Professional Documents
Culture Documents
Handouts - Oncology
Uploaded by
libalibzyrelleOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Handouts - Oncology
Uploaded by
libalibzyrelleCopyright:
Available Formats
* NLE * NCLEX * HAAD * PROMETRICS * DHA * MIDWIFERY * LET * RAD TECH * CRIMINOLOGY * DENTISTRY * PHARMACY * MED TECH
COMPREHENSIVE PHASE
HANDOUTS
ONCOLOGY
Prepared By: Ms. Jaidee Rojas, RN
MAY 2024 Philippine Nurse Licensure Examination Review
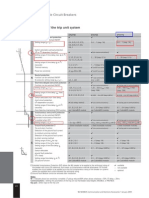
Cell cycle
Cancer
Cells grow uncontrollably which has a tendency to spread to other parts of the body
Oncology
Branch of science that deals with the study, treatment, diagnosis and prevention of cancer.
Carcinogenesis
Cell Adaptation
Risk factors:
1. Viruses and bacteria
2. Physical agents
3. Chemical agents
4. Genetics
5. Lifestyle factors
6. Hormonal agents
Cancer Prevention
PRIMARY PREVENTION
Achieve and maintain healthy weight gain
Adopt a physically active lifestyle
Consume a healthy diet
Limit consumption of alcoholic beverages
TOP RANK REVIEW ACADEMY, INC. Page 1 | 7
SECONDARY PREVENTION
Screening and early detection
TERTIARY PREVENTION
Preventing recurrence
Assessment for development of second malignancies
WARNING SIGNS OF CANCER
C: Change in bowel or bladder habits.
A: A sore that does not heal.
U: Unusual bleeding or discharge.
T: Thickening or lump in the breast or elsewhere.
I: Indigestion or difficulty in swallowing.
O: Obvious change in a wart or mole.
N: Nagging cough or hoarseness.
U: Unexplained anemia.
S: Sudden weight loss.
CANCER DIAGNOSIS
Tumor staging
Tumor grading
Diagnostic Procedures
Tumor marker identification
Analysis of biochemical mediators found in tumor tissue, blood, or other body fluids
Nuclear medicine
Uses IV injection or ingestion of imaging radioisotopes followed by imaging of
tissues that have concentrated the radioisotopes.
Mammography
Pap smear test
Colonoscopy
MRI vs CT scan vs PET scan
Ultrasound
Endoscopy
Fluoroscopy
TOP RANK REVIEW ACADEMY, INC. Page 2 | 7
Biopsy
Management of Cancer
SURGERY
Diagnostic
> Biopsy (Incisional vs excisional)
As Primary Treatment
> Chemosurgery > Cryosurgery
> Electrosurgery > Laser surgery
Prophylactic
Risk reduction surgery
Reconstructive
Attempt to improve function or for cosmetic effect
Palliative
Relieving symptoms and improve QOL
RADIATION THERAPY
• Neoadjuvant
• Prophylactic
• Palliative
Radiosensitive vs. Radioresistant
External vs Internal
CHEMOTHERAPY
Chemotherapeutic agents
CELL CYCLE SPECIFIC (S PHASE)
• TOPOISOMERASE I INHIBITOR: Irinotecan, Topotecan
• TOPOISOMERASE II INHIBITOR: Etoposide, Teniposide
• ANTIMETABOLITES: Cytarabine, 5-fluorouracil, Hydroxyurea, Methotrexate
•
CELL CYCLE SPECIFIC (M PHASE)
MITOTIC SPINDLE INHIBITORS
• PLANT ALKALOIDS: Vinblastine, Vincristine, Vinorelbine
• TAXANE: Paclitaxel, Docetaxel
CELL CYCLE NON-SPECIFIC
• ALKYLATING AGENT
• Busulfan, Carboplatin, Cisplatin, Cyclophosphamide, Nitrogen mustard, Thiotepa
• NITROSUREAS
• Carmustine, Lomustine
•
• ANTITUMOR ANTIBIOTICS
• Bleomycin, Dactinomycin, Daunorubicin, Doxorubicin, Epirubicin, Idarubicin
•
• HORMONAL AGENTS
• Tamoxifen, Fulvestrant, Goserelin
Side effects:
• Nausea and vomiting
• Stomatitis
• Anemia, leukemia, thrombocytopenia
• Kidney injury
• Cardiac toxicity
• Infertility
• Peripheral neuropathy
• Cognitive impairment
• Fatigue
NURSING CARE FOR PATIENTS WITH CANCER
RISK FOR INFECTION
• Place patient in a private room
• Inform patient to avoid contact with people who have known or recent infection
• Instruct staff in careful hand hygiene before and after entering room
• Avoid rectal or vaginal procedures, IM injections, insertion of urinary catheters
• Encourage patient to ambulate in room unless contraindicated.
TOP RANK REVIEW ACADEMY, INC. Page 3 | 7
• Assess IV sites for evidence of infection
RISK FOR IMPAIRED SKIN INTEGRITY
• Avoid the use of soaps, cosmetics, perfumes, lotions, powder in erythematous areas
• Avoid rubbing or scratching skin
• Avoid applying hot water bottles, heating pads
• Avoid exposing the area to sunlight or cold weather
• Avoid tight clothing; Use cotton clothing
IMPAIRED ORAL MUCOUS MEMBRANE INTEGRITY
• Assess oral cavity daily using the same assessment criteria or rating scale.
• Instruct patient to report oral burning, pain, areas of redness, open lesions on oropharyngeal mucosa and lips, pain associated
with swallowing, or decreased tolerance to temperature extremes of food.
• Encourage and assist as needed in oral hygiene.
• Advise patient to avoid irritants such as commercial mouthwashes, alcoholic beverages, and tobacco.
• Avoid irritating foods (acidic, hot, rough, and spicy);
• Use water-based moisturizers to protect lips.
IMPAIRED TISSUE INTEGRITY: ALOPECIA
• Discuss potential hair loss and regrowth with patient and family; advise that hair loss may occur on body parts other than the
head.
• Explore potential impact of hair loss on self- image, interpersonal relationships, and sexuality.
• Explain that hair growth usually begins again once therapy is completed.
Prevent or minimize hair loss through the following:
• Use mild shampoo and conditioner, gently pat dry, and avoid excessive shampooing
• Avoid excessive combing or brushing; use wide-toothed comb.
Suggest ways to assist in coping with hair loss.
• Purchase wig or hairpiece before hair loss.
• Begin to wear wig before hair loss.
IMPAIRED NUTRITIONAL STATUS (ANOREXIA, CACHEXIA, MALABSORPTION)
• Assess and address factors that interfere with oral intake or are associated with increased risk of decreased nutritional status.
• Initiate appropriate referrals for interdisciplinary collaboration to manage factors that interfere with oral intake.
• Suggest smaller, more frequent meals.
• Educate patient to avoid unpleasant sights, odors, and sounds in the environment during mealtime.
• If patient desires, serve alcoholic beverages at mealtime with foods.
• Consider cold foods, if desired.
IMPAIRED NUTRITIONAL STATUS (NAUSEA AND VOMITING)
• Assess the patient’s previous experiences and expectations of nausea and vomiting, including causes and interventions used.
• Adjust diet before and after drug administration according to patient preference and tolerance.
• Prevent unpleasant sights, odors, and sounds in the environment.
• Administer prescribed antiemetics, sedatives, and corticosteroids before chemotherapy and afterward as needed.
• Ensure adequate fluid hydration before, during, and after drug administration; assess intake and output
• Encourage frequent oral hygiene.
FATIGUE
• Encourage balance of rest and exercise; avoiding extended periods of inactivity. At minimum, promote patient’s normal sleep
habits.
• Encourage protein, fat, and calorie intake at least equal to that recommended for the general public.
• Encourage participation in planned exercise programs involving aerobic, resistance, and flexibility training based on individual
limitations and safety measures.
• Encourage the use of relaxation techniques and guided imagery.
CHRONIC PAIN
• Use pain scale to assess pain and discomfort characteristics: location, quality, frequency, duration, etc., at baseline and on an
ongoing basis.
• Assure patient that you know the pain is real and will assist them in reducing it.
• Address myths or misconceptions and lack of knowledge about the use of opioid analgesics.
• Collaborate with patient, primary provider, and other health care team members when changes in pain management are
necessary.
• Explore nonpharmacologic and complementary strategies to relieve pain and discomfort: distraction, imagery, relaxation,
cutaneous stimulation, acupuncture, etc.
GRIEF
• Encourage verbalization of fears, concerns, and questions regarding disease, treatment, and future implications.
• Explore previous successful coping strategies.
• Encourage ventilation of negative feelings, including projected anger and hostility, within acceptable limits.
• Involve spiritual advisor as desired by the patient and family.
• Allow for progression through the grieving process at the individual pace of the patient and family.
DISTURBED BODY IMAGE
TOP RANK REVIEW ACADEMY, INC. Page 4 | 7
• Identify threats to patient’s self-esteem (e.g., altered appearance, decreased sexual function, hair loss, decreased energy, role
changes). Validate concerns with patient.
• Encourage continued participation in activities and decision making.
• Encourage patient to verbalize concerns.
• Assist patient in self-care when fatigue, lethargy, nausea, vomiting, and other symptoms prevent independence.
• Assist patient in selecting and using cosmetics, scarves, hair pieces, hats, and clothing that increase their sense of attractiveness.
PROSTATE CANCER
Risk factors:
Unclear cause
Advancing age
Heavy metal exposure
Smoking
History of sexually transmitted infection
It is more common among men of African American descent.
Assessment:
Asymptomatic in early stages
Hard, pea-sized nodule or irregularities palpated on rectal examination
Gross, painless hematuria
Late sx: weight loss, urinary obstruction, and bone pain radiating from the lumbosacral area down the leg
The prostate-specific antigen level is elevated
Surgical interventions:
• Prostatectomy
• Transurethral resection of the prostate (TURP): The procedure involves insertion of a scope into the urethra to excise
prostatic tissue.
• Suprapubic prostatectomy: Removal of the prostate gland by an abdominal incision with a bladder incision.
• Retropubic prostatectomy: Removal of the prostate gland by a low abdominal incision without opening the bladder.
• Perineal prostatectomy: The prostate gland is removed through an incision made between the scrotum and anus.
CONTINOUOS BLADDER IRRIGATION
Decrease bleeding and to keep the bladder free from clots
• 1 lumen is for inflating the balloon (30 mL)
• 1 lumen is for instillation (inflow)
• 1 lumen is for outflow.
• Maintain traction on the catheter, if applied. Instruct the client to keep the leg straight.
• Run the solution at a rate, as prescribed, to keep the urine pink.
• Avoid heavy lifting, stressful exercise, driving, the Valsalva maneuver, and sexual intercourse for 2 to 6 weeks to prevent strain,
and to call the HCP if bleeding occurs
TESTICULAR CANCER
• Most often occurs between 15-40 years old
• Etiology: Genetics, Cryptorchidism
• Early detection: Monthly Testicular Self Exam
• Assessment: Painless testicular swelling; pulling sensation in scrotum
• Metastasis: Lymphadenopathy, Abdominal masses, gynecomastia, back, pone pain and respiratory symptoms.
Interventions:
• Radiation therapy or chemotherapy as needed.
• Unilateral orchiectomy; Radical orchiectomy; Retroperitoneal lymph node dissection.
• Discuss reproduction, sexuality and fertility information and options with the client.
• Post-operative interventions: Monitor for signs of bleeding, infection, IO, pain management.
• Instruct patient to avoid lifting and strenuous activity
CERVICAL CANCER
Risk factors:
Human papillomavirus (HPV) infection, Cigarette smoking, Reproductive behavior
Assessment:
Painless vaginal postmenstrual and postcoital bleeding
Foul-smelling or serosanguineous vaginal discharge
Pelvic, lower back, leg, or groin pain
Anorexia and weight loss
Leakage of urine and feces from the vagina
Dysuria, Hematuria
Interventions:
• Laser therapy: Boundaries of the lesion are visible during colposcopic examination.
• Cryosurgery: Freezing of the tissues
• Conization: Cone-shaped area of the cervix is removed; Allows the woman to retain reproductive capacity.
• Hysterectomy:
TOP RANK REVIEW ACADEMY, INC. Page 5 | 7
• Pelvic exenteration: The removal of all pelvic contents, for recurrent cancer if no evidence of tumor outside the pelvis and
no lymph node involvement exist.
TYPES OF PELVIC EXENTERATION
Anterior
Removal of the uterus, ovaries, fallopian tubes, vagina, bladder, urethra, and pelvic lymph nodes
Posterior
Removal of the uterus, ovaries, fallopian tubes, descending colon, rectum, and anal canal
Total
Combination of anterior and posterior
OVARIAN CANCER
Assessment:
Abdominal discomfort or swelling
Gastrointestinal disturbances
Dysfunctional vaginal bleeding
Abdominal mass
Elevated tumor marker (i.e., CA-125)
Interventions:
Radiation, chemotherapy
Total abdominal hysterectomy and bilateral salpingo-oophorectomy
ENDOMETRIAL (UTERINE) CANCER
Risk factors
1. Use of estrogen replacement therapy (ERT)
2. Nulliparity
3. Polycystic ovary disease
4. Increased age
5. Late menopause
6. Family history of uterine cancer 7. Obesity
8. Hypertension
9. Diabetes mellitus
Assessment
Abnormal bleeding, esp post-menopausal women
Vaginal discharge
Low back, pelvic, or abdominal pain
Enlarged uterus
Interventions
Radiation, chemotherapy; Progesterone therapy; Tamoxifen
Total abdominal hysterectomy and bilateral salpingo-oophorectomy
BREAST CANCER
Risk factors:
• Age, family history
• Early menarche and late menopause
• Previous cancer of the breast, uterus, or ovaries
• Nulliparity, late first birth
• Obesity
• High-dose radiation exposure to chest
Interventions:
Radiation therapy, chemotherapy; Hormonal manipulation; Surgery
Post operative interventions:
Monitor vital signs.
Position patient semi-fowler’s, affected arm elevated above the level of the heart
Encourage deep breathing exercises
Assess for infection, color changes, bleeding in surgical site
Maintain FE balance, diuretics and low salt diet for severe lymphedema.
LUNG CANCER
Risk factors: Cigarette smoking; Secondhand smoking; Environmental and occupational pollutants
Assessment:
• Cough, Wheezing, Dyspnea
• Hoarseness
• Hemoptysis, blood-tinged or purulent sputum
• Chest pain
• Anorexia and weight loss, weakness
• Diminished or absent breath sounds, respiratory changes
TOP RANK REVIEW ACADEMY, INC. Page 6 | 7
Interventions:
• Monitor vital signs, breath sounds, oxygen saturation.
• Position Fowler’s position; Administer oxygen PRN
• High calorie, high protein, high vitamin diet
• Administer bronchodilators, corticosteroids, analgesics as prescribed
• Provide activity and rest periods as tolerated
• Radiation, chemotherapy, surgery (Thoracotomy, Thoracotomy with lobectomy, Thoracotomy with segmental resection);
thoracentesis
PANCREATIC CANCER
Highly malignant, poor prognosis
Increased age, a history of diabetes mellitus, alcohol use, history of previous pancreatitis, smoking, ingestion of a high-fat diet, and
exposure to environmental chemicals.
Assessment:
• Nausea and vomiting; Jaundice
• Abdominal pain; Unexplained weight loss
• Clay-colored stools
• Glucose intolerance
Diagnostics:
• Endoscopic retrograde cholangiopancreatography
Interventions:
• Radiation
• Chemotherapy
• Whipple procedure
GASTRIC CANCER
No single causative agent has been identified
Risk factors:
H. pylori infection
Diet of smoked, highly salted, processed, or spiced foods
Smoking, alcohol and nitrate ingestion
History of gastric ulcers
Complications:
Hemorrhage, obstruction, metastasis, and dumping syndrome
Assessment:
Early:
• Indigestion Abdominal discomfort
• Full feeling Epigastric, back, or retrosternal pain
Late:
• Weakness and fatigue Anorexia and weight loss
• Nausea and vomiting Dysphagia and obstructive symptoms
• Iron deficiency anemia Ascites; Palpable epigastric mass
Interventions:
• Subtotal Gastrectomy
Billroth I
Gastroduodenostomy
Billroth II
Gastrojejunostomy
• Total Gastrectomy
Esophagojejunostomy
TOP RANK REVIEW ACADEMY, INC. Page 7 | 7
You might also like
- Cancer: Repared By: Glyzza Ann B. BatengaDocument21 pagesCancer: Repared By: Glyzza Ann B. BatengaCristina L. JaysonNo ratings yet
- Oncology NursingDocument89 pagesOncology NursingRennard Christian J. De PerioNo ratings yet
- Antineoplastic AgentsDocument83 pagesAntineoplastic AgentsDwynwen Aleaume GumapacNo ratings yet
- Oncology Nursing: Mohamed IdirssDocument65 pagesOncology Nursing: Mohamed IdirssBsoom .iNo ratings yet
- Nurses' Role in Chemotherapy SafetyDocument41 pagesNurses' Role in Chemotherapy Safetycristina_zaharia865440No ratings yet
- ChemotherapyDocument35 pagesChemotherapynikhl saulNo ratings yet
- Drug Study - Feb 16Document9 pagesDrug Study - Feb 16ciela00034No ratings yet
- ONCOLOGYDocument104 pagesONCOLOGYJhey MalanyaonNo ratings yet
- Case Study:: CholelithiasisDocument19 pagesCase Study:: CholelithiasisGillarhymesNo ratings yet
- Cellular Regulation Student VersionDocument15 pagesCellular Regulation Student VersionCruz YrNo ratings yet
- A2 2b Rle Final DraftDocument59 pagesA2 2b Rle Final DraftQuiannë Delos ReyesNo ratings yet
- Radiation TherapyDocument1 pageRadiation TherapyJayadi D. RaNo ratings yet
- Radiation TherapyDocument48 pagesRadiation TherapyajhaytidongNo ratings yet
- 3. Chemotherapy for Cancer-convertedDocument51 pages3. Chemotherapy for Cancer-convertedHarshika KDGNo ratings yet
- BREAST CANCER CASE PRESENTATIONDocument30 pagesBREAST CANCER CASE PRESENTATIONWendy EscalanteNo ratings yet
- Care of Patients With Cancer of The LiverDocument20 pagesCare of Patients With Cancer of The LiverJumar Vallo ValdezNo ratings yet
- Oncology Nursing: An IntroductionDocument46 pagesOncology Nursing: An IntroductionLea Andreau Echavez SunoganNo ratings yet
- CELLULAR ABERRATIONS DETECTION GUIDEDocument36 pagesCELLULAR ABERRATIONS DETECTION GUIDEmidoNo ratings yet
- Understanding Common Cancers in Sri LankaDocument15 pagesUnderstanding Common Cancers in Sri LankaThisal JayarathnaNo ratings yet
- Radiation TherapyDocument48 pagesRadiation TherapyISICLE GTNo ratings yet
- Anti NeoplasticDocument45 pagesAnti Neoplasticcrvckrocl cvkkcoNo ratings yet
- Nursing and End-of-Life CareDocument26 pagesNursing and End-of-Life CareShafiq Ur RahmanNo ratings yet
- Pediatric Oncology Nursing CareDocument33 pagesPediatric Oncology Nursing CareBSN2G- SABLA-ON LORRAINE ANNENo ratings yet
- Safety Guidelines For Chemotherapy and Radiation Therapy: By: Prof. Marites L. RoblezaDocument32 pagesSafety Guidelines For Chemotherapy and Radiation Therapy: By: Prof. Marites L. RoblezaJerry Able100% (1)
- Perawatan Paliatif: Divisi Onkologi Ginekologi FK UsuDocument41 pagesPerawatan Paliatif: Divisi Onkologi Ginekologi FK UsuPPDS Ivan PasaribuNo ratings yet
- Alterations in Urinary FunctionDocument35 pagesAlterations in Urinary FunctionAaLona RobinsonNo ratings yet
- Drugs For Neoplasia 2023Document24 pagesDrugs For Neoplasia 2023renz bartolomeNo ratings yet
- Elective II Group 1 Chronic IllnessDocument31 pagesElective II Group 1 Chronic IllnessAldrine Albor Anyayahan INo ratings yet
- Antimycobacterials - ReyesDocument22 pagesAntimycobacterials - ReyesVivian CaballeroNo ratings yet
- Radiotherapy NursingDocument35 pagesRadiotherapy NursingMarlon Rey AnacletoNo ratings yet
- Bachelor of Science in Nursing:: Course Module Course Unit WeekDocument8 pagesBachelor of Science in Nursing:: Course Module Course Unit WeekMaye ArugayNo ratings yet
- Chemotherapeutic and ImmunosupressiveDocument43 pagesChemotherapeutic and Immunosupressivearmanuel1390antNo ratings yet
- EBM of Herbal Medicine & Phytopharmaca (Safety and Efficacy)Document40 pagesEBM of Herbal Medicine & Phytopharmaca (Safety and Efficacy)Dwika HerdykiawanNo ratings yet
- Epidemiology of Oral CancerDocument26 pagesEpidemiology of Oral CancerSripriya NagarajanNo ratings yet
- Pharmacotherapy Acid PoisoningDocument5 pagesPharmacotherapy Acid PoisoningMeera ChikhaleNo ratings yet
- Care of The Clients With CancerDocument78 pagesCare of The Clients With Cancercasandra moranteNo ratings yet
- Health Problems Common in Pre SchoolerDocument6 pagesHealth Problems Common in Pre SchoolerHarvey T. Dato-onNo ratings yet
- Anti-NenoplasticsDocument1 pageAnti-NenoplasticsBaebee LouNo ratings yet
- Oral CancerDocument34 pagesOral Cancermalaiya_anuragNo ratings yet
- A. Antineoplastic DrugsDocument48 pagesA. Antineoplastic DrugsKim Shyen BontuyanNo ratings yet
- Cancer of The EsophagusDocument31 pagesCancer of The EsophagusBiway RegalaNo ratings yet
- Nursing Management of Clients with Cellular DisturbancesDocument10 pagesNursing Management of Clients with Cellular Disturbancese항해100% (3)
- ChemotherapyDocument39 pagesChemotherapyAnju Radhika100% (3)
- Cervical CancerDocument16 pagesCervical CancerChoi Gong JuNo ratings yet
- Cancer Detection & TreatmentDocument27 pagesCancer Detection & TreatmentJoo Reyes100% (1)
- Radiation Therapy PDFDocument1 pageRadiation Therapy PDFJames Joel ReyesNo ratings yet
- Care of Patients With Cancer of The LungsDocument20 pagesCare of Patients With Cancer of The LungsJumar Vallo ValdezNo ratings yet
- Dr. Stephen Holt-Dietary Supplement DispensationDocument36 pagesDr. Stephen Holt-Dietary Supplement DispensationStephen Holt MDNo ratings yet
- Oncology Nursing CareDocument120 pagesOncology Nursing CareJoy Q. LimNo ratings yet
- Antimalarial Drugs: Presenter Basil Mupita Rgn/BscneDocument35 pagesAntimalarial Drugs: Presenter Basil Mupita Rgn/BscneTapiwaNo ratings yet
- PoisoningDocument50 pagesPoisoningirenekhatete1No ratings yet
- Nclex & Cgfns Review Bullets 2Document12 pagesNclex & Cgfns Review Bullets 2blazegomezNo ratings yet
- Oncology Nursing CareDocument8 pagesOncology Nursing CareChelsea Aquino100% (2)
- Pengembangan Obat Kanker, HIV, RADocument21 pagesPengembangan Obat Kanker, HIV, RANurul AeniNo ratings yet
- Prevent NCDs through Lifestyle ChangesDocument37 pagesPrevent NCDs through Lifestyle ChangesMigz BolivarNo ratings yet
- Chemotherapy GuideDocument79 pagesChemotherapy GuidePrincess AglibutNo ratings yet
- Superficial Fungal Infections GuideDocument43 pagesSuperficial Fungal Infections GuideNoor AliNo ratings yet
- Community OSCE.Document26 pagesCommunity OSCE.aaaskgamerNo ratings yet
- TDS - Rheofinish 288 FDDocument2 pagesTDS - Rheofinish 288 FDVenkata RaoNo ratings yet
- Applications of Proton Exchange Membrane Fuel CellDocument20 pagesApplications of Proton Exchange Membrane Fuel CellRiri SasyNo ratings yet
- ADAB Member List Provides Contact Details for Development OrganizationsDocument8 pagesADAB Member List Provides Contact Details for Development OrganizationsShipon GhoshNo ratings yet
- Chap4 Q Consumer Behavior and Marketing StrategiesDocument14 pagesChap4 Q Consumer Behavior and Marketing StrategiesAdib WasiNo ratings yet
- GRADE 5 Answer Sheet q1 Module 9&10Document6 pagesGRADE 5 Answer Sheet q1 Module 9&10Jina Mellino OrbitaNo ratings yet
- PNLE III For Care of Clients With Physiologic and Psychosocial AlterationsDocument10 pagesPNLE III For Care of Clients With Physiologic and Psychosocial AlterationsANGELINE PALATINO100% (1)
- ETU 776 TripDocument1 pageETU 776 TripbhaskarinvuNo ratings yet
- Unit 4 - Site PlanningDocument22 pagesUnit 4 - Site PlanningvgdarchNo ratings yet
- Toxicological Effects of Extracts of The Leaves of Scoparia Dulcis On The Brain ofDocument5 pagesToxicological Effects of Extracts of The Leaves of Scoparia Dulcis On The Brain ofFrancis AbuludeNo ratings yet
- Xii Physical Education PracticalDocument3 pagesXii Physical Education PracticalAayush AdlakNo ratings yet
- Quality Operating Process: Manual of Operations Care of PatientsDocument4 pagesQuality Operating Process: Manual of Operations Care of PatientsPrabhat KumarNo ratings yet
- h04 High Sulphidation Epithermal Au Ag CuDocument6 pagesh04 High Sulphidation Epithermal Au Ag CuErenz Emerald AlexandriteNo ratings yet
- Fish Processing CGDocument41 pagesFish Processing CGmelisasumbilon100% (1)
- Dokumen - Tips Daewoo Service Manual Instrument Cluster Matiz-2023Document23 pagesDokumen - Tips Daewoo Service Manual Instrument Cluster Matiz-2023urexalg AlgériaNo ratings yet
- Chapter 3 - HTT547Document33 pagesChapter 3 - HTT547Faadhil MahruzNo ratings yet
- Clearing Clutter With Eft PDFDocument23 pagesClearing Clutter With Eft PDFIftikhar Hassun100% (2)
- Measuring Blood Pressure AccuratelyDocument2 pagesMeasuring Blood Pressure AccuratelyxmantestNo ratings yet
- Snap-On EEDM504D ManualDocument15 pagesSnap-On EEDM504D ManualSnafu168No ratings yet
- Nursing Research in Canada 4th Edition Wood Test BankDocument25 pagesNursing Research in Canada 4th Edition Wood Test BankAllisonPowersrjqo100% (51)
- Guide To Rural England - ShropshireDocument54 pagesGuide To Rural England - ShropshireTravel Publishing100% (2)
- SX SeriesDocument6 pagesSX SeriesmattuttezNo ratings yet
- Moderate and Extreme HypofractionationDocument32 pagesModerate and Extreme HypofractionationsamuelfsjNo ratings yet
- Concept Map (Cells: Sci Bio)Document1 pageConcept Map (Cells: Sci Bio)lu.justina100% (8)
- Food Hydrocolloids: Long Chen, Yaoqi Tian, Yuxiang Bai, Jinpeng Wang, Aiquan Jiao, Zhengyu JinDocument11 pagesFood Hydrocolloids: Long Chen, Yaoqi Tian, Yuxiang Bai, Jinpeng Wang, Aiquan Jiao, Zhengyu JinManoel Divino Matta Jr.No ratings yet
- G.R. No 198799, G.R. No. 229722, G.R. No. 189218Document2 pagesG.R. No 198799, G.R. No. 229722, G.R. No. 189218MACNo ratings yet
- Hydraulic Oil Hy-Gard Transmission John DeereDocument7 pagesHydraulic Oil Hy-Gard Transmission John DeereLuis Sanchez LlicoNo ratings yet
- Red Biotechnology ProjectDocument5 pagesRed Biotechnology ProjectMahendrakumar ManiNo ratings yet
- Raisin Vinegar Production: A Microbiological PerspectiveDocument9 pagesRaisin Vinegar Production: A Microbiological PerspectiveREGINE LOUISE VICTORIA SEVILLANo ratings yet
- Observation of Unknown SpectrumDocument3 pagesObservation of Unknown SpectrumOmar HusseinNo ratings yet
- Lucy Mayienga CV RecentDocument3 pagesLucy Mayienga CV Recentlucy.mayiengaNo ratings yet