Professional Documents
Culture Documents
Abarracoso, F. Urinary System
Uploaded by
fabarracoso24Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abarracoso, F. Urinary System
Uploaded by
fabarracoso24Copyright:
Available Formats
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
SCHOOLS OF NURSING and MIDWIFERY `
COLLABORATIVE MODULE FOR OUTCOMES-BASED AND FLEXIBLE
LEARNING IN Human Anatomy and Physiology - Lab
Student:__Abarracoso, Flora May A._______Student Number:_20-1-03777____
Name of Professor:_Mrs. Leila de Villa- Masajo_____Year Level/Section:_1st/ BSN 1-5__
LESSON/TOPIC:
Urinary System
INTENDED LEARNING OUTCOME
1. Identify the principal structure of the kidney.
2. Explain how kidney structure function.
INTRODUCTION
Physical Characteristics of Urine
The urinary system’s ability to filter the blood resides in about 2 to 3 million tufts
of specialized capillaries—the glomeruli—distributed more or less equally
between the two kidneys. Because the glomeruli filter the blood based mostly on
particle size, large elements like blood cells, platelets, antibodies, and albumen
are excluded. The glomerulus is the first part of the nephron, which then
continues as a highly specialized tubular structure responsible for creating the
final urine composition. All other solutes, such as ions, amino acids, vitamins,
• VIRTUE • EXCELLENCE • SERVICE
and wastes, are filtered to create a filtrate composition very similar to plasma.
The glomeruli create about 200 liters (189 quarts) of this filtrate every day, yet
you excrete less than two liters of waste you call urine.
Characteristics of the urine change, depending on influences such as water intake,
exercise, environmental temperature, nutrient intake, and other factors. Some of the
characteristics such as color and odor are rough descriptors of your state of hydration.
For example, if you exercise or work outside, and sweat a great deal, your urine will
turn darker and produce a slight odor, even if you drink plenty of water. Athletes are
often advised to consume water until their urine is clear. This is good advice; however,
it takes time for the kidneys to process body fluids and store it in the bladder. Another
way of looking at this is that the quality of the urine produced is an average over the
time it takes to make that urine. Producing clear urine may take only a few minutes if
you are drinking a lot of water or several hours if you are working outside and not
drinking much.
Normal Urine Characteristics
Characteristic Normal values
Color Pale yellow to deep amber
Odor Odorless
Volume 750–2000 mL/24 hour
pH 4.5–8.0
Specific gravity 1.003–1.032
Osmolarity 40–1350 mOsmol/kg
Urobilinogen 0.2–1.0 mg/100 mL
White blood cells 0–2 HPF (per high-power field of microscope)
Leukocyte None
esterase
Protein None or trace
Bilirubin <0.3 mg/100 mL
Ketones None
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
Nitrites None
Blood None
Glucose None
Urinalysis (urine analysis) often provides clues to renal disease. Normally, only
traces of protein are found in urine, and when higher amounts are found, damage
to the glomeruli is the likely basis. Unusually large quantities of urine may point to
diseases like diabetes mellitus or hypothalamic tumors that cause diabetes
insipidus. The color of urine is determined mostly by the breakdown products of
red blood cell destruction. The “heme” of hemoglobin is converted by the liver into
water-soluble forms that can be excreted into the bile and indirectly into the urine.
This yellow pigment is urochrome. Urine color may also be affected by certain
foods like beets snd berries. A kidney stone or a cancer of the urinary system
may produce sufficient bleeding to manifest as pink or even bright red urine.
Diseases of the liver or obstructions of bile drainage from the liver impart a dark
“tea” or “cola” hue to the urine. Dehydration produces darker, concentrated urine
that may also possess the slight odor of ammonia. Most of the ammonia
produced from protein breakdown is converted into urea by the liver, so ammonia
is rarely detected in fresh urine. The strong ammonia odor you may detect in
bathrooms or alleys is due to the breakdown of urea into ammonia by bacteria in
the environment. About one in five people detect a distinctive odor in their urine
after consuming asparagus; other foods such as onions, garlic, and fish can
impart their own aromas! These food-caused odors are harmless.
• VIRTUE • EXCELLENCE • SERVICE
Urine volume varies considerably. The normal range is one to two liters per day.
The kidneys must produce a minimum urine volume of about 500 mL/day to rid
the body of wastes. Output below this level may be caused by severe
dehydration or renal disease and is termed oliguria. The virtual absence of urine
production is termed anuria. Excessive urine production is polyuria, which may
be due to diabetes mellitus or diabetes insipidus. In diabetes mellitus, blood
glucose levels exceed the number of available sodium-glucose transporters in the
kidney, and glucose appears in the urine. The osmotic nature of glucose attracts
water, leading to its loss in the urine. In the case of diabetes insipidus, insufficient
pituitary antidiuretic hormone (ADH) release or insufficient numbers of ADH
receptors in the collecting ducts means that too few water channels are inserted
into the cell membranes that line the collecting ducts of the kidney. Insufficient
numbers of water channels (aquaporins) reduce water absorption, resulting in
high volumes of very dilute urine.
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
Urine Volumes
Volume Volume Causes
condition
Normal 1–2 L/day
Polyuria >2.5 L/day Diabetes mellitus; diabetes insipidus; excess caffeine
or alcohol; kidney disease; certain drugs, such as
diuretics; sickle cell anemia; excessive water intake
Oliguria 300–500 Dehydration; blood loss; diarrhea; cardiogenic
mL/day shock; kidney disease; enlarged prostate
Anuria <50 Kidney failure; obstruction, such as kidney stone or
mL/day tumor; enlarged prostate
The pH (hydrogen ion concentration) of the urine can vary more than 1000-fold,
from a normal low of 4.5 to a maximum of 8.0. Diet can influence pH; meats
lower the pH, whereas citrus fruits, vegetables, and dairy products raise the pH.
Chronically high or low pH can lead to disorders, such as the development of
kidney stones or osteomalacia.
Specific gravity is a measure of the quantity of solutes per unit volume of a
solution and is traditionally easier to measure than osmolarity. Urine will always
have a specific gravity greater than pure water (water = 1.0) due to the presence
of solutes. Laboratories can now measure urine osmolarity directly, which is a
more accurate indicator of urinary solutes than specific gravity. Remember that
osmolarity is the number of osmoles or milliosmoles per liter of fluid (mOsmol/L).
Urine osmolarity ranges from a low of 50–100 mOsmol/L to as high as 1200
mOsmol/L H O. 2
Cells are not normally found in the urine. The presence of leukocytes may indicate
a urinary tract infection. Leukocyte esterase is released by leukocytes; if
detected in the urine, it can be taken as indirect evidence of a urinary tract
infection (UTI).
Protein does not normally leave the glomerular capillaries, so only trace
amounts of protein should be found in the urine, approximately 10 mg/100 mL
in a random sample. If excessive protein is detected in the urine, it usually
means that the glomerulus is damaged and is allowing protein to “leak” into
the filtrate.
• VIRTUE • EXCELLENCE • SERVICE
Ketones are byproducts of fat metabolism. Finding ketones in the urine suggests
that the body is using fat as an energy source in preference to glucose. In
diabetes mellitus when there is not enough insulin (type I diabetes mellitus) or
because of insulin resistance (type II diabetes mellitus), there is plenty of
glucose, but without the action of insulin, the cells cannot take it up, so it remains
in the bloodstream. Instead, the cells are forced to use fat as their energy source,
and fat consumed at such a level produces excessive ketones as byproducts.
These excess ketones will appear in the urine. Ketones may also appear if there
is a severe deficiency of proteins or carbohydrates in the diet.
Nitrates (NO ) occur normally in the urine. Gram-negative bacteria
3
–
metabolize nitrate into nitrite (NO ), and its presence in the urine is indirect
2
–
evidence of infection.
There should be no blood found in the urine. It may sometimes appear in urine
samples as a result of menstrual contamination, but this is not an abnormal
condition. Now that you understand what the normal characteristics of urine
are, the next section will introduce you to how you store and dispose of this
waste product and how you make it.
The Urinary System and Homeostasis
All systems of the body are interrelated. A change in one system may affect all
other systems in the body, with mild to devastating effects. A failure of urinary
continence can be embarrassing and inconvenient, but is not life threatening.
The loss of other urinary functions may prove fatal. A failure to synthesize
vitamin D is one such example.
Vitamin D Synthesis
In order for vitamin D to become active, it must undergo a hydroxylation reaction
in the kidney, that is, an –OH group must be added to calcidiol to make calcitriol
(1,25
dihydroxycholecalciferol). Activated vitamin D is important for absorption of Ca in ++
the digestive tract, its reabsorption in the kidney, and the maintenance of normal
serum concentrations of Ca and phosphate. Calcium is vitally important in bone
++
health, muscle contraction, hormone secretion, and neurotransmitter release.
Inadequate Ca leads to disorders like osteoporosis and osteomalacia in adults
++
and rickets in children. Deficits may also result in problems with cell proliferation,
neuromuscular function, blood clotting, and the inflammatory response. Recent
research has confirmed that vitamin D receptors are present in most, if not all,
cells of the body, reflecting the systemic importance of vitamin D. Many scientists
have suggested it be referred to as a hormone rather than a vitamin.
Erythropoiesis
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
EPO is a 193-amino acid protein that stimulates the formation of red blood cells in
the bone marrow. The kidney produces 85 percent of circulating EPO; the liver,
the remainder. If you move to a higher altitude, the partial pressure of oxygen is
lower, meaning there is less pressure to push oxygen across the alveolar
membrane and into the red blood cell. One way the body compensates is to
manufacture more red blood cells by increasing EPO production. If you start an
aerobic exercise program, your tissues will need more oxygen to cope, and the
kidney will respond with more EPO. If erythrocytes are lost due to severe or
prolonged bleeding, or under produced due to disease or severe malnutrition, the
kidneys come to the rescue by producing more EPO. Renal failure (loss of EPO
production) is associated with anemia, which makes it difficult for the body to
cope with increased oxygen demands or to supply oxygen adequately even
under normal conditions. Anemia diminishes performance and can be life
threatening.
Blood Pressure Regulation
Due to osmosis, water follows where Na leads. Much of the water the kidneys
+
recover from the forming urine follows the reabsorption of Na . ADH stimulation of
+
aquaporin channels allows for regulation of water recovery in the collecting ducts.
Normally, all of the glucose is recovered, but loss of glucose control (diabetes
mellitus) may result in an osmotic dieresis severe enough to produce severe
dehydration and death. A loss of renal function means a loss of effective vascular
volume control, leading to hypotension (low blood pressure) or hypertension (high
blood pressure), which can lead to stroke, heart attack, and aneurysm formation.
The kidneys cooperate with the lungs, liver, and adrenal cortex through the renin–
angiotensin– aldosterone system. The liver synthesizes and secretes the inactive
precursor angiotensinogen. When the blood pressure is low, the kidney
synthesizes and releases renin. Renin converts angiotensinogen into angiotensin
I, and ACE produced in the lung converts angiotensin I into biologically active
angiotensin II. The immediate and short-term effect of angiotensin II is to raise
blood pressure by causing widespread vasoconstriction. angiotensin II also
stimulates the adrenal cortex to release the steroid hormone aldosterone, which
results in renal reabsorption of Na and its associated osmotic recovery of water.
+
The reabsorption of Na helps to raise and maintain blood pressure over a longer
+
term.• VIRTUE • EXCELLENCE • SERVICE
`
Regulation of Osmolarity
Blood pressure and osmolarity are regulated in a similar fashion. Severe hypo-
osmolarity can cause problems like lysis (rupture) of blood cells or widespread
edema, which is due to a solute imbalance. Inadequate solute concentration
(such as protein) in the plasma results in water moving toward an area of greater
• VIRTUE • EXCELLENCE • SERVICE
solute concentration, in this case, the interstitial space and cell cytoplasm. If the
kidney glomeruli are damaged by an autoimmune illness, large quantities of
protein may be lost in the urine. The resultant drop in serum osmolarity leads to
widespread edema that, if severe, may lead to damaging or fatal brain swelling.
Severe hypertonic conditions may arise with severe dehydration from lack of
water intake, severe vomiting, or uncontrolled diarrhea. When the kidney is
unable to recover sufficient water from the forming urine, the consequences may
be severe (lethargy, confusion, muscle cramps, and finally, death) .
Recovery of Electrolytes
Sodium, calcium, and potassium must be closely regulated. The role of Na +
and Ca homeostasis has been discussed at length. Failure of K regulation
++ +
can have serious consequences on nerve conduction, skeletal muscle
function, and most significantly, on cardiac muscle contraction and rhythm.
pH Regulation
Recall that enzymes lose their three-dimensional conformation and, therefore, their
function if the pH is too acidic or basic. This loss of conformation may be a
consequence of the breaking of hydrogen bonds. Move the pH away from the optimum
for a specific enzyme and you may severely hamper its function throughout the body,
including hormone binding, central nervous system signaling, or myocardial contraction.
Proper kidney function is essential for pH homeostasis.
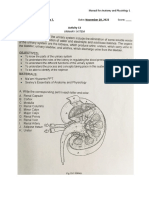
LAB EXERCISES
A. Urinary System Overview
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
Look at the paired, bean shaped kidneys
Urinary System: the organs of the MALE urinary system
1. Describe the main function of the urinary system.
Answer: the urinary system filters wastes and other unwanted substances from the blood and
excretes them as fluid waste called urine
2. What is the excretory product of the urinary system?
Answer: Urine
3. In men, the urethra passes through which two organs of the reproductive system?
Answer: the penis and the prostate
Urinary System: the organs of the female urinary system.
Complete the following statement so it accurately compares the male and
female urinary systems.
4. In the ______mail____________ urinary system, the
_____urethra______________ is much longer.
B. Urinary System Overview
Pelvic Region (Male). Use this view to answer the following questions.
1. The paired kidneys. How would you describe their relationship to the intestines
and the spine?
Answer: the kidneys are located on either side of the vertebral column, behind the
intestines
2. The bladder. Note that it rests on the pelvic floor. Imagine the urethra as it leaves
the bladder and follow its path. The first section of the male urethra passes through the
___prostate_____________.
3. The last section of the male urethra travels through the ______spongy_______
portion of the penis and the ____glans penis__________________ (the tip of the
penis).
The Pelvic Region (Female). Use this view to answer the following question:
1. The anterior peritoneum covering the abdominal organs. The peritoneum is a
______serous_________ membrane. The inner layer forms the lining that covers the
___internal organs _________.
• VIRTUE • EXCELLENCE • SERVICE
2. The kidneys are defined as retroperitoneal organs. What do you
think “retroperitoneal” means?
Answer: behind or dorsal to the peritoneum
3. The female bladder lies on the pelvic floor underneath
the_____uterus_______.
A. The Kidneys: Vasculature
Renal Vasculature (M). Use this view to answer the following questions.
1. In this view, you can see a cone-shaped endocrine gland on top of each kidney. These are
the ___adrenal glands _____, which release hormones affecting the function of the kidneys.
2. Select either of the large arteries entering the kidneys to view the renal blood supply and
use the book icon to read the definition.
Answer: Aorta
a. These large arteries are branches of
The____renal arteries__________.
b. The large arteries entering the kidneys are called the __renal arteries________
c. Which of these arteries is higher?
Answer: Left
d. Which is longer?
Answer: Right
3. Select either of the large veins leaving the kidneys to view the venous drainage of
the kidneys and use the book icon to read the definition.
a. These large vessels drain into the __inferior vena cava___________.
b.Which of these veins is higher?
Answer: Left
c. Which is longer?
Answer: Left
Note that as blood enters the kidneys, it brings oxygen to renal tissues and is filtered
by the kidneys. Blood leaving the kidneys is depleted of oxygen and has been filtered.
B. The Kidneys: Internal Anatomy
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
Kidney Section (F). Use this view to answer the following questions.
1. Define the following terms:
a. Adipose capsule- a mass of adipose tissue surrounding each kidney
b. Cortex- the outer layer of the kidney
c. Medulla- the inner layer of the kidney
2. Which structures make up the bulk of the renal pyramids?
Answer: they are made up mostly of nephrons
3. Where are the renal columns found?
Answer: In the medulla between the pyramids
4. Urine from the pyramids is channeled into the ___renal pelvis_____________
5. Locate the large renal pelvis in the center of the kidney. Urine from the renal pelvis
is channeled into the ___ureters____________.
6. Nephrons are the functional units of the kidneys that make up most of the cortex
and the medulla.
Answer:
a. Nephrons are composed of a series of ____tubules_____and
___arterioles_____________.
b. The primary site of filtration is in a spherical capillary network called the __renal
corpuscle_________________.
c. Inside the corpuscle, blood passes through a spherical capillary network called the
________glomerulus_________
d. Filtrate from the blood enters a cavity called the ___glomerular (bowmans) capsule___.
From there, the filtrate is passed through the tubules until it enters the renal pelvis as urine.
C. The Ureters and the Bladder
Ureters (M). Use this view to answer the following questions.
• VIRTUE • EXCELLENCE • SERVICE
1.The ureters.
a.What is the function of the ureters?
Answer: To deliver urine to the bladder
b. How is urine propelled through the ureters?
Answer: By contraction of smooth muscle
c. How long is each ureter?
Answer: 25-30 cm
2.The ureters enter the bladder. The ureters enter the bladder through openings in
the ____rear___________ bladder floor.
3.Both ureters. The triangular region of the bladder, marked by the entrance of the
two ureters and the external urethral orifice, is the ___trigone______ of the
bladder.
Bladder (F). Note that the bladder is located entirely inside the pelvis,
protected by the pelvic bones.
1.The bladder mucosa is covered by a __transtional______ epithelium and is
arranged in folds called ____rugae_____________.
2.A layer of smooth muscle, called the _____detrusor muscle________ gives the
bladder wall its elasticity.
3.Approximately how much urine can the bladder hold before the urge to micturate
is triggered?
Answer: 500 mL
Bladder Section (M). Locate and identify the function of the following structures
in the cross-section view.
1. Bladder inner surface- It plays two main roles: Temporary storage of urine – the
bladder is a hollow organ with distensible walls.
2. Detrusor muscle layer- To contract during urination to push the urine out of the bladder
and into the urethra. The detrusor muscle will relax to allow the storage of urine in the urinary
bladder.
3. Neck of the bladder (the region joining the urethra)- The area at the base of the trigone that
surrounds the internal urethral orifice that leads to the urethra.
D. The Male Urethra
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
1.Select any part of the urethra and use the book icon to read the definition. Locate and name
the three portions of the male urethra.
Answer: Prostatic, Membraneous, Spongy
2.The prostatic urethra is completely within the _____prostate (gland)________
3. In the prostate, the urethra is joined by paired ___ejaculatory______ ducts.
4.The membranous urethra passes through the _____urogenital diaphragm____ and
receives ducts from the paired ____bulbourethral________ glands.
5. Look at the corpus spongiosum and the spongy urethra and observe where it exits the
penis.
6.Next, observe the glans penis and the end of the spongy urethra. Note how it expands
slightly in the tip of the penis. The spongy portion of the urethra is divided into two sections:
the ____bulbar_______ section and the ____pendulous__________ section.
7.The male urethra carries two products: ____urine______ and ______semen________
Urethral Sphincter (M). Use this view to answer the following questions.
1. Locate the internal urethral sphincter. It controls the passage of urine from the bladder
into the urethra. Control of this sphincter is involuntary, and it opens when the volume of urine
in the bladder triggers the ____micturition__________ reflex.
2. A second, voluntary external urethral sphincter encircles the
____membranous_________ urethra. This muscle allows for voluntary control over
micturition.
E. The Female Urethra
Note that the bladder is located entirely within the pelvis under the uterus. Use
this view to answer the following questions.
1. Locate and select the urethra. It passes through the ___perineum_______and exits
through the _____vulva_________. With the urethra observe where it exits the vulva. It
is very small.
2. Locate the urethral orifice, which surrounds the end of the urethra. The urethral
orifice is contained inside the ___vestibule___________, directly in front of the
opening of the ______vagina________.
• VIRTUE • EXCELLENCE • SERVICE
Urethral Sphincters (F). Use this view to answer the following questions.
1. Select the neck of the bladder, where it joins the urethra. Now, hide the neck and
locate the internal urethral sphincter. This involuntary sphincter opens during the
____micturition_________reflex.
2. Locate the external urethral sphincter. This muscle allows for ____voluntary__________
control over micturition.
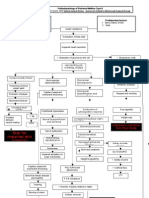
G. Microanatomy: Nephrons
1.Look at the cortex, the renal pyramids, and the renal columns of the medulla.
2.Locate the renal artery as it enters the kidney (it does not enter the renal pelvis as
the diagram suggests). The first branches of this artery that are located inside the
kidney are the ______renal artery__________ and these extend into the renal
columns as ______renal pyramids ___________. The branches that arc over each
pyramid are called ___arcuate arteries_______, and smaller branches called
___interlobar arteries_______ extend further into the cortex. These arteries supply
the nephrons.
3.Look at the Nephrons at the top. There are three nephrons in this view, but there
are approximately one million of them in each kidney. Nephrons are complex
structures that include a capsule, tubules, and associated blood vessels.
4.Locate the small, spherical glomerular capsule in the center nephron, at the top of
the image. Inside the capsule, you’ll see a spherical capillary network called a
__glomerulus_________. High blood pressure in these specialized capillaries forces
fluid out of the blood vessels and into the capsular space. This fluid, called filtrate
because it has been filtered by the glomerulus, leaves the capsule and enters the
___proximal convoluted tubule ________. As the tubule travels down into the
medullary pyramid, it is called the __descending limb of loop of henle________and
as it travels back up into the cortex, it is called the ___ascending limb of loop of henle
_______. As the filtrate passes through the loop of Henle (also called a nephron
loop), it is modified by the loop’s epithelium. These epithelial cells are
____cuboidal________in shape and have a “brush border,” meaning they are
covered with ___microvilli_______. As the tubule exits the medulla, it is called the
___ascending limb of loop of henle_______. As the tubule straightens out again and
exits via the renal pyramid, it is called a _____dct______.
5.As filtrate travels through the nephron loop, the tubule cells secrete
___creatine_______ and excess ions into the filtrate. As the loop travels down into the
medulla and back, it passes through salt gradients that facilitate the reabsorption of
____water________and other necessary molecules as required. 6.When these
processes are complete, the filtrate is called
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
_____urine_________. Fluid from the collecting duct flows into the
_____ureters___________.
7.Look for the arteriole entering the capsule to form the glomerulus. It is called the
___afferent arteriole______. The arteriole exiting the capsule, coming from the
glomerulus, is the __efferent arteriole_____. This arteriole branches into a network of
__________________________________ that surround the proximal and distal
convoluted tubules. These capillaries interact with the convoluted tubules to reabsorb
water and adjust the concentrations of solutes in the filtrate. Blood leaving the
peritubular capillaries enters the ____interlobular______ veins, which join the
__arcuate____veins that arc over the pyramids. The arcuate veins join to become the
__interlobar_____ veins in the renal columns. These join the __arcuate and
interlobar____ veins, which take blood out of the kidneys to drain into the ___inferior
vena cava _______.
8.Look at the nephron on the right side of the view. It has a much longer loop of Henle,
extending much further into the medulla, than the one in the center. The center nephron
is called a cortical nephron. The one on the right is a juxtamedullary nephron, as its
capsule is adjacent to the medulla. Approximately 20—30% of nephrons are
juxtamedullary nephrons, which are responsible for creating most of the physiological
gradients in the kidney. To help create these gradients, there are a series of capillaries,
branching from the peritubular capillaries and associated with the loop of Henle,
collectively called the ____vasa recta________. This network returns blood to the
efferent end of the peritubular capillaries and to the interlobular veins.
• VIRTUE • EXCELLENCE • SERVICE
PUTTING IT ALL TOGETHER
A.Draw an outline of the urinary system. Label each organ and use arrows to indicate the flow
of urine.
B.Answer the following questions:
1. What are the main differences between the male and female urinary systems?
Answer: males have a longer urethra than females and they also have prostates which affect
their ability to urinate as they get older.
2. Which structure gives us voluntary control over micturition for male and female?
Answer: external sphincter
3. Which of the following do you think is not a function of the kidney?
a. Removal of waste product from the body
b. Control of micturition
c. Regulation of electrolyte balance (e.g. sodium, potassium, and calcium)
d. Regulation of acid-base homeostasis
e. Controlling blood volume and maintaining blood pressure
Answer: B
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
• VIRTUE • EXCELLENCE • SERVICE
QF-PQM-035 (09.26.2020) Rev.2
EMILIO AGUINALDO COLLEGE
Gov. D. Mangubat Ave., Brgy. Burol Main, City of Dasmariñas, Cavite 4114, Philippines
Tel. Nos. (046) 416-4339/41 www.eac.edu.ph
ISO 9001:2015 CERTIFIED
SCHOOL OF NURSING QUALITY MANAGEMENT SYSTEM
• VIRTUE • EXCELLENCE • SERVICE
You might also like
- Lets Get Started - Urinalysis PDFDocument3 pagesLets Get Started - Urinalysis PDFSatya PramanaNo ratings yet
- Med Geeks Clinical Lab GuideDocument17 pagesMed Geeks Clinical Lab GuideHuy Hoang100% (1)
- Urine Analysis PracticalDocument53 pagesUrine Analysis PracticalMubasharAbrar100% (2)
- The Hearty Renal Diet Cookbook Delicious Kidney-Friendly Recipes To Manage Kidney Disease: Delicious Kidney-Friendly Recipes To Manage Kidney DiseaseFrom EverandThe Hearty Renal Diet Cookbook Delicious Kidney-Friendly Recipes To Manage Kidney Disease: Delicious Kidney-Friendly Recipes To Manage Kidney DiseaseNo ratings yet
- DM Type 2 PathophysiologyDocument3 pagesDM Type 2 PathophysiologyuzumakiruleNo ratings yet
- 25.1 Physical Characteristics of Urine - Anatomy and Physiology 2e - OpenStaxDocument4 pages25.1 Physical Characteristics of Urine - Anatomy and Physiology 2e - OpenStaxMarlene AngwaforNo ratings yet
- Urine AND Feces: Prepared By: Group 5Document37 pagesUrine AND Feces: Prepared By: Group 5Chantal RaymondsNo ratings yet
- Urinalysis Pre LabDocument6 pagesUrinalysis Pre LabbobbyNo ratings yet
- Lab 5 - The Urinary System: KidneyDocument6 pagesLab 5 - The Urinary System: Kidneymath_mallikarjun_sapNo ratings yet
- Analysis of UrineDocument22 pagesAnalysis of UrineFaith Domingo100% (1)
- Biochemistry of Urine: By: Jerome S. Montano, RMTDocument28 pagesBiochemistry of Urine: By: Jerome S. Montano, RMTAhuNo ratings yet
- UrineDocument17 pagesUrinealynne_pascua8530No ratings yet
- Urine Composition. Hormonal Regulation of UrinalysisDocument7 pagesUrine Composition. Hormonal Regulation of Urinalysisnandini pulavartiNo ratings yet
- Investigation of Polyuria and Polydipsia The Dog: DefinitionsDocument7 pagesInvestigation of Polyuria and Polydipsia The Dog: DefinitionsEmily CrossNo ratings yet
- BIOLOGY YR 12 WK 1 - 7Document33 pagesBIOLOGY YR 12 WK 1 - 7Filfine OkpenyiNo ratings yet
- Urinalysis PDFDocument56 pagesUrinalysis PDFTio AjhaNo ratings yet
- Fluid-Electrolyte Balance in Children: Dr. Wan Nedra K, Sp.A Bagian Ilmu Kesehatan Anak FK - YARSI, JakartaDocument48 pagesFluid-Electrolyte Balance in Children: Dr. Wan Nedra K, Sp.A Bagian Ilmu Kesehatan Anak FK - YARSI, JakartaAnggit EkawatiNo ratings yet
- Urine AnalysisDocument63 pagesUrine AnalysisAdarshBijapurNo ratings yet
- UrineDocument55 pagesUrineAbuzarNo ratings yet
- FLUID AND ELECTOLYTE IMBALANCE FinalDocument27 pagesFLUID AND ELECTOLYTE IMBALANCE FinalShiva BiradarNo ratings yet
- Liver Disease Study GuideDocument11 pagesLiver Disease Study GuideLauren OliveiraNo ratings yet
- Rine Analysis: Dr. Ola Samir Ziara Modified by Dr. Amal Al MaqadmaDocument39 pagesRine Analysis: Dr. Ola Samir Ziara Modified by Dr. Amal Al Maqadmaiman zainuddin100% (1)
- Routine UrinalysisDocument4 pagesRoutine UrinalysisDanica Joy Christelle L. PilarNo ratings yet
- Analysis of Abnormal UrineDocument12 pagesAnalysis of Abnormal Urinesingonstrings365No ratings yet
- Lesson 15 Fecalysis and Gastric AnalysisDocument39 pagesLesson 15 Fecalysis and Gastric AnalysisFaith TambongNo ratings yet
- Kidney Function Tests 2Document30 pagesKidney Function Tests 2kamalNo ratings yet
- Water Electrolytes Part Clinical BiochemistryDocument27 pagesWater Electrolytes Part Clinical BiochemistryAshraf FirdadNo ratings yet
- Urine AnalysisDocument53 pagesUrine AnalysisMaath KhalidNo ratings yet
- Interpretation of Urine DRDocument117 pagesInterpretation of Urine DRShanza AmaanNo ratings yet
- Urine Analysis FinalDocument112 pagesUrine Analysis FinalNischita JayarajNo ratings yet
- Urine Analysis: Assist. Prof. Biochemistry Dep., Faculty of Medicine Asu & UqDocument21 pagesUrine Analysis: Assist. Prof. Biochemistry Dep., Faculty of Medicine Asu & UqArjunaPamungkasNo ratings yet
- Pedia 2Document5 pagesPedia 2Devansh MoyalNo ratings yet
- Gastrointestinal System Disorders For PediaDocument92 pagesGastrointestinal System Disorders For PediaQuolette Constante100% (1)
- Clinical Lab Guide: by MedgeeksDocument17 pagesClinical Lab Guide: by MedgeeksHuy HoangNo ratings yet
- C17 - EviDocument13 pagesC17 - EviMarissaevisNo ratings yet
- Biochemical Aspect of DiarrheaDocument17 pagesBiochemical Aspect of DiarrheaLiz Espinosa0% (1)
- Term III Practical FileDocument31 pagesTerm III Practical FileShivam kumarNo ratings yet
- 4 BodyDocument35 pages4 Bodysinte beyuNo ratings yet
- Cholera AssignmentDocument2 pagesCholera AssignmentARISNo ratings yet
- Urinalysis TableDocument9 pagesUrinalysis TableMegNo ratings yet
- A Fluids and ElectrolytesDocument8 pagesA Fluids and ElectrolytesAnastasiafynnNo ratings yet
- Somaville University Faculty of Medicine Urology &nephrology Lecturer: DR - Osman Urine Analyze Presentation by Group ADocument49 pagesSomaville University Faculty of Medicine Urology &nephrology Lecturer: DR - Osman Urine Analyze Presentation by Group ALayla CabduqaadirNo ratings yet
- Hepatitis: Sukma Randani Ismono, S.Kep.,NsDocument18 pagesHepatitis: Sukma Randani Ismono, S.Kep.,NsRismaya NovitasariNo ratings yet
- CholeraDocument11 pagesCholeraNadhifa NauraNo ratings yet
- Chap69 PDFDocument3 pagesChap69 PDFIkrar SyahmarNo ratings yet
- Fluid and ElectrolytesDocument137 pagesFluid and ElectrolytesNano Baddour100% (1)
- Abeer Renal Function Testsamr Renal Function Tests Renal BlockDocument22 pagesAbeer Renal Function Testsamr Renal Function Tests Renal BlockAbeer AhmedNo ratings yet
- Clin Path Trans 3.05 Urinalysis (2b)Document6 pagesClin Path Trans 3.05 Urinalysis (2b)Reymart FernandezNo ratings yet
- Alteration in Fluid and Electrolyte Status Lecture NotesDocument11 pagesAlteration in Fluid and Electrolyte Status Lecture Notes0912247251No ratings yet
- Water and ElectrolytesDocument33 pagesWater and ElectrolytesCourtney Dela Fierra100% (1)
- Renal CalculiDocument28 pagesRenal Calculihailleyann33% (3)
- WaterDocument16 pagesWaterAUBREY LISAYENNo ratings yet
- 6 Essential NutrientsDocument133 pages6 Essential NutrientsLouisa Marie MirandaNo ratings yet
- Swu Phinma, College of Pharmacy 2020: Wr/Urinalysis - Html#Ixzz6Zxlj RQKH /Product-Manual/3008 - 3B - UrinalysisDocument7 pagesSwu Phinma, College of Pharmacy 2020: Wr/Urinalysis - Html#Ixzz6Zxlj RQKH /Product-Manual/3008 - 3B - UrinalysisTrex MarciiiNo ratings yet
- Dehidrasi Pada PediatricDocument35 pagesDehidrasi Pada PediatricRivaldy PrayudhaNo ratings yet
- Complete Urinalysis: A. Physical Characteristics of UrineDocument8 pagesComplete Urinalysis: A. Physical Characteristics of UrineKryza Dale Bunado BaticanNo ratings yet
- Fluids ElectrolytesDocument37 pagesFluids ElectrolytesAlpascaFirdausNo ratings yet
- Team Four: Activity 12Document81 pagesTeam Four: Activity 12Aura Naera Dandan Magarang100% (1)
- Chronic Kidney Disease (CKD) : Universidad de ManilaDocument4 pagesChronic Kidney Disease (CKD) : Universidad de ManilaKristine_Bacan_2085No ratings yet
- Renal Diet Cookbook for Beginners: Enjoy Delicious, Kidney-Friendly Recipes with Balanced Sodium, Phosphorus, and Potassium Levels [III EDITION]From EverandRenal Diet Cookbook for Beginners: Enjoy Delicious, Kidney-Friendly Recipes with Balanced Sodium, Phosphorus, and Potassium Levels [III EDITION]Rating: 5 out of 5 stars5/5 (18)
- Week 1 Introduction To Human Anatomy and Physiology With PathophysiologyDocument20 pagesWeek 1 Introduction To Human Anatomy and Physiology With Pathophysiologyfabarracoso24No ratings yet
- Abarracoso, F. Male Reproductive SystemDocument12 pagesAbarracoso, F. Male Reproductive Systemfabarracoso24No ratings yet
- Abarracoso, Flora May, SW8 BSN 1-6Document2 pagesAbarracoso, Flora May, SW8 BSN 1-6fabarracoso24No ratings yet
- ABARRACOSO A.-Act3-Ecfnurs1-6Document1 pageABARRACOSO A.-Act3-Ecfnurs1-6fabarracoso24No ratings yet
- ABARRACOSO A.act2, Ecfnurs 1-6Document1 pageABARRACOSO A.act2, Ecfnurs 1-6fabarracoso24No ratings yet
- ABARRACOSO R. Act1, Ecfnur 1-6Document4 pagesABARRACOSO R. Act1, Ecfnur 1-6fabarracoso24No ratings yet
- ABARRACOSO A, Ass1, nstp1-6Document1 pageABARRACOSO A, Ass1, nstp1-6fabarracoso24No ratings yet
- GT134 DamsDocument119 pagesGT134 Damsসোমনাথ মহাপাত্র0% (1)
- Anatomy and Physiology - Kidney - ForDocument3 pagesAnatomy and Physiology - Kidney - ForKristelle ModalesNo ratings yet
- Anatomy and Physiology of The Reptile Renal SystemDocument12 pagesAnatomy and Physiology of The Reptile Renal SystemEduardo LeónNo ratings yet
- Chapter 1 2 3Document77 pagesChapter 1 2 3Ferissa MohammadNo ratings yet
- Cambridge International AS & A Level: Biology 9700/41Document17 pagesCambridge International AS & A Level: Biology 9700/41srividhyaNo ratings yet
- Jurnal New 3 PDFDocument134 pagesJurnal New 3 PDFMahda LNNo ratings yet
- Kuliah 1 Proses Pembentukan UrineDocument30 pagesKuliah 1 Proses Pembentukan UrineImpi SusantiNo ratings yet
- Biology 2000 Paper I Marking SchemeDocument4 pagesBiology 2000 Paper I Marking Schemeapi-2642329075% (4)
- 5 - Physiology MCQ Body Fluids & HormonesDocument5 pages5 - Physiology MCQ Body Fluids & Hormonesaboody omerNo ratings yet
- Urinary SystemDocument5 pagesUrinary SystemJushelle Anne Tigoy Pilare100% (1)
- A Nursing Case StudyDocument105 pagesA Nursing Case StudyStephen Tumbaga75% (4)
- Renal Physiology PDFDocument24 pagesRenal Physiology PDFMishal IlyasNo ratings yet
- 2.0 Urinary SystemDocument45 pages2.0 Urinary Systemincognitus94100% (2)
- Expt 29 Urine Formation PDFDocument15 pagesExpt 29 Urine Formation PDFGene PabayosNo ratings yet
- Excretion in HumansDocument5 pagesExcretion in HumansGianina Shakila EdwardNo ratings yet
- Acute GlomerulonephritisDocument1 pageAcute GlomerulonephritisAyrheen FornolesNo ratings yet
- Renal Pharmacology 2023Document116 pagesRenal Pharmacology 2023sami MesfinNo ratings yet
- Excretory Products and Their Elimination Diagram+Matching BasedDocument31 pagesExcretory Products and Their Elimination Diagram+Matching Basedshivamkumarbgs724No ratings yet
- Endocrine SystemDocument42 pagesEndocrine SystemBio CheNo ratings yet
- Excretory SystemDocument37 pagesExcretory SystemBlister CountNo ratings yet
- Kidneys: Evaluating and Treating TheDocument42 pagesKidneys: Evaluating and Treating TheSebastián Hernández GarcíaNo ratings yet
- CBSE Class 11 Biology Sample Paper-01 (Solved)Document15 pagesCBSE Class 11 Biology Sample Paper-01 (Solved)cbsesamplepaperNo ratings yet
- D11.44 - Kel10 - Gagal Ginjal KronisDocument16 pagesD11.44 - Kel10 - Gagal Ginjal KronisNAZILLA PUTRINo ratings yet
- European J of Heart Fail - 2022 - Mullens - Renal Effects of Guideline Directed Medical Therapies in Heart Failure ADocument17 pagesEuropean J of Heart Fail - 2022 - Mullens - Renal Effects of Guideline Directed Medical Therapies in Heart Failure ALaura LizarazoNo ratings yet
- Sistem Perkemihan (: The Urinary System)Document25 pagesSistem Perkemihan (: The Urinary System)Dedy SavradinataNo ratings yet
- Answers To Questions: Activity 1: Hematocrit Determination (Pp. Pex-71-72)Document14 pagesAnswers To Questions: Activity 1: Hematocrit Determination (Pp. Pex-71-72)march33350% (2)
- Gnaps EmedicineDocument13 pagesGnaps Emedicineharyanti lupitaNo ratings yet
- Proteinuria A Guide To Diagnosis and AssDocument7 pagesProteinuria A Guide To Diagnosis and AssMarcelliaNo ratings yet
- Excretory Products and Their EliminationDocument9 pagesExcretory Products and Their EliminationBiju MylachalNo ratings yet
























































![Renal Diet Cookbook for Beginners: Enjoy Delicious, Kidney-Friendly Recipes with Balanced Sodium, Phosphorus, and Potassium Levels [III EDITION]](https://imgv2-1-f.scribdassets.com/img/word_document/623037346/149x198/5582c31ab3/1711569018?v=1)