Professional Documents
Culture Documents
Review of Peripheral Blood and Bone Marrow Malignant Disease
Uploaded by
ashjanbaslaib0 ratings0% found this document useful (0 votes)
36 views112 pagesBlood and bone marrow disease
Original Title
Review of peripheral blood and bone marrow malignant disease
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentBlood and bone marrow disease
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
36 views112 pagesReview of Peripheral Blood and Bone Marrow Malignant Disease
Uploaded by
ashjanbaslaibBlood and bone marrow disease
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 112
Header
Review of Peripheral Blood and Bone
Marrow Morphology: Malignant Diseases
Subhead
Mark D. Fleming, M.D., D.Phil.
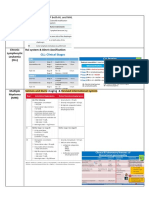
Hematopoietic Lineage Specific Markers
Hematopoietic T lymphoid Myeloid
CD45 (LCA) CD1a (immature) CD13
CD2 CD14 (monocytic)
Immaturity sCD3/cCD3 CD15
HLA-DR (MHC-II) CD4 CD33
CD34 CD5 CD64/65
TdT (lymphoid) CD7 (monocytic)
CD117 (myeloid) CD8 Myeloperoxidase
CD99 (immature) Lysozyme
B lymphoid
CD19 NK cell
CD20 CD16 Histochemistry
sCD22/cCD22 CD56 PAS (block-like in
CD10 (CALLA) ALL)
k/l Ig light chain MPO (myeloid)
sIg or cIg NSE (monocytic)
Normal B and T cell phenotypes
Acute Lymphoblastic Leukemia
Six year-old girl with T21 and cardiac
anomalies s/p repair now with lethargy
and pallor.
• WBC 5.7 K/uL
• Hb 8.7 g/dL
• Plt 95 K/uL
• 87% blasts
Peripheral blood,
flow cytometry:
• CD45- (dim)
• HLA-DR+
• CD19+
• CD20 variable+
• sCD22+
• CD10+
• sIg-
• CRLF2-
• TdT+
• T cell/myeloid-
TdT-
TdT+
DNA INDEX: 1.198
Cytogenetics:
47,XX,+21c[17]/56,sl,+X,dup(1)(q21q42),
add(2)(q37),+4,+6,+10,+14, +14,
+17,+21c,+mar[6]
B-ALL Cytogenetics
• High hyperdiploid B-ALL (51-66 • t(5;14)(q31;q32), IL3-@IGH
chromosomes) ~25% – Profound eosinophilia
- Corresponds to DNA Index of >1.16 – One of the few morphologically
- Gains of chromosomes 4, 10, 14, distinct ALLs
17, 21, X most common • t(1;19)(q23;p13.3), E2A-PBX1
- Most common cytogenetically • DS-ALL
evident karyotypic abnormality in
– Usually normal (47,+21c)
B-ALL
karyotype
• TEL-AML = ETV6-RUNX1 = – Cryptic CRLF2 translocations
t(12;21)(p13;q22) ~25%
– Cryptic translocation
• Need to do FISH or RT-PCR!
– Often associated with del 12p
(other copy of TEL)
– Most common translocation in B-
ALL
More B-ALL Cytogenetics
(bad actors)
• MLL rearranged • Ph-like B-ALL
– Most common ALL cytogenetics in – Tyrosine kinase fusions (e.g.,
infants EPOR, CRLF2)
– 11q23, multiple partners – ±JAK2/3 alterations
– Sometimes cryptic: FISH confirms – ± IKZF1 deletions
• Philadelphia chr positive (Ph+) • IKZF1 (Ikaros) deletions
– BCR-ABL, t(9;22)(q34;q11.2) • iAMP 21
– Karyotype/FISH/PCR • MYC
• RT-PCR p190: de novo ALL
• RT-PCR p210: CML and CML in blast – “L3” ALL is another disease!
crisis
• Hypodiploid ALL
– Fewer than 45 chromosomes
– Very poor prognosis
Bone marrow,
flow cytometry:
• CD45+ • sCD22+ • TdT-
• HLA-DR+ • CD10+ • T cell/myeloid-
• CD19+ • sIgM+
• CD20 + • Clonal sIgk
Burkitt Lymphoma/Leukemia
• Intermediate-sized lymphoid cells with mature chromatin and
deeply basophilic cytoplasm often with vacuolization.
– Lymphoma/leukemia are the same disease manifesting with different predominant
organ involvement: extramedullary tissues vs. blood/bone marrow
• Mature B cell immunophenotype
– CD45 bright/CD19/CD20/sCD22/CD10 positive
– Monotypic surface immunoglobulin kappa or lambda light chain
– Negative for CD34 and TdT
– Contrast with B-ALL that is often also CD10 positive, but has an otherwise immature
phenotype that is CD45 dim, TdT+, CD34±, and negative for sIg and often negative
for CD20.
• MYC rearrangement: brings MYC in proximity to the @Ig locus
enhancer, not a fusion cDNA/protein
– t(8;14)(q24;q32), MYC;@IGH
– t(8;22)(q24;q11), MYC;@IGL
– t(2;8)(p12;q24), MYC;@IGK
– (Sometimes del 11q, but this isn’t the boards answer)
12 y.o. boy with WBC 86.2 K/uL
and an anterior mediastinal mass
Flow
Peripheral blood
flow cytometry:
• CD45 dim+ • CD1a-
• HLA-DR- • CD2+
• CD117- • sCD3-
• CD34- • cCD3+
• TdT+ • CD5+
• CD7+
• CD10+ • CD4/8-
• Other B cell-
• Myeloid-
Cytogenetics:
– Normal karyotype
– FISH: chr 9p (CDKN2A) deletion
T lymphoblastic Leukemia/Lymphoma
• Distinction between leukemia • HOX11 (TLX1): 10q24
and lymphoma is “semantic” • HOX11L2 (TLX3): 5q35
• Many other hematopoietic
– Blood/bone marrow vs. tissue
transcription factors
manifestation of the same group of
diseases. • TAL1 translocations 1p32
– Leukemia often defined by the – Often cryptic interstitial deletion
presence of substantial marrow
involvement • Deletion of 9p is common
– P16/INK4A/CDKN2A
• Rearrangements between T cell
receptor loci and are most
common (unlike most B-ALL)
– TCR loci:
• a and d loci: 14q11.2
• b locus: 7q35
• g locus: 7p14-15
– Partner genes:
Bone marrow, CD1a-
flow cytometry: CD2+
sCD3-
CD45 dim+ cCD3+
HLA-DR+ CD5-
CD117 dim+ CD7+
CD34+ CD4-
TdT+ CD8-
CD19/20/22- CD13 dim+
CD10- Other myeloid-
T lymphoblastic Leukemia/Lymphoma
Immunophenotypes
• Often lack expression of one or more T lineage
markers:
– CD2, CD3, CD4, CD5, CD7, CD8
– May be CD10 (common ALL antigen/CALLA) positive
– Sometimes co-express myeloid markers
• Early T-precursor (ETP) phenotype
– Defined by gene expression pattern
– Immunophenotype is a surrogate:
• CD1a-, CD10-, CD8-, CD5 weak+ or negative
• Positive for one or more stem/myeloid markers: CD117, CD34,
HLA-DR, CD13, CD33, CD11b, CD65
Acute Myeloid Leukemia
16 y.o. girl with pancytopenia and
? peripheral blasts
Peripheral
Karyotype:
blood,
flow cytometry: 46,XX,t(15;17)(q22;q12)[20
• CD117+ • CD19/20/22- ]
• CD45 dim+
• HLA-DR- • CD13+ • CD2/CD5/CD7-
• CD34- • CD15+
• TdT- • CD64+ • MPO strongly+
Acute Promyelocytic Leukemia
• Defined by a retinoic receptor-a (RARA) translocation
- t(15;17)(q22;q12): PML;RARA
- All-trans retinoic acid (ATRA) sensitive
- Some variant translocations[e.g. t(11;17)(q23;q12)] are ATRA resistant
• Hypergranular Variant (typical or classic FAB M3)
- Hypergranular dysplastic promyelocytes, many with multiple Auer rods,
Intensely MPO+
- HLA-DR-/CD34-/CD117+/CD15+/CD64+/CD2-
• One of the few HLA-DR negative acute leukemias (T-ALL, AMKL, and some AMoL being
the other major exceptions)
• Microgranular variant (FAB M3v)
• Bi-lobed blasts with submicroscopic granules, only occasional
hypergranular promyelocytes, still intensely MPO+
- Often has a variant immunophenotpe: HLA-
DR+/CD34+/CD117+/CD15+/CD64+/CD2+
16 y.o. boy with a h/o AML s/p SCT
now with pancytopenia
Bone marrow, flow
cytometry: • CD7 dim+
• CD34+ • Other T cell-
• CD45 dim+ • CD13 dim+ • B cell-
• HLA-DR variably+ • CD33 dim+ • TdT-
• CD117+ • CD64/CD65 variably+ • MPO+
Cytogenetics
• Karyotype:
– 46,XY,inv(16)(p13.1q22)[3]/47,sl,+21[15]/46,XY[2]
• FISH:
– nuc ish(CBFBx2)(5'CBFB sep 3'CBFBx1)[84/200]
– Positive for a CBFB rearrangement (42.0% of cells)
Acute myelomonocytic leukemia with
inv(16)(p13.1q22) (FAB M4Eo)
11 y.o. girl with leukocytosis, anemia
and thrombocytopenia
Bone marrow aspirate: 10% blasts, dysplastic myeloid maturation
Bone marrow, flow cytometry:
• CD45 dim+ • CD19+
• HLA-DR+ • CD20/CD22-
• CD117 • CD10-
• CD34+
• CD13+
• TdT-/+ • CD33+
• MPO+ • Other myeloid-
• Cytogenetics
- 46, XX,t(8;21)(q22;q22)[15]/46,XX[5]
• FISH:
- Positive for an ETO/AML rearrangement (65% of cells).
Acute myeloid leukemia with t(8;21) (FAB M2)
“Core binding factor” (CBF) acute myeloid leukemia
• inv(16)(p13.1q22) or t(16;16)(p13.1;q22)
– FAB M4Eo
• Myelomonocytic differentiation with abnormal eosinophils
• “Eo-basos”—eosinophil precursors with basophilic granules.
– CBFB-MYH11
– FISH or RT-PCR necessary; often cryptic on karyotype
• t(8;21)(q22;q22)
– FAB M2 morphology
• Myeloid leukemia with maturation
• Salmon pink granules and long, slender Auer rods
– RUNX1-RUNX1T1; AML-ETO
• RUNX1 = AML1 = CBFA
– Karyotype or FISH
These and certain other AML are defined by cytogenetics, not blasts >30%
Infants with leukemia
Infant female with WBC 100 K cells/ul
Peripheral blood,
flow cytometry: Karyotype:
• CD45 dim+ • CD19+ • CD15-/+ 46,XX,t(4;11)(q21;q23)[20]
• HLA-DR+ • CD20-
• CD34+ • sCD22+ • T cell-
• TdT+ • CD10- • Other myeloid-
• sIg-
Infant female with WBC 100 K cells/ul
and multiple non-tender, violaceous
skin nodules
Peripheral blood flow
cytometry:
• CD45 dim+ • CD13 dim+
• HLA-DR+ • CD33-
• CD117 variably+ • CD14+
• CD34- • CD64+
• TdT- • CD65+
• MPO-
• B cell-
• T cell-
• Karyotype:
• 46,XX,t(6;13)(q27;q14),inv(10)(p12.2q21.1)[14]//46,XY[6]
• FISH:
nuc ish(MLLx3)(5'MLL sep 3'MLLx1)[176/200]
• Positive for a rearrangement of the MLL gene at 11q23 (88.0% of cells)
Acute monoblastic leukemia
• Large blasts, NSE+, often involving skin, CNS and
other extramedullary sites.
• MLL translocations common, particularly in
infants
– Many translocation partners
• t(9;11)(p23;q23), t(6;11)(q27;q23), t(10;11)(p12;q23),
t(11;19)(q23;p13.3), etc…
• t(4;11)(q21;q23) seen in ALL is unusual in AML
– Often not identifiable by karyotype
• MLL FISH required
– MLL translocations also seen in biphenotypic and
therapy-related leukemias
30-week pre-term female infant with
hydrops and common atrio-ventricular
canal
• WBC 76.1 K cells/uL
– 24% NRBCs
– 68% blasts
• HCT 39.5%
• PLT 360 K cells/uL
• PT/PTT 64/73.5, fibrinogen <35.
• Uric acid 7.8, LDH 2885
Peripheral blood, flow
cytometry:
• CD45 dim+
• HLA-DR-
• CD117+
• CD34+
• CD61 bright+
• CD41 bright+
• CD71 variable+
• CD4 variable+
• CD7 variable+
• CD56 subset+
• CD13 dim+
• CD33 dim+ to negative
• CD64 dim+ to negative
• Negative for HLA-DR, CD2,
CD10, CD14, CD15, CD16,
CD19, CD20, and MPO.
Transient Abnormal Myelopoiesis (TAM) of
Down Syndrome
• AKA: Transient Myeloproliferative Disorder (TMD)
• “Megakaryoblastic” proliferation occurring prior to or within days
of birth.
• 4B’s: Big, blue, blebby blasts
• CD34/CD117/CD71/CD41/CD61/CD4/CD7/CD11b/CD13+ blasts
that are HLA-DR-
• TAM associated with trisomy 21 and somatic GATA1 exon 2
mutations
– Results in expression of only a short isoform of GATA1
• 20-30% of individuals with TAM will evolve to acute
megakaryoblastic leukemia (DS-AMKL)
– Typically <30 months of age
– Acquisition of secondary chromosomal aberrations.
– Acquisition of secondary somatic mutations.
• Cohesin components (53%), CTCF (20%), EZH2, KANSL1 and other epigenetic regulators
(45%), Signaling pathways (47%).
• Immunophenotype indistinguishable from TAM.
Bone marrow aspirate, flow cytometry:
Blasts: 31% of viable events
• CD45 dim+
• CD117 variable+
• CD61+
• CD41+
• CD4+
• CD13 subset+
• CD33 diim+
• Negative: CD13, HLA-DR, CD56, CD2 and CD34
Reticulin
• 46,XY,add(1)(p34),t(1;2)(p13;p21),add(2)(p13),t(6;21)
(q23;q22),
add(14)(q22),del(17)(p11.2),add(22)(q13)[cp3]/46,X
Y[17]
• Acute Megakaryoblastic Leukemia (FAB M7)
• t(1;22)(p13;q13) RBM15-MKL1 = OTT-MAL
– Acute megakaryoblastic leukemia
– Infants without Down syndrome
• 18 mo. male with leukocytosis since the age of 10
mos.
• Non-dysmorphic
• Heart murmur
• Otherwise well
WBC 36.12 K cells/uL H 5.97 - 10.49
Hemoglobin 11.4 g/dL 11.0 - 12.8
Platelet 59 K cells/uL L 208 - 413
Neutrophil/Band 49 % 32 - 75
Lymphocyte 36 % 11 - 54
Monocyte 6% 4-9
Eosinophil 5% H 1-4
Atypical Lymphocyte 2% 0-4
Promyelocyte 1% 0-1
Other Cell 2%
NA
NRBC 1 0-1
Other data:
• HbF increased for age
• Bone marrow karyotype: 46,XY
• FISH negative for: monosomy 7,
trisomy 8, and a partial deletion of 7q.
• PTPN11 gene coding sequence:
c.227A>G/p.Glu76Gly (somatic)
Juvenile Myelomonocytic Leukemia (JMML)
Diagnostic criteria
I. Clinical and hematologic features (all 4 features mandatory)
• PB monocyte count ≥1 × 109/L
• Blast percentage in PB and BM <20%
• Splenomegaly
• Absence of Philadelphia chromosome (BCR/ABL1 rearrangement)
II. Genetic studies (1 finding sufficient)
• Somatic mutation in PTPN11 or KRAS or NRAS
• Clinical diagnosis of NF1 or NF1 mutation
• Germline CBL mutation and loss of heterozygosity of CBL
III. For patients without genetic features, besides the clinical and hematologic features
listed under I, the following criteria must be fulfilled:
• Monosomy 7 or any other chromosomal abnormality or at least 2 of the following
criteria:
• Hemoglobin F increased for age
• Myeloid or erythroid precursors on PB smear
• GM-CSF hypersensitivity in colony assay
• Hyperphosphorylation of STAT5
Blood 2016 127:2391-2405
Other
21 yo male with a longstanding history of
Crohn's disease treated with immune
suppression, including 6-MP
• Six-week history of symptoms consistent with macrophage
activation syndrome (MAS)
• s/p MAS-directed therapy including steroids, cyclosporine,
anakinra, and infliximab, with little improvement.
Bone marrow,
flow cytometry:
CD2 bright+ CD56+
~11% of events CD3 dim+ to negative Granyme/TIA1/PRF-
Lymphs with increased SSC CD5-
CD7+ B cell marker -
CD45 bright+ TCRab- Myeloid marker-
TdT- TCRg/d+
-
CD56
• Karyotype:
46,XY,i(7)(q10),+8,der(8;22)(q10;q10)
Hepatosplenic g/d-T cell lymphoma
• Rare leukemia/lymphoma
• Aberrant g/d T-cell phenotype
• Isochromosome 7q in most cases
• Sporadic: teenage males
• Immunosuppression associated: especially IBD
• Presents with
hepatosplenomegaly/cytopenias/HLH
Hemophagocytic lymphohistiocytosis/HLH
• Familial
– Usually <18 mos of age
– Decreased NK cell function
– Mutations in genes responsible for cytotoxic granule
exocytosis/function
• Infection
– Herpes viruses (esp. EBV)
– Many, many others…
• Malignancy-associated
– T cell lymphomas
– Anaplastic large cell lymphoma
Treat the underlying cause…e.g., HSCT for familial forms,
antimicrobials for infections, tumor-directed chemotherapy
16 y.o. male with a history of chronic
digital warts and an episode of atypical
mycobacterial lymphadenitis now with
pancytopenia
CD3
CD34
Diagnostic findings
• Morphology:
– Hypercellular marrow with multilineage dysplasia
and 4% blasts
• Cytogenetics:
– 45,XY,-7[13]/46,XY[7]
• Genetics:
– GATA2 c.1113G>T, p.N371K (germline)
Myelodysplastic Syndromes (MDS)
Clonal hematopoietic disorders characterized by:
• Cytopenias
– (Hgb <10g/dL ANC <1800/uL, Plt <100k/uL)
• Dysplasia (in >10% of a lineage)
• Recurrent genetic abnormalities
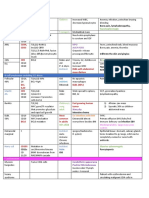
MDS categories WHO 2016
Republished with permission of The American Society of Hematology, from Bood, Arber DA, et al, 127,
2016; permission conveyed through Copyright Clearance Center, Inc.
Germline predisposition to MDS/AML
• Myeloid neoplasms with germ line predisposition without a preexisting
disorder or organ dysfunction
– AML with germ line CEBPA mutation
– Myeloid neoplasms with germ line DDX41 mutation
• Myeloid neoplasms with germ line predisposition and preexisting platelet
disorders
– Myeloid neoplasms with germ line RUNX7 mutation
– Myeloid neoplasms with germ line ANKRD26 mutation
– Myeloid neoplasms with germ line ETV6 mutation
• Myeloid neoplasms with germ line predisposition and other organ
dysfunction
– Myeloid neoplasms with germ line GATA2 mutation
– Myeloid neoplasms associated with BM failure syndromes
– Myeloid neoplasms associated with telomere biology disorders
– JMML associated with neurofibromatosis, Noonan syndrome or
– Noonan syndrome-like disorders
– Myeloid neoplasms associated with Down syndrome
Blood 2016 127:2391-2405
• 19 year old female with recent fatigue and a 5
lb weight loss
• Wisdom teeth extracted, and one month later
had difficult-to-control bleeding from the
extraction sites, WBC 469, Hgb 7.9, Hct 21.7,
Plt 671, showing a neutrophilic leukocytosis
with a left shift.
• Bone marrow biopsy/aspirate
90%
4.8%
• 46,XX,t(9;22)(q34;q11.2)[20]
• FISH positive for BCR-ABL1 rearrangement in 196/200 cells
• RT-PCR positive for p210 transcript
Chronic Myeloid Leukemia
• Clonal stem cell disorder • Evolves to:
– Classified as a – “Blast crisis”
myeloproliferative – Typically B-ALL in pediatric
neoplasm (MPN) patients
• Characterized by: – Myeloid more common in
– Neutrophilic leukocytosis adults
with a left shift • Other MPN
– Basophilia/Eosinophilia – Polcythemia vera (PV)
– Thromobocytosis • JAK2 V617F
– Anemia – Essential thromobocytosis
• Defined by: (ET)
• JAK2 V617F or CALR
– BCR-ABL translocation mutations
9 y.o. male with pancytopenia, bone
pain and “diffuse marrow signal
abnormality” by MRI
Desmin Myogenin
• Karyotype
– 49,XY,t(2;13)(q36;q14),+12,+14,+r[cp4]/46,XY[16]
• FISH
– nuc ish(FOXO1x2)(5'FOXO1 sep 3'FOXO1x1)
[27/500],(EWSR1x2)[500]
“Leukemic” Alveolar Rhabdomyosarcoma
Thank you!
mark.fleming@childrens.harvard.edu
Header
Supplemental Questions to Malignant Peripheral
Blood and Bone Marrow Review
Subhead
Mark D. Fleming, M.D., D.Phil.
Hx: 16 yo boy with pallor and bruising. Blood smear shows
anemia, thrombocytopenia, leukocytosis (100,000/mm3,
90% immature cells). Flow cytometry on blood shows cells
are TdT+, CD10+, CD3+, CD7+, CD4+, and CD8+.
A. AML
B. B-cell ALL
C. T-cell ALL
D. Hematogones
E. Mononucleosis
A. AML
B. B-cell ALL
C. T-cell ALL
D. Hematogone hyperplasia
E. Mononucleosis
Comment: The cells are T lymphoblasts by morphology
and flow cytometry. The atypical lymphs in mononucleosis
are T cells, but are larger and have abundant cytoplasm
often with scant cytotoxic granules and are mostly CD8
bright positive Hematogones are rarely seen in peripheral
blood. Very high white count, male sex and age, even in
the absence of a mediastinal mass, should make one think
about T-cell ALL
Hx: 6 yo boy with bone pain. Blood smear shows
pancytopenia, and 5% circulating immature cells (pictured).
Flow cytometry on marrow shows 80% cells are TdT+,
CD10+, CD19+, CD20-.
A. AML
B. B-cell ALL
C. T-cell ALL
D. Hematogones
E. Mononucleosis
A. AML
B. B-cell ALL
C. T-cell ALL
D. Hematogones
E. Mononucleosis
Comment: These cells are morphologically lymphoid and
have an immature B phenotype by flow cytometry.
Hematogones should show more of a spectrum of
maturation and are unlikely to completely replace the
normal marrow elements. Burkitt leukemia (BL) is certainly
in the differential, particularly given the vacuolization of the
cells. The immunophenotype is supportive of BL other than
the TdT positivity and lack of CD20 expression. Clonal
surface immunoglobulin staining and a MYC translocation
by cytogenetics/FISH would also be present in BL
Hx: 7 yo boy with an recent onset of vomiting and lethargy.
Blood smear shows increased neutrophils with a left shift and
8% abnormal cells. Bone marrow contains 60% of the same
cells. Flow cytometry shows that the cells are TdT-, CD10+,
CD19+, CD20+, sIg+.
A.Burkitt L/L
B.B-cell ALL
C.T-cell ALL
D.Hematogones
E.DLBCL
A. Burkitt L/L
B. B-cell ALL
C. T-cell ALL
D. Hematogones
E. DLBCL
Comment: Flow cytometry shows mature CD10+ B-cells, and
the morphology is that of Burkitt lymphoma, which occasionally
can have a leukemic phase. DLBCL is certainly a
consideration, but a truly leukemic phase (rather than just
marrow involvement), would be really unusual. A MYC
rearrangement by cytogenetics/FISH would also be
diagnostically helpful.
Hx: 13 yo boy with fatigue, weight loss, night sweats and
splenomegaly. Peripheral blood shows anemia,
thrombocytosis and leukocytosis (300,000/mm3).
A. Leukemoid Reaction
B. ALL
C. CML
D. JMML
E. AML
A. Leukemoid Reaction
B. ALL
C. CML
D. JMML
E. AML
Comment: A neutrophilic leukocytosis and a left shift with a
basophilia and thrombocytosis without increased blasts are
typical of chronic phase of CML. Cytogenetics/FISH
showing t(9;22)(q34;q11.2) would be diagnostic.
Leukemoid reaction is also in the differential, but basophilia
and an absence of monocytosis would be a bit unusual.
JMML is a disease of much younger children (typically <4,
certainly <8) and nearly always is associated with
thrombocytopenia.
Hx: 2 yo girl with new onset of fever and bronchitis. Has
maculo-papular rash and hepatosplenomegaly. Blood smear
has leukocytosis (100,000/mm3), anemia and
thrombocytopenia. Ancillary tests include fetal hemoglobin of
80% and normal blood karyotype.
A. Leukemoid Reaction
B. ALL
C. CML
D. JMML
E. AML
A. Leukemoid Reaction
B. ALL
C. CML
D. JMML
E. AML
Comment: Marked leukocytosis including monocytosis
without increased blasts or a basophilia are typical. As are
trombocytopenia and anemia often accompanied by
erythroblastosis. Elevation of fetal hemoglobin is characteristic
of JMML. Cytogenetics are typically normal and a BCR/ABL1
fusion is not present. Somatic mutations in the RAS signaling
pathway are common.
Hx: 1 yo boy with pallor and a rash. Blood smear shows
pancytopenia and circulating abnormal cells.
A. AML
B. CML
C. JMML
D. ALL
E. LGL leukemia
A. AML
B. CML
C. JMML
D. ALL
E. LGL leukemia
Comment: The large blasts with ample cytoplasm and
prominent nucleoli are suggestive of AML, but the Auer rod
is diagnostic of AML!
Hx: 8 yo boy with bruising. Blood smear shows anemia,
thrombocytopenia, and leukocytosis (30,000/mm3, 50%
blasts). Flow cytometry on marrow shows 50% blasts with
TdT+, MPO+, CD13+, CD33+, partial CD19+.
A. AML
B. CML
C. ALL
D. MDS
E. LGL Leukemia
A. AML
B. CML
C. ALL
D. MDS
E. LGL Leukemia
Comment: Morphology shows dysplastic myeloid maturation,
blasts with “salmon pink granules,” and a large Auer rods. Flow
cytometry shows a myeloid phenotype with coexpression of
CD19 and TdT. Although this is a “mixed” myeloid and B
lymphoid phenotype (? Mixed Phenotype Acute
Leukemia/MPAL) this constellation of findings is highly
associated with with t(8;21)(q22;q22) and RUNX1/RUNX1T1
fusion (i.e., AML with a recurrent cytogenetic abnormality) and
is defined as such as AML regardless of the phenotype or blast
count.
Hx: 8 yo girl with fever and palpable, non-painful macular
skin lesions. Blood smear shows anemia,
thrombocytopenia, and leukocytosis (140,000/mm3, 60%
blasts). Auer rod are not present. Flow cytometry shows
60% blasts that are CD34+, CD13+, CD33+, CD64+,
CD11b+/-, MPO-/+.
A. Chediak-Higashi
B. Basophilic Leukemia
C. AML, M4Eo
D. APML
E. ALL
A. Chediak-Higashi
B. Basophilic Leukemia
C. AML, M4Eo
D. APML
E. ALL
Comment: The blasts have a monocytic morphology a a
myelomonocytic phenotype, so this is AML. The strange,
darkly granulated cells are abnormal eosinophils—“Eo-
Basos”—a morphology that correlates with a karyotype of
inv(16) or t(16;16).
Hx: 13 yo girl with fever and swelling of one leg. Blood
smear shows anemia and thrombo-cytopenia. WBC
3400/mm3 with marked left shift. Marrow has 82% immature
myeloid cells as shown. Flow cytometry on marrow shows
MPO+, CD33+, CD13 partial+, HLA-DR-, CD34-.
A. Toxic maturation arrest
B. APML
C. CML
D. Mast cell leukemia
E. Technical artifact
A. Toxic maturation arrest
B. APML
C. CML
D. Mast cell leukemia
E. Technical artifact
Comment: Atypical promyelocytes, which may have multiple
Auer rods, rather than blasts characterize acute promyelocytic
leukemia (APML), which is associated with t(15;17) and a
PML/RARA fusion. These “blast equivalents” are typically
HLA-DR and CD34 negative
Hx: 19 yo girl with history of treatment for ALCL 2 years
prior. Now with persistent pancytopenia (WBC 800/mm3, no
circulating blasts). Marrow has 80% abnormal cells that by
flow cytometry are MPO-, CD33+, CD34-, CD13+, CD11b+,
CD14+.
A. Relapsed ALCL
B. JMML
C. ALL
D. de novo AML
E. Therapy-related AML
A. Relapsed ALCL
B. JMML
C. ALL
D. De novo AML
E. Therapy-related AML
Comment: The morphology and flow cytometry are those
of monoblasts, which is characteristic of therapy-related
AML, especially with rearrangements of the MLL gene at
chromosome 11q23.
Hx: 1 yo boy with fever and weight loss. Blood shows
anemia and neutropenia with 5% circulating blasts. Marrow
has 95% abnormal cells that by flow cytometry are MPO-,
CD33+, CD34-, HLA-DR-, CD41+, CD61+.
A. AML
B. AMkL
C. TAM
D. Neuroblastoma
E. Medulloblastoma
A. AML
B. AMkL
C. TAM
D. Neuroblastoma
E. Medulloblastoma
Comment: The immunophenotype and marrow
replacement indicate the megakaryoblastic variant of AML.
Megakaryoblasts may be small, resembling lymphoblasts.
Platelet-like cytoplasmic buds are common, but not
specific.
Hx: 6 mo girl with a large abdominal mass and elevated
serum catecholamines. Bone marrow aspirations contains
the cells pictured. Flow cytometry shows the cells to be
CD56+.
A. AML/myeloid sarcoma
B. Metastatic Wilms tumor
C. Osteoblasts
D. NK cell leukemia/lymphoma
E. Metastatic neuroblastoma
A. AML/myeloid sarcoma
B. Metastatic Wilms tumor
C. Osteoblasts
D. NK cell leukemia/lymphoma
E. Metastatic neuroblastoma
Comment: Clumps of small cells are most likely solid tumor.
CD56 not only marks natural killer cells but is also a neural
cell adhesion molecule. “Small” cells, sometimes associated
with pink fibrillary neuropil in the clinical context of elevated
catecholamines is characteristic of neuroblastoma. Clumps
of osteoblasts, which are common in aspirates from children,
can be mistaken for metastatic tumor
You might also like
- PDFDocument86 pagesPDFXuan TuanNo ratings yet
- DD HematologyDocument43 pagesDD HematologyDemianaNo ratings yet
- LMA Van Der Velden PDFDocument88 pagesLMA Van Der Velden PDFKarla Novoa PérezNo ratings yet
- Leukemia AcuteDocument7 pagesLeukemia AcutefallstarrNo ratings yet
- T NK CellDocument117 pagesT NK CellPpds MtatasuhartaNo ratings yet
- Leukocyte DisordersDocument20 pagesLeukocyte DisordersRaymond MalubayNo ratings yet
- 07 Flow Cytometric Findings in AMLDocument13 pages07 Flow Cytometric Findings in AMLcandiddreamsNo ratings yet
- 03 - Approach Hematolymphoid NeoplasmsDocument119 pages03 - Approach Hematolymphoid NeoplasmscandiddreamsNo ratings yet
- 06 Flow Cytometry in Diagnosis of ALLDocument30 pages06 Flow Cytometry in Diagnosis of ALLcandiddreamsNo ratings yet
- Minimal Residual Disease - PGPDocument76 pagesMinimal Residual Disease - PGPabhinav_choudhary03No ratings yet
- Haematology-Pdf - 1Document91 pagesHaematology-Pdf - 1shreyNo ratings yet
- Immunohistochemical Classification of Haematolymphoid TumoursDocument86 pagesImmunohistochemical Classification of Haematolymphoid TumoursNGUYEN QUYNHNo ratings yet
- Hemepath 10 19 17Document2 pagesHemepath 10 19 17Phoebe AjeroNo ratings yet
- Molecular - Uniparental Disomy:: NPM1 Frequently Harbors A 4 BP Insertion in LeukemiaDocument16 pagesMolecular - Uniparental Disomy:: NPM1 Frequently Harbors A 4 BP Insertion in LeukemiaKHNo ratings yet
- Role of Chemistry Lab in Diagnosis & TreatmentDocument34 pagesRole of Chemistry Lab in Diagnosis & TreatmentJacinta GachokiNo ratings yet
- 11-23-21 White Blood Cell DisordersDocument80 pages11-23-21 White Blood Cell DisordersdeNo ratings yet
- 1 Acute LeukemiaDocument14 pages1 Acute Leukemiaسمير هزاعNo ratings yet
- An Interesting Hematopathology Case: Christopher Julien PGY2Document41 pagesAn Interesting Hematopathology Case: Christopher Julien PGY2Christopher JulienNo ratings yet
- Molecular Diagnosis: in Oncology & GeneticsDocument119 pagesMolecular Diagnosis: in Oncology & GeneticsErika ArnitasariNo ratings yet
- Immunophenotyping - An Introduction by Brig Tahir Aziz AhmedDocument65 pagesImmunophenotyping - An Introduction by Brig Tahir Aziz AhmedOmair RiazNo ratings yet
- 11 DR Endang SRH Pitfall in B-Cell Non Hodgkin LymphomaDocument74 pages11 DR Endang SRH Pitfall in B-Cell Non Hodgkin LymphomaMita AdrianiNo ratings yet
- WhddidsorhkDocument50 pagesWhddidsorhkestherin909No ratings yet
- Hematologic Pathology p65-87Document23 pagesHematologic Pathology p65-87zeroun24100% (1)
- Leucemias Agudas: Kenny Mauricio Galvez HematologiaDocument62 pagesLeucemias Agudas: Kenny Mauricio Galvez HematologiaMichelle Ocampo ValenciaNo ratings yet
- Back Up Slide ALL SkingDocument20 pagesBack Up Slide ALL SkingFebry BieluciousNo ratings yet
- CD MneumonicDocument9 pagesCD Mneumonicgaa5No ratings yet
- Molecular Diagnosis: in Oncology & GeneticsDocument101 pagesMolecular Diagnosis: in Oncology & GeneticsSorin LazarNo ratings yet
- Acute Leukemias PDFDocument126 pagesAcute Leukemias PDFimran khanNo ratings yet
- Medicine2 - Myeloproliferative, Lymphoproliferative WorkshopDocument118 pagesMedicine2 - Myeloproliferative, Lymphoproliferative Workshopapi-3762917100% (1)
- Case 5 Workbook and DiscussionDocument14 pagesCase 5 Workbook and DiscussionBrahmananda ChakrabortyNo ratings yet
- Devesh Mishra Patho NotesDocument17 pagesDevesh Mishra Patho Notesmilli6No ratings yet
- Limfoproliferari Cronice MaligneDocument18 pagesLimfoproliferari Cronice MaligneAlice MuscaNo ratings yet
- Blastic Plasmacytoid Dendritic Cell Neoplasm. From Origin of The Cell To Targeted Therapies. 2016Document11 pagesBlastic Plasmacytoid Dendritic Cell Neoplasm. From Origin of The Cell To Targeted Therapies. 2016Eunice RojasNo ratings yet
- Immunology ROAMSDocument16 pagesImmunology ROAMSvkNo ratings yet
- Chronic Lymphocytic Leukemia (CLL) : Curs An IV - Limba Engleza 2012-2013Document49 pagesChronic Lymphocytic Leukemia (CLL) : Curs An IV - Limba Engleza 2012-2013Tresor MbuyiNo ratings yet
- Bone Pain, Lymphadenopathy,: CD34, CD33Document2 pagesBone Pain, Lymphadenopathy,: CD34, CD33Gabriella Santa LuciaNo ratings yet
- Lymphoproliferative Disorders: Chronic Lymphocytic Leukemia-CLL Hairy Cell Leukemia Plasma Cell DisordersDocument42 pagesLymphoproliferative Disorders: Chronic Lymphocytic Leukemia-CLL Hairy Cell Leukemia Plasma Cell DisordersyosefNo ratings yet
- AML Pita DR MardiahDocument71 pagesAML Pita DR MardiahSarly Puspita AriesaNo ratings yet
- Lecture 17 SlidesDocument44 pagesLecture 17 SlidesAniruddha RoyNo ratings yet
- Hemat 3 Notes 4the Chronic Lymphocytic Leukemias and LymphomaDocument11 pagesHemat 3 Notes 4the Chronic Lymphocytic Leukemias and LymphomaAadya RoshanNo ratings yet
- Acute LeukemiasDocument48 pagesAcute LeukemiaslaibaNo ratings yet
- ადამიანის CD ანტიგენებიDocument1 pageადამიანის CD ანტიგენებიEMD GROUP100% (1)
- Acute Lymphocytic Leukemia: MR: Mohammed Mahmoud AlhajDocument14 pagesAcute Lymphocytic Leukemia: MR: Mohammed Mahmoud Alhajحسن محمدNo ratings yet
- Acute Myeloid Leukemia - AML: Clinical BackgroundDocument12 pagesAcute Myeloid Leukemia - AML: Clinical BackgroundNyxa AbdullaNo ratings yet
- Lymphoproliferative DisordersDocument36 pagesLymphoproliferative DisordersBrett FieldsNo ratings yet
- ' / 5 Introduction of LeukemiasaDocument37 pages' / 5 Introduction of LeukemiasashaikhaboausaibaNo ratings yet
- 2nd BM NotesDocument1 page2nd BM NotesJ.P. PepitoNo ratings yet
- BoardReviewPart2B MalignantHemePathDocument207 pagesBoardReviewPart2B MalignantHemePathMaria Cristina Alarcon NietoNo ratings yet
- CD染色Document2 pagesCD染色陳以佑No ratings yet
- Solastra Tech Spec Sheet BrochureDocument5 pagesSolastra Tech Spec Sheet BrochurecandiddreamsNo ratings yet
- Lymphoma SymposiumDocument161 pagesLymphoma SymposiummaomaochongNo ratings yet
- IHC - InterpretareDocument185 pagesIHC - InterpretareAnca NeaguNo ratings yet
- Aml Patho Physiology & Classification - V RocchaDocument61 pagesAml Patho Physiology & Classification - V RocchaThuy NguyenNo ratings yet
- Hematopoietic Markers: Chromogranin SynaptophysinDocument1 pageHematopoietic Markers: Chromogranin SynaptophysinJUSASBNo ratings yet
- Acute Lymphoblastic Leukemia (ALL)Document14 pagesAcute Lymphoblastic Leukemia (ALL)Med PhuongNo ratings yet
- LNs HNDocument190 pagesLNs HNNinna Isabel VictorioNo ratings yet
- Cancer CytogeneticsDocument48 pagesCancer CytogeneticsDr.Santosh KumarNo ratings yet
- LeukemiasDocument31 pagesLeukemiasIsaac MwangiNo ratings yet
- Fast Facts: CAR T-Cell Therapy in Diffuse Large B-Cell Lymphoma: A practical resource for nursesFrom EverandFast Facts: CAR T-Cell Therapy in Diffuse Large B-Cell Lymphoma: A practical resource for nursesNo ratings yet
- Fantastic Yeasts and Where To Find Them: The Hidden Diversity of Dimorphic Fungal PathogensDocument9 pagesFantastic Yeasts and Where To Find Them: The Hidden Diversity of Dimorphic Fungal PathogensNithin SakthiNo ratings yet
- BACTERIOFERRITINDocument5 pagesBACTERIOFERRITINnurulunismuhNo ratings yet
- Week 10 Gene Environment InteractionDocument10 pagesWeek 10 Gene Environment InteractionGhulam MustafaNo ratings yet
- Anticancer For MedicineDocument81 pagesAnticancer For MedicineYusra SanyNo ratings yet
- Bioinformatika Dan Aplikasi Pada Bidang KesehatanDocument20 pagesBioinformatika Dan Aplikasi Pada Bidang Kesehataneka sukmawatidewiNo ratings yet
- Animal Cell Culture Book FreshneyDocument3 pagesAnimal Cell Culture Book FreshneyArchana Kumari Shaw100% (1)
- Sexual ReproductionDocument6 pagesSexual ReproductionAlyssa Margareth SorianoNo ratings yet
- Pnas 0602138103Document6 pagesPnas 0602138103edisonballaNo ratings yet
- Reproduction Part 2Document6 pagesReproduction Part 2KELVIN CHIBINDANo ratings yet
- Chart 1Document1 pageChart 1BAGUIO CATSNo ratings yet
- Sex Hormones: Dr. Lotfi S. Bin Dahman MD, PHD Clinical Biochemistry HucomDocument22 pagesSex Hormones: Dr. Lotfi S. Bin Dahman MD, PHD Clinical Biochemistry Hucomعبدالحكيم النهديNo ratings yet
- Developing A Balanced Business Model For Gene TherapyDocument4 pagesDeveloping A Balanced Business Model For Gene TherapySupriya KapasNo ratings yet
- Unifying Themes of LifeDocument33 pagesUnifying Themes of LifeRyan Dave MacariayNo ratings yet
- A Dynamic Method Based On The Specific Substrate Uptake Rate To Set Up A Feeding Strategy For Pichia PastorisDocument9 pagesA Dynamic Method Based On The Specific Substrate Uptake Rate To Set Up A Feeding Strategy For Pichia PastorisOscar Evrard ArruéNo ratings yet
- Panchy Et Al (2016) - Plant PhysiologyDocument23 pagesPanchy Et Al (2016) - Plant PhysiologyAna Luiza Atella de FreitasNo ratings yet
- Bradford University Thesis SubmissionDocument6 pagesBradford University Thesis Submissiondwsmjsqy100% (2)
- Quick Quiz: On Your Answer Sheet, Write in or Circle The Correct Letter For Each QuestionDocument2 pagesQuick Quiz: On Your Answer Sheet, Write in or Circle The Correct Letter For Each QuestionazharNo ratings yet
- Okamura 1999Document4 pagesOkamura 1999Araceli Enríquez OvandoNo ratings yet
- Link Download Ebook Anatomy and PhysiologyDocument87 pagesLink Download Ebook Anatomy and Physiologyarif100% (1)
- Antibody PanelDocument81 pagesAntibody PanelMa. Pe Delaine MendrosNo ratings yet
- (EAAP Scientific Series 112) J.F. Hocquette - S. Gigli - Indicators of Milk and Beef Quality-Wageningen Academic Publishers (2005)Document465 pages(EAAP Scientific Series 112) J.F. Hocquette - S. Gigli - Indicators of Milk and Beef Quality-Wageningen Academic Publishers (2005)William AvilaNo ratings yet
- PostLessonStudentsNotes Week3Document5 pagesPostLessonStudentsNotes Week3Xie NiyunNo ratings yet
- Azmietal 2022Document15 pagesAzmietal 2022Shayne BonayonNo ratings yet
- Table of Specification in 1GEN BIO 1STDocument3 pagesTable of Specification in 1GEN BIO 1STLouie DenostaNo ratings yet
- Molecular Origins of Human AttentionDocument260 pagesMolecular Origins of Human AttentionAndreea DumitrescuNo ratings yet
- The Beautiful Me: Physical SelfDocument34 pagesThe Beautiful Me: Physical SelfMariane Joy TecsonNo ratings yet
- (Methods in Molecular Biology, 2316) Ayala L. N. Rao, Irene Lavagi-Craddock, Georgios Vidalakis - Viroids - Methods and Protocols-Humana (2021)Document368 pages(Methods in Molecular Biology, 2316) Ayala L. N. Rao, Irene Lavagi-Craddock, Georgios Vidalakis - Viroids - Methods and Protocols-Humana (2021)kirbyNo ratings yet
- Question: in The Following Human Pedigrees, The Lled Symbols RepresenDocument2 pagesQuestion: in The Following Human Pedigrees, The Lled Symbols RepresenfjkgldjfNo ratings yet
- Modification of Mendelian Ratio II - Lethal Mutations & Epistasis (2 HRS) 2011Document35 pagesModification of Mendelian Ratio II - Lethal Mutations & Epistasis (2 HRS) 2011SITI BAZILAH BINTI BILAK KPM-GuruNo ratings yet
- Working With Genes3Document24 pagesWorking With Genes3Atharva PurohitNo ratings yet