Professional Documents
Culture Documents
Preoperative Diagnosis of Benign Thyroid Nodules With Indeterminate Cytology
Uploaded by
LaraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Preoperative Diagnosis of Benign Thyroid Nodules With Indeterminate Cytology
Uploaded by
LaraCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
original article
Preoperative Diagnosis of Benign Thyroid
Nodules with Indeterminate Cytology
Erik K. Alexander, M.D., Giulia C. Kennedy, Ph.D., Zubair W. Baloch, M.D., Ph.D.,
Edmund S. Cibas, M.D., Darya Chudova, Ph.D., James Diggans, Ph.D.,
Lyssa Friedman, R.N., M.P.A., Richard T. Kloos, M.D., Virginia A. LiVolsi, M.D.,
Susan J. Mandel, M.D., M.P.H., Stephen S. Raab, M.D., Juan Rosai, M.D.,
David L. Steward, M.D., P. Sean Walsh, M.P.H., Jonathan I. Wilde, Ph.D.,
Martha A. Zeiger, M.D., Richard B. Lanman, M.D., and Bryan R. Haugen, M.D.
A BS T R AC T
BACKGROUND
Approximately 15 to 30% of thyroid nodules evaluated by means of fine-needle aspi- From the Departments of Medicine
ration are not clearly benign or malignant. Patients with cytologically indeterminate (E.K.A.) and Pathology (E.S.C.), Brigham
and Women’s Hospital and Harvard
nodules are often referred for diagnostic surgery, though most of these nodules prove Medical School, Boston; Veracyte, South
to be benign. A novel diagnostic test that measures the expression of 167 genes has San Francisco, CA (G.C.K., D.C., J.D., L.F.,
shown promise in improving preoperative risk assessment. P.S.W., J.I.W., R.B.L.); the Departments of
Pathology (Z.W.B., V.A.L.) and Medicine
(S.J.M.), Perelman School of Medicine,
METHODS University of Pennsylvania, Philadelphia;
We performed a 19-month, prospective, multicenter validation study involving 49 clini- the Department of Medicine, Ohio State
University College of Medicine, Columbus
cal sites, 3789 patients, and 4812 fine-needle aspirates from thyroid nodules 1 cm or (R.T.K.); the Department of Pathology,
larger that required evaluation. We obtained 577 cytologically indeterminate aspi- University of Washington School of Medi-
rates, 413 of which had corresponding histopathological specimens from excised cine, Seattle (S.S.R.); Centro Diagnostico
Italiano, Milan (J.R.); the Department of
lesions. Results of a central, blinded histopathological review served as the reference Surgery, University of Cincinnati College of
standard. After inclusion criteria were met, a gene-expression classifier was used to Medicine, Cincinnati (D.L.S.); the Depart-
test 265 indeterminate nodules in this analysis, and its performance was assessed. ment of Surgery, Johns Hopkins University
School of Medicine, Baltimore (M.A.Z.);
and the Department of Medicine, Univer-
RESULTS sity of Colorado School of Medicine, Au-
Of the 265 indeterminate nodules, 85 were malignant. The gene-expression classifier rora (B.R.H.). Address reprint requests to
Dr. Alexander at the Thyroid Unit, Division
correctly identified 78 of the 85 nodules as suspicious (92% sensitivity; 95% confi- of Endocrinology, Metabolism and Dia-
dence interval [CI], 84 to 97), with a specificity of 52% (95% CI, 44 to 59). The betes, Brigham and Women’s Hospital,
negative predictive values for “atypia (or follicular lesion) of undetermined clinical 75 Francis St., Rm. PBB-B4, Boston, MA
02115, or at ekalexander@partners.org;
significance,” “follicular neoplasm or lesion suspicious for follicular neoplasm,” or or to Dr. Kennedy at Veracyte, Inc.,7000
“suspicious cytologic findings” were 95%, 94%, and 85%, respectively. Analysis of Shoreline Ct., Suite 250, South San Fran-
7 aspirates with false negative results revealed that 6 had a paucity of thyroid fol- cisco, CA 94080, or at giulia@veracyte
.com.
licular cells, suggesting insufficient sampling of the nodule.
This article was published on June 25, 2012,
CONCLUSIONS at NEJM.org.
These data suggest consideration of a more conservative approach for most patients N Engl J Med 2012.
with thyroid nodules that are cytologically indeterminate on fine-needle aspiration DOI: 10.1056/NEJMoa1203208
and benign according to gene-expression classifier results. (Funded by Veracyte.) Copyright © 2012 Massachusetts Medical Society.
n engl j med nejm.org 1
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
T
hyroid nodules are common and blood markers.19,20 Though useful, these markers
are usually benign.1 However, 5 to 15% have limited sensitivity and a limited negative pre-
prove to be malignant; accordingly, identi- dictive value21,22 and therefore fail to detect more
fication of a nodule 1 cm or larger in diameter than 33% of cancers.16 This rate is too high to be
often prompts a diagnostic evaluation.2,3 The helpful in making the difficult choice between
cornerstone of thyroid-nodule evaluation is fine- watchful waiting and diagnostic thyroid surgery.
needle aspiration,4 which enables the assessment Thus, currently available molecular markers fail
of cellular morphologic features that could not be to rule out cancer with sufficient certainty to
identified by means of clinical assessment or im- avoid surgery in most patients with indetermi-
aging. Preoperative, ultrasonographically guided nate nodules.
fine-needle aspiration has been shown to accu- Studies have described the development of
rately classify 62 to 85% of thyroid nodules as gene-expression classifiers that better distin-
benign, thereby avoiding diagnostic surgery.5 guish benign from malignant thyroid nodules.22
However, 15 to 30% of aspirations yield inde- To be of use in avoiding surgery, such a test
terminate cytologic findings,4 which include three would need to have high sensitivity and a high
subtypes: “atypia (or follicular lesion) of undeter- negative predictive value. However, these previ-
mined significance,” “follicular neoplasm or sus- ously reported genomic classifiers remain limited
picious for follicular neoplasm,” and “suspicious in their sensitivity, and their usefulness has not
for malignancy.”6,7 Most patients with cytologi- been validated in large groups of patients.22 Re-
cally indeterminate nodules are referred for diag- cently, a gene-expression classifier has been found
nostic thyroid surgery, but the majority prove to to help identify nodules that are benign rather
have benign disease.4,8 For these patients, thyroid than malignant. This classifier was shown to
surgery is unnecessary, yet it exposes them to a have a sensitivity exceeding 90% and a negative
2 to 10% risk of serious surgical complications, predictive value greater than 95% in a pilot
and most would require levothyroxine replace- study.23 We describe the results of a large, pro-
ment therapy for life.9-13 These data confirm the spective, double-blind, multicenter study validat-
critical need to improve the preoperative diag- ing this gene-expression classifier in patients with
nostic evaluation for patients with indeterminate indeterminate thyroid nodules.
cytologic findings on fine-needle aspiration.
Molecular analysis of thyroid tissue is poised to Me thods
become a powerful adjunct to visual microscopical
evaluation, since 60 to 70% of thyroid cancers STUDY DESIGN AND OVERSIGHT
harbor at least one known genetic mutation.14 The study was designed and supervised by the
Recent investigations have revealed the potential coprincipal academic investigators and by two
benefits of combined microscopical and molecular employees of Veracyte (the makers of this gene-
analysis of thyroid nodules.15 When indetermi- expression classifier), with oversight by a steer-
nate aspirates were analyzed for the presence of ing committee that met to review the study pro-
BRAF and RAS mutations and for RET/PTC and tocol and analysis. All authors reviewed the study
PAX8–PPARγ (peroxisome proliferator–activated data, vouch for the fidelity of the data and con-
receptor gamma 1) gene rearrangements, muta- duct of the study to the protocol, and approved
tions were found in 16% of cases.16 These ge- the decision to submit the manuscript for publi-
netic markers have high specificity and a high cation. No authors except those who are Veracyte
positive predictive value and therefore identify employees serve as consultants or hold equity or
which indeterminate nodules are malignant.17 equity options in the company. Samples were
Marker positivity can lead to a recommendation for tested at Veracyte in a laboratory certified ac-
total thyroidectomy rather than for hemithyroid- cording to the provisions of the Clinical Labora-
ectomy or watchful waiting. With this approach, tory Improvement Amendments, and the statisti-
a second thyroidectomy (so-called completion cal analysis was performed by two authors who
thyroidectomy) is avoided if the initial hemithy- are statisticians at Veracyte. The protocol was ap-
roidectomy reveals malignant nodules.18 This proved by both central and institution-specific
clinical scenario is similar to that described in investigational review boards. All patients pro-
reports on the use of epigenetic and peripheral- vided written informed consent to participate in
2 n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
Cytologically Indeterminate Thyroid Nodules
the study. The coprincipal investigators had full assessed for eligibility24,25 (median follow-up
access to all study data and analyses. The first time from time of sampling, 301 days). After
author wrote the first draft of the manuscript, surgery, local histopathological reports and
and no one other than the listed authors assisted slides were collected, and biopsied nodules were
in the writing. matched to resected nodules according to size
and location. All slides were deidentified and
STUDY POPULATION AND PROTOCOL scanned to construct a permanent digital file of
We performed a prospective, noninterventional, microscopical images, and the reference stan-
multicenter validation trial (VERA001) involving dard diagnosis was determined, as described in
patients with ultrasonographically confirmed thy- the Supplementary Appendix. Results that met the
roid nodules, 1 cm or larger in diameter, evalu- histopathological standard and results from the
ated by means of routine fine-needle aspiration. gene-expression classifier were maintained in
Throughout the study, both patients and physicians two separate, password-protected databases. On
were unaware of the results of testing with the completion of the study, unblinding and merging
gene-expression classifier (Afirma). Fine-needle of these data sets were performed by an inde-
aspiration samples were obtained from patients pendent third party. After the results became
at 49 U.S. sites (see the Supplementary Appendix, available, it was determined that 36 samples fell
available with the full text of this article at NEJM outside the 14-day shipping requirements speci-
.org). Study sites were representative of both aca- fied a priori in the protocol, 5 samples did not
demic and community centers in 26 states. The meet clinical eligibility criteria, and 5 separate
fine-needle aspirations consisted of two to five fine-needle aspirates represented duplicate aspi-
needle insertions within each nodule, and 99% rations from the same nodules performed at
were ultrasonographically guided. Initially, one different clinical visits. One additional sample
additional sample was obtained for genomic anal- was found to have insufficient referential integ-
ysis and was shipped frozen (on dry ice). Midway rity for inclusion, since the pathology experts
through the study, however, the protocol was could not independently confirm that the ultra-
modified: two needle insertions were added to sonographically aspirated nodule corresponded
improve the RNA yield, and samples were shipped to the tissue submitted for histologic analysis.
at a temperature of 2 to 25°C. There was no in- Therefore, 47 samples were excluded from the pri-
crease in procedural complications; thus, the com- mary analysis. (The reasons for exclusion are de-
mercially available test requires two needle inser- scribed in detail in the Supplementary Appendix.)
tions. For each enrolled patient, demographic and Gene-expression data are available at the Gene
thyroid-specific characteristics were recorded. Expression Omnibus website (www.ncbi.nlm.nih
Ultrasonographic data precisely confirmed the .gov/geo) under accession number GSE34289.
location and size of the nodules.
After fine-needle aspiration, local cytologic LABORATORY METHODS
reports were collected for all patients, and reports Detailed descriptions of the microarray assay, the
without a definitive benign or malignant local training of the gene-expression classifier, and
diagnosis were reviewed by three expert cytopa- the annotation of genes used by the classifier are
thologists, who reclassified each report according provided in the Supplementary Appendix and in
to three categories of the Bethesda System for prior reports.23 All training samples were inde-
Reporting Thyroid Cytopathology: atypia (or fol- pendent of the validation set used in this study
licular lesion) of undetermined significance, fol- and comprised thyroid samples with defined di-
licular neoplasm or lesion suspicious for follicular agnoses representing one of two classes: benign
neoplasm, and lesion suspicious for malignancy.7 or malignant. The locked algorithm uses expres-
Thyroid surgery was performed on the basis of sion of 167 genes to classify aspirated material
the clinical judgment of the treating physician at from thyroid nodules as either benign or suspi-
each study site, without knowledge of the results cious. There are 142 genes in the main classifier
on gene-expression classification. The study was (benign or suspicious) and 25 genes that initially
open for enrollment between June 23, 2009, and filter out rare neoplasms as the sample is pro-
December 3, 2010, and patients with confirmed cessed through a stepwise diagnostic algorithm
surgery scheduled before January 31, 2011, were in a series of “cassettes.” A linear modeling ap-
n engl j med nejm.org 3
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
proach was used for feature selection, and a sup- of undetermined significance, 31% follicular neo-
port-vector machine was used for classification. plasms or lesions suspicious for follicular neo-
plasm, and 21% lesions suspicious for malignan-
STATISTICAL ANALYSIS cy. Baseline characteristics of the patients and
Statistical analysis was performed with the use of nodules are shown in Table 1. Age, sex, clinical
R software, version 2.13. Continuous variables were risk factors, nodule size, and proportion of
analyzed by means of Student’s t-test and the samples collected at community versus academic
Wilcoxon rank-sum test. Categorical variables were centers did not differ significantly between the
analyzed with the use of Fisher’s exact test, and the primary study population (265 samples) and the
Holm procedure was used to correct for testing as- entire cohort of patients with resected cytologi-
sociations with multiple clinical variables. Sensitiv- cally indeterminate nodules (413 samples), and
ity, specificity, and negative and positive predic- these findings are representative of the targeted
tive values were calculated with the use of population.27 In addition to cytologically inde-
established methods.26 Two-sided P values of less terminate samples, we evaluated a randomly se-
than 0.05 were considered to indicate statistical lected subset of 47 cytologically benign and 55
significance. Confidence intervals for proportions cytologically malignant surgical samples obtained
are reported as two-sided exact binomial 95% from an independent group of patients.
confidence intervals.
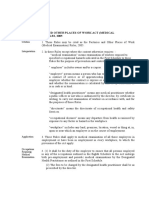
Performance of the Gene-Expression
R e sult s Classifier
Figure 1 summarizes the clinical performance
Characteristics of Patients and Nodules characteristics for all relevant sample groups.
To independently validate the results obtained with Of the 265 indeterminate fine-needle aspirates,
the gene-expression classifier, we prospectively 85 (32%) were classified as malignant on blinded
collected 4812 nodule aspirates from 3789 pa- histopathological review. The gene-expression
tients at 49 clinical sites in the United States over a classifier correctly identified 78 of the 85 malig-
19-month period. Of the 4812 samples, 577 were nant samples as “suspicious,” yielding a sensitiv-
indeterminate (12%); for 413 of the 577 samples, ity of 92% (95% confidence interval [CI], 84 to 97);
resection was subsequently performed, allowing 93 of 180 nonmalignant samples were correctly
for blinded histopathological review to define identified as benign by the gene-expression clas-
the reference standard. Of the resected samples, sifier, yielding a specificity of 52% (95% CI, 44 to
25 were used for training the classifier and for 59). For nodules classified as atypia (or follicular
analytic verification studies, and 10 were deter- lesions) of undetermined significance, the sensi-
mined to be ineligible (4 because the patient was tivity was 90% (95% CI, 74 to 98) and the speci-
younger than 21 years of age, 3 because the sam- ficity was 53% (95% CI, 43 to 63). For nodules
ples were not received intact, 2 because the nod- classified as follicular neoplasms or lesions sus-
ule size was <1 cm, and 1 because of a protocol picious for follicular neoplasm, the sensitivity
deviation at the time of enrollment); all 35 were was 90% (95% CI, 68 to 99) and the specificity
excluded from the final analysis. was 49% (95% CI, 36 to 62). For nodules classi-
Using predefined laboratory quality-control fied as lesions suspicious for malignancy, the
metrics, we successfully processed 328 samples sensitivity was 94% (95% CI, 80 to 99) and the
through the assay, which resulted in valid classi- specificity was 52% (95% CI, 30 to 74). The per-
fier results. A standard histopathological diagno- centage of malignant lesions in these three inde-
sis was available for 312 of these samples (95%). pendent categories was 24%, 25%, and 62%, re-
As noted above, 47 samples were excluded, leav- spectively, yielding respective negative predictive
ing 265 independent, indeterminate nodules for values of 95%, 94%, and 85%. Of 47 samples that
primary analysis (Fig. 1 in the Supplementary were cytologically benign, 3 (6%) were malignant
Appendix). on histopathological review. Although this could
Review of local cytopathological reports by the be considered an estimate of the false negative
central expert panel confirmed the indetermi- rate for cytologically benign samples, the pa-
nate classification of the nodules: 49% of samples tients may also have undergone surgery on the
were considered to be atypia (or follicular lesions) basis of other characteristics that distinguished
4 n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
Cytologically Indeterminate Thyroid Nodules
Table 1. Baseline Demographic and Clinical Characteristics of the Study Cohort.
Indeterminate Cytologic
Total Indeterminate Findings and Final Validation
Variable Enrollment Cytologic Findings Subsequent Surgery Set
Total no.
Samples 4812 577 413 265
Nodules 4775 567 403 265
Patients 3789 532 378 249
Type of study site — % of samples
Academic 21.4 34.1 37.3 35.1
Community 78.6 65.9 62.7 64.9
No. of fine-needle aspiration passes — % of samples
1 54.2 51.5 55.4* 43.4†
2 45.8 48.5 44.6* 56.6†
Age of patients — yr
Mean 53.2 52.8 51.8* 51.5
Range 18–91 19–85 19–85 22–85
Sex — no. of patients (%)
Male 696 (18.4) 116 (21.8) 84 (22.2) 55 (22.1)
Female 3093 (81.6) 416 (78.2) 294 (77.8) 194 (77.9)
Risk factors — no. of patients (%)
Radiation exposure — head, neck, or both 91 (2.4) 14 (2.6) 8 (2.1) 8 (3.2)
Family history of thyroid cancer 174 (4.6) 32 (6) 28 (7.4)* 18 (7.2)
Nodules
Size on ultrasonography — cm
Median 1.9 2.2 2.3 2.3
Range 0.6–11 0.75–10.3 0.75–10.3 1–9.1
Size group — no. of nodules (%)
<1.00 cm 37 (0.8) 4 (0.7) 3 (0.7) 0
1.00–1.99 cm 2503 (52.4) 230 (40.6) 153 (38.0) 102 (38.5)
2.00–2.99 cm 1204 (25.2) 153 (27.0) 111 (27.5) 76 (28.7)
3.00–3.99 cm 621 (13.0) 105 (18.5) 76 (18.9) 45 (17.0)
≥4.00 cm 392 (8.2) 74 (13.1) 60 (14.9) 42 (15.8)
Size not available 18 (0.4) 1 (0.2) 0 0
* P<0.05 for the comparison of results for patients who underwent surgery for indeterminate nodules versus patients who did not.
† P<0.05 for the comparison of results for patients who underwent surgery for indeterminate nodules and were included in the final validation
set versus those who were not included.
them from the general population. Nevertheless, variety of malignant subtypes were correctly
the gene-expression classifier correctly identified classified as suspicious for malignancy accord-
all 3 of these malignant samples as suspicious. ing to this test (Table 2). These included papil-
All 55 samples that were cytologically malignant lary, medullary, and follicular thyroid carcinomas
were classified as malignant on histopathologi- (including those with oncocytic features); poorly
cal evaluation, and all were considered to be sus- differentiated thyroid carcinomas; and thyroid
picious for malignancy according to the gene- lymphomas.
expression classifier (100% sensitivity). A wide There were seven false negative results (Table 3).
n engl j med nejm.org 5
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Figure 1. Performance of the Gene-Expression Classifier
Performance across the Primary Data Set of Indeterminate Nodules (N=265) (GEC), According to the Final Histopathological Diag-
Malignant reference Benign reference noses for Cytologically Indeterminate Samples.
GEC result standard (N=85) standard (N=180) NPV denotes negative predictive value and PPV posi-
Suspicious 78 87 tive predictive value.
Benign 7 93
Sensitivity, 92% (84–97); specificity, 52% (44–59); PPV, 47% (40–55);
NPV, 93% (86–97); prevalence of malignant lesions, 32% One was a Hürthle-cell carcinoma, and the other
Atypia of Undetermined Significance or Follicular Lesion of Undetermined six were papillary thyroid carcinomas. To better
Significance (N=129, 48.7%) understand potential causes of false negative
Malignant reference Benign reference results, we measured single molecular markers
GEC result standard (N=31) standard (N=98) described in the literature as being elevated in
Suspicious 28 46 papillary thyroid carcinoma. Two of these mark-
Benign 3 52
ers, cytokeratin 19 and CITED1 (Cpb/p300-inter-
Sensitivity, 90% (74–98); specificity, 53% (43–63); PPV, 38% (27–50);
NPV, 95% (85–99); prevalence of malignant lesions, 24%
acting transactivator 1) (neither of which was used
in the gene-expression classifier), were measured
Follicular or Hürthle-Cell Neoplasm or Suspicious for Follicular Neoplasm for signal intensity.28 The expression of both
(N=81, 30.6%)
markers was significantly lower in all six papil-
Malignant reference Benign reference
GEC result standard (N=20) standard (N=61) lary carcinoma samples with false negative re-
Suspicious 18 31 sults than in the samples correctly identified by
Benign 2 30 the classifier; the mean log2 difference in expres-
Sensitivity, 90% (68–99); specificity, 49% (36–62); PPV, 37% (23–52); sion intensity was 1.9 with cytokeratin 19 and 3.0
NPV, 94% (79–99); prevalence of malignant lesions, 25% with CITED1 (P<0.001 for both comparisons)
Suspicious for Malignancy (N=55, 20.8%) (Fig. 2). This finding suggests that assay failure
Malignant reference Benign reference
is not responsible for the six false negative cases.
GEC result standard (N=34) standard (N=21) We then investigated whether the absence of a
Suspicious 32 10 papillary thyroid carcinoma signal in the false
Benign 2 11 negative cases could be due to a paucity of thy-
Sensitivity, 94% (80–99); specificity, 52% (30–74); PPV, 76% (61–88); roid follicular cells in the sample. We evaluated
NPV, 85% (55–98); prevalence of malignant lesions, 62%
epithelial and thyroid follicular cell content by
Performance on Cytopathologically Benign Samples (N=47) assaying the following markers: cytokeratin 7,
Malignant reference Benign reference thyrotropin receptor, thyroglobulin, and thyroid
GEC result standard (N=3) standard (N=44) transcription factor 1.29 None of these markers
Suspicious 3 13 are used by the gene-expression classifier. Expres-
Benign 0 31
sion patterns showed that five of six papillary
Sensitivity, 100% (29–100); specificity, 70% (55–83); prevalence of
malignant lesions, 6%
carcinoma samples with false negative results had
low follicular cell content (three samples fell
Performance on Cytopathologically Malignant Samples (N=55) within the lowest 10% of all indeterminate sam-
Malignant reference Benign reference ples, and two other samples within the lowest
GEC result standard (N=55) standard (N=0)
20%). For three of the four markers, the differ-
Suspicious 55 0
Benign 0 0
ence in follicular content between the samples
Sensitivity, 100% (93–100); prevalence of malignant lesions, 100%
with false negative results and the samples with
true positive results was significant, with a mean
Performance across the Entire Data Set of Indeterminate Samples, When Both log2 difference of more than 1.4 (P≤0.004 for all
GEC Results and Reference Standard Were Available (before post hoc
exclusions) (N=312) comparisons).
Malignant reference Benign reference
Other potential causes of false negative re-
GEC result standard (N=100) standard (N=212) sults were considered. The rate of disagreement
Suspicious 87 100 between two experts on initial blind review was
Benign 13 112 14% (37 out of 265), and the rate of post-conferral
Sensitivity, 87% (79–93); specificity, 53% (46–60); PPV, 47% (39–54); disagreement in defining the reference standard
NPV, 90% (83–94); prevalence of malignant lesions, 32%
was 2% (see the Supplementary Appendix). How-
ever, none of the false negative results were found
6 n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
Cytologically Indeterminate Thyroid Nodules
Table 2. Performance of Gene-Expression Classifier, According to Histopathological Subtype.
Result with Gene-
Histopathological Subtype No. of Nodules (%) Expression Classifier
no. benign/no. suspicious
Benign
Total 180 (100)
Benign follicular nodule* 71 (39.4) 41/30
Follicular adenoma 64 (35.6) 37/27
Follicular tumor of uncertain malignant potential 11 (6.1) 5/6
Well-differentiated tumor of uncertain malignant potential 9 (5.0) 4/5
Hürthle-cell adenoma 21 (11.7) 4/17
Chronic lymphocytic thyroiditis 2 (1.1) 0/2
Hyalinizing trabecular adenoma 2 (1.1) 2/0
Malignant
Total 85 (100)
Papillary thyroid carcinoma† 42 (49.4) 4/38
Papillary thyroid carcinoma, follicular variant 19 (22.4) 2/17
Hürthle-cell carcinoma‡ 10 (11.8) 1/9
Follicular carcinoma§ 10 (11.8) 0/10
Medullary thyroid cancer 2 (2.4) 0/2
Malignant lymphoma 2 (2.4) 0/ 2
* One benign follicular nodule was a colloid nodule.
† One papillary thyroid carcinoma was the tall-cell variant.
‡ Among the Hürthle-cell carcinomas, eight showed capsular invasion and two showed vascular invasion.
§ Among the follicular carcinomas, four showed capsular invasion, one showed vascular invasion, four were well-differen-
tiated carcinomas not otherwise specified, and one was a poorly differentiated carcinoma.
among samples for which there was any disagree- Discussion
ment. We also tested demographic and clinical
factors such as age, sex, ethnic group, radiation This study describes the validation of a gene-expres-
exposure, nodule size, and family history. None sion classifier designed to identify benign, rather
were associated with false negative results. Anal- than malignant, nodules in a large population of
ysis of logistic factors, including time from fine- fine-needle aspirates with indeterminate cyto-
needle aspiration to nucleic acid extraction and logic findings. With the use of the gene-expres-
time from fine-needle aspiration to surgery, sion classifier, the negative predictive value was
showed no associations. An examination of RNA 95% for aspirates classified as atypia (or follicular
quality-control metrics, such as RNA integrity, lesions) of undetermined significance and 94% for
RNA concentration, and microarray quality met- aspirates classified as follicular neoplasms or le-
rics, also failed to show any association with false sions suspicious for follicular neoplasm, implying
negative results. We did notice a trend toward that thyroid nodules with these cytologic abnor-
false negative results in smaller nodules, using malities and benign gene-expression classifier
both ultrasonographic measurements (1.3 cm vs. results have a post-test probability of malignancy
2.2 cm, P = 0.14) and histopathological measure- that is similar to the probability for nodules with
ments (1.2 cm vs. 1.8 cm, P = 0.06). In total, these cytologically benign features on fine-needle aspi-
results suggest that insufficient nodule sam- ration.5,30 Although the negative predictive value for
pling rather than classifier error may be respon- aspirates with features suspicious for malignancy
sible for the false negative results in this study. was lower, at 85%, ascertainment of a 15% risk of
n engl j med nejm.org 7
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
RNA Integrity
Figure 2 (facing page). Molecular Signal Intensities in
* AUS–FLUS denotes atypia of undetermined significance or follicular lesion of undetermined significance, FC follicular carcinoma, FN–SFN follicular neoplasm or lesion suspicious for
Number
Samples of Papillary Thyroid Carcinoma (Including the
7.6
7.4
7.2
7.4
6.9
6.8
7.7
Follicular Variant and Tall-Cell Variant).
The box plots indicate the interquartile range and me-
dian value; the box plot whiskers indicate the most ex-
treme data points still within 1.5 times the interquar-
ng/μl
RNA
tile range from each edge of the box plot. Signal
7.6
6.5
38.2
8.6
31.1
18.1
2.0
intensity was stratified according to both the cytologic
(indeterminate [Cyto-I] or malignant [Cyto-M]) category
and the result (or “call”) of gene-expression classifica-
Malignant PTC, follicular variant
PTC, follicular variant Malignant PTC, follicular variant
tion (benign or suspicious). In each panel, the box plot
Final Histologic Diagnosis†
on the left shows false negative results (Cyto-I, benign;
6 samples), the box in the center shows true positive
Malignant HCC
Malignant PTC
Malignant PTC
Malignant PTC
Malignant PTC
results (Cyto-I, suspicious; 54 samples), and the box
Table 3. Cytologic Findings and Histopathological Diagnosis in Seven Patients with False Negative Results on Gene-Expression Classification.*
on the right shows true positive results (Cyto-M, suspi-
cious; 53 samples). Panels A and B show the signal in-
tensity of markers of thyroid cancer (cytokeratin 19 and
CITED1, respectively). Panels C through F show the
signal intensity of follicular-cell markers (cytokeratin 7,
thyrotropin receptor, thyroglobulin, and thyroid tran-
scription factor 1 [TTF-1], respectively). Dashed hori-
follicular neoplasm, HCC Hürthle-cell carcinoma, PTC papillary thyroid carcinoma, and SUSP suspicious for malignancy. zontal lines indicate the 10th, 20th, and 30th percen-
tiles of intensity for the marker in the entire cohort of
Expert 2
cytologically indeterminate samples. P values are for
PTC
PTC
PTC
PTC
PTC
FC
the difference in signal intensity between Cyto-I sam-
Pathological Diagnosis
ples classified as benign and those classified as suspi-
cious on the basis of gene-expression classification.
PTC, follicular variant
PTC, follicular variant
cancer may be useful in deciding whether to per-
form hemi-thyroidectomy or total thyroidectomy.
Expert 1
HCC
The observed sensitivity of 100% for cytologically
PTC
PTC
PTC
PTC
benign and cytologically malignant lesions pro-
vides strong independent evidence of the perfor-
mance of the gene-expression classifier. Howev-
er, the specificity of 70% for cytologically benign
AUS–FLUS
AUS–FLUS
AUS–FLUS
Diagnosis
Cytologic
lesions cautions that this test should not be used
FN–SFN
FN–SFN
SUSP
SUSP
in the analysis of samples with benign cytologic
features. Together, these data suggest that the
gene-expression classifier can be useful in mak-
On Ultrasonographic On Pathological
† The final histologic diagnosis was the reference standard.
Examination
ing important management decisions, such as
3.0
1.2
1.2
0.6
0.6
3.5
1.0
recommending watchful waiting in lieu of diag-
nostic surgery, in the case of nodules with inde-
Nodule Size
terminate cytologic features and benign findings
on subsequent testing with the gene-expression
cm
classifier.
Imaging
Patients with well-differentiated thyroid carci-
3.2
1.1
1.3
1.1
1.1
2.9
2.2
noma have an excellent prognosis, though appro-
priate surgical management is required.4,31 Cur-
rently, surgery is performed for both diagnostic
and therapeutic purposes in patients with inde-
Female
Female
Female
Female
Female
Sex
terminate aspirates. Published reports confirm the
Male
Male
high operative efficacy in surgical removal of thy-
roid cancer, but with a 2 to 10% rate of long-term
Patient
No.
morbidity from the procedure.9-11 Thus, surgery
3
4
5
6
7
1
2
should ideally be reserved for therapeutic pur-
8 n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
Cytologically Indeterminate Thyroid Nodules
A Cytokeratin 19 B CITED1
Intensity difference, 1.9; P<0.001 Intensity difference, 3; P<0.001
6 54 53 6 54 53
13 13
12 12
11 11
Intensity (log2)
Intensity (log2)
10 10
9 9
8 8
7 7
6 6
5 5
Cyto-I, Cyto-I, Cyto-M, Cyto-I, Cyto-I, Cyto-M,
Benign Suspicious Suspicious Benign Suspicious Suspicious
C Cytokeratin 7 D Thyrotropin Receptor
Intensity difference, 1.6; P<0.001 Intensity difference, 1.4; P=0.004
6 54 53 6 54 53
13 13
12 12
11 11
Intensity (log2)
Intensity (log2)
10 10 30%
30% 20%
9 20% 9
8 10% 8 10%
7 7
6 6
5 5
Cyto-I, Cyto-I, Cyto-M, Cyto-I, Cyto-I, Cyto-M,
Benign Suspicious Suspicious Benign Suspicious Suspicious
E Thyroglobulin F TTF-1
Intensity difference, 0.5; P=0.25 Intensity difference, 1.9; P<0.001
6 54 53 6 54 53
13 13
12 30% 12
20%
11 11
10%
Intensity (log2)
Intensity (log2)
10 10
9 9
30%
8 8 20%
7 7 10%
6 6
5 5
Cyto-I, Cyto-I, Cyto-M, Cyto-I, Cyto-I, Cyto-M,
Benign Suspicious Suspicious Benign Suspicious Suspicious
poses. The risk of cancer with a benign result on for follicular neoplasm is similar to the risk as-
gene-expression classifier testing for nodules clas- sociated with thyroid nodules that have benign
sified cytologically as atypia (or follicular lesions) cytologic features. Furthermore, implementation
of undetermined significance and for those classi- of the classifier in routine practice may afford cost
fied as follicular neoplasms or lesions suspicious savings, with a modest increase in quality-adjust-
n engl j med nejm.org 9
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
ed life-years, primarily by reducing unnecessary solute. Furthermore, five of six false negative re-
surgical resection.21 sults for papillary thyroid carcinoma occurred in
A key strength of this investigation is the in- samples for which the classifier failed to show
clusion of a wide range of community and aca- independent molecular signatures of papillary thy-
demic practice settings, geographic regions, and roid carcinoma and follicular content. This sug-
demographic characteristics of patients. Further- gests that aspects of nodule sampling such as the
more, we used local cytopathological reports to technique of fine-needle aspiration or the cellu-
classify nodules as having indeterminate cyto- lar heterogeneity of the nodule may contribute to
logic features, and although these reports were inaccurate results.33 Finally, the prevalence of can-
reviewed by a central panel of expert cytopatholo- cer in the study (32%) may differ from the preva-
gists to confirm the indeterminate classifica- lence previously reported in clinical practice,3,16
tion, our results reflect test performance based affecting estimates of the negative predictive val-
on local cytopathological assessment. This ap- ue. For example, a recent large study showed a 24%
proach makes the findings applicable to every- prevalence of cancer in clinical practice,16 and if
day patient care. With more than 4000 samples that prevalence is applied to this study, the over-
collected, the gene-expression classifier was vali- all negative predictive value increases to 95%.
dated on more than 12 benign and malignant In summary, this study shows that a gene-
histologic subtypes.32 Despite the study’s strengths, expression classifier can be used to identify a
such a protocol also uncovers several immutable subpopulation of patients with a low likelihood
realities, creating a practical limit to the test’s of cancer in a population of patients for whom
perfection. For example, even with histopathologi- diagnostic surgery is otherwise recommended.
cal analysis by leading experts, independent clas- Though each clinical decision must be individual-
sifications were discordant in 14% of cases (with a ized, these data suggest consideration of a more
discordance rate of 2% after the experts con- conservative clinical approach for patients who
ferred). Since this served as the reference standard have nodules with indeterminate cytologic fea-
against which the gene-expression classifier was tures on fine-needle aspiration and a benign re-
measured, the imperfect interobserver agreement sult on gene-expression classifier testing.
may have affected the sensitivity or specificity of Supported by research grants to the individual study institu-
tions from Veracyte.
the classifier, since pathological assessment of Disclosure forms provided by the authors are available with
benign versus malignant disease is not always ab- the full text of this article at NEJM.org.
References
1. Siegel R, Naishadham D, Jemal A. 6. Baloch ZW, Cibas ES, Clark DP, et al. low-risk papillary thyroid carcinoma.
Cancer statistics, 2012. CA Cancer J Clin The National Cancer Institute thyroid fine Arch Otolaryngol Head Neck Surg
2012;62:10-29. needle aspiration state of the science con- 2007;133:1245-53.
2. Gharib H, Papini E, Paschke R, et al. ference: a summation. Cytojournal 2008; 12. Esnaola NF, Cantor SB, Sherman SI,
American Association of Clinical Endo- 5:6. Lee JE, Evans DB. Optimal treatment
crinologists, Associazione Medicie Endo- 7. Cibas ES, Syed AZ. The Bethesda Sys- strategy in patients with papillary thyroid
crinologi, and European Thyroid Associa- tem for reporting thyroid cytopathology. cancer: a decision analysis. Surgery 2001;
tion medical guidelines for clinical Am J Clin Pathol 2009;132:658-65. 130:921-30.
practice for the diagnosis and manage- 8. Bryson PC, Shores CG, Hart C, et al. 13. Hundahl SA, Cady B, Cunningham
ment of thyroid nodules: executive sum- Immunohistochemical distinction of fol- MP, et al. Initial results from a prospec-
mary of recommendations. J Endocrinol licular thyroid adenomas and follicular tive cohort study of 5583 cases of thyroid
Invest 2010;33:Suppl:51-6. carcinomas. Arch Otolaryngol Head Neck carcinoma treated in the United States
3. Yassa L, Cibas ES, Benson CB, et al. Surg 2008;134:581-6. during 1996: an American College of Sur-
Long-term assessment of a multidisci- 9. Bergenfelz A, Jansson S, Kristoffers- geons Commission on Cancer Patient Care
plinary approach to thyroid nodule diag- son A, et al. Complications to thyroid sur- Evaluation Study. Cancer 2000;89:202-17.
nostic evaluation. Cancer 2007;111:508-16. gery: results as reported in a database 14. Moses W, Weng J, Sansano I, et al.
4. Cooper DS, Doherty GM, Haugen BR, from a multicenter audit comprising Molecular testing for somatic mutations
et al. Revised American Thyroid Associa- 3,660 patients. Langenbecks Arch Surg improves the accuracy of thyroid fine-
tion management guidelines for patients 2008;393:667-73. needle aspiration biopsy. World J Surg
with thyroid nodules and differentiated 10. Sosa JA, Bowman HM, Tielsch JM, 2010;34:2589-94.
thyroid cancer. Thyroid 2009;19:1167-214. Powe NR, Gordon TA, Udelsman R. The 15. Ferraz C, Eszlinger M, Paschke R.
[Erratum, Thyroid 2010;20:674-5.] importance of surgeons experience for Current state and future perspective of
5. Wang CC, Friedman L, Kennedy GC, clinical and economic outcomes from thy- molecular diagnosis of fine-needle aspi-
et al. A large multicenter correlation study roidectomy. Ann Surg 1998;228:320-30. ration biopsy of thyroid nodules. J Clin
of thyroid nodule cytopathology and his- 11. Shrime MG, Goldstein DP, Seaberg Endocrinol Metab 2011;96:2016-26.
topathology. Thyroid 2011;21:243-51. RM, et al. Cost effective management of 16. Nikiforov YE, Ohori NP, Hodak SP, et
10 n engl j med nejm.org
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
Cytologically Indeterminate Thyroid Nodules
al. Impact of mutational testing on the J Clin Endocrinol Metab 2011;96(11): Nagaraja HN, de la Chapelle A, Kloos RT.
diagnosis and management of patients E1719-E1726. Galectin-3, fibronectin-1, CITED-1, HBME1
with cytologically indeterminate thyroid 22. Eszlinger M, Paschke R. Molecular and cytokeratin-19 immunohistochemis-
nodules: a prospective analysis of 1056 fine-needle aspiration biopsy diagnosis of try is useful for the differential diagnosis
FNA samples. J Clin Endocrinol Metab thyroid nodules by tumor specific muta- of thyroid tumors. Mod Pathol 2005;18:48-
2011;96:3390-7. tions and gene expression patterns. Mol 57.
17. Nikiforov YE, Steward DL, Robinson- Cell Endocrinol 2010;322:29-37. 29. Fischer S, Asa SL. Application of im-
Smith TM, et al. Molecular testing for mu- 23. Chudova D, Wilde JI, Wang ET, et al. munohistochemistry to thyroid neo-
tations in improving the fine-needle aspi- Molecular classification of thyroid nod- plasms. Arch Pathol Lab Med 2008;132:
ration diagnosis of thyroid nodules. J Clin ules using high-dimensionality genomic 359-72.
Endocrinol Metab 2009;94:2092-8. data. J Clin Endocrinol Metab 2010;95: 30. Lewis CM, Chang K-P, Pitman M, Fa-
18. Kim ES, Kim TY, Koh JM, et al. Com- 5296-304. quin WC, Randolph GW. Thyroid fine-
pletion thyroidectomy in patients with 24. Whiting PF, Rutjes AW, Westwood needle aspiration biopsy: variability in re-
thyroid cancer who initially underwent ME, et al. QUADAS-2: a revised tool for porting. Thyroid 2009;19:717-23.
unilateral operation. Clin Endocrinol the quality assessment of diagnostic ac- 31. Bilimoria KY, Bentrem DJ, Ko CY, et
(Oxf) 2004;61:145-8. curacy studies. Ann Intern Med 2011; al. Extent of surgery affects survival for
19. Hu S, Ewertz M, Tufano RP, et al. De- 155:529-36. papillary thyroid cancer. Ann Surg 2007;
tection of serum deoxyribonucleic acid 25. Bossuyt PM, Reitsma JB, Bruns DE, et 246:375-81.
methylation markers: a novel diagnostic al. Towards complete and accurate report- 32. Prasad NB, Somervell H, Tufano RP,
tool for thyroid cancer. J Clin Endocrinol ing of studies of diagnostic accuracy: the et al. Identification of genes differentially
Metab 2006;91:98-104. STARD initiative. Am J Clin Pathol 2003; expressed in benign versus malignant
20. Milas M, Shin J, Gupta M, et al. Circu- 119:18-22. thyroid tumors. Clin Cancer Res 2008;14:
lating thyrotropin receptor mRNA as a 26. Altman DG, Bland JM. Diagnostic 3327-37.
novel marker of thyroid cancer: clinical tests 2: predictive values. BMJ 1994;309: 33. Fusco A, Gennaro C, Hui P, et al. As-
applications learned from 1758 samples. 102. sessment of RET/PTC oncogene activation
Ann Surg 2010;252:643-51. 27. Banks ND, Kowalski J, Tsai HL, et al. and clonality in thyroid nodules with in-
21. Li H, Robinson KA, Anton B, Sal- A diagnostic predictor model for indeter- complete morphological evidence of pap-
danha IJ, Ladenson PW. Cost-effective- minate or suspicious thyroid FNA sam- illary carcinoma. Am J Pathol 2002;160:
ness of a novel molecular test for cyto- ples. Thyroid 2008;18:933-41. 2157-67.
logically indeterminate thyroid nodules. 28. Prasad ML, Pellegata NS, Huang Y, Copyright © 2012 Massachusetts Medical Society.
n engl j med nejm.org 11
The New England Journal of Medicine
Downloaded from nejm.org on July 4, 2012. For personal use only. No other uses without permission.
Copyright © 2012 Massachusetts Medical Society. All rights reserved.
You might also like
- The Bethesda System for Reporting Thyroid Cytopathology: Definitions, Criteria and Explanatory NotesFrom EverandThe Bethesda System for Reporting Thyroid Cytopathology: Definitions, Criteria and Explanatory NotesNo ratings yet
- Nej Mo A 1203208Document11 pagesNej Mo A 1203208Iustin TudorNo ratings yet
- Chromosomal Microarray Versus Karyotyping For Prenatal Diagnosis - 2012Document10 pagesChromosomal Microarray Versus Karyotyping For Prenatal Diagnosis - 2012George CarvalhoNo ratings yet
- Molecular Testing of Thyroid NodulesDocument7 pagesMolecular Testing of Thyroid Nodulesayodeji78No ratings yet
- 2013 Clinical WES Nejmoa1306555Document10 pages2013 Clinical WES Nejmoa1306555MCuk2606No ratings yet
- 10b. Diagnosis Journal Review - Colorectal Cancer Screening NEJMDocument11 pages10b. Diagnosis Journal Review - Colorectal Cancer Screening NEJMPPDSNeurologiAgustus 2021No ratings yet
- Andressa Barreto Glaeser Bruna Lixinski Diniz Desirée Deconte Andressa Schneiders Santos Rafael Fabiano Machado Rosa Paulo Ricardo Gazzola ZenDocument9 pagesAndressa Barreto Glaeser Bruna Lixinski Diniz Desirée Deconte Andressa Schneiders Santos Rafael Fabiano Machado Rosa Paulo Ricardo Gazzola ZenLaura Sanchez SuarezNo ratings yet
- Molecular Testing For Thyroid Nodules: Review and Current StateDocument11 pagesMolecular Testing For Thyroid Nodules: Review and Current StateSilvina VernaNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofSuwandi ChangNo ratings yet
- Ebell 2016Document8 pagesEbell 2016Neurobites ESLNo ratings yet
- Achondroplasia Natural History Study (CLARITY)Document7 pagesAchondroplasia Natural History Study (CLARITY)jakelinelagoadvNo ratings yet
- Cytologic Patterns of Cervical Adenocarcinomas With Emphasis On Factors Associated With Underdiagnosis - Tumor DiathesisDocument9 pagesCytologic Patterns of Cervical Adenocarcinomas With Emphasis On Factors Associated With Underdiagnosis - Tumor Diathesisnakemi111No ratings yet
- Clinical Whole-Exome Sequencing For The Diagnosis of Mendelian DisordersDocument10 pagesClinical Whole-Exome Sequencing For The Diagnosis of Mendelian DisordersdssadkjlNo ratings yet
- Genome Sequencing As An Alternative To Cytogenetic Analysis in Myeloid CancersDocument12 pagesGenome Sequencing As An Alternative To Cytogenetic Analysis in Myeloid CancersJck YyNo ratings yet
- ORATORIO Ocrelizumab EMPPDocument12 pagesORATORIO Ocrelizumab EMPPalmarazneurologiaNo ratings yet
- AMP CancerDocument20 pagesAMP Cancerprateek bhatiaNo ratings yet
- Biswas2014 PDFDocument7 pagesBiswas2014 PDFDhruv MahajanNo ratings yet
- Journal Medicine: The New EnglandDocument11 pagesJournal Medicine: The New EnglandMohiuddin JishanNo ratings yet
- Molecular Testing For Thyroid Nodules: Review and Current StateDocument11 pagesMolecular Testing For Thyroid Nodules: Review and Current Statenaili nsnNo ratings yet
- Faustino 2008Document7 pagesFaustino 2008AbdelazizSeliemNo ratings yet
- Argani 2000Document15 pagesArgani 2000karen.cobenaNo ratings yet
- ShearWave Elastography Thyroid NodulesDocument8 pagesShearWave Elastography Thyroid Nodulesinfo8089No ratings yet
- Circulating Tumor Cells, Disease Progression, and Survival in Metastatic Breast CancerDocument11 pagesCirculating Tumor Cells, Disease Progression, and Survival in Metastatic Breast CancerwardaninurindahNo ratings yet
- The Diagnostic Criteria For Chronic EndometritisDocument7 pagesThe Diagnostic Criteria For Chronic EndometritisyuriescaidaNo ratings yet
- A Genomic StrategyDocument11 pagesA Genomic StrategyAmirahShalehaNo ratings yet
- Estudo Transversal HPV e Cancer - Lancet 1987Document4 pagesEstudo Transversal HPV e Cancer - Lancet 1987rafuxu22No ratings yet
- Cytogenetic Profile Predicts Prognosis of Patients With Clear Cell Renal Cell CarcinomaDocument8 pagesCytogenetic Profile Predicts Prognosis of Patients With Clear Cell Renal Cell CarcinomaRivan 21No ratings yet
- A H. S, MD, P D D S. G, MD B L. G, MD J W. K, MD C L. S, MD B P. M, MD S E. P, MD, P D P C - B, MDDocument2 pagesA H. S, MD, P D D S. G, MD B L. G, MD J W. K, MD C L. S, MD B P. M, MD S E. P, MD, P D P C - B, MDisandi rayandikaNo ratings yet
- Association of Plasma Biomarkers of Alzheimer Disease With Cognition and Medical Comorbidities in A Biracial CohortDocument10 pagesAssociation of Plasma Biomarkers of Alzheimer Disease With Cognition and Medical Comorbidities in A Biracial CohortPei-Hao ChenNo ratings yet
- The Alzheimer's Disease Neuroimaging Initiative - ArticleDocument68 pagesThe Alzheimer's Disease Neuroimaging Initiative - ArticleacbgdvNo ratings yet
- Cancer de PancreasDocument12 pagesCancer de PancreasRuben RoaNo ratings yet
- Provenge 2Document12 pagesProvenge 2api-675909478No ratings yet
- Detrano 1989Document7 pagesDetrano 1989Lilims LilithNo ratings yet
- HydrocephalusDocument9 pagesHydrocephalusDeby AnditaNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofPedro BurgosNo ratings yet
- Chung Et Al 2022 Solitary Fibrous Tumors of The Head and Neck A Single Institution Study of 52 PatientsDocument7 pagesChung Et Al 2022 Solitary Fibrous Tumors of The Head and Neck A Single Institution Study of 52 PatientsOumaima Ben KhalifaNo ratings yet
- Developing Best-Practice Models For The Therapeutic Use of Extracellular VesiclesDocument10 pagesDeveloping Best-Practice Models For The Therapeutic Use of Extracellular VesicleschenNo ratings yet
- Research Article: The Bethesda System For Reporting Thyroid Cytopathology: A Cytohistological StudyDocument8 pagesResearch Article: The Bethesda System For Reporting Thyroid Cytopathology: A Cytohistological StudyAbdullah KhalilNo ratings yet
- SGCE and Myoclonus Dystonia: Motor Characteristics, Diagnostic Criteria and Clinical Predictors of GenotypeDocument9 pagesSGCE and Myoclonus Dystonia: Motor Characteristics, Diagnostic Criteria and Clinical Predictors of GenotypeTalib AdilNo ratings yet
- Cystic Lesions of The Pituitary Clinicopathological Features Distinguishing Craniopharyngioma, Rathke - S Cleft Cyst, and Arachnoid Cyst, 1999Document11 pagesCystic Lesions of The Pituitary Clinicopathological Features Distinguishing Craniopharyngioma, Rathke - S Cleft Cyst, and Arachnoid Cyst, 1999CAMILO ARMANDO BENAVIDES BURBANONo ratings yet
- Criterios LESDocument10 pagesCriterios LESVALENTINA ARISTIZABAL MONTOYANo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofCristhian del CidNo ratings yet
- Bloodadvances 2022007569Document20 pagesBloodadvances 2022007569Yilianeth Mena DazaNo ratings yet
- Kim 2017Document14 pagesKim 2017Cota AncutaNo ratings yet
- Nejme 2400102Document3 pagesNejme 2400102linjingwang912No ratings yet
- 352 FullDocument3 pages352 FullAlexandria Firdaus Al-farisyNo ratings yet
- Preanalytics and Precision PathologyDocument18 pagesPreanalytics and Precision Pathologyedward100% (1)
- David A Goldfarb Renal Transplantation 2021Document2 pagesDavid A Goldfarb Renal Transplantation 2021alan.rangel.puenteNo ratings yet
- Clinical Features of Childhood Primary Ciliary Dyskinesia byDocument9 pagesClinical Features of Childhood Primary Ciliary Dyskinesia byMarcellaNo ratings yet
- Lahat2010 AngiosarcomaDocument9 pagesLahat2010 AngiosarcomaAntania IsyatiraNo ratings yet
- Histopathologic and Clinical Features of Medullary Microcarcinoma and C-Cell Hyperplasia in Prophylactic Thyroidectomies For Medullary CarcinomaDocument7 pagesHistopathologic and Clinical Features of Medullary Microcarcinoma and C-Cell Hyperplasia in Prophylactic Thyroidectomies For Medullary CarcinomaFeliciaFala-NeguleanuNo ratings yet
- Diagnostic Yield of Cytopathology in Evaluating Pericardial Effusions: Clinicopathologic Analysis of 419 SpecimensDocument10 pagesDiagnostic Yield of Cytopathology in Evaluating Pericardial Effusions: Clinicopathologic Analysis of 419 SpecimensAnca CucuNo ratings yet
- Development of iPSC-based Clinical Trial Selection Platform For Patients With Ultrarare DiseasesDocument17 pagesDevelopment of iPSC-based Clinical Trial Selection Platform For Patients With Ultrarare DiseasesValen EstevezNo ratings yet
- 1 - Colorectal CancerDocument11 pages1 - Colorectal CancerNatnicha foongfaNo ratings yet
- Cervical Cytology of Atypical Squamous Cells Cannot Exclude High-Grade SquamousDocument5 pagesCervical Cytology of Atypical Squamous Cells Cannot Exclude High-Grade SquamousInsan FitriyaniNo ratings yet
- Thyroid Nodules Diagnostic Evaluation Based OnDocument20 pagesThyroid Nodules Diagnostic Evaluation Based Ondiaspalma.medNo ratings yet
- Decision Making For Diagnosis and Management: Algorithms From Experts For Molecular TestingDocument15 pagesDecision Making For Diagnosis and Management: Algorithms From Experts For Molecular TestingFadi Al HajjiNo ratings yet
- Impact of Tumor Location On Nodal Evaluation of Colon Cancer 12 Lymph Nodes 2008Document8 pagesImpact of Tumor Location On Nodal Evaluation of Colon Cancer 12 Lymph Nodes 2008MARIO DCARLO TREJO HUAMANNo ratings yet
- OPERA OcrelizumabDocument14 pagesOPERA OcrelizumabalmarazneurologiaNo ratings yet
- Assessment of Tumor Infiltrating Lymphocytes Using.12Document9 pagesAssessment of Tumor Infiltrating Lymphocytes Using.12Muhammad Rifki100% (1)
- Thyroid Fine Needle Aspirate - A Post-Bethesda UpdateDocument10 pagesThyroid Fine Needle Aspirate - A Post-Bethesda UpdateLaraNo ratings yet
- Study of The Histological Profile of Papillary Thyroid Carcinomas Associated With Hashimoto's ThyroiditisDocument5 pagesStudy of The Histological Profile of Papillary Thyroid Carcinomas Associated With Hashimoto's ThyroiditisLaraNo ratings yet
- 2015 Doorbar2015 Human Papillomavirus Molecular Biology and Disease Association PDFDocument22 pages2015 Doorbar2015 Human Papillomavirus Molecular Biology and Disease Association PDFLaraNo ratings yet
- Management of Cervical Cytologic Abnormalities PDFDocument12 pagesManagement of Cervical Cytologic Abnormalities PDFLaraNo ratings yet
- Jurnal MeiristaDocument8 pagesJurnal Meiristameirista deviNo ratings yet
- Gac 311 NotesDocument26 pagesGac 311 NotesZAINABU OLANDONo ratings yet
- Rmu Surgery OspesDocument110 pagesRmu Surgery OspesHumna YounisNo ratings yet
- 5 Malado Guillain Barre SyndromeDocument7 pages5 Malado Guillain Barre SyndromeAllan CastroNo ratings yet
- APA Guidelines On The Prevention of Postoperative Vomiting in ChildrenDocument35 pagesAPA Guidelines On The Prevention of Postoperative Vomiting in ChildrenMaria Lucia RossiNo ratings yet
- CausationDocument5 pagesCausationmonique swanepoelNo ratings yet
- Malignant Hypertension: Hypertensive EmergenciesDocument7 pagesMalignant Hypertension: Hypertensive EmergenciesAbdul QuyyumNo ratings yet
- Gerson - The Little Enema BookDocument36 pagesGerson - The Little Enema BookBruno GonçalvesNo ratings yet
- 2020 09 - OCME Overdose ReportDocument10 pages2020 09 - OCME Overdose ReportJoe EskenaziNo ratings yet
- Hemolytic Disease of NewbornDocument15 pagesHemolytic Disease of Newborncyphochilus100% (1)
- Thyroid Disease Anesthetic ConsiderationsDocument30 pagesThyroid Disease Anesthetic ConsiderationsmirzaoctaNo ratings yet
- Biographic Data: Nursing Health HistoryDocument14 pagesBiographic Data: Nursing Health HistoryMae Jane AuzaNo ratings yet
- Ba Zhen Tang - 八珍湯 - Eight Treasures Decoction - Dang Gui and Ginseng Eight Combination - Chinese Herbs - American Dragon - Dr Joel Penner OMD, LAcDocument10 pagesBa Zhen Tang - 八珍湯 - Eight Treasures Decoction - Dang Gui and Ginseng Eight Combination - Chinese Herbs - American Dragon - Dr Joel Penner OMD, LAcangelesarenasNo ratings yet
- 2021 All Product Catalog - 20210601 - LowDocument87 pages2021 All Product Catalog - 20210601 - LowSridevi AnggrainiNo ratings yet
- Department of Medicine Report 2019Document49 pagesDepartment of Medicine Report 2019Taylor LaframboiseNo ratings yet
- Scalp Acupuncture Treatment Protocol For Anxiety Disorders: A Case ReportDocument6 pagesScalp Acupuncture Treatment Protocol For Anxiety Disorders: A Case ReportTanuku NetNo ratings yet
- Crocus Sativus L. (Saffron) in The Treatment of Premenstrual Syndrome: A Double-Blind, Randomised and Placebo-Controlled TrialDocument5 pagesCrocus Sativus L. (Saffron) in The Treatment of Premenstrual Syndrome: A Double-Blind, Randomised and Placebo-Controlled TrialhanaNo ratings yet
- Superficial and Deep Perivascular DermatitisDocument55 pagesSuperficial and Deep Perivascular DermatitisMarnie RoviraNo ratings yet
- GalactocelesDocument7 pagesGalactocelescleric25No ratings yet
- PhysioEx Exercise 7 Activity 1Document6 pagesPhysioEx Exercise 7 Activity 1Jorge CuevaNo ratings yet
- Hla B27Document8 pagesHla B27swamy cheekatlaNo ratings yet
- 151602106-PGI Rohtak-Sushmita Singh Case StudyDocument11 pages151602106-PGI Rohtak-Sushmita Singh Case Studysushmita singhNo ratings yet
- Medical Examination Rules 2005Document12 pagesMedical Examination Rules 2005MutuajmNo ratings yet
- Fat: An Emerging Player in The Field of Atrial FibrillationDocument4 pagesFat: An Emerging Player in The Field of Atrial FibrillationKevinJuliusTanadyNo ratings yet
- Slle Examination Content Guideline - March 05 PDFDocument16 pagesSlle Examination Content Guideline - March 05 PDFYahya Alkamali100% (1)
- Dissociative Identity DisorderDocument10 pagesDissociative Identity DisorderRizza Erika La Torre-FernandezNo ratings yet
- Medical History Assessment FormDocument1 pageMedical History Assessment FormzarinaNo ratings yet
- The Scoring Clinical Index For OnychomycosisDocument4 pagesThe Scoring Clinical Index For OnychomycosisPatricia Avalos C.No ratings yet
- The Kaohsiung J of Med Scie - 2013 - Tsai - Pyoderma Gangrenosum Intractable Leg Ulcers in Sjogren S SyndromeDocument2 pagesThe Kaohsiung J of Med Scie - 2013 - Tsai - Pyoderma Gangrenosum Intractable Leg Ulcers in Sjogren S SyndromeAsad KakarNo ratings yet
- Oxygen Toxicity - Signs and SymptomsDocument4 pagesOxygen Toxicity - Signs and SymptomsYoga SemadhiNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (23)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)