Professional Documents
Culture Documents
Micro Prefinal
Micro Prefinal
Uploaded by
farahjundan0 ratings0% found this document useful (0 votes)
9 views5 pagesStaphylococci are common bacteria that can cause opportunistic infections. While usually considered contaminants, they may cause infections in immunocompromised hosts. Staphylococcus aureus is a notorious pathogen, while S. saprophyticus commonly causes honeymoon cystitis. Species can be identified through tests of lysostaphin sensitivity, furazolidone sensitivity, carbohydrate utilization, and bacitracin sensitivity. Staphylococci are gram-positive cocci that can be distinguished from similar micrococci through coagulase testing.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentStaphylococci are common bacteria that can cause opportunistic infections. While usually considered contaminants, they may cause infections in immunocompromised hosts. Staphylococcus aureus is a notorious pathogen, while S. saprophyticus commonly causes honeymoon cystitis. Species can be identified through tests of lysostaphin sensitivity, furazolidone sensitivity, carbohydrate utilization, and bacitracin sensitivity. Staphylococci are gram-positive cocci that can be distinguished from similar micrococci through coagulase testing.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views5 pagesMicro Prefinal
Micro Prefinal
Uploaded by
farahjundanStaphylococci are common bacteria that can cause opportunistic infections. While usually considered contaminants, they may cause infections in immunocompromised hosts. Staphylococcus aureus is a notorious pathogen, while S. saprophyticus commonly causes honeymoon cystitis. Species can be identified through tests of lysostaphin sensitivity, furazolidone sensitivity, carbohydrate utilization, and bacitracin sensitivity. Staphylococci are gram-positive cocci that can be distinguished from similar micrococci through coagulase testing.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
Clin.
Usually considered Bacteria of
Microbiology 1 Significance contaminants of
clinical specimen,
this genus are
of primary
Undan, Farah Jayne A.
rarely implicated clinical
INTRODUCTION as cause of significance.
infections. May S. aureus is a
- Family: Micrococceae (Consist of gram positive cause notorious
cocci, arranged in tetrads (Under the microscope), opportunistic in an pathogen. S.
clusters) immunocompromi saprophyticus
- Genus: Staphylococcus sed host. cause
- Term “staphylococcus derived from Greek: honeymoon
o Staphyle= bunch of grapes (Arrangement) cyctisis
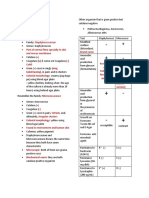
Lysostaphin Not lysed with Lysed with
o Kokkos= berry, meaning bacteria occurring
Sensitivity Test lysostaphin lysostaphin
in the grapelike clusters or berry (resistant) (Sensitive)
- They are common to be isolated in a laboratory Furazolidone Resistant to Susceptible to
- Infection that cause by this genus, such as S. Aureus, Sensitivity test antibiotic antibiotic
epidermidis, saprophyticus, lugdunensis, hemolyticus furazolidone furazolidone
species that are commonly causing human infection. Microdase test Positive Negative
- The name of the different species is based on the Oxygen Grow aerobically Facultative
morphological structure. Requirements (Obligate anaerobe (Can
- anaerobe) use either
aerobic
HISTORY respiration
and/or
- Robert Koch (1878)
fermentation
o First to see staphylococci in pus specimen depending on
- Louis Pasteur (1880) the availability
o First to cultivate on liquid medium of oxygen,
- Sir Alexander Ongston (1881) does not solely
o Named the bacteria as “staphylococcus) depend on
- Von Recklinghausen (1871) aerobic
o First observed in pus respiration for
growth)
- Rosenbach (1884)
Carbohydrate Utilize sugars Fermentative
o Named S. aureus (golden yellow colonies), S.
utilization oxidatively Fermentation.
albus (white colonies) (Glucose, sucrose, They ferment
- Passet (1885) & lactose) or not at carbohydrates.
o S. citreus (lemon yellow colonies) all in the O/F test. Metablic
Utilized sugar waste will
TAXONOMY oxidatively- depend.
- Staphylococcus cocci are gram positive cocci and Through oxidation
classified into 2 families (as per 1986 edn. Of Bacitracin Susceptible to 0.04 Resistant to
Sensitivity Test U of bacitracin 0.04 U of
Bergey’s Manual Systemic Bacteriology):
bacitracin
o Micrococcaceae (GPC, catalase positive) –
- Testing refers to the antibiotic that they are resistant
have 4 genera or susceptible.
Planococcus -
Micrococcus
Stomatococcus STAPHYLOCOCCI
Staphylococcus
- Resembles some of the some member of the
Micrococcus and
micrococacceae family. Specifically the genus
staphylococcus can cause
micrococcus
human infection
- Micrococci- catalase producing, coagulase negative,
o Steptococcaceae (GPC, catalase negative)
gram positive cocci that are usually found in the
- Newer edition staphylococci are: environment and as a member of indigenous skin
o Phylum: Firmicutes microbiota.
o Genus I - Often recovered with staphylococci.
o Family V: Staphylococcaceae - Differentiate micrococci and staphylococci through
o Order I: Bacillales coagulase test
o Class III: Bacilli - Stahylococci produce yellow pigment
- Catalase-producing and facultatively anaerobe except
DIFFERENCE BETWEEN STAPHYLOCOCCUS AND
for S. saccharolyticus, which is an obligate
MICROCOCCUS
anaerobe.
Characteristics Micrococcus Staphylococc - Coagulase positive because of the enzyme called
Tests us staphylocoagulase (can be present to other
Morphology Large gram- Gram positive staphylococci species)
positive cocci, cocci, - Non-motile, non-spore forming glucose fermenters
usually arrange in sometimes in - Normal inhabitants of the skin, mucous membrane
tetrads or in pair. pairs and in and intestines
short chains. - Staphylococci associated with human infections are
colonizers of various skin and mucosal surfaces
- Spherical cells that appear in clusters, or sometimes part of all lgG molecules except lgG3. It is
singly not an antigen-antibody specific reaction.
- Culture: BAP-colonies (4mm – 8mm) appear - Virulence factors
creamy, white or light gold, or “Butterly-looking” o Enterotoxins
while other species may have gray colonies; some o Toxic Shock Syndrome Toxin-1
species (S. aureus) may be Beta-hemolytic like S. Have the special p
aureus. o Exfloitive Toxin
- Current Classification To some age bracket they are very
o 32 species common, and be able to exhibit
o 15 subspecies disease and infection
o Coagulase positive -> Staphylococcus aureus o Cytolic Toxins
(Considered to be a notorious agent under o Enzymes
staphylococci that create infection to human
that may be life threatening) o Protein A
o Coagulase negative - Culture Characteristics
Staph epidermidis o Grow on ordinary media
Known to cause various o Manifesting diff. characteristic and colors of
acquired or nosocomial the colonies as well
infection o Temp 10-42°C. Optimum is 37°C
Staph hemolyticus o pH range 7.4 – 7.6
CAN ALSO BE o Aerobes, some strain of S. aureus are
RECOVERED IN THE facultative aerobes
WOUNDS, can cause o Facultative anerobes
infection in the wound
o Nutrient agar
Staph saprophyticus
Mannitol salt agar- Large (2-3mm
Mainly associated with UTI,
in diameter), circular, smooth, shiny,
isolated in the urine sample
opaque & easily emulsifiable colonies
of adolescent girls/young
Brain heart infusion agar- Yellow
women
pigment w/c does not diffuse into
Staph ludgunensis
medium
Commensal flora- benifiting from each Pigment carotene like lipoprotein
other Pigment production best at 22°C or
when glycerol monoacetate/milk is
Staph hominis incorporated into medium.
Can be found in a area that Glycerol, monoacetate and milk
can cause infection and is Blood agar- Beta-Hemolysis is
also rare observed.
Can cause infection in the Tryptic soy agar- circular, convex,
sculp and entire margin.
Staph Auricularis- ear infection o Nutrient slope
Staph capitis Oil paint appearance
The species Staphylococcus aureus o Blood sugar
Marked hemolysis on sheep blood
- Most notorious, responsible for numerous infection. agar
Ranging from mild to life threatening infection. 20-25% co2
- Infection that cause by aureus can be categorized Rabbit/sheep blood
suppurative or toxin mediated disease. o Mac Conkey Agar
- Toxin, these are substances which are being secreted Pink colonies due to lactose
by the bacterial cell fermentation
- Can be recovered in any clinical specimen If there is no pink colors= Non-
- Important cause of nosocomial infection lactose fermenters
- Continous to increase in producing community o Liquid media (If S. aureus)
acquired infection as well as drug resistance. Uniform turbidity in all area of the
- Morphology broth medium
o Gram-postive, spherical cells, mostly arrange o Selective medium
in irregular grape like clusters. Salt milk agar
o Polysaccharide capsule is only rarely found If the S. aureus in diff. media,
on cells. ant organisms can grow in
o The peptidoglycan layer us the major that media
structural components of the cell wall. It is Salt broth agar
important in the pathogenesis of Ludlam’s medium (Lithium
staphylococcal infections. Other important chloride, tellurite)
component of cell wall is teichoic acid. - Biochemical Reactions
o Protein A is the major protein component of - Reagent -> Result
the cell wall. It is located on the cell surface o Catalase -> Positive
but is also released into the culture medium o Indole -> Negative
during the cell growth. A unique property of o MR -> Positive
protein A. is its ability to bind to the Fc
o VP -> Positive Is an aggregation of infected
o Urease -> Positive furuncles. May form large abscesses.
o Nitrate reduction -> Positive It is a large area of redness, swelling
o Mannitol fermentation -> Postive and pain, punctuated by several sites
o Phosphatase production -> Positive of drainage pus.
o Impetigo- is a superficial cutaneous
RELATED INFECTIONS AND DISEASE infection that is commonly seen in children
and characterized by crusty lesions and
- Toxin-induced cases
vesicles surrounded by a red border.
o Scalded skin syndrome (SSS)- is an
A very superficial skin infection
extensive exfoliative dermatitis that occurs
common in children usually produces
primarily in newborns and previously
blisters or sores on the face, neck,
healthy children
hands and diaper area.
Toxin responsible for SSS- Epidermic
It is characterized by watery blisters,
o Toxic shock syndrome (TSS)- a rare but
which becomes putules and then
potentially fatal, multi-system disease that
honey coloured crust
is characterized by a sudden onset of fever,
o Purulent abscess
chills, vomiting, diarrhea, muscle aches, and
- Osteomyelitis (Deep Infection)
rashes, and which rapidly progresses to
o Inflammation of bone
hypertension and shock.
o Bacteria can get to the bone via bloodstream
o Sometimes cause death
and following an injury
o Example:
o Clinical features: pain, swelling, deformity,
Preformed, heat-resistant enterotoxin
defective healing, in some case pus flow
mediates staphylococcal food
o Diagnosis: X-ray, MRI, bone aspirates
poisoning (symptoms in 2-6 hours):
usually self-limiting) - Septic arthritis (children)
Exfoliative toxins A and B results in - Food poisoning
staphylococcal scalded skin ENZYME AND TOXINS PRODUCED BY STAPH.
syndrome; usually in infants and AUREUS
neonates
Can cause cutaneous erythema the 1. Coagulase
profiuos peeling o It coagulates the fibrinogen in the plasma.
Occur in hands and feet then spread Promotes the formation of a fibrin layer
to other parts around the staphylococci abscess thereby
10 days of medication with protecting the bacteria from phagocytosis.
antibiotics o There are two types:
Cell-bound coagulase or clumping
factor – is bound to the cell wall and
- Bacteremia and sepsis clots human, rabbit, or pig plasma by
- Urinary tract infection directly converting fibrinogen into
- Acutes bacterial endocarditis fibrin.
o Inflammation of the outer pusod Unbound or free coagulase – is an
o Enlargement of the heart extracellular enzyme that is not
- Cutaneous infections bound to the cell wall and causes clot
o Previous damage or injury formation when bacterial cells are
incubated with plasma.
o Folliculitis- mild inflammation of the hair
2. Hyaluronidase (Spreading-factor enzyme)
follicle or subcutaneous gland
o it enhances invasion and survival in the
A small red bump or pimple develops
tissue. Breaks down the hyaluronic acid that
at the infection sites of the hair
is present in the intracellular ground
follicle.
substances of connective tissues, resulting in
Sty: a sty is a folliculitis affecting
the spread of bacteria.
one or more hair follicles on the edge
3. Staphylokinase (Fibrinolysin)
of the upper and lower eyelid
o Causes fibrinolytic activities by dissolving
o Furuncles- are large raised superficial fibrin clots.
4. Lipase (Fat-splitting enzyme)
abscesses which can be an extension of
o Produced by both coagulase-positive and
folliculitis. Commonly known as boils.
Deep seated infection, originating coagulase-negative staphylococci. Essential
from folliculitis, (if infection extends for bacterial survival in sebaceous areas of the
from follicle to neighbor tissue) body and important in the formation of
Causes redness, swelling and severe furuncles, carbuncles and boils.
pain 5. Deoxyribonulease (Dnase) and phosphatase
Common found on the neck, armpit o Lowers the viscosity of exudates giving the
and groin regions. pathogen more mobility and destroys DNA.
Superficial abcesses 6. β- lactamase
o Carbuncles- develop from multiple - Breaks down penicillin and other β-lactam drugs.
furuncles which my advance into the More than 90% of clinical staphylococci isolates
deeper tissues and cause fever and chills are penicillin-resistant as a result of enzyme
leading to systemic infections. production.
7. Emterotoxin (Heat-stable) Slide method- used to screen catalase
o Acts as neurotoxins that stimulate vomiting positive colonies, detects cell bound
through the vagus nerve, produced by the coagulase or clumping factor.
majority of Staph.aureus isolates. Stable to (+) result : clot or coagulum
heating at 100 degree centigrade for 30 formation within 30 seconds.
minutes. Other slide coagulase Staph.
o Resistant to hydrolysis by gastric and jejunal are Staph. lugdunensis and
enzymes. Staph. schleiferi
o Examples of enterotoxins A,B,C1,C2,D,E and Tube method- considered sensitive
G to J but definitive method, detects
o A,B and D are responsible for food poisoning. extracellular or free coagulase
8. Leukocidin/Panton- Valentine Leukocidin (+) result : clot or coagulum
(Cytolytic toxin) formation after one to four
o It attacks and kills white blood cells, pore hours of incubation.
forming exotoxin that suppresses Other tube coagulase Staph.
phagocytosis and responsible for necrotizing are:
skin and soft tissue infections. o Staph.hyicus,
9. Hemolysin o Staph.intermedius,
o Causes anemia and make iron available for S.delphini
microbial growth. o S. schleiferi
o There are four (4) types of hemolysin: subsp.coagulans
Alpha-hemolysin (α) – predominany 2. Mannitol Fermentation Test
lysine that is produced by o Used to differentiate the pathogenic staph.
S.aureus.Destroys red blood cells, From non-pathogenic ones.
platelets, and macrophages, and o Culture medium is mannitol salt agar and pH
causes severe tissue damage. indicator is phenol red.
Beta- hemolysin (β) – destroys o (+) result: Yellow-colored S. aureus colonies
spingomycelin and RBC around 3. Tellurite glycine agar
nerves.It has enhanced haemolytic o This results in jet black colonies of S.aureus
activity on incubation at 35 degree 4. Polymyxin sensitivity tests
centigrade. o S.aureus is resistant to this test
Gamma- hemolysin ( γ) – less toxic 5. Voges-Proskauer (VP) test
than α and β –lysins, produced by all o Differentiates S. aureus from S. intermedius
S.aureus strains that cause RBC o (+) result: Pink color
injury in culture and produces
6. Deoxyribonuclease (Dnase) test
edematous lesions.
o Used to identify pathogenic species of
Delta-hemolysin (δ) – destroys RBC
staphylococci that produces Dnase.
and is associated with the Panton-
o Culture medium: DNA- methyl green agar
Valentine leukocidin.
o (+) result: Clear/ colorless zone around the
10. Exfoliatin serotypes A and B ( Superantigens)/
Epidermolytic toxins A and B test organism
o Is a serin protease that divides the METHICILLIN-RESISTANT STAPHYLOCOCCUS
intracellular bridges of the epidermidis and AUREUS (MRSA)
causes extensive sloughing of the epidermis
to produce a burn-like effect on the patient. - Resistant to antibiotics such as methicillin, nafcillin,
o Destroys the stratum granulosum and causes and oxacillin.
scalded-skin syndrome (SSS) or Ritter’s - Can be acquired after a prolonged stay in the hospital,
disease. close contact with individuals who are carriers of the
11. Toxic shock syndrome toxin 1 (TSST-1)/ organism, after-effects of a broad spectrum of
Enterotoxin F/Pyogenic exotoxin antibiotics treatments, and exposure to nasal
o A chromosomal-mediated toxin and causes secretions.
almost all cases of menstruation-associated - Can be controlled by proper isolation of the organism,
TSS rapid identification of the bacteria, hand hygiene,
o Stimulates the production of a large amount treatment of sources, and most importantly, a strict
compliance to infection control programs.
of cytokines that are responsible for the
- Three (3) types of MRSA:
symptoms.
1. Hospital-acquired (HA) MRSA
12. Protein A
2. Community-acquired (CA) MRSA
o Immunologically active substance that is
3. Health care associated community-Onset
found in the cell wall.
(HACO) MRSA
DIFFERENTIAL TEST FOR STAPH. AUREUS o (+) Chromogenic test: change in color of
MRSA colonies within 24-48 hours using
1. Coagulase Tests CHROM agar against colorless colonies of
o Best single criterion of pathogenicity of non- MRSA
Staph. aureus - Reagent: Rabbit plasma
o Anticoagulant: Ethylene diaminetetra-acetic COAGULASE NEGATIVE STAPHYLOCOCCUS
acid (EDTA) (CoNS)
o Two methods that can be used:
- S. epidermidis & S. saprophyticus
o They are coagulase-negative staphylococci o CHROM agar is a selective and differential
o Do not produce exotoxins medium for the isolation of MRSA
o Thus, they do not cause food poisoning or o Staphylococci grow easily in routine culture
toxic shot syndrome. media
- S. epidermidis o CoNS recovered from sterile sites and from
o Part of the normal flora if the skin and sites associated with indwelling devices
mucous membrane. should be considered potential pathogens.
o Cause of hospital-acquired infections o A low colony count for S. saprophyticus urine
o It is involved in indwelling catheters, culture is considered significant.
prosthetic materials, shunts, and surgery. 3. Catalase test – a heme enzyme that catalyzes the
o It is common of prosthetic heart valve decomposition of H2O2 to water and oxygen.
endocarditis o Differentiates staphylococci (+) from
o It also cause nosocomial bacteremia; sepsis in streptococci (-)
neonates peritonitis in patients with renal o Reagent is 3% H2O2 ; (+) presence of bubble
failure; cerebrospinal fluid shunt infections formation or effervescence.
o Often multiple antibiotic resistance- - 4. Coagulase test
methicilin o Reagent: Rabbit plasma ; (+) Clot or
- S. saprophyticus coagulum formation
o Commonly isolated from animals and their 5. Mannitol fermentation test
carcasses. o +) Yellow halo around colonies
o Coagulase and phosphatase – ve, urease & 6. Pyrrolidonyl arylamide (PYR) test
lipase +ve o Differentiates coagulase-positive
o S. saprophyticus is resistant to the antibiotic staphylococci by slide method. (+) Cherry
novobiocin, a characteristics used in lab to red; (-) No color change
distinguish it from S. epidermidis 7. Voges-Proskauer (VP) test
o Infections are almost always community o Differentiate staphylococci by tube method.
acquired. (+) Deep pink
o It causes mainly UTI, particularly in sexually 8. B-lactamase test
active young women. a. Cephalosporinase test – most useful and
o It is the second most common cause of UTI, widely used B-lactamase test
after E. coli in young women accounting for b. Acidimetric method
10-2-% c. Iodometric method
o Quinolones are commonly used in treatment 9. Antimicrobial testing
of S. saprophyticus UTI. o Drugs: Methicillin, oxacillin, cloxacillin and
- Staphylococcus lugdunensis dicloxacillin
o It is CoNS by tube method o Culture media: Vancomycin agar screen plate,
o Can be confused with S.aureus if slide Oxacillin-screen plate,Cefoxitin disk
diffusion, double-disk diffusion test
coagulase method is performed
10. Latex agglutination test
o More aggressive than the other CoNS in
o Used in detecting the clumping factor and
terms of infectivity
protein A.
o Contains the mecA gene that codes for
11. Molecular test
oxacillin resistance
o Used in identification of the mecA gene and
o Related infections include infective
gold standard for MRSA detection.
endocarditis, meningitis, septicaemia, UTI,
and skin and soft tissue infections. Streptococcus
o Novobiocin susceptible CoNS species are : S.
epidermidis, S.capitis, S.haemolyticus, - Species play an important role in the production of
S.hominis, S.lugdunensis, S.saccharolyticus diseases and infection
and S.warneri - There are 17 species in this genera that are catalase
o Novobiocin resistant CoNS species are: negative, gram positive cocci
- Is a non-catalase producers organism
S.saprophyticus, S.cohnii, S.kloosii and
- Streptococcus species
S.xylosus
o Streptococcus
LABORATORY DIAGNOSIS FOR STAPHYLOCOCCI o Aerococcus
o Lactococcus
- Specimens: Aspirated secretions (best sample),
purulent exudates, and joint fluids o Leukonostocs
1. Gram stain o Pediococcus
2. Culture: Media that can be used are the ff: BAP, - Over 100 species
MSA, PEA, CAN, BHI, thioglycollate, and - General characteristics: streptococcaceae
CHROM agar - Catalase negative, gram postitive cocci that is usally
o Colistin-nalidixic agar (CNA) used for arrange in pairs or chains
purulent exudates - Negative
o Phenylethyl alcohol (PEA) agar is enriched
with 5% sheep blood and is selective for
Gram-positive bacteria
o Mannitol salt agar (MSA) and PEA for
heavily contaminated specimens
You might also like
- PDF Document 2Document313 pagesPDF Document 2nasarcedaNo ratings yet
- Laboratory 11 EnterobacteriaceaeDocument9 pagesLaboratory 11 EnterobacteriaceaeRazmine RicardoNo ratings yet
- Staphylococcus and MicrococcusDocument4 pagesStaphylococcus and MicrococcusAmador GielasNo ratings yet
- A Numerical Taxonomic Study of The Dominant Bacteria Isolated From Tilapia IntestinesDocument10 pagesA Numerical Taxonomic Study of The Dominant Bacteria Isolated From Tilapia IntestinesPutri ArisyaNo ratings yet
- Thermophilic Organisms in Food Spoilage: Flat-Sour Aerobes: Keitha - ItoDocument7 pagesThermophilic Organisms in Food Spoilage: Flat-Sour Aerobes: Keitha - ItoNagarajanAbimanyuNo ratings yet
- EnterobacteriaceaeDocument8 pagesEnterobacteriaceaeWansun MaglangitNo ratings yet
- BACTE NonfermentativeDocument3 pagesBACTE NonfermentativeRichelyn Grace B. VenusNo ratings yet
- Nature: February 21, 1959Document1 pageNature: February 21, 1959Subash Arunagiri (RA1911009010004)No ratings yet
- Clinical Bacteriology MidtermDocument32 pagesClinical Bacteriology MidtermRazmine RicardoNo ratings yet
- Louis Pasteur, Fermentation, and A Rival: History of ScienceDocument4 pagesLouis Pasteur, Fermentation, and A Rival: History of ScienceSamNo ratings yet
- (Microbio) Staphyloccocus and Streptococcus-Dr. Salandanan (BHND)Document16 pages(Microbio) Staphyloccocus and Streptococcus-Dr. Salandanan (BHND)Lee Delos Santos100% (1)
- Klebsiella Pneumoniae: Metabolismo Bacteriano "Identificación Bacterias Gram Negativas"Document9 pagesKlebsiella Pneumoniae: Metabolismo Bacteriano "Identificación Bacterias Gram Negativas"Andrés RamírezNo ratings yet
- Atlas of Pyrenulaceae and Trypetheliaceae - Volume 1: Lichenized AscomycotaFrom EverandAtlas of Pyrenulaceae and Trypetheliaceae - Volume 1: Lichenized AscomycotaNo ratings yet
- Example of ExtremophilesDocument17 pagesExample of ExtremophilesSean Dykimbe GauzonNo ratings yet
- Study Stack - M (ASCP) EXAM Table Review PDFDocument9 pagesStudy Stack - M (ASCP) EXAM Table Review PDF장주연100% (2)
- Domain ArcheaaDocument3 pagesDomain ArcheaaAr-jhoanne VillafuerteNo ratings yet
- Amylase Bernfeld AssayDocument1 pageAmylase Bernfeld AssayLaxmikant KambleNo ratings yet
- Bacteriology 3Document17 pagesBacteriology 3JulanHalimuyakNo ratings yet
- Beta-Galactosidase Identification of Enterobacteria Including SalmonellaeDocument5 pagesBeta-Galactosidase Identification of Enterobacteria Including SalmonellaeJirapat ThonglekpechNo ratings yet
- Vibrio, Campylobacter, and HelicobacterDocument7 pagesVibrio, Campylobacter, and HelicobacterRach ReyesNo ratings yet
- Micro by DR - Hesham (GIT)Document65 pagesMicro by DR - Hesham (GIT)abcde990075No ratings yet
- The discovery of β-galactosidaseDocument3 pagesThe discovery of β-galactosidaseÁlvaro SousaNo ratings yet
- Alkali PhileDocument9 pagesAlkali PhileGhanshyamPatankarNo ratings yet
- Lecture MPDocument5 pagesLecture MPMichelle kate GamoloNo ratings yet
- 430 - Microbiology) Staphylococcus - Aureus, Epidermidis, Saprophyticus PDFDocument8 pages430 - Microbiology) Staphylococcus - Aureus, Epidermidis, Saprophyticus PDFMohammad ullah AhmadiNo ratings yet
- Lysine Iron Agar L: Art. No. 01-094Document2 pagesLysine Iron Agar L: Art. No. 01-094LuluNo ratings yet
- Staphylococcus - Aureus, Epidermidis, Saprophyticus AtfDocument8 pagesStaphylococcus - Aureus, Epidermidis, Saprophyticus AtfFeven AbrahamNo ratings yet
- Ferroplasma AcidiphilumDocument10 pagesFerroplasma AcidiphilumYupNo ratings yet
- MICRO Master ListDocument63 pagesMICRO Master ListDaniel Del RiscoNo ratings yet
- Bile Esculin Agar: Recommended ProcedureDocument2 pagesBile Esculin Agar: Recommended ProcedureBrendon MuriraNo ratings yet
- Klebsiella Shigella Yersinia: Have Little Value in IDDocument6 pagesKlebsiella Shigella Yersinia: Have Little Value in IDKenneth Jake Batiduan100% (1)
- Us 2809920Document4 pagesUs 2809920SmokeNo ratings yet
- Shifting Exams Reviewer For MEDTECH in ParasitologyDocument12 pagesShifting Exams Reviewer For MEDTECH in ParasitologyIwa RohasNo ratings yet
- Bacte Final ReviewerDocument14 pagesBacte Final ReviewerShiella Mae SalamanesNo ratings yet
- Microbiology 1.4 Gram Positive Cocci - Dr. Sia CungcoDocument10 pagesMicrobiology 1.4 Gram Positive Cocci - Dr. Sia CungcoRyn ShadowNo ratings yet
- Lesson 7 Streptococcus and EnterococcusDocument7 pagesLesson 7 Streptococcus and EnterococcusRazmine RicardoNo ratings yet
- 10.1515 - ZNC 2007 7 802Document6 pages10.1515 - ZNC 2007 7 802ayuk novaNo ratings yet
- ASCP ReviewerDocument8 pagesASCP Reviewergillian102290100% (6)
- Microbial World: VirusDocument18 pagesMicrobial World: VirusShyenNo ratings yet
- Student Notes: Micro 1: Davao Doctors College Medical Laboratory Science DepartmentDocument5 pagesStudent Notes: Micro 1: Davao Doctors College Medical Laboratory Science DepartmentMelody Jane PardilloNo ratings yet
- MC3 NotesDocument23 pagesMC3 NotesJustineNo ratings yet
- MLT Bacteriology Case PDFDocument6 pagesMLT Bacteriology Case PDFJames 'jps' SimanjuntakNo ratings yet
- Enterobacteriaceae CondensadaDocument4 pagesEnterobacteriaceae Condensadajoseadreannes.pinedaNo ratings yet
- 2.3 - EnterobacteriaceaeDocument39 pages2.3 - Enterobacteriaceaesajad abasNo ratings yet
- MICROBIOLOGY - Microbial Taxonomy, Cell Structure and Bacterial Metabolism, Growth & GeneticsDocument16 pagesMICROBIOLOGY - Microbial Taxonomy, Cell Structure and Bacterial Metabolism, Growth & GeneticsRobie LeañoNo ratings yet
- Microbiology A Laboratory Manual 11th Edition Cappuccino Solutions Manual 1Document36 pagesMicrobiology A Laboratory Manual 11th Edition Cappuccino Solutions Manual 1joshuawongawzspdkxjb100% (27)
- Acanthamoeba Strains Isolated From Organs of Freshwater FishesDocument8 pagesAcanthamoeba Strains Isolated From Organs of Freshwater FishestishaNo ratings yet
- Diseases and Infections of Snakes: A Review'Document16 pagesDiseases and Infections of Snakes: A Review'Samantha Orozco PinedaNo ratings yet
- Important Media and Biochemical Tests For Diagnostic Microbiology 2023Document3 pagesImportant Media and Biochemical Tests For Diagnostic Microbiology 2023yn6q5fc5pzNo ratings yet
- Biochemistry: Course Packet 01: Introduction To BiochemistryDocument2 pagesBiochemistry: Course Packet 01: Introduction To BiochemistryBarbie Lou100% (1)
- Yersinia 1Document10 pagesYersinia 1Veronica EugenioNo ratings yet
- Phylogenetc CharactersDocument5 pagesPhylogenetc CharactersHafsa ZeeshanNo ratings yet
- Module 6.5 MycologyDocument4 pagesModule 6.5 MycologyPNo ratings yet
- Hektoen Enteric Agar ProtocolDocument13 pagesHektoen Enteric Agar ProtocolYakisoba menNo ratings yet
- Week 8 - Bacteriology LectureDocument7 pagesWeek 8 - Bacteriology LectureReangg SerranoNo ratings yet
- Cheeke 1971 CJAS Saponin-RevDocument14 pagesCheeke 1971 CJAS Saponin-RevRinaERpienaNo ratings yet
- BIO 120 LE 1: Notatum Roqueforti Have Been Grown On SlopeDocument5 pagesBIO 120 LE 1: Notatum Roqueforti Have Been Grown On SlopeAnj VillaruelNo ratings yet
- Aureus C. Diphteriae (Man) : Classification Based On HaemolysisDocument4 pagesAureus C. Diphteriae (Man) : Classification Based On HaemolysisJulia IshakNo ratings yet
- Tmod Vignette CurrentDocument33 pagesTmod Vignette CurrentIsabelle MoscardiniNo ratings yet
- Topic 1 U4Document3 pagesTopic 1 U4api-263323894No ratings yet
- Intro To Biohacking: or "How I Learned To Stop Worrying and Love The Zombie Apocalypse"Document31 pagesIntro To Biohacking: or "How I Learned To Stop Worrying and Love The Zombie Apocalypse"rasromeoNo ratings yet
- American Center For Calculation of Biological Functionalities Amultidisciplinary Forum For Designing Therapeutic Interventions and PDFDocument10 pagesAmerican Center For Calculation of Biological Functionalities Amultidisciplinary Forum For Designing Therapeutic Interventions and PDFjzsinghNo ratings yet
- Dear Mom and Dad,: Read The Following Text and Answer The Question Number 1 - 5Document11 pagesDear Mom and Dad,: Read The Following Text and Answer The Question Number 1 - 5marlin100% (1)
- Module 7 Biotechnology PDFDocument15 pagesModule 7 Biotechnology PDFNizea Camille Navarro JavierNo ratings yet
- Syllabus DUDocument20 pagesSyllabus DUশর্ট সার্কিটNo ratings yet
- NHPDocument31 pagesNHPSUBANo ratings yet
- Urine TestsDocument398 pagesUrine TestsAliMohamad100% (1)
- Biomaterials and Cells For Neural Tissue EngineeringDocument60 pagesBiomaterials and Cells For Neural Tissue EngineeringYusser olguínNo ratings yet
- Alison Smith, Michael Witty-Heme, Chlorophyll, and Bilins - Methods and Protocols (2001)Document351 pagesAlison Smith, Michael Witty-Heme, Chlorophyll, and Bilins - Methods and Protocols (2001)Andres CastilloNo ratings yet
- Egg Inoculation ManualDocument115 pagesEgg Inoculation ManualdentamilanNo ratings yet
- Pcap C Case StudyDocument21 pagesPcap C Case StudyKate PedzNo ratings yet
- Himedia Mueller Hinton AgarDocument3 pagesHimedia Mueller Hinton AgarRizka SukmasariNo ratings yet
- Study of Histopathological Pattern of Thyroid Lesions: International Journal of Biomedical and Advance ResearchDocument10 pagesStudy of Histopathological Pattern of Thyroid Lesions: International Journal of Biomedical and Advance ResearchAprilia Fani PNo ratings yet
- Effects of Lactobacillus Bulgaricus in Soyghurt On Inhibition of Adhesion Klebsiella Pneumoniae Strains in HEp-2 Cell LinesDocument6 pagesEffects of Lactobacillus Bulgaricus in Soyghurt On Inhibition of Adhesion Klebsiella Pneumoniae Strains in HEp-2 Cell Linesprimayaa4758No ratings yet
- The Effects of Pituitary and Thyroid Disorders On Haemostasis, Potential Clinical ImplicationsDocument12 pagesThe Effects of Pituitary and Thyroid Disorders On Haemostasis, Potential Clinical ImplicationsTamara Silva FabresNo ratings yet
- Noonan Syndrome and Clinically Related Disorders (2011)Document25 pagesNoonan Syndrome and Clinically Related Disorders (2011)ramonaNo ratings yet
- I. Mother and Child HealthDocument70 pagesI. Mother and Child Healthconahs nasugbuNo ratings yet
- Herpetic Mucocutaneous Infections: HSV (HSV 1 & 2) & VZVDocument32 pagesHerpetic Mucocutaneous Infections: HSV (HSV 1 & 2) & VZVJaneNo ratings yet
- Dr. Alfadel Alshaibani - Hematology Board ReviewDocument258 pagesDr. Alfadel Alshaibani - Hematology Board ReviewHanadi UmhanayNo ratings yet
- Aquatic Microbiology Lectures: 1, 2, 3 Level: 4Document20 pagesAquatic Microbiology Lectures: 1, 2, 3 Level: 4nareman hassan100% (1)
- BIO 30 Lec 1 - 3 SummaryDocument6 pagesBIO 30 Lec 1 - 3 SummaryAnonymous w17gcfbpNo ratings yet
- Non Mendelian GeneticsDocument63 pagesNon Mendelian Geneticshenry james rosNo ratings yet
- Zoology Syllabus CBCSDocument12 pagesZoology Syllabus CBCSACADEMIC PUBLISHERS100% (1)
- Gigazyme X Tra: Our PlusDocument2 pagesGigazyme X Tra: Our PlusHemant Singh100% (1)
- ? PHARMA 3. Anti InfectivesDocument130 pages? PHARMA 3. Anti InfectivesMiguel Luis NavarreteNo ratings yet
- PhysioEx Exercise 12 Activity 1Document4 pagesPhysioEx Exercise 12 Activity 1t4gjzhpfjcNo ratings yet
- NCERT Exemplar For Class 12 Biology Chapter 6Document31 pagesNCERT Exemplar For Class 12 Biology Chapter 6Me RahaviNo ratings yet
- 10 Chapter 3Document12 pages10 Chapter 3SumitNo ratings yet