Wound Infection- • TCBS (Green)
marine water exposure
• Least pathogenic (otitis media,
• Sucrose Fermenting
5. V. alginolyticus wound infecions)
• TCBS (Yellow)
• Strict halophile
• Non-Sucrose Fermenting
6. V. mimicus • Non-halophile
• TCBS (Green)
• Fresh and salt water (reptile, fish) • Identified after Vibrio has been
• “Red Leg Disease” in frogs ruled out (same disease)
B. Aeromonas • Easily survive Freezing (Ice) • Grows on CIN (cefsulodin-
• Cellulitis and diarrhea irgasan-novobiocin) medium
• Self limiting infections • Does not grow on 6% NaCl
1. A. hydrophila —Gastroenteritis, wound infection • Oxidase, Catase, ONPG (+)
2. A. veronii veronii/shubertii —Wound infection • A. hydrophila: ß-hemolytic,
3. A. veronii biovar sobria —Septicemia IMVC: + - + +, Oxidase and
4. A. trota —Gastroenteritis ONPG (+)
Prepared by Jethro Rada Jr., RMT… puhon
9|Page
• Self-limiting Gastroenteritis
(Undercooked seafood) • Grows on CIN
• Bacteremmia, meningitis • Recently moved to
C. Plesiomonas shigelloides
• Cross-agglutinate with Shigella Enterobacteriaciae (except
(share antigenic and biochemical Oxidase +)
profiles)
• Broken Skin (water and soil) • Purple/violet on NA
D. Chromobacterium violaceum
• Cellulitis, abscess, septic shock • Glusose fermetor, oxidase (+)
• Indole and Oxidase (+)
• Microaerophilic,
• Capnophilic
Peptone Fermentors
• Assacharolytic
• Hippurate hydrolysis, oxidase
and catalase (+)
• UREASE (-)
• Abortion in Domestic animals • S-shaped, spiral, curved bacilli,
• Major cause of food poisoning, “Seagull-Wing” appearanc
Gastroenteritis, diarrhea, and • “Darting motility” on wet
septic arthritis mount
• GI and reproductive organs of • Single flagellum at one pole
A. Campylobacter animals • Transport media: Cary-Blaire
• Direct contact- handling of infected • Selective media: Campy BAP,
pets, exposure to animals Butzler, Modified Skirrow,
• Indirect-undercooked poultry and Medium V, Campy Thio,
meat, contaminated water Campy-colistin vancomycin
• Sexually transmitted amphotericin B, Charcoal
cefoperzone deoxycholate agar
• Most infections (Guillan-Barre) • Grows at 42˚C
• Most common cause of Bacterial • Cephalothin (R)
1. C. jejuni
Gastroenteritis worldwide • Nalidixic acid (S)
• Warm-blooded animals (birds) • Complement Lysis (+)
• Cattle and sheep • Does not grow at 42˚C
• Blood- specimen of choice • Incubated at 37˚C
2. C. fetus
• Rare cause of extraintestinal • Cephalothin (S)
infections- Septicemia, jaundice • Nalidixic acid (R)
3. C. coli • Pigs
• UREASE (+)
• Microscopic similar to
• Peptic and Duodenal Ulcers Campylobacter except
• Linked to Stomach Cancer Mulitiple flagella at one pole
• Chronic superficial gastritis/type • Urea Breath Test- labeled
B. Helicobacter pylori B gastritis CO2 is measure by scintillation
• Specimen: Gastric Biopsy materials counter (rapid urease rxn)
• No human reservoir • Media: Stuart medium, Choc,
• No exact means of transmission Skirrow, Brucella agar
• Christensen’s Urea medium,
fecal antigen detection
Fastidious • Oxidase, Catalase, Nitrite (+)
• Oxidase, Catalase (+)
• Member of HACEK (fastidious)
• Carbohydrate fermentor, nitrite
A. Haemophilus -important cause of endocarditis
(+)
• Normal flora of URT
• Nonmotile
Prepared by Jethro Rada Jr., RMT… puhon
10 | P a g e
• Obligate parasite on mucous • Choc agar- both X & V
membranes (“Mousy or Bleach-like odor)
• “Blood-lover” • SBA- X only (cannot grow if
• Growth requirements: Hemin (X pure if culture except
factor) – release from hemoglobin, Satellitism- around V factor
Nicotinamide-adenine dinucleotide/ producing oranisms: S. aureus,
NAD (V factor- heat labile) S. pneumoniae, Neisseria)
• QUAD plates
• Impregnated strips
• Do not grow on MAC
• Invasiveness (capsule) • Virulence factors: capsule, IgA
• Type B (Hib) – most invasive proteases, adherence,
infections, Pediatric population; lipooligosaccharide (LOS)
major cause of Meningitis in • Isolates should be tested for
children, Epiglottitis, arthritis, ß- lactamase
1. H. influenzae
cellulitis (cheek), acute pharyngitis
• Require both X and V
• Nontypeable – don’t have capsule,
• Will not grow on SBA
respiratory tract infections:
• Indole, Ornithine decarb (-)
sinusitis, otitis media, bronchitis,
pneuomonia • Urease (+)
• Same with H. influenzae but
• “Pink eye”- very contagious
2. H. aegyptius/biotype III Sucrose (+)
conjunctivitis
• Require both X and V
• Indole, Ornithine decarb (-)
• Brazilian Purpuric Fever (BPF)-
3. H. influenzae biogroup aegyptius • Urease (+)
invasive disease after conjunctivitis
• Require both X and V
• Chancroid (soft chancre) – genital • “School of Fish” formation
4. H. ducreyi ulcer and Buboes (swollen lymph • Require X factor only
nodes)- inguinal lymphadenopathy • Oxidase (-)
• Causative agent of endocarditis • ALA/Porphyrin Test (+) only
5. H. parainfluenzae, H.
• Low pathogenecity -test for Hemin (X), if (+) =
paraphrophilus
6. H. aphrophilus • Prefix “para”- require V factor would not require hemin
only for growth • H.aphrophilus – no factor req.
• Pasteurellosis (Cellulitis- most • “Sick” TSI reaction
common manifestation, • Grows on both CA and BA but
osteomyelitis meningitis, joint not MAC
B. Pasteurella multocida infections, pneumonia, • Oxidase, Catalase, Indole,
endophthalmitis) Nitrate (+)
• Normal RT/GI flora of animals: • Nonmotile, pleomorphic that
Cats & Dogs (bites,scratch, feces) shows Bipolar staining
• Brucellosis/“Undulent Fever” • Urease (+), OCN (+), H2S (+)
-Mediterranean/Malta/Gibraltar • Strict aerobe, some are
Neopolitan/Cyprus fever capnophilic, facultative
-Bang’s disease intracellular parasite, nonmotile
• Biosafety Level 3 organism • Serology- presumptive
C. Brucella • Potential Bioterrorism agent ∆ diagnosis (agglutinin
• Normal GI flora of animals absorption reaction)
• Infection from Contaminated Milk 1. Bone Marrow- most sensitive
products/exposure from slaughter 2. Biphasic Blood Culture Bottle
houses (abbatoir workers, • Fastidious but will grow on
veterinarian, meat packers) Brucella Agar, BYCE
(Brucella Buffered Charcoal
• Goats
1. B. melitensis Yeast Extract) , MTM, Farrel,
• Most common/pathogenic Kuzdas & Morse
Prepared by Jethro Rada Jr., RMT… puhon
11 | P a g e
2. B. suis • Swine • Fuchsin Dye inhibition (+)
• Capnophilic
3. B. abortus • Cattle
• Thionine Dye inhibition (+)
• Fuchsin Dye inhibition (+)
4. B. canis • Canines
• Only H2S (-)
5. B. neotomae • Dessert wood rat
• Do not cause human disease
6. B.ovis • Sheep
• Tularemia/“Deerfly Fever” • Glucose- “Cystine” Blood
-Skin ulcers (ulceroglandular), Agar- medium of choice
infections on lymph nodes • IsoVitalex supplemented CA
(glandular), eyes (ocuglandular), • BCYE
2. Francisella tularensis
lungs, oropharynx, and GI system • Ulcer scrapings (recommended)
• Carried by wild animals (deers, • Strict aerobe, facultative
rabbits, beavers, squirrels) intracellular parasite, nonmotile
• Insect (deerfly) and tick bites • Serology- Agglutination, DFA
• Biosafety Level 3 organism 1:160/fourfold- indicates
• Potential Bioterrorism agent ∆ tularemia
3. Legionella • Legionnaire’s Disease (severe • Oxidase, Hippurate hydrolysis
legionellosis) -pneumonia/febrile (+), assachrolytic, aerobic
• Pontiac Fever- flu like symptoms • Cannot grow on BA
• Water sources/systems: lakes, • BYCE- recommended
rivers, hot springs, humidifiers, • Urine antigen test- most
1. L. pneumophila whirlpools, air conditioning common
chillers (airborne)- bronchial wash • DFA test- most rapid
• Resistant to common chlorine (fluorescein isothiocyanate)
concentration • Autofluoresce when exposed
• Requires “L-Cysteine” to UV
2. L. micdadei • Pneumonia • Gelatinase, ß-lactamase (-)
4. Bordetella • Pertussis/“Whooping Cough” • Calcium alginate/Dacron swabs
• Three stages:
Catarrhal- general flu-like • Fastidious, Urease (-)
symptom • Mercury Droplets-like
Paroxysmal- repititive coughing, colonies, ß-hemolytic
“whoop” at the end • Bordet-Gengou (Potato
Convalescent- recovery phase infusion) agar
• From mucous membranes of the RT • Regan-Lowe (Charcoal-Horse
1. B. pertussis
of humans (Nasopharyngeal swab) blood agar)- also transport, best
• Virulence: • Amies transport medium
Pertussis toxin(PT)/ • Cephalexin are added to media
lymphocytosis promoting factor- • Will not grow on MAC
exotoxin, hemagglutinin, LPS, • Polymerase Chain Reaction -
Adenyl cyclase- most important best identification method
2. B. parapertussis • Mild respiratory infections • Fastidious, Urease (+)
• Kennel Cough in dogs
• Nonfastidious,
3. B. bronchiseptica*/bronchicanis • Contains silent copy of pertussis
• Rapid Urease (+)
toxin gene/RT infections
• Ubiquitous in the environment: soil, • TSI= K/K or K/NC (No
water, food, plants, milk Change) – first clue
Nonfermentors • Multidrug resistant • Non-spore forming
• Septicemia, meningitis, • Grow on SBA but varied
osteomyelitis, wound infections growth on MAC
Prepared by Jethro Rada Jr., RMT… puhon
12 | P a g e
• OF (Oxidative-Fermentative) • Oxidizer or Saccharolytic-
glucose test - Hugh and Leifson Acid/Yellow (+) on Open tube
formulation only
-determines if glucose is broken • Oxidizer/Fermentor-
down oxidatively or fermentatively Acid/Yellow (+) on both Open
• Two Tubes: and Close tube
1. Open- Unsealed • Asaccharolytic or Inert-
2. Close- Sealed with Mineral Green/Alkaline or neutral (-)
Oil/Vaspar(paraffin and petroleum) negative on both
A. Pseudomonas/Burkholderia* • Oxidase (+)
• “Swimmer’s Ear”/External Otitis • Green Metallic Sheen on
• Contact lens infections (Keratitis) “BA” due to Pyocyanin (+) -
• Jacuzzi/Hot Tub Syndrome blue water soluble pigment and
• Most common cause RT infections Pyoverdin- yellow/green
to Cystic Fibrosis patients fluorescein
• Bacteremia(Ecthyma gangrenosum) • “Fruity/Grape-like/Taco-
1. P. aeruginosa • Burn wound infections like/Corn tortillas odor
• Most important NBF (Non- • Blue-Green colonies on MAC
fermentative gram-negative bacilli) • “Pseudocel/CeTriMide
• Nosocomial infections (ICU), Agar”- enhances fluorescein
swimming pools, whirlpools production
• Member of pseudomonas • Seller’s or FN (Fluorescent-
fluorescent group Nitrate) media
• Resistant to many disinfectants • Very resitsant
2. P. fluorescens • Members of pseudomonas • Produce Pyoverdin
3. P. putida fluorescent group • Pyocyanin (-)
• Wrinkled, leathery, and
• Saprophyte, immunosupressed and adherent colonies
4. P. stutzeri
surgical patients • Light yellow/Brown pigment
• Lactose (-)
• Nonwrinkled colonies
• Second common cause to RT
• PC (P.cepacia) agar
5. B. cepacia* infections to Cystic Fibrosis
• Nonfluorescing yellow pigment
patients
• Lysine decarb (+)1/2
• Glanders (livestock disease-horses) • Nonmotile, grows on MAC
• CDC considers too dangerous for
6. B. mallei*
routine lab study Note: P. alcaligenes- do not
• Potential Bioterrorism agent ∆ produce Pyoverdin (fluorescein)
• Melioidosis/Pseudoglanders
-granulomatous pulmonary disease
• Wrinkled colonies
7. B. pseudomallei* • “Vietnamese Time Bomb”
• Lactose (+)
• Endemic to Southeast Asia,
northern Australia, found in soil
• Contaminants of swimming pool, • Yellow-pigmented
8. Sphingomonas (P.) paucimobilis hospital, and lab equipments pseudomonad
• Peritonitis, septicemia • Does not grow on MAC
• Misidentified as Salmonella • Produce large amount of H2S
9. Shewanella (P.) putrefaciens
(enteric) • Yellow colonies on HE
• Brevundimonas diminuta
• Comamonas species:
10. Other species • Brevundimonas vesicularis
P.acidovorans
Note: Ex-Pseudomonas: Bold • P.gladioli
P.testosteroni
• P.mendocina
• Methylobacterium extorguens
• P.alcaligens
Prepared by Jethro Rada Jr., RMT… puhon
13 | P a g e
• OXIDASE (-), Nitrite (-)
• Nonmotile, Catalase (+)
B. Acinetobacter • Nosocomial infections:
• Grows on MAC (Purplish
• *UTI, septicimia, pneumonia, Hue) and EMB
meningitis, tracheobronchitis, eye
1. A. baumanni (Herellea vaginicola) infections, endocarditis, cellulitis • Saccharolytic
2. A. lwoffii (Mima polymorpha) • Asaccharolytic
C. Stenotrophomonas (Xanthomonas) • Transient flora from hospitals* • OXIDASE (-), Maltose (+)
maltophilia • Not part of human flora • Lysine decarb (+) 2/2
Miscellaneous Nonfermentors
D. Alacaligenes species
1. A. faecalis/A. odorans
2. A. xylosoxidans
• With Peritrichous Flagella
E. Agrobacterium species
F. Oligella ureolytica
G. Ochrobactrum anthropi
• Nonmotile
H. Chryseobacterium/Flavobacterium
• Nosocomial, outbreaks of
1. C. meningosepticum
meningitis (contaminated • Oxidase (+)
2. C. odoratum
respiratory therapy equipment)
3. C. indologenes
• “Nebulizers”
I. Chryseomonas and Flavimonas K. Moraxella species
• Nonmotile
J. Sphingobacterium species 1. M. noliquefaciens/M. lacunata
2. M. phenylpyruvica/M. atlantae
Mycobacteria Photoreactivity: •Acid-Fast Bacilli
• Photochromogens- produce 1.Ziehl-Neelsen: heating/hot
Carotene pigment upon exposure to 2.
Kinyoun: cold
light •Nonmotile, non-spore forming,
• Scotochromogens- produce pigment strict aerobes
in light or the dark • Isolator Lysis-Centrifugation
• Nonchromogens- buff color System (ILCS)- saponin
• Catalase
Specimens: -30% H2O2 + Tween80
Sputum, Brochial washing, Urine,
Tuberculosis complex Blood and bone marrow, Stool, Media:
Tissue, other body fluids/CSF • Lowenstein-Jensen (LJ) agar
• NALC (N-Acetly-L-Cysteine) and • Petragnani, ATS
NaOH- use for liquefying/digestion • LJ-Gruft
and decontamination of sputum • Middlebrook solid (7H10,11)
• Nucleic acid assays: AccuProbe, • Middlebrook 7H9 broth/12,13
Strip assays, Direct nucleic -MGIT (M. growth index tube)
amplification, PCR, • BACTEC 460TB/BacTALERT
chromatography
• Cording (rough colonies)
• NIACIN (nicotinic acid)
• Tuberculosis
A. M. tuberculosis • NITRATE (+)
-“Ghon Complex”/Primary TB
• NAP (susceptible), T2H (R)
• Slow grower, Nonchromogen
• BGC vaccine (Bacille
• Bovine tuberculosis (cattles) Calmette-Guerin)
B. M. bovis
• Zoonotic • Susceptible to T2H/TCH
• Nonchromogen
C. M. africanum • Latest to be discovered
Prepared by Jethro Rada Jr., RMT… puhon
14 | P a g e
Nontuberculous/Aytpical/MOTT • Same with Tuberculous
• “Fried Egg”- dense center clns
• Most common systemic bacterial
A. M. avium complex/intracellulare • Slow grower= >7 days
infection in patients with
(MAC/MAI) • Nonchromogen
HIV/AIDS- lung/lymph infections
• Tellurite reduction (+)
• Nontuberculous mycobacterial
• Slow grower
Pulmonary Infections
B. M. kansasii • Photochromogen
• Isolated from tap water around the
• Nitrate (+)
world
• Isolated from Aquariums
• “Swimming Pool Granuloma”- • Photochromogen
C. M. marinum
Blue-Red subcutaneous nodule on
the elbow, knee= skin infection
• “Buruli ulceration”
D. M. ulcerans • Nonchromogen
• Skin leons/infection
E. M. gordonae • Tap-water Bacillus • Slow grower, Scotochromogen
• Cervical lymphadenitis • Slow grower
F. M. scrofulaceum
• Infections in chldren • Scotochromogen
• Requires hemin (ferric
G. M. haemophilium • Skin infection ammonium citrate)
• Grows on CA
• Weakly virulent
H. M. fortuitum/M. chelonae/M. • Abscesses, osteomyelitis, wound • Rapid grower= <7 days
abscessus and lung infection • Can grow on MAC without
crystal violet
• Crohn’s disease
I. M. paratuberculosis
• Regional enteritis
• Cannot be grown on artficial
• Leprosy/Hansen’s Disease
J. M. leprae media
• Armadillo- natural reservoir
• Diagnosis through skin lesions
Anaerobic Gram-Positive(+) Bacilli
Spore-Forming
(Exogenous Anaerobes)
A. Clostridium
• “Tackhead bacillus”
• Tetanus
• Round/Terminal spores-
• Lockjaw (Trismus), Distorted Grin
Resembles Tennis Racket or
1. C. tetani (Risus Sardonicus), “Spastic
Drumstick/lollipop
Paralysis”
• Motile, Gelatinase, Indole (+)
• Produce tetanospasmin
• Lecithinase, Lipase (-)
• Botulism- results to acute flaccid • Gelatinase, Indole,
paralysis and death Lecithinase, Lipase (+)
2. C. botulinum
-Infant botulism- most common • Motile
• Spoiled Canned-Good Bacillus • Spores resembles tennis racket
• Double Zone of ß-hemolysis
• Gas Gangrene (Myonecrosis)
on SBA, saccharolytic
• Major cause of Food Poisoning
• Reverse CAMP (+)
3. C. perfringens • Most important pathogen in the
• Nagler Test
genus
• Lecithinase (+) - EYA
• Post-abortion sepsis, enterocolitis
• NONMOTILE
Prepared by Jethro Rada Jr., RMT… puhon
15 | P a g e
• Antibiotic-associated
• CCFA (cycloserine-cefoxitin-
Pseudomembranous Colitis
fructose-agar)
4. C. difficile • Produce enterotoxin A/cytotoxin B
• Indole, Lecithinase, Lipase (-)
• Cultures should be performed on
• Motile
watery/unformed stools only
Non Spore-Forming
• Pelvic/genital actinomycosis- • “Spider Colonies” – first week
contaminated IUD (Intrauterine • “Molar Tooth” colonies- after
A. Actinomyces israelli/naeslundii device) • Exudates produce Sulfur
• Cervicofacial disease Granules
• Chest and abdomen infections • Capnophilic, Catalase (-)
• Called “Anaerobic diphteroids”
• Rarely pathogenic, NF of GIT/skin
B. Propionibacterium acnes/propionicus • Catalase, Indole (-)
• ACNE formation and SBE
(subacute bacterial endocarditis)
• Bacterial Vaginosis, PID, and • Curved bacillli
C. Mobiluncus
abdominal infections • Motile, Catalase, Indole (-)
• NF, helps to maintain acidic • Nonotile, Catalase (-)
D. Lactobacillus environment in the vagina • Aerotolerant anaerobes
• If low, increase risk of BV • Small a-hemolytic on SBA
E. Bifidobacterium • Nonpathogenic,
F. Eubacterium • NF of mouth and intestine
Anaerobic Gram-Negative(-) Bacilli
(Endogenous Anaerobes)
• Non-hemolytic on anaerobic
• Most common cause of anaerobic
BA
A. Bacteroides fragilis infections
• Bile Esculin (+) on BBE
B. ureolyticus • Normal flora of the colon
(bacteroides bile esculin) agar
• Produce foul odor
• Catalase (+)
• Brick Red Fluorescence
(young) and brown to black
• NF of RT, GIT, urogenital tract
(old) under UV light
B. Prevotella melaninogenica • Infections in the head, neck, UGT,
• Will grow on KVLB
and RT
(Kanamycin Vancomycin (R)
Laked Blood agar)
• Brick Red Fluorescence under
• NF of RT, GIT, urogenital tract
UV light
C. Porphyromonas • Infections in the head, neck, UGT,
• Will not grow on KVLB
and RT
• Susceptible to Vancomycin
• Trench Mouth- ulcerative
gingivitis
• Vincent’s Stomatitis/Angina
D. Fusobacterium • Opalescent with speckles
• Pulmonary, blood, sinus, dental
F. nucleatum- most common • Indole, Lipase (+)
infections and Brain abscesses-
F. necrophorum- more serious • Nitrate, Catalase (+)
associated with metastatic
conditions
Anaerobic Gram-Positive(+) Cocci
• Catalase (+)
A. Peptococcus niger • Produce Olive-Green colonies
that become Black
Prepared by Jethro Rada Jr., RMT… puhon
16 | P a g e
B. Peptostreptococcus anaerobius • NF of the intestine, female genital
P. magnus- Finegoldia magna tract, oral cavity, and respiratory • Inhibited by SPS (Sodium
P. asaccharolytica- Peptoniphilus tract Polyanethol Sulfonate)
asaccharolytica • Associated with Polymicrobial
C. Coprococcus species Liver, brain abscesses, wound
infections
Anaerobic Gram-Negative(-) Cocci
• Asaccharolytic
A. Veilonella
• Nitrite (+)
B. Acidaminococcus fermentans
C. Megasphaera elsdenii
Atypical Bacteria
• Obligate Intracellular Parasites
A. Chlamydia/Chlamydophila* • Cannot produce ATP
• Contain both DNA and RNA
• “Trachoma” (Leading cause of
Blindness)
• Inclusion conjunctivitis
• Lymphogranuloma venereum
(LGV) • Cytological Method
1. C. trachomatis
• NGU (Nongonococcal Urethritis) • Cell cultures, Serology
• Salpingitis- inflammation of the • NAATs (Nucleic Acid
Fallopian Tube Amplificatin Test)- most
• Perihepatitis (Fitz-Hugh-Curtis) common diagnostic method
Syndrome
• Psittacosis
2. C. psittaci* • Ornithosis
• Parrot Fever
• Formerly known as strain TWAR
3. C. pneumoniae* (Taiwan &America)
• Can cause Guillan-Barre Syndrome
• Smallest free-living organism
B. Mycoplasma • Fried-Egg appearance (Dienes
Stain) • M. pneumoniae involves
• Tracheobronchitis detection of cold agglutinins
• Primary Atypical Pneumonia that have anti-I specificity
(I antigen)
1. M. pneumoniae • Walking Pneumonia
Media:
• Eaton Agent/Pleuropneumonia-like
• For both- SP4 and A8 agars,
Organism (PPLO)
Shepard’s 10 B broth.
• PID (Pelvic Inflammatory Disease)
• For M. hominis- supplemented
2. M. hominis • Postpartum fever PPLO agar, Hayflick’s
• Salpingitis, Pyelonephritis Biphasic Medium.
• ‘T-strain mycoplasma’ • For Ureplasma- Shephard A-
• NGU (Nongonococcal Urethritis) 7B agar
C. Ureaplasma urealyticum
• Requires urea
D. Rickettsia/Orientia/Ehrlichia/
Disease Vector Reservoir
Coxiella/Bartonella/Anaplasma
• Rocky Mountain Spotted Fever
1. R. rickettsii Tick Dogs, Rodents
• Proteus OX-2
• Bouttoneuse Fever (Taches
2. R. conorii Tick Dogs, Rodents
Noires- Black Dot)
Prepared by Jethro Rada Jr., RMT… puhon
17 | P a g e
3. R. akari • Rickettsial Pox Chigger Mouse
• Epidemic Typhus
4. R. prowazekii Louse Flying Squirrel
• Brill-Zinsser Disease
5. R. typhi • Endemic (Murine) Thypus Rat flea Rats
6. O. tsutsugamushi • Scrub Thypus Mites/Chigger Rodents, Mice
7. B. quintana • Trench Fever Body Louse Humans
• Oroya Fever Sand Fly
8. B. bacilliformis Humans
• Verruga Peruana (Phlebotomus)
9. B. henselae • Cat Scratch Disease Cat
None
10. C. burnetii • Q Fever
(Inhalation)
11. E. canis • Ehrliciosis Tick
12. E. sennetsu • Sennetsu Fever Notes for Rickettsiae:
• Obligate Intracellular Parasites
• Human Monocytotropic
13. E. chaffeensis • Well-Felix serologic test
Ehrliciosis
(utilize Proteus antigen)
• Grown in embryonated eggs
• Human Granulocytotropic and tissue cells but required
14. A. phagocytophilum
Ehrliciosis biosafety lever 3 laboratory
when cultured
Spirochetes
A. Treponema
• Darkfield (White against
Black)
• Syphilis • Nontreponemal test- VDRL
• French Disease/Italian Disease (Venereal Disease Research
• Lues Laboratory)
1. T. pallidum
• The Great Pox • Treponemal test- FTA-ABS
• Jarisch-Herxheimer reaction (Fluorescent Treponemal
(during treatment) Antibody Absorption) and TP-
PA (Treponema Pallidum
Particulate Antigen)
2. T. pallidum subsp pertenue • Yaws
• Bejel
3. T. pallidum subsp endemicum
• Endemic Syphilis
4. T. carateum • Pinta
• Can be examined under Light
B. Borrelia
Microscope
• Direct Microscopic Exam
• Relapsing Fever
(most useful): Blood smear –
• Tick-borne (Ornithodorus)
1. B. recurrentis Giemsa or Wright Stain
• Louse-borne (Pediculus humanus • Also Darkfield
humanus)
• Kelly’s medium
• Lyme Disease
• Pseudojuvenile Rheumatoid
2. B. burgdorferi Arthritis • Western Immunoblotting
• Erythema Chronicum Migrans -
Bull’s Eye rash
Prepared by Jethro Rada Jr., RMT… puhon
18 | P a g e
C. Leptospira • Have Hooked Ends • Corkscrew motility
1. L. biflexa • Saprophytic leptospiras
• Leptospirosis
• Weil’s Disease (Icteric)/ Infectious • Direct examination (Darkfield),
Jaundice Blood- most sensitive, CSF,
and Urine
• Pretibial fever
2. L. interrogans • Silver Stain
• Ft. Bragg fever
• Media: EMJH (Ellinghausen-
• March fever
McCullough-Johnson-Harris),
• Seven-day fever Fletcher’s, and Stuart
• Swineherder’s disease
Miscellaneous Organisms
• Infections caused by animal bites, • Gram (-) Bacilli
which result to ‘Cellulitis’ • “Starlike center colonies” in
1. Actinobacillus/Aggregatibacter*
• Asso. w/ endocarditis and gum SBA
actinomycetemcomitans
disease • Dots and Dashes of Morse
• Member of HACEK (fastidious) Code (Staining)
• Human Bite Wounds and
• Gram (-) Bacilli, oxidase (+)
Clenched-Fist Wounds on the face
• Seldom found of pure cutures
2. Eikenella corrodens • Abscesses of the Oral cavity
• Flat spreading on BA
• Endocarditis
• “Pitting of Agar”
• Member of HACEK (fastidious)
• Gram Variable (+ appear -)
• Bacterial Vaginosis
Coccobacilli
• Isolation may not be clinically
3. Gardnerella vaginalis • Presence of Clue Cells
significant, cultures are not
• Amsel and Nugent scoring
recommended
systems are used
• Streptobacillary Ratbite
Fever/Streptobacillosis
• Gram (-) Bacilli
• “Haverhill Fever”
4. Streptobacillus moniliformis • Infusion Broths – (Dextrose
-Erythema Arthriticum
Veal and Tomato Extract Veal)
Epidemicum (milk or waterborne)
• Develop L Forms
• Spirillary Ratbite Fever
5. Spirillum minor/Spirillum morsus
• Sodoku • Gram (-) Spirilla
muris
• Spirillosis
• Gram (-) Bacilli, nonmotile
• associated with endocarditis • Weak Indole Positive (-)?
6. Cardiobacterium hominis
• Member of HACEK (fastidious) • Oxidase (+), Catalase (-)
• Will grow on SBA, +YE
• Whipple’s Disease (Intestinal
7. Tropheryma whippelii • Gram (+) Bacilli
lipodystrophy)
• “Gliding motility” on
• Periodontal disease Darkfield Microscopy
8. Capnocytophaga species
• Isolated from oral cavity, • Gram (-) Bacilli
• Fermentor, Fastidious
References: Success in Clinical Laboratory Science, Pearson (Fourth Edition) by Ciulla and Lehman
Lecture Notes in Bacteriology for AUP MLS 100% Students, by Ferdinand Mendoza
Prepared by Jethro Rada Jr., RMT… puhon
You might also like
- Dermatology Notes for Medical StudentsFrom EverandDermatology Notes for Medical StudentsRating: 4 out of 5 stars4/5 (5)
- NEW! Cursed Objects and Demon InfestationDocument21 pagesNEW! Cursed Objects and Demon Infestationspidey4No ratings yet
- Infectious-Disease Tables PDFDocument81 pagesInfectious-Disease Tables PDFMiguel CuevasNo ratings yet
- Vaginal Discharge GuidelineDocument4 pagesVaginal Discharge GuidelineGung Bagvs SaputraNo ratings yet
- S. Aureus, Cons: S.Epidermidis, Cons: S.SaprophyticusDocument14 pagesS. Aureus, Cons: S.Epidermidis, Cons: S.SaprophyticusMugiNo ratings yet
- MCQ GynecologyDocument25 pagesMCQ GynecologyAli Alhaddi80% (5)
- Bacteriology DemonstrationsDocument12 pagesBacteriology Demonstrationshamody662002100% (1)
- Detailed Micro ChartDocument6 pagesDetailed Micro Chartmatt100% (1)
- Communicablediseaseqa 140829080936 Phpapp02Document20 pagesCommunicablediseaseqa 140829080936 Phpapp02Keiarah Kath Estrada CallaoNo ratings yet
- Special MicrobiologyDocument68 pagesSpecial MicrobiologyrefuapalackyNo ratings yet
- Bacteria List Exam 1 PDFDocument16 pagesBacteria List Exam 1 PDFJamesHowsonNo ratings yet
- Drug StudyDocument10 pagesDrug StudybaniniycsebNo ratings yet
- BacteriologyDocument20 pagesBacteriologyOj Alimbuyuguen100% (2)
- STi PresentationDocument20 pagesSTi PresentationPheywood1234No ratings yet
- Bacteriology Midterms GomezDocument20 pagesBacteriology Midterms GomezAive BelistaNo ratings yet
- Bacteriology 1: - Non MotileDocument27 pagesBacteriology 1: - Non MotileYeshaa MiraniNo ratings yet
- Bacteria-Borne Diseases Handout 2022Document3 pagesBacteria-Borne Diseases Handout 2022Anna CrisNo ratings yet
- StaphylococcusDocument4 pagesStaphylococcusipad backupNo ratings yet
- Slide XDocument21 pagesSlide XKok MerngNo ratings yet
- Staphylococci: MaheshyadavDocument36 pagesStaphylococci: MaheshyadavMuhammad IlhamNo ratings yet
- StaphDocument6 pagesStaphpekibelssNo ratings yet
- 1.01 - Staphylococcus, Haemophilus, Bordatella, Brucella, FrancisellaDocument5 pages1.01 - Staphylococcus, Haemophilus, Bordatella, Brucella, FrancisellaPrincess MarielleNo ratings yet
- Bacteria Chart FINAL 3 2Document32 pagesBacteria Chart FINAL 3 2Йеша Маниш МираниNo ratings yet
- Staphylococc I: Ni Nyoman Desi Bintari, S.Si.,M.SiDocument36 pagesStaphylococc I: Ni Nyoman Desi Bintari, S.Si.,M.SiDesi BintariNo ratings yet
- Screenshot 2022-06-27 at 4.04.28 PMDocument98 pagesScreenshot 2022-06-27 at 4.04.28 PMikraanmohamedmahamuudNo ratings yet
- MicroPara Compre Review 2021 - Dr. HemedezDocument65 pagesMicroPara Compre Review 2021 - Dr. HemedezStephenMontoyaNo ratings yet
- Bacteriology by Dhshan Hassan DhshanDocument48 pagesBacteriology by Dhshan Hassan Dhshanعلي الكوافي100% (1)
- 1 Bacte Mtap 1Document12 pages1 Bacte Mtap 1DENISE MARA�ANo ratings yet
- Week-6.1 GramPositiveCocci 1stpartDocument6 pagesWeek-6.1 GramPositiveCocci 1stpartRegine Delos SantosNo ratings yet
- Bacte Midterm (Walang Pictures)Document21 pagesBacte Midterm (Walang Pictures)AL-HUSSEIN NAWABNo ratings yet
- Gram Positive - Cocci PDFDocument4 pagesGram Positive - Cocci PDFJasmine BunaoNo ratings yet
- Qname Class Gram RXN, Morph, Char Tsi RXN Medium Colonies Diseases Caused Virulence Factors, Toxins and Enzymes Lab DXDocument6 pagesQname Class Gram RXN, Morph, Char Tsi RXN Medium Colonies Diseases Caused Virulence Factors, Toxins and Enzymes Lab DXsorryandreosayanisalreadytakenNo ratings yet
- Bacteria PDFDocument13 pagesBacteria PDFJohn Christopher LucesNo ratings yet
- 16-PYOGENIC COCCI and 17 - NEISSERIADocument5 pages16-PYOGENIC COCCI and 17 - NEISSERIAJesette KhoNo ratings yet
- Microbiology Lec 2 - Clinical Bacteriology - Gram Positive CocciDocument68 pagesMicrobiology Lec 2 - Clinical Bacteriology - Gram Positive CocciRochelle Joyce AradoNo ratings yet
- Clinical Bacteriology MidtermDocument32 pagesClinical Bacteriology MidtermRazmine RicardoNo ratings yet
- Chapter 14: STAPHYLOCOCCI: StaphylococcusDocument8 pagesChapter 14: STAPHYLOCOCCI: StaphylococcusJezzah Mae CañeteNo ratings yet
- Reviewer - Bacteriology FINALS - ANGELES, ANGELICDocument38 pagesReviewer - Bacteriology FINALS - ANGELES, ANGELICAngelic AngelesNo ratings yet
- MICROBIOLOGYDocument94 pagesMICROBIOLOGYKiranNo ratings yet
- MODULE 6 Supplement APRIL 2018 PDFDocument3 pagesMODULE 6 Supplement APRIL 2018 PDFEryll Paolo AleaNo ratings yet
- Chart - Gram Positive BacteriaDocument2 pagesChart - Gram Positive BacteriaRedNo ratings yet
- Cpe Common Diagnoses 6-4-2021Document9 pagesCpe Common Diagnoses 6-4-2021Shubham HarishNo ratings yet
- Common Cause: Staphylococcus Spp. Streptococcus Spp. Enterococcus SPPDocument8 pagesCommon Cause: Staphylococcus Spp. Streptococcus Spp. Enterococcus SPPAdel mohammadNo ratings yet
- Paraproteinemia (Multiple Myeloma)Document15 pagesParaproteinemia (Multiple Myeloma)YunQingTanNo ratings yet
- C16-Aerobic Gram BacilliDocument9 pagesC16-Aerobic Gram BacilliJezzah Mae CañeteNo ratings yet
- MSK StaphDocument3 pagesMSK Staphعبدالرحمن عابدNo ratings yet
- Notes: Bacillus Anthracis (Anthrax)Document6 pagesNotes: Bacillus Anthracis (Anthrax)Woo Rin ParkNo ratings yet
- S. Pyogenes: 4, 6B, 9V, 14, 18C, 19F, 23F Conjugated With Nontoxic Diphtheria-ToxinDocument1 pageS. Pyogenes: 4, 6B, 9V, 14, 18C, 19F, 23F Conjugated With Nontoxic Diphtheria-ToxinRica MarquezNo ratings yet
- Bacte Midterm Di TaposDocument9 pagesBacte Midterm Di TaposAL-HUSSEIN NAWABNo ratings yet
- Med Micro BugsDocument16 pagesMed Micro BugsKaitlyn CabreraNo ratings yet
- Pathology Week 2 FKHDocument5 pagesPathology Week 2 FKHAnna TohNo ratings yet
- Chapter 15: Streptococci, Enterococcus, and Other Catalase-Negative, Gram-Positive CocciDocument9 pagesChapter 15: Streptococci, Enterococcus, and Other Catalase-Negative, Gram-Positive CocciJezzah Mae CañeteNo ratings yet
- Parasitology Table 1Document5 pagesParasitology Table 1William BufNo ratings yet
- BACTERIADocument14 pagesBACTERIARochelle Joyce AradoNo ratings yet
- AEROBIC, GRAM POS BACILLI NON-SPORE FORMER (Nahaeminrmt)Document7 pagesAEROBIC, GRAM POS BACILLI NON-SPORE FORMER (Nahaeminrmt)Rach ReyesNo ratings yet
- Small Intestine 01 PDFDocument9 pagesSmall Intestine 01 PDFfadoNo ratings yet
- Pedia Bacte Table 08amDocument25 pagesPedia Bacte Table 08ampedia blue bookNo ratings yet
- Rickettsial DiseasesDocument9 pagesRickettsial Diseasesaminshafihassan902No ratings yet
- 1-Pyogenic CocciDocument77 pages1-Pyogenic CocciMooNy LibyaNo ratings yet
- Enterobacteriaceae 2Document11 pagesEnterobacteriaceae 2odhiambo samwelNo ratings yet
- Gram Positive Cocci Reviewer 1Document6 pagesGram Positive Cocci Reviewer 1alianaNo ratings yet
- Streptococci and Enterococci and OthersDocument11 pagesStreptococci and Enterococci and OthersthedarkwingNo ratings yet
- Gram Negative CocciDocument3 pagesGram Negative CocciAlexander PanodNo ratings yet
- Paraproteinemia (Multiple Myeloma) - : Monoclonal Plasma Cells Destructive Bony Lesions (OSTEOLYTIC) Multiple SitesDocument11 pagesParaproteinemia (Multiple Myeloma) - : Monoclonal Plasma Cells Destructive Bony Lesions (OSTEOLYTIC) Multiple SitesYunQingTanNo ratings yet
- Culture MediaDocument2 pagesCulture MediaAJNo ratings yet
- MaslowDocument1 pageMaslowAJNo ratings yet
- Anemia of Impaired and Defective Production of N CellsDocument5 pagesAnemia of Impaired and Defective Production of N CellsAJNo ratings yet
- UntitledDocument1 pageUntitledAJNo ratings yet
- General History PDFDocument52 pagesGeneral History PDFAJNo ratings yet
- Finals Notes 1Document3 pagesFinals Notes 1AJNo ratings yet
- Re Finals TranscribedDocument8 pagesRe Finals TranscribedAJNo ratings yet
- Second Quarter Business Simulation ABM 12Document10 pagesSecond Quarter Business Simulation ABM 12AJNo ratings yet
- Literary CriticismsDocument8 pagesLiterary CriticismsAJNo ratings yet
- 2019 2020 Immersion DistributionDocument2 pages2019 2020 Immersion DistributionAJNo ratings yet
- Examine The Title of The Poem: Decontrusting "Spelling" by Margaret AtwoodDocument2 pagesExamine The Title of The Poem: Decontrusting "Spelling" by Margaret AtwoodAnthony ChanNo ratings yet
- NSG Care of Gynecological Problems Compile NoteDocument19 pagesNSG Care of Gynecological Problems Compile NoteAce WolverineNo ratings yet
- Through A Glass Darkly: A Disappointing New Biography of King Sebastian of Portugal. A Review/essay by Harold B. JohnsonDocument10 pagesThrough A Glass Darkly: A Disappointing New Biography of King Sebastian of Portugal. A Review/essay by Harold B. Johnsonricardo_farneseNo ratings yet
- Case Taking SheetDocument3 pagesCase Taking Sheetssrkm guptaNo ratings yet
- Filipino Masculinity: Camilo A.B. Naraval, MD MSC Health Management and Research GroupDocument43 pagesFilipino Masculinity: Camilo A.B. Naraval, MD MSC Health Management and Research GroupkimcharriseNo ratings yet
- Ophthalmia neonatorumIIDocument29 pagesOphthalmia neonatorumIIgopscharanNo ratings yet
- Myiasis - "Community Dermatology Journal"Document12 pagesMyiasis - "Community Dermatology Journal"chaariaNo ratings yet
- Health 9 Venereal Diseases: - Caused by A Bacteria Named Chlamydia TrachomatisDocument8 pagesHealth 9 Venereal Diseases: - Caused by A Bacteria Named Chlamydia TrachomatisClaire MedianaNo ratings yet
- Sexually Transmitted Diseases OverviewDocument45 pagesSexually Transmitted Diseases OverviewJean De Vera MelendezNo ratings yet
- 5.1 - Infectious Diseases PDFDocument8 pages5.1 - Infectious Diseases PDFVince Alvin DaquizNo ratings yet
- Psychology Internals ContentDocument23 pagesPsychology Internals ContentMohit KapseNo ratings yet
- Determinant Factors That Influence The Prevalence of Gonorrhea in Female Sex Wokers in YogyakartaDocument12 pagesDeterminant Factors That Influence The Prevalence of Gonorrhea in Female Sex Wokers in YogyakartaSiti MaesarohNo ratings yet
- Brief History SyphilisDocument10 pagesBrief History SyphilisMichał Jakub WagnerNo ratings yet
- Guideline Antibiotic RationalDocument35 pagesGuideline Antibiotic RationalIstianah EsNo ratings yet
- Algorithm MkacsDocument1 pageAlgorithm MkacsKrystel SeseNo ratings yet
- Jurnal KelDocument3 pagesJurnal Kelandre erlisNo ratings yet
- Caso Clínico - Neisseria GonorrhoeaeDocument7 pagesCaso Clínico - Neisseria GonorrhoeaeRigobertoNo ratings yet
- Ethically Impossible PCSBIDocument220 pagesEthically Impossible PCSBIYuying TsongNo ratings yet
- ID For ABIM - Parham 2014Document140 pagesID For ABIM - Parham 2014Jeronim H'gharNo ratings yet
- Ophthalmia NeonatorumDocument12 pagesOphthalmia NeonatorumDemewoz Fikir100% (2)
- Etextbook 978 0134019192 Microbiology With Diseases by TaxonomyDocument62 pagesEtextbook 978 0134019192 Microbiology With Diseases by Taxonomylashawn.fain938100% (48)
- Licensure 2019 Telegram Group: Test 12.... ObstetricsDocument6 pagesLicensure 2019 Telegram Group: Test 12.... ObstetricsKumah Wisdom100% (1)
- STD QuizDocument97 pagesSTD Quizapi-298576907No ratings yet
- STDDocument49 pagesSTDJanneel CannonierNo ratings yet