Professional Documents
Culture Documents
11 - Sexually Transmitted Diseases
Uploaded by
Kaela Beatrice Sy LatoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
11 - Sexually Transmitted Diseases
Uploaded by
Kaela Beatrice Sy LatoCopyright:
Available Formats
👫
Sexually Transmitted Diseases
are infections that are passed from one person to another through sexual contact
infection
w MO but no sx
most commonly used in the medical field
px can be contagious and carry the potential for the disease to develop
not all STIs could develop into a disease
disease
w MO and w sx
all STDs are preceded by STI
Causes
bacteria, parasites, yeast, and viruses
most STDs affect both men and women, but in many cases, the health problem they
cause can be more severe in women
pregnant woman and have STD → serious health problem in babies
reproductive system in women is more complex → a lot of target sites and
organs for diseases to develop
STDs
Syphilis
Gonorrhea
Chlamydia
Genital Herpes
Human Papilloma Virus
Sexually Transmitted Diseases 1
Trichomoniasis
caused by a protozoan (parasite)
women → foul-smelling vaginal discharge, genital itching, painful
urination
treatment = Metronidazole 500mg bid for 7d
men → typically don't have sx
treatment = Metronidazole 2g sid po for 7d
alternative for metronidazole = Tinidazole 2g po sid
📌 there are more than 20 different types of STIs
Syphilis
aka The Great Imitator
sx will look like other diseases
can be mistakenly diagnosed if you are just looking at the manifestation
Causative agent
Treponema pallidum
cork-screw shaped spirochete
thrives in moist regions of the body and survives and reproduces only
when there is very little O2 present
easily killed by heat, drying, sunlight, disinfectants
cant be infected by having contact w toilet seats, contaminated bath
towels, or beddings
can live in collected blood for 24 hrs
rare cases of transmission during blood transfusion
Transmission
Sexually Transmitted Diseases 2
only about 1 in 10 people exposed to the bacterium will develop syphilis
ppl w syphilis can acquire HIV more easily and are transmitted to others
Close personal contact
Sexual contact — horizontal spread
9 out of 10 cases of Syphilis
Transplacental infection of the fetus — vertical spread
mother → baby
Enters minute abrasions/mucous membrane
There are 4 types of Treponema spp.
venereal
T. pallidum
sexual contact
nonvenereal/endemic trepanomatoses
nonsexual diseases
other 3 spp.
Incubation Period — 3 weeks
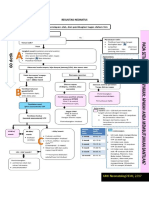
4 Stages of T. pallidum infection (Primary, Secondary, Latent, Tertiary)
not all patients go through all stages
can infect the genitalia, anus, urethra, lips, mouth
Primary Stage
positive for lesions
chancre — 3 weeks after infection
can take up to 90 days
highly contagious cuz the open wound is steaming w
spirochetes
Sexually Transmitted Diseases 3
SIGNS AND SYMPTOMS
Swelling of the groins in the glands but not usually sore or tender
painless sore or open sore — aka wet ulcer — will develop
one to a few chancres
Sore heals after a few weeks without treatment
lasts for 3-6 weeks w/o treatment
chancres can appear in the genitalia, cervix, lips, mouth, anus
swollen glands
Transmission
contact w the ulcer
highly contagious stage = presence of open sores
if pregnant → can cross the placenta (ToRCHeS)
birth defect, stillbirth, miscarriage
Secondary Stage
Sexually Transmitted Diseases 4
the latent period of 3-30 yrs
other symptoms appear 3-6 weeks after the sores appear
after open sores heal
SIGNS AND SYMPTOMS
headaches, general aches
loss of appetite and maybe a fever
fatigue, sore throat, weight loss, swollen glands, muscle pain
dark red rash for a few weeks or months (backs, legs, arms, hands,
feet)
body rash that will last for 2-6 weeks (palms of the hands and
soles of the feet)
Latent (hidden) Stage
1 out of 3 ppl who had untreated syphilis could suffer serious damage to
the nervous system
MO can go to the heart, brain, and other organs
Latent syphilis can last for years
occurs 1-20 years after the start of the infection
a period of time when there are no visible signs or symptoms of syphilis
cuz sores and rashes have already gone, but still have the infection
Sexually Transmitted Diseases 5
Without tx, the infected person will continue to have syphilis in their
body even though there are no signs or symptoms.
Early latent infection occurred within the past 12 months
early 12 months
Late latent syphilis is where infection occurred more than 12 months ago
late 12 months
important to know the stage cuz tx may differ among the stages
Tertiary Stage
disease may recur
painful permanent ulcers on the skin
lesions on ligaments, joints, and on bones
can attack the nervous system, the heart, and blood vessels that results in
blindness, paralysis, and insanity
neurosyphilis — invasion of the nervous system
at any stage of the infection, syphilis can invade the nervous
system and cause a wide range of symptoms including altered
behavior, headache, difficulty in coordinating muscle movements,
paralysis, sensory deficits, dementia
ocular syphilis can also occur at any stage of the infection
involve almost any eye structure
vision changes, decrease in visual acuity, permanent blindness
Congenital Syphilis
It is acquired after the 1st three months of pregnancy
pregnant mother → fetus or unborn baby
can result in stillbirth, prematurity, and a wide spectrum of clinical
manifestations
Manifestations
Sexually Transmitted Diseases 6
Serious infection resulting in intrauterine death
Congenital abnormalities, which may be obvious at birth
Silent infection, which may not be apparent until about two years of age
Diagnosis
T. pallidum can’t be grown in vitro
exception of Koch‘s Postulates
obligate internal parasite
requires a mammalian host to survive
absence of mammalian cells, T. pallidum will be killed by the absence of
nutrients, exposed to heat and O2
rabbits are the animal model that is almost exclusively studied in the
laboratory
monkeys are expensive
unlike mice, rabbits develop the s/sx of human primary and
secondary syphilis
testes of rabbits were shown to be particularly susceptible to T.
pallidum infection
📌 the Wassermann reaction for syphilis – actually utilizes a
nontreponemal lipid antigen, cardiolipin, and measures an antibody
that is incapable of interacting with the offending pathogen
Microscopic identification
Dark-field microscopy
Direct fluorescent antibody testing on the specimen (lesions, placenta,
umbilical cord)
Can’t be seen in gram stain
nucleic acid-based amplification assay
Sexually Transmitted Diseases 7
PCR (polymerase chain reaction) that are used in specialized labs
Serology for screening
VDRL
RPR
Non-Specific Tests
VDRL — Venereal Disease Research Lab
measures the Ab produced when the px comes in contact w T. pallidum
RPR — Rapid Plasma Reagin
measures the Ab
check the progress of tx for active syphilis
after the course of effective antibiotic therapy
see the number of Ab dropping cuz of the lower number of T.
pallidum
antigens are not in treponemal in origin — allows the detection of
antibodies
blood or spinal fluid samples
not specific — can detect HIV, malaria, lupus, and certain types of
pneumonia
need confirmatory test if (+) result
Shows (+) result within 4-6 wks of infection (or 1-2 wks after the primary
chancre appears)
Sexually Transmitted Diseases 8
A negative test is normal = no Ab present
doesn't necessarily mean the px doesn't have syphilis cuz the Ab may not
be detectable during the early period
not detectable up to 3 months after the infection
depend on the stage of the disease
the test sensitivity to detect syphilis is high — 98% — if it is in the
middle stages
not that sensitive during the early stages
A positive test result may mean you have syphilis
If the test is positive, the next step is to confirm the results with an FTA-
ABS test, which is a more specific
need to confirm cuz it may cross-react if px have other illness
Specific Tests
Treponemal antigens extracted from T. pallidum
FTA-ABS
Fluorescent Treponemal Antibody Absorption
Px’s serum is first absorbed with nonpathogenic treponemes to
remove cross-reacting antibodies before reaction with T. pallidum
pre-absorbed px’s serum is added to the slide and if the px has
been infected w syphilis → Ab will be present → Ab will cross-
react w the antigens added (antigen containing T. pallidum)
with Direct Fluorescent Antibody Testing
a solution containing an antibody and a fluorescent dye is added
to the sample of the cell
if the organism is present in the sample, the Ab sticks and will glow
when viewed under a fluorescent microscope
glow = T. pallidum is present
Sexually Transmitted Diseases 9
considered as the confirmatory assay w high specificity and
sensitivity
TPHA
T. pallidum hemagglutination Assay
same with T. pallidum Particle Agglutination Assay (TPPA)
Confirms a (+) result with the non-specific test is truly due to syphilis
fewer false (+) results
Treatment
Drug of choice
Penicillin (Benzathine Penicillin G)
long-acting Benzathine Penicillin can cure early stages of syphilis
(primary, secondary, and early latent)
CDC recommends 3 doses of long-acting Benzathine Penicillin at
weekly intervals for late latent or latent syphilis of unknown
duration (dk if early or late)
Tetracycline or Doxycycline (for patients allergic to penicillin)
only acceptable alternatives for late latent or latent syphilis of
unknown duration
Doxycycline 100mg po bid
Tetracycline 500mg po qid for 28 days
Primary and secondary syphilis among px w HIV
Benzathine Penicillin 2.4 million units IM in a single dose
confirmed or highly probable congenital syphilis
aqueous crystalline Pen G (aka Procaine Pen G) is given via IM in a
single daily dose for 10days
if Procaine Penicillin cant be given, alternative is Tetracycline and
Doxycycline
don't give Tetracycline to babies cuz of SE so Doxycycline
Sexually Transmitted Diseases 10
A person usually cannot transmit syphilis 24 hours after starting
treatment
treatment will cure the infection but will not repair any damage that had
already been done
only prevent further damage
management of sex partners
anyone treated w syphilis should not have sex until there are sores
or rashes that are not yet completely healed cuz still contagious
even after treatment
can have reinfenction
sexual transmission of T. pallidum is thought to occur when
mucocutaneous syphilitic lesions are present
person exposed to a px having primary, secondary, or early latent syphilis
should be evaluated
inform sexual partner confidentially
need to undergo clinical and serological test for them to be treated
Gonorrhea
colloquially known as the “clap”
clap refers to the old Frecnh term “clapier”, which means brothel
gonorrhea was thought to be easily spread in these places
“Tulo” in Filipiino
common infection in young ppl
Causative agent
Neisseria gonorrhoeae
a gm (-) diplocococcus
Transmission
Sexually Transmitted Diseases 11
not spread by kissing, hugging, sharing of bath towels, use of swimming pools,
toilet seats, sharing of cutleries or plates cuz they cant survive outside the body
Sexual contact from person to person
Infected mother to the baby during childbirth
does not cross the placenta
only when they pass thru the birth canal
Risk of Infection after single intercourse:
50% — women
acquisition site involves multiple mucosal sites in the lower female
genitalia (urethra, cervix, bartholin glands, ractal, pharynx, conjunctiva)
20% — men
Symptoms
sometimes, ggonorrhea may not exhibit symptoms but can cause serious health
problems even w/o sx
Develops within 2-7 days of infection
Women –— almost always asymptomatic (or mild sx) — or usually mistaken
as a bladder or milder vaginal infection
vaginal discharge
pelvic inflammatory disease (PID)
many organs in the reproductive system are inflamed
Chronic pelvic pain
heavy bleeding during menstruation, bleeding between menstrual periods,
pain during sexual contact, pain or burning when passing urine
Men — urethral discharge (TULO) and dysuria
Infertility
especially in women (PID)
Sexually Transmitted Diseases 12
infection in women’s reproductive organs above the cervix,
nagkakaroon ng damage or inflammation in the fallopian tubes or
ovary
untreated gonorrhea (esp w PID) → infertility, pregnancy problem,
pelvic pain
Diagnosis
Microscopy and culture of discharges and other specimens
gm (-) intracellular diplococci
swab sample
part of the body infected (cervix, urethra, penis, rectum, throat)
urine test
gram staining
Antibiotic susceptibility test
performed cuz of the development of resistance of N. gonorrheae to a lot
of antibiotics
Serologic tests are unsatisfactory
Treatment
The incidence of resistance is increasing
recommended antibiotics
Penicillin — previously DOC of N. gonorrheae
discovered to have developed resistance mediated by plasmid
production of beta-lactamase
Ciprofloxacin
tx w quinolones (e.g. levofloxacin) — mainstay tx for N.
gonorrheae in the US
removed cuz of resistance
*Ceftriaxone
Sexually Transmitted Diseases 13
CDC recommends a single dose of 500mg IM Ceftriaxome
Alternatives
Gentamicin + Azithromycin
cephalosporin allergy
Cefixime
if Ceftriaxome is not available
Cefixime 800mg po in a single dose
Prophylactic use has no effect in preventing sexually acquired gonorrhea
Ophthalmic antibacterial agents are effective for babies born to mothers with
gonorrhea — gonorrheal ophthalmia neonatorum
Sexually Transmitted Diseases 14
Prevention if the mother is known to have gonorrhea and the baby is born
(normal or cesarean birth)
lower risk if birth thru cesarean section
C section is advised when the mother is known to have STD
Erythromycin is given immediately after birth
little risk of developing uncomplicated gonococcal infection among infants
and children
Chlamydia
most widely commonly reported STD in the US — along w Herpes
easy to cure, but when left untreated, can lead to infertility in women
Causative agent
Chlamydia trachomatis
gm (-) bacterium
infects the epithelium of the cervix, urethra, rectum, lungs, and eyes
cause of most frequently reported STD and most ppl w this infection are
asymptomatic
untreated infection → PID → infertility, ectopic pregnancy
Serotypes
A, B, Ba, C — eye infection (trachoma) → blindness
D-K — urethritis, PID, ectopic pregnancy, neonatal pneumonia or neonatal
conjunctivitis
cause genital infection and associated ocular and respiratory
infections
L1, L2, L3 — LGV (Lymphogranuloma venereum)
px may notice changes in the genital area
genital papules, ulcers, swelling of the lymph glands
Sexually Transmitted Diseases 15
Transmission
sexual intercourse
ocular-genital contact through the birth canal
Clinical Effects
most women are asymptomatic but can cause PID → urethritis, cervicitis,
salpingitis, conjunctivitis, bartholinitis
salpingitis — inflammation of the fallopian tubes
bartholinitis — infection of the Bartholin’s glands (located on either
side of the vagina behind the labia)
symptomatic in men (urethritis, epididymitis, proctitis, conjunctivitis)
epididymitis — inflammation of the epididymis (tube located at the
back of the testicle where the tube stores and carries sperm)
proctitis — inflammation of the lining of the rectum
Diagnostic Tests
cell culture
direct antigen detection (Direct EIA)
aka Enzyme Immunoassay (EIA), Enzyme-Linked Immunoassay
detection of chlamydial antigen in the specimen
microscopically
stained with fluorescein-conjugated monoclonal antibodies and viewed
by UV microscopy — direct fluorescent antibody (DFA)
fluorescein is an organic compound that is used as a synthetic
coloring agent
nucleic acid amplification test (NAAT)
amplification of the DNA that is present in Chlamydia trachomatis
more sensitive and more specific than other tests for chlamydia
performed w the use of urine from both men and women
Sexually Transmitted Diseases 16
eliminates the need for pelvic examination in women
Treatment
chinecheck if may other STI para combination ibibigay
Chlamydia is not susceptible to beta-lactam antibiotics
in pregnancy or breastfeeding
Azithromycin, Erythromycin, Amoxicillin
Doxycycline/Tetracycline — which is also recommended for patients infected
with gonorrhea
Erythromycin should be used for babies
3-5 weeks after the medication, the physician usually recommends another test
for chlamydia to ensure that the tx has been effective and the infection has
been cleared
if it is deemed safe for the px = single dose of Azithromycin, 1-week course
of Amoxicillin or Erythromycin
Genital Herpes
commonly caused by HSV through sexual contact
after the initial infection, the virus will lie dormant in the body and become reactive
several times a year
can cause pain, itching, and sores in the genital area
Sexually Transmitted Diseases 17
Causative agent
HSV1
transmitted by saliva causing oropharyngeal infection in children and
later life, after reactivation, cold sores
oral herpes → cold sores, blisters around the mouth, fever
can spread from the mouth → genitalia
HSV2
venereal route
transmitted thru sexual intercourse
Transmission
open sores
saliva from a partner w an oral herpes infection
genital fluid
skin in the oral area of a partner w oral herpes
skin in the genital area of a partner w genital herpes
Clinical Manifestations
no to mild symptoms (can go unnoticed) or mistaken for other skin conditions
(pimples)
usually appear 1 or more blisters around the genitals, mouth, and rectum
— blister outbreak
can leave a painful sore that may take a week or more to heal
Primary genital lesion (penis or vulva) 3 – 7 days after infection
Vesicles that break down to form painful ulcers
Local lymph nodes are swollen
Fever, headache, malaise
Diagnosis
Sexually Transmitted Diseases 18
ulcer swabs
ELISA method
detect and measure Ab in the blood
Ab related to the condition
screening tool before an in-depth test is ordered
sample will be added w an antigen related to the condition it is being tested
if blood has Ab → react w antigen added to the sol’n
have to check if Ab bound to the antigen by adding an enzyme
enzyme usually changes color when the Ab in the sample reacts w
the antigen
reporter enzyme — report the presence of Ab bound to antigen
by the change in color
Clinical appearance
Treatment
no cure cuz its a virus
symptomatic treatment only
Acyclovir
oral to reduce the frequency of recurrence
IV for systemic complications
Famciclovir, Valacyclovir
Human Papilloma Virus
common STI
Papillomavirus can infect the skin or mucosal surfaces
Types 6, 11, 12, 16, 18 and 31
some types can cause health problems from genital warts to severe cancer
Sexually Transmitted Diseases 19
Transmission
vaginal or anal sex
close skin to skin contact during sexual intercourse
can be contagious even w/o sx
Transmitted sexually and cause genital warts
Warts (condylomata acuminata) appear on the penis, vulva, and perianal
regions
Best removed by a laser, acetic acid wash, and cauterization
Associated with cervical cancer (types 16 and 18)
Papanicolaou
George Papanicolou pioneered the cytopathology and early cancer detection
who developed the pap smear test
A pap smear is used to detect abnormal cells which may develop into cancer
screening for cervical cancer
the doctor will insert a speculum (metal or plastic), which helps in holding
the walls of the vagina apart to allow a clear view of the cervix
sample of the mucus and cells will be scraped off from the cervix or
endocervix using a spatula or small surgical brush
Sexually Transmitted Diseases 20
sample of cells is evenly applied on a glass slide → spray a fixative →
microscopic examination
Pap smear result
(-) = normal cervical cells
(+) = abnormal or unusual cells
doesn't always mean px has cancer, needs confirmatory
depends on the type of cells
atypical squamous cell of undetermined significance
thin and flat cells that grow on the surface of a healthy cervix
squamous intraepithelial lesions
pre-cancerous
may take years to become cancerous
minor changes in the size, shapes, and characteristics of the
cells
atypical glandular cell
unclear if cancerous
further testing will be required to check if the cell is cancerous
squamous cell cancer
sure cancer
pap smear that is so abnormal that the cytologist is almost
sure that cancer is present
basta abnormal cell → doctor will perform colposcopy
procedure in which a special magnifying instrument, a
colposcope, is used to examine tissues in the cervix, vulva, and
vagina to rule out if cancer or noncancer type
A cervical examination to detect warts and other abnormal growths which
become visible as white patches of skin
Sexually Transmitted Diseases 21
STD
Sexually Transmitted Diseases 22
You might also like
- HumRep Module7 EXPLOREDocument15 pagesHumRep Module7 EXPLOREVina OringotNo ratings yet
- Case Study On SyphillisDocument18 pagesCase Study On Syphillisdia_pee100% (1)
- Sexually Transmitted DiseaseDocument3 pagesSexually Transmitted DiseaseKim FresnilloNo ratings yet
- Sexually Transmitted Diseases (STD) : Team 3 - Group 19 - Class D-2012 University of Medicine and PharmacyDocument29 pagesSexually Transmitted Diseases (STD) : Team 3 - Group 19 - Class D-2012 University of Medicine and PharmacyMikaNo ratings yet
- In WomenDocument6 pagesIn Womenkayeemperado997No ratings yet
- STD 101Document42 pagesSTD 101Clarice BedicoNo ratings yet
- Primary SyphilisDocument3 pagesPrimary SyphilisEqah TajuddinNo ratings yet
- 11 Spirochetes 130520112830 Phpapp02Document61 pages11 Spirochetes 130520112830 Phpapp02Manisanthosh KumarNo ratings yet
- Sexually Transmitted DiseasesDocument120 pagesSexually Transmitted DiseasesGliza Jane100% (4)
- High School STD: By: Monica D. DixonDocument14 pagesHigh School STD: By: Monica D. DixonMonica D DixonNo ratings yet
- SYPHILISDocument6 pagesSYPHILISKhristine Dyanne San JoaquinNo ratings yet
- Sexual Trasmission DiseaseDocument9 pagesSexual Trasmission Diseasevivekanand100% (2)
- NSTPDocument2 pagesNSTPBernadette ArrojoNo ratings yet
- 3 Percent: Ivy Marie R. Maratas BSED Mathematics 1-2 Understanding The Self (GE 1)Document8 pages3 Percent: Ivy Marie R. Maratas BSED Mathematics 1-2 Understanding The Self (GE 1)Ivy Marie MaratasNo ratings yet
- Prepared By-V.S. Krishna Prasad Slot B1: Ethics and Values Prof. Sivakumar SDocument23 pagesPrepared By-V.S. Krishna Prasad Slot B1: Ethics and Values Prof. Sivakumar SduddeanudeepNo ratings yet
- Sexually Transmitted Diseases: John Potayr E Jude Moscos ODocument19 pagesSexually Transmitted Diseases: John Potayr E Jude Moscos OJenna OlileNo ratings yet
- Biology PresentationDocument28 pagesBiology PresentationEshetu DerssehNo ratings yet
- UTS-STDs-TOMAS SF. COLARINADocument15 pagesUTS-STDs-TOMAS SF. COLARINAAngela Kim T. DaragNo ratings yet
- Being An HFLE Teacher Portfolio1Document23 pagesBeing An HFLE Teacher Portfolio1raianna rogersNo ratings yet
- Health 8: Issues and Problems Related To Human SexualityDocument14 pagesHealth 8: Issues and Problems Related To Human SexualityAizel Mae Consas /Amado HernandezNo ratings yet
- LBM 4 Genital UlcerDocument9 pagesLBM 4 Genital UlcerDhex WiesnuwNo ratings yet
- Quickly Cure Syphilis with Powerful Natural RemediesFrom EverandQuickly Cure Syphilis with Powerful Natural RemediesRating: 5 out of 5 stars5/5 (3)
- A Simple Guide to Sexually Transmitted DiseasesFrom EverandA Simple Guide to Sexually Transmitted DiseasesRating: 5 out of 5 stars5/5 (9)
- A. Gonorrhea: Sexually Transmitted InfectionDocument7 pagesA. Gonorrhea: Sexually Transmitted InfectionHeron BayaninNo ratings yet
- Session ONE-Concepts of HIV - AIDS - STIs-STDs - Public Health HygieneDocument7 pagesSession ONE-Concepts of HIV - AIDS - STIs-STDs - Public Health Hygienenzainga lukasNo ratings yet
- StdsDocument14 pagesStdsJumar Divinagracia DimpasNo ratings yet
- Sexually Transmitted Disease: Submitted By: John Philip M. Lacas (BSN Iii-D Group 3)Document30 pagesSexually Transmitted Disease: Submitted By: John Philip M. Lacas (BSN Iii-D Group 3)John Philip M. Lacas RNNo ratings yet
- Syphilis: Castro, Khristine Marie Laudencia BSNDocument8 pagesSyphilis: Castro, Khristine Marie Laudencia BSNPlan Can JoxNo ratings yet
- Health 4: "Feeling Under The Weather" Is A Phrase That Means You Are Not Feeling Well. When YouDocument10 pagesHealth 4: "Feeling Under The Weather" Is A Phrase That Means You Are Not Feeling Well. When Youpedro calungsodNo ratings yet
- Understanding Sexually Transmitted Diseases (STD) : A Guidebook To Better Sexual Health (Men) - Free EbookDocument22 pagesUnderstanding Sexually Transmitted Diseases (STD) : A Guidebook To Better Sexual Health (Men) - Free EbookDr Tan & PartnersNo ratings yet
- SyphilisDocument21 pagesSyphilisNinfa LansangNo ratings yet
- Sexually Transmitted Infections - Lecture NotesDocument10 pagesSexually Transmitted Infections - Lecture NotesMa. Loucel RodriguezNo ratings yet
- Form 2 Chap 4 DiseasesDocument15 pagesForm 2 Chap 4 Diseasesscribble_55No ratings yet
- What Is SyphilisDocument12 pagesWhat Is SyphilisBheru LalNo ratings yet
- Safe Sex No Regrets BookletDocument9 pagesSafe Sex No Regrets BookletThat Cat in the Hat.No ratings yet
- Sexually Transmitted Disesase.: Ralph Gabriel QuinalDocument16 pagesSexually Transmitted Disesase.: Ralph Gabriel QuinalJohn Michael MonteflacoNo ratings yet
- Transmision SexualDocument4 pagesTransmision SexualAMYNo ratings yet
- HEALTH 8: Communicable DiseaseDocument31 pagesHEALTH 8: Communicable DiseaseElissah S PabilonaNo ratings yet
- Basic Health Care Series: Sexually Transmitted Diseases (STD)From EverandBasic Health Care Series: Sexually Transmitted Diseases (STD)Rating: 5 out of 5 stars5/5 (1)
- Stds Causes Treatment ChancroidDocument7 pagesStds Causes Treatment ChancroidShen YeNo ratings yet
- All About SyphilisDocument13 pagesAll About Syphilisjohnaaquino12No ratings yet
- Sexually Transmitted Infections and HIV/AIDSDocument36 pagesSexually Transmitted Infections and HIV/AIDSPrabhjeet kaurNo ratings yet
- What Are Sexually Transmitted Diseases (STDS) ?Document24 pagesWhat Are Sexually Transmitted Diseases (STDS) ?Safiqah AinNo ratings yet
- STI ExamplesDocument11 pagesSTI ExamplesabcdefghiNo ratings yet
- Herpes Indicators Herpes Indicators in Woman1887scribdDocument3 pagesHerpes Indicators Herpes Indicators in Woman1887scribdMichael WhiteNo ratings yet
- STD 2023Document25 pagesSTD 2023Limuel Andrei LazoNo ratings yet
- HIV SIDA-WPS OfficeDocument12 pagesHIV SIDA-WPS OfficeJorge EugenioNo ratings yet
- Bio Project - 1 InvestigatoryDocument12 pagesBio Project - 1 Investigatoryanonymous user 345No ratings yet
- Sexually Transmitted Diseases: Krizzia Jana P. MolinaDocument20 pagesSexually Transmitted Diseases: Krizzia Jana P. MolinaKrizzia Jana MolinaNo ratings yet
- Sexually Transmitted DiseaseDocument38 pagesSexually Transmitted Diseaserana arslanNo ratings yet
- Issues and Problems Related To Human SexualityDocument23 pagesIssues and Problems Related To Human SexualityGeeya Mariel AntonioNo ratings yet
- 1 Trainer's Guide: 1.1 Learning Objectives Training Other Crew MembersDocument12 pages1 Trainer's Guide: 1.1 Learning Objectives Training Other Crew MembersГерман ЯковлевNo ratings yet
- Genital Herpe2Document5 pagesGenital Herpe2Blood Heart <3No ratings yet
- Measles, Tuberculosis and Whooping CoughDocument11 pagesMeasles, Tuberculosis and Whooping CoughPriyanka SinghNo ratings yet
- Grade 9 Why Do We Fall IllDocument43 pagesGrade 9 Why Do We Fall IllMehala Sri AurobindoNo ratings yet
- Sexually Transmitted Disease (STD)Document102 pagesSexually Transmitted Disease (STD)uhurtme100% (10)
- Sexually Transmitted Diseases Sexually Transmitted InfectionDocument35 pagesSexually Transmitted Diseases Sexually Transmitted InfectionYiğit GündüzNo ratings yet
- Syphilis Is An STD That Can Cause LongDocument3 pagesSyphilis Is An STD That Can Cause LongPaulyn BaisNo ratings yet
- Sexually Transmitted InfectionsDocument8 pagesSexually Transmitted InfectionsEmilio Antang JrNo ratings yet
- Research 1Document2 pagesResearch 1Kaela Beatrice Sy LatoNo ratings yet
- Acid-Base EquilbriaDocument67 pagesAcid-Base EquilbriaKaela Beatrice Sy LatoNo ratings yet
- Gen Bio 4 Nervous SystemDocument10 pagesGen Bio 4 Nervous SystemKaela Beatrice Sy LatoNo ratings yet
- Gen Bio 3 MuscoskeletalDocument19 pagesGen Bio 3 MuscoskeletalKaela Beatrice Sy LatoNo ratings yet
- Bio DataDocument43 pagesBio DataahilrejiNo ratings yet
- Resusitasi NeonatusDocument7 pagesResusitasi NeonatusIqbal Miftahul HudaNo ratings yet
- Cryptosporidiosis in Ruminants: Update and Current Therapeutic ApproachesDocument8 pagesCryptosporidiosis in Ruminants: Update and Current Therapeutic ApproachesDrivailaNo ratings yet
- Dade InnovinDocument7 pagesDade InnovinchaiNo ratings yet
- Temporal Bone Radiology ReadyDocument136 pagesTemporal Bone Radiology Readyadel madanyNo ratings yet
- Clinicopathologic Conference: Governor Celestino Gallares Memorial Hospital Department of Obstetrics and GynecologyDocument57 pagesClinicopathologic Conference: Governor Celestino Gallares Memorial Hospital Department of Obstetrics and GynecologyramwshNo ratings yet
- Clinical Pharma 2Document156 pagesClinical Pharma 2RebwarNo ratings yet
- Checklist - Assisting - Circulating DeliveryDocument2 pagesChecklist - Assisting - Circulating DeliveryLue Vigiem M. GuiasNo ratings yet
- RH Factor PGDocument3 pagesRH Factor PGapi-375530349No ratings yet
- Legal Aspects of MedicationDocument17 pagesLegal Aspects of MedicationRitaNo ratings yet
- Filosofi Kesehatan MasyarakatDocument4 pagesFilosofi Kesehatan MasyarakatJennilynn YusameNo ratings yet
- Standard Operating Procedure (Biochemistry - Diasys RESPONS - 910)Document17 pagesStandard Operating Procedure (Biochemistry - Diasys RESPONS - 910)Aniruddha ChatterjeeNo ratings yet
- TSH CalsetDocument2 pagesTSH CalsetovieNo ratings yet
- PHARM 315: Cheza May Baldado BS Pharm IIIDocument12 pagesPHARM 315: Cheza May Baldado BS Pharm IIIKathleen B BaldadoNo ratings yet
- A Guide For G6PDDocument4 pagesA Guide For G6PDshimeath delrosarioNo ratings yet
- Narrative Report ContentsDocument15 pagesNarrative Report ContentsGladie Ann Dela RosaNo ratings yet
- Dental Management of The Patient With HIVAIDS 2002Document6 pagesDental Management of The Patient With HIVAIDS 2002drkameshNo ratings yet
- Obstetric Nursing Study GuideDocument69 pagesObstetric Nursing Study GuideValerie100% (3)
- Pass PACES in Single AttemptDocument101 pagesPass PACES in Single AttemptSOMNATHNo ratings yet
- OB - Normal Labor and DeliveryDocument51 pagesOB - Normal Labor and DeliveryJosh Matthew Rosales33% (3)
- Medicago Sativa LloydDocument4 pagesMedicago Sativa LloydDr Rushen SinghNo ratings yet
- Pharmacology of The GIT System: CIC Ragasa, RN-MDDocument70 pagesPharmacology of The GIT System: CIC Ragasa, RN-MDCarmencita Ileen Ragasa - AhmedNo ratings yet
- 2926 Getinge Da Vinci Brochure 190301 en NonusDocument5 pages2926 Getinge Da Vinci Brochure 190301 en NonusHELIONo ratings yet
- RS5573 FONA 1000S User Manual 6476381 Ver2 201604 EN CN Reg SADocument36 pagesRS5573 FONA 1000S User Manual 6476381 Ver2 201604 EN CN Reg SAJuan carlos Isaza gNo ratings yet
- Aace - Ace - 2016 - Comprehensive Clinical Practice Guidelines For Medical Care of Patients With ObesityDocument203 pagesAace - Ace - 2016 - Comprehensive Clinical Practice Guidelines For Medical Care of Patients With ObesityLintang AdhiNo ratings yet
- 14th Century - Black DeathDocument16 pages14th Century - Black DeathJean-pierre NegreNo ratings yet
- Hirschsprung's Disease, PDFDocument1 pageHirschsprung's Disease, PDFMr. LNo ratings yet
- Yaman Walid KassabDocument282 pagesYaman Walid KassabHeryanti PusparisaNo ratings yet
- Osteoconduction and OsteoinductionDocument6 pagesOsteoconduction and OsteoinductiontofssbiNo ratings yet
- Women S Health MidtermDocument30 pagesWomen S Health MidtermKatarzyna CiesielskaNo ratings yet