Professional Documents
Culture Documents
Screenshot 2023-03-08 at 4.19.00 PM
Uploaded by
RenadCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Screenshot 2023-03-08 at 4.19.00 PM
Uploaded by
RenadCopyright:
Available Formats
COPD
Chronic Obstructive
Pulmonary Disease (COPD)
In module IGCP
You are working in a GP surgery. Your next
patient is Mrs Irene Smith, who is 65 years
old. You note that she has a past medical
history of hypertension for which she takes
Ramipril, but apart from that she is an
infrequent visitor to the surgery. You note
that she had a DVT diagnosed after the birth
of her second child but has not had any
problems with blood clots since then.
COPD – Themed Case Introduction
In case Chronic Obstructive Pulmonary
Disease (COPD)
Introduction
Video Player
http://www.taibahumbbs.com/wp-
content/uploads/2016/11/copd-
introduction_hd.mp4?_=1
00:00
02:31
Case introduction
You are working in a GP surgery. Your next
patient is Mrs Irene Smith, who is 65 years
old. You note that she has a past medical
history of hypertension for which she takes
Ramipril, but apart from that she is an
infrequent visitor to the surgery. You note
that she had a DVT diagnosed after the birth
of her second child but has not had any
problems with blood clots since then.
Video Player
http://www.taibahumbbs.com/wp-
content/uploads/2016/11/copd1_hd.mp4?
_=2
What are your initial thoughts about
Irene’s problems based on the
information so far? What other questions
would you like to ask Irene at this point
that might help you make a differential
diagnosis?
Irene is describing shortness of breath on
exertion. The differential diagnosis of
shortness of breath is huge, but Irene also
mentions symptoms in keeping with a chest
infection. This might prompt us to think that
she may be developing a problem with her
respiratory system.
We might therefore want to keep the
following diagnoses in mind as we ask Irene
some more questions:
· asthma, COPD
· Pulmonary embolism (given previous
history of DVT)
· Reaction to Ramipril
· Lung fibrosis
· Angina
· Restrictive lung disease, pulmonary
fibrosis
Remind yourself of which history taking
questions in a respiratory and cardiac
history will help differentiate the possible
diagnoses.
Why is it relevant to ask about Irene’s
smoking? How do you take a smoking
history?
Irene may well have a smoking-related lung
disease, therefore it is very important to take
a smoking history. Taking a detailed smoking
history entails finding out the following
information.
Are they a current smoker?
What age did they start smoking?
Do they smoke cigarettes or roll-ups?
How many cigarettes a day do they smoke?
(if they smoke roll-ups, how much tobacco is
used in a week?- half an ounce of tobacco is
around 20 cigarettes)
Have they ever smoked more or less than
they do now?
Any breaks from smoking?
Have they ever tried to give up?
Does anyone else in the house smoke i.e are
they a passive smoker?
What is a “pack year”?
A “pack year” is a way of quantifying an
individuals’ exposure to tobacco over time.
It is calculated by multiplying the number of
packs of cigarettes smoked per day by the
number of years smoked. For example, a
person who smokes 20 cigarettes per day (ie
one pack) for 10 years will have a 10 pack-
year smoking history.
A person who has smoked 40 cigarettes per
day (cpd) for 30 years will have a 60 pack-
year history.
What is Irene’s pack year smoking history?
What is Irene’s pack year smoking
history?
Irene has smoked 20 cpd from the ages of 15
to 60, and then 10 cpd from 60-65.
Therefore her pack year history will be 45 X 1
+ 0.5 X 5 = 47.5 pack years
What is your differential diagnosis?
At this stage, the differential diagnosis could
be chronic obstructive airways disease,
asthma, or extrinsic allergic alveolitis
(although the history does not reveal any
triggers for this, so makes it less likely). Heart
failure can cause wheeze, but she does not
give any symptoms of this in the history.
What investigations would you like to
request?
The most useful investigation at this point
would be lung function tests, but other
investigations should be considered such as
a chest x-ray and ECG.
Could you give any treatment at this
stage? PLEASE PAY ATTENTION TO
ETR -PLATFORM
Inhalers to treat a tight chest and wheeze
could be started, to provide Irene with some
symptomatic relief whilst we awaiting further
investigations.
You examine Irene
You find that her chest is slightly hyper
inflated, and she has a polyphonic expiratory
wheeze.
There is no clubbing and you can’t find any
enlarged lymph nodes.
Her heart sounds are normal and she
doesn’t have any pedal oedema.
After listening to Irene’s case, what is
your differential diagnosis?
The top differential diagnosis here is COPD,
but late onset asthma may also be a
possibility.
What are the indications for each of the
tests? What will they help show or
exclude?
A chest Xray will show any signs of infection
or pulmonary oedema. Lung function tests
will help determine whether Irene has an
obstructive or restrictive lung disease, and
whether there is any reversibility. An ECG
could demonstrate any evidence of
ischaemic heart disease, arrhythmia or signs
of right sided heart strain secondary to an
underlying lung condition.
What are the psychosocial issues
affecting Irene?
Irene has more than likely developed a chronic lung condition,
which is going to impact upon her everyday life. She will need to
make some changes to her lifestyle including stopping smoking,
which can be a very difficult habit to break. Her husband still
smokes which may cause more difficulty for Irene or potential
tension in the household. Her decline in lung function may be
permanent, restricting her current lifestyle. This may lead to
depression, and Irene’s GP should be vigilant for this.
COPD – Background Science
In case Chronic Obstructive Pulmonary
Disease (COPD)
There is a strong suspicion that Irene is
suffering from Chronic Obstructive
Pulmonary Disease. This is a disease almost
entirely caused by smoking. The hallmark
symptoms of COPD are:
· Shortness of breath
· Chronic cough
· Sputum production
Please watch the following video by
Professor Woodhead which gives an
excellent overview of the epidemiology,
pathophysiology, treatment and natural
progression of this disease.
Video Player
00:00
00:00
Spirometry
One of the tests used in diagnosing COPD is
spirometry. Spirometry machines measure
the volume and flow rate of inspiration and
expiration, and can therefore be used to
diagnose obstructive and restrictive lung
diseases. Modern Spirometers are portable
and available in nearly all GP practices. NICE
guidelines recommend that all patients
suspected of having COPD undergo
spirometry. It is therefore important that all
clinicians are able to interpret spirometry
results and graphs. Please look at the links
below, which explains spirometry in more
detail. It is important to have a clear
understanding of the definitions of FVC, FEV1
and FEV1/FVC
Pulmonary Function Tests – Spirometer
Video Player
00:00
00:00
Disease severity
The GOLD (Global Initiative for Chronic
Obstructive Lung disease) criteria are used
to classify the severity of COPD, according to
the degree of airflow limitation. Familiarise
yourself with the table below.
Treatment
There are pharmacological treatments
available for the management of COPD,
however the single most important
intervention is to stop smoking.
An overview of each of the pharmacological
treatments available is shown in the video
lecture below by Dr Cathy Armstrong. Please
note that this lecture also covers treatment
for asthma.
Video Player
00:00
00:00
Inhaler therapy forms an important part of
the treatment of stable COPD. Familiarise
yourself with the “Algorithm 2a: Use of
Inhaled therapies” table on page 56 of the
NICE guidelines.
What treatments are used for asthma,
COPD or both?
B2 agonists, Ipratroprium, inhaled
corticosteroids and tablet corticosteroids are
used for both asthma and COPD. In practice,
theophylline is not as commonly used for
asthma as it is for COPD, but can be
indicated in difficult cases. Magnesium
typically is used for treating an acute
exacerbation of asthma, but is also used in
an acute exacerbation of COPD.
Leukotriene receptor antagonists are only
used in asthma, whereas carbocisteine is
only used to aid sputum production in
COPD. Sodium cromoglicate is not often
used for asthma.
Can you give some examples of each of
the generic names for:
· ICS
· LABA
· LAMA
· Combination inhaler
· ICS: Clenil, QVAR, pulmicort
· LABA: Serevent
· LAMA: Spiriva
· SAMA: Atrovent
· Combination inhaler: Seretide,
Symbicort, Fostair
COPD and Oxygen
Administration of oxygen to patients with
COPD requires careful consideration. Many
patients with COPD suffer from Type II
respiratory failure and therefore
administration of too much oxygen may be
detrimental. Arterial Blood Gases are used to
determine whether the patient is in Type I or
Type II respiratory failure, and whether it is
compensated or uncompensated.
What is the difference between Type I
respiratory failure and Type II respiratory
failure?
Type I respiratory failure is also known as
hypoxaemic failure, and is defined by a PaO2
of less than 8kPa. It indicates a serious
underlying pathology with the lungs such as
infection, oedema or a shunt.
Type II respiratory failure is also known as
ventilatory failure, results when PaCO2 is
more than 7. Reduced ventilatory effort can
be a result of gas trapping, such as in COPD
and severe asthma, due to chest wall
deformities, muscle weakness or central
causes of respiratory depression.
What is the pathological process that
leads to Type II respiratory failure in
COPD? What physiological compensatory
mechanisms occur in the body to reduce
the level of acidaemia?
In COPD the elastic recoil of the lungs is lost.
This causes gas trapping and reduced
excretion of carbon dioxide. In the blood, the
carbon dioxide combines with water to form
carbonic acid. In an acute setting, the
increased acid levels in the blood would
lower the pH levels and the patient would
become unwell very quickly. However when
carbon dioxide retention is progressive, as if
often the case in chronic COPD, the body can
compensate for this by utilising the
bicarbonate buffer system of the blood. The
kidneys are stimulated to reabsorb more
bicarbonate, which acts as a base and
neutralises the carbonic acid, thus restoring
the pH back to the normal range.
What are the clinical features of
hypercapnia?
· Dilated pupils
· Bounding pulse
· Hand flap
You might also like
- COPD Causes, Symptoms, Diagnosis, Treatment & PreventionDocument1 pageCOPD Causes, Symptoms, Diagnosis, Treatment & Preventiondonnabarro02No ratings yet
- D5W (Dextrose 5%) ClassDocument4 pagesD5W (Dextrose 5%) ClassHanilyn ArdinaNo ratings yet
- 1406 IAL Biology WBI05 01 Scientific ArticleDocument8 pages1406 IAL Biology WBI05 01 Scientific ArticleMohamed NaaifNo ratings yet
- Asthma Cheat SheetDocument8 pagesAsthma Cheat SheetervinalisdayaniNo ratings yet
- COPD Case Pres2Document29 pagesCOPD Case Pres2Kelly Queenie Andres100% (1)
- Copd Case StudyDocument6 pagesCopd Case StudyChrischia Yvonne GualbertoNo ratings yet
- 70, - H 35 - H 2 - O N, L T: T: E G D - Develop A Self Management PlanDocument11 pages70, - H 35 - H 2 - O N, L T: T: E G D - Develop A Self Management PlanjljoioiuNo ratings yet
- PT Case: Copd Exacerbation: DedicationDocument10 pagesPT Case: Copd Exacerbation: DedicationDianaLopezBorjaNo ratings yet
- COPD Treatment, DiagnoseDocument8 pagesCOPD Treatment, Diagnoseaghamohsin1No ratings yet
- COPD Case StudyDocument3 pagesCOPD Case Studyshazel chiasaokwuNo ratings yet
- LC Yuliati-19340019Document5 pagesLC Yuliati-19340019Tiara PutriNo ratings yet
- What Is Chronic Obstructive Pulmonary Disease?Document10 pagesWhat Is Chronic Obstructive Pulmonary Disease?Charles Dhanniel BawasNo ratings yet
- History and Physical Exam For COPDDocument10 pagesHistory and Physical Exam For COPDCathy GuerreroNo ratings yet
- Resarch Outputs Batch 3Document82 pagesResarch Outputs Batch 3Joemar Pastera PelegrinoNo ratings yet
- Description: Back To TopDocument21 pagesDescription: Back To Toprovergzz88No ratings yet
- Our Lady of Fatima University - ValenzuelaDocument3 pagesOur Lady of Fatima University - ValenzuelaMeriam Estepa MartinezNo ratings yet
- 4 Bronchial AsthmaDocument9 pages4 Bronchial Asthmashanfiza_92No ratings yet
- Chronic Obstructive Pulmonary Disease COPDDocument25 pagesChronic Obstructive Pulmonary Disease COPDKat OrtegaNo ratings yet
- Diseases of The Respiratory and Circulatory SystemDocument18 pagesDiseases of The Respiratory and Circulatory SystemRaiah GuerraNo ratings yet
- Ever Smoked COPDDocument8 pagesEver Smoked COPDSimon WilliamsNo ratings yet
- Chronic Obstructive Pulmonary Disease, MMRC Grade 1: Primary ImpressionDocument5 pagesChronic Obstructive Pulmonary Disease, MMRC Grade 1: Primary ImpressionJayson Joseph AngloNo ratings yet
- Chronic Obsrtructive Pulmonary DiseaseDocument11 pagesChronic Obsrtructive Pulmonary Diseasepreeti sharmaNo ratings yet
- A Study On Chronic Obstructive Pulmonary DiseasesDocument12 pagesA Study On Chronic Obstructive Pulmonary DiseasesHamid RazaNo ratings yet
- Op Op Op OpDocument4 pagesOp Op Op OpVannie MaramotNo ratings yet
- Patient Prep: Follow Guidelines On P. 65 of Clinical PacketDocument4 pagesPatient Prep: Follow Guidelines On P. 65 of Clinical PacketKatherine AmbrosiaNo ratings yet
- A Case Presentation On Chronic Obstructive Disease (COPD)Document18 pagesA Case Presentation On Chronic Obstructive Disease (COPD)Harvey T. Dato-onNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD) : Coronavirus (COVID-19)Document4 pagesChronic Obstructive Pulmonary Disease (COPD) : Coronavirus (COVID-19)Kalet GamayNo ratings yet
- Chronic Bronchitis, Emphysema and COPD ('Smoker's Lung')Document3 pagesChronic Bronchitis, Emphysema and COPD ('Smoker's Lung')Alina AdrianaNo ratings yet
- Medical Case II NEWDocument31 pagesMedical Case II NEWTria MeirissaNo ratings yet
- Protocol 2Document14 pagesProtocol 2Hamid RazaNo ratings yet
- Review of Related LiteratureDocument4 pagesReview of Related LiteratureIvy Yvonne Quinico MalubagNo ratings yet
- 3817 Respiratory PreworkDocument3 pages3817 Respiratory PreworkAhmad BustamiNo ratings yet
- CaseFiles FamilyMed Notes 5Document150 pagesCaseFiles FamilyMed Notes 5vesv86% (7)
- Why We Investigate Asthma PatientsDocument5 pagesWhy We Investigate Asthma PatientsustaztNo ratings yet
- Shortness of Breath Nursing Diagnosis and Nursing Care PlansDocument13 pagesShortness of Breath Nursing Diagnosis and Nursing Care PlansRuffy AbdulazisNo ratings yet
- Family Medicine NotesDocument32 pagesFamily Medicine Noteslalee704100% (8)
- AEBADocument6 pagesAEBAAtirah AaNo ratings yet
- Case Study Asthma Group 2Document17 pagesCase Study Asthma Group 2Kennedy PelicoNo ratings yet
- Elsa Ayu Wulandari (19340004)Document4 pagesElsa Ayu Wulandari (19340004)Tiara PutriNo ratings yet
- Copd - 2 Penting 13Document14 pagesCopd - 2 Penting 13Rahmat MuliaNo ratings yet
- COPDDocument52 pagesCOPDswapnil3250No ratings yet
- Bio Santos Resu CombineDocument8 pagesBio Santos Resu Combinelyka resurreccionNo ratings yet
- COPD - Salmorin & SatairapanDocument13 pagesCOPD - Salmorin & SatairapanMichelle SatairapanNo ratings yet
- 2 - Respiratory Passmedicine Q. Bank PART I 2017Document336 pages2 - Respiratory Passmedicine Q. Bank PART I 2017'محمد علي' محمد لافي100% (1)
- COPD Diet: A Beginner's 3-Week Step-by-Step Guide to Managing COPD Symptoms, With Curated Recipes and a Meal PlanFrom EverandCOPD Diet: A Beginner's 3-Week Step-by-Step Guide to Managing COPD Symptoms, With Curated Recipes and a Meal PlanNo ratings yet
- COPDDocument8 pagesCOPDNader Smadi100% (1)
- COPD CasepresentationDocument10 pagesCOPD CasepresentationSandra KartikaNo ratings yet
- COPDDocument25 pagesCOPDCharles S. Williams RRT, AE-C100% (3)
- Pulmonary DiseasesDocument14 pagesPulmonary DiseasesJari JariNo ratings yet
- Nursing Care of PlanDocument16 pagesNursing Care of PlanDbyNo ratings yet
- Case Presentation On Copd - Shaik NazmaDocument29 pagesCase Presentation On Copd - Shaik NazmaDeepikaNo ratings yet
- Spirometry in PracticeDocument24 pagesSpirometry in Practiceuser_at_scribd100% (1)
- Nama: Nurul Khasanah NPM: 19340011 Prodi: Profesi Bidan, 19 LCDocument4 pagesNama: Nurul Khasanah NPM: 19340011 Prodi: Profesi Bidan, 19 LCTiara PutriNo ratings yet
- COPD NotesDocument38 pagesCOPD NotesKudingLimMingYaoNo ratings yet
- Cop D BrochureDocument44 pagesCop D BrochureheartbcglNo ratings yet
- Case-Based Learning Thoracic Medicine: Chronic Obstructive Pulmonary DiseaseDocument22 pagesCase-Based Learning Thoracic Medicine: Chronic Obstructive Pulmonary DiseaseAnonymous HNTNhspNo ratings yet
- Copd Treatment - Google SearchDocument1 pageCopd Treatment - Google SearchLuca WadeNo ratings yet
- The Essential COPD Diet Cookbook:The Complete Nutrition Guide To Shed Excess Fats, Build Muscle And Unleash Your Body Potential With Meal Plan And Nourishing RecipesFrom EverandThe Essential COPD Diet Cookbook:The Complete Nutrition Guide To Shed Excess Fats, Build Muscle And Unleash Your Body Potential With Meal Plan And Nourishing RecipesNo ratings yet
- Acute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAcute Respiratory Distress Syndrome, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Is It Okay To Drink Alcohol On Steroids - Google SearchDocument1 pageIs It Okay To Drink Alcohol On Steroids - Google SearchEsin SyurmeliNo ratings yet
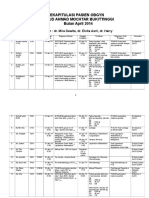
- Rekapitulasi Pasien Obgyn Apr 2014 2Document20 pagesRekapitulasi Pasien Obgyn Apr 2014 2Ressy Dara AmeliaNo ratings yet
- CT and MRI of Abdomen and PelvicDocument1,691 pagesCT and MRI of Abdomen and PelvicĐức Khang NguyễnNo ratings yet
- Reading Test-02 Part - B - CDocument15 pagesReading Test-02 Part - B - Cbinu mathai100% (1)
- MEdication ErrorsDocument6 pagesMEdication ErrorsBeaCeeNo ratings yet
- Marijuana and EpilepsyDocument17 pagesMarijuana and EpilepsyOmar AntabliNo ratings yet
- Immune Response To Infectious DiseaseDocument2 pagesImmune Response To Infectious Diseasekiedd_04100% (1)
- Medoroga& Its ManagementDocument6 pagesMedoroga& Its ManagementChintamani VeerrajuNo ratings yet
- tmpD824 TMPDocument12 pagestmpD824 TMPFrontiersNo ratings yet
- Ginjal Polikistik PDFDocument15 pagesGinjal Polikistik PDFAgunkRestuMaulanaNo ratings yet
- Atrial Fibrillation Topic DiscussionDocument23 pagesAtrial Fibrillation Topic Discussionapi-567600964No ratings yet
- 270 Scientists Call On Spotify To Take Action Over - Dangerous - Misinformation On Joe Rogan Podcast - IFLScienceDocument4 pages270 Scientists Call On Spotify To Take Action Over - Dangerous - Misinformation On Joe Rogan Podcast - IFLScienceDigiti inNo ratings yet
- Animal Care QP U1Document12 pagesAnimal Care QP U1boho14No ratings yet
- Ascites Hrs B WPDocument101 pagesAscites Hrs B WPGhias Un Nabi TayyabNo ratings yet
- PamphletDocument2 pagesPamphletapi-25931970033% (3)
- Endodontic Treatment PlanDocument44 pagesEndodontic Treatment Planlinh nguyễnNo ratings yet
- Diabetesmeds AcceptablecombDocument2 pagesDiabetesmeds AcceptablecombCotton LogicNo ratings yet
- HYPOTHYROIDISMDocument11 pagesHYPOTHYROIDISMVarun SinghNo ratings yet
- Introduction To Anaesthesia: Fatiş Altındaş Department of AnesthesiologyDocument26 pagesIntroduction To Anaesthesia: Fatiş Altındaş Department of AnesthesiologymochkurniawanNo ratings yet
- Benign - Malignant Ovarian TumorsDocument34 pagesBenign - Malignant Ovarian TumorsAhmed AyasrahNo ratings yet
- Media File 4: PathophysiologyDocument1 pageMedia File 4: PathophysiologyhazeeeNo ratings yet
- Elementary Reading Comprehension Test 02 PDFDocument4 pagesElementary Reading Comprehension Test 02 PDFroxanaNo ratings yet
- Feeding Disorders in ChildrenDocument65 pagesFeeding Disorders in Childrendrhananfathy100% (5)
- APAC Comarision of Registration Guidelines 2014 PDFDocument54 pagesAPAC Comarision of Registration Guidelines 2014 PDFAnu PariyarathNo ratings yet
- Determinants of HealthDocument29 pagesDeterminants of HealthMayom Mabuong92% (12)
- ConceptMap AMLDocument1 pageConceptMap AMLnursing concept mapsNo ratings yet
- 01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFDocument26 pages01 - Pharmacotherapy Pearls For Emergency Neurological Life Support PDFawinsyNo ratings yet
- IMA Monthly Report Form JulyDocument4 pagesIMA Monthly Report Form JulyInternetStudioNo ratings yet
- Test Bank For Health Psychology 7th Edition TaylorDocument21 pagesTest Bank For Health Psychology 7th Edition Taylorwoodwardpunction2vq46zNo ratings yet
- Bell 2015Document5 pagesBell 2015Afien MuktiNo ratings yet