Professional Documents
Culture Documents
Pain Management After C Section 3.5.18
Uploaded by
May VerOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pain Management After C Section 3.5.18
Uploaded by
May VerCopyright:
Available Formats
Managing Pain after Your Cesarean (C-section)
A C-section delivery is a major surgery. Most women need pain medication after the birth. Controlling pain
makes it easier to feed and take care of your baby. Pain can stop you from wanting to walk or take deep
breaths which can make it easier for you to get blood clots or chest infections (pneumonia).
There are several medicines that can help with pain after surgery. These medicines work better together than
a high dose of one medicine by itself. It can be hard to remember what medicines you have taken. The sheet
below will help you keep track.
Ibuprofen (Motrin/Advil) and acetaminophen (Tylenol)
These two medicines can be taken at the same time, and they have few side effects. We recommend taking
ibuprofen and acetaminophen together on a schedule, 4 times each day, for 2 weeks after you leave the
hospital. Missing doses increases the chances of feeling worse pain. A stronger medication (Narcotic/Opioid)
may be needed to help reduce the pain if you have a missed dose. Narcotics have more side effects for you
and the baby. Remember to take food with Ibuprofen since it can upset your stomach.
You should not take ibuprofen if you have bleeding in your stomach or intestines, a clotting disorder, severe
kidney disease, an allergy to aspirin or NSAIDS, or have had gastric bypass surgery.
You should not take acetaminophen if you have liver disease or an allergy to acetaminophen.
Opioid pain medications: Oxycodone, hydrocodone or hydromorphone
Opioids can make you sleepy, nauseated, and constipated. Only take opioids if your pain is not controlled with
ibuprofen and acetaminophen. Bring any opioid pills that you have left over the outpatient pharmacy at UNC
Hospital or UNC Hillsborough. They will get rid of them properly so no harm occurs to anyone else
(http://bit.ly/UNCMedSafe), or return them to an Operation Medicine Drop location
(http://bit.ly/NCMedDrop). There is a risk that these medications can be misused and become habit forming.
Always use these opioid painkillers as directed by a health care provider.
Breastfeeding and medication
Many moms want to know if these medications are safe for their baby if they breastfeed. All these
medications are in breast milk in small amounts. When taking your medicine as ordered, the amount is small
and is safe for your baby. If your baby is not waking for feedings (8 or more feedings every day), is limp or is
feeding poorly, call your baby’s provider right away.
Healing after your C-section
It's important to get rest and eat well after your c-section. Ask friends and family to help with household tasks
and care for older children in the home. Encourage visitors to bring a meal or help with chores. At night, it may
help to set up “shifts” with your support person for a 5-6 hour period. During this time, the support person
can bring baby to you to breastfeed while you are resting in bed. Then, you can go back to sleep while another
caregiver takes care of burping, diaper changes, and settling your baby.
When to call your provider
Your pain should gradually get better. Call your provider if:
• Your pain is getting worse or you need more oxycodone then the day before.
• You have a fever of 101 F (38.3 Celsius) or higher
• The skin around your incision is turning pink or red
• Your incision opens
• There is blood or any fluid is draining from your incision
During regular business hours, call your prenatal care provider. After hours and weekends, call the UNC page
operator, 984-974-1000, and ask for the OB provider on call.
Approved by NC Women’s Hospital Patient Education Committee, March 5th, 2018
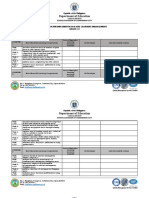
Your Pain Medications
You can use this chart to keep track of when you've taken your pain medication.
Day Ibuprofen Acetaminophen Your pain, on a Oxycodone
Dose # / Time 600 mg, every 6 650 mg, every 6 scale of 0-10 5 mg, if your pain
hours hours is greater than 4
1/ [] [] ()
Discharge
2/ [] [] ()
3/ [] [] ()
Day
4/ [] [] ()
1/ [] [] ()
Day 1 after
discharge
2/ [] [] ()
3/ [] [] ()
4/ [] [] ()
1/ [] [] ()
Day 2 after
discharge
2/ [] [] ()
3/ [] [] ()
4/ [] [] ()
1/ [] [] ()
Day 3 after
discharge
2/ [] [] ()
3/ [] [] ()
4/ [] [] ()
1/ [] [] ()
Day 4 after
discharge
2/ [] [] ()
3/ [] [] ()
4/ [] [] ()
1/ [] [] ()
Day 5 after
discharge
2/ [] [] ()
3/ [] [] ()
4/ [] [] ()
1/ [] [] ()
Day 6 after
discharge
2/ [] [] ()
3/ [] [] ()
4/ [] [] ()
Approved by NC Women’s Hospital Patient Education Committee, March 5th, 2018
You might also like
- Autogenic TrainingDocument243 pagesAutogenic TrainingDemosten100% (4)
- Please Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - English 1Document2 pagesPlease Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - English 1mommie magicNo ratings yet
- Please Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - English 2Document2 pagesPlease Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - English 2mommie magicNo ratings yet
- Please Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - Non-Verbal Reasoning 1Document2 pagesPlease Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - Non-Verbal Reasoning 1Paul ScottNo ratings yet
- 11 Plus Queen Elizabeths School 11 PDFDocument1 page11 Plus Queen Elizabeths School 11 PDFmommie magicNo ratings yet
- Please Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - Mathematics 2Document1 pagePlease Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - Mathematics 2biju mathewNo ratings yet
- Test 6Document1 pageTest 6Zawata Afnan ShararaNo ratings yet
- Please Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - Verbal Reasoning 1Document2 pagesPlease Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - Verbal Reasoning 1Paul ScottNo ratings yet
- Please Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - Mathematics 1Document1 pagePlease Mark Boxes With A Thin Horizontal Line Like This .: Familiarisation Answer Sheet - Mathematics 1mommie magicNo ratings yet
- Alternity Skill SheetsDocument8 pagesAlternity Skill SheetsGregory HuelsenbeckNo ratings yet
- Service Bulletin: Issued by Canon Europa N.VDocument6 pagesService Bulletin: Issued by Canon Europa N.Valfred vivien bossonNo ratings yet
- Neet 2018 Exam: Answer Key (Code-AA)Document1 pageNeet 2018 Exam: Answer Key (Code-AA)Kembhavi SMNo ratings yet
- General Information (Cover Sheet) Date: - / - / - : Section 46.3 (B)Document29 pagesGeneral Information (Cover Sheet) Date: - / - / - : Section 46.3 (B)Gino AndersonNo ratings yet
- Ar 1 Science Year 4 Paper 2Document9 pagesAr 1 Science Year 4 Paper 2aliya aliyaNo ratings yet
- Questioner For De-Mat AcquisitionDocument4 pagesQuestioner For De-Mat AcquisitionRonit RoyNo ratings yet
- Sains DLP Y4 Paper 2Document8 pagesSains DLP Y4 Paper 2rasputein69No ratings yet
- DRP Test Templates FullDocument6 pagesDRP Test Templates Fullkhattab.agencyNo ratings yet
- Science Year 4 Paper 2 (40 Marks)Document9 pagesScience Year 4 Paper 2 (40 Marks)Nsem RaoNo ratings yet
- BFT 223Document4 pagesBFT 223Santheya RamanNo ratings yet
- Please Mark Like This .: English Test DDocument2 pagesPlease Mark Like This .: English Test DJaneNo ratings yet
- DB Project Proposal TemplateDocument3 pagesDB Project Proposal TemplateBama DamaNo ratings yet
- Filing of Leave ( - ) : Revised 1994Document1 pageFiling of Leave ( - ) : Revised 1994Michelle YuNo ratings yet
- Neet 2018 Answer Key Code ZZDocument1 pageNeet 2018 Answer Key Code ZZSubhabrata MabhaiNo ratings yet
- Ȁ - 4Q80 (4qxii ȌDocument27 pagesȀ - 4Q80 (4qxii ȌReinaldo CamposNo ratings yet
- IiftansDocument12 pagesIiftansIpshita RanjanaNo ratings yet
- Ȁ - Ͷͺ (4QXII Ȍ -Document20 pagesȀ - Ͷͺ (4QXII Ȍ -Reinaldo CamposNo ratings yet
- Manyacat: ManyaDocument13 pagesManyacat: Manyaapi-3719468No ratings yet
- 1678736990276checklist de Manutenção - VidenciDocument5 pages1678736990276checklist de Manutenção - VidenciRenan CorradiniNo ratings yet
- Please Mark Like This .: English Test ADocument2 pagesPlease Mark Like This .: English Test AJaneNo ratings yet
- BTS 04 QP (Aatp)Document29 pagesBTS 04 QP (Aatp)Muk esh.NNo ratings yet
- Nahum/ - Ͷͺʹ -Document7 pagesNahum/ - Ͷͺʹ -Reinaldo CamposNo ratings yet
- Tabe Lce Pat 290919050227Document2 pagesTabe Lce Pat 290919050227ANNo ratings yet
- Clinical Pathway Pre Eklampsi BeratDocument3 pagesClinical Pathway Pre Eklampsi BeratSudirtoNo ratings yet
- EUT 442 2016 2017 Sem2 PDFDocument7 pagesEUT 442 2016 2017 Sem2 PDFRina YeohNo ratings yet
- Relational Algebra DBMS Q&ADocument3 pagesRelational Algebra DBMS Q&AJoyceNo ratings yet
- RA Datalog Tutorial SolDocument3 pagesRA Datalog Tutorial Solstudy materialNo ratings yet
- RA-Datalog-Tutorial - Sol PDFDocument3 pagesRA-Datalog-Tutorial - Sol PDFOperation ResearchNo ratings yet
- Assignment 6 Solar ERGY 420Document14 pagesAssignment 6 Solar ERGY 420Mostafa Ahmed ZeinNo ratings yet
- University of Cambridge International Examinations International General Certificate of Secondary Education English As A Second LanguageDocument8 pagesUniversity of Cambridge International Examinations International General Certificate of Secondary Education English As A Second LanguageSPITFAXSNo ratings yet
- Please Mark Like This .: English Test BDocument2 pagesPlease Mark Like This .: English Test BJaneNo ratings yet
- Matrices Previous Years Board Questions 2000 To 2020 With Solutions of Isc Class 12 MathsDocument22 pagesMatrices Previous Years Board Questions 2000 To 2020 With Solutions of Isc Class 12 MathsAnanthi DNo ratings yet
- University of Cambridge International Examinations International General Certificate of Secondary EducationDocument8 pagesUniversity of Cambridge International Examinations International General Certificate of Secondary EducationMay TahaNo ratings yet
- JNV ReasDocument13 pagesJNV ReasSushant KumarNo ratings yet
- Administrator Remarks: Quiz 11 - Section 1 #0000002538 - On May 4, 2017 15:48Document4 pagesAdministrator Remarks: Quiz 11 - Section 1 #0000002538 - On May 4, 2017 15:48tunahan küçükerNo ratings yet
- Proyecto The Ultimate CherchaDocument2 pagesProyecto The Ultimate CherchatheultimatecherchaNo ratings yet
- Audiology Output Not CorrectDocument3 pagesAudiology Output Not Correctsunilverma2010No ratings yet
- ePARmedX Physician Clearance Form 2014Document2 pagesePARmedX Physician Clearance Form 2014Hermoine GrangerNo ratings yet
- Assessment Protocol and Forms (Oct 2019)Document31 pagesAssessment Protocol and Forms (Oct 2019)Michael ChanNo ratings yet
- C1100 SM O-77-78 CorrectedDocument3 pagesC1100 SM O-77-78 CorrectedStefan TintilaNo ratings yet
- DSS - 4Q79d (4QXIId) Full PDFDocument1 pageDSS - 4Q79d (4QXIId) Full PDFReinaldo CamposNo ratings yet
- Fragments 1-2: 4Q79 (4QXII Ȍ - IonDocument1 pageFragments 1-2: 4Q79 (4QXII Ȍ - IonReinaldo CamposNo ratings yet
- Ruta Mas Corta2 PDFDocument2 pagesRuta Mas Corta2 PDFmarisaNo ratings yet
- PDF Kurasa Kasihmu Koor Campuran CompressDocument2 pagesPDF Kurasa Kasihmu Koor Campuran CompressRsppb PertamedikaNo ratings yet
- Single Elimination Tournament Brackets: InstructionsDocument21 pagesSingle Elimination Tournament Brackets: InstructionsWavewenasNo ratings yet
- NC2630 - System Analysis and Design L4 Memo Sup 2013Document9 pagesNC2630 - System Analysis and Design L4 Memo Sup 2013bronstoffNo ratings yet
- Single Elimination Tournament Brackets: InstructionsDocument21 pagesSingle Elimination Tournament Brackets: InstructionsHivzo BektovicNo ratings yet
- Single-Elimination-Bracket TEMPLATESDocument22 pagesSingle-Elimination-Bracket TEMPLATESsummerdawn2317No ratings yet
- Abraham Tjoa - Iiic-1321094083Document16 pagesAbraham Tjoa - Iiic-1321094083Abraham TjoaNo ratings yet
- Laporan Praktikum Statistika Dan Probabilitas: Nama: Abraham Tjoa NIM: 1321094083Document16 pagesLaporan Praktikum Statistika Dan Probabilitas: Nama: Abraham Tjoa NIM: 1321094083Abraham TjoaNo ratings yet
- Illustrated Synopsis of Dermatology and Sexually Transmitted DiseasesDocument1 pageIllustrated Synopsis of Dermatology and Sexually Transmitted DiseasesManoj PavanNo ratings yet
- 2020 Taiwan - Acute Pancreatitis GuidelineDocument10 pages2020 Taiwan - Acute Pancreatitis Guideline吳任爵No ratings yet
- Taylor Norris Resume 2024 1Document3 pagesTaylor Norris Resume 2024 1api-724277113No ratings yet
- President Michael Sata's Speech To The Second Session of The Eleventh National AssemblyDocument76 pagesPresident Michael Sata's Speech To The Second Session of The Eleventh National AssemblyPMRCZAMBIANo ratings yet
- RA11166 National HIV Law PresentationDocument40 pagesRA11166 National HIV Law PresentationRoots of HealthNo ratings yet
- Infection Control Programmes To Control Antimicrobial ResistanceDocument53 pagesInfection Control Programmes To Control Antimicrobial ResistanceDimas RfNo ratings yet
- General Risk Assessment Form: Part A. Assessment DetailsDocument7 pagesGeneral Risk Assessment Form: Part A. Assessment DetailsBuster SmithNo ratings yet
- Traditional and Complementary Medicine: SciencedirectDocument10 pagesTraditional and Complementary Medicine: SciencedirectAuliaulfaNo ratings yet
- Ebr MacalolotDocument4 pagesEbr Macalolotquen.chuaNo ratings yet
- Lorma Colleges Con Template Nursing Care Plan With Fdar Related Learning ExperienceDocument4 pagesLorma Colleges Con Template Nursing Care Plan With Fdar Related Learning ExperienceMark Jason GalangNo ratings yet
- Apta Code of EthicsDocument13 pagesApta Code of Ethicskim suhoNo ratings yet
- Who Uhc Sds 2019.6 EngDocument98 pagesWho Uhc Sds 2019.6 EngKusnadi CilukNo ratings yet
- Notice: Applications, Hearings, Determinations, Etc.: Millette, Michael J., M.D.Document4 pagesNotice: Applications, Hearings, Determinations, Etc.: Millette, Michael J., M.D.Justia.comNo ratings yet
- Horizontal ViolenceDocument6 pagesHorizontal Violenceapi-312055738No ratings yet
- Cabadbaran MAPEH 10 MELCDocument13 pagesCabadbaran MAPEH 10 MELCHoney NakilaNo ratings yet
- Clinical Trials in Korea - Why KoreaDocument9 pagesClinical Trials in Korea - Why KoreaTony LowNo ratings yet
- B.C. Doctors Call C. Difficile Handling at Burnaby Hospital 'Medical Negligence'Document11 pagesB.C. Doctors Call C. Difficile Handling at Burnaby Hospital 'Medical Negligence'ProvinceNewspaperNo ratings yet
- Alternative TherapyDocument2 pagesAlternative TherapysathyasindhujaNo ratings yet
- Community PharmacyDocument5 pagesCommunity PharmacyAnoosha FarooquiNo ratings yet
- The Role of Architecture in Promoting Healing Environments in The Design of Small, Rural HospitalsDocument6 pagesThe Role of Architecture in Promoting Healing Environments in The Design of Small, Rural Hospitalsellica123No ratings yet
- Physiotherapy CoursesDocument7 pagesPhysiotherapy Courseskannadiparamba100% (1)
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary Detailsyenduri sampathNo ratings yet
- LISTENING PRACTICE TEST 2 (Ex4 - Ex6)Document3 pagesLISTENING PRACTICE TEST 2 (Ex4 - Ex6)awklenguyenNo ratings yet
- Donaldsons' Essential Public Health (PDFDrive)Document375 pagesDonaldsons' Essential Public Health (PDFDrive)anibiris12No ratings yet
- Pill Cam - 2Document2 pagesPill Cam - 2Anil MekalaNo ratings yet
- Aric Vrnada 2Document18 pagesAric Vrnada 2Indra GunawanNo ratings yet
- Evidence Based Reading FormatDocument1 pageEvidence Based Reading Formatako at ang exoNo ratings yet
- Brit J Clinical Pharma - 2021 - Tusino - Rethinking The Role of Research Ethics Committees in The Light of Regulation EUDocument7 pagesBrit J Clinical Pharma - 2021 - Tusino - Rethinking The Role of Research Ethics Committees in The Light of Regulation EUCanache DamianNo ratings yet
- Lesson 4-Uniform Hospital Discharge Data SetDocument14 pagesLesson 4-Uniform Hospital Discharge Data SetSwamyNo ratings yet