Professional Documents
Culture Documents
Code Status and Advance Directives
Uploaded by
sehrCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Code Status and Advance Directives
Uploaded by
sehrCopyright:
Available Formats
Applies To: All HSC Hospitals
Responsible Department: Office of Clinical Affairs
Title: Code Status Orders and Advance Directives Procedure
Patient Age Group: ( ) N/A (X) All Ages ( ) Newborns ( ) Pediatric ( ) Adult
DESCRIPTION
The purpose of this procedure is to describe the procedures for documenting a patient’s code
status and/or advance directive.
REFERENCES
• Policy, Advance Directives and Patient Self-Determination
• Policy, Age of Majority and Emancipation of Minors
• Policy, Cardiopulmonary Resuscitation (CPR) Procedure, Documentation and
Quality Improvement
• Policy, Patient Rights and Responsibilities
• NMSA 24-7A-1 through 24-7A-18, New Mexico Uniform Health Care Decisions Act
AREAS OF RESPONSIBILITY
• Office of Clinical Affairs
• Nursing Council
PROCEDURE
1. Code Status Orders
a. Appropriate discussion of code status and advance directives with patients and
families is encouraged.
b. A Code Status Order will ordinarily be considered only when a patient has an
incurable medical condition or an irreversible terminal illness process such that
all-inclusive life-sustaining efforts would not be medically indicated or
appropriate, or would be futile.
c. If the patient has the capacity to make medical decisions, the order will be
discussed with the patient and the patient must agree with the order before it is
given.
d. If the patient has an advance directive, the patient’s wishes as expressed in the
advance directive will be respected pursuant to the New Mexico Uniform Health
Care Decisions Act.
e. If the patient has been determined to lack the capacity to make medical decisions,
the patient’s guardian, agent or surrogate decision-maker pursuant to the New
Mexico Uniform Health Care Decisions Act will be consulted and must agree
with the order before it is given. If that guardian, agent or surrogate decision-
maker disagrees with the patient’s advance directive, the advance directive takes
precedence, pursuant to the New Mexico Uniform Health Care Decisions Act.
f. When appropriate, an unemancipated minor patient should be involved in the
decision-making process and may assent.
g. When appropriate, the wishes of the immediate family should also be considered
in arriving at the decision.
Title: Code Status and Advance Directives
Owner: Associate Dean for Clinical Affairs
Effective Date: 7/18/2008
Doc. #2348
Page 1 of 4
h. In the event of ethical conflicts or difficulties in decision-making, the treatment
team may wish to consult with the Biomedical Ethics Committee to facilitate
discussion and decision making.
i. The Code Status Order will be written, signed, dated, and timed by the attending
physician; or by the house officer or allied healthcare professional (AHP) with the
approval of the attending physician after discussion. The circumstances
surrounding the order will be documented in the patient’s chart by the ordering
practitioner. Documentation will include:
i. a summary of the medical situation;
ii. the outcome of consultation with other practitioners, if indicated;
iii. a statement summarizing the disclosure of information and outcome of
discussions with the patient, guardian, agent or surrogate decision-maker,
if such occurred.
j. Nursing staff and clerical staff will follow usual procedures for taking off the
order, and will also flag any existing physical chart to indicate that a Code Status
Order is in effect.
k. A Code Status Order remains in effect until an order cancelling the Code Status
Order is written by the attending physician; or by the house officer or AHP with
the approval of the attending physician after discussion. If a Code Status Order is
cancelled, nursing staff and clerical staff will follow usual procedures for taking
off the cancelling order, and will also remove any flags that had been placed on
the patient’s physical chart related to the cancelled Code Status Order.
l. A Code Status Order, or an order cancelling a Code Status Order, must be
handwritten in the paper chart, or entered into the electronic medical record, by
the ordering practitioner. Verbal or telephone orders will not be accepted for
initiation or cancellation of a Code Status Order.
m. For the purposes of this policy, a Code Status Order stating ‘Do Not Resuscitate’
or ‘No Code’ means that in the event of a cardiopulmonary arrest, none of the
following interventions will be initiated:
i. cardiopulmonary resuscitation (CPR)
ii. electrical defibrillation/cardioversion
iii. cardiac pacing
iv. mechanical ventilation
v. intubation (endotracheal or nasotracheal)
vi. manual bag/mask ventilation
vii. tracheostomy
viii. administration of medications for the purpose of cardiopulmonary
resuscitation (this includes, but is not limited to, vasoactive agents, pressor
agents, antiarrhythmic agents, or sodium bicarbonate).
n. For the purposes of this policy, a Code Status Order stating ‘Do Not Intubate’
means that the patient will not be intubated (including endotracheally,
nasotracheally, or through a tracheostomy). Other resuscitative efforts may or
may not be implemented, in accordance with whatever other Code Status Order(s)
or advance directives are in effect.
o. The patient, or the patient’s advance directive, or the patient’s guardian, agent or
surrogate decision-maker pursuant to the New Mexico Uniform Health Care
Decisions Act, may also have decided that limited or less than full resuscitative
effort should be made in the event of the patient having a cardiopulmonary arrest.
Title: Code Status and Advance Directives
Owner: Associate Dean for Clinical Affairs
Effective Date: 7/18/2008
Doc. #2348
Page 2 of 4
In these circumstances, a ‘Do Not Resuscitate’ or ‘No Code’ order SHOULD
NOT be used. Instead, a Code Status Order should be written specifying what
interventions are to be implemented or not implemented. A ‘Do Not Intubate’
order is an example of such a Code Status Order.
p. This document should not be construed to mean that the therapeutic interventions
commonly used during resuscitative efforts may not be used in the routine care of
a patient exclusive of a cardiopulmonary arrest. For example, a patient with a ‘No
Code’ order in place who develops a cardiac arrhythmia without cardiopulmonary
arrest may still be treated with an anti-arrhythmic agent as part of routine patient
care.
q. Specific to patients undergoing procedures in the operating room or otherwise
requiring general sedation or anesthesia, consent to the procedure and to the
anesthesia includes consent to associated temporary intubation for administration
of anesthetic agents and to sustain respiratory status during the procedure; and
consent to temporary use of therapeutic interventions also associated with
resuscitative efforts (e.g., the use of pressor agents). These temporary measures
should not be seen as conflicting with a Code Status Order. The treating clinician
may wish to clarify these matters with the patient, or with the patient’s guardian,
agent or surrogate decision-maker, prior to the procedure.
r. Whether or not a Code Status Order is in effect, every necessary measure will be
taken to relieve the patient’s suffering and to maintain the patient’s comfort.
s. In the event of a cardiopulmonary arrest, and if there is no Code Status Order in
effect, cardiopulmonary resuscitation may be initiated when clinically
appropriate.
2. Advance Directives
a. When a treating clinician determines that the patient has an advance directive, the
treating clinician will obtain a copy of the advance directive for inclusion in the
patient’s medical record. The treating clinician will also document in the Problem
List section of the patient’s medical record that an advance directive exists (e.g.
“Advance Directive in Effect”).
b. When a patient with an advance directive in effect is admitted, the admitting
attending physician, house officer or AHP will include in the admission orders a
statement that an advance directive is in effect. The admitting attending
physician, house officer or AHP is also strongly encouraged to include in the
admitting orders, progress notes, or admission history a statement about where the
advance directive may be located (e.g., “A copy of the advance directive is in the
Legal section of the patient’s chart.”).
c. The patient’s treatment team will familiarize themselves with the contents of the
advance directive.
d. When discussing an advance directive with a patient, family members, surrogate
or guardian, the clinician may wish to consider discussion of code status,
including cardiopulmonary resuscitation; resuscitative medications; cardiac
pacing; intubation; mechanical ventilation; enteral or parenteral feeding; ongoing
IV fluid use; dialysis; blood transfusion; and invasive procedures or surgeries.
Clinical judgment is, however, always the first guide in any such discussion.
e. The treatment team may also wish to review the University Hospitals policy
Advance Directives and Patient Self-Determination, and NMSA 24-7A-1 through
24-7A-18, New Mexico Uniform Health Care Decisions Act.
Title: Code Status and Advance Directives
Owner: Associate Dean for Clinical Affairs
Effective Date: 7/18/2008
Doc. #2348
Page 3 of 4
DEFINITIONS
1. ‘Code Status Order’ – A code status order is a medical order for the resuscitative efforts a
patient (or patient’s surrogate) wishes to occur, or not to occur.
2. ‘Advance Directive’ – An advance directive is a statement of instructions for health care
made by a person with capacity. In particular, an advance directive usually states the
person’s wishes for health care in the event that they develop a seriously debilitating or
terminal illness.
3. ‘Allied Healthcare Professional’ (AHP) – For the purposes of this document, an AHP is
an advanced practice nurse or physician assistant who is a member of the associate
medical staff and a member of the patient’s treatment team.
4. ‘Capacity’ – Capacity is an individual's ability to understand and appreciate the nature
and consequences of proposed health care, including its significant benefits, risks and
alternatives to proposed health care; and to make and communicate an informed health-
care decision.
SUMMARY OF CHANGES
Replaces the previous policies, “No Code or DNR” (5/1999), and “Do Not Resuscitate in
Operating Room” (2/2005).
RESOURCES/TRAINING
• Biomedical Ethics Committee
• Office of Risk Management
• Office of Clinical Affairs
• Office of University Counsel
DOCUMENT APPROVAL & TRACKING
Item Contact Date Approval
Owner Associate Dean for Clinical Affairs
Clinical Operations PPG Committee
Committee(s) Y
UNMHSC Medical Executive Committee
Nursing Officer Judy Spinella, MBA, MSN, RN, Chief Nursing Officer Y
Medical Director/Officer Robert Bailey MD, Associate Dean for Clinical Affairs Y
Official Approver Robert Katz, MD, Vice President for Clinical Affairs
Official Signature
Official Approver Steve McKernan, Vice President for Clinical Operations
Official Signature
Effective Date 7/18/2008
Origination Date 7/1985
Issue Date Clinical Operations P&P Coordinator 7/18/2008
Title: Code Status and Advance Directives
Owner: Associate Dean for Clinical Affairs
Effective Date: 7/18/2008
Doc. #2348
Page 4 of 4
You might also like
- Peri - Operative Nursing: Learning Manual DescriptionDocument41 pagesPeri - Operative Nursing: Learning Manual DescriptionCezanne Cruz100% (4)
- IV Study Guide 2013Document78 pagesIV Study Guide 2013Kaloy KamaoNo ratings yet
- Criticare 8100 Owners Manual PDFDocument182 pagesCriticare 8100 Owners Manual PDFKroumson Ben AboubacarNo ratings yet
- General Consent and Informed Consent in HospitalsDocument5 pagesGeneral Consent and Informed Consent in HospitalsDnyanesh Aitalwad100% (1)
- Nabh Hand Book EnglishDocument26 pagesNabh Hand Book EnglishRashmi Sharma100% (5)
- Writing Patient Care OrdersDocument2 pagesWriting Patient Care OrdersNephrology On-DemandNo ratings yet
- DNRDocument3 pagesDNRAak CeyeNo ratings yet
- DNR OrderDocument3 pagesDNR OrderStephanie Joy EscalaNo ratings yet
- DO NOT RESUSCITATE (DNR) BY DR Shahid Bashir ChaudharyDocument2 pagesDO NOT RESUSCITATE (DNR) BY DR Shahid Bashir ChaudharyshahidchaudharyNo ratings yet
- Do Not Attempt Resuscitation (DNAR) Decisions in The Perioperative PeriodDocument36 pagesDo Not Attempt Resuscitation (DNAR) Decisions in The Perioperative PeriodMichael BenjaminNo ratings yet
- Removal of External Ventricular Drainage Catheter or Intracranial Pressure Device (Adult, Peds)Document4 pagesRemoval of External Ventricular Drainage Catheter or Intracranial Pressure Device (Adult, Peds)Dot DitNo ratings yet
- Do Not Resuscitate in The Operating Room - Suspend or Not To SuspendDocument4 pagesDo Not Resuscitate in The Operating Room - Suspend or Not To SuspendEsteban García EcheverryNo ratings yet
- Discharge Assignment FinalDocument6 pagesDischarge Assignment FinalWendera T. S CooperNo ratings yet
- 02.15 - Labor & DeliveryDocument6 pages02.15 - Labor & DeliveryHoney Semafranca PlatolonNo ratings yet
- Directives: PR Actice GuidelineDocument8 pagesDirectives: PR Actice GuidelineDivina D Galvez-BeronioNo ratings yet
- Sedation Policy LPCH 6 11Document24 pagesSedation Policy LPCH 6 11Tribowo WicaksonoNo ratings yet
- Guidelines For Surgery Outside The Operating Rooms: Elliot Krane, M.DDocument9 pagesGuidelines For Surgery Outside The Operating Rooms: Elliot Krane, M.DilovenursingcaNo ratings yet
- IHOP - 09.13.06 - Initiating and Monitoring RestraintsDocument5 pagesIHOP - 09.13.06 - Initiating and Monitoring RestraintsYazt HyukkieNo ratings yet
- ICE's Hunger Strike ProtocolsDocument5 pagesICE's Hunger Strike ProtocolsLatino RebelsNo ratings yet
- Assesmen Revisi LindaDocument11 pagesAssesmen Revisi Lindawahyu agustinaNo ratings yet
- Dr. MagedDocument7 pagesDr. MagedmagedNo ratings yet
- Ethics in Ot and Patient PreparationDocument8 pagesEthics in Ot and Patient Preparationjosphinenthenya001No ratings yet
- Konsep Clinical PrivilegesDocument5 pagesKonsep Clinical PrivilegesFebryan Cahya PermanaNo ratings yet
- Quality IndicatorsDocument10 pagesQuality IndicatorsKanna NikithaNo ratings yet
- Principles of Surgery: Section 1Document10 pagesPrinciples of Surgery: Section 1Antonella Angulo CruzadoNo ratings yet
- Week 6 DocsDocument18 pagesWeek 6 DocsSHERMINA HASANNo ratings yet
- Informed Consent 1Document11 pagesInformed Consent 1Edah HumaidahNo ratings yet
- Venepuncture Delegate Notes 0118Document27 pagesVenepuncture Delegate Notes 0118Rohit ShindeNo ratings yet
- NaharDocument42 pagesNahargrace0122rnNo ratings yet
- IF - Ethico-Moral PracticeDocument9 pagesIF - Ethico-Moral PracticeDharylle CariñoNo ratings yet
- Legal and Ethical Aspects of Critical Care NursingDocument66 pagesLegal and Ethical Aspects of Critical Care NursingJamille Abenir Lopez100% (2)
- Preoperative Nursing NotesDocument3 pagesPreoperative Nursing NotesPaul Alfred SoNo ratings yet
- Consent Forms V Informed ConsentDocument5 pagesConsent Forms V Informed Consentcamilarahal4No ratings yet
- Consent-Nsw AuDocument3 pagesConsent-Nsw AuNguyễn Nhật HoàngNo ratings yet
- Preoperative EvaluationDocument65 pagesPreoperative Evaluationdr_trialNo ratings yet
- Motorcycle DiariesDocument5 pagesMotorcycle DiariesTharun kumarNo ratings yet
- MSDSDocument31 pagesMSDSNoor ButtNo ratings yet
- The University Hospital Medical Staff Rules RegulationsDocument12 pagesThe University Hospital Medical Staff Rules RegulationsJose C Bello Jr.No ratings yet
- G AnesthesiaPersonnelDocument3 pagesG AnesthesiaPersonnelSudhakar AvanigaddaNo ratings yet
- Wound Debridement (Adult, Neonatal, Peds) PDFDocument4 pagesWound Debridement (Adult, Neonatal, Peds) PDFPangestu KelvinNo ratings yet
- Perioperative NursingDocument13 pagesPerioperative NursingLeah MalateNo ratings yet
- SP8 Lumbar PunctureDocument5 pagesSP8 Lumbar PunctureAgeng RestiNo ratings yet
- Protocol Hospital NurseDocument8 pagesProtocol Hospital NurseDeepak patelNo ratings yet
- Informed Consent Image Guide PDFDocument6 pagesInformed Consent Image Guide PDFRavish MalhotraNo ratings yet
- Bedside Sheets Safety FullDocument6 pagesBedside Sheets Safety FullHue LeNo ratings yet
- Enforceability of The DNR OrdersDocument9 pagesEnforceability of The DNR OrdersMary Grace ChewNo ratings yet
- Admission of PatientDocument7 pagesAdmission of PatientSheyn FajardoNo ratings yet
- Roles of Bone Marrow Transplant Unit Nurses IncludesDocument10 pagesRoles of Bone Marrow Transplant Unit Nurses IncludesGleden UmayamNo ratings yet
- Risk 201008 Medical Records and You PDFDocument4 pagesRisk 201008 Medical Records and You PDFFitra PringgayudaNo ratings yet
- Southwestern University PHINMA School of Medicine Department of Medical Jurisprudence & Medical Ethics Medical Ethics and ProfessionalismDocument8 pagesSouthwestern University PHINMA School of Medicine Department of Medical Jurisprudence & Medical Ethics Medical Ethics and Professionalismthe urvashiNo ratings yet
- NMC CBT Mock Test 2Document13 pagesNMC CBT Mock Test 2Charles Osiako100% (1)
- Chain of Command ProcedureDocument7 pagesChain of Command ProceduresehrNo ratings yet
- Green-Book-Chapter-5Document5 pagesGreen-Book-Chapter-5QworldNo ratings yet
- Referral and Transfer of PatientDocument2 pagesReferral and Transfer of Patientf7.medicalcorporationNo ratings yet
- Orthopaedic Surgery - Pre and Post Operative Management in AdultsDocument30 pagesOrthopaedic Surgery - Pre and Post Operative Management in AdultsMa. Ferimi Gleam BajadoNo ratings yet
- Lumbar PunctureDocument5 pagesLumbar Puncturesetanpikulan100% (1)
- Guidelines For Ambulatory Anesthesia and Surgery PDFDocument2 pagesGuidelines For Ambulatory Anesthesia and Surgery PDFsherlingNo ratings yet
- Directives: PR Actice GuidelineDocument8 pagesDirectives: PR Actice GuidelineJanine AndersonNo ratings yet
- BGH - CAre PlanDocument55 pagesBGH - CAre PlanmalaramamurthyNo ratings yet
- ID - DocumentationDocument4 pagesID - DocumentationDharylle CariñoNo ratings yet
- Construction and RenovationDocument2 pagesConstruction and RenovationsehrNo ratings yet
- Management of Environmental DesignDocument2 pagesManagement of Environmental DesignsehrNo ratings yet
- General PurchasingDocument1 pageGeneral PurchasingsehrNo ratings yet
- 05 Tools For Valuing Creativity and InnovationDocument11 pages05 Tools For Valuing Creativity and InnovationsehrNo ratings yet
- Risk Based Regulation of Pharmacy Full Draft RevisedDocument39 pagesRisk Based Regulation of Pharmacy Full Draft RevisedsehrNo ratings yet
- FullDocument228 pagesFullsehrNo ratings yet
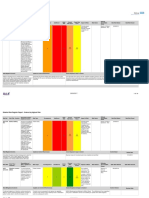
- Risk RegisterDocument16 pagesRisk RegistersehrNo ratings yet
- DrMortonCooper WinningWithYourVoice OCR PROOFED PDFDocument91 pagesDrMortonCooper WinningWithYourVoice OCR PROOFED PDFMano SinghNo ratings yet
- Article Balanced ScorecardDocument2 pagesArticle Balanced ScorecardJi YuNo ratings yet
- Sample Literature Review PDFDocument6 pagesSample Literature Review PDFSubrahmanian NampoothiryNo ratings yet
- PEDIATRIC BURN Clin NorthDocument8 pagesPEDIATRIC BURN Clin NorthRaul PerezNo ratings yet
- Placenta Previa 08Document42 pagesPlacenta Previa 08Sam Ngugi100% (1)
- Numazu Emergency - MayDocument1 pageNumazu Emergency - Mayapi-308447912No ratings yet
- Failure of Amalgam Restoration PDFDocument2 pagesFailure of Amalgam Restoration PDFJaime0% (1)
- Ch05. Lifting and Moving PatientsDocument64 pagesCh05. Lifting and Moving PatientsDamianus Danny100% (1)
- Cerebral PalsyDocument11 pagesCerebral PalsyprasadNo ratings yet
- The Michigan Appropriateness Guide For Intravenous Catheters (MAGIC)Document48 pagesThe Michigan Appropriateness Guide For Intravenous Catheters (MAGIC)Suren VishvanathNo ratings yet
- DH ResumeDocument3 pagesDH Resumeapi-455273650No ratings yet
- Background: Pediatric Chickenpox Next Section: PathophysiologyDocument12 pagesBackground: Pediatric Chickenpox Next Section: PathophysiologyRachel Johann Aquinto100% (1)
- Medical and Mental Health NeedsDocument10 pagesMedical and Mental Health NeedsKim OlsenNo ratings yet
- Chapter 21 PancreasDocument102 pagesChapter 21 PancreasMACON824No ratings yet
- Modul English IDocument326 pagesModul English I177 Gede Agus Purna YogaNo ratings yet
- Strategic Plan: University of Florida College of DentistryDocument15 pagesStrategic Plan: University of Florida College of DentistrySatya AsatyaNo ratings yet
- AnisometropiaDocument2 pagesAnisometropiaAstidya MirantiNo ratings yet
- Marfan SyndromeDocument6 pagesMarfan SyndromeNurhidayu PauziNo ratings yet
- Understanding and Managing Breast Milk JaundiceDocument7 pagesUnderstanding and Managing Breast Milk JaundiceJulian RiveraNo ratings yet
- Amitriptyline HCLDocument2 pagesAmitriptyline HCLGLen CaniedoNo ratings yet
- Soal Uts BikDocument7 pagesSoal Uts Bikfitriani simanjuntakNo ratings yet
- OEM III Module SpecificationsDocument18 pagesOEM III Module SpecificationsCarlosperezm100% (1)
- NOVEMBER 10, 2021 DAY 2 Intensive Care Unit: Critical Care TeamDocument7 pagesNOVEMBER 10, 2021 DAY 2 Intensive Care Unit: Critical Care TeamLeslie PaguioNo ratings yet
- Blake VegliaDocument4 pagesBlake Vegliaapi-400338931No ratings yet
- 14.1 The Hole Inside The Heart ABSTRAKDocument11 pages14.1 The Hole Inside The Heart ABSTRAKYudhistira AdiNo ratings yet
- Wills Eye Manual, The: Office and Emergency Room Diagnosis and Treatment of Eye DiseaseDocument2 pagesWills Eye Manual, The: Office and Emergency Room Diagnosis and Treatment of Eye Diseaseandi uznul0% (1)
- Positions in SurgeryDocument18 pagesPositions in SurgeryRaquel M. MendozaNo ratings yet
- LEAH ALESNA REYES, ROSE NAHDJA, JOHNNY, and minors LLOYD and KRISTINE, all surnamed REYES, represented by their mother, LEAH ALESNA REYES, petitioners, vs. SISTERS OF MERCY HOSPITAL, SISTER ROSE PALACIO, DR. MARVIE BLANES, and DR. MARLYN RICO,respondents.Document9 pagesLEAH ALESNA REYES, ROSE NAHDJA, JOHNNY, and minors LLOYD and KRISTINE, all surnamed REYES, represented by their mother, LEAH ALESNA REYES, petitioners, vs. SISTERS OF MERCY HOSPITAL, SISTER ROSE PALACIO, DR. MARVIE BLANES, and DR. MARLYN RICO,respondents.Ge LatoNo ratings yet
- Intrathecal MorphineDocument6 pagesIntrathecal MorphineJoana MoreiraNo ratings yet