Professional Documents
Culture Documents
Polymyalgia Rheumatica - Lancet (2023)
Uploaded by
1DMANUEL Suarez MejiaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Polymyalgia Rheumatica - Lancet (2023)
Uploaded by
1DMANUEL Suarez MejiaCopyright:
Available Formats
www.memodiapp.
com
Seminar
Polymyalgia rheumatica
Georgina Espígol-Frigolé, Christian Dejaco, Sarah L Mackie, Carlo Salvarani, Eric L Matteson, Maria C Cid
Polymyalgia rheumatica is an inflammatory disease producing pain and stiffness, mainly in the shoulders and pelvic Lancet 2023; 402: 1459–72
girdle, in people older than 50 years. Elevation of acute phase reactants is common due to the inflammatory nature of Published Online
the disease. Since there are no specific diagnostic tests, diagnosis requires the exclusion of other diseases with similar October 10, 2023
https://doi.org/10.1016/
presentations. Imaging has helped to identify the pathological substrate of polymyalgia rheumatica and it is
S0140-6736(23)01310-7
increasingly used to support clinical diagnosis or to detect coexistent giant cell arteritis. Although polymyalgia
Department of Autoimmune
rheumatica does not clearly impair survival or organ function, it can have a detrimental effect on quality of life. Diseases, Hospital Clínic de
Glucocorticoids at 12·5–25·0 mg prednisone per day are effective in inducing remission in most individuals but, Barcelona, Barcelona, Spain
when tapered, relapses occur in 40–60% of those affected and side-effects are common. Assessment of disease activity (G Espígol-Frigolé MD,
Prof M C Cid MD); Department
can be difficult because pain related to common comorbidities such as osteoarthritis and tendinopathies, can return
of Medicine, University of
when glucocorticoids are reduced, and acute phase reactants are increased less during flares in individuals undergoing Barcelona, Barcelona, Spain
treatment or might increase for other reasons. The role of imaging in assessing disease activity is not yet completely (G Espígol-Frigolé, Prof M C Cid);
defined. In the search for more efficient and safer therapies, tocilizumab and sarilumab have shown efficacy in Institut d’Investigacions
Biomèdiques August Pi i
randomised controlled trials and additional targeted therapies are emerging. However, judicious risk–benefit balance
Sunyer (IDIBAPS), Barcelona,
is essential in applying therapeutic innovations to people with polymyalgia rheumatica. Spain (G Espígol-Frigolé,
Prof M C Cid); Department of
Introduction rheumatica is about three times more common than Rheumatology, Medical
University Graz, Graz, Austria
Polymyalgia rheumatica is a chronic inflammatory giant cell arteritis and about 75% of people with the (C Dejaco MD); Department of
disease involving the periarticular structures of the condition are women.4 Almost all people with polymyalgia Rheumatology, Hospital of
proximal joints almost exclusively in individuals older rheumatica are older than 50 years, and the prevalence of Brunico (SABES-ASDAA),
than 50 years. Polymyalgia rheumatica is clinically the disease is highest among people aged 70–80 years.4 Teaching Hospital of the
Paracelsus Medical University,
characterised by pain and stiffness in the neck, shoulders, As with giant cell arteritis, there is a north–south gradient Brunico, Italy (C Dejaco); Leeds
and pelvic girdle along with systemic symptoms and in the northern hemisphere, with the highest incidence, Institute of Rheumatic and
elevation of acute phase reactants.1,2 Diagnosis and ranging from 41 to 113 cases per 100 000 people aged Musculoskeletal Medicine,
classification of polymyalgia rheumatica is mainly based 50 years and older, in Scandinavia.5 The reason for this University of Leeds, Leeds, UK
(S L Mackie MD); Leeds
on clinical grounds and requires careful evaluation to distribution is unknown but genetic and environmental Biomedical Research Centre,
exclude other diseases. Several imaging modalities can factors might contribute. Differences in reported Leeds Teaching Hospitals NHS
be increasingly useful to clinicians during the diagnostic incidences can also be confounded by socioeconomic Trust, Leeds, UK (S L Mackie);
process.3 Glucocorticoids in the medium-dose range are factors. A population-based study from Olmsted County, Division of Rheumatology,
Azienda USL-IRCCS di Reggio
still the mainstay of treatment since the efficacy of Emilia, Reggio Emilia, Italy
immunosuppressive drugs as glucocorticoid-sparing (C Salvarani MD); Azienda
agents remains controversial.1–3 Trials published in the Search strategy and selection criteria Ospedaliera-Universitaria di
past couple of years indicate that targeted therapies will Modena, University of Modena
We searched PubMed for articles published in English from and Reggio Emilia, Reggio
soon expand the therapeutic horizon for people with database inception to May 31, 2023, using the term Emilia, Italy (C Salvarani);
polymyalgia rheumatica. Disease activity and remission “polymyalgia rheumatica” AND “epidemology”, Division of Rheumatology,
are still difficult to assess because comorbidities, “pathophysiology”, “pathogenesis”, “clinical symptoms”,
Mayo Clinic College of Medicine
and Science, Rochester, MN,
common in older adults, can produce mimicking “clinical findings”, “laboratory findings”, “blood test”, USA (Prof E L Matteson MD)
symptoms. Although polymyalgia rheumatica is not in “abnormalities”, “diagnosis”, “classification”, “imaging”, “giant- Correspondence to:
itself a life-threatening disease or destructive condition cell arteritis”, “immune mediated diseases”, “autoimmune Prof Maria C Cid, Department of
leading to irreversible joint or organ damage, side-effects diseases”, “treatment”, “glucocorticoids”, “immunosuppressive Autoimmune Diseases, Hospital
from chronic glucocorticoid treatment are common in drugs”, “biologic agents”, “targeted therapies”, “disease
Clínic de Barcelona,
these individuals.3 Barcelona 08036, Spain
activity”, “relapses”, or “outcome measures”. Special emphasis mccid@clinic.cat
This Seminar aims to provide an updated general was invested in articles published in the past 5 years, but some
overview of polymyalgia rheumatica, with special focus relevant older publications highly regarded or not completely
on consolidated aspects of the underlined points and on covered by more recent publications were also included.
advances made over the past 5 years. Reference lists of papers were also considered. Articles judged
more relevant to the topics covered were selected by the
Epidemiology authors. Among those, randomised controlled trials,
Polymyalgia rheumatica is among the most common prospective studies, or studies with a larger population sample
inflammatory rheumatic diseases in older adults (aged size than similar studies were preferred. Originality and clarity
≥ 50 years). The epidemiology of polymyalgia rheumatica were also considered. Due to space limitations, some relevant
is difficult to investigate because of the absence of contributions had to be omitted. Abstracts were not included
specific diagnostic tests, and the overlapping spectrum of in the main text.
the disease with giant cell arteritis. However, polymyalgia
www.thelancet.com Vol 402 October 21, 2023 www.memodiapp.com 1459
www.memodiapp.com
Seminar
MN, USA reported an incidence of 63·9 cases per 100 000 extrapolated to polymyalgia rheumatica. It is assumed that
per year and a prevalence of 701 cases per 100 000 people ageing, genetics, and innate and adaptive immune
older than 50 years.4 A much lower incidence is detected mechanisms against unknown triggers play a role.20,21 The
in southern Europe with an incidence rate of influence of ageing, supported by polymyalgia rheumatica
13 cases per 100 000 per year reported in Italy6 and demography, has been scarcely investigated. Increased
13·52 cases per 100 000 per year in Spain.7 A study from numbers of immunosenescent, autoreactive cells have
Buenos Aires in Argentina, discloses an incidence and been detected in peripheral blood from people with
prevalence similar to Europe8 and the incidence of polymyalgia rheumatica or with giant cell arteritis.22
polymyalgia rheumatica in South Korea has been Abnormalities in innate immune response have been also
reported as 2·06 cases per 100 000, with a prevalence of reported and include altered pattern of toll-like receptor
8·21 cases per 100 000 in 2012.9 Polymyalgia rheumatica expression in peripheral blood mononuclear cells,23,24
does not clearly affect life expectancy.10,11 neutrophil activation,12 and phagocyte dysfunction.24 Like
giant cell arteritis, polymyalgia rheumatica risk is
Pathophysiology increased in individuals carrying HLA-DRB1.04 or
The pathogenesis of polymyalgia rheumatica is incom HLA-DRB1.01 alleles,25–27 supporting the role of adaptive
pletely understood (figure 1). Polymyalgia rheumatica immune mechanisms in its pathogenesis. However, this
shares demographic and peripheral blood abnormalities association has been less consistent than in giant cell
with giant cell arteritis, suggesting common pathogenic arteritis, possibly because the classification of polymyalgia
mechanisms eventually targeting different tissues rheumatica relies on clinical assessment with no specific
(eg, synovial structures, arteries, or both). Immuno tests and polymyalgia rheumatica cohorts can be
pathologic studies are much more abundant in giant cell heterogeneous.
arteritis than in polymyalgia rheumatica due to the easy As with giant cell arteritis, most people with active
availability of tissue (via temporal artery biopsy), polymyalgia rheumatica have a remarkable acute phase
commonly obtained for diagnosis. Consequently, some response, increased production of IL-6 by circulating
pathogenetic principles of giant cell arteritis are frequently monocytes, and elevated serum concentrations of
Peripheral blood compartment Tissue
Th17 compartment
Subacromial
cytokines bursa
Monocytes Th17
IL-6 lymphocyte
Macrophages
GM-CSF
Tc1
lymphocyte
IL-6 IFN-γ
IFN-γ
Activated
neutrophil Adhesion
molecule
Decrease in
regulatory T cells and in
Th1 CD8+ T lymphocytes* IFN-γ
lymphocyte and B lymphocytes* Th17
lymphocyte? Neovessels
Autoreactive
T cells Th1
lymphocyte
Figure 1: Pathophysiological clues derived from immunopathological studies in polymyalgia rheumatica
Clues to polymyalgia rheumatica pathogenesis are derived from observational studies performed with peripheral blood, synovial fluid, and synovial tissue. The left
panel shows changes identified by several authors in the distribution of cell subsets in peripheral blood, indicating neutrophil activation,12 an increase in Th1 and Th17
lymphocytes, and a decrease in B lymphocytes and regulatory T lymphocytes.13–15 Increased IL-6 concentrations might drive the systemic inflammatory response
typically found in most patients. In synovial tissue (right panel), expression of cytokines related to myeloid cell activation (ie, GM-CSF), Th1 (ie, IFNg) and Th17
differentiation (ie, IL-6) have been observed.16,17 Macrophages are also present, as well as neovessels expressing adhesion molecules that could contribute to
additional inflammatory cell recruitment.16–19 GM-CSF=granulocyte-macrophage colony-stimulating factor. Tc1=T-cytotoxic-type 1 cell. Th1=T-helper-type 1 cell.
Th17= T-helper-type 17 cell. *Changes in CD8+ lymphocytes remain controversial.
1460 www.memodiapp.com www.thelancet.com Vol 402 October 21, 2023
www.memodiapp.com
Seminar
IL-6.28–30 Other abnormalities detected in peripheral blood referred to as remitting seronegative symmetric synovitis
include a decrease in CD8+ T lymphocytes and with pitting oedema (RS3PE) syndrome, reflects
B lymphocytes, an increase in T lymphocytes producing prominent distal tenosynovitis of the extensor tendons of
T-helper-type 1 (Th1) and 17 (Th17) cytokines, and a hands or feet, variably associated with joint synovitis, and
decrease in regulatory T cells.13–15 These changes are can be the main reason for the peripheral inflammatory
usually less prominent than in giant cell arteritis.13–15 symptoms and subcutaneous oedema.33,34 However,
Tissue studies are scarce16–19 but, as with giant cell RS3PE is not exclusive to polymyalgia rheumatica. Carpal
arteritis, recent observational immuno pathological tunnel syndrome due to tenosynovitis of wrist flexors has
studies have shown expression of cytokines related to been observed in 14% of patients.33
Th1 and Th17 pathways in involved tissue (figure 1).16,17
Laboratory abnormalities
Clinical manifestations Laboratory findings are non-specific but indicate the
Polymyalgia rheumatica is clinically characterised by inflammatory nature of polymyalgia rheumatica: elevated
aching and stiffness in the neck, torso, shoulders, and erythrocyte sedimentation rate (ESR) and C-reactive
pelvic girdle, the so called polymyalgic syndrome.31 The protein (CRP), normochromic normocytic anaemia,
onset is often sudden, but full clinical features can take thrombocytosis, hypoalbuminaemia, elevated fibrinogen
several days to develop. Stiffness can predominate in the levels, and raised α2 globulin proteins are commonly
morning but can extend to the entire day and aching detected.1,3 Both ESR and CRP should be requested.
interferes with night sleep. Bilateral shoulder pain Elevated ESR (at least 40 mm/h) has been included in
radiating distally towards the elbows is the most common all sets of classification criteria for polymyalgia
manifestation in most people with polymyalgia rheumatica.32,35–40 but a nearly normal ESR does not
rheumatica (70–95%), whereas neck and hip girdle pain completely exclude diagnosis, as low ESR has been
are less frequent (50–70%).1,31,32 Pelvic girdle pain is reported in 7–20% of people with polymyalgia
reported along the groin and lateral aspects of the hips, rheumatica.1 CRP is nearly always elevated in untreated
and frequently radiates to the posterior aspect of the polymyalgia rheumatica, with concentrations greater
thighs and knees. Although it can begin in one shoulder than 0·5 mg/dL in 99% of individuals at diagnosis.41,42
or hip, in the vast majority of cases it soon becomes Thus, a normal ESR and CRP are infrequent and require
bilateral.1,31,32 On examination, people with polymyalgia referral to exclude mimicking conditions, as the
rheumatica have painful and restricted range of active diagnosis of polymyalgia rheumatica is unlikely.41,42
and often passive movements of the shoulders and hips, Autoantibodies, including antinuclear antibodies, anti-
without detectable proximal joint swelling, and with cyclic citrullinated peptide antibodies and rheumatoid
tenderness upon compressing the upper part of the factor are typically negative; however, in approximately
extremities. A typical finding in people with polymyalgia 10% of older adults rheumatoid factor can be non-
rheumatica is the inability to actively abduct the specifically positive, usually at low titre.43 These tests are
shoulders past 90 degrees. Muscle weakness can be helpful in patients in whom mimicking inflammatory
difficult to explore in symptomatic individuals but is not rheumatic diseases can be considered (table 1).
a characteristic feature of initial polymyalgia rheumatica.
However, recurrent disease and glucocorticoid treatment Diagnosis and classification
can eventually decrease muscle trophism and strength. Clinical diagnosis
Systemic manifestations such as low-grade fever, The diagnosis of polymyalgia rheumatica is based on
depression, fatigue, anorexia, and weight loss occur in up clinical grounds and the exclusion of other diseases that
to 40% of people with polymyalgia rheumatica.1,31,32 High, can present with the polymyalgic syndrome (table 1).39,40
spiking fevers are uncommon in polymyalgia rheumatica Accordingly, the diagnosis of polymyalgia rheumatica
in the absence of giant cell arteritis.1,31,32 conveys a substantial uncertainty and requires expertise to
About 50% of people with polymyalgia rheumatica avoid overdiagnosis or underdiagnosis.44,45 Rheumatic
have distal musculoskeletal manifestations.33–35 (both inflammatory and non-inflammatory) diseases can
Specifically, one quarter of individuals with the condition present with similar symptoms and are the most common
have pain and swelling in the knees (40%) and diseases mimicking polymyalgia rheumatica. Typical
wrists (40%).33–35 Involvement of the metacarpophalangeal polymyalgia rheumatica manifes tations and even
joints is less common, but not exceptional, as suggestive ultrasound findings can develop in people with
25% of all patients have peripheral arthritis mimicking late-onset rheumatoid arthritis.40 Calcium pyrophosphate
other rheumatic diseases.33 In contrast to rheumatoid deposition disease and—less frequently—spondylo
arthritis, the arthritis is asymmetric, and non-erosive. arthropathies or late-onset systemic lupus erythematosus
Finally, diffuse distal extremity swelling with pitting can also present with the polymyalgic syndrome. Other
oedema mostly over the dorsum of the hands and wrists, diseases (ie, malignancies, infections, endocrinopathies,
but also over the ankles and tops of the feet, is seen in or neurodegenerative disorders) can occasionally mimic
around 8–12% of patients.33,34 This condition, often polymyalgia rheumatica. Important clinical clues pointing
www.thelancet.com Vol 402 October 21, 2023 1461
www.memodiapp.com
Seminar
Clinical clues Actions and tests
Step 1: identification of the polymyalgic syndrome
Patient consultation because of aching New onset of pain and stiffness in the upper and sometimes lower Detailed history and examination; ESR and CRP
girdles
Step 2: exclusion of mimicking diseases with appropriate tests or specialist referral
Inflammatory rheumatic diseases with typical joint involvement
Late-onset rheumatoid arthritis Symmetrical distal peripheral arthritis and erosions Anti-cyclic citrullinated peptides, rheumatoid factor; imaging*
Late-onset spondylarthritis Inflammatory low-back pain and stiffness, and enthesitis Imaging
Late-onset systemic lupus erythematosus Systemic manifestations (eg, skin and serositis) Antinuclear antibodies, anti-dsDNA, other autoantibodies,
complement
Calcium pyrophosphate deposition disease† Knee and wrist involvement; dens axis also frequently involved Imaging; synovial fluid examination (presence of crystals)
Inflammatory rheumatic diseases with predominant systemic involvement
Inflammatory myopathies Weakness and myalgia predominate, no clear stiffness, and systemic Creatine kinase, autoantibodies; electromyogram; muscle MRI;
involvement (eg, skin and lung) and muscle biopsy
Systemic vasculitis other than giant cell Myalgia predominates over stiffness and systemic involvement Urinalysis, anti-neutrophil cytoplasmic antibodies detection,
arteritis (eg, skin; kidney; lung; ear, nose, and throat; and peripheral neuropathy) cryoglobulins, complement; electromyogram; imaging; and biopsy
of involved sites
Non-inflammatory rheumatic diseases
Osteoarthritis† Mechanical pain, stiffness, or deformities Physical examination; ESR and CRP‡ (not elevated); imaging
Tendinopathies† Mechanical pain and limited range of motion Physical examination and imaging
Chronic pain syndromes† Long-lasting, diffuse, non-inflammatory pain without objective clinical Physical examination and imaging; ESR and CRP‡ (not elevated)
signs and with trigger points and fatigue
Other
Malignancies (eg, multiple myeloma and Widespread pain and no stiffness; focal manifestations of the primary Blood tests guided by clinical assessment: marked elevation of ESR
bone metastasis) tumour; and systemic features compared with CRP; hepatic function, LDH, and protein
electrophoresis and immunofixation; tumour markers; and imaging
(PET-CT), endoscopy (to rule out gastrointestinal or lung
malignancies, when contextually indicated), and biopsies
Subacute and chronic infections (eg, Fever, systemic features, focal manifestations (eg, new heart murmur, Cultures and serology; procalcitonin; arthrocentesis; imaging,
endocarditis, septic arthritis) skin lesions, back pain, mono-articular arthritis); marked elevation of as guided by clinical assessment
CRP compared with ESR
Neurodegenerative (eg, Parkinson’s disease Gradual onset, stiffness with weakness and muscle atrophy, rather than No elevation of ESR and CRP‡; specialist evaluation
and amyotrophic lateral) pain; other neurological features (eg, gait disturbance, hyperreflexia,
clonus, muscle fibrillation, tremor)
Drug-induced myopathy Intake of a potentially myopathic drug (ie, statins); myalgia Creatine kinase, anti-HMGCR antibodies, and muscle biopsy
and weakness predominate in selected cases
Endocrinopathies (eg, thyroid disease and Weakness more prominent than pain; other features of hyperthyroidism APR can be elevated in hyperthyroidism; creatine kinase and
hyperparathyroidism) (eg, tremor, tachycardia, diarrhoea, weight loss) or hypothyroidism transaminases can be elevated, thyroid-stimulating hormone,
(eg, bradycardia, constipation, weight gain) calcium and phosphorous, and parathyroid hormone
Osteomalacia Diffuse pain and weakness Vitamin D; imaging
Step 3: exclusion of giant cell arteritis
People with features that could suggest giant Cranial symptoms, extremity claudication, temporal artery APR highly elevated or temporal artery biopsy; imaging of cranial
cell arteritis abnormalities, marked systemic symptoms vessels, large-vessel imaging, or both
Step 4: specialist referral
Diagnostic uncertainty: alternative diagnosis Age <60 years; chronic onset (>2 months); lack of shoulder involvement; Tests guided by clinical clues; normal or extremely elevated APR
(same as previous step) lack of inflammatory stiffness; prominent weakness; marked systemic
features; coexisting, potentially confounding, comorbidities; features
of other rheumatic diseases; suspicion of giant cell arteritis; and
incomplete, poorly sustained, or no response to glucocorticoids
Treatment optimisation for polymyalgia Inability to reduce glucocorticoids due to relapsing disease, Differentiating active disease from comorbidities,
rheumatica contraindications to glucocorticoids therapy, early glucocorticoids immunosuppressive treatment, targeted therapies, and inclusion in
side-effects, and need for long-term glucocorticoids (>2 years) clinical trials
This table is based on expert opinion. APR=acute phase reactants. CRP=C-reactive protein. dsDNA=double-stranded DNA. ESR=erythrocyte sedimentation rate. *Imaging: x-ray, ultrasound, MRI or PET-CT, as
contextually indicated. †Might coexist with polymyalgia rheumatica. ‡Common comorbidities in older adults (aged ≥50 years) could independently produce mild elevation of these markers (ie, mild infection
and anaemia of any cause).
Table 1: Stepwise approach to the diagnosis of polymyalgia rheumatica
towards polymyalgia rheumatica are the presence of weakness, rigidity, constitutional symptoms, or multi-
proximal inflammatory pain and stiffness along with organ involvement are more prominent than pain,
elevation of acute phase reactants. When features such as physicians should be alert to alternative diagnoses, such
1462 www.thelancet.com Vol 402 October 21, 2023
www.memodiapp.com
Seminar
as muscle disorders, neurodegenerative diseases, or Biceps tenosynovitis Subdeltoid bursitis
malignancies (table 1). Conversely, widespread pain or
peripheral joint involvement might suggest metastasis or A B
myeloma or other rheumatic diseases, respectively.
Normal or very high levels of acute phase reactants are not
typical of polymyalgia rheumatica and should prompt
referral for consideration of other diseases. Clinically
guided blood tests and imaging as detailed in table 1 are *
useful for the diagnosis of polymyalgia rheumatica and
exclusion of other conditions. Physicians should be aware
that features of other diseases could also emerge during
follow-up.
C D
Role of imaging
Imaging in its various modalities (eg, ultrasound, MRI,
[¹⁸F]fluorodeoxyglucose [¹⁸FDG]-PET, or ¹⁸FDG-PET-CT
for better anatomic reference) has greatly contributed to
identifying the pathological substrate of polymyalgia
rheumatica. Ultrasound findings increase the specificity
of classification criteria (see next section) and can be
useful in primary care to substantiate findings suggestive
of polymyalgia rheumatica or to detect potentially
confounding diseases such as tendinopathies or crystal
deposition diseases.40 Although there is no specific lesion
for polymyalgia rheumatica, ultrasound and MRI studies
indicate that mild bilateral subacromial or subdeltoid
bursitis occurs in 32–93% of people with the condition.
Furthermore, shoulder capsulitis (69%), rotator cuff
tendonitis (72%), and biceps tenosynovitis (37–60%) are
common findings in untreated individuals with
polymyalgia rheumatica (figure 2).46–49 Bilateral synovitis
of shoulders (26–52%) and hips (18–32%), as well as
peripheral joint involvement, particularly tenosynovitis
of extensor tendons at hands (67%) are also compatible
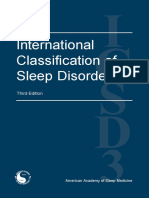
with a diagnosis of polymyalgia rheumatica,46–49 whereas Figure 2: Characteristic ultrasound and PET-scan imaging findings in people with polymyalgia rheumatica
extensive synovial proliferation or erosions should (A) Cross-sectional view of biceps tenosynovitis. Asterisk denotes the biceps tendon, which is surrounded by
hypoechoic fluid, pointed to by arrows. (B) Longitudinal view of subdeltoid bursitis. Arrows delimitate the hypoechoic
prompt suspicion for another diagnosis, particularly fluid within the bursa. (C) Increased [¹⁸F]fluorodeoxyglucose (¹⁸FDG) uptake by PET scan in the shoulders and
rheumatoid arthritis.48 Bilateral trochanteric bursitis has trochanteric areas (arrows). (D) Increased ¹⁸FDG uptake by PET scan in the cervical and interspinous areas (arrows).
been observed in up to 90% of patients in early imaging
studies,50 whereas later studies only found this lesion in predominant pelvic girdle symptoms.58–60 Peritendinous
about 20% of people with polymyalgia rheumatica.40 and intratendinous contrast enhancement of various
PET can show ¹⁸FDG uptake in the shoulders, tendons (eg, gluteus medius and minimus tendons at the
sternoclavicular joints, hips, ischial tuberosities, and insertion into the major trochanter, rectus femoris tendon
hips.51,52 Another characteristic lesion of polymyalgia at the proximal insertion, and adductor longus origins at
rheumatica is interspinous bursitis of the cervical and the inferomedial pubic symphysis) emerges as the most
lumbar spine, observed using ultrasound, MRI, remarkable abnormality.58,59 Inflammation seems to
or ¹⁸FDG-PET in approximately 50% of patients originate in the peritendineum and secondarily extend to
(figure 2).51,53–55 However, inflammation at that site is only bursae and joints.58,59 Isolated inflammation of joints was
inconsistently associated with neck and lumbar pain or not observed. Another study using MRI and ¹⁸FDG-PET
stiffness.53–55 supported this observation, revealing that ¹⁸FDG uptake at
Scores for PET evaluation have been proposed in the ischial tuberosity corresponded to hamstring
retrospective studies yielding 96·9–98·8% sensitivity peritendonitis rather than to ischial bursitis.61,62
and 92·8–95·2% specificity for the diagnosis of Predominant tendinous involvement was also observed at
polymyalgia rheumatica but need to be validated by the knees.63 Extracapsular inflammation at the pelvis
prospective assessment.56,57 seemed also to better differentiate polymyalgia rheumatica
MRI studies have provided deeper insight into the from late-onset rheumatoid arthritis, while the pattern of
anatomical structures involved in people with inflammation at the shoulders was similar in both
www.thelancet.com Vol 402 October 21, 2023 1463
www.memodiapp.com
Seminar
diseases.60 Although histopathological confirmation would These criteria highlight the importance of hip involvement
be necessary to substantiate these observations, these and, unlike late-onset rheumatoid arthritis, the absence of
studies provide novel insights into the anatomical target rheumatoid factor and anti-citrullinated peptide antibodies
of inflammation in polymyalgia rheumatica. (panel).40 Complete response to medium-dose
Imaging can also be helpful to uncover coexisting giant glucocorticoids—that were included in some previous
cell arteritis in people with polymyalgia rheumatica.51,64–66 criteria—was reached in only 71% of participants and,
Ultrasound has been more widely used and validated to conversely, glucocorticoids temporarily alleviated
detect involvement of cranial and axillary arteries symptoms of other conditions. Response to glucocorticoid
and ¹⁸FDG-PET to detect large-vessel vasculitis.67–70 The treatment did not improve sensitivity or specificity and,
clinical relevance of systematically screening for consequently, was not included in the final criteria. An
subclinical giant cell arteritis in people with new, typical innovation of the EULAR and ACR classification criteria
polymyalgia rheumatica is unclear. effort is the use of musculoskeletal sonography of shoulder
and hip girdle structures. Bilateral subacromial or
Classification criteria subdeltoid bursitis and trochanteric bursitis in patients
Classification criteria are useful for characterising with inflammatory pain of the shoulder or pelvic girdle is
diseases for investigation purposes, especially for highly suggestive of polymyalgia rheumatica in the
diseases with no single specific diagnostic features such absence of peripheral joint involvement.40 The sensitivity
as polymyalgia rheumatica. The criteria influence the of the EULAR and ACR criteria for polymyalgia
assessment of disease epidemiology and the selection of rheumatica is 68%, and specificity is 78%, increasing to 81%
affected individuals for clinical trials. Classification with the use of ultrasound, which mostly helps to
criteria aim to include the most typical features of the distinguish it from degenerative disorders.
disease, which differentiate polymyalgia rheumatica Analysis of independent datasets reveals that EULAR
from other musculoskeletal conditions, mainly late-onset and ACR criteria have the best discriminatory
rheumatoid arthritis and considering these criteria can performance when both sensitivity and specificity are
also assist physicians in diagnosis. considered.71 Evaluations of these criteria in other patient
Various criteria sets based on retrospective medical populations disclosed estimates of sensitivity of
record review have been used over the years.32,35–40 In 2012, 85·2–92·6% and specificity of 57·7–81·5%.71–74 Adding
the European Alliance of Associations for Rheumatology ultrasound, the specificity estimates for these criteria
(formerly European League Against Rheumatism; EULAR) ranged from 52·0% to 91·3%.71–74 In the EULAR and
and American College of Rheumatology (ACR) ACR study, 8% of people initially classified as having
classification criteria for polymyalgia rheumatica were polymyalgia rheumatica had another diagnosis at
developed using a prospective longitudinal methodology. 6 months, and 4·7% of controls were reclassified as
polymyalgia rheumatica by the end of follow-up.40
Panel: The European Alliance of Associations for Polymyalgia rheumatica in the context of other
Rheumatology (formerly European League Against diseases
Rheumatism) and American College of Rheumatology Giant cell arteritis
proposed classification criteria for polymyalgia Polymyalgia rheumatica and giant cell arteritis might be
rheumatica in 201240 part of a disease spectrum.75,76 Approximately 40–60% of
Patients aged 50 years or older with bilateral shoulder aching people with biopsy or imaging-proven giant cell arteritis
and abnormal C-reactive protein concentrations or an have polymyalgia rheumatica.1 Polymyalgia rheumatica
increased erythrocyte sedimentation rate, plus at least might precede clinically apparent giant cell arteritis by
4 points (without ultrasonography) or at least 5 points (with weeks, months, or years; appear simultaneously with giant
ultrasonography) from: cell arteritis; or develop after a self-limiting episode of
• Morning stiffness for more than 45 min (2 points) cranial symptoms77 or during a relapse, even if polymyalgia
• Hip pain or restricted range of motion (1 point) rheumatica manifestations were not present at the time of
• Absence of rheumatoid factor or anti-citrullinated giant cell arteritis diagnosis.78,79 The proportion of people
protein antibodies (2 points) primarily presenting with polymyalgia rheumatica and
• Absence of other joint involvement (1 point) found to have asymptomatic giant cell arteritis is more
• If ultrasonography is available, at least one shoulder with variable, ranging from 0% to more than 40%.1,51,67–80 The
subdeltoid bursitis, biceps tenosynovitis, or glenohumeral number depends on selection criteria (ie, how stringently
synovitis (either posterior or axillary), as well as at least isolated polymyalgia rheumatica is defined and cranial
one hip with synovitis or trochanteric bursitis (1 point) symptoms excluded); pre-test suspicion, since not all
• If ultrasonography is available, both shoulders with people with polymyalgia rheumatica are routinely imaged
subdeltoid bursitis, biceps tenosynovitis, or glenohumeral or have a biopsy taken to rule out giant cell arteritis; and
synovitis (1 point) how giant cell arteritis is defined (eg, biopsy, imaging, or
classification criteria). Giant cell arteritis might be
1464 www.thelancet.com Vol 402 October 21, 2023
www.memodiapp.com
Seminar
suspected when there are cranial symptoms (which are equivalent at a dose of 12·5–25·0 mg per day.91 Within
sometimes very mild) or temporal artery abnormalities at this recommended range, the dose can be adapted to
physical examination (eg, tenderness, hardness, bodyweight and possible risk factors for refractory disease
asymmetric, and weak or absent pulse) and need to be for which an increased dose might be preferred (see next
confirmed by temporal artery biopsy or vascular imaging. section).91,92 Conversely, in the context of comorbidities
In the absence of cranial symptoms, giant cell arteritis increasing the risk for glucocorticoid-related adverse
might be suspected in people with marked systemic events (ie, diabetes, hypertension, osteoporosis, and
manifestations, persistently elevated acute phase reactants, obesity), a reduced initial dose can be chosen.
vascular pain in the lower extremities, or incomplete Response to glucocorticoids is usually rapid—within a
response to the dose range of glucocorticoids used in few days to 1 week in most cases. However, in some
polymyalgia rheumatica (see upcoming sections).65,69,81,82 As patients, response is slower than a week. In a follow-up
previously mentioned, imaging of large vessels can help to study of 85 people with new-onset polymyalgia rheumatica
detect giant cell arteritis in these patients. People in whom response was defined as a 70% reduction of
primarily presenting with polymyalgia rheumatica can symptoms on the visual analogue scale for patients’ global
subsequently develop cranial symptoms of giant cell assessment, 27% of participants did not completely
arteritis and are at risk of cranial ischaemic complications respond to standard glucocorticoid therapy after 4 weeks
when cranial manifestations of giant cell arteritis appear, and 20% did not completely respond after 12 weeks.93
such as headache, visual symptoms, or jaw claudication.77 Once remission is achieved, prednisone is reduced to
Patients with polymyalgia rheumatica with no cranial 10 mg per day within 4–8 weeks, and the daily dose
symptoms in whom large-vessel vasculitis is discovered by subsequently tapered by approximately 1 mg per day per
imaging might be at reduced risk of cranial ischaemic month until discontinuation if remission is maintained.
complications.51 The usual minimum duration of glucocorticoid therapy
Some people with polymyalgia rheumatica could have is 9–12 months; however, some patients can sustain
minimal periadventitial and vasa vasorum infiltrates remission with shorter treatment periods.94 Longer
noted on temporal artery biopsy, which are not irrelevant treatment is often required when relapses occur. It is not
but are not specific enough to confirm the diagnosis of uncommon for people with polymyalgia rheumatica to
giant cell arteritis.83 These features can also appear in require low-dose glucocorticoid therapy (≤5 mg per day)
other diseases, including small-vessel vasculitis, for several years, and sometimes treatment is lifelong.95
infection, and malignancy.84 Glucocorticoids are usually administered as a single dose
in the morning. In cases of severe night pain, the dose
Other immune-mediated diseases can be split, usually administering a third of the daily
Physicians need to be aware that other immune-mediated dose in the evening.91
diseases can appear in people with polymyalgia For select patients (eg, those with a low adherence to
rheumatica. Autoimmune thyroid disease, autoimmune oral therapies), an alternative to oral glucocorticoids can
hepatitis, primary biliary cholangitis, Sjögren’s syndrome, be intramuscular methylprednisolone, usually started at
or inflammatory bowel disease have been reported.85–87 120 mg every 3 weeks with subsequent dose tapering.91
Polymyalgia rheumatica can develop in people One randomised trial reported decreased weight gain
with malignancies treated with immune checkpoint and decreased cumulative glucocorticoid dose in the
inhibitors.88–90 The prevalence is low, ranging from less group receiving intramuscular methylprednisolone
than 1% to 2·1% of treated patients and reports are scarce, treatment compared with those receiving conventional
mainly limited to retrospective studies.88–90 Polymyalgia oral therapy—efficacy was similar.96
rheumatica features in these patients are not always Long-term oral glucocorticoid therapy carries risks of
typical. About 25% of patients in this group do not fulfil many potential toxicities across multiple organ systems
EULAR and ACR classification criteria for polymyalgia (ie, osteoporosis, hypertension, weight gain, diabetes, and
rheumatica and peripheral arthritis or RS3PE is more cataracts).97–99 Even low-dose glucocorticoids can increase
frequent than in primary polymyalgia rheumatica. In such cardiovascular risk in the long term100 and studies indicate
patients, acute phase reactants are less likely to be elevated that frailty, resulting from persistent inflammation,
and response to glucocorticoids is not always satisfactory, reduced physical activity, or chronic glucocorticoid use,
requiring higher doses or additional treatment. can affect a substantial proportion of these patients.101
Methotrexate, hydroxychloroquine, or tocilizumab have Fatigue and depression exemplify the complex and
been used to alleviate symptoms in these patients, but time-dependent interplay of the effects of inflammatory
more data are needed on their effectiveness.88–90 activity and treatment-related adverse effects in
polymyalgia rheumatica.102 Fatigue and depression are
Management also strongly influenced by contextual factors including
Glucocorticoids multimorbidity.
Glucocorticoids are the cornerstone of initial treatment. Prevention and treatment of glucocorticoid-related
Current practice is to start with oral prednisone or an adverse events are crucial aspects of care in polymyalgia
www.thelancet.com Vol 402 October 21, 2023 1465
www.memodiapp.com
Seminar
rheumatica.103 Measures include regular monitoring of Targeted therapies
blood pressure, serum glucose, and other cardiovascular TNF-α blockers were the first targeted biological agents
risk factors as well as screening and prevention of tested in polymyalgia rheumatica, but they did not show
osteoporosis, and appropriate calcium and vitamin D any benefit.111,112
intake. On the basis of fracture risk assessment and The effect of anti-IL6 receptor antibody tocilizumab
national thresholds for preventive therapy, antiresorptive has been shown in two published randomised controlled
therapies should be considered.103 Non-pharmacological trials from 2022.113,114 In a phase 2/3 trial, 36 people with
interventions such as exercise, muscle strengthening, new polymyalgia rheumatica were randomly assigned to
and interaction with support groups when available are receive either subcutaneous tocilizumab (162 mg per
advised to minimise fatigue and depression.91 week) or placebo for 16 weeks (1:1 ratio).113 All participants
received oral prednisone 20 mg, tapered down to 0 mg
Broad-spectrum immunosuppressive agents over 11 weeks. The primary endpoint, which was
To avoid relapses and reduce glucocorticoid exposure glucocorticoid-free remission at 16 weeks, was reached
and side-effects, several glucocorticoid-sparing agents by 12 (63%) of 19 people receiving tocilizumab, but only
have been tried. Among immunosuppressive drugs, by 2 (12%) of 17 people receiving placebo. Additionally,
methotrexate has been the most widely studied; time to first relapse was longer in the intervention group
however, results are conflicting.104–107 One trial showed than in the control group (130 vs 82 days, p=0·007) and
that methotrexate led to a reduction of relapses tocilizumab treated participants had a lower cumulative
compared with placebo,104 and two trials suggested a glucocorticoid dose after 24 weeks than those treated
lower cumulative glucocorticoid dose in the with the placebo (781 mg vs 1290 mg, p<0·001).113 In a
methotrexate group,104,105 whereas other studies were phase 3 randomised controlled trial evaluating the
unable to substantiate these results.106,107 The 2015 EULAR efficacy of tocilizumab in relapsing polymyalgia
and ACR recommendations for the management of rheumatica, 101 people with persistent disease activity
polymyalgia rheumatica consider methotrexate for (CRP polymyalgia rheumatica activity score >10; see next
treatment of patients at high risk of relapse or long-term section) requiring ≥10 mg prednisone per day, were
glucocorticoid therapy (see next section) as well as those randomly assigned to receive tocilizumab (8 mg/kg
with risk factors for glucocorticoid-related adverse every 4 weeks) or placebo.114 The primary efficacy
events (ie, pre-existing osteoporosis, diabetes, endpoint, evaluated at 24 weeks, was a CRP–polymyalgia
hypertension, or overweight).91 The methotrexate doses rheumatica activity score of less than 10 with daily
tested in trials (7·5–10·0 mg oral methotrexate per prednisone of 5 mg or less, or after decreasing daily
week) were cautious and inferior to those frequently prednisone dose by 10 mg or more. This endpoint was
used in clinical practice (up to 25 mg oral or reached by 67% of tocilizumab recipients compared with
subcutaneous methotrexate per week). The long-term 31% of participants receiving placebo (p<0·001).114
follow-up of a clinical trial did not show a reduction of Overall, these studies indicate that the addition of
glucocorticoid-related side-effects after 5 years in tocilizumab to glucocorticoids can be of benefit in
patients receiving oral methotrexate (10 mg per week); individuals with polymyalgia rheumatica, enabling
however, this study used a relatively low dose and was faster glucocorticoid tapering and a reduction in
limited by a steady loss of trial participants.107 Although cumulative glucocorticoid dose compared with placebo.
generally well tolerated, methotrexate is not exempt of The use of tocilizumab as monotherapy is not clearly
side-effects (eg, nausea, fatigue, leucopenia, infection, supported by existing evidence.115–117 In these trials,
and hair loss) and cannot be used in patients with adverse events were similar in both arms. Adverse events
reduced kidney function. in patients treated with tocilizumab include elevation
Other conventional synthetic immunosuppressants of transaminases, cytopenias, hyperlipidaemia, and
have been studied for polymyalgia rheumatica, but this infection.
has been rare. Two case series suggested beneficial A phase 3 randomised controlled trial testing the IL-6
effects of leflunomide in people with difficult to treat receptor blocker sarilumab in individuals with relapsing
polymyalgia rheumatica and giant cell arteritis.108,109 A or refractory polymyalgia rheumatica was terminated
randomised, double-blind, placebo controlled, phase 3 prematurely due to protracted recruitment exacerbated
trial with leflunomide 20 mg per day or placebo along by the COVID-19 pandemic, but results from the
with 26-week glucocorticoid tapering is currently recruited and analysed 118 participants favoured
recruiting (NCT03576794). Azathioprine was tested in a sarilumab over placebo.118 As a result, the US Food and
pooled analysis of people with polymyalgia rheumatica Drug Administration approved sarilumab in February,
and giant cell arteritis, revealing a reduced mean 2023, for the treatment of individuals with inadequate
prednisone dose after 1 year in the azathioprine group.110 response to glucocorticoids or relapsing polymyalgia
Because of the scarcity of data, these agents are currently rheumatica.
not recommended as first-line treatment for people with Although the exact role of B lymphocytes in the
polymyalgia rheumatica.90 pathogenesis of polymyalgia rheumatica remains elusive
1466 www.thelancet.com Vol 402 October 21, 2023
www.memodiapp.com
Seminar
(figure 1),15,16,18 a small randomised controlled trial minimise unnecessary treatment toxicity, but this
from 2021 indicates that B-cell depletion with rituximab depends on accurate assessment of disease activity.121 The
might be effective in people with newly diagnosed or need to improve patient outcomes and the availability of
relapsing polymyalgia rheumatica. 11 (48%) of potential new therapies has prompted efforts to better
23 participants in the rituximab group and five (21%) of 24 define disease activity status and outcomes to be
in the placebo group had glucocorticoid-free remission measured in clinical trials.122
at 21 weeks.119 Larger trials are needed to define the role
of rituximab in the treatment of people with polymyalgia Relapses
rheumatica. A small, single-arm trial included 14 people Relapse is defined as an increase in polymyalgia
(three with newly diagnosed polymyalgia rheumatica rheumatica activity, usually occurring during
and 11 with relapsing polymyalgia rheumatica) who were glucocorticoid tapering or discontinuation, and resulting
treated with 10 mg per day of the JAK inhibitor, in re-escalation of therapy. When symptoms recur and a
tofacitinib, along with 15 mg prednisone per day with a flare is suspected, detailed clinical evaluation is necessary
standardised tapering. Remission (requiring 2·5 mg to exclude other conditions or reappearance of chronic
prednisone per day) was reached by 86% of participants pain due to comorbidities (ie, osteoarthritis) and masked
at 24 weeks.120 The efficacy and safety of targeted by glucocorticoids. In observational studies, 43% of people
therapies needs to be evaluated in large randomised with polymyalgia rheumatica relapsed at least once
controlled trials. Additional ongoing clinical trials in within the first year of diagnosis.95 Those who relapsed
people with polymyalgia rheumatica are summarised in during the first 6 months were more likely to require
table 2. long-term treatment beyond 2 years.123 Female sex,124,125
peripheral arthritis,33 high levels of ESR and CRP,41,125 and
Assessment of disease activity a combination of low haemoglobin and high serum
Appropriate management of people with polymyalgia levels of soluble IL-6 receptor,126 have been associated
rheumatica requires an accurate appraisal of disease with an elevated relapse rate; these findings, however,
activity to adjust therapy, distinguishing activity from require confirmation. Fast glucocorticoid tapering might
comorbidities and treatment-related side-effects. An also be associated with relapses.127
accurate balance between activity and long-term Clinical flares are usually associated with a rise in acute
treatment toxicity is crucial for patients. A treat-to-target phase reactants. Elevation can be slight during
approach to polymyalgia rheumatica might help to glucocorticoid therapy,41,42 and even normal in individuals
Rationale Characteristics Population Status Trial number
Baricitinib (JAK1 and Efficacy in other rheumatic diseases; case Multicentre, randomised, double- 34 early onset Recruiting NCT04027101
JAK2 inhibitor) reports in polymyalgia rheumatica; small trial blind, phase 2 trial
with tofacitinib in polymyalgia rheumatica
ABBV-154 (anti-TNF Local delivery of GRM; avoiding systemic Multicentre, randomised, double- 200 relapsing Recruitment NCT04972968
and glucocorticoid- effects of glucocorticoid blind, phase 2 trial Completed
receptor conjugate)*
Abatacept Inhibition of CD28-mediated T-cell activation; Multicentre, randomised, double- 34 early onset Recruiting NCT03632187
efficacy in giant cell arteritis and rheumatoid blind, phase 3 trial
arthritis
Leflunomide Immunosuppressive agent; efficacy in Multicentre, randomised, double- 94 newly Recruiting NCT03576794
rheumatoid arthritis; small series in blind, phase 3 trial diagnosed
polymyalgia rheumatica; observational studies
in giant cell arteritis and polymyalgia
rheumatica
Low-dose IL-2 Stimulation of regulatory T cells to suppress Open label, phase 2 15 Unknown NCT04062006
inflammation
SPI-62† HSD-1 inhibitor, to avoid systemic effects of Non-randomised, single-blind, 48 Recruiting NCT05436652
glucocorticoids phase 2
Rituximab B-cell depletion, efficacy in a small RCT in Randomised, parallel assignment, 114 recently Recruiting NCT05533125
polymyalgia rheumatica phase 3 diagnosed
Rituximab B-cell depletion, efficacy in a small RCT in Randomised, parallel assignment, 174 relapsing Recruiting NCT05533164
polymyalgia rheumatica phase 3
Secukinumab Fully human anti-IL-17A antibody Multicentre, randomised, double- 360 relapsing Recruiting NCT05767034
blind, phase 3
GRM=glucocorticoid receptor modulator. HSD-1= hydroxysteroid dehydrogenase type 1. RCT=randomised controlled trial. *Anti-TNF monoclonal antibody conjugated to a
GRM. It selectively delivers GRM to the activated immune cells that express transmembrane TNF. Intended to increase overall efficacy while reducing systemic effects of
conventional glucocorticoids. †Small-molecule inhibitors of 11β-HSD-1. This enzyme converts inactive cortisone to active cortisol in tissues.
Table 2: Ongoing clinical trials in patients with polymyalgia rheumatica
www.thelancet.com Vol 402 October 21, 2023 1467
www.memodiapp.com
Seminar
treated with IL-6 receptor blockers (see next section), due pain, stiffness, physician function, and laboratory
to the direct inhibition of the acute phase reactant markers and corresponding instruments to measure
synthesis.128,129 Except in this context, relapses with these domains for clinical trials.136,137
completely normal acute phase reactants are infrequent41,42
and overdiagnosis of polymyalgia rheumatica flare needs Other outcome measures
to be avoided by referral to expert centres since other A comprehensive Glucocorticoid Toxicity Index has been
conditions can present with a polymyalgic syndrome developed to support systematic assessment for
(table 1). Conversely, inflammatory indices can some glucocorticoid toxicity in trials designed to reduce
times rise for other reasons in the absence of clinically glucocorticoid exposure.97 An OMERACT initiative that
active disease and isolated fluctuations in acute phase included participants with polymyalgia rheumatica and
reactants should not be considered relapse in the absence physicians led to the inclusion of fatigue,138–140 which is
of clinical symptoms. not specifically assessed in the expert-developed Gluco
Glucocorticoid-induced adrenal insufficiency, with corticoid Toxicity Index. Although these instru ments
symptoms of arthralgia, myalgia, malaise, abdominal pain, were developed for investigational purposes their content
and fatigue, can occur in 11% of people receiving long-term can guide physicians in the long-term management of
treatment, particularly when prednisone dose is reduced to polymyalgia rheumatica.
less than 7·5 mg per day, and can further complicate Isolated polymyalgia rheumatica does not convey life-
relapse assessment.130 The absence of more characteristic threatening complications and does not lead to permanent
symptoms and laboratory abnormalities of polymyalgia organ damage; however, the burden of recurrent disease
rheumatica can prompt the suspicion of adrenal and glucocorticoid side-effects can deeply impair the
insufficiency. Adrenal insufficiency can be substantiated by quality of life of some people with the condition.136,137 Both
a short 250 mg corticotropin stimulation test and might physical and mental components of generic measures of
require endocrinologist consultation, particularly in the health-related quality of life, including the Medical
context of infection or acute stress. Most cases resolve over Outcomes Study Short Form 36 and Euroqol EQ-5D, are
time with slow tapering. Treatment, inflammation, or affected by polymyalgia rheumatica.136,137 On average,
inactivity-related muscle weakness, as well as osteoarthritis health-related quality of life improves with time but there
and tendinopathies, common in this age group, can also is substantial heterogeneity in polymyalgia rheumatica
make assessment of response and relapse difficult (table 1). trajectories over time.138–140 A polymyalgia rheumatica-
The role of imaging for assessing relapse remains specific patient-reported outcomes measure, including
unclear. Follow-up studies using different imaging assessment of four domains (ie, symptoms, function,
methods have indicated that reduction of inflammation- psychological and emotional wellbeing, and glucocorticoid
related abnormalities only partly parallels clinical side-effects), has been developed.141 Although these
improvement. In one study, 20 people with polymyalgia assessments have been developed for research, they are
rheumatica received three infusions of tocilizumab at relevant to patients and need to be considered, together
weeks 0, 4, and 8 and were followed up clinically, by with patient preferences and values, in shared decision
¹⁸FDG-PET-CT and MRI.116 Although all participants had making for optimal care.
clinical remission or low disease activity at week 12, only
moderate reduction of inflammatory lesions at shoulders Future directions for practice and research
and hips were observed by imaging. Other studies There are many unmet needs in the diagnosis and
revealed similar results.131–133 Whether residual imaging management of people with polymyalgia rheumatica.
abnormalities correspond to smouldering inflammation The role of imaging in its various modalities in the
or to remodelling, and whether these findings are relevant diagnosis and assessment of disease activity needs to be
for therapeutic decisions and long-term outcomes is better defined and validated. Disease stratification
unclear. Imaging as a tool to monitor polymyalgia according to severity and risk of unfavourable outcomes
rheumatica activity is still investigational. needs to be defined, along with the role of imaging and
There is no universally agreed definition of polymyalgia serum or tissue biomarkers for this purpose. Current
rheumatica relapse for research studies.134 A threshold treatment options are inadequate, particularly for people
level in the CRP–polymyalgia rheumatica activity score with truly refractory or relapsing polymyalgia rheumatica
has been used to define relapse.135 However, polymyalgia and those with or at high risk of glucocorticoid-related
rheumatica activity score also incorporates a physician adverse events. A better understanding of polymyalgia
global assessment that introduces circularity to validation rheumatica physiopathology could lead to a more
studies. In general, the reference standard for assessing accurate selection of biomarkers and targeted therapies.
relapse definitions relies on subjective clinical judge Clinical trials support the clinical benefit of several
ment, which is not perfect and might be influenced targeted therapies, particularly tocilizumab and
by contextual factors. The Outcome Measures in sarilumab. Where specialist referral is indicated, fast-
Rheumatology (OMERACT) polymyalgia rheumatica track clinics might play a role in speeding diagnosis,
working group identified a core domain set including stratifying severity, and optimising treatment.
1468 www.thelancet.com Vol 402 October 21, 2023
www.memodiapp.com
Seminar
Since polymyalgia rheumatica does not lead to permanent 9 Kim Y, Seo GH, Lee S, et al. Epidemiology of polymyalgia
organ damage and targets older individuals (aged ≥50 years) rheumatica in Korea. J Rheum Dis 2014; 21: 297–302.
10 Partington R, Muller S, Mallen CD, Abdul Sultan A, Helliwell T.
with increased vulnerability, the trade-off between the Mortality among patients with polymyalgia rheumatica: a retrospective
benefits and risks of new therapies, which might increase cohort study. Arthritis Care Res (Hoboken) 2021; 73: 1853–57.
risk of infection (eg, rituximab and JAK inhibitors), 11 Raheel S, Shbeeb I, Crowson CS, Matteson EL. Epidemiology of
polymyalgia rheumatica 2000–2014 and examination of incidence
malignancy, or vascular morbidity (eg, JAK inhibitors), and survival trends over 45 years: a population-based study.
compared with low-dose gluco corticoid monotherapy Arthritis Care Res (Hoboken) 2017; 69: 1282–85.
maintenance, needs to be carefully evaluated. 12 Michailidou D, Johansson L, Kuley R, et al. Immune complex-
mediated neutrophil activation in patients with polymyalgia
Contributors rheumatica. Rheumatology (Oxford) 2023; 62: 2880–86.
MCC and GE-F designed the outline of this Seminar. All authors 13 Martínez-Taboada VM, Blanco R, Fito C, Pacheco MJ,
contributed by writing two sections and thoroughly reviewed the Delgado-Rodríguez M, Rodríguez-Valverde V. Circulating CD8+ s in
sections written by others. MCC and GE-F composed the final polymyalgia rheumatica and giant cell arteritis: a review.
manuscript, which was reviewed and approved by all contributors. Semin Arthritis Rheum 2001; 30: 257–71.
Declaration of interests 14 Samson M, Audia S, Fraszczak J, et al. Th1 and Th17 lymphocytes
expressing CD161 are implicated in giant cell arteritis and
GE-F reports consulting fees from Janssen, GSK, and CSL Vifor, and
polymyalgia rheumatica pathogenesis. Arthritis Rheum 2012;
meeting travel support from Boehringer Ingelheim. CD reports grant
64: 3788–98.
support from AbbVie, Novartis, and Celgene; consulting fees, speaker
15 van der Geest KS, Abdulahad WH, Chalan P, et al. Disturbed B cell
fees, or both honoraria from AbbVie, Roche, Sanofi, Galapagos, Lilly,
homeostasis in newly diagnosed giant cell arteritis and polymyalgia
Janssen, Novartis, and Sparrow; participation in advisory boards for rheumatica. Arthritis Rheumatol 2014; 66: 1927–38.
Roche, Sanofi, AbbVie, Janssen, Novartis, Eli Lilly, Galapagos, and 16 Reitsema RD, Jiemy WF, Wekema L, et al. Contribution of
Sparrow; meeting travel support from AbbVie, Roche, Sanofi, Galapagos, pathogenic T helper 1 and 17 cells to bursitis and tenosynovitis in
Eli Lilly, Janssen, and Novartis; and royalties from Oxford University polymyalgia rheumatica. Front Immunol 2022; 13: 943574.
Press and SAGE journals. CD reports participation in the EULAR 17 Jiemy WF, Zhang A, Boots AMH, et al. Expression of interleukin-6
congress committee. SLM received a research grant from CSL Vifor and in synovial tissue of patients with polymyalgia rheumatica.
from the National Institute of Health Research; consulting fees from Ann Rheum Dis 2023; 82: 440–42.
AbbVie, AstraZeneca, Roche/Chugai, and Sanofi; lecturing fees from 18 Meliconi R, Pulsatelli L, Uguccioni M, et al. Leukocyte infiltration
Pfizer, UCB, and CSL Vifor; and meeting travel support from Roche/ in synovial tissue from the shoulder of patients with polymyalgia
Chugai and Pfizer. SLM is a patron of the charity Polymyalgia rheumatica. Quantitative analysis and influence of corticosteroid
Rheumatica and Giant Cell Arteritis UK. CS reports consulting fees from treatment. Arthritis Rheum 1996; 39: 1199–207.
AbbVie, Boehringer Ingelheim, Roche, Lilly, Galapagos, Pfizer, Novartis, 19 Meliconi R, Pulsatelli L, Melchiorri C, et al. Synovial expression of
and Amgen, and royalties from UpToDate. ELM reports a research grant cell adhesion molecules in polymyalgia rheumatica.
from AbbVie; consulting fees, lecturing fees, or both from Boehringer Clin Exp Immunol 1997; 107: 494–500.
Ingelheim and Novartis; royalties from UpToDate; and speaker fees from 20 Carvajal Alegria G, Boukhlal S, Cornec D, Devauchelle-Pensec V.
Practice Point Communication. ELM reports participation in advisory The pathophysiology of polymyalgia rheumatica, small pieces of a
boards for National Institutes of Health and Horizon Therapeutics. big puzzle. Autoimmun Rev 2020; 19: 102670.
MCC reports consulting fees from GSK, AbbVie, CSL Vifor, Janssen, and 21 Hysa E, Gotelli E, Sammorì S, et al. Immune system activation in
AstraZeneca; royalties from UpToDate; and a research grant and meeting polymyalgia rheumatica: which balance between autoinflammation
travel support from Kiniksa Pharmaceuticals. MCC reports participation and autoimmunity? A systematic review. Autoimmun Rev 2022;
21: 102995.
in advisory boards for GSK, CSL Vifor, and AstraZeneca.
22 Dejaco C, Duftner C, Al-Massad J, et al. NKG2D stimulated T-cell
Acknowledgments autoreactivity in giant cell arteritis and polymyalgia rheumatica.
Figure 1 was designed by Catalyzing Science. MCC was funded by Ann Rheum Dis 2013; 72: 1852–59.
Ministerio de Ciencia e Innovación (AEI//10.13039/501100011033 23 Álvarez Rodríguez L, López-Hoyos M, Mata C, et al. Expression and
[PID2020-114909RB-I00]) and by the Vasculitis Foundation. function of toll-like receptors in peripheral blood mononuclear cells
of patients with polymyalgia rheumatica and giant cell arteritis.
References Ann Rheum Dis 2011; 70: 1677–83.
1 González-Gay MA, Matteson EL, Castañeda S. Polymyalgia 24 Álvarez-Rodríguez L, López-Hoyos M, Calvo-Alén J,
rheumatica. Lancet 2017; 390: 1700–12. Aurrecoechea E, Villa I, Martínez-Taboada VM. Phagocyte
2 Dejaco C, Brouwer E, Mason JC, Buttgereit F, Matteson EL, dysfunction in polymyalgia rheumatica and other age-related,
Dasgupta B. Giant cell arteritis and polymyalgia rheumatica: current chronic, inflammatory conditions. J Leukoc Biol 2013; 94: 1071–78.
challenges and opportunities. Nat Rev Rheumatol 2017; 13: 578–92. 25 Haworth S, Ridgeway J, Stewart I, Dyer PA, Pepper L, Ollier W.
3 Camellino D, Matteson EL, Buttgereit F, Dejaco C. Monitoring and Polymyalgia rheumatica is associated with both HLA-DRB1*0401
long-term management of giant cell arteritis and polymyalgia and DRB1*0404. Br J Rheumatol 1996; 35: 632–35.
rheumatica. Nat Rev Rheumatol 2020; 16: 481–95. 26 Combe B, Sany J, Le Quellec A, Clot J, Eliaou JF. Distribution of
4 Crowson CS, Matteson EL. Contemporary prevalence estimates for HLA-DRB1 alleles of patients with polymyalgia rheumatica and giant
giant cell arteritis and polymyalgia rheumatica, 2015. cell arteritis in a Mediterranean population. J Rheumatol 1998;
Semin Arthritis Rheum 2017; 47: 253–56. 25: 94–98.
5 Sharma A, Mohammad AJ, Turesson C. Incidence and prevalence 27 Salvarani C, Boiardi L, Mantovani V, et al. HLA-DRB1 alleles
of giant cell arteritis and polymyalgia rheumatica: a systematic associated with polymyalgia rheumatica in northern Italy:
literature review. Semin Arthritis Rheum 2020; 50: 1040–48. correlation with disease severity. Ann Rheum Dis 1999; 58: 303–08.
6 Salvarani C, Macchioni P, Zizzi F, et al. Epidemiologic and 28 Dasgupta B, Panayi GS. Interleukin-6 in serum of patients with
immunogenetic aspects of polymyalgia rheumatica and giant cell polymyalgia rheumatica and giant cell arteritis. Br J Rheumatol
arteritis in northern Italy. Arthritis Rheum 1991; 34: 351–56. 1990; 29: 456–58.
7 González-Gay MA, Vázquez-Rodríguez TR, Lopez-Diaz MJ, et al. 29 Roche NE, Fulbright JW, Wagner AD, Hunder GG, Goronzy JJ,
Epidemiology of giant cell arteritis and polymyalgia rheumatica. Weyand CM. Correlation of interleukin-6 production and disease
Arthritis Rheum 2009; 61: 1454–61. activity in polymyalgia rheumatica and giant cell arteritis.
8 Martínez Perez JM, Mollerach FB, Scaglioni V, et al. Incidence and Arthritis Rheum 1993; 36: 1286–94.
prevalence of polymyalgia rheumatica and giant cell arteritis in a 30 Alvarez-Rodríguez L, Lopez-Hoyos M, Mata C, et al. Circulating
healthcare management organization in Buenos Aires, Argentina. cytokines in active polymyalgia rheumatica. Ann Rheum Dis 2010;
J Rheumatol 2023; 50: 93–97. 69: 263–69.
www.thelancet.com Vol 402 October 21, 2023 1469
Seminar
31 Salvarani C, Pipitone N, Versari A, Hunder GG. Clinical features of 52 Henckaerts L, Gheysens O, Vanderschueren S, Goffin K,
polymyalgia rheumatica and giant cell arteritis. Nat Rev Rheumatol Blockmans D. Use of 18F-fluorodeoxyglucose positron emission
2012; 8: 509–21. tomography in the diagnosis of polymyalgia rheumatica—
32 Chuang T-Y, Hunder GG, Ilstrup DM, Kurland LT. Polymyalgia a prospective study of 99 patients. Rheumatology (Oxford) 2018;
rheumatica: a 10-year epidemiologic and clinical study. 57: 1908–16.
Ann Intern Med 1982; 97: 672–80. 53 Camellino D, Paparo F, Morbelli S, Cutolo M, Sambuceti G,
33 Salvarani C, Cantini F, Macchioni P, et al. Distal musculoskeletal Cimmino MA. Interspinous bursitis is common in polymyalgia
manifestations in polymyalgia rheumatica: a prospective followup rheumatica, but is not associated with spinal pain. Arthritis Res Ther
study. Arthritis Rheum 1998; 41: 1221–26. 2014; 16: 492.
34 Salvarani C, Gabriel S, Hunder GG. Distal extremity swelling with 54 Falsetti P, Acciai C. Ultrasound in assessment of cervical
pitting edema in polymyalgia rheumatica. Report on nineteen cases. interspinous bursitis in polymyalgia rheumatica. Joint Bone Spine
Arthritis Rheum 1996; 39: 73–80. 2013; 80: 342–43.
35 Healey LA. Long-term follow-up of polymyalgia rheumatica: 55 Salvarani C, Barozzi L, Cantini F, et al. Cervical interspinous
evidence for synovitis. Semin Arthritis Rheum 1984; 13: 322–28. bursitis in active polymyalgia rheumatica. Ann Rheum Dis 2008;
36 Bird HA, Esselinckx W, Dixon ASJ, Mowat AG, Wood PHN. 67: 758–61.
An evaluation of criteria for polymyalgia rheumatica. 56 van der Geest KSM, van Sleen Y, Nienhuis P, et al. Comparison and
Ann Rheum Dis 1979; 38: 434–39. validation of FDG-PET/CT scores for polymyalgia rheumatica.
37 Jones JG, Hazleman BL. Prognosis and management of Rheumatology (Oxford) 2022; 61: 1072–82.
polymyalgia rheumatica. Ann Rheum Dis 1981; 40: 1–5. 57 Moreel L, Boeckxstaens L, Betrains A, et al. Diagnostic accuracy and
38 Nobunaga M, Yoshioka K, Yasuda M, Shingu M. Clinical studies of validation of 25F-fluorodeoxyglucose positron emission tomography
polymyalgia rheumatica. A proposal of diagnostic criteria. Jpn J Med scores in a large cohort of patients with polymyalgia rheumatica.
1989; 28: 452–56. Front Med (Lausanne) 2022; 9: 1026944.
39 Dasgupta B, Salvarani C, Schirmer M, et al. Developing 58 Fruth M, Seggewiss A, Kozik J, Martin-Seidel P, Baraliakos X,
classification criteria for polymyalgia rheumatica: comparison of Braun J. Diagnostic capability of contrast-enhanced pelvic girdle
views from an expert panel and wider survey. J Rheumatol 2008; magnetic resonance imaging in polymyalgia rheumatica.
35: 270–77. Rheumatology (Oxford) 2020; 59: 2864–71.
40 Dasgupta B, Cimmino MA, Maradit-Kremers H, et al. 2012 59 Fruth M, Buehring B, Baraliakos X, Braun J. Use of contrast-
provisional classification criteria for polymyalgia rheumatica: enhanced magnetic resonance imaging of the pelvis to describe
a European League Against Rheumatism/American College of changes at different anatomic sites which are potentially specific for
Rheumatology collaborative initiative. Ann Rheum Dis 2012; polymyalgia rheumatica. Clin Exp Rheumatol 2018;
71: 484–92. 36 (suppl 114): 86–95.
41 Cantini F, Salvarani C, Olivieri I, et al. Erythrocyte sedimentation 60 Mackie SL, Pease CT, Fukuba E, et al. Whole-body MRI of patients
rate and C-reactive protein in the evaluation of disease activity and with polymyalgia rheumatica identifies a distinct subset with
severity in polymyalgia rheumatica: a prospective follow-up study. complete patient-reported response to glucocorticoids.
Semin Arthritis Rheum 2000; 30: 17–24. Ann Rheum Dis 2015; 74: 2188–92.
42 Salvarani C, Cantini F, Niccoli L, et al. Acute-phase reactants and 61 Owen CE, Poon AMT, Lee ST, et al. Fusion of positron emission
the risk of relapse/recurrence in polymyalgia rheumatica: tomography/computed tomography with magnetic resonance
a prospective followup study. Arthritis Rheum 2005; 53: 33–38. imaging reveals hamstring peritendonitis in polymyalgia
rheumatica. Rheumatology (Oxford) 2018; 57: 345–53.
43 Lopez-Hoyos M, Ruiz de Alegria C, Blanco R, et al. Clinical utility of
anti-CCP antibodies in the differential diagnosis of elderly-onset 62 Owen CE, Poon AMT, Yang V, et al. Abnormalities at three
rheumatoid arthritis and polymyalgia rheumatica. musculoskeletal sites on whole-body positron emission
Rheumatology (Oxford) 2004; 43: 655–57. tomography/computed tomography can diagnose polymyalgia
rheumatica with high sensitivity and specificity.
44 Donskov AO, Mackie SL, Hauge EM, et al. An international survey
Eur J Nucl Med Mol Imaging 2020; 47: 2461–68.
of current management practices for polymyalgia rheumatica by
general practitioners and rheumatologists. Rheumatology (Oxford) 63 Kobayashi K, Nakagomi D, Kobayashi Y, et al. Ultrasound of
2023; 62: 2797–805. shoulder and knee improves the accuracy of the 2012 EULAR/ACR
provisional classification criteria for polymyalgia rheumatica.
45 Muller S, Whittle R, Hider SL, et al. Longitudinal clusters of pain
Rheumatology (Oxford) 2022; 61: 1185–94.
and stiffness in polymyalgia rheumatica: 2-year results from the
PMR Cohort Study. Rheumatology (Oxford) 2020; 59: 1906–15. 64 Slart RHJA. FDG-PET/CT(A) imaging in large vessel vasculitis
and polymyalgia rheumatica: joint procedural recommendation of
46 Nakamura H, Kamada K, Tarumi M, Tanimura S, Shibata Y,
the EANM, SNMMI, and the PET Interest Group (PIG), and
Horita T. Gadolinium-enhanced magnetic resonance imaging in
endorsed by the ASNC. Eur J Nucl Med Mol Imaging 2018;
shoulders contributes accurate diagnosis and predicting recurrence
45: 1250–69.
to patients with polymyalgia rheumatica. Clin Exp Rheumatol 2021;
39: 84–90. 65 Prieto-Peña D, Martínez-Rodríguez I, Loricera J, et al. Predictors of
positive 25F-FDG PET/CT-scan for large vessel vasculitis in patients
47 Cimmino MA, Parodi M, Zampogna G, Barbieri F, Garlaschi G.
with persistent polymyalgia rheumatica. Semin Arthritis Rheum
Polymyalgia rheumatica is associated with extensor tendon
2019; 48: 720–27.
tenosynovitis but not with synovitis of the hands: a magnetic
resonance imaging study. Rheumatology (Oxford) 2011; 66 Hemmig AK, Gozzoli D, Werlen L, et al. Subclinical giant cell
50: 494–99. arteritis in new onset polymyalgia rheumatica. A systematic review
and meta-analysis of individual patient data. Semin Arthritis Rheum
48 Camellino D, Duftner C, Dejaco C. New insights into the role of
2022; 55: 152017.
imaging in polymyalgia rheumatica. Rheumatology (Oxford) 2021;
60: 1016–33. 67 Schmidt WA, Gromnica-Ihle E. Incidence of temporal arteritis in
patients with polymyalgia rheumatica: a prospective study using
49 Mackie SL, Koduri G, Hill CL, et al. Accuracy of musculoskeletal
colour Doppler ultrasonography of the temporal arteries.
imaging for the diagnosis of polymyalgia rheumatica: systematic
Rheumatology (Oxford) 2002; 41: 46–52.
review. RMD Open 2015; 1: e000100.
68 Burg LC, Karakostas P, Behning C, Brossart P, Kermani TA,
50 Cantini F, Niccoli L, Nannini C, et al. Inflammatory changes of hip
Schäfer VS. Prevalence and characteristics of giant cell arteritis in
synovial structures in polymyalgia rheumatica. Clin Exp Rheumatol
patients with newly diagnosed polymyalgia rheumatica—
2005; 23: 462–68.
a prospective cohort study. Ther Adv Musculoskelet Dis 2023;
51 Blockmans D, De Ceuninck L, Vanderschueren S, Knockaert D, 15: 1759720X221149963.
Mortelmans L, Bobbaers H. Repetitive 18-fluorodeoxyglucose
69 Mekenyan L, Karalilova R, Todorov P, Tepeliev N, Batalov A.
positron emission tomography in isolated polymyalgia rheumatica:
Imaging methods in polymyalgia rheumatica: a systematic review.
a prospective study in 35 patients. Rheumatology (Oxford) 2007;
Rheumatol Int 2023; 43: 825–40.
46: 672–77.
1470 www.thelancet.com Vol 402 October 21, 2023
Seminar
70 Slart RHJA, Nienhuis PH, Glaudemans AWJM, Brouwer E, 89 Kostine M, Finckh A, Bingham CO, et al. EULAR points to consider
Gheysens O, van der Geest KSM. Role of 25F-FDG PET/CT in large for the diagnosis and management of rheumatic immune-related
vessel vasculitis and polymyalgia rheumatica. J Nucl Med 2023; adverse events due to cancer immunotherapy with checkpoint
64: 515–21. inhibitors. Ann Rheum Dis 2021; 80: 36–48.
71 Camellino D, Cimmino MA. Are the new ACR/EULAR criteria the 90 Cappelli LC, Bingham CO 3rd. Expert perspective: immune
ultimate answer for polymyalgia rheumatica classification? checkpoint inhibitors and rheumatologic complications.
J Rheumatol 2016; 43: 836–38. Arthritis Rheumatol 2021; 73: 553–65.
72 Ozen G, Inanc N, Unal AU, et al. Assessment of the new 2012 91 Dejaco C, Singh YP, Perel P, et al. 2015 recommendations for the
EULAR/ACR clinical classification criteria for polymyalgia management of polymyalgia rheumatica: a European League
rheumatica: a prospective multicenter study. J Rheumatol 2016; Against Rheumatism/American College of Rheumatology
43: 893–900. collaborative initiative. Arthritis Rheumatol 2015; 67: 2569–80.
73 Weigand S, Ehrenstein B, Fleck M, Hartung W. Joint involvement 92 Cimmino MA, Parodi M, Montecucco C, Caporali R. The correct
in patients with early polymyalgia rheumatica using high-resolution prednisone starting dose in polymyalgia rheumatica is related to
ultrasound and its contribution to the EULAR/ACR 2012 body weight but not to disease severity. BMC Musculoskelet Disord
classification criteria for polymyalgia rheumatica. J Rheumatol 2014; 2011; 12: 94.
41: 730–34. 93 Matteson EL, Maradit-Kremers H, Cimmino MA, et al. Patient-
74 Macchioni P, Boiardi L, Catanoso M, Pazzola G, Salvarani C. reported outcomes in polymyalgia rheumatica. J Rheumatol 2012;
Performance of the new 2012 EULAR/ACR classification criteria for 39: 795–803.
polymyalgia rheumatica: comparison with the previous criteria in a 94 Partington RJ, Muller S, Helliwell T, Mallen CD, Abdul Sultan A.
single-centre study. Ann Rheum Dis 2014; 73: 1190–93. Incidence, prevalence and treatment burden of polymyalgia
75 Cantini F, Niccoli L, Storri L, et al. Are polymyalgia rheumatica and rheumatica in the UK over two decades: a population-based study.
giant cell arteritis the same disease? Semin Arthritis Rheum 2004; Ann Rheum Dis 2018; 77: 1750–56.
33: 294–301. 95 Floris A, Piga M, Chessa E, et al. Long-term glucocorticoid
76 Gonzalez-Gay MA. Giant cell arteritis and polymyalgia rheumatica: treatment and high relapse rate remain unresolved issues in the
two different but often overlapping conditions. real-life management of polymyalgia rheumatica: a systematic
Semin Arthritis Rheum 2004; 33: 289–93. literature review and meta-analysis. Clin Rheumatol 2022;
77 Hernández-Rodríguez J, Font C, García-Martínez A, et al. 41: 19–31.
Development of ischemic complications in patients with giant cell 96 Dasgupta B, Dolan AL, Panayi GS, Fernandes L. An initially double-
arteritis presenting with apparently isolated polymyalgia blind controlled 96 week trial of depot methylprednisolone against
rheumatica: study of a series of 100 patients. Medicine (Baltimore) oral prednisolone in the treatment of polymyalgia rheumatica.
2007; 86: 233–41. Br J Rheumatol 1998; 37: 189–95.
78 Martinez-Lado L, Calviño-Díaz C, Piñeiro A, et al. Relapses and 97 Miloslavsky EM, Naden RP, Bijlsma JW, et al. Development of a
recurrences in giant cell arteritis: a population-based study of Glucocorticoid Toxicity Index (GTI) using multicriteria decision
patients with biopsy-proven disease from northwestern Spain. analysis. Ann Rheum Dis 2017; 76: 543–46.
Medicine (Baltimore) 2011; 90: 186–93. 98 Tieu J, Cheah JT, Black RJ, et al. Improving benefit-harm
79 Alba MA, García-Martínez A, Prieto-González S, et al. Relapses in assessment of glucocorticoid therapy incorporating the patient
patients with giant cell arteritis: prevalence, characteristics, and perspective: the OMERACT glucocorticoid core domain set.
associated clinical findings in a longitudinally followed cohort of Semin Arthritis Rheum 2021; 51: 1139–45.
106 patients. Medicine (Baltimore) 2014; 93: 194–201. 99 Hoon E, Ruediger C, Gill TK, Black RJ, Hill CL. A qualitative study
80 De Miguel E, Macchioni P, Conticini E, et al. Prevalence and of patient perspectives related to glucocorticoid therapy in
characteristics of subclinical giant cell arteritis in polymyalgia polymyalgia rheumatica and giant cell arteritis.
rheumatica. Rheumatology (Oxford) 2023; published online May 2. Open Access Rheumatol 2019; 11: 189–98.
https://doi.org/10.1093/rheumatology/kead189. 100 Pujades-Rodriguez M, Morgan AW, Cubbon RM, Wu J. Dose-
81 Warrington KJ, Jarpa EP, Crowson CS, et al. Increased risk of dependent oral glucocorticoid cardiovascular risks in people with
peripheral arterial disease in polymyalgia rheumatica: a population- immune-mediated inflammatory diseases: a population-based
based cohort study. Arthritis Res Ther 2009; 11: R50. cohort study. PLoS Med 2020; 17: e1003432.
82 Colaci M, Dichiara J, Aprile ML, et al. Use of 18F-fluorodeoxyglucose 101 Sattui SE, Jannat-Khah D, Lally L, Lieber SB, Mandl LA, Spiera RF.
positron emission tomography-computed tomography in patients Prevalence of frailty in patients with polymyalgia rheumatica and
affected by polymyalgia rheumatica and persistent increase of acute association with health-related quality of life, cognition and
phase reactants. Front Med (Lausanne) 2022; 9: 1042620. sarcopenia. Rheumatology (Oxford) 2022; 61: 4455–64.
83 Chatelain D, Duhaut P, Loire R, et al. Small-vessel vasculitis 102 Vivekanantham A, Blagojevic-Bucknall M, Clarkson K, Belcher J,
surrounding an uninflamed temporal artery: a new diagnostic Mallen CD, Hider SL. How common is depression in patients with
criterion for polymyalgia rheumatica? Arthritis Rheum 2008; polymyalgia rheumatica? Clin Rheumatol 2018; 37: 1633–38.
58: 2565–73. 103 Duru N, van der Goes MC, Jacobs JW, et al. EULAR evidence-based
84 Le Pendu C, Meignin V, Gonzalez-Chiappe S, Hij A, and consensus-based recommendations on the management of
Galateau-Sallé F, Mahr A. Poor predictive value of isolated medium to high-dose glucocorticoid therapy in rheumatic diseases.
adventitial and periadventitial infiltrates in temporal artery Ann Rheum Dis 2013; 72: 1905–13.
biopsies for diagnosis of giant cell arteritis. J Rheumatol 2017; 104 Caporali R, Cimmino MA, Ferraccioli G, et al. Prednisone plus
44: 1039–43. methotrexate for polymyalgia rheumatica: a randomized, double-
85 Teufel A, Weinmann A, Kahaly GJ, et al. Concurrent autoimmune blind, placebo-controlled trial. Ann Intern Med 2004; 141: 493–500.
diseases in patients with autoimmune hepatitis. J Clin Gastroenterol 105 Ferraccioli G, Salaffi F, De Vita S, Casatta L, Bartoli E. Methotrexate
2010; 44: 208–13. in polymyalgia rheumatica: preliminary results of an open,
86 Ferrari SM, Fallahi P, Ruffilli I, et al. The association of other randomized study. J Rheumatol 1996; 23: 624–28.
autoimmune diseases in patients with Graves’ disease (with or 106 van der Veen MJ, Dinant HJ, van Booma-Frankfort C,
without ophthalmopathy): review of the literature and report of a van Albada-Kuipers GA, Bijlsma JW. Can methotrexate be used as a
large series. Autoimmun Rev 2019; 18: 287–92. steroid sparing agent in the treatment of polymyalgia rheumatica
87 Partington R, Muller S, Mallen CD, Abdul Sultan A, Helliwell T. and giant cell arteritis? Ann Rheum Dis 1996; 55: 218–23.
Comorbidities in patients with polymyalgia rheumatica prior to and 107 Cimmino MA, Salvarani C, Macchioni P, et al. Long-term follow-up
following diagnosis: a case control and cohort study. of polymyalgia rheumatica patients treated with methotrexate and
Semin Arthritis Rheum 2020; 50: 663–72. steroids. Clin Exp Rheumatol 2008; 26: 395–400.
88 Calabrese C, Kirchner E, Kontzias A, Velcheti V, Calabrese LH. 108 Adizie T, Christidis D, Dharmapaliah C, Borg F, Dasgupta B.
Rheumatic immune-related adverse events of checkpoint therapy Efficacy and tolerability of leflunomide in difficult-to-treat
for cancer: case series of a new nosological entity. RMD Open 2017; polymyalgia rheumatica and giant cell arteritis: a case series.
3: e000412. Int J Clin Pract 2012; 66: 906–09.
www.thelancet.com Vol 402 October 21, 2023 1471
Seminar
109 Diamantopoulos AP, Hetland H, Myklebust G. Leflunomide as a 126 Pulsatelli L, Boiardi L, Pignotti E, et al. Serum interleukin-6
corticosteroid-sparing agent in giant cell arteritis and receptor in polymyalgia rheumatica: a potential marker of relapse/
polymyalgia rheumatica: a case series. BioMed Res Int 2013; recurrence risk. Arthritis Rheum 2008; 59: 1147–54.
2013: 120638. 127 Hernández-Rodríguez J, Cid MC, López-Soto A, Espigol-Frigolé G,
110 De Silva M, Hazleman BL. Azathioprine in giant cell arteritis/ Bosch X. Treatment of polymyalgia rheumatica: a systematic review.
polymyalgia rheumatica: a double-blind study. Ann Rheum Dis 1986; Arch Intern Med 2009; 169: 1839–50.
45: 136–38. 128 Stone JH, Tuckwell K, Dimonaco S, et al. Glucocorticoid dosages
111 Salvarani C, Macchioni P, Manzini C, et al. Infliximab plus and acute-phase reactant levels at giant cell arteritis flare in a
prednisone or placebo plus prednisone for the initial treatment of randomized trial of tocilizumab. Arthritis Rheumatol 2019;
polymyalgia rheumatica: a randomized trial. Ann Intern Med 2007; 71: 1329–38.
146: 631–39. 129 Devauchelle-Pensec V, Saraux L, Berthelot JM, et al. Assessing
112 Kreiner F, Galbo H. Effect of etanercept in polymyalgia rheumatica: polymyalgia rheumatica activity when C-reactive protein is
a randomized controlled trial. Arthritis Res Ther 2010; 12: R176. unavailable or uninterpretable. Rheumatology (Oxford) 2018;
113 Bonelli M, Radner H, Kerschbaumer A, et al. Tocilizumab in 57: 666–70.
patients with new onset polymyalgia rheumatica (PMR-SPARE): 130 Sagar R, Mackie S, W Morgan A, Stewart P, Abbas A. Evaluating
a phase 2/3 randomised controlled trial. Ann Rheum Dis 2022; tertiary adrenal insufficiency in rheumatology patients on long-term
81: 838–44. systemic glucocorticoid treatment. Clin Endocrinol (Oxf) 2021;
114 Devauchelle-Pensec V, Carvajal-Alegria G, Dernis E, et al. Effect of 94: 361–70.
tocilizumab on disease activity in patients with active polymyalgia 131 Palard-Novello X, Querellou S, Gouillou M, et al. Value of (18)
rheumatica receiving glucocorticoid therapy: a randomized clinical F-FDG PET/CT for therapeutic assessment of patients with
trial. JAMA 2022; 328: 1053–62. polymyalgia rheumatica receiving tocilizumab as first-line
115 Chino K, Kondo T, Sakai R, et al. Tocilizumab monotherapy for treatment. Eur J Nucl Med Mol Imaging 2016; 43: 773–79.
polymyalgia rheumatica: a prospective, single-center, open-label 132 Huwart A, Garrigues F, Jousse-Joulin S, et al. Ultrasonography and
study. Int J Rheum Dis 2019; 22: 2151–57. magnetic resonance imaging changes in patients with polymyalgia
116 Devauchelle-Pensec V, Berthelot JM, Cornec D, et al. Efficacy of rheumatica treated by tocilizumab. Arthritis Res Ther 2018; 20: 11.
first-line tocilizumab therapy in early polymyalgia rheumatica: 133 Laporte JP, Garrigues F, Huwart A, et al. Localized myofascial
a prospective longitudinal study. Ann Rheum Dis 2016; 75: 1506–10. inflammation revealed by magnetic resonance imaging in recent-
117 Akiyama M, Kaneko Y, Takeuchi T. Tocilizumab in isolated onset polymyalgia rheumatica and effect of tocilizumab therapy.
polymyalgia rheumatica: a systematic literature review. J Rheumatol 2019; 46: 1619–26.
Semin Arthritis Rheum 2020; 50: 521–25. 134 Leeb BF, Bird HA. A disease activity score for polymyalgia
118 Spiera R, Unizony S, Warrington KJ, et al. Sarilumab for relapse of rheumatica. Ann Rheum Dis 2004; 63: 1279–83.
polymyalgia rheumatica during glucocorticoid taper. N Engl J Med 135 Binard A, de Bandt M, Berthelot JM, Saraux A. Performance of the
2023; 389: 1263–72. polymyalgia rheumatica activity score for diagnosing disease flares.
119 Marsman DE, den Broeder N, van den Hoogen FHJ, Broeder AA, Arthritis Rheum 2008; 59: 263–69.
van der Maas A. Efficacy of rituximab in patients with polymyalgia 136 Twohig H, Mitchell C, Mallen C, Adebajo A, Mathers N. “I suddenly
rheumatica: a double-blind, randomised, placebo-controlled, proof- felt I’d aged”: a qualitative study of patient experiences of
of-concept trial. Lancet Rheumatol 2021; 3: e758–66. polymyalgia rheumatica (PMR). Patient Educ Couns 2015;
120 Zhang L, Li J, Yin H, et al. Efficacy and safety of tofacitinib in 98: 645–50.
patients with polymyalgia rheumatica: a phase 2 study. 137 Mackie SL, Hughes R, Walsh M, et al. “An impediment to living
Ann Rheum Dis 2023; 82: 722–24. life”: why and how should we measure stiffness in polymyalgia
121 Dejaco C, Kerschbaumer A, Aletaha D, et al. Treat-to-target rheumatica? PLoS One 2015; 10: e0126758.
recommendations in giant cell arteritis and polymyalgia 138 Yates M, Owen CE, Muller S, et al. Feasibility and face validity of
rheumatica. Ann Rheum Dis 2023; published online Feb 24. outcome measures for use in future studies of polymyalgia
https://doi.org/10.1136/ard-2022-223429. rheumatica: an OMERACT study. J Rheumatol 2020; 47: 1379–84.
122 Dejaco C, Duftner C, Cimmino MA, et al. Definition of remission 139 Mackie SL, Twohig H, Neill LM, et al. The OMERACT core domain
and relapse in polymyalgia rheumatica: data from a literature set for outcome measures for clinical trials in polymyalgia
search compared with a Delphi-based expert consensus. rheumatica. J Rheumatol 2017; 44: 1515–21.
Ann Rheum Dis 2011; 70: 447–53. 140 Twohig H, Owen C, Muller S, et al. Outcomes measured in
123 Aoki A, Kobayashi H, Yamaguchi Y. Predictors of long-term therapy polymyalgia rheumatica and measurement properties of
with glucocorticoid in polymyalgia rheumatica. Mod Rheumatol instruments considered for the OMERACT core outcome set:
2021; 31: 417–20. a systematic review. J Rheumatol 2021; 48: 883–93.
124 Cimmino MA, Parodi M, Caporali R, Montecucco C. Is the course 141 Twohig H, Mitchell C, Mallen CD, Muller S. Development and
of steroid-treated polymyalgia rheumatica more severe in women? psychometric evaluation of the PMR-Impact Scale: a new patient
Ann N Y Acad Sci 2006; 1069: 315–21. reported outcome measure for polymyalgia rheumatica.
125 Lee JH, Choi ST, Kim JS, et al. Clinical characteristics and Rheumatology (Oxford) 2023; 62: 758–65.
prognostic factors for relapse in patients with polymyalgia
rheumatica (PMR). Rheumatol Int 2013; 33: 1475–80. Copyright © 2023 Elsevier Ltd. All rights reserved.
1472 www.thelancet.com Vol 402 October 21, 2023
You might also like
- Icsd 3 PDFDocument383 pagesIcsd 3 PDFAndré S C de Oliveira100% (1)
- CR174Document57 pagesCR174vaidyamNo ratings yet
- CC and MCC List For DRG CodingDocument1 pageCC and MCC List For DRG Codinge-MedTools100% (2)
- The Neurology of Ageing: What Is NormalDocument11 pagesThe Neurology of Ageing: What Is NormalEsther EunikeNo ratings yet
- Clinician's Guide To ADHD Comorbidities in Children and Adolescents Case Studies 2019 PDFDocument148 pagesClinician's Guide To ADHD Comorbidities in Children and Adolescents Case Studies 2019 PDFfadel bilondatu100% (3)
- Polymyalgia Rheumatica 2023Document14 pagesPolymyalgia Rheumatica 2023Carlos Alfredo Vargas Quintero100% (1)
- 2015 PMR GuidelinesDocument7 pages2015 PMR GuidelinesAbdulAzizNo ratings yet
- 1 s2.0 S014067362301961X MainDocument16 pages1 s2.0 S014067362301961X MainAnaNo ratings yet
- Polymyalgia rheumatica Seminar reviews epidemiology, genetics, and treatmentDocument13 pagesPolymyalgia rheumatica Seminar reviews epidemiology, genetics, and treatmentjhonnyNo ratings yet
- Cushing's Syndrome (Lancet)Document16 pagesCushing's Syndrome (Lancet)Irma OnofreNo ratings yet
- Review: Paolo Spagnolo, Giulio Rossi, Rocco Trisolini, Nicola Sverzellati, Robert P Baughman, Athol U WellsDocument14 pagesReview: Paolo Spagnolo, Giulio Rossi, Rocco Trisolini, Nicola Sverzellati, Robert P Baughman, Athol U Wellsandra mNo ratings yet
- Gota NEJMDocument11 pagesGota NEJMPerejiloNo ratings yet
- Ankylosing Spondylitis Review JournalDocument12 pagesAnkylosing Spondylitis Review Journaloccha_fun08100% (1)
- PMR Review in The ClinicDocument16 pagesPMR Review in The Clinickromatin9462No ratings yet
- PARANEOPLASTICDocument8 pagesPARANEOPLASTICMuhammad Imran MirzaNo ratings yet
- Sjogren NEJMDocument9 pagesSjogren NEJMJosué DávilaNo ratings yet
- Advances in Managing Thyroid Eye DiseaseDocument9 pagesAdvances in Managing Thyroid Eye DiseaseHerpian NugrahadilNo ratings yet
- Aritmia 3Document1 pageAritmia 3Anonymous NVBCqKWHNo ratings yet
- MastitisDocument27 pagesMastitisLaprida RecoletaNo ratings yet
- Seminar: Joachim Sieper, Denis PoddubnyyDocument12 pagesSeminar: Joachim Sieper, Denis PoddubnyyDaniel FernandezNo ratings yet
- Smolen 2016Document16 pagesSmolen 2016downloadcmpNo ratings yet
- ArticleDocument9 pagesArticleVictor ValarezoNo ratings yet
- Multiple Sclerosis Lancet 2018Document15 pagesMultiple Sclerosis Lancet 2018Sarah Miryam CoffanoNo ratings yet
- Review: Maria Fleseriu, Fabienne Langlois, Dawn Shao Ting Lim, Elena V Varlamov, Shlomo MelmedDocument23 pagesReview: Maria Fleseriu, Fabienne Langlois, Dawn Shao Ting Lim, Elena V Varlamov, Shlomo MelmedAaron PeñaNo ratings yet
- Salvar An I 2012Document13 pagesSalvar An I 2012maandre123No ratings yet
- Primary Sjögren's Syndrome: Clinical PracticeDocument9 pagesPrimary Sjögren's Syndrome: Clinical PracticelauramarhNo ratings yet
- Salaffi2018 Article RelationshipBetweenInterstitia PDFDocument9 pagesSalaffi2018 Article RelationshipBetweenInterstitia PDFAurelia-Maria MireuțăNo ratings yet
- MJR 30 1 1Document2 pagesMJR 30 1 1landoo oooNo ratings yet
- 1 s2.0 S0140673615002755 mainFINALDocument11 pages1 s2.0 S0140673615002755 mainFINALTeju SutejoNo ratings yet
- Pola 2017Document10 pagesPola 2017RobertoNo ratings yet
- Clinical Practice: Ted R. Mikuls, M.D., M.S.P.HDocument11 pagesClinical Practice: Ted R. Mikuls, M.D., M.S.P.HRichy Escobar PNo ratings yet
- Gross Total Versus Subtotal Surgical Resection in the Management of CraniopharyngiomasDocument6 pagesGross Total Versus Subtotal Surgical Resection in the Management of CraniopharyngiomasshokoNo ratings yet
- Diagnosis and Management of Rheumatoid Arthritis A ReviewDocument13 pagesDiagnosis and Management of Rheumatoid Arthritis A ReviewLilik HandayaniNo ratings yet
- Go 4Document7 pagesGo 4Yuffaa AinayyaaNo ratings yet
- Gota - Med ClínicaDocument6 pagesGota - Med ClínicaDayana DávilaNo ratings yet
- ASIA Syndrome Following Breast Implant Placement: Case CommunicationsDocument3 pagesASIA Syndrome Following Breast Implant Placement: Case Communicationssilvana31No ratings yet
- Acromegaly Pathogenesis, Diagnosis, and ManagementDocument23 pagesAcromegaly Pathogenesis, Diagnosis, and ManagementPaolo MessinaNo ratings yet
- Rheumatoid Arthritis Lancet 2009Document14 pagesRheumatoid Arthritis Lancet 2009pispi_896094No ratings yet
- 2017 Article 141 Part9Document5 pages2017 Article 141 Part9Karina MonasaNo ratings yet
- Imaging of SpondylodiscitisDocument17 pagesImaging of SpondylodiscitisRoxana StanciuNo ratings yet
- PBD in Pediatric AchalasiaDocument6 pagesPBD in Pediatric AchalasiamuhammadfahmanNo ratings yet
- Spondylodiscitis Severity Code: Scoring System For The Classification and Treatment of Non-Specific SpondylodiscitisDocument9 pagesSpondylodiscitis Severity Code: Scoring System For The Classification and Treatment of Non-Specific SpondylodiscitisEduardo RodriguezNo ratings yet
- AnotherDocument11 pagesAnotherTudor DumitrascuNo ratings yet
- The Management of Diabetic Foot in The EmergencyDocument7 pagesThe Management of Diabetic Foot in The EmergencyIJAR JOURNALNo ratings yet
- Multiple Sclerosis Progression Time For A New Mechanism-Driven FrameworkDocument11 pagesMultiple Sclerosis Progression Time For A New Mechanism-Driven FrameworkasasakopNo ratings yet
- A Comprehensive Review of Sarcoidosis Treatment For PulmonologistsDocument20 pagesA Comprehensive Review of Sarcoidosis Treatment For PulmonologistsjaimeferNo ratings yet
- Fimmu 13 915081Document15 pagesFimmu 13 915081Zakia MaharaniNo ratings yet
- Review: Mircea Chirica, Luigi Bonavina, Michael D Kelly, Emile Sarfati, Pierre CattanDocument12 pagesReview: Mircea Chirica, Luigi Bonavina, Michael D Kelly, Emile Sarfati, Pierre CattanRonald MoraNo ratings yet
- Jurnal 2Document13 pagesJurnal 2Ainun Jariah FahayNo ratings yet
- The Rationale of Surgical Treatment in Pediatric Spine TuberculosisDocument6 pagesThe Rationale of Surgical Treatment in Pediatric Spine TuberculosisSpica KentNo ratings yet
- Prevention of Surgical Site Infections in Orthopaedic Surgery: A Synthesis of Current RecommendationsDocument16 pagesPrevention of Surgical Site Infections in Orthopaedic Surgery: A Synthesis of Current RecommendationsPankaj VatsaNo ratings yet
- Lancet Sclerosi MultiplaDocument15 pagesLancet Sclerosi MultiplaMr. LNo ratings yet
- Syndrom X in English, From My Dr. Thesis in 2004Document65 pagesSyndrom X in English, From My Dr. Thesis in 2004Mila VidinNo ratings yet
- LancetDocument11 pagesLancetvieira.beatrizNo ratings yet
- Choice of Tube Extremity For Emission of The Lowest Radiation Dose in Pediatric PatientsDocument5 pagesChoice of Tube Extremity For Emission of The Lowest Radiation Dose in Pediatric PatientsGênesis Ribeiro LeiteNo ratings yet
- AR para ManosDocument22 pagesAR para ManosAndres CasteloNo ratings yet
- Wormald 2019Document18 pagesWormald 2019araliNo ratings yet
- Update οn the diagnosis and management of systemic lupus erythematosusDocument12 pagesUpdate οn the diagnosis and management of systemic lupus erythematosusCarlos Enrique Almonte MarínNo ratings yet
- Lupus Diagnostico y Manejo BMJ 2020Document12 pagesLupus Diagnostico y Manejo BMJ 2020david231123No ratings yet
- Update On Gout 2012:, Nathalie BussoDocument5 pagesUpdate On Gout 2012:, Nathalie BussoMoha MohaNo ratings yet
- Maggot Debridement Therapy of Infected UlcersDocument12 pagesMaggot Debridement Therapy of Infected UlcersVonny Nurmalya MegawatiNo ratings yet
- Necrolytic Migratory Erythema Impact On Prognosis and Diagnosis of Glucagonoma A Case ReportDocument4 pagesNecrolytic Migratory Erythema Impact On Prognosis and Diagnosis of Glucagonoma A Case ReportHerald Scholarly Open AccessNo ratings yet
- Repetitive Strain Injury LANCET 2007Document8 pagesRepetitive Strain Injury LANCET 2007Alfredo Luiz CostaNo ratings yet
- Hip 2012 9568Document5 pagesHip 2012 9568Fadlu ManafNo ratings yet
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesFrom EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNo ratings yet
- Impacts of COVID-19 On Caregivers of Childhood Cancer SurvivorsDocument10 pagesImpacts of COVID-19 On Caregivers of Childhood Cancer Survivorsjudith retanaNo ratings yet
- Clinical Practice Guidelines For Management of Bipolar DisorderDocument16 pagesClinical Practice Guidelines For Management of Bipolar DisorderKavita kumariNo ratings yet
- Counting The Cost: Servaas Van Der Berg & Nic SpaullDocument32 pagesCounting The Cost: Servaas Van Der Berg & Nic Spaulljillian50% (2)
- Tulburare Depresiva SecundaraDocument5 pagesTulburare Depresiva SecundaraRamona Fodor100% (1)
- A Novel Clinical Grading Scale To Guide The Management of Crusted ScabiesDocument6 pagesA Novel Clinical Grading Scale To Guide The Management of Crusted ScabiesFelisiana KasmanNo ratings yet
- The Geriatric Patient Use of Acute Geriatrics UnitDocument7 pagesThe Geriatric Patient Use of Acute Geriatrics Unitlee suk moNo ratings yet
- RRT in ElderlyDocument8 pagesRRT in ElderlySupandy HasanNo ratings yet
- Weight-Gain in Psychiatric TreatmentDocument19 pagesWeight-Gain in Psychiatric Treatmentsvetlavb8063No ratings yet
- Springer: Tokyo Berlin Heidelberg New York Barcelona Budapest Hong Kong London Milan Paris Santaclara SingaporeDocument153 pagesSpringer: Tokyo Berlin Heidelberg New York Barcelona Budapest Hong Kong London Milan Paris Santaclara SingaporeCarlos EsescritorNo ratings yet
- RMO Assessment Form 2016Document8 pagesRMO Assessment Form 2016Tp HoangNo ratings yet
- Perspective: Treatment-Based Classification System For Low Back Pain: Revision and UpdateDocument10 pagesPerspective: Treatment-Based Classification System For Low Back Pain: Revision and UpdateVizaNo ratings yet
- HSRCDocument53 pagesHSRCAbhishek Kumar SharmaNo ratings yet
- The Use of Oral Human Grade Ivermectin With Supplements Known As Immunomodulators For Treating Patients With COVID 19 Infections at HomeDocument16 pagesThe Use of Oral Human Grade Ivermectin With Supplements Known As Immunomodulators For Treating Patients With COVID 19 Infections at HomeAthenaeum Scientific PublishersNo ratings yet
- Office of The Sangguniang Bayan: Municipality of Delfin AlbanoDocument17 pagesOffice of The Sangguniang Bayan: Municipality of Delfin AlbanoGrace Managuelod GabuyoNo ratings yet
- Merritt-Putnam Symposium 2017Document32 pagesMerritt-Putnam Symposium 2017Ruda AlessiNo ratings yet
- Risk Adjustment of Health-Care Performance MeasureDocument12 pagesRisk Adjustment of Health-Care Performance MeasureAmbarNo ratings yet
- Treatment of Comorbid Conduct Turgay AlmagorDocument14 pagesTreatment of Comorbid Conduct Turgay AlmagormailmanatNo ratings yet
- Social AnxietyDocument21 pagesSocial AnxietyRini DewiNo ratings yet
- CKD5 HDDocument10 pagesCKD5 HDsari murnaniNo ratings yet
- Improving Outcomes For Breast Cancer SurvivorsDocument280 pagesImproving Outcomes For Breast Cancer SurvivorsHồ Q. ThuậnNo ratings yet
- Final Manuscript Chapter 1 Group 101Document64 pagesFinal Manuscript Chapter 1 Group 101YoshNo ratings yet
- 1997 - Enhancing Sexuality - Therapis Guide PDFDocument97 pages1997 - Enhancing Sexuality - Therapis Guide PDFDan Simion0% (1)
- North American Journal of Medical SciencesDocument8 pagesNorth American Journal of Medical SciencesbacabacadongdongNo ratings yet
- Diabetes and Stroke: Effects, Outcomes, and ManagementDocument2 pagesDiabetes and Stroke: Effects, Outcomes, and ManagementBraithwaite UmentaNo ratings yet
- The Study of Primary Psychotic Disorders With Concurrent Substance Abuse in Terms of Their Diagnostic StabilityDocument12 pagesThe Study of Primary Psychotic Disorders With Concurrent Substance Abuse in Terms of Their Diagnostic StabilitySynthiaNo ratings yet