Professional Documents
Culture Documents
Acute Fia
Uploaded by
Andrei MurariuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Fia
Uploaded by
Andrei MurariuCopyright:
Available Formats
Emergency Department WXH
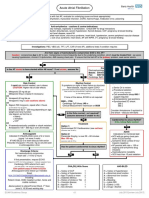
Acute Atrial Fibrillation
For all patients with fast AF, evaluate for underlying cause and treat appropriately:
Infection, hyperthyroidism, dehydration, myocardial infarction, COPD, haemorrhage, medication error, poisoning
Anti-arrhythmics – cautions & contra-indications:
All may be negatively inotropic, especially in combination. Check BNF for drug interactions
Amiodarone: Sino-atrial block and conduction disturbances, severe hypotension, thyroid disease, CCF, pregnancy & breast-feeding.
Flecainide: Atrial flutter, CCF, structural heart disease, recent MI
B-blockers: asthma / COPD, uncontrolled heart failure, sick sinus syndrome, heart block, hypotension, severe peripheral vascular disease
Ca channel blockers: heart failure, hypotension, sick sinus syndrome, heart block, AF with WPW, VT, pregnancy & breast-feeding
Digoxin: heart block, WPW, VT
Investigations: FBC, VBG (all), TFT, LFT, CXR (if new AF), additional tests if condition requires
Are there signs of haemodynamic compromise DUE to the AF?
Caution: compromise due to AF is rare. Compromise is more frequently due to the underlying condition, which must be treated first: eg sepsis
causing hypotension, chronic LV dysfunction, AMI causing chest pain. If unsure that the fast AF is the primary problem, seek senior advice
No Yes
Contacts
Is the AF known to have started within 48 hours? If not certain, assume No
Electrophysiology SpR at Barts (24/7):
Mobile: 07810 878 450
Fax: 0207 600 3069
No Yes Cardiology SpR: bleep 417 (in hours)
Rate Control Rhythm Control Synchronised DC Cardioversion
If rapid rate control needed, use iv doses If symptoms or signs of heart failure or structural
CAUTION: Higher risk of side-effects heart disease, request urgent ECHO Senior Dr to review
(CAUTION: dilated cardiomyopathy may have few clinical signs. Procedural sedation
1. Metoprolol 25 mg tds po Rate control may be preferred if significant co-morbidities
(RSI not usually required)
Metoprolol 5mg iv (repeat if necessary) or frail elderly patient)
Call anaesthetist bleep 095 if
OR If none of the above, ECHO is not required
support required
2. Verapamil 40 mg tds po Anteroposterior pad positions
Verapamil 5 mg iv (see cautions above) 0900 – 1700:
Synchronised DC shock:
OR Cardiology SpR bleep 417 or
200 J
3. Digoxin 500 mcg po/iv, repeat after 4 hours Clinical Measurement Technician on 5101
360 J
(a third dose may be given)
Maintenance 62.5 – 250 mcg depending on age, Consider Amiodarone if resistant to
weight and renal function 2nd shock – discuss with Barts
Use digoxin as first line in: Is the Echo normal / not required?
No
elderly (assume abnormal if unable to do)
immobile Yes Cardioverted to sinus rhythm?
CCF
If No, follow Rate Control
OR Treatment
4. If haemodynamically unstable or shock resistant: Option 1:
Amiodarone 150 – 300 mg iv over 20 minutes Yes
Synchronised DC Cardioversion (see red box)
(success rate 70-90%)
Admit
Anticoagulate Option 2: Indications for monitored bed:
Indicated if CHA2DS2VASc score of 2 or more Flecainide 2mg/kg iv over 30 – 60 minutes ACS with on-going chest pain
(score 1 or more if male) Max 150 mg (even if ECG normal)
IF HAS-BLED 3 or more discuss with senior (success rate 40-70%) Ischaemic ECG (unless 6 hour
Prescribe clexane 1.5 mg / kg sc od until seen in troponin negative)
anticoagulation clinic AF persists with rate > 130 or
Has the patient cardioverted to sinus rhythm? ongoing anti-arrhythmic drug
infusions
Discharge Criteria:
Haemodynamic instability
No haemodynamic compromise
No Yes GCS less than 15 post sedation
Heart rate < 110 for 2 hours
If first presentation, request ECHO
(Use cardiology ix referral form and fax to 5952)
Refer to Rapid access heart rhythm clinic CHA2DS2VASc Score HAS-BLED
(fax form with ECGs – AF and post cardioversion)
C = history of CCF 1 H = history of hypertension 1
Give patient copy of letter & ECGs H = history of hypertension 1 A = Abnormal renal function 1
A = Age 75 years or more 2 A = Abnormal liver function 1
Anticoagulant Clinic follow-up if needed: D = Diabetes Mellitus 1 S = Stroke 1
Fax anticoagulation form to 020 8535 6452 S = History of stroke or TIA 2 B = Bleeding 1
V = Vascular disease 1 L = Labile INR 1
All referral forms can be found on the ED desk A = Age 65 – 74 1 E = Elderly (> 65) 1
top in the forms and letters folder S = Sex (female) 1 D = Drugs / Alcohol 1
ECAM Guidelines Group v2 November 2014 [review November 2017]
Emergency Department
Acute Atrial Fibrillation
Lead Author
Consultant Emergency Medicine
Co-Authors / Collaborators
Consultant Cardiologists
Anticoagulation Nurses
Reference Documents
Management of Atrial Fibrillation, NICE CG180, June 2014
British National Formulary
ECAM Guidelines Group v2 November 2014 [review November 2017]
You might also like
- Acute Fia2Document2 pagesAcute Fia2Andrei MurariuNo ratings yet
- Algorithm 1: Initial Evaluation and Management: Symptoms of Possible ACSDocument6 pagesAlgorithm 1: Initial Evaluation and Management: Symptoms of Possible ACSNenyNo ratings yet
- Prescribing in Chest PainDocument4 pagesPrescribing in Chest PainYY_1992No ratings yet
- Section 2artfibDocument2 pagesSection 2artfibIain Tarrant-MurphyNo ratings yet
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingFrom EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo ratings yet
- ACS Algorithm 2016 PDFDocument1 pageACS Algorithm 2016 PDFrabin1994No ratings yet
- Fast Facts: Optimización del tratamiento de las fluctuaciones motoras en la enfermedad de Parkinson: Adaptando el tratamiento al pacienteFrom EverandFast Facts: Optimización del tratamiento de las fluctuaciones motoras en la enfermedad de Parkinson: Adaptando el tratamiento al pacienteNo ratings yet
- ACLS Simplify AlgorithmDocument6 pagesACLS Simplify AlgorithmKristine Monforte Coma UritaNo ratings yet
- Primary Care Guidelines VertigoDocument1 pagePrimary Care Guidelines VertigoSyahidatul Kautsar NajibNo ratings yet
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesFrom EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesRating: 4 out of 5 stars4/5 (1)
- Uro Gyn NotesDocument13 pagesUro Gyn NotesSheema ShNo ratings yet
- Clinical Guideline: Fibrinolytic Checklist Fibrinolytic ChecklistDocument4 pagesClinical Guideline: Fibrinolytic Checklist Fibrinolytic ChecklistRoi LevinzonNo ratings yet
- FlashcardsforStep2Part2 PDFDocument12 pagesFlashcardsforStep2Part2 PDFLoyla RoseNo ratings yet
- Graded Concept Map 2Document1 pageGraded Concept Map 2api-727701816No ratings yet
- ENT Vertigo FINAL v0.41Document1 pageENT Vertigo FINAL v0.41Farmasi BhamadaNo ratings yet
- Acute Medicine: Shock: Inadequate Tissue and Organ PerfusionDocument3 pagesAcute Medicine: Shock: Inadequate Tissue and Organ Perfusionmyat252No ratings yet
- Cardio ACLS PDFDocument9 pagesCardio ACLS PDFfrankies fpNo ratings yet
- Periarestne AritmijeDocument10 pagesPeriarestne AritmijeMustafa ŠabićNo ratings yet
- DS Male SurgicalDocument6 pagesDS Male SurgicalErryl Justine AdvinculaNo ratings yet
- Drug Study 3Document5 pagesDrug Study 3jasper pachingelNo ratings yet
- 26) Approach To Pediatric ArrhythmiasDocument44 pages26) Approach To Pediatric ArrhythmiasJude AlyousefNo ratings yet
- TachycardiaDocument7 pagesTachycardiaArvind SahniNo ratings yet
- ACLS ChartDocument1 pageACLS ChartJev DespiNo ratings yet
- Pediatric Bradycardia With A Pulse and Poor Perfusion AlgorithmDocument1 pagePediatric Bradycardia With A Pulse and Poor Perfusion AlgorithmRadhiatul MardhiahNo ratings yet
- Handbook of AnesthesiologyDocument176 pagesHandbook of AnesthesiologyarmelzahfauziNo ratings yet
- Advanced Cardiac Life SupportDocument37 pagesAdvanced Cardiac Life SupportRoy Acosta GumbanNo ratings yet
- On Call ComplaintsDocument3 pagesOn Call ComplaintsrashaNo ratings yet
- AlgorithmACLS Tachycardia 200612Document1 pageAlgorithmACLS Tachycardia 200612YassarNo ratings yet
- ACLS-Pediatric Wide Complex Tachycardia: Sample Medical GuidelinesDocument2 pagesACLS-Pediatric Wide Complex Tachycardia: Sample Medical GuidelinesFebrialitaFatoniNo ratings yet
- Algoritma Ambulance - PHCDocument11 pagesAlgoritma Ambulance - PHCYassarNo ratings yet
- Acute Coronary Syndromes - HandoutDocument4 pagesAcute Coronary Syndromes - Handoutapi-641524095No ratings yet
- Agitated PatientDocument2 pagesAgitated PatientCassandra GeldenhuysNo ratings yet
- Dvanced Cardiac Life SupportDocument72 pagesDvanced Cardiac Life Supportolivia100% (1)
- Atrial Fibrillation - Student ResidencyDocument6 pagesAtrial Fibrillation - Student Residencyapi-404356063No ratings yet
- ICSI Stroke June2019 v2Document55 pagesICSI Stroke June2019 v2PerwiraNo ratings yet
- Arrhythmias: Clinical DiagnosisDocument4 pagesArrhythmias: Clinical DiagnosispaveethrahNo ratings yet
- Drug Study (Epinephrine, Lidocaine, Diazepam)Document6 pagesDrug Study (Epinephrine, Lidocaine, Diazepam)Abigaile Operiano100% (2)
- PY365 - Atrial FibrillationDocument60 pagesPY365 - Atrial FibrillationAli KamaliNo ratings yet
- Management of Acute Coronary Syndrome / NSTEMI: Purpose of The GuidelineDocument7 pagesManagement of Acute Coronary Syndrome / NSTEMI: Purpose of The GuidelineSahera Nurhidayah NasutionNo ratings yet
- Atrial Fibrillation TDDocument6 pagesAtrial Fibrillation TDapi-594366475No ratings yet
- Estatus EpilépticoDocument16 pagesEstatus EpilépticoLizbeth PalomecNo ratings yet
- CARDIOLOGY Notes by MeDocument33 pagesCARDIOLOGY Notes by MeJanie-Vi GorospeNo ratings yet
- ACLS 2020 Algorithms: American Heart Association 2020 GuidelinesDocument8 pagesACLS 2020 Algorithms: American Heart Association 2020 GuidelinesNofi Nurina100% (4)
- Shock: Shout For Help/Activate Emergency ResponseDocument6 pagesShock: Shout For Help/Activate Emergency ResponseandiyanimalikNo ratings yet
- Oral Surgery Prelim NotesDocument6 pagesOral Surgery Prelim Notesabsjob1No ratings yet
- Reanimacion CardiopulmonarDocument15 pagesReanimacion CardiopulmonarVictoriano ValienteNo ratings yet
- Advanced Cardiac Life SupportDocument8 pagesAdvanced Cardiac Life Supportcool kipsNo ratings yet
- CVS1 - K25 - Cardiac EmergencyDocument34 pagesCVS1 - K25 - Cardiac EmergencyAdmin neuro-usu.idNo ratings yet
- 7698alorithm SeizureDocument3 pages7698alorithm Seizureboromeus abyasa daniswara100% (1)
- Common Emergency Drugs 2019Document6 pagesCommon Emergency Drugs 2019Sohair Areez MuhammadNo ratings yet
- Acute Coronary Syndrome: History and Clinical Assessment Suggest ACSDocument12 pagesAcute Coronary Syndrome: History and Clinical Assessment Suggest ACSginongNo ratings yet
- Acls Pharmacology OverviewDocument11 pagesAcls Pharmacology OverviewzoyaligNo ratings yet
- Algo Bradycardia DikonversiDocument5 pagesAlgo Bradycardia DikonversiDaniel SitungkirNo ratings yet
- Ventricular Fibrillation/ Pulseless Ventricular Tachycardia AlgorithmDocument2 pagesVentricular Fibrillation/ Pulseless Ventricular Tachycardia AlgorithmsafasayedNo ratings yet
- Pulseless Ventricular Tachycardia/Ventricular Fibrillation Algorithm (Figure 8-5)Document1 pagePulseless Ventricular Tachycardia/Ventricular Fibrillation Algorithm (Figure 8-5)Dyan IslamiNo ratings yet
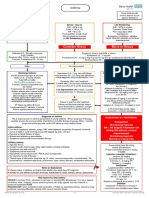
- AsthmaDocument2 pagesAsthmaAndrei MurariuNo ratings yet
- Hypertension: Hypertensive Emergency Hypertensive UrgencyDocument2 pagesHypertension: Hypertensive Emergency Hypertensive UrgencyAndrei MurariuNo ratings yet
- Chest PainDocument5 pagesChest PainAndrei MurariuNo ratings yet
- Physiotherapeutic Management of Patients With Pregnancy-Related Pelvic Girdle PainDocument24 pagesPhysiotherapeutic Management of Patients With Pregnancy-Related Pelvic Girdle PainAndrei MurariuNo ratings yet
- Question Bank For Chapter#6Document11 pagesQuestion Bank For Chapter#6krishnam rajuNo ratings yet
- Properties of Equality PDFDocument1 pageProperties of Equality PDFR. I. P.No ratings yet
- Posttraumatic Stress Disorder (PTSD) and War-Related StressDocument56 pagesPosttraumatic Stress Disorder (PTSD) and War-Related Stresshiggjp3No ratings yet
- Environmental Science 15th Edition Miller Solutions Manual DownloadDocument20 pagesEnvironmental Science 15th Edition Miller Solutions Manual DownloadBrett Bunch100% (20)
- E9sht I C C I W D SDocument213 pagesE9sht I C C I W D SMAMBO95TLNo ratings yet
- Rossmann Repair Training Guide - Google SlidesDocument167 pagesRossmann Repair Training Guide - Google Slidesmirza baigNo ratings yet
- 2022 Specimen Paper 1 Mark Scheme 1Document4 pages2022 Specimen Paper 1 Mark Scheme 1Herman HermanNo ratings yet
- Practice 4Document11 pagesPractice 4Justine Rs Dela TorreNo ratings yet
- Roger Ghanem, David Higdon, Houman Owhadi (Eds.) - Handbook of Uncertainty Quantification-Springer International Publishing (2017)Document2,035 pagesRoger Ghanem, David Higdon, Houman Owhadi (Eds.) - Handbook of Uncertainty Quantification-Springer International Publishing (2017)Jaime Andres Cerda Garrido100% (1)
- Customer - Reprint DhoniDocument1 pageCustomer - Reprint DhoniBaljit SinghNo ratings yet
- SLC Past and Future Hustrulid KvapilDocument26 pagesSLC Past and Future Hustrulid KvapilkinsaeyaNo ratings yet
- Single Nozzle Air-Jet LoomDocument7 pagesSingle Nozzle Air-Jet LoomRakeahkumarDabkeyaNo ratings yet
- List BRG TGL 12Document49 pagesList BRG TGL 12Rizal MuhammarNo ratings yet
- Cess 172Document30 pagesCess 172MaryadiNo ratings yet
- Baby Checklist: Room Furniture Baby Wear Baby BeddingDocument2 pagesBaby Checklist: Room Furniture Baby Wear Baby BeddingLawrence ConananNo ratings yet
- Routes of Medication AdministrationDocument2 pagesRoutes of Medication AdministrationTracy100% (6)
- Weirs: 2. Open Channel Flow 4. Flumes IndexDocument25 pagesWeirs: 2. Open Channel Flow 4. Flumes IndexlordsethdarknessNo ratings yet
- VIC Routing Model PreprocessingDocument11 pagesVIC Routing Model PreprocessingpchrisrlNo ratings yet
- Solution Manual For Laboratory Manual in Physical Geology 11th by American Geological InstituteDocument9 pagesSolution Manual For Laboratory Manual in Physical Geology 11th by American Geological InstituteKarenAcevedotkoi100% (40)
- Scripture Passages Suitable For Lectio Divina: 1 John 4:7-11Document2 pagesScripture Passages Suitable For Lectio Divina: 1 John 4:7-11Victor AugustoNo ratings yet
- Backpacking South America Travel Guide 2020Document59 pagesBackpacking South America Travel Guide 2020sarthak.j6969No ratings yet
- Nanostructural State of AlloysDocument6 pagesNanostructural State of AlloysCristina PostolacheNo ratings yet
- Handling CFGDocument22 pagesHandling CFGRadit BentoNo ratings yet
- Interpretation of Results ReportingDocument7 pagesInterpretation of Results ReportingMerill Harrelson LibanNo ratings yet
- Microbiology QuestionsDocument5 pagesMicrobiology QuestionsNaeem AminNo ratings yet
- Module I: Introduction To Environmental PollutionDocument14 pagesModule I: Introduction To Environmental PollutionAman John TuduNo ratings yet
- Lesson 3.1 Algebraic TermsDocument4 pagesLesson 3.1 Algebraic TermsCresencia Juliana DaluzNo ratings yet
- Grade 11 Learning GuideDocument28 pagesGrade 11 Learning GuideMary-Rose Casuyon100% (1)
- Massage Intake FormDocument2 pagesMassage Intake Formapi-253959832No ratings yet
- Apexification Using Different Approaches - Case Series Report With A Brief Literature ReviewDocument12 pagesApexification Using Different Approaches - Case Series Report With A Brief Literature ReviewIJAR JOURNALNo ratings yet