Professional Documents
Culture Documents
Physical Assessment Guide Nose Mouth Throat and Sinuses
Uploaded by
Rhelina Min0 ratings0% found this document useful (0 votes)
52 views4 pagesOriginal Title
Physical-Assessment-Guide-Nose-Mouth-Throat-and-Sinuses
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
52 views4 pagesPhysical Assessment Guide Nose Mouth Throat and Sinuses
Uploaded by
Rhelina MinCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
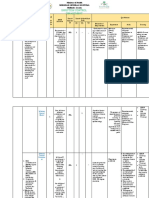
ASSESSMENT OF THE NOSE, MOUTH, THROAT AND SINUSES
INTERVIEWING AND RECORDING ASSESSMENT FINDINGS
Use the following Nursing History Checklist to interview and record your findings from a
mouth, throat, nose, and sinus assessment of a peer, friend, or family member.
Nursing History Checklist
Nursing History Guide to Collect Subjective Data
Current Symptoms
1. Mouth problems (tongue or mouth sores or
lesions, gum or mouth redness, swelling,
bleeding, or pain)
2. Sinus problems (pain over sinuses, postnasal
drip)?
3. Nose problems (nose bleeds, stuffy nose,
cannot breathe through one or both nostrils,
change in ability to smell or taste)?
Past History
1. Previous problems with mouth, throat, nose,
pr sinuses (surgeries or treatment; how much
and how often)?
2. Use of nasal sprays?
3. History of tooth grinding?
4. Last dental exam? Fit of dentures?
Family History
1. Family history of oral, nasal, or sinus cancer
or chronic problems?
Lifestyle and Health Practices
1. Daily practice of oral care, tooth care, or
denture care?
2. Usual diet?
3. History of smoking, use of, how much, and
how often?
4. Use of alcohol (how much and how often)?
PERFORMING PHYSICAL ASSESSMENT
Use the following Physical Assessment Checklist to examine the eye of a peer, friend, or
family member. Column 1 can be used by you to guide your physical assessment. Column 2
may be used for your documentation.
Physical Assessment Checklist
Physical Assessment Guide to Collect Objective Data
Assessment Skill
1. Gather equipment (gloves, cotton gauze pads,
penlight, speculum attached to otoscope, tongue
blade) hand hygiene, provide privacy
2. Identify the client and explain procedures to
client
Mouth
1. Inspect the lips. Observe lip consistency and
color.
2. Inspect the teeth and gums. Ask the client to
open the mouth. Note the number of teeth,
color, and condition. Note any repairs such as
crowns and any cosmetics such as veneers. Ask
the client to bite down as though chewing on
something and note the alignment of the lower
and upper jaws. Put on gloves and retract the
client’s lips and cheeks to check gums for color
and consistency.
3. Inspect the buccal mucosa. Use a penlight
and tongue depressor to retract the lips and
cheeks to check color and consistency. Also
note Stenson’s ducts (parotid ducts) located on
the buccal mucosa across from the second
upper molars
4. Inspect and palpate the tongue. Ask client to
stick out the tongue. Inspect for color, moisture,
size, and texture. Observe for fasciculations
(fine tremors), and check for midline protrusion.
Palpate any lesions present for induration
(hardness).
5. Assess the ventral surface of the tongue. Ask
the client to touch the tongue to the roof of
mouth, and use a penlight to inspect the ventral
surface of the tongue, frenulum, and area under
the tongue.
Palpate the area if you see lesions, if the client
is over age 50, or if the client uses tobacco or
alcohol. Note any induration. Check also for a
short frenulum that limits tongue motion (the
origin of “tongue-tied”).
6. Inspect for Wharton’s ducts—openings from
the submandibular salivary glands— located on
either side of the frenulum on the floor of the
mouth.
7. Observe the sides of the tongue. Use a
square gauze pad to hold the client’s tongue to
each side. Palpate any lesions, ulcers, or
nodules for induration
8. Check the strength of the tongue. Place your
fingers on the external surface of the client’s
cheek. Ask the client to press the tongue’s tip
against the inside of the cheek to resist pressure
from your fingers. Repeat on the opposite
cheek.
9. Check the anterior tongue’s ability to taste.
Place drops of sugar and salty water on the tip
and sides of tongue with a tongue depressor.
10. Inspect the hard and soft palates and uvula.
Ask the client to open the mouth wide while you
use a penlight to look at the roof. Observe color
and integrity
11. Note odor. While the mouth is wide open, note
any unusual or foul odor.
12. Assess the uvula. Apply a tongue depressor to
the tongue (halfway between the tip and back of
the tongue) and shine a penlight into the client’s
wide-open mouth. Note the characteristics and
positioning of the uvula. Ask the client to say
“aaah” and watch for the uvula and soft palate to
move.
13. Inspect the tonsils. Using the tongue
depressor to keep the mouth open wide, inspect
the tonsils for color, size, and presence of
exudate or lesions. Grade the tonsils.
14. Inspect the posterior pharyngeal wall.
Keeping the tongue depressor in place, shine
the penlight on the back of the throat. Observe
the color of the throat, and note any exudate or
lesions. Before inspecting the nose, discard
gloves and perform hand hygiene
Nose
1. Inspect and palpate the external nose. Note
nasal color, shape, consistency, and
tenderness.
2. Check patency of air flow through the nostrils
by occluding one nostril at a time and asking
client to sniff.
3. Inspect the internal nose. To inspect the
internal nose, use an otoscope with a short
wide-tip attachment or you can also use a nasal
speculum and penlight. s. If an otoscope is
unavailable, use a penlight and hold the tip of
the nose slightly up. A nasal speculum with a
penlight also facilitates good visualization.
Sinuses
1. Palpate the sinuses. When an infection is
suspected, the nurse can examine the sinuses
through palpation, percussion, and
transillumination. Palpate the frontal sinuses by
using your thumbs to press up on the brow on
each side of nose.
2. Palpate the maxillary sinuses by pressing with
thumbs up on the maxillary sinuses
3. Percuss the sinuses. Lightly tap (percuss) over
the frontal sinuses and over the maxillary
sinuses for tenderness.
4. Transilluminate the sinuses. If sinus
tenderness was detected during palpation and
percussion, transillumination will let you see if
the sinuses are filled with fluid or pus.
Transilluminate the frontal sinuses by holding a
strong, narrow light source snugly under the
eyebrows (the room should be dark). Repeat
this technique for the other frontal sinus.
5. Transilluminate the maxillary sinuses by
holding a strong, narrow light source over the
maxillary sinus and asking the client to open his
or her mouth. Repeat this technique for the
other maxillary sinus
Analysis of Data
1. Formulate a Nursing Diagnosis
2. Formulate collaborative problems
3. Make necessary referrals
You might also like
- Examination of The ThroatDocument10 pagesExamination of The Throatsejal3vijNo ratings yet
- Health Assessment ChecklistDocument14 pagesHealth Assessment ChecklistLindy JaneNo ratings yet
- Examination of NoseDocument63 pagesExamination of NoseDr Sravya M VNo ratings yet
- Functional Examination of NoseDocument12 pagesFunctional Examination of Nosevinnu kalyanNo ratings yet
- Anatomy of The Eye EYE: Extaocular StructuresDocument5 pagesAnatomy of The Eye EYE: Extaocular StructuresfLOR_ZIANE_MAENo ratings yet
- Approach To An Unconscious Patient-OyeyemiDocument41 pagesApproach To An Unconscious Patient-OyeyemiOyeyemi AdeyanjuNo ratings yet
- Health AssessmentDocument2 pagesHealth AssessmentrojeanrubinoNo ratings yet
- Wound DressingDocument18 pagesWound DressingKristi Elly YoehanaNo ratings yet
- Lab Guide: Musculoskeletal AssessmentDocument6 pagesLab Guide: Musculoskeletal AssessmentDaisy MellaNo ratings yet
- Respiratory Care and Breathing ExercisesDocument13 pagesRespiratory Care and Breathing ExercisesLiane BartolomeNo ratings yet
- Week 2 Electrolyte Imbalance Group Work INSTRUCTOR 1 PDFDocument8 pagesWeek 2 Electrolyte Imbalance Group Work INSTRUCTOR 1 PDFMaica LectanaNo ratings yet
- 2 - BPE - Eye ExaminationDocument50 pages2 - BPE - Eye ExaminationZauhar NurdildayevaNo ratings yet
- Rinnes and WebersDocument22 pagesRinnes and WebersSelvi YapNo ratings yet
- Assessing Head, Face and NeckDocument112 pagesAssessing Head, Face and NeckHyacinth Jane Dela PeñaNo ratings yet
- CholeraDocument4 pagesCholeraBeth AvelinoNo ratings yet
- Assessment of The Renal and Urinary Tract Syatems NewDocument27 pagesAssessment of The Renal and Urinary Tract Syatems NewMay LindaNo ratings yet
- Acute Rheumatic FeverDocument20 pagesAcute Rheumatic Feverfaizal samadNo ratings yet
- Embryology of The Ear and Its AnatomyDocument20 pagesEmbryology of The Ear and Its AnatomyElisa NNo ratings yet
- Tetanus (Lockjaw) PDFDocument8 pagesTetanus (Lockjaw) PDFGLADYS MAY GUDELOS MEJIASNo ratings yet
- Blood Glucose Test ExplainedDocument3 pagesBlood Glucose Test ExplainedDiana MuañaNo ratings yet
- Procedure Checklist Chapter 19: Assessing The Ears and HearingDocument2 pagesProcedure Checklist Chapter 19: Assessing The Ears and HearingjthsNo ratings yet
- Child Ear Infection CausesDocument9 pagesChild Ear Infection CausesMona Santi NainggolanNo ratings yet
- BERA Test Explained: What is Brainstem Evoked Response AudiometryDocument34 pagesBERA Test Explained: What is Brainstem Evoked Response Audiometryassumpta0% (1)
- Neurological Assessment ToolsDocument52 pagesNeurological Assessment ToolsJosephine George JojoNo ratings yet
- Factors Affecting Blood Pressure (BPDocument3 pagesFactors Affecting Blood Pressure (BPKarl Ian MaliwatNo ratings yet
- Assessment of The AbdomenDocument98 pagesAssessment of The Abdomenyanna aNo ratings yet
- MENINGITIS Lesson PlanDocument12 pagesMENINGITIS Lesson PlannidhiNo ratings yet
- Conjuctiva Project NewDocument19 pagesConjuctiva Project NewMakhanVermaNo ratings yet
- Chest InjuryDocument52 pagesChest InjuryJeyaganesh SellvarajuNo ratings yet
- What Is The Difference Between A Vial & An Ampule?Document2 pagesWhat Is The Difference Between A Vial & An Ampule?Gousul alamNo ratings yet
- Acute Incisional Hernia: Theme From September 2011 ExamDocument146 pagesAcute Incisional Hernia: Theme From September 2011 ExamVimal Kumar YadavNo ratings yet
- Checklist Exam of EarDocument4 pagesChecklist Exam of EarCes Melisse DNo ratings yet
- DONNING and DOFFING PPEDocument16 pagesDONNING and DOFFING PPEDranlie LagdamenNo ratings yet
- NSG 300c Care Plan 1Document10 pagesNSG 300c Care Plan 1api-521018364No ratings yet
- Functional Status QuestionnaireDocument7 pagesFunctional Status QuestionnaireTO Joss AguilarNo ratings yet
- BR AsthmaDocument17 pagesBR AsthmaAkarsh RamNo ratings yet
- OncologyDocument175 pagesOncologyabdurehmanNo ratings yet
- Operating Room Delivery Instruments GuideDocument59 pagesOperating Room Delivery Instruments GuideMayolianne DumayNo ratings yet
- Neurological Exam Lecture NotesDocument26 pagesNeurological Exam Lecture NotesNaveen KovalNo ratings yet
- Diabetes Mellitus - Nursing CareDocument51 pagesDiabetes Mellitus - Nursing CareJoice DasNo ratings yet
- Tracheostomy: S.No: Time Specific Objective Content Teachin G Activity Learning Activity Av Aids EvaluationDocument13 pagesTracheostomy: S.No: Time Specific Objective Content Teachin G Activity Learning Activity Av Aids EvaluationaparnaNo ratings yet
- Tracheostomy CareDocument11 pagesTracheostomy CareRiza Angela Barazan100% (1)
- Acute Otitis Media: Symptoms, Causes, DiagnosisDocument11 pagesAcute Otitis Media: Symptoms, Causes, DiagnosisAnkita BramheNo ratings yet
- Lesson Notes - Insulin PenDocument6 pagesLesson Notes - Insulin PenNicole Marin-Ching100% (1)
- Atopic DermatitisDocument26 pagesAtopic DermatitisninarizkiNo ratings yet
- Dr. Naitik D Trivedi & Dr. Upama N. Trivedi: 10. Urinary SystemDocument27 pagesDr. Naitik D Trivedi & Dr. Upama N. Trivedi: 10. Urinary SystemKunal DangatNo ratings yet
- Bells Palsy DorisDocument37 pagesBells Palsy DoristheychemNo ratings yet
- Range of Motion Exercises for Joint MobilityDocument5 pagesRange of Motion Exercises for Joint MobilityLevy DuranNo ratings yet
- Respiratory System AssessmentDocument13 pagesRespiratory System Assessmentavinash dhameriyaNo ratings yet
- Ministry of Health hospital infection control departments staffing guideDocument3 pagesMinistry of Health hospital infection control departments staffing guideSherina EddingNo ratings yet
- Assessing The Respiratory System (Thorax & Lungs)Document3 pagesAssessing The Respiratory System (Thorax & Lungs)JENNA ELOISA UYNo ratings yet
- Allergic RhinitisDocument10 pagesAllergic Rhinitisjaikishan marathe 69No ratings yet
- TVU Nursing Care PlanDocument19 pagesTVU Nursing Care Planjyoti singhNo ratings yet
- Anatomy of the Ear BreakdownDocument44 pagesAnatomy of the Ear Breakdownrinaldy agungNo ratings yet
- Bisecting and Parelling TechniqueDocument32 pagesBisecting and Parelling TechniqueArka Saha100% (1)
- Cystic FibrosisDocument35 pagesCystic Fibrosisvani reddyNo ratings yet
- Mouth Throat Nose and Sinuses Assessment FindingsDocument5 pagesMouth Throat Nose and Sinuses Assessment FindingsChris SmithNo ratings yet
- Skill: Assessing The Mouth and Oropharynx: Lips and Buccal MucosaDocument3 pagesSkill: Assessing The Mouth and Oropharynx: Lips and Buccal MucosaAlmira GamaoNo ratings yet
- Pet - Assessing The Mouth and OropharynxDocument2 pagesPet - Assessing The Mouth and Oropharynxgenesis victorinoNo ratings yet
- Assessing Mouth and OropharynxDocument2 pagesAssessing Mouth and OropharynxAlyssa Laine Garcia LadieroNo ratings yet
- Micp Report Group 6Document14 pagesMicp Report Group 6Rhelina MinNo ratings yet
- Micp Report Group 6Document14 pagesMicp Report Group 6Rhelina MinNo ratings yet
- Unds Assignment 1Document2 pagesUnds Assignment 1Rhelina MinNo ratings yet
- Group 5 - Laboratory ReportDocument4 pagesGroup 5 - Laboratory ReportRhelina MinNo ratings yet
- Script For Head To NeckDocument7 pagesScript For Head To NeckRhelina MinNo ratings yet
- ABDOMENDocument3 pagesABDOMENRhelina MinNo ratings yet
- Nursing Theory FoundationsDocument67 pagesNursing Theory FoundationsRhelina MinNo ratings yet
- Proposal of Virtual Group Games 2Document1 pageProposal of Virtual Group Games 2Rhelina MinNo ratings yet
- CH 21 27 ANSWER KEYDocument3 pagesCH 21 27 ANSWER KEYRhelina MinNo ratings yet
- Retdem ScriptDocument1 pageRetdem ScriptRhelina MinNo ratings yet
- Importance of Education in HealthcareDocument2 pagesImportance of Education in HealthcareRhelina MinNo ratings yet
- Biodiversity and The Healthy SocietyDocument2 pagesBiodiversity and The Healthy SocietyRhelina MinNo ratings yet
- Learning Kit 1: Effective Reading Strategies to Improve ComprehensionDocument4 pagesLearning Kit 1: Effective Reading Strategies to Improve ComprehensionRhelina MinNo ratings yet
- ASSESSMENTDocument2 pagesASSESSMENTRhelina MinNo ratings yet
- Critique PaperDocument2 pagesCritique PaperMarie ThereseNo ratings yet
- Semi-Detailed Lesson Plan in T.L.E FoodsDocument3 pagesSemi-Detailed Lesson Plan in T.L.E Foodsgracelyn riveraNo ratings yet
- Megaloblastic AnemiasDocument15 pagesMegaloblastic AnemiasimnnayakNo ratings yet
- Learning Activity SheetDocument2 pagesLearning Activity Sheetsenbonzakura019No ratings yet
- Approach To Child With Headache: Dr. Vijaya Kumar Chikanbanjar 2nd Year Resident Department of PediatricsDocument49 pagesApproach To Child With Headache: Dr. Vijaya Kumar Chikanbanjar 2nd Year Resident Department of Pediatricsar bindraNo ratings yet
- Safety and Influence of A Novel Powder Form of Coconut Inflorescence Sap On Glycemic Index and LipidDocument1 pageSafety and Influence of A Novel Powder Form of Coconut Inflorescence Sap On Glycemic Index and LipidPriscila CerqueiraNo ratings yet
- Ebook Conflict and Communication 1St Edition Jandt Test Bank Full Chapter PDFDocument27 pagesEbook Conflict and Communication 1St Edition Jandt Test Bank Full Chapter PDFgladysvanx3z100% (9)
- Bilateral Congenitally Missing Second Premolars in A Growing Female PatientDocument5 pagesBilateral Congenitally Missing Second Premolars in A Growing Female PatientIJAR JOURNALNo ratings yet
- Effects of A Capacitive-Resistive Electric Transfer Therapy OnDocument8 pagesEffects of A Capacitive-Resistive Electric Transfer Therapy OnAnna Lygia LunardiNo ratings yet
- List of Allianz Efu Network (Panel) Hospitals: Hospital Name Address Telephone # KarachiDocument6 pagesList of Allianz Efu Network (Panel) Hospitals: Hospital Name Address Telephone # KarachiFaizan BasitNo ratings yet
- Board and Reviewer Assignments for Convened IRB ReviewDocument5 pagesBoard and Reviewer Assignments for Convened IRB ReviewMuhammad Zaryab KhanNo ratings yet
- HEALTH-CARE SYSTEMS: CULTURAL, SOCIAL AND PROFESSIONAL ASPECTSDocument16 pagesHEALTH-CARE SYSTEMS: CULTURAL, SOCIAL AND PROFESSIONAL ASPECTSWasima TabassumNo ratings yet
- Cookery1-SPECIALIZED-FINAL 1Document37 pagesCookery1-SPECIALIZED-FINAL 1Princess Aira Malveda100% (1)
- The Tamil Nadu Dr. M.G.R. Medical University, CHENNAI - 600 032Document18 pagesThe Tamil Nadu Dr. M.G.R. Medical University, CHENNAI - 600 032ArtemisNo ratings yet
- (24513105 - BANTAO Journal) Oral and Salivary Changes in Patients With Chronic Kidney DiseaseDocument6 pages(24513105 - BANTAO Journal) Oral and Salivary Changes in Patients With Chronic Kidney DiseaseVera Radojkova NikolovskaNo ratings yet
- Time Magazine USA - December 22 2023Document98 pagesTime Magazine USA - December 22 2023paccs2006No ratings yet
- Observing Gender SensitivityDocument54 pagesObserving Gender SensitivityOrlando NajeraNo ratings yet
- Csec English SbaDocument16 pagesCsec English Sbamartenio martin65% (31)
- Filipino Help Seeking For Mental Health Problems and Associated Barriers and Facilitators: A Systematic ReviewDocument17 pagesFilipino Help Seeking For Mental Health Problems and Associated Barriers and Facilitators: A Systematic ReviewYuvenn YV Cajilig CanutoNo ratings yet
- November 2022 Philippine Nurse Licensure Examination ResultsDocument6 pagesNovember 2022 Philippine Nurse Licensure Examination ResultsRappler0% (1)
- Vale FormDocument1 pageVale FormRANDY BAOGBOGNo ratings yet
- Sylvia PlathDocument12 pagesSylvia Plathapi-534201968No ratings yet
- The Movie "PK" AnalysisDocument2 pagesThe Movie "PK" AnalysisKerstmis “Scale” NataliaNo ratings yet
- JVSM 2325 4645 05 0032Document9 pagesJVSM 2325 4645 05 0032Yayew MaruNo ratings yet
- Employees' Financial Literacy, Behavior, Stress and WellnessDocument12 pagesEmployees' Financial Literacy, Behavior, Stress and WellnessYong Leigh LocusamNo ratings yet
- Feasibility Study 1Document69 pagesFeasibility Study 1Andre Christian Ang100% (2)
- The History of The Treatment of Maxillo-Facial TraumaDocument21 pagesThe History of The Treatment of Maxillo-Facial TraumaThanh NguyễnNo ratings yet
- NCP For PoisoningDocument2 pagesNCP For PoisoningLorie Yvonne Quibin Agullana100% (1)
- Reducing Negativity in A WorkplaceDocument12 pagesReducing Negativity in A WorkplaceAna Jane Morales CasaclangNo ratings yet
- Vijaya Diagnostic HIV Test ReportDocument1 pageVijaya Diagnostic HIV Test Reportpasham bharat simha reddy100% (1)