Professional Documents
Culture Documents
Brachial Plexus Injuries - Trauma - Orthobullets
Uploaded by
manan shroffCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Brachial Plexus Injuries - Trauma - Orthobullets
Uploaded by
manan shroffCopyright:
Available Formats
Search topic, case, evidence or media...
Join now Login
Free CME
Updated: Jun 30 2022
Brachial Plexus Injuries
Jason McKean MD
EXPERTS BULLETS CARDS QUESTIONS CASES EVIDENCE VIDEO/PODS
128 242 17 15 1 29 7
3.8 (126)
58 Expert Comments Topic Podcast
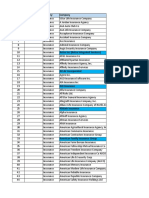
IMAGES
SUMMARY
Brachial plexus injuries (BPIs) can involve any degree of injury at any level of the plexus and range from
obstetric injuries to traumatic avulsions.
Diagnosis requires focused physical examination with EMG/NCS and MRI studies used for conRrmation as
needed.
Treatment can be conservative versus operative depending on the age of patient, chronicity of injury, degree
of injury and nerve root involvement.
EPIDEMIOLOGY
Anatomic location
supraclavicular injuries
complete involvement of all roots is most common
75%-80% of traumatic BPIs
C5 and C6 upper trunk (Erb palsy)
20%-25% of traumatic BPIs
C8, T1 or lower (Klumpke palsy)
0.6%-3.0% of traumatic BPIs
ETIOLOGY
Mechanism
high speed vehicle accidents (mostly motorcycle)
83% of traumatic BPIs
caudally forced shoulder
predominantly affect upper brachial plexus
with high enough energy all roots can be affected
forced arm abduction (as in grabbing onto something while falling)
predominantly affects lower roots
Brachial Plexus injuries include
traumatic injury (this topic)
obstetric brachial plexus injury
Erb's palsy
Klumpke palsy
burners and stingers
Parsonage-Turner Syndrome
ANATOMY
Anatomy
brachial plexus motor and sensory innervation
CLASSIFICATION
Preganglionic vs. postganglionic
preganglionic
avulsion proximal to dorsal root ganglion
involves CNS which does not regenerate – little potential recovery of motor function (poor
prognosis)
lesions suggesting preganglionic injury:
Horner’s syndrome
disruption of sympathetic chain
winged scapula medially
loss of serratus anterior (long thoracic nerve) leads to medial winging (inferior
border goes medial)
loss of rhomboids (dorsal scapular nerve) leads to lateral winging (superior medial
border drops downward and protrudes laterally and posteriorly)
presents with motor deRcits (bail arm)
both pre- and postganglionic lesions can present with bail arm
sensory absent
absence of a Tinel sign or tenderness to percussion in the neck
normal histamine test (C8-T1 sympathetic ganglion)
intact triple response (redness, wheal, bare)
elevated hemidiaphragm (phrenic nerve)
rhomboid paralysis (dorsal scapular nerve)
serratus anterior (long thoracic nerve)
normal sensory nerve action potential (SNAP)
evaluation
EMG may show loss of innervation to cervical paraspinals
postganglionic
involve PNS, capable of regeneration (better prognosis)
presentation
presents with motor deRcit (bail arm)
sensory deRcits
evaluation
EMG shows maintained innervation to cervical paraspinals
abnormal histamine test
only redness and wheal, but NO bare
ClassiRcation based on location
Upper Lesion: Erb's Palsy (C5,6)
Introduction Physical Exam
Most common obstetric brachial plexopathy Clinically, the arm will be adducted, internally rotated, at
Results from an excessive displacement of head to shoulder; pronated, extended at elbow (“waiter’s tip”)
opposite side and depression of shoulder on the same C5 deRciency
side producing traction on plexus. -axillary nerve deRciency (weakness in deltoid, teres
Occurs during a didcult delivery in infants or fall onto minor)
shoulder in adults -suprascapular nerve deRciency (weakness in
Best prognosis supraspinatus, infraspinatus)
-musculocutaneous nerve deRciency (weakness to
biceps)
C6 deRciency
-radial nerve deRciency (weakness in brachioradialis,
supinator)
Lower Lesion: Klumpke Palsy (C8,T1)
Introduction Physical Exam
Rare in obstetric palsy DeRcit of all of the small muscles of the hand (ulnar and
Usually avulsion injuries caused by excessive abduction median nerves)
(person falling from height clutching on an object to save Clinically, presents as “claw hand”
himself) -wrist held in extreme extension because of the
Other causes may include cervical rib, or lung mets in unopposed wrist extensors
lower deep cervical lymph nodes -hyperextension of MCP due to loss of hand intrinsics
Frequently associated with a preganglion injury and -bexion of IP joints due to loss of hand intrinsics
Horner's Syndrome
Poor prognosis
Total Palsy (C5-T1)
Introduction Physical Exam
A form of brachial plexopathy Leads to a baccid arm
Worst prognosis Involves both motor and sensory
PRESENTATION
History
high energy injury
Physical exam
Horner's syndrome
features include
drooping of the eyelid
pupillary constriction
anhidrosis
usually show up three days after injury
represents disruption of sympathetic chain via C8 and/or T1 root avulsions
severe pain in anesthetized limb
correlates with root avulsion
important muscles to test
serratus anterior (long thoracic nerve) and rhomboids (dorsal scapular nerve)
if they are functioning then it is more likely the C5 injury is postganglionic
pulses
check radial, ulnar and brachial pulses
arterial injuries common with complete BPIs
IMAGING
Radiographs
chest radiograph
recommended views
PA and lateral
fractures to the Rrst or second ribs suggest damage to the overlying brachial plexus
evidence of old rib fractures can be important if an intercostal nerve is needed for nerve transfer
inspiration and expiration can demonstrate a paralyzed diaphragm (indicates upper nerve root
injury)
cervical spine series
recommended views
AP and lateral
transverse process fracture likely indicates a root avulsion
scapular and shoulder series
recommended views
at least AP and axillary (or equivalent)
scapulothoracic dissociation is associated with root avulsion and major vascular injury
clavicle
recommended views
orthogonal views
fracture may indicate brachial plexus injury
CT myelography
indications
gold standard for deRning level of nerve root injury
avulsion of cervical root causes dural sheath to heal with meningocele
scan should be done 3-4 weeks after injury
allows blood clot in the injured area to dissipate and meningocele to form
MRI
indications
suspect injury is distal to nerve roots
can visualize much of the brachial plexus
CT/myelogram demonstrates only nerve root injury
Rndings
traumatic neuromas and edema
mass lesions in nontraumatic neuropathy of brachial plexus and its branches
consistent with injury include
pseudomeningocele (T2 highlights water content present in a pseudomeningocele )
empty nerve root sleeves (T1 images highlight fat content nerve roots and empty sleeves)
cord shift away from midline (T1 highlights fat of cord)
STUDIES
Electromyography (EMG)
tests muscles at rest and during activity
Rbrillation potentials (denervation changes)
as early as 10-14 days following injury in proximal muscles
as late as 3-6 weeks in distal muscles
can help distinguish preganglionic from postganglionic
examine proximally innervated muscles that are innervated by root level motor branches
rhomboids
serratus anterior
cervical paraspinals
Nerve conduction velocity (NCV)
performed along with EMG
measures sensory nerve action potentials (SNAPs)
distinguishes preganglionic from postganglionic
SNAPs preserved in lesions proximal to dorsal root ganglia
cell body found in dorsal root ganglia
if SNAP normal and patient insensate in ulnar nerve distribution
preganglionic injury to C8 and T1
if SNAP normal and patient insensate in median nerve distribution
preganglionic injury to C5 and C6
Nerve action potential (NAPs)
often intraoperative
tests a nerve across a lesion
if NAP positive across a lesion
preserved axons
or signiRcant regeneration
can detect reinnervation months before EMG
NAP negative-neuropraxic lesion
NAP positive- axonotmetic lesion
Sensory and Motor Evoked Potential
more sensitive than EMG and NCV at identifying continuity of roots with spinal cord (positive Rnding)
a negative Rnding can not differentiate location of discontinuity (root avulsion vs. axonotmesis)
perform 4-6 weeks after injury to allow for Wallerian degeneration to occur
stimulation done at Erb's point and recording done over cortex with scalp electrodes (transcranial)
TREATMENT
Nonoperative
observation alone waiting for recovery
indications
most managed with closed observation
guns shot wounds (in absence of major vascular damage can observe for three months)
signs of neurologic recovery
advancing Tinel sign is best clinical sign of effective nerve regeneration
Operative
immediate surgical exploration (< 1 week)
indications
sharp penetrating trauma (excluding GSWs)
iatrogenic injuries
open injuries
progressive neurologic deRcits
expanding hematoma or vascular injury
techniques
nerve repair
nerve grafting
neurotization
early surgical intervention (3-6 weeks)
indicated for near total plexus involvement and with high mechanism of energy
delayed surgical intervention (3-6 months)
indications
partial upper plexus involvement and low energy mechanism
plateau in neurologic recovery
best not to delay surgery beyond 6 months
techniques
usually involves tendon/muscle transfers to restore function
TECHNIQUES
Direct nerve repair
rarely possible due to traction and usually only possible for acute and sharp penetration injuries
Nerve graft
commonly used due to traction injuries (postganglionic)
preferable to graft lesions of upper and middle trunk
allows better chance of reinnervation of proximal muscles before irreversible changes at motor
end plate
donor sites include sural nerve, medial brachial nerve, medial antebrachial cutaneous nerve
vascularized nerve graft includes ulnar nerve when there is a proven C8 and T1 avulsion (mobilized on
superior ulnar collateral artery)
Neurotization (nerve transfer)
transfer working but less important motor nerve to a nonfunctioning more important denervated
muscle
use extraplexal source of axons
spinal accessory nerve (CN XI)
intercostal nerves
contralateral C7
hypoglossal nerve (CN XII)
intraplexal nerves
phrenic nerve
portion of median or ulnar nerves
pectoral nerve
Oberlin transfer
ulnar nerve used for upper trunk injury for biceps function
Muscle or tendon transfer
indications
isolated C8-T1 injury in adult (reinervation unlikely due to distance between injury site and hand
intrinsic muscles)
priorities of repair/reconstruction
elbow bexion (musculocutaneous nerve)
shoulder stability (suprascapular nerve)
brachial-thoracic pinch (pectoral nerve)
C6-C7 sensory (lateral cord)
wrist extension / Rnger bexion (lateral and posterior cords)
wrist bexion / Rnger extension
intrinsic function
technique
gracilis most common free muscle transfer
PROGNOSIS
Recovery of reconstructed plexus can take up to 3 years
nerve regeneration occurs at speed of 1mm/day
Good prognostic variables
infraclavicular plexus injuries have better prognosis than supraclavicular injuries
upper plexus injuries have improved prognosis
preservation of hand function
Poor prognostic variables
root avulsion (preganglionic injuries) have worst prognosis
not repairable
other surgeries such as arthrodesis and tendon transfers may be needed
Login
Please Login to add comment
ORTHO Bullets
TOPICS TECHNIQUES FEATURES PRODUCTS HELP
Trauma Trauma Cards PEAK & Study Plans FAQ
Spine Spine QBank PASS Platform Tutorial Vid…
Shoulder & Elbow Shoulder & Elbow Cases Self-Assessment Ex… PASS Tutorial Videos
Knee & Sports Knee & Sports Topics POCL FREE CME IPhone App
Pediatrics Pediatrics Evidence Price Chart Android App
Recon Recon Posts Contact Us
Hand Hand Videos
Foot & Ankle Foot & Ankle Events Facebook YouTube
Pathology Pathology
Twitter LinkedIn
Basic Science Approaches
TikTok Instagram
Anatomy
BULLET HEALTH Company Our Team Privacy Policy Terms of Use
© 2023 Lineage Medical, Inc. All rights reserved
You might also like
- 2-HEAD AND NECK PrintDocument30 pages2-HEAD AND NECK Printsaddam hussain100% (1)
- Data Legacy InsuranceCos SourceRSDocument48 pagesData Legacy InsuranceCos SourceRSrishu1527No ratings yet
- Brain Death Death by Neurologic Criteria.15Document21 pagesBrain Death Death by Neurologic Criteria.15Anusha PervaizNo ratings yet
- Pa Tho Physiology of Spinal Cord InjuryDocument1 pagePa Tho Physiology of Spinal Cord InjuryGenel Joseph Jacildo Peñaflor100% (2)
- Neuromyelitis Optica Spectrum Disorder and Other.15Document30 pagesNeuromyelitis Optica Spectrum Disorder and Other.15Doaa Mokhtar100% (1)
- Readers Digest Asia Feburary 2021Document134 pagesReaders Digest Asia Feburary 2021FURY FURIONNo ratings yet
- How May I Make My Penis More Robust? Answer That NowDocument2 pagesHow May I Make My Penis More Robust? Answer That NowEsbensen59TRUENo ratings yet
- CXC Csec English A June 2015 p1Document16 pagesCXC Csec English A June 2015 p1Rihanna Johnson100% (1)
- Chronic Traumatic Encephalopathy.12Document21 pagesChronic Traumatic Encephalopathy.12wmtxbbNo ratings yet
- Uworld RationalesDocument2 pagesUworld RationalesMelissa Sapp67% (3)
- Ataxia 10Document19 pagesAtaxia 10Cristina GhizdavetNo ratings yet
- Chapter 2 Fire Fighter SafetyDocument2 pagesChapter 2 Fire Fighter SafetyMuhammad Alshikh100% (1)
- List of CosmeticsDocument9 pagesList of Cosmeticsasit_m0% (1)
- Wastemanagement 161028065024Document80 pagesWastemanagement 161028065024Atharva MansabdarNo ratings yet
- Management of Cerebral Edema, Brain Compression,.4Document29 pagesManagement of Cerebral Edema, Brain Compression,.4Jorge MontenegroNo ratings yet
- Cluster Headache and Other Trigeminal Autonomic CephalalgiasDocument19 pagesCluster Headache and Other Trigeminal Autonomic CephalalgiasBryan100% (1)
- PMDC Community Medicine Mcqs PDFDocument280 pagesPMDC Community Medicine Mcqs PDFJay KNo ratings yet
- Brochure Philippine Laws On Environmental PollutionDocument8 pagesBrochure Philippine Laws On Environmental PollutionElvin JuniorNo ratings yet
- Flygt IOM 3152-181Document56 pagesFlygt IOM 3152-181veromesa0% (1)
- Acetabular Fractures - Trauma - OrthobulletsDocument1 pageAcetabular Fractures - Trauma - OrthobulletsAlfonsoSalvadorLopezNo ratings yet
- Brain Atlas of Human Anatomy With MRIDocument1 pageBrain Atlas of Human Anatomy With MRIBerk HalilbeyoğluNo ratings yet
- Spinal Anesthesia in Pediatric Patients: ArticleDocument11 pagesSpinal Anesthesia in Pediatric Patients: ArticlenurfitriaNo ratings yet
- Cerebral Vasospasme After Traumatic Brain InjuryDocument10 pagesCerebral Vasospasme After Traumatic Brain Injurydavid wyantoNo ratings yet
- Neoplastic Myelopathies: Continuumaudio Interviewavailable OnlineDocument22 pagesNeoplastic Myelopathies: Continuumaudio Interviewavailable OnlineDalwadi1No ratings yet
- Alternatif 2 PDFDocument1 pageAlternatif 2 PDFMaxwell CollegeNo ratings yet
- 4250 Lec21 15Document10 pages4250 Lec21 15Carlos Enrique Pijo PerezNo ratings yet
- Imaging The Anatomy of The Brachial Plexus: Review And: Self-Assessment ModuleDocument9 pagesImaging The Anatomy of The Brachial Plexus: Review And: Self-Assessment ModuleAjversonNo ratings yet
- Neurologic Complications of Lyme Disease: Review ArticleDocument11 pagesNeurologic Complications of Lyme Disease: Review ArticleHenry DanielNo ratings yet
- AJR Teaching File: Intraventricular Mass: Clinical HistoryDocument4 pagesAJR Teaching File: Intraventricular Mass: Clinical HistoryDokdem AjaNo ratings yet
- Evaluation of Total Corneal Power MeasurementsDocument7 pagesEvaluation of Total Corneal Power MeasurementsMariana Luzardo bravoNo ratings yet
- Nidya Luluk Koleb PDFDocument1 pageNidya Luluk Koleb PDFMaxwell CollegeNo ratings yet
- DW M8推荐书Document6 pagesDW M8推荐书NAYAN PATELNo ratings yet
- Head and Spine Injuries: Life Supporting FunctionsDocument34 pagesHead and Spine Injuries: Life Supporting FunctionskasreedharNo ratings yet
- Basal Nuclei and ConnectionsDocument27 pagesBasal Nuclei and ConnectionsZoya MoraniNo ratings yet
- Colin Wilhelm, Marcus Del Bianco, Siavash Mojibian, Minkyung Kim, Grant MastickDocument1 pageColin Wilhelm, Marcus Del Bianco, Siavash Mojibian, Minkyung Kim, Grant MastickColin WilhelmNo ratings yet
- Musculo TemporalDocument4 pagesMusculo TemporalSimón Pérez LópezNo ratings yet
- Brain Stem 2 w4Document7 pagesBrain Stem 2 w4ZED AlanaziNo ratings yet
- Recovery From Post-Stroke AphasiaDocument7 pagesRecovery From Post-Stroke AphasiaMoileon2011No ratings yet
- Regional Anesthesia For Scapular Fracture Surgery: An Educational Review of Anatomy and TechniquesDocument6 pagesRegional Anesthesia For Scapular Fracture Surgery: An Educational Review of Anatomy and TechniquesSean SmythNo ratings yet
- Brain CirculationDocument1 pageBrain CirculationNoisy KenNo ratings yet
- Magnetic Resonance Imaging of The Temporomandibular Joint: Michelle A. Wessely, Martin F YoungDocument8 pagesMagnetic Resonance Imaging of The Temporomandibular Joint: Michelle A. Wessely, Martin F YoungrewassallfotosNo ratings yet
- Neuropathy HistopathologyDocument1 pageNeuropathy HistopathologyJesse ChusidNo ratings yet
- Acute Intestinal Distress Syndrome: The Importance of Intra-Abdominal PressureDocument17 pagesAcute Intestinal Distress Syndrome: The Importance of Intra-Abdominal PressureAndrea Melo RualesNo ratings yet
- Leptomeningeal Enhancement Radiology Reference ArticleDocument1 pageLeptomeningeal Enhancement Radiology Reference ArticleRabi Phui-onNo ratings yet
- Intradural Spinal Cord Tumors: UpplementDocument1 pageIntradural Spinal Cord Tumors: Upplementlauzark gashbellNo ratings yet
- Kagramian Fshd-PosterDocument1 pageKagramian Fshd-Posterapi-700030358No ratings yet
- Sedation in Neurocritical Patients: Is It Useful?: ReviewDocument7 pagesSedation in Neurocritical Patients: Is It Useful?: ReviewAditiaPLNo ratings yet
- Dolor Crónico - ResumenDocument26 pagesDolor Crónico - ResumenLuis Torres QuesadaNo ratings yet
- Suprapatellar Nailing of Tibial Fractures .21Document6 pagesSuprapatellar Nailing of Tibial Fractures .21Guna NikhilNo ratings yet
- 7-Vertigo Related To Central Nervous System.-CompressedDocument21 pages7-Vertigo Related To Central Nervous System.-CompressedOlga Manco GuzmánNo ratings yet
- Trigeminal - Neuralgia 2Document25 pagesTrigeminal - Neuralgia 2FKUPR 2017No ratings yet
- Endo Logbook FormsDocument3 pagesEndo Logbook FormsAmethystVonNo ratings yet
- Spinal Cord InjuriesDocument76 pagesSpinal Cord InjuriesSuji Merline100% (2)
- Magnetic Resonance Imaging of The Shoulder: C T S DDocument16 pagesMagnetic Resonance Imaging of The Shoulder: C T S DJuan PagesNo ratings yet
- Disorders of The Spinal Cord and RootsDocument9 pagesDisorders of The Spinal Cord and RootsMariana Hoyos GallegoNo ratings yet
- Acute Treatment of Patients With SpinalDocument76 pagesAcute Treatment of Patients With SpinalAzmi FarhadiNo ratings yet
- Ajr 08 1316Document9 pagesAjr 08 1316EdsonR GhNo ratings yet
- Brachial Plexus Injury LatestDocument37 pagesBrachial Plexus Injury LatestRajhmuniran KandasamyNo ratings yet
- Repetitive Transcranial Magnetic Stimulation For Neuropsychiatric DisordersDocument7 pagesRepetitive Transcranial Magnetic Stimulation For Neuropsychiatric DisordersMuskaan KhannaNo ratings yet
- Neuropathic Pain in Daily Practice: Teddy Wijatmiko, DR - SP.SDocument52 pagesNeuropathic Pain in Daily Practice: Teddy Wijatmiko, DR - SP.SeciNo ratings yet
- 01.01. Cellular Response To InjuryDocument15 pages01.01. Cellular Response To InjuryMiguel C. DolotNo ratings yet
- 21436-Vascular Anatomy - VilelaDocument12 pages21436-Vascular Anatomy - VilelaashleyNo ratings yet
- Material Docent Temes 2 I 3 PDFDocument2 pagesMaterial Docent Temes 2 I 3 PDFFlorian TubertNo ratings yet
- Spinal Cord Herniation Why Anterior ThoracicDocument5 pagesSpinal Cord Herniation Why Anterior ThoracicShahid KhanNo ratings yet
- Cuts Poster JB Cfs 2Document1 pageCuts Poster JB Cfs 2api-465519286No ratings yet
- Feigl 2020Document8 pagesFeigl 2020eralp cevikkalpNo ratings yet
- 1 s2.0 S1878875019327561 MainDocument21 pages1 s2.0 S1878875019327561 MainandresNo ratings yet
- Anxitatea Periop - Review - 2018Document11 pagesAnxitatea Periop - Review - 2018Fiorel Loves EveryoneNo ratings yet
- 10 23736@S1973-9087 17 04749-9Document8 pages10 23736@S1973-9087 17 04749-9Kings AndrewNo ratings yet
- The Anatomical Foundations of Regional Anesthesia and Acute Pain MedicineFrom EverandThe Anatomical Foundations of Regional Anesthesia and Acute Pain MedicineNo ratings yet
- Compressive Neuropathies of the Upper Extremity: A Comprehensive Guide to TreatmentFrom EverandCompressive Neuropathies of the Upper Extremity: A Comprehensive Guide to TreatmentDean G. SotereanosNo ratings yet
- Psychological Communication Barriers PosterDocument1 pagePsychological Communication Barriers PostereliyaziyaNo ratings yet
- Hba1C: Quality System CertifiedDocument4 pagesHba1C: Quality System CertifiedNonameNo ratings yet
- Respaper 1Document48 pagesRespaper 1Xayezi AblenNo ratings yet
- Research Proposal-1Document28 pagesResearch Proposal-1sowsthikaNo ratings yet
- Bahasa Inggris Swot Madam Gie Sweet Cheek BlushedDocument8 pagesBahasa Inggris Swot Madam Gie Sweet Cheek Blushedanon_681594518No ratings yet
- HSC 430 - Lesson Plan Underage DrinkingDocument11 pagesHSC 430 - Lesson Plan Underage Drinkingapi-487139726No ratings yet
- Gases Toxicos Irritantes PDFDocument6 pagesGases Toxicos Irritantes PDFLUIS ANDRES JUAREZ CALLENo ratings yet
- Sensory Design of Easy-To-Chew Food For Elderly: - Ingredients and Manufacturing Conditions With Focus On Meat and CarrotDocument23 pagesSensory Design of Easy-To-Chew Food For Elderly: - Ingredients and Manufacturing Conditions With Focus On Meat and CarrotCaguioa Mark Anthony G.No ratings yet
- Direct Black 22Document4 pagesDirect Black 22DHRUVNo ratings yet
- Liver Vascular Anatomy - A RefresherDocument10 pagesLiver Vascular Anatomy - A Refresherilham nugrohoNo ratings yet
- ODMP Sustainable Livestock Management - Watering Points Appendix 1 - Borehole DataDocument35 pagesODMP Sustainable Livestock Management - Watering Points Appendix 1 - Borehole DataAse JohannessenNo ratings yet
- NFPA Review of The Incident by Ken MastrulloDocument3 pagesNFPA Review of The Incident by Ken MastrullotatacpsNo ratings yet
- Étude de La Prévalence Et de L'incidence Du Cancer de La Prostate Dans Le Nord Cameroun: Coût Et Prise en ChargeDocument8 pagesÉtude de La Prévalence Et de L'incidence Du Cancer de La Prostate Dans Le Nord Cameroun: Coût Et Prise en ChargeHerve KadaNo ratings yet
- (OSHPD 1, 2, 3 & 4) See Sections 404.0 Through 418.0. (SFM) Air Filters Shall Comply With All Requirements ofDocument0 pages(OSHPD 1, 2, 3 & 4) See Sections 404.0 Through 418.0. (SFM) Air Filters Shall Comply With All Requirements ofOanh NguyenNo ratings yet
- Jonsen 4 Box MethodDocument5 pagesJonsen 4 Box MethodsawsanNo ratings yet
- Surat Permintaan Obat Dinkes BaruDocument21 pagesSurat Permintaan Obat Dinkes BaruHafizh JhunkoNo ratings yet
- Moth Balls: Safety Data SheetDocument9 pagesMoth Balls: Safety Data SheethafilrediandikaNo ratings yet
- KP Astrology Rules of PredictionDocument4 pagesKP Astrology Rules of PredictionRajeshNo ratings yet