Professional Documents
Culture Documents
Chapter 30 - Calcium Homeostatis
Uploaded by
CapuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 30 - Calcium Homeostatis
Uploaded by
CapuCopyright:
Available Formats
Chapter
30
Calcium Homeostasis
R O B I N M. Z AVO D
Drugs Covered in This Chapter*
Selective estrogen receptor • Etidronate disodium Teriparatide
modulators • Ibandronate sodium Monoclonal antibody
• Bazedoxifene acetate • Pamidronate disodium
• Denosumab
• Lasofoxifene • Risedronate sodium
• Tiludronate disodium Inorganic salts
• Raloxifene hydrochloride
• Toremifene citrate • Zoledronic acid • Calcium salts
Calcitonin • Gallium nitrate
Bisphosphonates
• Sodium fluoride
• Alendronate sodium Cinacalcet hydrochloride • Strontium ranelate
• Clodronate tetrasodium
Abbreviations
AF-2, activation factor-2 HMG-CoA, hydroxymethylglutaryl– PTH, parathyroid hormone
ATP, adenosine triphosphate coenzyme A RANKL, receptor activator of nuclear
BMD, bone mineral density IM, intramuscular factor-kB ligand
CaSR, calcium-sensing receptor IV, intravenous RRE, raloxifene responding element
DIOP, drug-induced osteoporosis NaF, sodium fluoride SAR, structure–activity relationship
DNA, deoxyribonucleic acid NHANES III, National Health and SC, subcutaneous
ER, estrogen receptor Nutrition Examination Survey III SERM, selective estrogen receptor
ERE, estrogen responding element 1,25(OH)2D3, modulator
ERT, estrogen replacement therapy 1,25-dihydroxycholecalciferol UGT, uridine diphosphate
FDA, U.S. Food and Drug 25(OH)D3, 25-hydroxycholecalciferol glucuronosyltransferase
Administration PPARg2, peroxisome proliferator-
activated receptor g2
*
Drugs listed include those available inside and outside of the United States; drugs available outside of the United States are shown in italics.
964
Lemke_Chap30.indd 964 12/9/2011 3:59:11 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 965
SCENARIO
Kathryn Neill, PharmD
PJ is a 70-year-old woman with hypertension, gastroesophageal PJ takes alendronate each morning with only a glass of water.
reflux, and osteoporosis. She was prescribed alendronate and After 30 minutes she takes ramipril, omeprazole, and calcium with
calcium 6 months ago, but the resulting improvement in bone coffee. Additional calcium doses are taken with lunch and supper.
density is less than expected. The pharmacist interviews PJ. Her PJ has lost weight the last few months due to an unsettled stomach.
current medications are alendronate 10 mg daily, calcium car-
bonate 500 mg three times daily with meals, omeprazole 20 mg (The reader is directed to the clinical solution and chemical analy-
daily, and ramipril 5 mg daily. sis of this case at the end of the chapter).
INTRODUCTION along the bone surface. Cortical bone is remodeled at
the rate of 3% per year, whereas 25% of trabecular bone,
Three primary hormones—calcitonin, parathyroid hor- which has a considerably higher surface area, is remod-
mone, and vitamin D—control the homeostatic regula- eled annually (3). In terms of calcium turnover in bone,
tion of calcium and its principle counterion, inorganic approximately 500 mg are removed and replaced on a
phosphate. Homeostatic control of these ions is essen- daily basis.
tial not only for the moderation of longitudinal bone Both inorganic and organic components are pres-
growth and bone remodeling but also for blood coagu- ent in the bone. The highly crystalline inorganic com-
lation, neuromuscular excitability, plasma membrane ponent is hydroxyapatite, and the collagen matrix
structure and function, muscle contraction, glycogen comprises the major portion (90%) of the organic
and adenosine triphosphate (ATP) metabolism, neu- component. The collagen matrix serves as the foun-
rotransmitter/hormone secretion, and enzyme catalysis dation for hydroxyapatite mineralization. Osteocalcin
(1). In an average 70-kg adult, approximately 1 kg of cal- and osteonectin are minor organic constituents that
cium is found, 99% of which is located in the bone. The promote binding of hydroxyapatite and calcium to the
principle calcium salt contained in the hydroxyapatite collagen matrix and regulate the rate of bone mineral-
crystalline lattice of teeth and bones is Ca10(PO4)6(OH)2. ization, respectively (5).
Similarly, approximately 500 to 600 g of phosphate are In general, peak bone mass occurs between 30 and
present, 85% of which is found in the bone. The nor- 40 years of age (3,6) and is dependent on genetic factors
mal plasma concentration of calcium is approximately as well as proper intake of calcium, maintenance of qual-
4.5 to 5.7 mEq/L, 50% of which is protein bound. The ity nutrition, and participation in weight-bearing exercise
remainder of the calcium is either complexed to cor- (6). Thereafter, peak bone mass progressively declines at
responding counterions (46%) or exists in its ionized the rate of 0.3% to 0.5% of cortical bone per year (3).
form (4%). It is only the ionized form of calcium that After menopause, bone loss is accelerated (2% per year
is tightly hormonally regulated (varies less than 5% to in the spine) (6) for a period of 5 to 10 years because
10%) (1,2). Because serum calcium concentrations of the loss of estrogen. This can result in up to a 30%
fluctuate, so do the plasma levels of the hormones decrease in bone mineral density.
associated with calcium homeostasis. Serum phospho-
rous levels vary with age, diet, and hormonal status.
The most common form of phosphate in the blood
(pH 7.4) is HPO 2-4 .
HORMONAL REGULATION OF SERUM
The bone is composed of two distinct tissue structures:
CALCIUM LEVELS
cortical (compact) bone and trabecular (cancellous) Arnaud has developed a “butterfly model” that provides
bone (3). Eighty percent of the skeleton is composed a diagrammatic view of the complex interrelationships
of cortical bone (e.g., long bones such as the humerus, among the three hormones (parathyroid, calcito-
radius, and ulna) (4,5), which is a relatively dense tis- nin, and vitamin D) that control calcium homeosta-
sue (80% to 90% calcified) (4) that provides structure sis (serum concentrations of ionic calcium) and their
and support (3). Bone marrow cavities, flat bones, and target organs (bone, kidney, and intestine) (Fig. 30.1)
the ends of long bones are all composed of trabecular (7). The right side (B loops) of the butterfly model
bone, which is considerably more porous (5% to 20% describes the processes that increase the serum calcium
calcified) (4,5). To maintain healthy, well-mineralized concentration in response to hypocalcemia; the left side
bone, a continuous process of bone resorption (loss of (A loops) depicts the events that occur in response to
ionic calcium from bone) and bone formation occurs hypercalcemia.
Lemke_Chap30.indd 965 12/9/2011 3:59:11 AM
966 PART III / PHARMACODYNAMIC AGENTS
CLINICAL SIGNIFICANCE
As our knowledge about the devel- agents and improved the quality of life for countless individu-
opment and risk factors associ- als affected by calcium homeostasis disorders. Understanding
ated with disruptions in calcium the development of individual disease processes involved in
homeostasis has increased, so too have disorders of calcium homeostasis (e.g., osteoporosis, osteo-
the modalities available to prevent and/or petrosis, hyperparathyroidism, and Paget’s disease) and the
treat these disease processes. In general, disorders of calcium pharmacodynamic effects of individual compounds used to
homeostasis involve the development of bone disease and/or treat these disorders is paramount for the practitioner making
alterations in serum calcium concentration. In the most basic therapeutic decisions. Incorporation of these factors into the
sense, the development of bone disease is simply an inequity therapeutic plan is necessary to target the valued pharmaco-
between bone breakdown and bone formation, which also may dynamic effects of these agents while minimizing unwanted
result in an altered serum calcium concentration. In addition or harmful effects. For example, the selection of raloxifene to
to bone disease, disruptions in normal serum calcium concen- treat osteoporosis in a patient with severe gastroesophageal
trations may be related to an imbalance in calcium intake and reflux disease, as opposed to an oral bisphosphonate, which
renal calcium elimination. These disturbances can result from could increase the likelihood of developing erosive esophagi-
various factors, including increased activity of cells that cause tis. Finally, it is also important for the clinician to recognize
bone breakdown, decreased activity of cells that form new bone, the capacity of certain entities used to treat calcium disorders
decreased absorption of calcium, or irregularities in levels of to be allergenic or more prone to produce adverse effects so
hormones that affect calcium absorption and influence cells that selection of the best agent for an individual patient is
involved in bone maintenance. An increased understanding of facilitated.
these physiologic pathways has led to the development of mul-
tiple classes of agents targeting the different mechanisms for Kathryn Neill, PharmD
evolution of these disease processes, including selective estro- Hospital Experiential Director
gen receptor modulators, bisphosphonates, and various calcium Assistant Professor
salts. Critical Care Specialist
Application of the principles of medicinal chemistry has Department of Pharmacy Practice
resulted in the formulation of agents with additional routes of College of Pharmacy
administration, increased potency, and decreased frequency University of Arkansas for Medical Sciences
of dosing. These advances have increased the utility of these Little Rock, Arkansas
Calcitonin and serves to oppose the hormonal effects of parathyroid
hormone. In response to a hypercalcemic state (Fig. 30.1,
S S B loops), increased calcitonin secretion drives serum
Cys Gly Asn Leu Ser Thr Cys Met Leu Gly Thr Tyr Thr Gln calcium concentrations down via stimulation of urinary
Asp excretion of both calcium and phosphate (loop 3B), pre-
Phe vention of calcium resorption from the bone via inhibition
Asn of osteoclast activity (loop 1B), and inhibition of intestinal
H2N O Lys absorption of calcium (loop 2B). When serum calcium
Pro Ala Gly Val Gly Ile Ala Thr Gln Pro Phe Thr His Phe concentrations are low (hypocalcemia), the release of cal-
citonin is slowed, thereby activating loops 1A, 2A, and 3A.
Human calcitonin
Parathyroid Hormone
Human calcitonin is a 32–amino acid peptide (molecular Parathyroid hormone (PTH) is biosynthesized as a 115–
weight, 3,527 daltons) biosynthesized in the parafollicular amino acid preprohormone in the rough endoplasmic
“C” cells found within the thyroid gland. This hormone reticulum of the parathyroid gland and is cleaved to the
contains a critical disulfide bridge between residues 1 and prohormone (90 amino acids) in the cisternal space of
7, with the entire amino acid sequence required for bio- the reticulum (Fig. 30.2). The active hormone is finally
logic activity. The carboxy-terminal residue is a proline produced (84 amino acids; molecular weight, 9,500 dal-
amide. “Procalcitonin,” a precursor peptide, has been tons) in the Golgi complex and is stored in secretory
identified and proposed to facilitate intracellular trans- granules in the parathyroid gland. This gland is exqui-
port and secretion. Calcitonin is secreted in response to sitely sensitive to serum calcium concentrations and is
elevated serum calcium concentrations (>9 mg/100 mL) able to monitor these levels via calcium-sensing receptors
Lemke_Chap30.indd 966 12/9/2011 3:59:11 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 967
FIGURE 30.1 The Arnaud’s butterfly model for regulating calcium homeostasis consists of three overlapping loops that interlock and
relate to one another through the serum concentrations of ionic calcium (SCa), parathyroid hormone (PTH), and calcitonin (CT). The right
side (B loops, where B refers to the effects of CT) of the model describes the physiologic processes that increase the serum calcium con-
centration in response to hypocalcemia; the left side (A loops, where A refers to the effects of PTH) of the model depicts the events that
decrease the serum calcium concentration in response to hypercalcemia. Loop 1 bone resorption; loop 2 intestinal absorption; loop 3 renal
excretion; SPi, serum inorganic phosphate; UPi, urinary inorganic phosphate. (Adapted from Arnaud CD. Calcium homeostasis: regulatory
elements and their integration. Fed Proc 1978;37:2557–2560, with permission).
(CaSR). These cell surface receptors help cells to react calcium (Fig. 30.1, loop 2A), and in combination with
to micromolar changes in the concentration of ionized active vitamin D, promotes bone resorption (Fig. 30.1,
calcium in the serum (8). Binding of calcium to these loop 1A). PTH stimulates bone resorption by several
receptors facilitates activation of phospholipase C and, mechanisms: 1) transformation of osteoprogenitor cells
ultimately, inhibition of PTH secretion. The relatively into osteoclasts is stimulated in the presence of PTH, 2)
short-acting PTH is secreted from the parathyroid gland PTH promotes the deep osteocytes to mobilize calcium
chief cells in response to a hypocalcemic state and serves from perilacunar bone, and 3) surface osteocytes are
to oppose the hormonal effects of calcitonin (1). Unlike stimulated by PTH to increase the flow of calcium out of
calcitonin, the biologic activity of PTH resides solely in the bone. In addition, the secretion of PTH stimulates the
residues 1 to 34 in the amino terminus. biosynthesis, activation, and release of the third hormone
PTH decreases renal excretion of calcium (Fig. 30.1, associated with calcium homeostasis, vitamin D. When
loop 3A), indirectly stimulates intestinal absorption of serum calcium concentrations are high, the release of
PTH is inhibited.
H2N Met Met Ser Ala Lys Asp Met Val Lys Val Vitamin D
Met
Ser Arg Ala Leu Phe Cys Ile Ala Leu Met Val Ile Derived from cholesterol, vitamin D is biosynthesized
Asp from its prohormone cholecalciferol (D3), the product
Gly Lys Ser Val Lys Lys Arg Ser Val Ser Glu Ile Gln of solar ultraviolet irradiation of 7-dehydrocholesterol in
1 2 Leu the skin (2). In 1966, it was first recognized that vitamin
Arg Glu Met Ser Asn Leu His Lys Gly Leu Asn His Met
D must undergo activation via two oxidative metabolic
Val steps (Fig. 30.3). The first oxidation to 25-hydroxycho-
Glu Trp Leu Arg Lys Lys Leu Gln Asp Val His lecalciferol [25(OH)D3: calcifediol; Calderol] occurs in
Asn the endoplasmic reticulum of the liver and is catalyzed by
HO2C Gln Ser Lys Ala Lys [79...35] Phe
vitamin D 25-hydroxylase. This activation step is not regu-
FIGURE 30.2 Preproparathyroid hormone is the 115–amino acid lated by plasma calcium concentrations. The major circu-
protein indicated above. Cleavage at site 1 gives rise to propara- lating form (10 to 80 mg/mL) is 25(OH)D3, which also is
thyroid hormone (89 amino acids), whereas cleavage at site 2 gives the primary storage form of vitamin D (2). In response to
rise to parathyroid hormone (PTH, 84 amino acids). The protein a hypocalcemic state and the secretion of PTH, a second
shown in red is teriparatide (34 amino acids). oxidation step is activated in the mitochondria of the
Lemke_Chap30.indd 967 12/9/2011 3:59:12 AM
968 PART III / PHARMACODYNAMIC AGENTS
H 3C CH3 H 3C CH3 concert with PTH to enhance active intestinal absorption of
CH3 CH3 calcium, to stimulate bone resorption, and to prohibit renal
excretion of calcium (2,9). If serum calcium or 1,25-calcitriol
hv concentrations are elevated, then vitamin D 24-hydroxylase
HO (in renal mitochondria) is activated to oxidize 25(OH)D3
CH2 to inactive 24,25-dihydroxy-cholecalciferol and to further
7-Dehydrocholesterol Cholecalciferol oxidize active vitamin D to the inactive 1,24,25-trihydrox-
HO
ylated derivative. Both the 1,24,25-trihydroxylated and the
24,25-dihydroxylated products have been found to suppress
Liver PTH secretion as well. Several factors have been identified
in the regulation of the biosynthesis of vitamin D, includ-
ing low phosphate concentrations (stimulatory) as well as
H3C CH3 H 3C CH3
OH OH pregnancy and lactation (stimulatory).
CH3 CH3
NORMAL PHYSIOLOGY
Kidney
During growth periods in childhood and early adult-
CH2 CH2 hood, bone formation characteristically exceeds bone
HO HO
loss. In young adulthood, bone formation and bone
OH
resorption are nearly equal. After the age of 40 years,
1,25-Dihydroxycholescalciferol 25-Hydroxycholecalciferol however, bone resorption is slightly greater than bone
formation, and this results in a gradual decline in skel-
FIGURE 30.3 Bioactivation of vitamin D. etal mass. Osteoblasts, osteoclasts, and osteocytes are the
three types of cells that make up the bone remodeling
kidney, catalyzed by vitamin D 1a-hydroxylase (2,9). The unit or bone metabolizing unit and, therefore, are largely
product of this reaction, 1,25-dihydroxycholecalciferol responsible for the bone remodeling process (3,4).
[1,25(OH)2D3: 1,25-calcitriol; Rocaltrol, Calcijex] is the The bone remodeling process is comprised of two
active form of vitamin D. Its concentration in the blood opposing activities, bone resorption and bone forma-
is 1/500 that of its monohydroxylated precursor. The bio- tion. Bone resorption is launched when osteocytes and
synthesis of vitamin D is tightly regulated based on the those cells that line the bone surface release cytokines
serum concentrations of calcium, phosphate, PTH, and and growth factors (Fig. 30.4). These endogenous sub-
active vitamin D (2). stances signal osteoblasts to release receptor activator of
Sterol-specific cytoplasmic receptor proteins (vitamin nuclear factor-kB ligand (RANK-ligand or RANKL), a
D receptor) mediate the biologic action of vitamin D (9). cytokine (10). This ligand interacts with and activates its
The active hormone is transported from the cytoplasm to receptor (RANK) found on 1) the surface of osteoclast
the nucleus via the vitamin D receptor, and as a result of the precursor cells, which stimulates osteoclast differentia-
interaction of the hormone with target genes, a variety of tion, and 2) the surface of mature osteoclasts, which pro-
proteins are produced that stimulate the transport of cal- motes activation (10). RANKL also decreases osteoclast
cium in each of the target tissues. Active vitamin D works in apoptosis.
Cytokines*
RANKL
RANKL Active
Osteoclast
Osteoblast Osteoclasts
precursor cells
Growth factors*
*Involved in
osteoblast Integrin Cathepsin K
maturation Osteoprotegrin
Acidic media
Inhibitory Resorption Bone
Stimulatory (deminerization)
FIGURE 30.4 Bone resorption involving receptor activator of nuclear factor-kB ligand (RANKL).
Lemke_Chap30.indd 968 12/9/2011 3:59:13 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 969
Osteoclasts are the large multinucleated cells of Other methods under development that measure BMD
hemopoietic origin that are responsible for carrying out include ultrasound, traditional x-rays, and blood/urine
the bone resorption or destroying process (6). Cytokines tests (6). Traditional x-rays can identify the site of frac-
(including RANKL), PTH, and the active form of vita- ture, but they cannot measure BMD (3). Blood/urine
min D are responsible for activation of these cells. Bone- tests can identify if the patient is suffering from a medi-
lining flat cells, derived from “retired” osteoclasts and cal condition that is contributing to the loss of BMD and
osteoblasts, are located on the bone surface (3). The can identify important biochemical markers that can
function of these flat cells is thought to serve to iden- assess the rate of bone resorption and bone turnover.
tify areas of the bone that have become weakened or The measurement of serum calcium, phosphorous, and
misshapen and to send a signal to the bone remodel- vitamin D levels also may provide insight regarding the
ing unit to prepare the bone. Lining cells then digest cause of decreased BMD (3). Often, patients suffer from
the outer layer of the bone matrix in preparation for multiple vertebral compression fractures without seek-
bone remodeling. As part of the bone resorption pro- ing treatment other than an over-the-counter analgesic,
cess, the osteoclast membrane comes into contact with and the diagnosis of osteoporosis occurs only after the
the bone surface and, in the presence of integrin, forms patient has already lost significant (as much as 30%)
an impermeable “sealing zone” of approximately 500 to bone mass.
1,000 mm in size (2,6). The ruffled border of the osteo-
clast membrane secretes hydrogen ions, H+ ATPase, and
the cysteine protease cathepsin K (11). As a result, this DISEASE STATES ASSOCIATED WITH
microenvironment becomes acidified, and ultimately, ABNORMAL CALCIUM HOMEOSTASIS
bone demineralization occurs (6). Several types of lyso-
somal enzymes have been proposed to digest the colla- Osteoporosis
gen matrix, thereby pitting the bone surface to a depth Osteoporosis is a skeletal disease that is characterized
of 50 mm (3–6). by loss of bone mass as well as microarchitectural dete-
Osteoblasts, which are of mesenchymal origin and rioration of the bone tissue. This disease is associated
are formed in the bone marrow, stimulate bone forma- with increased bone fragility and susceptibility to frac-
tion (6). In the maturation process, osteoblasts undergo ture. It is a condition that is characterized not by inad-
multiple cell divisions and, in so doing, express the gene equate bone formation but, rather, by a deficiency in the
products that are needed to form the bone matrix or production of well-mineralized bone mass. Whereas no
osteoid, as well as those products responsible for miner- medical cause typically is evident in primary osteopo-
alization of that tissue (3,6). It is in the rough endoplas- rosis (3), secondary osteoporosis classically stems from
mic reticulum that the biosynthesis of the bone matrix medical illness or medication use. There are two types of
protein occurs (4). Multiple endogenous substances are primary adult osteoporosis, type I, or postmenopausal,
involved in osteoblast maturation, including many cyto- and type II, or senile (Table 30.1) (15,16). In type I
kines (interleukins and granulocyte-macrophage colony- osteoporosis, there is an accelerated rate of bone loss
stimulating factor), as well as hormones and growth via enhanced resorption at the onset of menopause. In
factors. this form of the disease, the loss of trabecular bone is
Not only are osteoblasts involved in bone forma- threefold greater than the loss of cortical bone. This
tion, but they also have a role in limiting bone resorp- disproportionate loss of bone mass is the primary cause
tion. Produced by osteoblasts, osteoprotegerin binds to of the vertebral crush fractures and the wrist and ankle
RANKL and therefore prevents its interaction with its fractures experienced by postmenopausal women. In
RANK receptors on the osteoclast (11). As a result, osteo- type II osteoporosis, which is associated with aging, the
clast differentiation and bone resorption are inhibited. degree of bone loss is similar in both trabecular and cor-
Quantification of bone mineral density (BMD) can tical bone and is caused by decreased bone formation by
be measured by noninvasive radiographic tests, such as the osteoblasts (5).
single-photon or dual-photon absorptiometry (spine, Drug- or disease-induced, or type III, osteoporosis
hip, and total body), dual-energy x-ray absorptiometry (Table 30.2) accounts for up to 30% of the cases of
(spine, hip, and total body), peripheral dual-energy vertebral fractures reported annually. It can be caused
x-ray absorptiometry (wrist, heel, and finger), single by a variety of factors, including long-term suppres-
energy x-ray absorptiometry (wrist or heel), quantitative sion of osteoblast function, an inhibition of calcium
computed tomography (spine), peripheral quantitative absorption from the gut, altered vitamin D metabolism,
computed tomography (wrist), and quantitative ultra- or excessive loss of calcium in the urine (17). Disease
sound (heel, shin bone, and knee cap) (3,12–14). Dual- states or pharmacologic therapies that result in estro-
energy x-ray absorptiometry is considered to be the gold gen deficiency, hyperparathyroidism, hyperthyroidism,
standard for measuring bone density and has an accu- or hypogonadism have been correlated with the devel-
racy that exceeds 95% (4). These techniques measure opment of osteoporosis (6,13,17,18). Drug-induced
the attenuation of x-rays or gamma rays as they cross the osteoporosis (DIOP) is associated with the use of glu-
spine, hip, or radius before they reach the detector (6). cocorticoids, thyroid hormone replacement, lithium,
Lemke_Chap30.indd 969 12/9/2011 3:59:13 AM
970 PART III / PHARMACODYNAMIC AGENTS
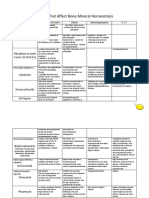
TABLE 30.1 Classification of Osteoporosis (15)
Etiology Type I (postmenopausal) Type II (senile) Type II(secondary)
Increased Osteoclast Decreases Osteoblast Activity and Bone Drug Therapies;
Activity and Bone Resorption Formation; Decreased GI Ca Absorption Disease States
Typical age at diagnosis (years) 50–75 >70 Any age
Gender ratio (women:men) 6:1 2:1 1:1
Typical fracture site Vertebrae, distal radius Femur, neck, hip Vertebrae, hip,
extremities
Bone morphology Decreased trabecular bone Decreased trabecular and normal cortical bone Decreases cortical bone
Rate of bone loss (per year) 2%–3% 0.3%–0.5% Variable
antiepileptic agents, selective serotonin reuptake According to the National Health and Nutrition Exami-
inhibitors, proton pump inhibitors, thiazolidinedio- nation Survey III (NHANES III) the National Osteoporosis
nes, methotrexate, cyclosporine, aromatase inhibitors, Foundation estimates that more than 10 million Americans
gonadotropin-releasing hormone agonists, and immu- have osteoporosis and an additional 33.6 million have
nosuppressive therapy (6,17–21). See Table 30.3 for low BMD of the hip (23). It is projected that by 2020,
a list of the drug-specific mechanisms associated with these numbers will increase to 14 and 47 million, respec-
DIOP (17). tively (24). With these increases, it is anticipated that the
After estrogen deficiency related to menopause, number of hip fractures will double or triple by 2040.
long-term therapy with glucocorticoids represents the Approximately 40% of United States white women and
most prevalent cause of DIOP. As much as 3% to 27% of 13% of United States white men will experience at least
total bone loss can occur within the first 6 to 12 months one fracture related to low BMD in their lifetime. The
of glucocorticoid therapy (17). From a mechanistic chance of a 50-year-old woman experiencing a hip, verte-
perspective, glucocorticoids cause an initial increase in bral, or forearm fracture is 17%, 15%, and 16%, respec-
bone resorption as a result of their ability to increase tively. It is predicted that by age 80, 27% of women will be
RANKL and macrophage colony-stimulating factor. osteopenic and 70% will be osteoporotic. It has been esti-
This results in an increase in osteoclastogenesis and mated that approximately 20% of hip fracture patients
a decrease in osteoclast apoptosis. With the ability of will require long-term nursing home care. A surprising
the glucocorticoids to cause an increase in peroxisome 60% of hip fracture patients do not regain full function,
proliferator-activated receptor g2 (PPARg2) signaling and within 3 to 4 months of hip fracture, as many as 25%
and a decrease in Wnt signaling protein, a decrease in die as a result of secondary complications (e.g., pneumo-
osteoblast formation and function and an increase in nia or infection). Mortality also is increased 17% after
osteoblast apoptosis result, and there is a decrease in both femoral and vertebral fractures. Whereas postmeno-
bone formation (22). pausal African Americans have the lowest rate of osteo-
Vitamin D deficiency, as the cause of pseudohyper- porosis (4%), Native Americans have the highest (12%)
parathyroidism, is a common cause of osteoporosis in with Hispanic and Asian postmenopausal women falling
elder persons who are institutionalized and lack ade- in between (10% for both) (25). Additional risk factors
quate sunlight exposure (2). Many of the older antiepi- associated with osteoporosis are presented in Table 30.4.
leptic agents induce cytochrome P450 24A1 (CYP24A1) Given these statistics, osteoporosis should be considered
enzymes, which catalyze the conversion of vitamin D to a significant health problem that only stands to worsen
inactive metabolites (17). unless appropriate interventions are pursued.
TABLE 30.2 Causes of Secondary (Type III) Osteoporosis
Gastrointestinal diseases Anorexia nervosa, chronic liver disease, malabsorption syndromes
(e.g., celiac disease, Crohn disease, gastric bypass, short bowel disease)
Nutritional excesses or deficiencies Alcoholism, calcium, vitamin D, protein deficiency, excess vitamin A, total parenteral nutrition.
Endocrine-based diseases Acromegaly, diabetes mellitus (types 1 and 2), disease-related elevated hormone levels
(hypercortisolism, hyperthyroidism, hyperparathyroidism), disease-related suppressed hormone levels
Other disease states Chronic obstructive pulmonary disease, hemophilia, myeloma, and some other cancers
Drugs Corticosteroids, aromatase inhibitors, thiazolidinediones, antiepileptic agents
Lemke_Chap30.indd 970 12/9/2011 3:59:13 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 971
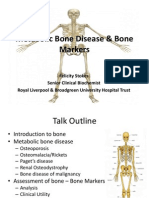
TABLE 30.3 Mechanisms Related to Drug-Induced Osteoporosis
Drug Therapy Proposed Mechanism Leading to Altered Bone Mineral Density (BMD) Citations in Reference 17
Aromatase inhibitors Inhibit conversion of androgens to estrogen 62
Gonadotropin-releasing hormone agonists Antiandrogenic effect on pituitary gland suppressing testosterone 70
(results in hypogonadism)
Thyroid hormone replacement therapy Increase in osteoclast activation and RANKL 81
Antipsychotic agents Stimulation of prolactin secretion lowers estrogen and testosterone levels 99, 100
(results in hypogonadism)
Lithium Hyperparathyroidism 104–106
Thiazolidinediones Decreases osteoblast differentiation and function via PPARg activation 117–119
Loop diuretics Enhances renal calcium excretion 15
Osteopetrosis increase in the production of vitamin D. The left wing of
Osteopetrosis, also known as marble bone disease, describes Arnaud’s butterfly model (Fig. 30.1) is then activated to
a group of heritable disorders that are centered on a increase serum calcium concentrations. In the absence
defect in osteoclast-mediated bone resorption. There are of calcitonin, osteoclast activity is unregulated; therefore,
four autosomal recessive forms and one autosomal domi- bone resorption is accelerated. In acute cases of hypo-
nant form of osteopetrosis (Table 30.5) (26). It generally calcemia, specifically in the case of hypocalcemic tetany,
is characterized by abnormally dense, brittle bone and PTH is administered to correct the hormonal imbalance.
increased skeletal mass. Unlike osteoporosis, this disor-
der results from decreased osteoclast activity, which has Hypercalcemia
an effect on both the shape and structure of the bone. A state of hypercalcemia (Table 30.7) will promote
In very extreme cases, the medullary cavity, which houses calcitonin biosynthesis and release. As a result, PTH
bone marrow, fills with new bone, and production of biosynthesis and its secretion are inhibited, as is the
hematopoietic cells is hampered. Like osteoporosis, this production of vitamin D. The right wings of Arnaud’s
disease can be detected radiographically and appears as butterfly model (Fig. 30.1, B loops) are then activated
though there is a “bone within a bone.” There is limited to decrease serum calcium concentrations. In the pres-
evidence that bisphosphonates can induce osteopetrosis ence of calcitonin, osteoclast activity is inhibited, so bone
via their inhibition of osteoclast activity (27). resorption is slowed. In acute cases of hypercalcemia, cal-
citonin is administered to reestablish calcium homeosta-
Hypocalcemia sis. Hypercalcemia also can be treated with sulfate salts,
Hypocalcemia can be caused by PTH deficiency, vitamin ethylenediaminetetraacetic acid (EDTA), furosemide,
D deficiency, various pharmacologic agents, and miscella- ethacrynic acid, glucocorticoids, and plicamycin.
neous disorders (Table 30.6) (28). A state of hypocalcemia
will inhibit calcitonin release. This results in an elevation Hypoparathyroidism
of PTH biosynthesis and release and indirectly causes an Hypoparathyroidism is caused by decreased serum PTH
concentrations. It is characterized by hypocalcemia,
hyperphosphatemia, and reduced levels of circulating
TABLE 30.4 Lifestyle and Genetic Risk Factors for vitamin D. The right wing of Arnaud’s butterfly model
Osteoporosis predominates (Fig. 30.1), and serum calcium concentra-
Lifestyle Factors Genetic Factors
tions precipitously decrease. Administration of intrave-
nous (IV) calcium gluconate and PTH serves to acutely
Smoking Female correct plasma calcium levels. Chronic oral administra-
Sedentary lifestyle Family history
tion of active vitamin D as well as calcium supplements
has been effective in maintaining appropriate serum cal-
Calcium intake Small frame cium concentrations.
Milk intolerance Early menopause
Pseudohypoparathyroidism
Excessive caffeine
In this disease state, levels of PTH are normal or even
Excessive alcohol elevated; however, serum calcium concentrations are low.
End-organ insensitivity to PTH has been proposed to be
Nulliparity
the cause of the hypocalcemic state. Treatment of this
Lemke_Chap30.indd 971 12/9/2011 3:59:14 AM
972 PART III / PHARMACODYNAMIC AGENTS
TABLE 30.5 Human Osteopetrosis Genotypes
Gene Involved Function of Gene Clinical Symptoms Patients Affected (%)
Autosomal recessive disorders
CAII Carbonic acid and proton production Less severe: may improve with age, short <5
stature, no hematologic failure
TCIRG1 Proton pump Severe: apparent in infancy, visual impairment, ∼60
hypocalcemia, death by 10 years of age
CLCN7 Chloride channel Severe: apparent in infancy, similar to TCIRG1 ∼15
symptoms
Intermediate: apparent in infancy but less
aggressive, osteomyelitis, fractures
Gl/gl Unknown Extremely severe: death within months <5
Autosomal dominant disorder
CLCN7 Chloride channel Frequent fractures, osteomyelitis, some more
severe (like recessive disorders)
condition with calcium and vitamin D has proven to be
successful. H OH H
Hyperparathyroidism
H H
Increased levels of PTH lead to moderately to severely
elevated serum calcium concentrations and, as a result,
a significant loss of calcium from the bone (2). Deposits HO H HO H
of calcium salts in soft tissue, as well as formation of renal H
OH
H
OH
calculi, also can result from this hormonal imbalance.
Treatment of this condition with salmon calcitonin, loop Paricalcitol (Zemplar) Doxercalciferol (Hectorol)
diuretics, or other classical treatments for hypercalcemia
has been favorable. The IV vitamin D analog paricalci- This analog also is indicated for the treatment of
tol, which is used for both prevention and treatment of secondary hyperparathyroidism. Doxercalciferol cap-
hyperparathyroidism secondary to chronic renal failure, sules should be administered three times weekly at the
has been shown to reduce PTH levels by an average of time of dialysis along with close monitoring of calcium
30% after 6 weeks of treatment. Whereas paricalcitol is and phosphate levels. Treatment of secondary hyper-
a fully active form of vitamin D, doxercalciferol requires parathyroidism with vitamin D therapy is problem-
activation by the liver. atic, however, because it often leads to hypercalcemia,
TABLE 30.6 Causes of Hypocalcemia
PTH Deficiency Vitamin D Deficiency Drugs Miscellaneous
Hypoparathyroidism Nutritional deficiency Chemotherapeutic agents Osteoblastic metastases
Pseudohypoparathyroidism Gastrointestinal malabsorption Diuretics Phosphate infusion
Furosemide
Hypomagnesemia Renal Inhibitors of bone resorption Rapid infusion of citrate buffered plasma
Failure or blood or large amounts of albumin
Tubule disorders
Nephrotic syndrome
Hepatobiliary disease
(decreases synthesis)
Pancreatic disease
(malabsorption)
Anticonvulsant therapy
(malabsorption, abnormal
metabolism)
Lemke_Chap30.indd 972 12/9/2011 3:59:14 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 973
TABLE 30.7 Calcium Homeostasis-Related Disorders
Type of Disorder Treatment Examples
Disorders leading to hypercalcemia Fluids, low-calcium diet, sulfate, loop diuretics, Hyperparathyroidism
glucocorticoids, calcitonin, EDTA Hypervitaminosis D
Sarcoidosis
Neoplasia
Hyperthyroidism
Immobilization
Paget disease of the bone
Disorders of bone remodeling Bisphosphonates, calcitonin, estrogen, calcium, Osteoporosis
fluoride, PTH + vitamin D
EDTA, ethylenediaminetetraacetic acid.
hyperphosphatemia, or both because of increased intes- and are present at elevated levels. Patients afflicted with
tinal absorption of both calcium and phosphorous (29). this painful condition often suffer from multiple com-
In patients with chronic renal failure, CaSR agonists are pression fractures. Administration of calcitonin and
able to limit progression of hyperparathyroidism and oral calcium and phosphate supplements had been the
growth of the parathyroid gland. treatment of choice until the bisphosphonate risedro-
nate sodium was approved by the U.S. Food and Drug
Rickets and Osteomalacia Administration (FDA). Daily administration of rise-
During the Industrial Revolution, there was widespread dronate sodium (see later discussion of bisphospho-
incidence of rickets in both children and adults, because nates) results in a decreased rate of bone turnover and
inadequate exposure to sunlight prevented the biosynthe- a decrease in the levels of serum alkaline phosphatase
sis of the precursor to active vitamin D in the skin. Both and urinary hydroxyproline, two biochemical markers
rickets and osteomalacia are metabolic bone diseases that of bone turnover (4,30). A significant advantage to treat-
are characterized by poor bone mineralization. Without ment with the bisphosphonates is long-term suppression
adequate plasma levels of vitamin D and calcium, deposi- of the disease. Calcium supplementation, which often
tion of the calcium salts in the bone markedly decreases. is necessary in these patients, must be dosed separately
Vitamin D supplementation (to improve intestinal absorp- from risedronate sodium, because calcium- and alumi-
tion of calcium and mineralization of the bone) as well as num- or magnesium-containing antacids interfere with
oral calcium supplementation are required to treat these absorption of the bisphosphonates.
diseases once established. The incidence of rickets in
the United States dropped dramatically through vitamin DRUG THERAPIES USED TO TREAT
D–supplemented food programs. The increased use of OSTEOPOROSIS
milk substitutes (e.g., soy) and reduced exposure to sun-
light has recently led to a rise in rickets. Rickets is still Agents used in the treatment and prevention of osteo-
considered to be a worldwide health problem. porosis are categorized as antiresorptive agents or bone-
In addition to the classical environmental or nutri- forming agents depending on the primary mechanism
tional cause of these diseases, both osteomalacia and rick- of action (31). For most of the effective therapies, bone
ets can have a pharmacologic origin as a result of chronic mass is observed to increase for the first few years of treat-
treatment with anticonvulsants (phenobarbital and phe- ment. Eventually, however, all the pits or lacunae will be
nytoin) or glucocorticoids. These agents interfere with filled in with new bone, and no additional increase in
intestinal absorption of calcium and, thereby, cause pseu- bone mass will occur. Antiresorptive agents have been
dohyperparathyroidism. As a result, an increase in bone shown to increase bone mass by as much as 8% to 9%
turnover and a decrease in the formation of appropri- at the lumbar spine and 3% to 6% in the femoral neck.
ately mineralized bone are observed. In these patients, Once a diagnosis of osteoporosis and the likely cause has
treatment with vitamin D improves calcium absorption, been established, it is important to consider both patient
ultimately enhancing mineralization of the bone. fracture history and general medical history when
selecting the appropriate treatment for a given patient
Paget Disease of the Bone (Table 30.8)(32).
Paget disease of the bone (Table 30.7) is characterized
by excessive bone resorption, followed by replacement Antiresorptive Agents
of the normally mineralized bone with soft, poorly min- Estrogen Analogs—Estrogen Replacement Therapy
eralized tissue (30). It has been determined that the MECHANISM OF ACTION The precise mechanism by which
osteoclasts have an abnormal structure, are hyperactive, estrogen prevents bone resorption has not been elucidated;
Lemke_Chap30.indd 973 12/9/2011 3:59:14 AM
974 PART III / PHARMACODYNAMIC AGENTS
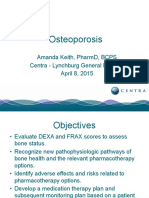
TABLE 30.8 Osteoporosis Treatment Selection Criteria (32)
Patient Data Alendronate Risedronate Raloxifene Calcitonin Teriparatide
PM women: (+) osteoporosis/(+) fracture X X X X X
PM women: (+) osteoporosis/(−) fracture X
Men: (+) osteoporosis X X
Corticosteroid-induced osteoporosis X X
(+) Esophageal or upper GI disorder (−) (−) X X
(+) Vasomotor symptoms X X (−) X
(+) Venous thromboembolic event X X (−) X
(+) Vertebral compression fracture pain X
X, recommended; (−), not recommended; GI, gastrointestinal; PM, postmenopausal.
however, it has been proposed to be associated with inhi- and that which is considered to be standard therapy is
bition of osteoclast activity. Limited evidence supports 0.625 mg/d of conjugated estrogens (Premarin); how-
the presence of estrogen-specific receptors (present on ever, a 0.3 mg/d dose of esterified estrogen (e.g., Menest)
osteoclasts) having a biochemical role in the regula- has been shown to be adequate for the prevention of
tion of bone remodeling (15). Estrogen improves cal- osteoporosis (5). Estrogen replacement therapy (ERT) is
cium absorption, promotes calcitonin biosynthesis, and available in several types of formulations, including trans-
increases the vitamin D receptors on osteoclasts. Although dermal patches (e.g., 17b-estradiol: Climera, Estraderm,
the primary mechanism of action remains unclear and its Menostar, or Vivelle).
use is controversial at best, estrogen replacement therapy Initiated at the onset of menopause, this therapy also
(i.e., 17b-estradiol, estrone sodium sulfate, or 17-ethinyl has favorable effects on serum cholesterol levels (reduces
estradiol) has value in the treatment and prevention of low-density lipoprotein and elevates high-density lipopro-
osteoporosis (31,33–35). tein levels). Women taking ERT have found relief from
hot flashes, vaginal dryness, and urinary stress inconti-
OH O nence (31). It is recommended that the estrogen be
combined with a progestin for those women with an
intact uterus so as to decrease the risk of endometrial
HO HO
cancer (15).
17β-estradiol Estrone
Selective Estrogen Receptor Modulators
OH RALOXIFENE (EVISTA) Tamoxifen citrate, classified chemi-
C CH
cally as a triarylethylene, was developed as an anties-
trogenic agent and as a selective estrogen receptor
HO
modulator (SERM). It is indicated as adjuvant therapy
in the treatment of axillary node–negative or –posi-
17-Ethinyl estradiol tive breast cancer following partial or full mastectomy.
Raloxifene hydrochloride, a benzothiophene derivative,
In light of the findings of the Women’s Health Initiative also may be considered a semirigid analog of tamoxifen
study, the FDA recommends the use of short-term hor- (Fig. 30.5) (36).
mone replacement therapy (estrogen and progestin) in The two drugs are similar in that they both possess
the prevention of osteoporosis only in select cases. The agonist activity in certain tissues (e.g., bone and cardio-
pharmacokinetics of the estrogens are covered in detail vascular) and antagonist activity in others (e.g., breast
in Chapter 41 (33,34). and uterus) (see Chapter 41) (6,31). Raloxifene hydro-
chloride, the first SERM approved for the prevention of
osteoporosis in postmenopausal women, acts as an estro-
THERAPEUTIC EFFECTS Fractures of the spine, wrist, and hips gen agonist on receptors in osteoblasts and osteoclasts
decrease by 50% to 70%, and spinal bone density increases but as an antagonist at breast and uterine estrogen recep-
by 5%, in those women treated with estrogen within 3 tors. This selective action means that this agent does not
years of the onset of menopause and for 5 to 10 years increase the risk of endometrial or breast cancer, as is
thereafter (5,13,36,37). The minimum dose required the case with long-term tamoxifen therapy. Because this
Lemke_Chap30.indd 974 12/9/2011 3:59:14 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 975
HO Pharmacokinetics Raloxifene hydrochloride is rapidly
S absorbed following oral administration, with an estimated
CH3
CI 60% absorption, but it has a very low bioavailability (2%),
OH CH3
H associated with extensive phase II metabolism. The metab-
N O N
O H3C O olites are excreted via the bile, with potential enterohe-
patic recycling that could account for the interaction
Raloxifene hydrochloride (Evista) Tamoxifen (Nolvadex) with cholestyramine. Supportive of the enterohepatic
recycling is the half-life of 28 hours. Metabolism of raloxi-
FIGURE 30.5 Structures of raloxifene and tamoxifen highlighting fene hydrochloride occurs to a great extent in the intes-
the structural similarity between the two drugs.
tine and consists of glucuronide conjugation catalyzed
by uridine diphosphate glucuronosyltransferase (UGT)
(40–42). The UGT1A family is responsible for intestinal
agent does not have a stimulatory effect at its receptors human metabolism, as shown in Figure 30.6. Efflux by
on most tissues, it does not prevent the hot flashes and intestinal cells of the resulting glucuronide occurs via
other symptoms of menopause as estrogen does (5). P-glycoprotein and multidrug resistance–related protein.
The combination of rapid metabolism and efflux can
Therapeutic Action Clinical trials have shown that ral- account for the low bioavailability.
oxifene hydrochloride, in combination with oral calcium
supplementation, decreases the risk of vertebral fracture LASOFOXIFENE (FABLYN) Lasofoxifene is a very potent sec-
and promotes bone formation, albeit to a lesser extent ond-generation SERM in clinical trials in the United
than with estrogen. Raloxifene hydrochloride has been States and approved in the European Union for the
shown to have a beneficial effect on lipid profiles (13). treatment and prevention of osteoporosis in postmeno-
Raloxifene hydrochloride should not be administered pausal women (Fig. 30.7). At low doses, this agent has
in combination with cholestyramine (decreased absorp- been shown to prevent bone loss and decrease serum
tion), warfarin (prothrombin times and international cholesterol (dose range, 0.01 to 20.0 mg/day). In early
normalized ratios must be monitored more closely), clinical trials, lasofoxifene improved BMD in the lum-
and those drugs that are highly protein bound, such bar spine by 3% (after 12 months of therapy), which is
as clofibrate, diazepam, ibuprofen, indomethacin, and twice the improvement observed with similar treatment
naproxen. using raloxifene. Improvement in hip BMD was similar
for both agents. Interestingly, a more pronounced reduc-
Structure–activity Relationship From a structural per- tion in low-density lipoprotein cholesterol was observed
spective, the only pure antiestrogens are 7a-substituted with lasofoxifene treatment than with raloxifene treat-
estrogens (31). In the triarylethylene class of agents (e.g., ment. Despite the fact that phase III clinical trial data
tamoxifen), the A ring phenol is critical for interaction indicate that there is an increase in deaths from stroke
with the portion of the estrogen receptor (ER) pro- and cancer, lasofoxifene was approved by the European
tein referred to as the activation factor-2 (AF-2) region, Commission in March 2009 for the treatment of osteopo-
because it mimics the essential 3-phenol group found rosis fractures in postmenopausal women.
in estrogen (31). This interaction initiates a change in
protein conformation to the form of the receptor able OSPEMIFENE Ospemifene is a SERM in clinical trials for
to interact with a specific deoxyribonucleic acid (DNA) the treatment of postmenopausal osteoporosis and
sequence known as the estrogen responding element
(ERE). As a result, activation of a specific group of genes
occurs, and protein biosynthesis ensues. The orientation
O
of the three aryl rings in a propeller type of arrangement UGT1A8 O N
Raloxifene
also is important for tight receptor binding and biologic
activity (31). In raloxifene hydrochloride, the substi- COOH
tuted benzothiophene ring mimics the estrogen A ring; O S OH
OH
however because of the presence of a semirigid, amine- UGT1A10 H
HO Raloxifene-6-β-glucuronide
containing side chain, raloxifene is unable to inter- OH
act with AF-2 (38,39). As a result, interaction with ERE
is prevented and antiestrogenic action is observed in O
N
reproductive tissues. The raloxifene hydrochloride–ER
complex, in concert with specific adapter proteins, is also O
COOH
OH
able to interact with and activate a raloxifene responding O
OH S
element (RRE). Activation of this DNA sequence facili- H
HO
tates activation of another group of genes responsible for OH Raloxifene-4'-β-glucuronide
the production of proteins that allows for agonist action
in nonreproductive tissues (38,39). FIGURE 30.6 Metabolism of raloxifene.
Lemke_Chap30.indd 975 12/9/2011 3:59:14 AM
976 PART III / PHARMACODYNAMIC AGENTS
fractures, as well as an increase in BMD in the lumbar
N OH
O O spine, hip, and femur. Presently, the drug has not been
approved for treatment of osteoporosis.
Bisphosphonates
MECHANISM OF ACTION The bisphosphonates are synthetic
HO in origin and are designed to mimic pyrophosphate,
Cl where the oxygen in P-O-P is replaced with a carbon
Lasofoxifene Ospemifene atom to create a nonhydrolyzable backbone (Fig. 30.8)
(36,37). Because pyrophosphate is a normal constituent
N
CH3 of bone, these analogs selectively bind to the hydroxy-
O N apatite portion of the bone and can bind to and stabilize
O CH3
calcium phosphate effectively (37,45). The bisphospho-
nates (Fig. 30.9) effectively inhibit osteoclast prolifera-
tion, decrease osteoclast activity, reduce osteoclast life
N
OH
span, and as a result, decrease the number of sites along
HO the bone surface where bone resorption occurs (37).
CH3 Cl This is largely accomplished via inhibition of the meval-
onate pathway within osteoclasts, as well as via inhibition
Bazedoxifene Toremifene
of ATP-dependent enzymes. By these three mechanisms,
FIGURE 30.7 Investigational second-generation selective estrogen the bisphosphonates are able to limit bone turnover and
receptor modulators. allow the osteoblasts to form well-mineralized bone with-
out opposition (3). The precise mechanisms of action of
postmenopausal vaginal atrophy (Fig. 30.7). It is a known these antiresorptive agents have not been elucidated; it is
metabolite of toremifene, a triphenylethylene deriva- equally uncertain whether all the bisphosphonates act by
tive used to treat breast cancer. Ospemifene has been a similar mechanism (37). To date, cell surface receptors
shown to have beneficial effects on the bone without have not been identified, nor has a second messenger
significant estrogen-related side effects. The beneficial system been detected. There is evidence that bisphos-
effect observed on bone stems from this agent’s ability phonates inhibit the mevalonate pathway (specifically
to increase osteoblast proliferation and, as a result, to farnesyl diphosphate synthase) within osteoclasts, as well
enhance bone mineralization as well as bone formation. as inhibit ATP-dependent enzymes (impairing cellular
Unlike tamoxifen, ospemifene does not induce osteocyte energetics), both of which are associated with inhibition
apoptosis (43). Presently the New Drug Application sub- of osteoclast activity.
mitted to the FDA under the trade name of Ophena lists
treatment of postmenopausal vaginal atrophy as the only STRUCTURE–ACTIVITY RELATIONSHIPS From a structural per-
indication. spective, the bisphosphonates have been proposed to have
specific molecular interactions with their biologic target
BAZEDOXIFENE (VIVIANT) Bazedoxifene is an indole-based for drug action, even though precise structure–activity
SERM that is under investigation for the treatment and relationships (SARs) have not been elucidated. In fact,
prevention of postmenopausal osteoporosis (Fig. 30.7). the exact molecular target is still under investigation. The
It also is being evaluated in combination with Premarin central carbon of the geminal phosphonate has been sub-
(conjugated estrogens). Bazedoxifene acetate displaces stituted with a variety of functional groups to yield a large
17b-estradiol from ERs and has excellent binding affin- family of compounds with differing physicochemical and
ity for the receptor itself. Unlike raloxifene hydrochlo- biologic properties (37). The SAR studies (Fig. 30.8)
ride, this agent does not cause hot flashes at the doses have concluded that a hydroxyl substituent (R1) maxi-
required to have a beneficial effect on bone. In addition, mizes the affinity of the agent for the hydroxyapatite as
it does not cause uterine or mammary gland stimulation
(44). Wyeth received approvable letters from the FDA for
the use of bazedoxifene acetate in the prevention and
OO OO
treatment of postmenopausal osteoporosis in 2007 and P
O P
2008, respectively. R1 O
O C
O O
P R2 P
O O
TOREMIFENE Toremifene citrate (Fig. 30.7), a SERM O O
approved for the treatment of breast cancer (Fareston),
is under investigation in patients undergoing androgen- Pyrophosphate Bisphosphonate
R1 = hydroxy
deprivation therapy in the treatment of advanced pros- R2 = varies
tate cancer. Preliminary results from phase III clinical
trials indicate a 50% reduction in the rate of osteoporotic FIGURE 30.8 Bisphosphonate structure–activity relationships.
Lemke_Chap30.indd 976 12/9/2011 3:59:15 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 977
A. Investigational bisphosphonates:
CH3
H PO3H
Cl PO3H N PO3H N PO3H
2 Na 2 Na H2N Na H3C Na
PO3H2
Cl PO3H PO3H HO HO PO3H2
Clodronate Incadronate Neridronate Olpadronate
B. Clinically used bisphosphonates.
H3C PO3H Na PO3H Na PO3H2 PO3H Na
H2N Cl S
HO PO3H
Na HO PO3H2 HO PO3H Na PO3H Na
N
Etidronate disodium Alendronate sodium Risedronate sodium Tiludronate disodium
CH3
H2N PO3H Na PO3H2 H3C (CH2)4 N PO3H2
N N
HO PO3H Na HO PO3H2 HO PO3H Na
Pamidronate disodium Zoledronic acid Ibandronate sodium
FIGURE 30.9 Bisphosphonates, both investigational and clinically used.
well as improves the antiresorptive character of the agent the rapid rate of clearance, the bisphosphonates enjoy
(31,46). The character of the R2 substituent varies widely a short circulating half-life and very limited drug expo-
and clearly has a significant influence on the potency of sure to nontarget tissues (37). Because the bisphospho-
this class of compounds (Fig. 30.9). The R2 amino–sub- nates are only released from the bone when the bone is
stituted bisphosphonates (pamidronate disodium, alen- resorbed, they have a tissue half-life of 1 to 10 years; how-
dronate sodium, and neridronate) are more potent than ever, these agents remain pharmacologically active only
etidronate disodium and clodronate disodium (not avail- while they are exposed on bone resorption surfaces (45).
able in the United States). The R2 3-carbon amino linear
chain for alendronate sodium is more potent than the SPECIFIC DRUGS
R2 2-carbon derivative pamidronate disodium and the Etidronate Disodium (Didronel) and Tiludronate Disodium
R2 6-carbon analog neridronate (31). Alkylation of the (Skelid) Agents in the first generation of bisphos-
amine functional group improves potency as is demon- phonates that were dosed continuously produced
strated by compounds with N substituted amino alkyls poorly mineralized bone, because there was no inter-
at R2 (e.g., olpadronate and ibandronate sodium) and val for appropriate bone mineralization to occur (3).
those that contain rings at R2 (e.g., risedronate sodium, Subsequent studies that used a cyclic dosing schedule
incadronate, tiludronate disodium, and zoledronic acid). (400 mg/d for 2 weeks, followed by 2.5 months of cal-
The third-generation analogs contain a basic heterocyclic cium supplementation only) showed improvement in
side chain at R2 tethered to the central carbon by a variety bone mineralization (13,43). Both of these bisphospho-
of linkages (potency: NH > CH2 > S > O) (31,46). Because nates have been approved for treatment of Paget disease
structural variation of R2 has a significant effect on of the bone but not for the treatment of osteoporosis
potency, it can be surmised that R2 interacts at an “active (5). Tiludronate disodium is approximately 10-fold more
site” and participates in a specific molecular interaction. potent than etidronate disodium and, when given orally
The bisphosphonate itself as well as the hydroxyl group at for 6 months (200, 400, or 800 mg/d), increases BMD by
R1 also should be included as critical SAR features (31). 2% (Fig. 30.9) (6). No further bone loss was detected in
patients 6 months after cessation of therapy.
PHARMACOKINETICS To date, four generations of bisphos-
phonates have been developed for the treatment of Alendronate Sodium (Fosamax) The second-generation
osteoporosis (Fig. 30.9). Absorption of these agents agent alendronate sodium was the first bisphosphonate
from the gut is quite poor (1% to 5%) because of their agent approved by the FDA for the prevention and treat-
polar nature, and as a therapeutic class, they have lim- ment of osteoporosis and Paget disease of the bone and
ited cellular penetration (13). Up to 50% of the actual is 1,000-fold more potent than etidronate disodium
absorbed dose is taken up specifically by the bone within (Fig. 30.9) (45,47). Alendronate sodium is also indicated
4 to 6 hours, and the rest is exclusively excreted by the for the treatment of glucocorticoid-induced osteoporosis.
kidney (6,36). Uptake of these agents in the bone is con- This derivative, when dosed continuously (5 to 10 mg/d for
centrated in areas of the bone that are actively undergo- osteoporosis and 40 mg/d for Paget disease of the bone)
ing remodeling (45). Between the selective uptake and and given with oral calcium supplements (500 mg/d),
Lemke_Chap30.indd 977 12/9/2011 3:59:15 AM
978 PART III / PHARMACODYNAMIC AGENTS
produced well-mineralized bone and significantly improved
BMD (7% in the spine and 4% in the hip) within 18 months ADDITIONAL DOSAGE FORMS
(6). In addition, the vertebral fracture rate was shown to
decrease by 47%. A side effect associated with alendro-
nate sodium, chemical esophagitis, has been attributed to A unique formulation of alendronate sodium, FOSAMAX PLUS
inadequate intake of water and lying down after taking the D, includes 70 mg of alendronate sodium and 2,800 IU or 5,600
medication (2,3,13,36). Specific patient instructions were IU of vitamin D3 (i.e., a 7-day supply of both the bisphospho-
developed to limit the incidence of upper gastrointestinal nate and vitamin D). This formulation should not be used in
problems and include: 1) taking the medication with 6 to patients with severe kidney disease or low serum calcium levels
and should not be the only therapy used to correct a vitamin
8 ounces of water on arising in the morning, 2) remaining
D deficiency.
in an upright position for at least 30 minutes after taking
Risedronate sodium with calcium carbonate (Actonel with
the medication, and 3) delaying drinking other liquids/
Calcium) represents an additional type of packaging for this
eating for at least 30 minutes, if not 1 to 2 hours, to allow class of agents. It addresses the Surgeon General’s Report on
maximal absorption of the agent. To enhance absorption, Bone Health and Osteoporosis, which states that treatments for
calcium supplements and any aluminum- or magnesium- osteoporosis need to be made simpler and more structured.
containing antacids should be dosed separately from agents Sold in units that contain a 1-month supply, each week of ther-
in this class. These agents are not recommended in patients apy includes a total of seven tablets, including one 35-mg tab-
with renal impairment (serum creatinine, <2.5 mg/dL), a let of risedronate and six 500-mg tablets of calcium carbonate.
history of esophageal disease, gastritis, or peptic ulcer (5).
In an attempt to address the inconvenience associated with
tablet administration, a once-weekly, 70-mg buffered effer-
vescent formulation of alendronate is under investigation. The oral bioavailability of this agent is extremely poor
(0.6%) and is adversely affected by the presence of food,
Risedronate Sodium (Actonel) The third-generation agent beverages other than water, and other medications,
risedronate sodium has been approved for the treatment including calcium or vitamin D supplements and ant-
of osteoporosis (both postmenopausal and in men), acids. Because of the increased calcium content in min-
Paget disease of the bone, and glucocorticoid-induced eral water, patients should not take this medication with
osteoporosis (Fig. 30.9). Risedronate sodium is 1,000- to this type of water. Drugs that inhibit gastric acid secre-
5,000-fold more potent than etidronate disodium. At the tion (e.g., H2 antagonists and proton pump inhibitors)
end of an 18-month study, 53% of patients who took risedro- actually promote ibandronate sodium absorption. Like
nate sodium for 2 months remained in remission, as com- the other agents in this therapeutic class, ibandronate
pared to 14% of patients who took etidronate disodium, sodium is not metabolized, and that which is not bound
an earlier-generation bisphosphonate, for 6 months. Oral to the bone (40% to 50% of the absorbed dose) is elimi-
administration of this agent suffers from the same prob- nated renally unchanged. It does not inhibit the CYP450
lems as that of other bisphosphonate agents. Risedronate isozymes. This agent does not require any dosage adjust-
sodium should not be given to patients with creatinine ment for patients with hepatic impairment or mild to
clearance of less than 30 mL/min. A once-weekly, delayed- moderate renal impairment (creatinine clearance, >30
release formulation (Atelvia) that can be taken immedi- mL/min). Ibandronate sodium should not be prescribed
ately after breakfast with 4 ounces of water was approved for patients with severe renal impairment (creatinine
by the FDA in October 2010. Other oral formulations of clearance, <30 mL/min).
risedronate sodium include tablets to be consumed daily
(5 mg), weekly (35 mg), and monthly (150 mg). Zoledronic Acid (Reclast) Zoledronic acid is approved
for the treatment of glucocorticoid-induced osteoporosis
Ibandronate Sodium (Boniva) Ibandronate sodium is and prevention and treatment of postmenopausal osteo-
approved for the treatment and prevention of osteopo- porosis, male osteoporosis, and Paget disease of the bone
rosis in postmenopausal women and has a mechanism (Fig. 30.9). For the treatment of osteoporosis, zoledronic
of action that is identical to the other bisphosphonate acid is formulated as a 5-mg, once-yearly IV infusion. The
agents (Fig. 30.9). Administered daily (2.5 mg), ibandro- frequency of IV infusion decreases to 5 mg every 2 years
nate sodium has been clinically shown to reduce the risk for the prevention of osteoporosis. In order to prevent
of vertebral fractures by 62% (48). If administered on an hypocalcemia, concomitant calcium (1,500 mg) and vita-
intermittent basis (20 mg), it reduces the risk of vertebral min D (800 to 1,000 IU) intake and/or supplementation
fractures by 50%. Ibandronate sodium (2.5 mg daily), is recommended in patients being treated for osteopo-
along with 500 mg of supplemental calcium, has been rosis. On the day of treatment, patients should drink at
clinically shown to increase BMD in the hip (1.8%), fem- least two glasses of water and eat normally.
oral neck (2.0%), and lumbar spine (3.1%). A 150-mg Osteonecrosis of the jaw has been reported in patients
formulation has been approved by the FDA for once- receiving IV bisphosphonate therapy (49). The majority
monthly administration as well as a 3-mg IV formulation of the patients who developed osteonecrosis of the jaw
for quarterly administration. were undergoing chemotherapy (typically for multiple
Lemke_Chap30.indd 978 12/9/2011 3:59:15 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 979
myeloma, breast, prostate, or lung cancers), taking corti- treatment of osteoporosis is 100 IU/d (46). Initially only
costeroids, and had undergone a dental procedure (e.g., available by IM or SC injection, the peptide hormone
tooth extraction). The FDA recommends that patients calcitonin-salmon is available as a nasal spray (Miacalcin)
receive a thorough dental examination before initiation and as a rectal suppository (6). A recombinant DNA
of IV bisphosphonate therapy and that they avoid inva- form of calcitonin-salmon (Fortical) is available as a nasal
sive dental work during treatment. spray. The bioavailability of calcitonin-salmon nasal spray
In October 2010, the FDA approved safety labeling shows great variability (range, 0.3% to 30.6% of an IM
changes for the bisphosphonates in response to reports dose). It is absorbed rapidly from the nasal mucosa, with
of an increase in risk of atypical femur fracture in patients peak plasma concentrations appearing 30 to 40 minutes
undergoing long-term bisphosphonate therapy (50,51). after nasal administration, compared with 16 to 25 min-
In addition, an increase in the risk of developing esopha- utes following parental dosing. Calcitonin-salmon is read-
geal cancer has surfaced in patients with approximately ily metabolized in the kidney, with an elimination half-life
5 years of oral bisphosphonate use. Because of these calculated at 43 minutes. As a result, the intranasal dose
adverse effects, it is recommended that clinicians weigh required is 200 IU/d (3). Once the Miacalcin nasal pump
the benefits against the potential risks. has been activated, the bottle may be kept at room tem-
The remaining bisphosphonates, pamidronate diso- perature until the medication is finished (2 weeks).
dium and zoledronic acid, are approved for treatment
of hypercalcemia of malignancy as well as other cancer THERAPEUTIC APPLICATION Calcitonin therapy requires the
conditions and will be discussed later in the chapter. concomitant oral administration of elemental calcium
(500 mg/d, see Table 30.9). Clinical studies have shown
Calcitonin (Calcimar [IV, subcutaneous]; Miacalcin and that the combination of intranasal calcitonin-salmon
Fortical [nasal spray]) (200 IU/d), oral calcium supplementation (>1,000 mg/d
Calcitonin (see earlier discussion in this chapter) has of elemental calcium), and vitamin D (400 IU/d) has
been approved for the treatment of postmenopausal decreased the rate of new fractures by more than 75%
osteoporosis, hypercalcemia of malignancy, and Paget and has improved vertebral BMD by as much as 3% annu-
disease of the bone. Several sources are available (e.g., ally (3). Calcitonin prevents the abnormal bone turn-
eel, human, salmon, and porcine). The calcitonin iso- over characteristic of Paget disease of the bone and has
lated from salmon is the preferred source, because it has antiresorptive activity. In the presence of calcitonin, the
greater receptor affinity and a longer half-life than the osteoclast brush borders disappear, and the osteoclasts
human hormone (3,7). Calcitonin is commercially avail- move away from the bone surface undergoing remodel-
able as synthetic calcitonin-salmon, which contains the ing (52). Side effects are significantly more pronounced
same linear sequence of 32 amino acids, as occurs in nat- when calcitonin-salmon is administered by injection and
ural calcitonin-salmon. Calcitonin-salmon differs struc- can include nausea, vomiting, anorexia, and flushing.
turally from human calcitonin at 16 of 32 amino acids Because calcitonin-salmon is protein in nature, the possi-
(see Fig. 30.10 for primary structure differences between bility of a systemic allergic reaction should be considered,
human and salmon calcitonin). The pharmacologic and appropriate measures for treatment of hypersensitiv-
activity of these calcitonins is the same, but calcitonin- ity reaction should be readily available. Although calcito-
salmon is approximately 50-fold more potent on a weight nin-salmon does not cross the placenta, it may pass into
basis than human calcitonin with a longer duration of breast milk. Calcitonin-salmon is a possible alternative to
action. The duration of action for calcitonin salmon is ERT; however, only limited evidence suggests that it has
8 to 24 hours following intramuscular (IM) or subcutane- efficacy in women who already have fractures. Resistance
ous (SC) administration and 0.5 to 12.0 hours following to calcitonin-salmon can result from the development of
IV administration. The parenteral dose required for the neutralizing antibodies (53).
S S
Cys Ser Asn Leu Ser Thr Cys Val Leu Gly Lys Leu Ser Gln Glu Leu His Lys Leu Gln
1 5 10 15 20
Thr Tyr Pro Arg Thr Asn Thr Gly Ser Gly Thr Pro-NH2 Salmon CT
25 30
S S
Cys Gly Asn Leu Ser Thr Cys Met Leu Gly Thr Tyr Thr Gln Asp Phe Asn Lys Phe His
1 5 10 15 20
Thr Phe Pro Gln Thr Ala Ile Gly Val Gly Ala Pro-NH2 Human CT
25 30
FIGURE 30.10 Primary structures of salmon and human calcitonin (CT). Similarities are highlighted in red.
Lemke_Chap30.indd 979 12/9/2011 3:59:15 AM
980 PART III / PHARMACODYNAMIC AGENTS
In addition to its antiresorptive action via suppres- demonstrates 95% bioavailability, and is quickly elimi-
sion of osteoclast activity, calcitonin-salmon exhibits a nated via both hepatic and extrahepatic routes. The half-
potent analgesic effect and has provided considerable life is 1 hour when administered SC. Metabolic studies
relief to those patients suffering from the pain associ- have not been performed on teriparatide; however, the
ated with Paget disease of the bone and osteoporosis. entire PTH preprohormone has been shown to undergo
This analgesic effect is a result of calcitonin-stimulated enzyme-mediated transformations in the liver. Dizziness
endogenous opioid release. The potency of this anal- and leg cramps are the most commonly reported adverse
gesic effect has been demonstrated to be 30- to 50-fold side effects.
that of morphine in selected patients. Calcitonin is pre- Temporary increases in serum calcium levels occur
ferred over estrogen and the bisphosphonates when following administration of teriparatide. As a result, this
treatment of both osteoporosis and related bone pain agent is contraindicated in patients who are predisposed
is warranted. to hypercalcemia. Some evidence suggests that these
elevations in serum calcium levels may cause a patient
who is taking digitalis to experience digitalis toxicity
Bone-Forming Agents
(55). Teriparatide should not be prescribed to patients
Teriparatide (Forteo) with Paget disease of the bone, children, young adults,
In 2002, the FDA approved teriparatide for the treat- women who are pregnant or nursing, and patients who
ment of postmenopausal osteoporosis in patients who have received skeletal radiation therapy (52). Because of
have a high risk of fracture, for the treatment of glu- an increased incidence of osteosarcoma (malignant bone
cocorticoid-induced osteoporosis, and to increase bone tumors) observed in rats, teriparatide also carries a black
mass in men with primary or hypogonadal osteoporosis box warning.
who have a high risk of fracture (54). Teriparatide is
recombinant human PTH 1-34 (Fig. 30.2), the biologi- Inorganic Salts
cally active portion of the endogenously produced pre- CALCIUM SALTS Appropriate intake of calcium during
prohormone. Unlike the bisphosphonates, which are childhood, adolescence, and early adulthood increases
classified as bone restorative agents, teriparatide is the peak BMD and may reduce the overall risk of developing
first approved bone-forming agent. Bone formation is osteoporosis. For those who are at low risk of develop-
possible because of the ability of this agent to increase ing osteoporosis and have adequate BMD, consumption
the number of osteoblasts. Although teriparatide of the recommended amounts of calcium (1,300 mg/d
enhances the function of both osteoclasts and osteo- of elemental calcium for teenagers, 1,000 mg/d for pre-
blasts, the exposure incidence dictates its effect on the menopausal women and men, and 1,200 mg/d for post-
skeleton. If administered once daily or intermittently, menopausal women) typically is sufficient to prevent
teriparatide preferentially enhances osteoblastic func- bone loss (56,57). This often can be accomplished by
tion, and bone formation occurs. Continuous expo- eating a well-balanced diet. For patients with established
sure to endogenous PTH may result in poor skeletal osteoporosis or areas of poorly mineralized bone, cal-
composition because of enhanced osteoclast-mediated cium supplementation alone is not sufficient to reverse
bone resorption (52). After 18 months of treatment, the bone loss or to significantly improve mineralization
lumbar BMD increased up to 12% in postmenopausal of the bone (13).
women. After 10 months of treatment, 53% of men had It should be noted that a study conducted by Bolland
an increase of 5% or greater in spine BMD. The risk for et al. (58) reported that calcium supplementation in
developing new vertebral fractures was reduced by 65% postmenopausal women may be correlated with signifi-
after 21 months of treatment, and the number of non- cant increases in the rates of vascular events.
vertebral fragility fractures was reduced by 53% (35). The actual amount of elemental calcium that is pres-
There is limited evidence that teriparatide can regrow ent in the available calcium salts varies considerably;
jaw bone that has been damaged by osteonecrosis and however, no one particular salt has been identified as an
periodontitis. exceptional source of elemental calcium (Table 30.9).
A black box warning from the FDA advises that treat- Absorption of calcium from the gastrointestinal tract
ment with teriparatide should be avoided in patients (25% to 40%) improves under acidic conditions; there-
with an increased baseline risk for osteosarcoma and that fore, those medications that change the acidic environ-
treatment should not exceed 2 years in duration. ment of the stomach (e.g., H2 antagonists and proton
Administered as a once-daily, 20-mg SC injection in the pump inhibitors) have an adverse effect on calcium
thigh or abdominal wall, teriparatide is a clear, colorless absorption (3). Total daily doses of elemental calcium
liquid that is available as a 750 mg/3 mL, prefilled, dispos- that exceed 500 mg should be spaced out over the day
able pen that requires refrigeration. Concurrent calcium to improve absorption (5,56). The more water soluble
(1,000 mg) and vitamin D (400 IU) supplementation and, therefore, more easily absorbed salts (e.g., citrate,
is recommended. Treatment for longer than 2 years is lactate, and gluconate) are less dependent on the acidic
not recommended. Teriparatide is rapidly absorbed, environment for appropriate absorption and would be
Lemke_Chap30.indd 980 12/9/2011 3:59:15 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 981
TABLE 30.9 Percent of Elemental Calcium Content in Various Salts (3)
Salt Calcium (%) Elemental Calcium (mg/tablet)
Calcium carbonate 40
Tums (500 mg chewable) 200 mg
Titilac (1 g/5 mL suspension) 400 mg/5 mL
Alka-Mints (850 mg chewable) 340 mg
Os-Cal 500 (1,250 mg tablet) 500 mg
Viactive (1,250 mg chewable) 500 mg
Tricalcium phosphate 39
Calcium chloride 27
Tribasic calcium phosphate 23
Posture (1,565.2 mg tablets) 600 mg
Calcium citrate 21
Citrical (950 mg tablets) 200 mg
Citrical Liquitab (2,376 mg effervescent tablets) 500 mg
Calcium lactate 13
Generics (325 mg tablets) 42 mg
Generics (650 mg tablets) 84 mg
Calcium gluconate 9
Neo-Calglucon (1.8 g/5 mL syrup) 115 mg/5 mL
appropriate alternatives for patients who produce low improve bone mass (vertebra, 5% per year; femoral neck,
levels of acid. Calcium carbonate is a poorly soluble form 2% per year) and to decrease the number of vertebral
of calcium, but it is inexpensive and only requires the fractures (59,60).
patient to take a few tablets per day with acidic food or
beverages like citrus juice (56). Monoclonal Antibody-Based Therapies
RANKL Inhibitor
SODIUM FLUORIDE Sodium fluoride (NaF) promotes the DENOSUMAB (PROLIA) Denosumab (Prolia) has been
proliferation and activity of osteoblasts and is classified as approved by the FDA for the treatment of postmeno-
a nonhormonal bone-forming agent. Because treatment pausal women with osteoporosis at high risk for frac-
with NaF induces bone formation, it is essential that this ture. Denosumab is a fully human monoclonal antibody
therapy be coupled with oral calcium supplementation to RANKL, where it functions as a RANKL inhibitor
(1,000 mg/d). Additionally, NaF exhibits moderate anti- (Fig. 30.4). The RANKL receptor is expressed on the
resorptive activity, because it inhibits osteoclastic activity surface of osteoclasts and osteoclast precursors. When
when it is absorbed into the bone matrix. In the treat- bound to its receptor, RANKL promotes the formation
ment of osteoporosis, the therapeutic window for this and activation of osteoclasts. To balance the effects of
agent is fairly narrow: Doses less than 45 mg/d are sub- RANKL, osteoblasts produce osteoprotegerin, which
therapeutic, and doses in excess of 75 mg/d impair bone binds to RANKL and prevents it from binding to and
mineralization. In addition, the bone that is formed in activating its receptor, modulating the production
the presence of NaF is neither as well mineralized nor as and activation of osteoclasts (61). When an individual
strong as normal bone tissue. In fact, some studies have develops osteoporosis, this balance is “disrupted,” and
demonstrated that patients taking sodium fluoride have RANKL overwhelms osteoprotegerin activity, causing
increased bone fragility despite the increase in bone mass significant bone loss. Denosumab was designed to mimic
and, as a result, have an increased nonvertebral fracture the biochemical effects of osteoprotegerin. Studies show
rate as compared to the placebo group (5,31,46). As a that denosumab is more effective in improving BMD
result, its use in the treatment of osteoporosis has not (4% to 7%) than weekly administration of alendronate
been approved and is considered to be somewhat con- (5%) (61). Denosumab is reported to reduce the risk
troversial. Several studies have examined the benefits of of vertebral fraction (68%), hip fracture (40%), and
continuous versus cyclic dosing of NaF in the treatment nonvertebral facture (20%). This agent is administered
of osteoporosis. Intermittent dosing (25 mg twice a day subcutaneously once every 6 months and has been asso-
for 12 months, followed by 2 months of calcium supple- ciated with adverse events including back pain (35%),
mentation alone) of a slow-release formulation of NaF serious infections, hypocalcemia, and osteonecrosis of
with 400 mg of calcium citrate was shown to effectively the jaw.
Lemke_Chap30.indd 981 12/9/2011 3:59:15 AM
982 PART III / PHARMACODYNAMIC AGENTS
Cathepsin K Inhibitor The hydroxymethylglutaryl–coenzyme A (HMG-CoA)
ODANACATIB Odanacatib selectively inhibits cathepsin K, reductase inhibitors, otherwise known as the statins, have
a cytosolic cysteine protease. Produced by osteoclasts, been found to increase bone formation via enhanced
this protease is responsible for degradation of the col- activity of the bone morphogenic protein 2 (BMP-2)
lagen matrix found in bone tissue. gene. This gene increases osteoblast differentiation. In
addition, by inhibiting HMG-CoA reductase, the statins
H3C
F not only prevent the biosynthesis of cholesterol but also
CF3 CH3 prevent the formation of compounds associated with
H
N CN osteoclast activation (67). Unfortunately, clinical data
N
H
O
from several large studies conflict, and further study is
warranted before the statins can be considered as a viable
H3C
S treatment for osteoporosis (68).
O O
There are a number of investigational agents in the
Odanacatib pipeline that act through very novel mechanisms of
action (Table 30.10). These include calcilytic inhibitors,
Phase II clinical studies with odanacatib show that inhibitors of protein tyrosine kinase C-src, and Dkk1
treatment for 2 years resulted in an increase in BMD at monoclonal antibodies (66,69).
the lumbar spine and hip (62). Odanacatib is being eval-
uated in large-scale phase III clinical trials on vertebral,
hip, and nonvertebral fractures. DRUG THERAPIES USED TO TREAT
HYPERPARATHYROIDISM
Miscellaneous Therapies Increased levels of PTH lead to moderately to severely
Strontium ranelate (Protelos) is an orally active agent elevated serum calcium concentrations and alterations
that can be classified as both an antiresorptive agent and in phosphorous metabolism (2). To modulate the levels
a bone-forming agent (63,64). of PTH released from the parathyroid gland chief cells,
regulation of CaSR sensitivity is required. An agonist at
O this receptor, a calcimimetic, serves to activate the recep-
NC
O O
Sr2+
tor, whereas an antagonist at this receptor is classified as
O N O a calcilytic. There are two types of calcimimetic agents:
S
Sr2+ O O those that activate the CaSR directly (type I), and those
O that require the presence of a cation, such as calcium or
magnesium (type II), for activation (70). Type I calcimi-
Strontium ranelate metics are polycations (e.g., magnesium and neomycin).
The first and second generations of type II calcimimet-
It is able not only to stimulate replication of preosteo- ics are phenylalkylamine based. They have an indirect/
blastic cells to promote bone formation but also is able to allosteric action on CaSR mediated by a conformational
decrease osteoclastic activity to prevent bone resorption. alteration of these receptors.
Biochemical markers for bone formation (e.g., bone-
specific alkaline phosphatase), which normally decrease Cinacalcet Hydrochloride (Sensipar)
in the presence of antiresorptive therapy, are elevated
in the presence of strontium ranelate (65). Strontium CH3
ranelate is active by virtue of the strontium cation and N
H HCl
not the anion portion of the drug. Lumbar spine BMD
increased 11.4% in patients treated with this new agent. CF3
Although approved as second-line therapy for the treat-
ment of osteoporosis in a number of European nations, Cinacalcet hydrochloride (Sensipar)
Protelos is not FDA approved (66).
TABLE 30.10 Classes of Experimental Agents for Treatment of Abnormal Calcium Homeostasis
Class Action
Antiresorptive Agents
Cathepsin K inhibitors Prevent degradation of collagen matrix
C-src kinase inhibitors Prevent formation of osteoclast sealing zone
Bone-Forming Agents
Calcilytic agents Inhibit calcium-sensing receptors to promote PTH release
Dkk1 monoclonal antibody Inhibitor of negative regulators of Wnt signaling
Lemke_Chap30.indd 982 12/9/2011 3:59:16 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 983
Cinacalcet is the first type II calcimimetic agent approved function occurs when single doses of this agent exceed
that improves CaSR sensitivity to calcium (29,71). 4 mg and the infusion duration is less than 15 minutes
When calcium is bound to the CaSR, phospholipase C (74). It is recommended that patients be well hydrated
is activated, and the secretion of PTH is inhibited. In before infusion. If serum calcium levels do not fall to
the presence of cinacalcet, not only is a decrease in normal levels, retreatment is appropriate, but retreat-
PTH levels observed, but a decrease in serum calcium ment is not recommended until 7 days have elapsed
and phosphorous levels is also observed. This repre- from the initial treatment. For the treatment of mul-
sents a significant therapeutic advantage over vitamin tiple myeloma and metastatic bone lesions, a 4-mg ini-
D–based treatments for secondary hyperparathyroidism tial dose is recommended, followed by additional doses
(29). Cinacalcet hydrochloride is a second-generation every 3 to 4 weeks for 9 to 15 months (prostate can-
calcimimetic approved for the treatment of secondary cer, 15 months; breast cancer, 12 months; other solid
hyperparathyroidism in patients with chronic kidney tumors, 9 months).
disease on dialysis and for the treatment of hypercalce- Zoledronic acid is a white, crystalline powder that is
mia in patients with parathyroid cancer. It can be used available in vials for reconstitution for IV infusion over at
alone, with vitamin D, and/or with a phosphate binder least 15 minutes. It does not undergo metabolic transfor-
(72). mation and does not inhibit CYP450 enzymes. Clearance
of this agent is dependent on the patient’s creatinine
clearance, not on dose. Serum creatinine levels should
DRUG THERAPIES USED TO TREAT be evaluated prior to every treatment. Zoledronic
HYPERCALCEMIA OF MALIGNANCY acid is contraindicated in patients with severe renal
impairment.
Zoledronic Acid (Zometa) Zoledronic acid should not be mixed with infusion
Zoledronic acid, a bisphosphonate, was approved by solutions that contain calcium (e.g., lactated Ringer’s)
the FDA in 2001 for the treatment of hypercalcemia and should be administered via IV infusion in its own
of malignancy, a metabolic complication that can be line. Because of the possibility of a serious deteriora-
life-threatening (Fig. 30.9). Hypercalcemia of malig- tion in renal function, the manufacturer requires strict
nancy can occur in up to 50% of patients diagnosed adherence to the infusion duration being no less than
with advanced breast cancer, multiple myeloma, and 15 minutes.
non–small-cell lung cancer. This condition arises when
chemical moieties produced by the tumor cause over- Pamidronate Disodium (Aredia)
stimulation of osteoclasts. When there is an increase
Pamidronate disodium, a second-generation bisphos-
in bone degradation, there is a concomitant release of
phonate, is 100-fold more potent than etidronate
calcium into the plasma. When serum concentrations
disodium for the treatment of hypercalcemia of malig-
of calcium rapidly elevate, the kidneys are unable to
nancy (Fig. 30.9) (6). It has also been approved for
handle the overload, and hypercalcemia results. This
the treatment of Paget disease of the bone and for
can lead to dehydration, nausea, vomiting, fatigue, and
osteolytic bone metastases of breast cancer and osteo-
confusion. Zoledronic acid effectively decreases plasma
lytic lesions of multiple myeloma. When used to treat
calcium concentrations via inhibition of bone resorp-
bone metastases, pamidronate disodium decreases
tion (inhibition of osteoclastic activity and induction
osteoclast recruitment, decreases osteoclast activity,
of osteoclast apoptosis). It also prevents the increase in
and increases osteoclast apoptosis (75). Administered
osteoclastic activity caused by tumor-based stimulatory
by IV infusion, a single dose is typically sufficient for
factors. In addition, zoledronic acid has been approved
the treatment of hypercalcemia and Paget disease of
by the FDA for the treatment of multiple myeloma and
the bone. In the treatment of osteolytic lesions of mul-
bone metastases associated with solid tumor–based can-
tiple myeloma, monthly administration is indicated.
cers (e.g., prostrate and lung) (73).
Pamidronate disodium is cleared renally and therefore
Cancer treatment–induced bone loss is a major
is contraindicated in patients with deteriorated renal
adverse effect associated with endocrine-based can-
function.
cer therapies. These therapies may depress ovarian
function (e.g., goserelin acetate), decrease ER acti-
vation (e.g., ER antagonist), and/or inhibit estrogen Gallium Nitrate (Ganite)
biosynthesis (e.g., aromatase inhibition) all of which
will lead to significant bone loss. Zoledronic acid has O
Ga3+
demonstrated efficacy in reducing or delaying these O N O
complications. 3
The maximum recommended dose for the treat-
ment of hypercalcemia of malignancy is 4 mg every 3 Gallium nitrate has been approved for the treatment
to 4 weeks. A clinically significant deterioration in renal of hypercalcemia of malignancy in patients who do not
Lemke_Chap30.indd 983 12/9/2011 3:59:16 AM
984 PART III / PHARMACODYNAMIC AGENTS
respond to hydration (46). Its effectiveness stems from DRUG THERAPY USED IN THE TREATMENT
its ability to inhibit bone resorption despite the pres- OF HYPOPARATHYROIDISM
ence of tumor-derived factors that promote calcium
loss from the bone. Administered by infusion over 24 Parathyroid Hormone [rDNA 1-84] (Preos)
hours, the typical dose is 200 mg/m2/day for 5 consecu- In 2007, the FDA Office of Orphan Products Development
tive days. A lower dose is recommended if the symptoms granted orphan drug designation for Preos for the treat-
of hypercalcemia are mild (100 mg/m2/d for 5 days). ment of hypoparathyroidism (Fig. 30.2). Structurally iden-
Steady-state is achieved in 24 to 48 hours. Maintenance tical to endogenous PTH, the recombinant human PTH
of patient hydration is essential during treatment. is administered once daily as an SC injection. Although
Gallium nitrate is not significantly metabolized and is Preos shares a common mechanism of action with teripa-
largely excreted through the kidneys. It is contraindi- ratide, it has been suggested that the C-terminal region
cated in patients with severe renal impairment. Renal may possess valuable biologic activity mediated by a novel
function should be closely monitored in all patients receptor that specifically interacts with this portion of the
receiving this agent. peptide hormone.
SCENARIO: OUTCOME AND ANALYSIS
Outcome it is not a CO2 generator, this adverse effect is not commonly
experienced with calcium citrate. Absorption of calcium in the
Kathryn Neill, PharmD
duodenum is dependent upon active vitamin D. Dietary vitamin
The pharmacist recommends changing the calcium carbonate D intake is rarely adequate to meet the recommended 800–1,000
to calcium citrate 200 mg with 200 IU of vitamin D (two tablets units per day (some researchers now recommend 2000 units per
three times daily); limiting caffeine intake to no more than two day), and supplementation is usually necessary, especially for
servings daily; and separating the administration of ramipril seniors who may have even higher daily requirements.
from calcium by 2 hours. Calcium should be separated from doses of other medi-
cations by 2 hours to prevent chelation, which can result in
Chemical Analysis decreased absorption and therapeutic effects. As a divalent cat-
Victoria F. Roche and S. William Zito ion, calcium will be chelated by electron-rich (nucleophilic) atoms
like oxygen. Both ramipril and alendronate have many nucleo-
The oral bioavailability of calcium ranges from approximately
philic oxygen atoms that could sequester calcium ion, as shown
5% to 45%. Absorption is dependent on salt form, dose, pres-
below.
ence of gastric acid, and presence of activated vitamin D.
Calcium absorption is increased when administered with meals 2
2 2 2
as a result of increased secretion of gastric acid in response to a Ca Ca Ca Ca
food bolus. The increased gastric acidity releases calcium from 2
O
O H
H H O P
water insoluble salt forms (like calcium carbonate) and allows its C2H5 O O
Ca O O Ca
2
C O C H2N
absorption. For example, calcium carbonate absorption increases O
H
H O P 2
as much as 30% when taken with a meal. Absorption of calcium HN C N
2 O
O Ca
H H Ca
citrate is greater than other salt forms because it is freely water CH3 H 2
Ca
soluble and does not require the action of strong acid to break
down the salt to release the calcium. Therefore, it is the most Calcium chelated by ramipril Calcium chelated by alendronate
efficacious calcium supplement for patients with achlorhydria.
It would be important to counsel PJ to take alendronate
CaCO3 CaCl2
with a full glass of water and to remain in a sitting or stand-
Calcium carbonate Calcium citrate ing position for at least 30 minutes because this bisphospho-
nate can induce a chemical esophagitis that could exacerbate
As it dissolves in the gastric acid, calcium carbonate can cre- the distress PJ is experiencing from other GERD-related
ate gas (CO2) in the stomach, resulting in stomach upset. Because pathologies.
Lemke_Chap30.indd 984 12/9/2011 3:59:16 AM
CHAPTER 30 / CALCIUM HOMEOSTASIS 985
CASE STUDY
Victoria Roche and S. William Zito
JA is a 73-year-old woman who had polio 58 years ago. Although hearing, Paget’s disease predisposes patients to the development
she had maintained a very active lifestyle throughout her youth of osteosarcoma, a rare and therapeutically challenging bone
and most of her adulthood, postpolio syndrome (PPS) has signifi- cancer. It is important that JA be treated for this disease because,
cantly restricted her mobility and she now uses a wheelchair at in addition to these serious complications and the compounding
home and a power chair to get around outside. JA’s relative lack of of her pain, she would be at high risk for compression fractures
activity during the past 5 years has caused a troublesome weight from the stress she must put on her arms when she transfers to
gain, and she now carries close to 185 pounds on a 5′5″ frame. and from her wheelchair and power chair.
The extreme fatigue that is a hallmark of PPS is complicated by JA’s current medications include the proton pump inhibi-
osteoarthritis in the joints of her upper extremities that came from tor pantoprazole sodium (Protonix) for gastric hyperacidity and
years of walking in full leg braces with the aid of canes. Some days pregabalin (Lyrica) for neuropathic pain in her feet. She takes
the fatigue and the joint pain are so disabling that she just stays 1,000 mg of elemental calcium daily (2 Viactiv calcium chews)
in bed and sleeps, saying it is the only place she is comfortable. and 2,000 IU of vitamin D. She is depending on you, her ambu-
JA was recently diagnosed with Paget’s disease of the bone, latory care pharmacist, to select the right therapy to keep her
a disorder characterized by the deterioration and demineraliza- going in the face of this newest health challenge. You contem-
tion of bone. In addition to exacerbating osteoarthritis and lead- plate the structures of three potential drug candidates shown
ing to loss of below.
CH3O NH
OCH3 OH OH N
O H O H O H O
H
N N N N O
H2N N N N N
N H O H O H O H HN NH2
O
S O H2N O
O OH S
N NH2 O OH O NH2 HN O
N HO O
Na HN NH O H O H O H O
O N N N NH
N N N N
F2 CH NH H O H O H O H
O HN
S NH2 NH2 N
HN O
Pantoprazole sodium H NH2
O O N O
O O O O
H3C H H
HN N HN N N
CH CH2 CH CH2 COOH N N
HO H H
H3C O H
CH2-NH2 NH O
HN O
O NH
H 2N N O
Pregabalin H
NH2 NH
O OH
PO3H2
O HN O
CH3-(CH2)4 N (CH2)2 C PO3H2 H
2 HO N
N
CH3 OH H
O O
O N
1 NH2 HN
NH2
HO
O O O
H H H H
N NH N N N
HN N N
O O H H O
O OH O O
O NH2 O N
O H H
N S S NH
N OH
NH2
H O O
HO NH2 NH O
O NH2 HO O NH2
NH2 NH HO
NH NH O
O O O
H H H
O N N N
O N N N N O
N H H H H
O O O O
OH NH OH
N
NH NH2 NH
H2N O
O
O O O
H H H
N N N
O N N N N
H
O
H
O
H
O 3
HO OH HO
1. Conduct a thorough and mechanistic SAR analysis of the 2. Apply the chemical understanding gained from the SAR
three therapeutic options in the case. analysis to this patient’s specific needs to make a thera-
peutic recommendation.
Lemke_Chap30.indd 985 12/9/2011 3:59:17 AM
986 PART III / PHARMACODYNAMIC AGENTS
References 38. Grese TA, Sluka JP, Bryant HU, et al. Benzopyran selective estrogen receptor
modulators (SERMs): pharmacological effects and structural correlation with
1. Copp DH. Calcitonin: discovery, development, and clinical application. Clin raloxifene. Bioorg Med Chem Lett 1996;6:903–908
Invest Med 1994;17:268–277. 39. Bryant HU, Glasebrook AL, Yang NN, et al. A pharmacologic review of raloxi-
2. Bouillon R, Carmeliet G, Boonen S. Aging and calcium metabolism. Bailliere’s fene. J Bone Miner Metab 1996;14:1–9.
Clin Endocrinol Metab 1997;11:341–365. 40. Kemp DC, Fan PW, Stevens JC. Characterization of raloxifene glucuronida-
3. Haines ST, Caceres B, Yancey L. Alternatives to estrogen replacement therapy tion in vitro: contribution of intestinal metabolism to presystemic clearance.
for preventing osteoporosis. J Am Pharm Assoc 1996;36:707–715. Drug Metab Dispos 2002;30:694–700.
4. Christenson RH. Biochemical markers of bone metabolism: an overview. Clin 41. Jeong EJ, Lin H, Hu M. Disposition mechanisms of raloxifene in the human
Biochem 1997;30:573–593. intestinal Caco-2 model. J Pharmacol Exp Ther 2004;310:376–386.
5. Miller DR, Hanel HJ. Prevention and treatment of osteoporosis. US 42. Jeong EJ, Liu Y, Lin H, et al. Species- and disposition model-dependent
Pharmacist 1999;24:81–90. metabolism of raloxifene in gut and liver: role of UGT1A10. Drug Metab
6. Rodan GA. Emerging therapies in osteoporosis. Ann Rpts Med Chem Dispos 2005;33:785–794.
1994;29:275–285. 43. Gennari L. Ospemifene. Curr Opin Invest Drugs 2004;5:448–455.
7. Arnaud CD. Calcium homeostasis: regulatory elements and their integration. 44. Gruber C, Gruber D. Bazedoxifene. Curr Opin Invest Drugs 2004;5:1086–1093.
Fed Proc 1978;37:2557–2560. 45. Diener KM. Bisphosphonates for controlling pain from metastatic bone dis-
8. Iqbal J, Zaidi M, Schneider AE. Cinacalcet hydrochloride. IDrugs ease. Am J Health Syst Pharm 1996;53:1917–1927.
2003;6:587–592. 46. Caggiano TJ, Zask A, Bex F. Recent advances in bone metabolism and osteo-
9. DeLuca HF, Zierold C. Mechanisms and functions of vitamin D. Nutr Rev porosis research. Ann Rpts Med Chem 1991;26.
1998;56:S4–S10. 47. Ashworth L. Focus on alendronate. Formulary 1996;31:23–30.
10. Raisz LG. Pathogenesis of osteoporosis: concepts, conflicts and prospects. 48. Riley TN, DeRuitter J. New drug review. US Pharmacist 2003:95–104.
J Clin Invest 2005;115:3318–3325. 49. King AE, Umland EM. Osteonecrosis of the jaw in patients receiving intrave-
11. U.S. Department of Health and Human Services. Chapter 2: the basics of nous or oral bisphosphonates. Pharmacotherapy 2008;28:667–677.
bone in health and disease. In: Bone Health and Osteoporosis: A Report of 50. U.S. Food and Drug Administration. Bisphosphonates (osteoporosis drugs): label
the Surgeon General (2004). Available at: http://www.surgeongeneral.gov/ change—atypical fractures update. Available at: http://www.fda.gov/Safety/
library/bonehealth/. Accessed January 19, 2011. MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/
12. Schaefer B, Cone S. Increasing awareness of osteoporosis: a community phar- ucm229244.htm. Accessed January 14, 2011.
macy’s experience. US Pharmacist 1998;23:72–85. 51. Schmidt GA, Horner KE, McDanel DL, et al. Risks and benefits of long-term
13. Francis RM. Management of established osteoporosis. Br J Clin Pharmacol bisphosphonate therapy. Am J Health Syst Pharm 2010;67:e12–e19.
1998;45:95–99. 52. Reginster J. Calcitonin for prevention and treatment of osteoporosis. Am J
14. Saljoughian M. Postmenopausal osteoporosis. US Pharmacy 2003;28:18–35. Med 1993;95(Suppl 5A):44S–47S.
15. Hansen LB, Follin Vondracek S. Prevention and treatment of nonpostmeno- 53. Gennari C, Agnusdei D, Camporeale A. Long-term treatment with calcitonin
pausal osteoporosis. Am J Health Syst Pharm 2004;61:2637–2656. in osteoporosis. Horm Metab Res 1993;25:484–485.
16. Watts NB, Bilezikian JP, Camacho PM, et al. American Association of Clinical 54. Freeman TR. Teriparatide: a novel agent that builds new bone. J Am Pharm
Endocrinologists medical guidelines for clinical practice for the diagnosis and Assoc 2003;43:535–537.
treatment of postmenopausal osteoporosis. Endocr Pract 2010;16(Suppl 3):1–37. 55. LoBuono C. New osteoporosis drug is first to form bone. Drug Topics 2003:24.
17. O’Connell MB, Borgelt LM, Bowles SK, et al. Drug-induced osteoporosis in 56. American Pharmaceutical Association. Special Report. Therapeutic Options for
the older adult. Aging Health 2010;6:501–518. Osteoporosis. Washington, DC: American Pharmaceutical Association, 1993.
18. Reid DM, Harvie J. Secondary osteoporosis. Bailliere’s Clin Endocrinol Metab 57. Institute of Medicine, National Academy of Sciences. Dietary reference intakes
1997;11:83–99. for calcium and vitamin D. Available at: http://iom.edu/Reports/2010/
19. Diem SJ, Blackwell TL, Stone KL, et al. Use of antidepressants and rates of hip Dietar y-Reference-Intakes-for-Calcium-and-Vitamin-D/DRI-Values.aspx.
bone loss in older women. Arch Intern Med 2007;167:1240–1245. Updated November 20, 2010.
20. Gray SL, LaCroix AZ, Larson J, et al. Proton pump inhibitor use, hip fracture 58. Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older
and change in bone mineral density in postmenopausal women. Arch Intern women receiving calcium supplementation: randomized controlled trial. BMJ
Med 2010;179:765–771. 2008;336:262–266.
21. Riche DM, King ST. Bone loss and fracture risk associated with thiazolidinedi- 59. American Pharmaceutical Association. New product bulletin. Miacalcin nasal
one therapy. Pharmacotherapy 2010;30:716–727. spray. Washington, DC: American Pharmaceutical Association, 1996.
22. van Brussel MS, Bultink IE, Lems WF. Prevention of glucocorticoid-induced 60. Pak CYC, Sakhaee K, Rubin C, et al. Update of fluoride in the treatment of
osteoporosis. Exp Opin Pharmacother 2009;10:997–1005. osteoporosis. Endocrinologist 1998;8:15–20.
23. National Osteoporosis Foundation. Clinicians guide to prevention and treatment 61. Bekker PJ, Holloway DL, Rasmussen AS, et al. A single-dose placebo-con-
of osteoporosis, revised January 2010. Available at: http://www.nof.org/sites/ trolled study of AMG 162, a fully human monoclonal antibody to RANKL in
default/files/pdfs/NOF_ClinicianGuide2009_v7.pdf. Accessed January 10, 2011. postmenopausal women. J Bone Miner Res 2004;19:1059–1066.
24. International Osteoporosis Foundation. Facts and statistics about osteopo- 62. Bone HG, McClung MR, Roux C, et al. Odanacatib, a cathepsin-K inhibitor
rosis and its impact. Available at: http://www.iofbonehealth.org/facts-and- for osteoporosis: a two year study in postmenopausal women with low bone
statistics.html. Accessed January 10, 2011. density. J Bone Miner Res 2010;25:934–936.
25. Barrett-Connor E, Siris ES, Wehren LE, et al. Osteoporosis and fracture risk in 63. Meunier PJ, Roux C, Seeman E, et al. The effects of strontium ranelate on the
women of different ethnic groups. J Bone Miner Res 2005;20:185–194. risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl
26. Tolar J, Teitelbaum SL, Orchard PJ. Osteopetrosis. N Engl J Med J Med 2004;350:459–468.
2004;351:2839–2849. 64. Reginster J-Y, Lecart M-P, Deroisy R, et al. Strontium ranelate—a new paradigm
27. Whyte MP, Wenkert D, Clements KL, et al. Bisphosphonate-induced osteopo- in the treatment of osteoporosis. Expert Opin Investig Drugs 2004;13:857–864.
rosis. N Engl J Med 2003;349:457–463. 65. Marie PJ. Strontium ranelate: a novel mode of action optimizing bone forma-
28. Suneja M. Hypocalcemia. Available at: http://www.emedicine.com/med/ tion and resorption. Osteoporosis Int 2005;16(Suppl 1):S7–S10.
topic1118.htm. Updated September 3, 2010. Accessed January 21, 2011. 66. Gogakos AI, Cheung MS, Bassett JHD, et al. Bone signaling pathways and
29. Block GA, Martin, KJ, De Franciso AL. Cinacalcet for secondary hyperparathy- treatment of osteoporosis. Expert Rev Endocrinol Metab 2009;4:639–650.
roidism in patients receiving hemodialysis. N Engl J Med 2004;350:1516–1525. 67. Gonyeau M. Statins and osteoporosis: a clinical review. Pharmacotherapy
30. Reginster J-YL, LeCart M-P. Efficacy and safety of drugs for Paget’s disease of 2005;25:229–243.
bone. Bone 1995;17:485S–488S. 68. Richard AA, Harrison TM. Efficacy of HMG-CoA reductase inhibitors in treat-
31. De Silva Jardine P, Thompson D. Antiosteoporosis agents. Ann Rpts Med ing osteoporosis. Am J Health Syst Pharm 2002;59:372–377.
Chem 1996;31:211–220. 69. Burkiewicz J, O’Connell MB. New approaches to the management of osteopo-
32. Hisel TM, Phillips BB. Update on the treatment of osteoporosis. Formulary rosis. American Pharmacists Association Highlights Newsletter 2010;13:S1–S12
2003;38:223–243. 70. Joy MS, Kshirsagar A, Franceschini N. Calcimimetics and the treatment of pri-
33. Rossouw JE, et al. Risks and benefits of estrogen plus progestin in healthy mary and secondary hyperparathyroidism. Ann Pharmacother 2004;38:171–180.
postmenopausal women. Principal results from the Women’s Health Initiative 71. Franceschini N, Joy MS, Kshirsagar A. Cinacalcet HCl: a calcimimetic agent
randomized controlled trial. JAMA 2002;288:321–333. for the treatment of primary and secondary hypoparathyroidism. Expert
34. Women’s Health Initiative Steering Committee. Effects of conjugated equine Opin Investig Drugs 2003;12:1413–1421.
estrogen in postmenopausal women with hysterectomy. JAMA 2004;291: 72. Hussar DA. New drugs of 2004. J Am Pharm Assoc 2005;45:185–218.
1701–1712. 73. Michaelson MD, Smith MR. Bisphosphonates for treatment and prevention of
35. Greenblatt D. Treatment of postmenopausal osteoporosis. Pharmacotherapy bone metastases. J Clin Oncol 2005;23:8219–8224.
2005;25:574–584. 74. Zometa prescribing information. Available at: http://www.pharma.
36. Francis RM. Bisphosphonates in the treatment of osteoporosis in 1997: a us.novartis.com/product/pi/pdf/Zometa.pdf. Updated October 2009.
review. Curr Ther Res 1997;58:656–678. Accessed January 20, 2011.
37. Yates AJ, Rodan GA. Alendronate and osteoporosis. Drug Discov Today 75. Van Poznak CH. The use of bisphosphonates in patients with breast cancer.
1998;3:69–78. Cancer Control 2002;9:480–489.
Lemke_Chap30.indd 986 12/9/2011 3:59:17 AM
You might also like
- Antioxidants and Reactive Oxygen Species in PlantsFrom EverandAntioxidants and Reactive Oxygen Species in PlantsNicholas SmirnoffNo ratings yet
- Iminosugars: From Synthesis to Therapeutic ApplicationsFrom EverandIminosugars: From Synthesis to Therapeutic ApplicationsPhilippe CompainNo ratings yet
- NSAIDs and GI Drugs PharmacologyDocument46 pagesNSAIDs and GI Drugs PharmacologyLeonibel GhloeNo ratings yet
- Zinc Overview PDFDocument11 pagesZinc Overview PDFLê Nguyễn Hoàng Anh100% (1)
- Antioxidant Properties of A North American Ginseng Extract: David D. Kitts, Arosha N. Wijewickreme and Chun HuDocument10 pagesAntioxidant Properties of A North American Ginseng Extract: David D. Kitts, Arosha N. Wijewickreme and Chun HuYohandry Cruz AvilaNo ratings yet
- Calcium Phosphorus Metabolic DisordersDocument102 pagesCalcium Phosphorus Metabolic DisordersAME DENTAL COLLEGE RAICHUR, KARNATAKANo ratings yet
- Non Hormonal AgentsDocument5 pagesNon Hormonal AgentsMarianne CruzNo ratings yet
- Calcium Metabolism PresentationDocument103 pagesCalcium Metabolism PresentationmeghaNo ratings yet
- NeurotransmittersDocument92 pagesNeurotransmittersClare DucutNo ratings yet
- Dr. Smijal PG Its Year Department of PeriodonticsDocument98 pagesDr. Smijal PG Its Year Department of PeriodonticsMax FaxNo ratings yet
- Calcium and phosphorus metabolism competency tableDocument8 pagesCalcium and phosphorus metabolism competency tableSaranNo ratings yet
- General Treatment of PoisoningDocument21 pagesGeneral Treatment of PoisoningpikachuNo ratings yet
- Mineral Ebook - TeamEvilGSPDocument50 pagesMineral Ebook - TeamEvilGSPnathanNo ratings yet
- Pharmacology Module-7Document6 pagesPharmacology Module-7maurizemedija15No ratings yet
- Pain Management - Lecture 6 Print OutDocument66 pagesPain Management - Lecture 6 Print OutNoor A. ZakiNo ratings yet
- Biochemistry Midterm RecallsDocument3 pagesBiochemistry Midterm Recallssuper novaNo ratings yet
- Case StudyDocument9 pagesCase Studyharshe vNo ratings yet
- Chemistry of Nucleotides - Copy (Autosaved)Document33 pagesChemistry of Nucleotides - Copy (Autosaved)Zille HummaNo ratings yet
- Pharmacy Training - Gastro Intestinal TractDocument56 pagesPharmacy Training - Gastro Intestinal TractDylanSalam100% (1)
- IM (4.3.4) Micronutrients. Student NotesDocument6 pagesIM (4.3.4) Micronutrients. Student Notesmd85vccszzNo ratings yet
- Clinical Chemistry: International Unit KatalDocument11 pagesClinical Chemistry: International Unit KatalAngelica Joy GonzalesNo ratings yet
- Bio Inorganic 1 PPT ChemistryDocument57 pagesBio Inorganic 1 PPT ChemistryShantanu MawaskarNo ratings yet
- Determination of Iron, Magnesium and Zinc in FoodDocument19 pagesDetermination of Iron, Magnesium and Zinc in FoodShailaja NeaupaneNo ratings yet
- Glucocorticoids and Mineralocorticoids: Roles and EffectsDocument27 pagesGlucocorticoids and Mineralocorticoids: Roles and EffectsAmrit GaireNo ratings yet
- Copper - Uses, Interactions, Mechanism of Action - DrugBank OnlineDocument115 pagesCopper - Uses, Interactions, Mechanism of Action - DrugBank OnlineamiNo ratings yet
- General Treatment of PoisoningDocument21 pagesGeneral Treatment of PoisoningpikachuNo ratings yet
- Enzymes (Group 1)Document30 pagesEnzymes (Group 1)Danielle AboyNo ratings yet
- BIKTOK - Week 4Document35 pagesBIKTOK - Week 4Tiara FibriNo ratings yet
- BDS Biochemistry SyllabusDocument4 pagesBDS Biochemistry SyllabusAnandNo ratings yet
- Chapter 28 AdrenocorticoidsDocument36 pagesChapter 28 AdrenocorticoidsCapuNo ratings yet
- KP 1.4.2.4 MineralDocument47 pagesKP 1.4.2.4 MineralSri Rahma LizaNo ratings yet
- Physiology RenalDocument14 pagesPhysiology Renalahmedsalah565vvvNo ratings yet
- Ankita PerioDocument37 pagesAnkita PerioOindrila GhoshNo ratings yet
- Vitamin DDocument51 pagesVitamin DMeriam AntonyNo ratings yet
- SteroidsDocument25 pagesSteroidsalhusien.abd2000No ratings yet
- Nutrition and VitaminDocument70 pagesNutrition and VitaminTob JurNo ratings yet
- Basal GangliaDocument76 pagesBasal GangliaHussain ANo ratings yet
- MineralDocument15 pagesMineralKriti KumariNo ratings yet
- MSB 202: Neurolocomotor: Neurotransmitters - Overview of Metabolism (Anabolism and Catabolism)Document42 pagesMSB 202: Neurolocomotor: Neurotransmitters - Overview of Metabolism (Anabolism and Catabolism)Jacob MasikaNo ratings yet
- Vitamins and MineralsDocument91 pagesVitamins and MineralsPyaesone AungNo ratings yet
- ULYA UTI FASRINI, DR., M.BiomedDocument47 pagesULYA UTI FASRINI, DR., M.BiomedralichramNo ratings yet
- Common Maintenance Medications: Brand Name Generic Name TierDocument4 pagesCommon Maintenance Medications: Brand Name Generic Name Tierstephanie valerioNo ratings yet
- Kontras Agent MRIDocument68 pagesKontras Agent MRIFajar FitriansyahNo ratings yet
- Agents That Affect Bone Mineral Homeostasis PDFDocument4 pagesAgents That Affect Bone Mineral Homeostasis PDFCas BuNo ratings yet
- Enzymes HoDocument9 pagesEnzymes Hochristian redotaNo ratings yet
- Terapi Cairan PD AnakDocument62 pagesTerapi Cairan PD AnakadeNo ratings yet
- Nucleotides and Nucleic AcidDocument56 pagesNucleotides and Nucleic AcidMrs RehanNo ratings yet
- Sirtuin and Metabolic Kidney Disease: Shu Wakino, Kazuhiro Hasegawa and Hiroshi ItohDocument8 pagesSirtuin and Metabolic Kidney Disease: Shu Wakino, Kazuhiro Hasegawa and Hiroshi ItohMedranoReyesLuisinNo ratings yet
- Cancer Foye's Principles of Medicinal Chemistry-1219-1286Document68 pagesCancer Foye's Principles of Medicinal Chemistry-1219-1286minhxuan100% (3)
- Minerals As Antioxidants: Presented By: A.Selva Arockiam CRI CsicdsrDocument101 pagesMinerals As Antioxidants: Presented By: A.Selva Arockiam CRI CsicdsrSelvaArockiamNo ratings yet
- Unit-2 BPDocument80 pagesUnit-2 BPsrinusmart192No ratings yet
- Brat Er 2000Document13 pagesBrat Er 2000Carla MantillaNo ratings yet
- NiacinDocument13 pagesNiacinapi-388948078No ratings yet
- Glorfindelz Note With AnswerDocument41 pagesGlorfindelz Note With AnswerInah Mae Coleen CapuyanNo ratings yet
- Carbohydrate Metabolism: Sylvia Rianissa PutriDocument47 pagesCarbohydrate Metabolism: Sylvia Rianissa PutriMeilia AndiniNo ratings yet
- PR STEPLADDER CTS AmmaliaDocument27 pagesPR STEPLADDER CTS AmmaliaAmmalia RachmiNo ratings yet
- Trace Elements GuideDocument70 pagesTrace Elements GuideYosanonNo ratings yet
- Trace Elements: DR Manjuprasad Moderater:Dr Ravichandra VDocument50 pagesTrace Elements: DR Manjuprasad Moderater:Dr Ravichandra Vgabb bbNo ratings yet
- MineralsDocument26 pagesMineralsامجد حسين جواد كاظمNo ratings yet
- Antiarritmicos PPT FinalDocument81 pagesAntiarritmicos PPT FinalCarolina González RiveraNo ratings yet
- The Natural Bone Building HandbookDocument60 pagesThe Natural Bone Building HandbookSunpetal2No ratings yet
- Albanese - Imaging of Prosthetic Joints - A Combined Radiological and Clinical Perspective PDFDocument185 pagesAlbanese - Imaging of Prosthetic Joints - A Combined Radiological and Clinical Perspective PDFSergio Gordillo Tovar100% (1)
- Presentation On Osteoporosis: Submitted To: Dr. Divya Vohra Submitted By: Sharique Raza M.pharm Jamia HamdardDocument38 pagesPresentation On Osteoporosis: Submitted To: Dr. Divya Vohra Submitted By: Sharique Raza M.pharm Jamia Hamdardsri susantiiNo ratings yet
- Jurnal BrotowaliDocument11 pagesJurnal Brotowalidesy amaliaNo ratings yet
- Alveolar Bone LossDocument10 pagesAlveolar Bone LossKhaled Al GhaebNo ratings yet
- Host Modulation Therapy - An Innovative Paradigm inDocument8 pagesHost Modulation Therapy - An Innovative Paradigm inpaper kitaNo ratings yet
- 10.1016/j.ymgme.2016.11.045: Abstracts / Molecular Genetics and Metabolism 120 (2016) S17 - S145 S29Document2 pages10.1016/j.ymgme.2016.11.045: Abstracts / Molecular Genetics and Metabolism 120 (2016) S17 - S145 S29Larisa IliescuNo ratings yet
- Final Project PDFDocument75 pagesFinal Project PDFuzzal ahmedNo ratings yet
- Metabolic Bone Disease & Bone Markers - SlidesDocument46 pagesMetabolic Bone Disease & Bone Markers - Slidesmonday125100% (1)
- Host ModulationDocument101 pagesHost ModulationVikrant SainiaNo ratings yet
- Principles of Periodontology Dentino - Et - Al-2013-Periodontology - 2000Document38 pagesPrinciples of Periodontology Dentino - Et - Al-2013-Periodontology - 2000Denisa FloreaNo ratings yet
- Bone Key 2012183Document8 pagesBone Key 2012183Jesus MendezNo ratings yet
- Osteoporosis Treatment and Prevention OptionsDocument55 pagesOsteoporosis Treatment and Prevention OptionsFarhan FauziNo ratings yet
- 1885 2Document73 pages1885 2JuhiJahan AmanullahNo ratings yet
- Basic Science OITE ReviewDocument91 pagesBasic Science OITE ReviewICH KhuyNo ratings yet
- Osteoporosis and OsteopeniaDocument29 pagesOsteoporosis and OsteopeniaShruti Maroo - RathiNo ratings yet
- Laporan Kegiatan Perpanjangan STRDocument44 pagesLaporan Kegiatan Perpanjangan STRFransiskus KharismaNo ratings yet
- Acetabular Revision Surgery in MajorDocument223 pagesAcetabular Revision Surgery in MajorWilson A. Quintero100% (2)
- Frazier-Bowers Et Al, 2016Document11 pagesFrazier-Bowers Et Al, 2016Julio AbarzuaNo ratings yet
- Host ModulationDocument7 pagesHost ModulationDr. Minkle GulatiNo ratings yet
- Bone and Bone Graft HealingDocument12 pagesBone and Bone Graft HealingJayanth PerumalNo ratings yet
- Hormonal Regulation of Calcium and Phosphate MetabolismDocument11 pagesHormonal Regulation of Calcium and Phosphate MetabolismpuchioNo ratings yet
- Bone Metabolism: German VersionDocument17 pagesBone Metabolism: German VersionDapot SianiparNo ratings yet
- PN 1Document1 pagePN 1Florin Eugen ConstantinescuNo ratings yet
- Advances in Orthodontic TreatmentDocument12 pagesAdvances in Orthodontic Treatmentpopat7850% (2)
- University of Miami Division or Oral and Maxillofacial Surgery Position Paper On Drug Induced Osteonecrosis of The Jaws 2014Document26 pagesUniversity of Miami Division or Oral and Maxillofacial Surgery Position Paper On Drug Induced Osteonecrosis of The Jaws 2014Deb SNo ratings yet
- Chapter 80 Parathyroid Hormone, Calcitonin, Calcium and Phosphate Metabolism, Vitamin D, Bone, and TeethDocument12 pagesChapter 80 Parathyroid Hormone, Calcitonin, Calcium and Phosphate Metabolism, Vitamin D, Bone, and Teethputri aisheNo ratings yet
- 2018 Glucocorticoid-Induced OsteoporosisDocument10 pages2018 Glucocorticoid-Induced OsteoporosisMiguel Angel Carrasco MedinaNo ratings yet
- Root Resorption: Challenge To The Endodontist: Acta Scientific Dental SciencesDocument11 pagesRoot Resorption: Challenge To The Endodontist: Acta Scientific Dental SciencesMuhammadDeniRahmanNo ratings yet
- Metabolic EmergenciesDocument48 pagesMetabolic EmergenciesKhanszarizennia Madany AgriNo ratings yet