Professional Documents
Culture Documents
Investigation and Differential Diagnosis of Stafne
Uploaded by
swayampradeepmohapatraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Investigation and Differential Diagnosis of Stafne
Uploaded by
swayampradeepmohapatraCopyright:
Available Formats
[Downloaded free from http://www.joomr.org on Tuesday, February 14, 2017, IP: 45.45.147.
87]
Case Report
Investigation and differential diagnosis of
Stafne bone cavities with cone beam computed
tomography and magnetic resonance imaging:
Report of two cases
Elif Tarim Ertas, Meral Yırcalı Atıcı, Fahrettin Kalabalik, Ozlem Ince1
Department of Oral and Maxillofacial Radiology, Faculty of Dentistry, İzmir Katip Çelebi University, 1Department of Radiology, Sifa University
Research and Training Hospital, İzmir, Turkey
A B S T R A C T
Stafne bone cavity (SBC), commonly known as Stafne bone cyst or defect is mostly asymptomatic, appearing as a unilateral, round
or ovoid, radiolucent defect with thick and corticated border. Defects that are referred as pseudocysts generally occur in mandibular
molar region, below the mandibular canal at the lingual side of the mandible and may grow slowly in time. They have been also located
lingually in the anterior mandible above the mylohyoid muscle, and on the ascending ramus just inferior to mandibular condyle or very
rarely buccal region of the ascending ramus. The aim of this case report is to present two unusual cases of SBC detected incidentally
during radiographic examination with cone beam computed tomography and magnetic resonance imaging findings. In the first case,
significant enlargement caused vestibular resorption of the buccal cortex, which is a rare finding with SBCs and in the second case
the large bone resorption reached up to the mental foramen.
Key words: Cone beam computed tomography, magnetic resonance imaging, panoramic radiography, salivary gland depression,
Stafne bone cavity
Introduction Radiographically, they are unilocular, round or ovoid
radiolucent cyst like defects with well-defined, thick and
corticated border and their diameter size varies 1-3 cm.[2]
Stafne bone cavity (SBC), is an asymptomatic bone depression
Nevertheless they can be seen multilocular with irregular
which is referred as pseudocyst without epithelial lining.[1] In
general, they occur in the mandibular molar region, related to borders.[4]
the submandibular gland below the mandibular canal. Rarely,
The differential diagnosis of mandibular depressions
they appear apical region of the premolars and canines of the
includes several pathologic entities, such as, odontogenic
anterior mandible, associated with the sublingual glands above
the mylohyoid muscle.[2] Etiology of SBC is unknown, but cyst, simple bone cyst, ameloblastoma, hemangioma,
the surrounding tissue or facial artery mechanical pressures myxoma, central giant cell lesion, fibro-osseous lesions,
can be origin of this developmental anomaly.[3] multiple myeloma, eosinophilic granuloma, benign salivary
gland tumors, neurogenic tumors, and metastatic disease.[1,5-7]
Access this article online If SBC have well-defined, thick and corticated borders and
Quick Response Code: oval shape under the mandibular canal in contact with the
Website:
www.joomr.org
base of the mandible, differential diagnosis can be easy.
However, if they are noticed higher or above the mandibular
DOI: canal and have no connection with the mandibular base
10.4103/2321-3841.170617 with irregular borders, can cause misdiagnose. Computed
tomography (CT) or magnetic resonance imaging (MRI)
Address for correspondence: Dr. Elif Tarim Ertas, Aydınlık Evler Mahallesi, Cemil Meriç Caddesi, 6780 Sokak. No. 48, 35640-Çiğli, İzmir,
Turkey. E-mail: dt.eliftarim@yahoo.com
92 Journal of Oral and Maxillofacial Radiology / September-December 2015 / Vol 3 | Issue 3
[Downloaded free from http://www.joomr.org on Tuesday, February 14, 2017, IP: 45.45.147.87]
Ertas, et al.: Investigation of Stafne bone cavities
should be useful for differential diagnose.[3] In this case largeness of the lesion and to view its dimensions and borders,
report, two unusual cases of posterior and anterior Stafne CBCT (NewTom 5G; QR, Verona, Italy) was performed
bone cysts are presented with three-dimensional cone-beam [Figure 2]. Examination of the axial images of the CBCT
CT (CBCT) and MRI findings. scan showed a mandibular lingual wall defect at the molar
region with vestibular extension, which causes resorption
Case Reports of the vestibular cortex [Figure 2a]. The cross-sectional
images presented the invagination of the lingual cortex up
Case 1 to the buccal cortex [Figure 2b]. Figure 3 shows the three-
A 51-year-old male patient was referred to our clinic for dimensional (3D) CBCT volume rendering reconstructed
routine dental examination and periodontal treatment. The images of the patient showed lingual bone defect field.
radiolucent area, which was located at the posterior right
molar region of the mandible below the inferior dental In the literature vestibular cortical resorption is an unusual
canal, had been identified on a panoramic radiograph finding so to learn the content of the cavity, MRI was
[Figure 1]. The patient had no complaints concerning this performed. In the defective cavity located in the alveolar
region, and his medical history was ordinary and he had no arcus two components with different signal intensities were
trauma or surgery history of the jaws. At the right posterior detected. In the T1 fat-saturated, T2 fat saturated, and T1
region of the mandible and submandibular region, there fat saturated contrasted MRI images, the posterior part of
was no swelling or abnormality. He had no pain during the bone cavity is filled with anteriosuperior part of the
palpation. Along the distribution of the inferior alveolar submandibular gland. In T1 and T2 sequences, anterior
and mental nerves, revealed intact sensation. part of the cavity showed hiperintens signals, which is
compatible with proteinaceous content in this area. No
Stafne bone cavity was considered for the radiolucent area fatty content was detected in fat saturated sequences in
located under the mandibular canal but because of the the anterior part [Figure 4].
Figure 1: The radiolucent area, which was located at the posterior right
molar region of the mandible below the inferior dental canal on panoramic
radiography
Figure 2: (a) The cross-sectional images presented the invagination of the
lingual cortex up to the buccal cortex. (b) The axial images of the cone beam
computed tomography scan showed a mandibular lingual wall defect at the
molar region with vestibular extension
a b c
Figure 4: (a) Coronal short tau inversion recovery, (b and c) postcontrast
axial T1 FSE, images shows that the posterior part of mandibular defect is
filled with soft tissue that is continuous and identical in signal with that of
Figure 3: Three-dimensional cone beam computed tomography volume submandibular gland, and the anterior part is filled with proteinaceous soft
rendering reconstructed images of the patient showed lingual bone defect field tissue
Journal of Oral and Maxillofacial Radiology / September-December 2015 / Vol 3 | Issue 3 93
[Downloaded free from http://www.joomr.org on Tuesday, February 14, 2017, IP: 45.45.147.87]
Ertas, et al.: Investigation of Stafne bone cavities
Final diagnose of the lesion was made as a posterior variant any connection with the apex of premolars [Figure 6b]. 3D
of SBC and the patient was informed about the lesion and CBCT volume rendering reconstructed images revealed a
scheduled follow-up appointments for every 6 months. bone defect at the anterior mandible [Figure 7].
Case 2 Successively, to learn the content of the cavity since
A 38-year-old male patient was referred to our clinic for this location is not as common as a posterior variant of
routine dental examination and prosthetic management. A SBC, MRI was performed. In the T1 fat-saturated, T2 fat
panoramic radiograph of the patient revealed a radiolucent saturated, and T1 fat saturated contrasted MRI images, the
area at the right first and second premolar region of the bone cavity is filled with soft tissue that is, continuous and
mandible below the root of the premolars [Figure 5]. The identical in signal with that of the mylohyoid muscle. This
patient’s medical and dental history was not contributory. is clearly seen in all types of sequences in various plains
There was no pain and no symptoms such as expansion in in Figure 8.
this region. Along the distribution of the inferior alveolar
and mental nerves, revealed intact sensation. In order to Final diagnose of the lesion was made as an anterior variant
eliminate the diagnosis of the radicular cyst, vitality test of SBC and the patient was informed about the lesion and
was performed, and teeth were vital. recommended follow-up appointments for every 6 months.
We performed CBCT (NewTom 5G; QR, Verona, Italy) scan
to the definite, exact location of the lesion and to confirm
the diagnosis of the entity [Figure 6]. Two-dimensional
multiplanar reconstructed CBCT axial images revealed
that the radiolucent area located on the anterior region of
the mandible lingually with mental foramen relationship
[Figure 6a]. The cross-sectional images showed depression
of the lingual cortex below the premolar region without
Figure 6: (a) The cross-sectional images showed depression of the lingual
cortex below the premolar region without any connection with apex of
premolars. (b) cone beam computed tomography axial images revealed
that the cavity located on the anterior region of the mandible with mental
foramen relationship
Figure 5: A panoramic radiograph of the patient revealed a radiolucent area
below the root of the premolars
Figure 8: (a) Sag T1 FSE, (b) coronal short tau inversion recovery, (c) contrast
Figure 7: Three-dimensional cone beam computed tomography volume COR T1 FSE (d) contrast axial T1 FSE, images shows that the mandibular
rendering reconstructed images revealed a bone defect at the anterior defect is filled with tissue that is continuous and identical in signal with that
mandible of mylohyoid muscle
94 Journal of Oral and Maxillofacial Radiology / September-December 2015 / Vol 3 | Issue 3
[Downloaded free from http://www.joomr.org on Tuesday, February 14, 2017, IP: 45.45.147.87]
Ertas, et al.: Investigation of Stafne bone cavities
Discussion follow-up periods.[15,16] Prechtl et al.[15] presented a SBC case
with significant enlargement during 17 years period. Kao
et al.[16] presented a mandibular fracture related to Stafne
Stafne bone cavities are asymptomatic, ovoid-shaped,
bone defect. Consequently, imaging techniques and follow-
homogeneous, well-defined radiolucent lingual bone
up radiographs are important to diagnose these cavities.
defects, which are usually detected incidentally on routine
Panoramic radiographs may ensure knowledge concerning
radiographic examinations.[2] There are variances in the
the diagnosis of SBC. Since CBCT provides examination
location of SBC. The most common location of SBC is
the suspicious radiolucent lesions in all sections with lower
submandibular gland fossa close to the inferior border of
radiation exposure and higher speed, it might be used for
the mandible, beneath the inferior dental canal, which is
diagnosis of SBC cases instead of CT imaging.[17] Moreover,
termed posterior variant of SBC. In our first case, SBC
to identify the contents of the cavity, MRI with superior
is located at the posterior mandibular region close to
soft tissue characterization and differentiation and without
the inferior border of the mandible. The lingual anterior
ionizing radiation should be preferred.[18]
variant of SBC is 7 times less frequent than the posterior
variant, which is located near the apical region of the
Conclusion
premolars, associated with the sublingual glands such as
our second case. Lingual and especially buccal bone cavities
of ascending ramus are very rare findings such as in our Differential diagnose of SBCs from other possible
previously reported case.[8,9] pathologies that may require treatment and imaging
technique selection according to case is significant. CBCT
Several hypotheses have been offered for the etiology and MRI might be serious for a definitive diagnosis.
of SBC, and the cause is still controversial. According Moreover, especially in cases with critical size to monitor
to Stafne,[8] bone cavities are developmental failures in the alterations in size to reduce the risk of fractures follow-
the ossification process in the region that is occupied ups are very important and the patients should be informed
by cartilage. Philipsen et al.[1] declared that hyperplastic and warned about the condition.
or hypertrophic salivary glands pressure on the bone
surface can cause the formation of SBCs. Minowa et al.[10] Acknowledgments
hypothesized that SBC is the result of erosion caused by
an acquired vascular lesion or lipoma. This case report reported on in a poster presentation at The
European Society of Head and Neck Radiology (ESHNR)
Stafne bone defects (SBDs) can include generally salivary Congress, İzmir, Turkey, October 03-05, 2013.
glands in accordance with their placement but can also
include fat, connective tissue, lymphoid tissue, muscle and References
blood vessels and even SBCs can be empty.[11] Shimizu
et al.[3] reported that SBDs which have a connection with 1. Philipsen HP, Takata T, Reichart PA, Sato S, Suei Y. Lingual and buccal
the base of the mandible generally include soft tissues. In mandibular bone depressions: A review based on 583 cases from
a world-wide literature survey, including 69 new cases from Japan.
accordance with Shimizu et al.,[3] our first case, the posterior
Dentomaxillofac Radiol 2002;31:281-90.
part of the bone cavity was filled with submandibular gland, 2. Murdoch-Kinch CA. Developmental disturbances of the face and
but anterior part of the cavity was filled with proteinaceous jaws. In: White SC, Pharoah MJ, editors. Oral Radiology Principles and
content. No fatty content was detected. In the literature, Interpretation. 6th ed. Missouri: Mosby, Elsevier; 2009. p. 574.
3. Shimizu M, Osa N, Okamura K, Yoshiura K. CT analysis of the Stafne’s
anterior SBCs commonly contained normal or inflamed
bone defects of the mandible. Dentomaxillofac Radiol 2006;35:95-102.
salivary sublingual salivary gland tissue.[12] In our second 4. Etöz M, Etöz OA, Sahman H, Sekerci AE, Polat HB. An unusual case of
case, the content of the cavity was mylohyoid muscle, which multilocular Stafne bone cavity. Dentomaxillofac Radiol 2012;41:75-8.
is a rare finding in the literature. 5. Belmonte-Caro R, Vélez-Gutiérrez MJ, García De La Vega-Sosa FJ,
García-Perla-García A, Infante-Cossío PA, Díaz-Fernández JM, et al. A
Stafne’s cavity with unusual location in the mandibular anterior area.
Generally, no surgical treatment is necessary for SBCs, Med Oral Patol Oral Cir Bucal 2005;10:173-9.
which are anatomic rather than pathologic. Clinical and 6. Branstetter BF, Weissman JL, Kaplan SB. Imaging of a Stafne bone cavity:
radiographical examinations are adequate to confirm the What MR adds and why a new name is needed. AJNR Am J Neuroradiol
static nature of cavities.[13,14] Surgical management and 1999;20:587-9.
7. Drage N, Renton T, Odell E. Atypical stafne bone cavity. Clin Radiol
biopsy can be performed when the diagnosis is unclear[1,3] Extra 2003;58:51-3.
or to reduce the risk of the fractures when the defect 8. Stafne E. Bone cavities situated near the angle of the mandible. J Am
has a critical size or has an alteration in size during the Dent Assoc 1942;29:1969-72.
Journal of Oral and Maxillofacial Radiology / September-December 2015 / Vol 3 | Issue 3 95
[Downloaded free from http://www.joomr.org on Tuesday, February 14, 2017, IP: 45.45.147.87]
Ertas, et al.: Investigation of Stafne bone cavities
9. Ertas ET, Atıcı MY, Kalabalık F, Ince O. An unusual case of double J Craniomaxillofac Surg 2013;41:270-3.
idiopathic ramus-related Stafne bone cavity. Oral Radiol 2013;29:193-7. 16. Kao YH, Huang IY, Chen CM, Wu CW, Hsu KJ, Chen CM. Late
10. Minowa K, Inoue N, Sawamura T, Matsuda A, Totsuka Y, Nakamura M. mandibular fracture after lower third molar extraction in a patient
Evaluation of static bone cavities with CT and MRI. Dentomaxillofac with Stafne bone cavity: A case report. J Oral Maxillofac Surg
Radiol 2003;32:2-7. 2010;68:1698-700.
11. Reuter I. An unusual case of Stafne bone cavity with extra-osseous 17. Kopp S, Ihde S, Bienengraber V. Differential diagnosis of stafne
course of the mandibular neurovascular bundle. Dentomaxillofac idiopathic bone cyst with Digital Volume Tomography (DVT).
Radiol 1998;27:189-91. J Maxillofac Oral Surg 2010;9:80-1.
12. De Courten A, Küffer R, Samson J, Lombardi T. Anterior lingual 18. Segev Y, Puterman M, Bodner L. Stafne bone cavity — Magnetic
mandibular salivary gland defect (Stafne defect) presenting as a residual resonance imaging. Med Oral Patol Oral Cir Bucal 2006;11:E345-7.
cyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:460-4.
13. Quesada-Gómez C, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C.
Stafne bone cavity: A retrospective study of 11 cases. Med Oral Patol
Oral Cir Bucal 2006;11:E277-80.
14. Neville BW, Dann DD, Allen CM, Bouquot JE. Developmental Defects Cite this article as: Ertas ET, Atici MY, Kalabalik F, Ince O. Investigation
of the Oral and Maxillofacial Region. Oral and Maxillofacial Pathology. and differential diagnosis of Stafne bone cavities with cone beam computed
tomography and magnetic resonance imaging: Report of two cases. J Oral
3rd ed. St. Louis: Saunders-Elsevier; 2009. p. 25.
Maxillofac Radiol 2015;3:92-6.
15. Prechtl C, Stockmann P, Neukam FW, Schlegel KA. Enlargement of a
Source of Support: Nil. Conflicts of interest: None declared.
Stafne cyst as an indication for surgical treatment - A case report.
96 Journal of Oral and Maxillofacial Radiology / September-December 2015 / Vol 3 | Issue 3
You might also like
- Circulatory System QuestionsDocument4 pagesCirculatory System QuestionsJohn Vincent Gonzales50% (2)
- Common Questions About Oppositional Defiant Disorder - American Family PhysicianDocument12 pagesCommon Questions About Oppositional Defiant Disorder - American Family Physiciando lee100% (1)
- Compounded Sterile Products Stability Compendium-AntineoplasticsDocument0 pagesCompounded Sterile Products Stability Compendium-AntineoplasticsRahmalia 'lia Cudby' PrihanantoNo ratings yet
- Probiotics, Prebiotics and The Gut Microbiota: Ilsi Europe Concise Monograph SeriesDocument40 pagesProbiotics, Prebiotics and The Gut Microbiota: Ilsi Europe Concise Monograph Seriesjimmy7forever100% (1)
- PEDIA Nursing NCLEX Bullets Part 1Document166 pagesPEDIA Nursing NCLEX Bullets Part 1Russel Myron Adriano AdvinculaNo ratings yet
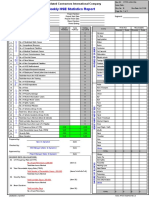
- Hse Statistics Report Pp701 Hse f04 Rev.bDocument1 pageHse Statistics Report Pp701 Hse f04 Rev.bMohamed Mouner100% (1)
- Textbook of Craniofacial Growth - 1st Ed PDFDocument396 pagesTextbook of Craniofacial Growth - 1st Ed PDFCarissa100% (3)
- Medsurg 3 Exam 1Document55 pagesMedsurg 3 Exam 1Melissa Blanco100% (1)
- Role of Radiographs in Pdl. DiseaseDocument71 pagesRole of Radiographs in Pdl. DiseaseDrKrishna Das0% (1)
- Case Study - FractureDocument58 pagesCase Study - FractureChristian97% (31)
- Pathophysiology of Typhoid FeverDocument3 pagesPathophysiology of Typhoid FeverKristofer Karlo Cabrera Castillo0% (1)
- Sinonasal Imaging PDFDocument17 pagesSinonasal Imaging PDFBelanny DwiNo ratings yet
- Radiography Jaw LesionsDocument19 pagesRadiography Jaw LesionssrikantnairNo ratings yet
- CBCT Findings of Periapical Cemento-Osseous Dysplasia: A Case ReportDocument4 pagesCBCT Findings of Periapical Cemento-Osseous Dysplasia: A Case ReportRestaWigunaNo ratings yet
- DMFR 52088107Document4 pagesDMFR 52088107Roisah Yunan NegariNo ratings yet
- Stafne's Bone Cyst (SBC)Document8 pagesStafne's Bone Cyst (SBC)Mehmed KiossovNo ratings yet
- Osteochondroma of The Mandibular Condyle: About A CaseDocument3 pagesOsteochondroma of The Mandibular Condyle: About A CaseasclepiuspdfsNo ratings yet
- 2016 Benign Jaw Lesions PDFDocument17 pages2016 Benign Jaw Lesions PDFMaria Alejandra AtencioNo ratings yet
- Traumatic Bone Cyst of Idiopathic Origin? A Report of Two CasesDocument5 pagesTraumatic Bone Cyst of Idiopathic Origin? A Report of Two CasesjulietNo ratings yet
- 9 PDFDocument3 pages9 PDFDennis hayonNo ratings yet
- Large Cemento-Ossifying Fibroma of The Mandible Involving TheDocument4 pagesLarge Cemento-Ossifying Fibroma of The Mandible Involving TheDessy Dwi UtamiNo ratings yet
- Sara Pavlović Marko PongracDocument34 pagesSara Pavlović Marko Pongraclenami_91No ratings yet
- External CholesteatomDocument5 pagesExternal CholesteatomIvana SupitNo ratings yet
- Pseudo-Ankylosis Caused by Osteoma of The Coronoid Process: Case Report - Tumors/CystsDocument3 pagesPseudo-Ankylosis Caused by Osteoma of The Coronoid Process: Case Report - Tumors/CystsSaurabh SatheNo ratings yet
- TMP EADFDocument5 pagesTMP EADFFrontiersNo ratings yet
- Cemento-Osseous DysplasiaDocument5 pagesCemento-Osseous DysplasiaFatima AliNo ratings yet
- Cemento Ossifying Fibroma: A Case ReportDocument4 pagesCemento Ossifying Fibroma: A Case ReportBima Ewando KabanNo ratings yet
- 下颌颊分叉囊肿 2例病例报告(英文) - 刘耀然.caj 2023 02 14 14 16 20 213Document3 pages下颌颊分叉囊肿 2例病例报告(英文) - 刘耀然.caj 2023 02 14 14 16 20 213朱嘉琪No ratings yet
- Khalid, 356Document4 pagesKhalid, 356Indah VitasariNo ratings yet
- Low-Grade Osteosarcoma of The MandibleDocument5 pagesLow-Grade Osteosarcoma of The MandibleGalih AryyagunawanNo ratings yet
- Radiologic Techniques Used To Evaluate The Temporomandibular Joint ConventionalDocument10 pagesRadiologic Techniques Used To Evaluate The Temporomandibular Joint ConventionalEm EryNo ratings yet
- Calcifying Odontogenic Cyst With Atypica PDFDocument5 pagesCalcifying Odontogenic Cyst With Atypica PDFHerminaElenaNo ratings yet
- Radiological Aspects of Apical Periodontitis: Sisko Huumonen & Dag ØrstavikDocument23 pagesRadiological Aspects of Apical Periodontitis: Sisko Huumonen & Dag ØrstavikAsadulla KhanNo ratings yet
- Benign Cementoblastoma: Case ReportDocument3 pagesBenign Cementoblastoma: Case ReportpsyNo ratings yet
- Imaging in Oral Cancers: Ead and Eck YmposiumDocument14 pagesImaging in Oral Cancers: Ead and Eck YmposiumHayyu F RachmadhanNo ratings yet
- Quiste Residual Con CalcificacionesDocument4 pagesQuiste Residual Con CalcificacionesCARLOS DARIO MERINO BUSTAMANTENo ratings yet
- 2021 Publication Case Report - Frontal MucoceleDocument3 pages2021 Publication Case Report - Frontal MucoceleMade RusmanaNo ratings yet
- Mandibular Buccal Bifurcation Cyst: Case Report and Literature ReviewDocument5 pagesMandibular Buccal Bifurcation Cyst: Case Report and Literature Reviewboooow92No ratings yet
- Bilateral Maxillary Buccal Bone Exostosis: Rare Case ReportDocument4 pagesBilateral Maxillary Buccal Bone Exostosis: Rare Case Reportegi007No ratings yet
- Broadie 2Document12 pagesBroadie 2Stefana NanuNo ratings yet
- Radiographic, CT and MRI Features of Cherubism: CasereportDocument6 pagesRadiographic, CT and MRI Features of Cherubism: CasereportTaufik ShidkiNo ratings yet
- CA LS Bướu Nhiều Hốc - Multilocular Radiolucency in the Body of MandibleDocument4 pagesCA LS Bướu Nhiều Hốc - Multilocular Radiolucency in the Body of MandibleThành Luân NguyễnNo ratings yet
- Diagnose of Submandibular Abscess PDFDocument13 pagesDiagnose of Submandibular Abscess PDFElvitrianaNo ratings yet
- (klp.1) Isd-48-147Document6 pages(klp.1) Isd-48-147pala bapakmuNo ratings yet
- Aneurysmal Bone CystDocument5 pagesAneurysmal Bone CystDipti PatilNo ratings yet
- Radiographs in Periodontal DiseaseDocument23 pagesRadiographs in Periodontal Diseasev.shivakumarNo ratings yet
- Odontogenickeratocyst Clinically Mimicking Osteomyelitis - A Rare Case ReportDocument4 pagesOdontogenickeratocyst Clinically Mimicking Osteomyelitis - A Rare Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- IndianJRadiolImaging223195-1839113 050631Document14 pagesIndianJRadiolImaging223195-1839113 050631syedmiskin006No ratings yet
- Oral CencerDocument14 pagesOral CencerVilaseca224466No ratings yet
- Idiopathic Condylar ResorptionbDocument12 pagesIdiopathic Condylar ResorptionbBelizNo ratings yet
- A Bilocular Radicular Cyst in The Mandible With Tooth Structure Components InsideDocument5 pagesA Bilocular Radicular Cyst in The Mandible With Tooth Structure Components InsideRoza LindaNo ratings yet
- Pof CR1Document4 pagesPof CR1Swab IndonesiaNo ratings yet
- Linfoma Extranodal en Cabeaza y CuelloDocument5 pagesLinfoma Extranodal en Cabeaza y CuelloCARLOS DARIO MERINO BUSTAMANTENo ratings yet
- SAARC ENT Conference - Leison Maharjan - External Auditory Canal CholesteatomaDocument1 pageSAARC ENT Conference - Leison Maharjan - External Auditory Canal CholesteatomaAshokNo ratings yet
- Recurrent Aneurysmal Bone Cyst of The Mandibular Condyle With Soft Tissue ExtensionDocument5 pagesRecurrent Aneurysmal Bone Cyst of The Mandibular Condyle With Soft Tissue ExtensionlalajanNo ratings yet
- Double Mandibular Osteotomy With Coronoidectomy For Tumours in The Parapharyngeal SpaceDocument5 pagesDouble Mandibular Osteotomy With Coronoidectomy For Tumours in The Parapharyngeal SpaceSree BanNo ratings yet
- Jurnal 22 PDFDocument4 pagesJurnal 22 PDFsriwahyuutamiNo ratings yet
- Ohns 3 182Document8 pagesOhns 3 182kalixinNo ratings yet
- COF4Document4 pagesCOF4ton viet nguyenNo ratings yet
- Mixed Periapical Lesion: An Atypical Radicular Cyst With Extensive CalcificationsDocument4 pagesMixed Periapical Lesion: An Atypical Radicular Cyst With Extensive CalcificationsResa YudhistiNo ratings yet
- CT, CBCT, MriDocument2 pagesCT, CBCT, Mrialaa.elsamy936No ratings yet
- Cranium 3Document26 pagesCranium 3giant nitaNo ratings yet
- Mandibular Posterior Anatomic Limit For MolarDocument8 pagesMandibular Posterior Anatomic Limit For MolarRommy MelgarejoNo ratings yet
- Aggressive Orthokeratinized Odontogenic CystDocument5 pagesAggressive Orthokeratinized Odontogenic CystSooraj SNo ratings yet
- JDentImplant41101-6122697 170026Document4 pagesJDentImplant41101-6122697 170026Dragos CiongaruNo ratings yet
- Bleiker 1939Document13 pagesBleiker 1939Carla SantosNo ratings yet
- Dent Update 2022 49 646-649Document4 pagesDent Update 2022 49 646-649Fatma HarmadaniNo ratings yet
- Australian Dental Journal - 2008 - Spencer - Odontogenic Myxoma Case Report With Reconstructive ConsiderationsDocument4 pagesAustralian Dental Journal - 2008 - Spencer - Odontogenic Myxoma Case Report With Reconstructive ConsiderationsMarkNo ratings yet
- Juvenile Ossifying Fibroma of The Mandible: A Case ReportDocument7 pagesJuvenile Ossifying Fibroma of The Mandible: A Case Reportabeer alrofaeyNo ratings yet
- Craniofacial Develeopement of Mandible and Its Applied AspectDocument97 pagesCraniofacial Develeopement of Mandible and Its Applied AspectswayampradeepmohapatraNo ratings yet
- Future Dental Journal: SciencedirectDocument8 pagesFuture Dental Journal: SciencedirectdrvinitaNo ratings yet
- Biology of Tooth MovmentDocument100 pagesBiology of Tooth MovmentswayampradeepmohapatraNo ratings yet
- Rabea 2018Document8 pagesRabea 2018swayampradeepmohapatraNo ratings yet
- Final Test RESIT 61 TNDocument4 pagesFinal Test RESIT 61 TNosamyyNo ratings yet
- Unit 4 ReadingDocument4 pagesUnit 4 ReadingElvantNo ratings yet
- Abreviaciones ChatDocument4 pagesAbreviaciones ChatrojarodNo ratings yet
- CBST LastDocument5 pagesCBST LastMozma AwanNo ratings yet
- General Profile: - Pa - 6mos Old - Female - Filipino - Roman Catholic - Alang-Alang Mandaue CityDocument18 pagesGeneral Profile: - Pa - 6mos Old - Female - Filipino - Roman Catholic - Alang-Alang Mandaue CityRj FornollesNo ratings yet
- Labiomandibular Paresthesia Caused by Endodontic Treatment - An Anatomic and Clinical Study PDFDocument13 pagesLabiomandibular Paresthesia Caused by Endodontic Treatment - An Anatomic and Clinical Study PDFAlexandra DumitracheNo ratings yet
- MedicalerrorDocument38 pagesMedicalerrorchanda jabeenNo ratings yet
- Accessories Rangebrochure60000217Document36 pagesAccessories Rangebrochure60000217dessy susantyNo ratings yet
- Questions and Answers 1Document7 pagesQuestions and Answers 1api-382372564No ratings yet
- Sitogenetika Dan Peranannya Dalam Keganasan Hematologi: ResearchDocument23 pagesSitogenetika Dan Peranannya Dalam Keganasan Hematologi: ResearchFebryanti Priskila SilaenNo ratings yet
- The Endocrine System and Feedback MechanismsDocument8 pagesThe Endocrine System and Feedback MechanismsJame SmithNo ratings yet
- Efficacy of Doctorvox On Mutational FalsettoDocument8 pagesEfficacy of Doctorvox On Mutational FalsettoANA CRISTINA MENDEZ DIAZNo ratings yet
- Full Download Test Bank For Ebersole and Hess Gerontological Nursing and Healthy Aging 2nd Canadian Edition by Touhy PDF Full ChapterDocument36 pagesFull Download Test Bank For Ebersole and Hess Gerontological Nursing and Healthy Aging 2nd Canadian Edition by Touhy PDF Full Chapteradrianblackiadxetkrqm100% (15)
- Factory Farming in The Developing WorldDocument10 pagesFactory Farming in The Developing WorldDaisyNo ratings yet
- Bile Esculine TestDocument2 pagesBile Esculine TestVincent OngNo ratings yet
- Lecture 3 Innate ImmunityDocument26 pagesLecture 3 Innate ImmunitytimcarasNo ratings yet
- SBI3U Unit 1Document5 pagesSBI3U Unit 1Sara SNo ratings yet
- CENE Course Outline On Psychiatric NursingDocument3 pagesCENE Course Outline On Psychiatric NursingJohn Ryan BuenaventuraNo ratings yet
- Nursing ShortageDocument16 pagesNursing Shortageapi-240927368No ratings yet
- Semmelweis' Handwashing & Lister's Antiseptic TechniqueDocument22 pagesSemmelweis' Handwashing & Lister's Antiseptic TechniqueNewNo ratings yet
- Science: Quarter 1 - Module 1: Week 1-2Document31 pagesScience: Quarter 1 - Module 1: Week 1-2Kirt Dimamay HilarioNo ratings yet