Professional Documents
Culture Documents
KassabR - Care Map 3
KassabR - Care Map 3
Uploaded by
ranakassab7Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
KassabR - Care Map 3
KassabR - Care Map 3
Uploaded by
ranakassab7Copyright:
Available Formats
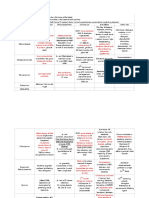
Acute prerenal failure HCC (2023)
Clotrimazole
Betamethazone
(Lotrisone) Topical
BID, apply on armpits
and groin (pt refused)
Tinea Cruris (2013)
GIVEN TO PATIEN: Phytoplex
(Miconazole nitrate 2%) anti-
fungal powder applied on
affected areas (armpits and Mentally challenged (2023) surgical
groin) comlications Dementia Kidney failure
decreased
stress and unfamiliar Immobility due to Dehydration and Metabolic
hearing loss (2019) multi-morbidity HOH
depression environment Obesity (pt's malnutrition disturbances Patient Demographics:
weight is 255 lbs) KEY
Pt Initials: M.W
pt does not drink water Age: 69
unless reminded and he decrease in thirst Sun exposure Functional Advanced age Gender: Male are at Gender: Male Primary Medical
NANDA
Quetiapine/Seroquel Auditory drinks very little water when Renal disease Urinary or fecal retention Risk Factors
dependance (69yo) high risk
100mg PO at night hallucinations
Impaired mental alertness (2018) reminded Ethnicity: white Diagnosis Goal
Code status: Full Code
DOA: 09.09.23 Nursing intervention
340ml fluid intake in decrease in fluid dehydration Pathophysiology Mediactions
12 hours intake Polypharmacy AD: Yes (since 2012 but no new Rationale
Elevated LDL cholesterol level (2018) information was given after 2012)
decrease in waste Fall Risk: High Possible
Paitent's Data
UO is concentrated Labs and Diagnostics
removal from blood Allergies: NKA Complications
(dark yellow) dehydration
Tamsulosin (Flomax) Isolation: standard Evaluation/modification
0.4mg PO qd BPN associated with Nocturia (2016)
Increase in BUN (no Admitting diagnosis: Metabolic
(pt refused) evidence of increased encephalopathy secondary to Clinical Manifestation Patient Related=
BUN because patient dehydration Yellow highlight
chemical and electrolytes keep refusing drawing
imbalance in the blood his blood) Erickson's level: Integrity vs
HTN (2012)
Despair past medical History
Current surgery (NA)
Vitamin C 500mg PO
Mild cerebral atrophy (HCC - chronic) qd (pt refused)
Metabolic
Encephalopathy
(change in mental
status) Zinc sulfate 220mg
PO qd (pt refused) PRIORITY NANDA #1:Dehydration R/T advanced age and decreased fluid intake, history of present illness, non-
Hyperlipidemia type IV compliance AEB confusion, decrease in thirst sensation due to advanced age, fluid intake is 340ml (100ml water
and 240ml soup and coffee), UO is 350ml, urine color is dark yellow and concentrated, patient refuses to drink
water.
right sided frontal
right upper temporal left temporal occipital
Atherosclerosis of aorta (HCC - gyrus disruption
or
junction disruption
or basal ganglion Goal: at the end of the shift, the patient will be more hydrated. AEB patient will have clear yellow urine, output 40-
disruption
chronic) 50ml/hour, and finish around 700-1000ml of his water pitcher in 12 hours.
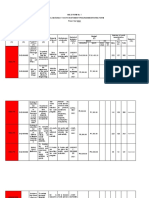
Nursing assessment/intervention:
cholinergic deficiency
Assessment/Monitoring:
Obesity with BMI of 36.6 with
comorbidity 1- I: Assess the patient's hydration by assessing skin turgor and mucosa, and monitor VS q 4 hours
Rationale: if skin tents and takes a few seconds to repel back to its position, it indicates dehydration. Decreases in
BP, increase in HR, increase in temperature, and dry mucosa can be an indicator of dehydration.
-Decrease in Ach PR: The skin wasn't tenting, probably because of obesity, but his mucosa and lips were dry; his blood pressure was
-Decrease in Melatonin
-Increase in Dopamine,
152/89, HR was average between (60-100bpm), and his temperature was normal < 99F.
Priority problem: Noncompliance/refusal R/T patient's altered mental status, LOC and confusion, hearing difficulty and complexity of health Norepinephren and Glutemate
2- I: Assess the patient's intake, output, and urine color.
regimen AEB, pt refuses to take his morning medication, pt refuses his blood to be drawn for lab results (last lab done was 09.11.23), patient
Rationale: Dehydration can result in acute confusion, delirium, and altered mental status; checking the output
refuse his Vital signs to be taken, patient unwilling to respond to nurses when doing their assessment and kick them out of the room, Labile mood, every time the patient voids and ensuring the patient has enough fluid intake of around 1000ml in 12 hours can
other alteration in Seratonin,
HOH, refuse to start an IV on him. prevent complications like confusion and delirium.
histamine and Y-aminobutyric acid
PR: The patient's output at 8:00 in the morning was 200ml - then he voided another time at 16:00, and the output
Goal: was 150ml; his urine characteristics were dark yellow, and he had a loss of ability to follow instructions, a decrease
inflammatory cytokines (C-reactive
By the end of the shift, the patient will be more compliant and implement a positive behavior AEB, VS will be taken q 4 hours (08:00-12:00-16:00), protein, interleukins, interferon and
in orientation, and confused behavior.
the patient will accept taking his medications prescribed for him, start an IV, Improve mood and behavior, and improve the ability to do his ADLs, TNF-alpha) affect the blood brain
barrier permeability Management/Intervention:
pt will allow the phlebotomist to draw his blood.
3- Encouraging fluid intake, at least 2L/day, unless contraindicated.
Rationale: our bodies are made of water. Water boosts physical and mental activity and allows us to flush waste
Nursing Interventions: impairment in products out. Keeping the body hydrated prevents constipation, headache, confusion, and other complications.
cerebral oxidative PR: The patient only had 100ml of water, and the rest of the fluid intake was taken from coffee and soup, 240ml.
metabolism
Assessment/intervention: 4- Check for alternatives; provide ice chips, soups, orange juice, and other fluids other than raw water or flavored
1- I: assess the patient's mental status: LOC (awake, alerted, tired, or lethargic); assess for concentration, clarity of speech, and memory; assess water if provided at the hospital.
mood (depressed, anxious, angry, euphoric); assess the patient's affect (flat, blunted, elated, labile, nervous), assess for hallucinations and Rationale: if someone struggles with drinking water, they can drink flavored water, soups, coffee, or any liquid that
oxidative stress can be counted in the patient's daily fluid intake.
illusions and assess the patient thought process (like see if their thought process is logical, or tangential), ask about their plans in the future and
PR: the patient had half of his soup, did not drink his juice, and had a full cup of coffee in the morning (240ml)
about awareness of their illness. Ask the patient about their family history, relationship with family and friends, and where he lived before, and try
to obtain more information about his life.
alterationin cerebral Patient Education:
Rationale: a brief MSE assessment is used for patients with an altered mental status and can help the nurse know the severity of the patient's
blood flow 5- I: Educate the patient to set an alarm to remind themselves and have the water in front of them so they can
mental condition and maybe identify the reason for the refusal. remind themselves about water and collaborate with the PCT to remind them to drink water.
PR: LOC (awake, alert), mood (angry and anxious, frustrated, agitated, low tolerance for others in the morning), affect (flat, labile). The patient Rationale: geriatric patients have decreased thirst receptors, and they only drink water if reminded because they
refused lab work and all medications in the morning and refused the 4:00 a.m. Vital signs to be taken. do not feel thirsty as younger adults do and are not moving as much, so they do not feel thirsty.
impairment of substance
2- I: Assess the causes of non-adherence and who is in charge of the patient's care delivery to the brain PR: the patient was reminded to drink water.
Rationale: knowing the cause of refusal can facilitate how the nurse can intervene and manage because sometimes the cause can be solved. 6- I: Collaborate with the kitchen (after consulting with the patient's MD) to include fruits that have increased water
PR: the patient does not like needles and does not want to be poked, so he is not letting us start an IV on him. content, like oranges, melons, grapes, cucumbers, and watermelon, and decrease food high in sodium.
Management/Intervention: decrease in oxygen Rationale: some fruits can include high water content, which can help increase the patient's hydration.
and/or sugar in brain
3- I: Be firm about taking vital signs, lab work, and giving medications to improve the patient's health. PR: the patient had finished all his fruit plate for lunch.
tissue
permanent
Rationale: sometimes difficult patients can have these habits of manipulating and refusing for no reason, so it is essential to educate the patient, Irreversible brain
damage
Evaluation: At the end of the shift, the goal was not met AEB, the patient's Urine output was still concentrated and
be firm, and have strict, respectful boundaries. dark, and the patient did not finish the 700-1000ml plan set for him (he had 340ml only).
decreased Oxygen and
PR: VS were taken throughout the day, and antifungal powder was applied. glucose in the brain Dementia
4- I: Simplify complex care and involve the patient to make sure that information is easy to understand for the patient Modification:
If untreated Seizure -A temporary solution can be convincing the patient to allow us to start an IV on him to provide him with some IV
Rationale: The patient is hard of hearing, so one of the reasons for non-compliance can be not knowing what the nurse or the MD is saying to alteration on
fluids
him, which can increase the patient's frustration and non-compliance. neurotrasmission
Coma - round more frequently with the collaboration with the PCT, like every hour, to remind the patient about fluid intake
PR: simplifying care was involved when care was provided to the patient; I explained that I had to apply the antifungal powder to his groin and and have him drink it in front of us if possible.
armpit areas to help decrease the rash and redness. impaired cerebral Death - ask the patient about his water temperature preference; he might like it with extra ice, so he is not drinking as
metabolism much.
Patient education: - Include fruits for breakfast, lunch, and dinner instead of desserts high in sugar.
- collaborate with the kitchen to make smoothies for the patient.
5- I: Educate the patient about their diagnosis and be patient. neural and cellular
behaving out of character and -reassess the hydration status and I&O.
Rationale: The complexity of the information, the patient's cognitive limitation, and lack of access to resources can make information harder for dysfunction
act differently than their normal
the patient to understand, so providing printed form and using simplicity in explanation can help the patient's adherence and understanding of behavior baseline
their diagnosis.
lack of concentration
PR: I did not involve education about their diagnosis; neither did the nurse.
6- I: Educate the patient about the risks of not taking the medications and the benefits of taking their medication. confusion
Rationale: knowing the risks of noncompliance can increase the patient's awareness about the danger of not taking their medication. neurobehavioral and disorganized thinking
brain dysfunction
PR: The patient was not given education about risks and benefits on the day of care. cognitive symptoms
decreased
fatigue
mobility
Evaluation: at the end of the shift, the goal was partially met AEB patient allowed me to take his VS at (08:00-12:00-16:00), the patient agreed to furgetfulness
apply the antifungal powder but not the rest of his medications. The patient refused to do his lab work and refused to start an IV on him. Swollen legs (Edema
problem thinking in the right and left Risk for DVT
lower extremeties)
Modification: alteration of
-Involve the social worker or the patient's psychiatrist if available. consiousness
-Investigate more about whether the patient has someone close to him whom he would like to see (having a close friend or family member can Heparin 5000units/ml
Improve the patient's behavior and compliance with the medication regimen) under HIPPA guidelines. SQ q12hrs BID (pt
refused)
-Educate the patient about their diagnosis and the risks of not taking their medications.
Mini NANDA #3: Depression R/T Loneliness, mental illness, hearing problem,
mood swings, medication side effects when taken AEB, the patient does not
MINI NANDA #1: Impaired skin integrity R/T poor hygiene, altered mental have family, kids, or friends (he was kicked out from home at a younger age),
auditory hallucinations, labile mood, HOH and does not have a hearing aid, love
status, self-care deficit, and self-neglect, fungal infection AEB rash on the
Mini NANDA #2: risk for DVT R/T patient's spending time alone, the patient takes Quetiapine/Seroquel
bilateral groin, pt has right groin stitches, very malodorous moist and
Interventions:
bleeding skin tag, rash and redness around armpits. Tinea Cruris spread on immobility, Obesity, comorbidities, Pt has non-
armpits, groin, and left abdomen. pitting edema in his RLE and LLR, the patient is 1- The patient is HOH; being unable to hear what people are saying can increase
255lbs and barely moves, the patient has BP of the risk of depression, so it is important to use small, short words when speaking
Interventions:
1- Tinea cruris infection can be found around the groin area a lot because 152/89, hyperlipidemia causes an increased risk to the patient.
References 2- Collaborate with the PT, OT, and PCT to keep the patient busy, exercising and
the site is generally moist in males, so it is essential to maintain good of clot formation.
walking to decrease their time spent alone.
Boss, J. B., & Huether, S. E. (2019). Alterations in cognitive systems, cerebral hemodynamics, and motor function. In McCance & Huether’s Pathophysiology: the hygiene and keep the area dry and clean. Interventions:
1- Apply SED to help decrease the swelling and prevent 3- use therapeutic communication and give a lot of support, allowing the patient to
2- Apply topical antifungal medication, Clotrimazole Betamethasone
biologic basis for disease in adults and children (pp. 517–518). Elsevier. clot formation in the lower extremities. speak, ask open-ended questions, ask the patient what they enjoy doing, and try
(Lotrisone) Topical BID on armpits and groin twice a day, and apply the
2- Educate the patient about taking the prescribed to offer it at the hospital if possible.
Harding, M. M., Kwong, J., & Hagler, D. (2020). Lewis’s medical-surgical nursing: assessment and management of clinical problems. Elsevier. powder when the area is moist. Heparin SQ 5000 units/ml to prevent clot formation. 4- find out if the patient has any spiritual beliefs and offer the religious support that
3- Educate the patient to clean the area after voiding, keep the site dry, 3- Educate the patient to do AROM exercises in bed
Swearingen, P. L. (2016). All-in-one nursing care planning resource: Medical-surgical, pediatric, maternity, and psychiatric-mental health. Elsevier.
never wear tight clothes, and keep legs separated when in bed. the hospital has.
You might also like
- ITR DentalDocument3 pagesITR Dentalnelmark.pepitoNo ratings yet
- Gad Plan 2018Document21 pagesGad Plan 2018Vilma Magno MorgadoNo ratings yet
- 5.1 Combi Project PlanDocument3 pages5.1 Combi Project PlanmartinNo ratings yet
- Pedia Nursing DocuDocument4 pagesPedia Nursing DocuMelanie SalidoNo ratings yet
- Drug Study Form Drug Name Classification Mechanism of Action Side Effects/ Adverse Effects Nursing Considerations/ Patient and Family TeachingDocument2 pagesDrug Study Form Drug Name Classification Mechanism of Action Side Effects/ Adverse Effects Nursing Considerations/ Patient and Family TeachingXerxes DejitoNo ratings yet
- BH - Example Poster 2Document1 pageBH - Example Poster 2wanzhen0527No ratings yet
- McCammon Focused Assessment #1Document2 pagesMcCammon Focused Assessment #1Ashley Constant McCammonNo ratings yet
- Mar April 2022Document1,425 pagesMar April 2022Shai SdmpNo ratings yet
- Rekap Berkala 23Document1 pageRekap Berkala 23Pat BelNo ratings yet
- Drug Study Form Drug Name Classification Mechanism of Action Side Effects/ Adverse Effects Nursing Considerations/ Patient and Family TeachingDocument2 pagesDrug Study Form Drug Name Classification Mechanism of Action Side Effects/ Adverse Effects Nursing Considerations/ Patient and Family TeachingXerxes DejitoNo ratings yet
- Terbutaline SulfateDocument1 pageTerbutaline SulfateIvanne Hisoler100% (2)
- Cot 2012 English Canada v02.02 1 0Document410 pagesCot 2012 English Canada v02.02 1 0MDBNo ratings yet
- Concept Map - Surgical GroupDocument25 pagesConcept Map - Surgical GroupIan ChristianNo ratings yet
- Pathophysiology DM1Document5 pagesPathophysiology DM1Andree GalloNo ratings yet
- Tuberculosis Provided Services: Male 20 Y/o and Above Female 20 Y/o and AboveDocument1 pageTuberculosis Provided Services: Male 20 Y/o and Above Female 20 Y/o and Abovehazel pernadaNo ratings yet
- Clinical DepressionDocument7 pagesClinical DepressionEdward XiamNo ratings yet
- Surrenderer Process Flow ChartDocument1 pageSurrenderer Process Flow ChartPingotMagangaNo ratings yet
- September 19, 2021-Community Engagement and Serbisyong TamaDocument2 pagesSeptember 19, 2021-Community Engagement and Serbisyong TamaJudy Ann Jude AdornaNo ratings yet
- ContraceptionDocument1 pageContraceptionSibel ErtuğrulNo ratings yet
- Galang Ds1Document1 pageGalang Ds1galang.andrea.mNo ratings yet
- Encephalopathy HepaticumDocument2 pagesEncephalopathy Hepaticumtitis dwi tantiNo ratings yet
- Primario Desconocido NCCN Head-And-neck 2020Document8 pagesPrimario Desconocido NCCN Head-And-neck 2020d.ayala1006No ratings yet
- DRUG STUDY MetronidazoleDocument3 pagesDRUG STUDY MetronidazoleCelline Isabelle ReyesNo ratings yet
- Cot 2012Document410 pagesCot 2012AnonymousNo ratings yet
- Drug Study - LithiumDocument3 pagesDrug Study - LithiumPRINCESS KOBAYASHINo ratings yet
- Assessment and Concept Map Care Plan: Elizabeth RouxDocument6 pagesAssessment and Concept Map Care Plan: Elizabeth Rouxapi-507304905No ratings yet
- IM Peptic Ulcer Concept Map 2.0Document1 pageIM Peptic Ulcer Concept Map 2.0TrisNo ratings yet
- 0.5 ML Repeat at 4-8weeks After First Dose and at 6-12 Months After Second DoseDocument2 pages0.5 ML Repeat at 4-8weeks After First Dose and at 6-12 Months After Second DoseLenneth Ann M. LozadaNo ratings yet
- 5.yuva Clinic - (AFHC) Reporting FormatsDocument11 pages5.yuva Clinic - (AFHC) Reporting Formats0700139993No ratings yet
- Mahogany ST., Rabe Subd. Tagum City: Tagum Doctors College, IncDocument1 pageMahogany ST., Rabe Subd. Tagum City: Tagum Doctors College, IncJanella Kyle ParejaNo ratings yet
- Team DR Acharya Inpatient ListDocument7 pagesTeam DR Acharya Inpatient ListMumtaNo ratings yet
- The Oligopoly in Business: Download FreeDocument5 pagesThe Oligopoly in Business: Download FreeMark Raniel AntazoNo ratings yet
- Health Teaching PlanDocument8 pagesHealth Teaching Planrain َNo ratings yet
- WSPS Mental Health Infographics PosterDocument1 pageWSPS Mental Health Infographics PosterIain GidleyNo ratings yet
- Smoke Buddy!: By: Subhojit Dhar Vishesh Soni Sujal Bansal Uday Bhaskar Gajavalli Tejaditya SankranthiDocument14 pagesSmoke Buddy!: By: Subhojit Dhar Vishesh Soni Sujal Bansal Uday Bhaskar Gajavalli Tejaditya SankranthiVishesh SoniNo ratings yet
- Electrical Burn - IE - Nayve, Rarugal, AzaulaDocument18 pagesElectrical Burn - IE - Nayve, Rarugal, AzaulaFrnz RiveraNo ratings yet
- Creating Shared Value Sustainability Report 2023 enDocument89 pagesCreating Shared Value Sustainability Report 2023 enNajib SaadNo ratings yet
- Drug Study Form Drug Name Classification Mechanism of Action Side Effects/ Adverse Effects Nursing Considerations/ Patient and Family TeachingDocument2 pagesDrug Study Form Drug Name Classification Mechanism of Action Side Effects/ Adverse Effects Nursing Considerations/ Patient and Family TeachingXerxes DejitoNo ratings yet
- Omeprazol Brand - Generi C Name Action Contraindica Tion Indication S Adverse Reaction Prioritized Nursing Consideration SDocument5 pagesOmeprazol Brand - Generi C Name Action Contraindica Tion Indication S Adverse Reaction Prioritized Nursing Consideration SJM RomiasNo ratings yet
- Generic Name Dosage Action Indication Contraindication Side Effects Nursing ConsiderationsDocument4 pagesGeneric Name Dosage Action Indication Contraindication Side Effects Nursing ConsiderationsMaria Theszha ANo ratings yet
- Https - WWW - Ncbi - NLM - Nih - Gov PMC Articles PMC5396830Document14 pagesHttps - WWW - Ncbi - NLM - Nih - Gov PMC Articles PMC5396830dori sanchezNo ratings yet
- Drugs For Amebiasis: Vaginalis), GiardiasisDocument6 pagesDrugs For Amebiasis: Vaginalis), GiardiasisCarla C. FernandezNo ratings yet
- Shoulder Pain v2Document8 pagesShoulder Pain v2DindaNo ratings yet
- Davao Doctors College Nursing Program Drug Study: General Malvar St.,DavaocityDocument3 pagesDavao Doctors College Nursing Program Drug Study: General Malvar St.,DavaocityJerremy LuqueNo ratings yet
- Annual-Barangay-Youth-Investment-Program-Monitorig - Form 2021Document8 pagesAnnual-Barangay-Youth-Investment-Program-Monitorig - Form 2021J J. LamitaNo ratings yet
- Quartenary Ammonium Compound - OdsDocument1 pageQuartenary Ammonium Compound - OdsFafnirNo ratings yet
- Sodium and PotassiumDocument1 pageSodium and Potassiumjoan1alejo1espirituNo ratings yet
- Diane Pills Drug StudyDocument4 pagesDiane Pills Drug StudyDawn EncarnacionNo ratings yet
- FIX Fishbone Kesling 1Document5 pagesFIX Fishbone Kesling 1hotparsaulianNo ratings yet
- Drugs Used For Hyperthyroidism - Sunga, Saara Paula BiancaDocument6 pagesDrugs Used For Hyperthyroidism - Sunga, Saara Paula BiancaBea SungaNo ratings yet
- Case Study Older Brand (24 November 2020)Document8 pagesCase Study Older Brand (24 November 2020)IMBOOST INDONESIANo ratings yet
- Ie Dementia AlzheimersdiseaseDocument14 pagesIe Dementia AlzheimersdiseaseSusana SeradillaNo ratings yet
- Cerebral Palsy - A Help Guide. Authors Nadire Berker and Selim Yalin 2003Document145 pagesCerebral Palsy - A Help Guide. Authors Nadire Berker and Selim Yalin 2003Kakha MouravidzeNo ratings yet
- Agency Treatment Service (S) Residential # Mat Slots # Detox Beds # Residential BedsDocument3 pagesAgency Treatment Service (S) Residential # Mat Slots # Detox Beds # Residential BedsNEWS CENTER Maine100% (1)
- Drug StudyDocument4 pagesDrug StudyBobot Julius Oropeza100% (2)
- 2Nd Year First Bimonthly Exam Schedule: SubjectDocument2 pages2Nd Year First Bimonthly Exam Schedule: SubjectMicah Ley OlposNo ratings yet
- Ferrous Sulfate Drug StudyDocument1 pageFerrous Sulfate Drug StudyAgeededin HartNo ratings yet
- AICTE CorporateBestPracticesDocument13 pagesAICTE CorporateBestPracticesramar MNo ratings yet
- Organic Food: Why?: A - The Main Reason For The Popularity of Organic FoodDocument2 pagesOrganic Food: Why?: A - The Main Reason For The Popularity of Organic FoodMy Linh HuynhNo ratings yet
- BSC 2085 Anatomy and Physiology NCLEX Final Exam Predictor Study Guide (Verified and Correct Answers, 200 Questions Secure Highscore) Latest 2021Document131 pagesBSC 2085 Anatomy and Physiology NCLEX Final Exam Predictor Study Guide (Verified and Correct Answers, 200 Questions Secure Highscore) Latest 2021abbieNo ratings yet
- Dissertation On BreastfeedingDocument8 pagesDissertation On BreastfeedingNeedHelpWriteMyPaperVirginiaBeach100% (1)
- General Psychology - PDF - Psychology - MindDocument57 pagesGeneral Psychology - PDF - Psychology - MindAishleyNo ratings yet
- PSDS Graduation SpeechDocument2 pagesPSDS Graduation SpeechRobert Kier Tanquerido TomaroNo ratings yet
- Ielts GT Writing Task 2Document20 pagesIelts GT Writing Task 2Raga SownthariyaNo ratings yet
- The Consent Checklist: Meg-John BarkerDocument16 pagesThe Consent Checklist: Meg-John BarkerKayla Hook100% (1)
- Nonfiction Reading Test Reading: Directions: Read The Following Passage and Answer The Questions That Follow. Refer ToDocument3 pagesNonfiction Reading Test Reading: Directions: Read The Following Passage and Answer The Questions That Follow. Refer ToturtlelxNo ratings yet
- Effectiveness of Stabilization Exercises and Conventional Physiotherapy in Subjects With Knee OsteoarthritisDocument8 pagesEffectiveness of Stabilization Exercises and Conventional Physiotherapy in Subjects With Knee OsteoarthritisNovella FauduNo ratings yet
- RecommendationDocument25 pagesRecommendationCT MacaraegNo ratings yet
- MCT - Patnaik Grading (1984)Document6 pagesMCT - Patnaik Grading (1984)Yurany RodriguezNo ratings yet
- Roy, Neuman, King ReviewerDocument2 pagesRoy, Neuman, King ReviewerJustine Marie AguilarNo ratings yet
- Application of The Repetitions in Reserve Based.10Document8 pagesApplication of The Repetitions in Reserve Based.10Nicolás BastarricaNo ratings yet
- Textbook Moss Adams Heart Disease in Infants Children and Adolescents Including The Fetus and Young Adult Robert E Shaddy Ebook All Chapter PDFDocument54 pagesTextbook Moss Adams Heart Disease in Infants Children and Adolescents Including The Fetus and Young Adult Robert E Shaddy Ebook All Chapter PDFtimothy.caldwell636100% (10)
- Bonus Utilization of Fascination in Therapeutic PracticesDocument8 pagesBonus Utilization of Fascination in Therapeutic PracticesGrosseQueueNo ratings yet
- Astro Diagnosis VirgoDocument42 pagesAstro Diagnosis VirgoOvn Murthy100% (1)
- Safety Data Sheet: Page 1 of 6 Msds For #01037 - Testor Enamel PaintDocument6 pagesSafety Data Sheet: Page 1 of 6 Msds For #01037 - Testor Enamel PaintJake VergaraNo ratings yet
- Latest Resume BuelaDocument3 pagesLatest Resume BuelaCleeve Humprey BuelaNo ratings yet
- PublishedVersion COR2-17014719Document16 pagesPublishedVersion COR2-17014719HandayaniNo ratings yet
- MindMed Announces Positive Topline Results From Phase 2b Trial of MM-120 in Generalized Anxiety DisorderDocument5 pagesMindMed Announces Positive Topline Results From Phase 2b Trial of MM-120 in Generalized Anxiety DisorderWKYC.comNo ratings yet
- RA-Vocabulary (U1-L1-family Relation and Friendship)Document2 pagesRA-Vocabulary (U1-L1-family Relation and Friendship)Kiên ĐinhNo ratings yet
- 402 OkeyDocument21 pages402 OkeyrafabarajimNo ratings yet
- BSCI MANUAL 2.0 EN Annex 7 BSCI Buyers Checklist PDFDocument2 pagesBSCI MANUAL 2.0 EN Annex 7 BSCI Buyers Checklist PDFAsafo BoualouchNo ratings yet
- Psychosocial ActivitiesDocument18 pagesPsychosocial ActivitiesRyan Q. Blanco50% (2)
- Brent D Goff vs. Victoria J Goff 08-3-03291-3 PDFDocument217 pagesBrent D Goff vs. Victoria J Goff 08-3-03291-3 PDFEric YoungNo ratings yet
- P90X Nutrition Guide 12-29-091Document12 pagesP90X Nutrition Guide 12-29-091Primerra TimmonsNo ratings yet
- Luce Penney - Resume - January 2024 - UpdatedDocument6 pagesLuce Penney - Resume - January 2024 - Updatedhemanth vNo ratings yet
- Medical Doctors Practice Regarding The Upper Gastrointestinal Bleeding Management at Mohammed Salih Edris Bleeding CenterDocument7 pagesMedical Doctors Practice Regarding The Upper Gastrointestinal Bleeding Management at Mohammed Salih Edris Bleeding CenterInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Health Assessment ToolDocument3 pagesHealth Assessment ToolGail GenturalezNo ratings yet
- Aided AAC Systems Among Individuals With Hearing LossDocument16 pagesAided AAC Systems Among Individuals With Hearing LossBayazid AhamedNo ratings yet