Professional Documents
Culture Documents
Tranz
Uploaded by
Mary Kaye Yvonne OtillaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tranz
Uploaded by
Mary Kaye Yvonne OtillaCopyright:
Available Formats
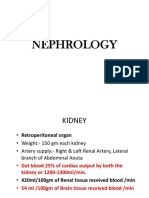
CC2 LEC
FLUIDS AND ELECTROLYTES
SODIUM
WATER ● Aka: natrium
A. Introduction ● Major extracellular cation
➔ 40-75% of body weight ● principal osmotic particle outside the cell
➔ Function: ● Major contributor of osmolarity: together with Cl and HCO3
◆ Transport nutrients to the cells ● Concentration depends on intake and water excretion
◆ Removes waste products ● (+) serum abnormalities = urine Na & osmolarity
➔ Location: ● Every 100 mg/dL increase in glucose = decrease 1.6 mmol/L
◆ ICF: ⅔ Na
◆ ECF: ⅓ ● Ref value:
➔ Intravascular (25%) and interstitial fluid (75) ○ 135-145 mmol/L (serum)
○ 136-150 mmol/L (CSF)
DISTRIBUTION OF BODY WATER IN ADULT ● Critical value:
○ 160 mmol/L (hypernatremia)
Compartment % of Body Weight % of total Body H2O ○ 120 mmol/L (hyponatremia)
Extracellular 20 33 HORMONES
1. Aldosterone - Na retention and K excretion
Plasma 5 8 2. Atrial Natriuretic factor (ANF)
(Intravascular)
● Antihypertensive agent
● Tissue source: cardiac atria
Interstitial 15 25
● block aldosterone and renin secretion
● inhibits action of angiotensin II and vasopressin
Intracellular 40 67
● promotes natriuresis
B. Osmolality - concentration ng ions is maintained by:
1. Passive transport - Passive movement of ions METHODS OF ANALYSIS
across a membrane. 1. Emission Flame Photometry
2. Active transport - Requires energy to move ions 2. Ion selective electrode - glass aluminum silicate: most
across a membrane. ATPase-dependent ion commonly used
pumps. 3. Atomic absorption spectrophotometry
Definition: concentration of solutes per kg of solvent (millimoles/kg) 4. Colorimetry
Regulated by: ● Albanese and Lein
a. Thirst Sensation - Response to consume more fluid. ○ Na is precipitated as ZN uranyl acetate
Prevents water deficit. ○ end color: yellow
b. Arginine vasopressin hormone (AVP) - HYPERNATREMIA
● Antidiuretic hormone (ADH). ● increase Na concentration:
● Increase reabsorption of water in kidneys. ○ >145 mmol/L
● Suppressed in excess H2O load ○ 150-160 mmol/L: moderate water deficit
● Activated in H2O deficit ○ >165 mmol/L: severe water deficit
c. Renin-angiotensin-aldosterone system (RAAS) ● causes: loss of water, gain of Na or both
d. Atrial Natriuretic Peptide (ANP): Increase Na+ and H20 ● 1-2% water deficit = severe thirst
excretion in the kidney ● perspiration and breathing: 1L/day water loss
e. Glomerular Filtration Rate (GFR): Increase with vol. ● chronic hypernatremia: indicative of hypothalamic disease
Expansion and decrease with volume depletion.
Excess water loss
Determination :
● Diabetes insipidus
● Osmolality (Serum or Urine) ● Renal tubular disorder
● Any substance dissolve in a solvent will:
● Prolonged diarrhea
○ Dec freezing point by 1.858C
○ Inc boiling point by 0.52C ● Profuse sweating
○ Dec vapor pressure (dew point) by 0.3 mmHg ● Severe burns
○ Inc osmotic pressure by 17,000 mmHg ● Vomiting
● Main contributors are Na+, Cl-, Urea and Glucose ● Hyperventilation
Increase intake or retention
FLUIDS AND ELECTROLYTES ● Hyperaldosteronism (Conn’s disease)
● Sodium bicarbonate infusion
● Ions capable of carrying electric charge
● Increased oral or IV intake of NaCl
○ Cations and anions
● Electroneutrality: equal number of cations and anions Ingestion of water intake
● Average water content: 40-75%
○ ECF: ⅓ (16 L) HYPONATREMIA
○ ICF: ⅔ (24 L) ● decrease Na concentration
● 30 L fluid passes from blood to tissue spaces ○ >135 mmol/L
● Sweat: 50 mmol/L sodium + 5 mmol/L potassium ○ 125-130/L: + symptoms
● Salt content: main determinant of ECF volume
○ 130 mmol/L clinical concerns
● Dec vasopressin: 10-20 L fluid excretion daily
● Edema: 3 L fluid retention ○ <125 mmol/L severe neuropsychiatric symptoms
● Plasma: 12% higher fluid content than the whole blood ● (+) glucose or mannitol, glycine & ketones (seen in DM)
● SIADH: decrease aldosterone, increase water retention
PHYSIOLOGIC IMPORTANCE
● K and Na have inverse relationship in the kidney
1. Volume and osmotic regulation - Na. Cl, k reabsorption
2. For myocardial rhythm and contractility - K, Ca, Mg
Increase sodium loss
3. Important cofactors in enzyme activation - Ca, Mg, Zn, Cl, K
4. For the regulation of ATP ion pumps - Mg ● Diuretic use
5. For neuromuscular excitability - K, Ca, Mg ● Saline infusion
6. For the production and use of ATP from the glucose - Mg, Increase water retention
PO4 ● Renal failure
7. Maintenance of acid- base balance - HC03, K, Cl, PO4 ● Nephrotic syndrome
8. Replication of DNA and translation of mRNA - Mg ● Aldosterone deficiency
● Cancer
VILLAGRACIA, JALEN C. MT 3-YA-8 1
CC2 LEC
Increase water retention ○ oral or IV infusion
● SIADH ● Use of immunosuppressive drugs
● Hepatic cirrhosis ○ Tacrolimus and Cyclosporine
● Primary polydipsia ● Extracellular shift
● CNS abnormalities ○ Acidosis
● Myxedema ○ Muscle/cellular injury
● Barterr’s syndrome ○ Chemotherapy
○ Vigorous exercise
HYPONATREMIA WITH NRF ○ Digitalis intoxication
PSEUDOHYPERKALEMIA
Cause Serum Na Urine Na 24hr Urine Serum K
urine Na Osmolalit inc plasma K levels with normal ECG
y causes:
Overhydr D D D D N- D Hemolysis High blast counts (leukemias)
ation
Thrombocytosis Recentrifugation of SST
Diuretics D D I D D
Prolonged tourniquet application Blood stores on ice
SIADH D I I I N-D
Fist clenching Iv fluid
Adrenal Mild I N I I
Failure
HYPOKALEMIA
Bartter’s D D I D D ● plasma K levels: 3.0-3.4 mmol/L (mild)
syndrome
● dec Mg = dec K
● dec plasma K (retained) to balance secrete another cation
Diabetic D N N N I
Hyperos (NH4 ion)
molarity ● Impaired renal function/renal loss: increase aldosterone
● Extra renal loss: diarrhea
PSEUDOHYPONATREMIA ● Gastrointestinal loss
● systematic error in measurement ○ gastric suction and laxative abuse
● Artificial hyponatremia: hyperlipidemia and hypoproteinemia ○ intestinal tumor and malabsorption
● DECREASE NA = INCREASE lipids, proteins, hemoglobin, ● cancer and radiotherapy
K ● Intracellular shift: alkalosis and insulin overdose
● Renal loss: diuretics, Hyperaldosteronism, cushing’s
syndrome, leukemia, barrter’s syndrome, gitelman’s
POTASSIUM
● Aka: kalium syndrome, malignant hypertension
● Major intracellular cation
● total plasma body potassium = 2% PSEUDOHYPOKALEMIA: leukocytosis: decrease K levels if left at
● K in RBC: 105 mmol/L room temperature
● filtered in glomeruli, reabsorbed by proximal tubule
● ascending loop of Henle: K, Na, Cl EFFECTS TO CARDIAC MUSCLE
● single most important analyte Hyperkalemia Hypokalemia
● function: heart contraction, neuromuscular excitability, ICF
volume and hydrogen ion regulation dec resting membrane potential inc resting membrane potential
● ref value: 3.5-5.2 mmol/L (RMP) (RMP)
● critical values:
○ 6.5 mmol/L: hyperkalemia inc cell excitability dec cell excitability
○ 2.5 mmol/L: hypokalemia
Plasma levels: arrhythmia and paralysis
METHOD OF ANALYSIS ● 6-7 mmol/L: alter
● hemolysis of 0.5% RBC = increase 0.5 mmol/L ECG
● 8mmol/L: lack of
● platelet release: plasma levels are decrease 0.1-0.7 mmol/L
muscle excitability
compared to serum ● 10mmol/L: fatal,
● muscular act cardiac arrest
○ increase 0.3-1.2 mmol/L: mild-moderate exercise
○ increase 2-3 mmol/L: vigorous exercise, fist Cessation of contraction
clenching
● prolonged contact of serum to RBC
pH imbalance, drugs, hormones
● prolonged tourniquet application
● preferred sample: heparinized plasma Hyperkalemia Hypokalemia
1. Emission Flame photometry Acidosis = inc 0.2-1.7 mmol/L Alkalosis (0,1) = dec 0.4 mmol/L
2. Ion selective electrode - valinomycin gel dec insulin inc aldosterone
3. Atomic absorption spectrophotometry Therapeutic K Insulin and catecholamines
4. Colorimetry Hyperkalemic drugs
● Lockhead and Purcell
● end color: blue violet CHLORIDE
● major extracellular anion
HYPERKALEMIA ● chief counter ion of sodium
● increase concentration ● functions: water balance, osmotic pressure (Na & Cl), blood
● 3 major mechanism of increase K: volume, electroneutrality
○ reduced aldosterone: hyporeninemic, ● enzyme activator: AMS
hypoaldosteronism ● excreted via: urine and sweat
○ renal failure; most common, dec GFR and dec ● ref value: 98-107 mmol/L
tubular secretion
○ reduced distal delivery of solution METHODS OF ANALYSIS
● Decreased renal excretion ● marked hemolysis: dec Cl levels (dilution)
○ acute/chronic renal failure ● slightly lower values: post prandial specimen
○ severe hydration ● dec Cl = inc HC03
○ addison’s disease ● interference: bromide, cyanide, cysteine
● increase intake
VILLAGRACIA, JALEN C. MT 3-YA-8 2
CC2 LEC
1. Mercuric titration (Schales and Schales)
Increase Calcium Dec calcium
● indicator diphenylcarbazone
● end prod: HgCl2
Prolonged contact to pRBC Venous occlusion
● end color: blue violet Recumbent posture Acidosis
2. Spectrophotometric Alkalosis Dehydration
● Mercuric Thiocyanate (Whitehorn titration method): Tetany Hemoconcentration
reddish complex Parathyroid disease (primary Parathyroid hormone - related
● Ferric perchlorate: colored complex hypocalcemia) protein (PTHRP)
3. Coulometric Amperometric titration Renal failure Secondary hyperparathyroidism
Estrogen (ionized calcium)
● Cotlove Chloridometer
4. Ion Selective Electrode
● ion exchange membrane
● most commonly used
Hypercalcemia Hypocalcemia
DIAGNOSTIC SIGNIFICANCE
Primary hyperparathyroidism Alkalosis
Hyperchloremia Hypochloremia Cancer (lung and mammary) vitamin D deficiency
Acidosis primary hypoparathyroidism
Renal tubular acidosis Prolonged vomiting inc vitamin D’ acute pancreatitis
Diabetes insipidus Aldosterone deficiency multiple myeloma hypomagnesemia
Salicylate intoxication Metabolic alkalosis sarcoidosis malabsorption syndrome
Primary hyperparathyroidism Salt losing nephritis hyperthyroidism renal tubular failure
Metabolic acidosis Milk-alkali syndrome
Prolonged diarrhea
PHOSPHORUS
CALCIUM ● counter ion of K
● 99% is the bone: 1% in blood and ECF ● omnipresent: 85% in bones, 15% in the ECF
● maximal absorbed in the duodenum ● inverse relationship with calcium
● absorption is best at acidic pH ● maximally absorbed in jejunum
● urinary excretion: major net loss ● function: phosphorylation of glucose, co-entry of K
● function: blood coagulation, neural transmission, enzyme ● inorganic phosphate: most predominant in serum
act, excitability of skeletal and cardiac muscle ● ref value: 2.7-4.5 mg/dl (adult)
● ref value: ○ 4.5-5.5 mg/dl (child)
● total calcium: 8.6 to 10 mg/dl (adult) ○ <1.0 g.dL or 0.3 mmol/L (severe)
○ 8.8 to 10.8 (child) ● Inorganic phosphorus
● ionized calcium: 4.6 to 5.3 mg/dL (adult) ○ organic phosphate: principal anion within the cells
○ 4.8 to 5.5 mg/dl (child) ○ inorganic phosphate: part of the blood buffer
● Forms of calcium ● Forms of phosphorus
○ Ionized - 50% ○ free or unbound form: 55%
○ Protein bound - 40% ○ complexed with ions: 35%
○ Complexed with anions - 10% ○ protein bound: 10%
● Ionized calcium: sensitive and specific calcium disorders
● dec 1 g/dl serum albumin = dec 0.8 mg/dL total Ca+ HORMONES AFFECTING PHOSPHATE LEVELS
1. Parathyroid hormone - decreases phosphate by excretion
FACTORS AFFECTING CALCIUM LEVELS 2. Calcitonin - inhibits bone resorption
1. 1,25-dihydroxycholecalciferol (Act Vit D3) - increase 3. Growth hormone - increases renal phosphate reabsorption
intestinal absorption, kidney reabsorption, mobilization from
bones METHODS OF ANALYSIS
2. Parathyroid hormone (PTH) ● fasting is required: inc carbohydrate diet = dec phosphorus
● increase kidney reabsorption, mobilization from ● pH dependent
bones, activates bones resorption ● separate pRBC and serum immediately
● dec urinary Ca loss ● PO4: form measure in the lab
● stimulates Vit D to Vit D3 (kidneys) ● mEq/L: unit of measurement
3. Calcitonin ● circadian rhythm: inc in late morning, dec evening
● thyroid hormone
● secreted by parafollicular C cells 1.. Fiske Subbarow method (Ammonium molybdate method)
● inhibits: PTH, Vit D3, bone resorption ● most commonly used
● inc urinary Ca loss ● reducing agents: Pistol (Amino naphthol sulfonic acid), Elon
(Methyl amino phenol), Ascorbic acid, Senidine
METHODS OF ANALYSIS (N-phenyl-p-phenylene diamine hydrochloride)
specimen of choice: serum ● end product: ammonium molybdate complex
dec pH of reagent: inc liberation of Ca from albumin ● end color: blue
1. Precipitation and redox titration ● wavelength: 340 nm at alkaline pH
a. Clark collip precipitation
end product: Oxalic acid DIAGNOSTIC SIGNIFICANCE
end color: purple Hyperphosphatemia Hypophosphatemia
b. Ferro Ham Chloranilic Acid precipitation
end product: Chloranilic acid ● Hypoparathyroidism Alcohol abuse
end color: purple ● Renal failure Primary hyperthyroidism
2. Ortho-Cresolphthalein Complexone dyes (colorimetric) ● Lymphoblastic Avitaminosis D
dye: arzeno III leukemia Myxedema
Mg inhibitor: 8-hydroxyquinolone (chelator) ● Hypervitaminosis D Transcellular shift (major(
● Renal tubular defects
3. EDTA titration (Bachra, Dowel and Sobel)
(inc phosphate, dec
4. Ion selective electrode: liquid membrane calcium, inc BUN and
5. Atomic Absorption Spectrophotometry: ref method Creatinine)
6. Emission Flame Photometry: orange - red
DIAGNOSTIC SIGNIFICANCE
(+) symptoms: total calcium levels <7.5 mg/dL (1.88 mmol/L) MAGNESIUM
● 2nd major intracellular cation
● 4th most abundant cation in body
● enzyme activator: CK and ALP
VILLAGRACIA, JALEN C. MT 3-YA-8 3
CC2 LEC
● stored in 53% bones, 46% muscles and soft tissues , 1%
serum and RBC
● dec Mg = dec K
● ref value: 1.2-2.1 mEq/L
● 5 mmol/L (life threatening
● function: vasodilator; dec uterine hyperactivity in eclampsia;
inc uterine blood flow; maintaining structures of DNA, RNA,
ribosomes; synthesis of CHO, CHON, lipids; neuromuscular
transmission; cofactor; regulate movement of K in the
myocardium
● forms of phosphorus:
● free/ionized - 55%
● protein bound- 30%
● complexed with anions - 15%
FACTORS AFFECTING MAGNESIUM LEVELS
1. Parathyroid hormone - inc renal reabsorption of magnesium
and inc intestinal absorption of magnesium
2. Aldosterone and Thyroxine - inc renal excretion of
magnesium
METHODS OF ANALYSIS
1. Colorimetric method
a. Calmagite method: reddish-violet complex
b. Formazendye method: colored complex
c. Magnesium thymol blue method: colored complex
2. Atomic absorption spectrophotometry: reference method
3. Dye-Lake method
a. Titan yellow dye
clayton yellow
thiazole yellow
DIAGNOSTIC SIGNIFICANCE
Hypermagnesemia Hypomagnesemia
Diabetic coma Acute renal failure
Addison’s disease malnutrition
Chronic renal failure malabsorption syndrome
increase of antacids, enemas, chronic alcoholism
and, cathartics severe diarrhea
BICARBONATE
2nd most abundant anion in the ECF
HCO3 = undissociated NaHC03, carbonate, carbamate
accounts 90% of total CO2
inc bicarbonate; renal failure
function: major component of the blood buffer system
specimen: blood anaerobically collected (serum/heparinized)
specimen left uncapped: dec 6 mmol/L
METHOD OF ANALYSIS
1. Ion selective electrode - pCO2 electrode
2. Enzymatic - phosphoenolpyruvate carboxylase and
phosphoenolpyruvate dehydrogenase
VILLAGRACIA, JALEN C. MT 3-YA-8 4
CC2 LEC
TUMOR MARKERS Alkaline Phosphatase (ALP)
Increased ALP activities are seen:
Hyperplasia ● Primary or secondary liver cancer.
▪ Involves the multiplication of cells in an organ or tissue, which may ● Metastatic cancer with bone or liver involvement.
consequently have increased in volume. ● Placental ALP, regan isoenzyme, elevates in a variety of
▪ Serves a useful purpose and is controlled by stimuli malignancies, including ovarian, lung, gastrointestinal
▪ Elevation of tumor markers is transient cancers and Hodgkin’s disease.
Neoplasia Prostatic acid phosphatase (PAP)
▪ Unregulated and serves no purpose ● It is used for staging prostate cancer and for monitoring
▪ Elevation of tumor markers will be a long lasting phenomenon if not therapy.
treated ● Osteogenic sarcoma
● Multiple myeloma
Angiogenesis - It is a vital and complex biological process, forming ● Bone metastasis of other cancers and in some benign
new capillaries from pre-existing blood vessels and infusing tissue with conditions such as osteoporosis and hyperparathyroidism.
supplies of oxygen and nutrients.
Prostate Specific Antigen (PSA)
Differentiation - It is the process by which specialized cells becomes ● The clinical use of PAP has been replaced by PSA. PSA is
more specialized cells. much more specific for screening or for detection early
cancer. It is found in mainly prostatic tissue.
STAGES OF CANCER ● Urinary bladder cateterization and digital rectal examination
Stage 1- usually means that a cancer is relatively small and contained may lead an increased PSA level in serum.
within the organ it started in ● The ratio between free and total PSA is an reliable marker
Stage 2 - usually means that the tumor is larger than in stage 1, but for differentiation of prostatic cancer from benign prostatic
the cancer has not started to spread into the surrounding tissues. hyperplasia.
Sometimes stage 2 means that cancer cells have spread into lymph ● The greatest clinical use of PSA is in the monitoring of
nodes close to the tumor. This depends on the particular type of cancer treatment.
Stage 3 - usually means the cancer is larger. It may have started to ● This treatment includes radical prostatectomy, radiation
spread into surrounding tissues and there are cancer cells in the lymph therapy and antiandrogen therapy.
nodes in the area ● The PSA level should fall below the detection limit.
Stage 4 - means the cancer has spread from where it started to ● This may require 2-3 weeks. If it is still at a high level after
another body organ. This is also called secondary or metastatic cancer 2-3 weeks, it must me assumed that residual tumor is
present.
Many cancers are associated with the abnormal production of some
molecules which can be measured in plasma. These molecules are
known as tumor markers.
● Biological substance synthesized and released by cancer
cells
● Substance produced by the host in response to cancerous
tissue
● Present in:
○ -Circulation
○ -Cavity fluids
○ -Cell membrane
○ -Cytoplasm/nucleus of the cell
A good tumor marker should have those properties: Calcitonin
1. A tumor marker should be present in or produced by tumor itself. ● Calcitonin is a hormone which decreases blood calcium
2. A tumor marker should not be present in healthy tissues. concentration.
3. Plasma level of a tumor marker should be at a minimum level in ● Its elevated level is usually associated with medullary thyroid
healthy subjects and in benign conditions. cancer.
4. A tumor marker should be specific for a tissue, it should have ● Lung CA, breast, kidney, liver and in nonmalignant
different immunological properties when it is synthesized in other conditions such as pulmonary diseases, pancreatitis, Paget’s
tissues. disease, hyperparathyroidism, myeloproliferative disordes
5. Plasma level of the tumor marker should be in proportion to the both and pregnancy
size of tumor and activity of tumor.
6. Half life of a tumor should not be very long Human Chorionic Gonadotropin (hCG)
7. A tumor marker should be present in plasma at a detectable level, ● It is a glycoprotein appears in pregnancy. Its high levels is a
even though tumor size is very small useful marker for tumors of placenta and some tumors of
testes.
Tumor markers can be classified as respect with the type of the ● hCG is also at a high level in patients with primary testes
molecule: insufficiency.
1. Enzymes or isoenzymes (ALP, PAP) ● hCG does not cross the blood-brain barier. Higher levels
2. Hormones (calcitonin) may indicate metastasis in the brain.
3. Oncofetal antigens (AFP, CEA)
4. Carbohydrate epitopes recognised by monoclonal antibodies (CA ONCOFETAL ANTIGENS - Most reliable markers in this group are
15-3,CA 19-9, CA125) α-fetoprotein(AFP) and carcinoembryonic antigen (CEA)
5. Receptors (Estrogen, progesterone)
6. Oncogenes and tumor suppressor genes (BRCA1 and 2 ) α-Fetoprotein (AFP)
● α-fetoprotein is a marker for hepatocellular and germ cell
Potential uses of Tumor Markers carcinoma.
Screening in general population ● AFP is useful for screening (AFP levels greater than 1000
Differential diagnosis of symptomatic patients µg/L are indicative for cancer except pregnancy),
Clinical staging of cancer determining prognosis and monitoring therapy of liver
Estimating tumor volume cancers.
As a prognostic indicator for disease progression ● AFP and hCG combined are useful in classifying and staging
Evaluating the success of treatment germ cell tumors. One or both markers are increased in
Detecting the recurrence of cancer those tumors.
Monitoring reponse to therapy
VILLAGRACIA, JALEN C. MT 3-YA-8 5
CC2 LEC
Carcinoembryonic antigen (CEA) 1) Protooncogenes which are responsible for normal cell growth and
● It is a cell-surface protein and a well defined tumor marker. differentiation
● CEA is a marker for colorectal, gastrointestinal, lung and 2) Tumor suppressor genes which are involved in recognition and
breast carcinoma. repair of damaged DNA.
● CEA levels are also elevated in smokers and some patients 3)Apoptosis-related genes are responsible for regulation of apoptosis
having benign conditions such as cirrhosis, rectal polips, 4)DNA repair genes
ulcerative colitis and benign breast disease. Alterations on these genes may lead tumor development.
● CEA testing should not be used for screening. Some tumors
don’t produce CEA. It is useful for staging and monitoring Susceptible DNA repair genes:
therapy. ● BRCA1 and BRCA2 are specific genes in inherited
predisposition for developing breast and ovarian cancer, and
CARBOHYDRATE MARKERS mutations on these genes are newly measured in some
● These markers either are antigens on the tumor cell surface laboratories.
or are secreted by tumor cells. ● Mismatch-repair genes are mutated in some colon cancers
● They are high-molecular weight mucins or blood group
antigens. Monoclonal antibodies have been developed
against these antigens.
● Most reliable markers in this group are CA 15-3, CA 125 and
CA19-9.
CA 15-3
● CA 15-3 is a marker for breast carcinoma. Elevated CA 15-3
levels are also found in patients with pancreatic, lung,
ovarian, colorectal and liver cancer and in some benign
breast and liver diseases.
● It is not useful for diagnosis. It is most useful for monitoring
therapy.
CA 125
● Although CA 125 is a marker for ovarian and endometrial
carcinomas, it is not specific. CA 125 elevates in pancreatic,
lung, breast, colorectal and gastrointestinal cancer, and in
benign conditions such as cirrhosis, hepatitis, endometriosis,
pericarditis and early pregnancy.
● In the detection of recurrence, use of CA 125 level as an
indicator is about 75 % accurate.
CA 19-9
● CA 19-9 is a marker for both colorectal and pancreatic
carcinoma. However elevated levels were seen in patients
with hepatobiliary, gastric, hepatocellular and breast cancer
and in benign conditions such as pancreatitis and benign
gastrointestinal diseases.
● CA 19-9 levels correlate with pancreatic cancer staging.
● It is useful in monitoring pancreatic and colorectal cancer.
β2 -microglobulin
β2 -microglobulin is a marker for multiple myeloma, Hodgkin
lymphoma. It also increases in chronic inflammation and viral hepatitis.
Ferritin
Ferritin is a marker for Hodgkin lymphoma, leukemia, liver, lung and
Breast cancer
breast cancer.
CA 15-3 Monitoring
HER-2 Monitoring
Thyroglobulin It is a useful marker for detection of differentiated
CA 27.29 Monitoring
thyroid cancer.
Ovarian cancer
Immunoglobulin
CA 125 Monitoring
● Monoclonal paraproteins appear as sharp bands in the
Pancreatic cancer
globulin area of the serum protein electrophoresis.
CA19-9 Monitoring
● Bence-Jones protein is a free monoclonal immunoglobulin
light chain in the urine and it is a reliable marker for multiple
myeloma.
RECEPTOR MARKERS
● Estrogen and progesterone receptors are used in breast
cancer as indicators for hormonal therapy.
● Patients with positive estrogen and progesterone receptors
tend to respond to hormonal treatment.
C-erbB2 (HER-2 Neu)
● It is receptor for epidermal growth factor (EGF) but it doesn’t
contain EGF binding domain. It serves as a co-receptor in
EGF action
● In the case of increased expression of C-erbB2 leads the
auto-activation and increased signal transduction
● An important factor for carcinogenesis and metastasis
● Normal cell growth may be over grown in some cancer
GENETIC CHANGES
Four classes of genes are implicated in development of cancer:
VILLAGRACIA, JALEN C. MT 3-YA-8 6
CC2 LEC
MIDTERMS WEEK 1: BLOOD GAS AND PH
MEASUREMENT
ACID-BASE Balance
● dissociation of H2CO3 increased HCO3 in RBC causing it to
diffuse into the plasma
● HCO3 and H2CO3 are renewable Assessment of Acid-Base Balance
● HCO3 + H2CO3 ratio = 20:1
LUNGS
● respiratory control: CO2 excretion
● CO2 diffuses into alveoli and is eliminated through ventilation STEP 1: Evaluate pH
● pH 7.40: optimum for arterial blood
● chloride-isohydric shift: buffering effects of hemoglobin causing
venous blood to be 0.03 unit lower in pH
● each Celsius above 37: Inc pH by 0.015
● To maintain pH:
● neutralize acid as they are generated
● elimination of the acid permanently on a continuous basis.
KIDNEY
● excretion: generation of alkali or reabsorption of HCO3 from the
glomerular filtrate and add it to the blood
● 50-100 mmol/L of acid: must be excreted daily by the kidney
(urine pH is 4.5)
STEP 2: Evaluate lungs
● pCO2: index or efficiency of gas exchange
● not a measure of CO2 concentration
● total CO2: CO2 + H2CO3 + HCO3
● ref range: 19-24 mmol/L - arterial
○ 22-26 mmol/L - venous
● inc heparin: blood = inc pCO2 (12-15%)
● inc pCO2: barbiturates, morphine, alcoholism
● To maintain pH: retention of elimination of CO2
STEP 3: Evaluate kidneys
● To maintain pH:
○ excreting acid: NH4
○ reabsorption of HCO3
Plasma and Urine Bicarbonate
● inc HCO3: IV infusion of lactate, acetate, and HCO3 STEP 4: Evaluate oxygenation
● dec HCO3: Diuretic, reduced, reabsorption, chronic nephritis ● hypoxia: dec pO2
● HCO3 excretion rate ● reflects availability
26-30 mmol/L Urinary excretion of HCO3 ● changes rapidly
● dec 60-70% venous blood
10 mEq/day Normal excretion rate ● O2 dissociation/ association = pO2 + affinity of hemoglobin
● dec pO2: myocardial infarction, intestinal pneumonia, congestive
dec 25 mmol/L Ceased excretion of HCO3 heart failure, people living in high altitude area
Blood Buffers
1. HCO3: H2CO3: major extracellular blood buffer
2. Plasma proteins: weak acid/base
3. Hemoglobin: O2 carrying
a. 1 gram hemoglobin carries 1.39 ml of oxygen
b. 1 mole of hemoglobin binds 1 mole of oxygen
4. Inorganic phosphate
STEP 5: Evaluate compensation
a. HPO4:H2PO4 = 3:1
● the respiratory and metabolic system works together to keep the
body’s acid base balance within normal limit
Henderson-Hasselbach Equation
● pH depends on the ratio of HCO3 and pCO2
RESPIRATORY ACIDOSIS
● expresses acid base relationship and relates the pH of a solution
to the dissociation properties of the weak acid
●
RESPIRATORY ALKALOSIS
VILLAGRACIA, JALEN C. MT 3-YA-8 7
CC2 LEC
METABOLIC ACIDOSIS Allen’s test
● test done to determine that collateral circulation is present from
the ulnar artery in case thrombosis occur in the radial artery
Pre-analytical considerations:
● standing specimen: dec pH, Inc pCO2, dec pO2
● chilled: dec pH-RBC metabolism consumes O2 and liberates
METABOLIC ALKALOSIS acidic metabolites
● glycolysis: dec pH
● inc anticoagulant: dec pH: most common error
● dec temperature: inc oxygen solubility, oxyhemoglobin curve shift
to the left
Quality control
● 3 levels of control: acidosis, normal, alkalosis
● 1 level control sample every 8 hours
● 3 level control every 24 hours
● single point calibration: used as a “drift check” to detect changes
in response and/or deterioration in performance
METHODS
Gasometer
● Van Slyke
● Natelson:
○ Mercury: vacuum
○ Caprylic alcohol: anti-foam
○ Lactic acid
○ NaOH and NaHSO3
ACID-BASE DISORDER Electrodes
Respiratory acidosis A. pH: potentiometry
● inc CO2: slow breathing 1. Silver-silver chloride electrode: ref electrode
● compensation: kidneys: retain HCO3 and excretion of acid 2. calomel electrode (Hg2Cl2): ref electrode
● after compensation: inc pCO2, inc HCO3, pH <7.4 3. glass electrode: most common
● maximal compensation requires 5 days (90% in 3 days) B. pO2
● restriction of NaCl: inc HCO3 1. Clark electrode: polarography-amperometry
● inc 10 mmHg pCO2: inc 1 mEq/L HCO3 C. pCO2
● COPD, Myasthenia gravis, CNS disease, Drug overdose 1. Severinghaus electrode: potentiometry
(morphine, barbiturates, opiates), Botulism, Stroke, Myxedema, pO2 continuous monitoring
Pneumonia A. Transcutaneous (TC) electrode
Respiratory alkalosis ● place on directly to the skin
● dec CO2: rapid breathing ● neonates and infants
● psychogenic stimulation: inc pH ● non-invasive
● compensation: kidneys: dec reabsorption HC03
● after compensation: dec pCO2, dec HCO3, pH >7.4 Factos
● compensation completed: 2-3 days 1. Temperature
● dec 10mmHg pCO2: dec 2 mEq/L HCO3 ● optimum: 37C +/- 0.1
● + hypokalemia ● most impotratnt factor
● anxiety, severe pain, aspirin overdose, hepatic cirrhosis, gram ● inc 1C = dec 7% pO2, inc 3% pCO2
negative sepsis, salicylate, progesterone, drugs, pregnancy ● electrode sample chamber
Metabolic acidosis 2. Inc plasma proteins
● dec HCO3 ● inc pO2: build up on electrode membrane
● K efflux 3. Bacterial contamination
● compensation: lungs: dec pCO2 (hyperventilation) ● dec pO2: bacterial consumption
● after compensation: dec HCO3, dec pCO2, pH <7.4 4. Improper specimen transport
● compensation completed: 12-24 hours ● dec pH, inc PCO2, dec pO2
● dec 1 mEq/L HCO3: dec 1-1.3 mmHg pCO2 5. Air bubbles
● + hyperkalemia and hyperchloremia ● inc pO2: 4mmHg/2 mins
● DIabetic ketoacidosis (Normochloremic, low/elevated anion gap), ● dec pCO2: 4mmHg/2 mins
lactic acidosis (alcoholism), renal failure, diarrhea
Metabolic alkalosis
● inc HCO3
● compensation: lungs: inc pCO2 (hypoventilation)
● after compensation: inc HCO3, inc pCO2, pH >7.4
● compensation completed: 12-24 hours
● inc 10 mEq/L HCO3: inc 6 mmHg pCO2
● +hypokalemia and hypochloremia
● Vomiting (Cl loss)
METHODS OF ANALYSIS
Arterial Blood Glass
● specimen: arterial blood
● anticoagulant: lithium heparin
● ratio: 0.05 ml heparin/ml of blood
● syringe: tuberculin
● winged infusion set not recommended
● collected anaerobically
VILLAGRACIA, JALEN C. MT 3-YA-8 8
CC2 LEC
MIDTERMS WEEK 2: INTRO TO ENDOCRINE Hypothalamic cells
Magnocellular Neurons
SYSTEM ● Supraoptic nuclei - Arginine Vasopressin (AVP) aka Anti-Diuretic
Hormone (ADH)
Endocrine System ● Paraventricular nuclei - oxytocin
● A network of DUCTLESS tissue organs capable of synthesizing,
storing, and secreting a substance (stimulant/inhibitor) Pituitary gland (hypophysis)
● Considered to be the regulatory system of the body. ● Master Gland
(homeostasis) ● Located in the Sella Turcica of the sphenoid bone
● Connected to the infundibular, stalk to the median eminence of
Functions of the Endocrine System the hypothalamus
● Control chemical and water balance in the body. ● General function: Feedback Loops, Pulsatile Secretion and
● Control growth and metabolism. Diurnal rhythm
● Control embryonic development and preparation for nurturing a ● Functional by 7th-9th week gestation
newborn.
● Influence sexual behavior, stimulate growth and maturation of the Feature Function of Pituitary Glands
gonads. ● Feedback loop
● Feedback to the nervous system. ○ Short Feedback Loop
○ Long Feedback Loop
Operational Mechanism ○ Ultrashort feedback loop
● Nervous system monitors environment (NS sends message to ○ Open-loop
endocrine gland) ● Pulsatile secretion
● Endocrine glands produce and secrete hormones into blood ○ LH median interpulse is 55 mins (peak at 40 mins)
(hormones hit target organ) ○ GH median enterprise is 2-3 hours
● Target organ produces substances (substance is picked up by ● Diurnal variation
receptors and brain stops sending message to endocrine glands) ○ Regulated through external signals (Light-Dark
changes; Daylight-Darkness)
Endocrinology ● Zeitgeber
● Study of hormones, hormone producing glands, and abnormalities ○ (timer giver) process of synchronizing external
of hormones and hormone producing glands. cues with the internal biologic clocks.
Disorders related to the Endocrine System 3 Major Structures
● Tumors, Damage to cells or tissues, Hyposecretion, ● Adenohypophysis - anterior pituitary gland
Hypersecretion ● Neurohypophysis - posterior pituitary glands
● Intermediate lobe - pars intermedialis
Hormones
● are secretions of endocrine glands that act upon a specific tissue Neurohypophysis (Posterior Pituitary Gland)
organs other than its source ● Storage region for ADH and Oxytocin
● defined as a substance that acts at a site distant from its place of ● Connected to supraoptic (ADH) and paraventricular (Oxytocin)
origin nuclei of the Magnicellular apparatus of the hypothalamus
● its action may be described as a FEEDBACK MECHANISM ● Not a true endocrine gland
● Hormone release is stimulated by nipple suckling and serum
Feedback Mechanism osmolality.
● Positive feedback - increase in the product results to elevation of
the activity of the system. Oxytocin (Neurohypophyseal Secretions)
● Negative feedback - increase in the product results to decreased ● Stimulates smooth muscle contraction of uterus and mammary
activity of the system. glands.
● Labor and parturition
Types of Hormone Action ● Ejection of milk
● Endocrine - classic simple
● Paracrine - adjacent cell, interstitial space Antidiuretic Hormone (ADH) or Vasopressin (AVP)
● Autocrine - self-acting (Neuropophyseal Secretions)
● Juxtacrine - adjacent cell, direct contact ● aka Arginine Vasopressin, Vasopressin
● Exocrine - lumen of gut ● ADH or AVP
● Neurocrine - neural hormone of nearby cells ● central role in water balance
● Neuroendocrine -neural hormone for distance cells ● acts on V2 receptors lining the epith of collecting ducts and
● Intracrine - action within the cell source ascending loop of henle
Structural Class of Hormones Diabetes Insipidus
● Peptide/proteins - large molecules and cannot cross the cell ● Excessive urination with increased urine output
membrane. ● AVP deficiency
○ exists in form of secretory granules (cleavable) ● Result of tumor, trauma, and autoimmunity
○ Water soluble and not protein bound ● Low lvls of AVP and High plasma Osm = DI
● Glycoproteins - FSH, hCG. TSH, EPO ● Water deprivation with series of serum and urine OSm
● Polypeptides - ACTH, ADH, GH, Angiotensin, Calcitonin, determination may also be used.
Cholecystokinin, Gastrin, Glucagon, INsulin,
Melanocyte-Stimulating Hormone, Oxytocin, PTH, Prolactin, Syndrome of Inappropriate ADH
Somatostatin ● Euvolemic
● Steroids - lipid molecules with cholesterol as precursor ● hypoosmolar
○ water INSOLUBLE and protein-bound ● hyponatremia with
○ Produced by Adrenal Glands, Gonads and ● hyperosmolar urine
Placenta ● inability to dilute urine
○ Ex: aldosterone, cortisol, estrogen, progesterone,
testosterone, and Activated VIt D2 Adenohypophysis (Anterior Pituitary Gland)
● Amines - AA derivatives and considered as a intermediary ● true endocrine gland
between steroids and protein hormones ● largest part of the pituitary gland
○ Ex: Adrenaline, Noradrenaline, Thyroxine, ● produces and secretes tropic and/or direct effector
Triiodothyronine peptide/glycoprotein hormones
VILLAGRACIA, JALEN C. MT 3-YA-8 9
CC2 LEC
• Help regulate contraction of smooth and cardiac muscles and
secretion of glands
ADENOHYPOPHYSEAL SECRETION
• Help maintain activities of immune system
CELLS
• Plays a role in the smooth sequential integration of growth and
SOMATOtrophs Growth Hormone/ development
SOMATOtropin • Contribute to the basic processes of reproduction, gamete
production, nourishment of the fetus and embryo
LACTOtrophs proLACTin • Help maintain homeostasis
THYROtrophs THYROID Stimulating Hormone Types of Hormones
• Circulating hormones/Endocrines: acts on distant target cells
GONADOtrophs GONADOtropins (Follicle • Local Hormones
Stimulating Hormone and ▫ Paracrines
Luteinizing Hormone) ▫ Autocrines
CORTICOtrophs Cleavable prooiomelanocortin Functional Types of Hormones
(ACTH, b-endorphin,
• Releasing Hormones: ▫ from hypothalamus; promote secretion of Ant.
b-lipotropin)
Pituitary hormones
• Inhibitory Hormones: ▫ from hypothalamus & GIT; suppress the
Tropic Hormones - acts on endocrine organ secretion of a particular hormone
Gonadotropins • Tropic Hormones: ▫ stimulate growth & activity of other endocrine
● FSH - folliculogenesis (women) and spermatogenesis (men) glands
● LH - Leydig Cells’ testosterone production and ovulation • Effector Hormones: ▫ secreted by all endocrine glands & w/ non
● TSH - stimulates thyroid activity endocrine cells as targets
● ‘ACTH - stimulates adrenal cortex
Steroids
Direct effectors - acts on peripheral tissues • Derived from cholesterol
● GH - direct effect on substrate metabolism in numerous • transported to blood stream through attachment to transport protein •
tissue (ex. liver) E.g. ▫ aldosterone ▫ cortisol ▫ estrogen ▫ progesterone ▫ testosterone ▫
● Prolactin - breast tissue development and (with El and androgens
progesterone) and initiation and maintenance of lactation.
Biogenic Amines(AA)
2 Physiologic Regulatory Systems • tyrosine
• Endocrine system ▫ Thyroid hormones
• Nervous system T3-triiodothyronine
▫ Neuroendocrine System T4-thyroxine
▫ Adrenal hormones
Endocrine System Epinephrine
• consists of ductless glands, which secrete hormone directly into the Norepinephrine/Cathecholamines
circulatory system
Peptides and Proteins
• synthesized by rough ER
• hypothalamic releasing and inhibiting hormone
• E.g. ▫ oxytocin ▫ ADH ▫ insulin ▫ glucagon ▫ GH ▫ calcitonin ▫ PTH
Glycoproteins
• AA derivatives with CHO groups
• e.g. ▫ TSH ▫ FSH ▫ LH
Eicosanoids
• Fatty acids
• with 20 carbon atom fatty acid (arachidonic fatty acid), involved in
cellular activity
• E.g. ▫ prostaglandin
Major Glands of Endocrine System
• Pituitary Gland
• Thyroid Gland
• Parathyroid Gland
• Adrenal Gland
• Pancreas
• Reproductive Glands (ovaries & testes)
• Thymus Gland
• Pineal Gland
Hormones
• Greek word “hormon” → to set in motion
• Intercellular chemical signal transported to act on tissues at another
site of the body to influence their activity
• Transfer information and instructions from one set of cells to another
Characteristics of hormones Hypothalamus
• Produced by a specific endocrine gland • Portion of the brain located in the walls and floor of third ventricle
• Hormones are released directly from the endocrine gland to the blood • Collection of specialized cells located at the central part of the brain
circulation and carried to the site of action as a free hormone or bound • Control the pituitary gland by production of chemicals that stimulate
to transport protein or suppress hormone secretion of pituitary
• Acts at a specific site (target site) to induce certain characteristic,
biochemical changes. RESPONSE PATTERN
1. Open-loop negative feedback mechanism
Functions of Hormones: Ex. Hypothalamus
• Regulate the chemical composition and volume of the ECF
• Help regulate metabolism and energy balance
VILLAGRACIA, JALEN C. MT 3-YA-8 10
CC2 LEC
Idiopathic Galactorrhea
● Lactation occuring in women with normal prolactin levels is
defined as idiopathic galactorrhea
● This condition is usually seen in women who have been pregnant
several times and has no pathologic implication.
Growth Hormone
● Most abundant
● Secretion is erratic and short burst
2. Pulsatility – pulse frequency of secretion ● Ave. interpulse of 2-3hrs (highest during sleep)
• INCREASING the frequency of GnRH pulses – reduces the ● Release is promoted by GHRH
gonadotroph secretory response decreasing the pulse frequency, ● INCREASED IN: Acromegaly, Gigantism, Chronis malnutrition,
increases the amplitude of the subsequent LH impulse. renal disease, cirrhosis, and sepsis
● DECREASED: hyperglycemia, obesity and hypothyroidism.
3. Cyclicity – ▫ Nervous system – regulates this function
▫ Hormone secretion is dependent on the time of the day. ACROMEGALY
▫ Ex. ACTH – peak occurs in the morning ● GH excess in adults. Mostly due to Pituitary Tumor (>50ng/mL or
220pmol/L)
Hormones: ● Characterized by overgrowth of the bones and soft tissues (face
• TRH: thyrotropin releasing hormones and extremities)
• GnRH: gonadotropin releasing hormone ● Usually with diastema (gap between the frontal teeth)
• GH-IH: growth hormone inhibiting hormone ● A hypermetabolic condition thus heat intolerance and excessive
• GH-RH: growth hormone releasing hormone sweating may also be present.
• CRH: corticotropin releasing hormone
• PIF: prolactin inhibiting factor Management of Hypersecretion of GH
● Treatment is tumor ablation (transhpenoidal adenomectomy)
Hypophysiotropic hormones ● Irradiation
● Somatostatin analogs and dopaminergic agonists.
● Pegvisomant
Screening Test
● Somatomedin C or insulin-like growth hormone test
● Acromegaly: increased IGF-1
● GHD-low: IGF-1
Confirmatory Test
● Oral glucose loading test
● Overnight fasting
GONADOTROPINS ● The patient is given a 100g oral glucose load
● FSH - folliculogenesis in women and spermatogenesis in men ● GH is measured at time zero and at 60 and 120 minutes after
● LH - testosterone production of Leydig cells and ovulation and glucose ingestion.
final follicular growth ● Following oral glucose loading. GH is undetectable in normal
patients.
THYROTROPIN
● THYROID STIMULATING HORMONE - GIGANTISM
● main stimulus for iodine uptake by thyroid ● Juvenile GH excess
● GH excess before long-bone growth
CORTICOTROPIN
● ADRENOCORTICOTROPIC HORMONE GH deficiency
● Feedback hormone for/of cortisol ● In children due to tumors such as craniopharyngiomas (Dwarfism)
● Regulates adrenal androgen synthesis ● In adults due to structural and functional abnormalities of the
● Deficiency may lead to atrophy of adrenal gland’s G and R zone pituitary gland.
● Aging
PROLACTIN
● Aka Luteotropic Hormone/Luteotropin Screening Tesr
● Structurally similar to GH ● Exercise test: Physical Activity Test
● Initiates and maintains lactation ● Patient prep: Complete Rest for 30 mins (Fasting Serum)
● Promotes breast development in conjunction with Progesterone
and Estrogen Confirmatory Test:
● Considered as stress hormone ● Insulin Tolerance Test - GOLD STANDARD
● Arginine Stimulation Test - 2nd GS
PROLACTINOMA
● Most common pituitary tumor HYPOPITUITARISM
● PREMENOPAUSAL: Irreg mens/amenorrhea, infertility or ● Panhypopituitarism - general loss of pituitary function.
galactorrhea ● Monotropic hormone deficiency - one type of adeno hypertrophic
● MEN/POSTMENOPAUSAL: pituitary mass (Headache and Visual cell.
complaints), reduced libido
Pineal gland
Conditions associated to Hyperprolactinemia Midbrain
Pituitary adenoma Melatonin
Infertility Nerve stimuli
Amenorrhea Sleep wake cycle
Galactorrhea
Acromegaly PITUITARY GLAND
Renal Failure • small egg shaped gland located at the base of the brain beneath the
Cirrhosis hypothalamus
Primary and Secondary Hypothyroidism • master gland
Polycystic Ovary Syndrome • divided into 2 lobes: anterior & posterior
Anterior Pituitary Gland
• Composed of three cell types:
VILLAGRACIA, JALEN C. MT 3-YA-8 11
CC2 LEC
▫ Chromophobe (50%) ▫ Acidophilic (40%) ▫ Basophilic (10%)
FSH: growth and maturity of ovarian follicles, estrogen secretion,
FIVE types of cell by immunological tests: promotes endometrial changes, spermatogenesis
1. Somatotroph – GH
2. Lactotrophs – Prolactin LH: ovulation and secretion of androgens and progesterone, initiates
3. Thyrotroph – TSH secretory phase of mens, formation of corpus luteum and development
4. Gonadotroph – α and β subunits of FSH & LH of testicular cells
5. Corticotroph – Proopiomelanocortin (POMC) - ACTH β endorphin &
β lipotrophin Adrenocorticotropic Hormone (ACTH)
• acts on the adrenal cortex to stimulate growth and secretion of
Anterior Pituitary Gland corticosteroids
• GH, PRL, TSH, FSH, LH, ACTH • follows circadian rhythm
▫ regulates the activity of thyroid, adrenals, and reproductive • elevated during times of stress
glands
• also secretes ENDORPHINS Summary:
▫ acts on the nervous system and reduce feelings of pain • GH: growth of bone and soft tissues
• PRL: for lactation
Adenohypophysis hormones • TSH: release of thyroid hormones
• FSH: growth of the follicle (female) and initial wave of
spermatogenesis (male)
• LH: ovulation and final follicular growth (female) and production of
testosterone (male)
• ACTH: release of cortisol
Posterior Pituitary Gland
• Oxytocin or pitocin: for contraction of uterus and ejection of milk
primed with estrogen
• ADH or arginine vasopressin or pitressin: permeability of kidney
tubules
Growth Hormone (Somatotropin) Oxytocin
• exerts major effects on cartilage and growth of long bones • Major effect: smooth muscle contraction
▫ AA transport and nucleic acid & CHON synthesis • Stimulates contraction of the gravid uterus
▫ increases hepatic glucose effect w/ anti-insulin effect in • Contributes directly to uterine contractions during labor on the
muscles myometrium and promotes prostaglandin secretion • Hemostasis at the
▫ increases lipolysis elevating plasma free FA (ketogenesis in placental site after delivery
diabetes) • HL: 3-5 minutes
FACTORS AFFECTING GH SECRETION Significance
• Useful test in some pregnant women in predicting preterm labor
• Oat cell carcinoma of the lung and adenocarcinoma of the pancreas
Arginine vasopressin
• Maintain osmotic homeostasis by regulating balance
• Nonapeptide that acts on the DCT and collecting tubules of the
kidneys
• Urine/serum /pl asma osmolality and thirst may stimulate ADH
secretion
• 5-10% drop in blood volume and blood pressure triggers
(baroreceptors) the release ADH
Hormones that influences secretion and metabolic effects of GH: • Responsible for the maintenance of blood volume, pressure and
thyroxine, cortisol, estrogen, somatostatin, somatotropin releasing tonicity
factor • Basal plasma vasopressin: 2.3-3.1pg/uL
• Diagnostic test: Overnight water deprivation test
Prolactin (PRL)
• acts directly on mammary glands DISEASES ASSOCIATED WITH HORMONES OF THE PITUITARY
• controls the initiation and maintenance of lactation GLAND
▫ induces ductal growth, development of breast lobular Dwarfism
alveolar system and synthesis of specific milk proteins • hyposecretion of GH during growth years
• requires priming by estrogens, progestins, corticosteroids, thyroid • types:
hormones, and insulin ▫ Achrondroplasia
• Men: 1-20ng/mL ▫ Hypoachondroplasia
• Women: 1-25 ng/mL ▫ Spondyloepiphyseal Dysplasia
▫ Diastrophic dysplasia
3 Forms of Circulating Prolactin:
1. Non-glycosylated monomer - major form Test of GH insufficiency
2. Big prolactin - consists of dimeric and trimeric glycosylated form • Stimulation tests
3. Macro-prolactin – which is less physiologically active for ▫ After exercise or during sleep, GH normally increases
▫ Clonidine (potent GH stimulant)
Specimen consideration
• Collect 3-4 hours after the patient awakes GH deficiency
• Highest level: 4-8am; 8-10pm • Gold standard test: insulin tolerance test
• 2nd confirmatory test: L-DOPA or Arginine stimulation test
Thyroid Stimulating Hormone (TSH)
• Increases: GH excess
▫ size of thyroid follicular cells • Over production of GH
▫ release of thyroxine from thyroid colloid follicles • Gigantism → childhood
▫ uptake of iodide by thyroid cells from ECF • Acromegaly → Adults
▫ thyroxine biosynthesis
• differentiates pituitary (2°) hypothyroidism from primary Screening test
hypothyroidism • Somatomedin C test
VILLAGRACIA, JALEN C. MT 3-YA-8 12
CC2 LEC
• Fasting serum - Specimen requirement SIADH
• Complete rest - Specimen requirement • Occurs when there is uncontrolled secretion of ADH without any
known stimulus for such release
Gigantism • hypersecretion of GH during childhood • ADH is release even though the blood volume is normal or increased
and plasma osmolality is low
Acromegaly • hypersecretion of GH during adulthood • Ectopic tumor production of ADH: small cell carcinoma of the lung
Features: • CNS disease
• coarse facial features • Pulmonary disease
• soft tissue thickening (lips) • Administration of certain drugs
• spade like hands • Diagnosis: Water load test
• protruding jaw (prognathism)
• Sweating Laboratory Measurement of Some Hormones Secreted by the
• impaired glucose tolerance or DM Pituitary Gland
Diagnosis of Acromegaly
• OGTT and GH measurement
• Hyperglycemia should suppress GH to <1 ug/L
• After treatment, failure to suppress GH below 2 ug/L may cause
higher prevalence of DM, heart disease, and hypertension
Galactorrhea
• inappropriate production of breast milk
• due to hypersecretion of PRL
• symptoms: irregular menstruation, menopausal symptoms, milk
discharges, difficulty in getting erection, breast tenderness and
enlargement
Amenorrhea
• absence of menstrual cycle in females Growth Hormone Immunoassay
• due to hypersecretion of PRL • uses specific GH antibody
Impotence • require multiple measurements
• inability to attain penile erection in males ▫ draw specimens every 20-30 minutes over a 12-24 hours
• due to hypersecretion of PRL period
• Insulin tolerance test: to produce hypoglycemia and provoke GH
Infertility release
• lack of FSH and LH in both male and female ▫ Basal: 2-5 ng/mL or ug/L
• inability to conceive after 1 year of unprotected intercourse ▫ Insulin tolerance: >10 ng/mL
Arginine/L-dopa: >7.5 ng/mL
Cushing’s disease
• hypersecretion of ACTH hGH-EASIA
• leads to bilateral adrenal hyperplasia and cortisol overproduction • solid phase Enzyme Amplified Sensitivity Immunoassay
• Obesity!!! • Mab 1-hGH-Mab-HRP
• absorbance is measured after colorimetric reaction
Addison’s disease ▫ Day: <0.2-10 uIU/mL
• secondary (ACTH) or tertiary (CRH) adrenal insufficiency ▫ Night: 30 uIU/mL
• hyposecretion of glucocorticoids and aldosterone
Prolactin Immunoassay L
Polyuria • homologous competitive binding immunoassay/sandwich technique
• deficient ADH production or action • uses two or more antibodies directed at different parts of the PRL
▫ Hypothalamic DI molecule
▫ Nephrogenic DI • hook effect
▫ Psychogenic or primary polydypsia ▫ Adult male: 3-14.7 ng/mL or ug/L
▫ Adult female: 3.8-23 ng/mL or ug/
Syndrome of Inappropriate ADH Secretion (SIADH) ▫ Pregnancy, 3rd tri: 95-473 ng/mL
• autonomous sustained production of AVP in the absence of known
stimuli for its release ACTH Immunoassay
• malignancy, CNS diseases, pulmonary disorders drug therapies • chemiluminescence and ELISA
• decreased urine volume, increased sodium concentration and urine • related test: cortisol
osmolality • reacts with intact ACTH and ACTH fragments
▫ Adults: 5-80 pg/mL (X 0.22= pmol/L)
HYPOPITUITARISM ▫ Specimen: P, EDTA
• Panhypopituitarism ▫ tumors ▫ trauma ▫ radiation therapy ▫ infarction ▫
infection ▫ familial ▫ idiopathic Dynamic Function Test
• Monotropic hormone deficiency • stimulating or suppressing a particular hormonal axis, and observing
the appropriate hormonal response
True Diabetes Insipidus ▫ If excess is suspected, conduct a suppression test
• Hypothalamic/neurogenic/cranial/ central diabetes insipidus ▫ If deficiency is suspected, conduct a stimulation test
• Deficiency of ADH with normal ADH receptor, due to hypothalamic or ▫ Stimulus: exogenous analogue of a trophic hormone or a biochemical
pituitary disease or physiological stress like hypoglycemia or exercise
• Failure of the pituitary gland to secrete ADH
• Large volume of urine is excreted (3-20L/day) Insulin Stress Test
• done when hypopituitarism is suspected
True Diabetes Insipidus • also known as Insulin Tolerance Test
• Hypothalamic/neurogenic/cranial/ central diabetes insipidus • insulin is administered to produce hypoglycemic stress (<2.2 mmol/L)
• Deficiency of ADH with normal ADH receptor, due to hypothalamic or • Tests the ability of Anterior Pituitary Gland to produce ACTH and GH
pituitary disease ▫ GH >6 ug/L
• Failure of the pituitary gland to secrete ADH ▫ Cortisol > 500 nmol/L
• Large volume of urine is excreted (3-20L/day)
VILLAGRACIA, JALEN C. MT 3-YA-8 13
CC2 LEC
TRH Test Ovulatory phase: 0.2-17.2 mIU/mL (0.2-17.2 IU/L) L
• assesses the adequacy of Anterior Pituitary Reserve, or to evaluate uteal phase: 1.1-9.2 mIU/mL (1.1-9.2 IU/L)
hypothalamic disease (TSH response to TRH is delayed: TSH higher ▫ Postmenopausal: 19.3-100.6 IU/L
at 60’ than 20’) ▫ Male: 1-15.4 mIU/mL (1-15.4 IU/L)
▫ Hyperthyroidism: pituitary response to TRH is flat
(TSH<2mU/L) ADH Measurement
▫ Hypothyroidism: exaggerated response (>25 mU/L) • measures the amount of antidiuretic hormone, or vasopressin, in
• TRH is given as an IV bolus blood
• Blood sampling done at 0, 20, and 60 minutes • Related tests: sodium and osmolality
▫ 270-280 mOsm/kg: <1.5 pg/mL (<1.4 pmol/L)
GnRH Test ▫ 280-285 mOsm/kg: <2.5 pg/mL (<2.3 pmol/L)
• assesses hypogonadism ▫ 285-290 mOsm/kg: 1-5 pg/mL (0.9-4.6 pmol/L)
• can be done together with anterior pituitary function test (IST, TRH, ▫ 290-295 mOsm/kg: 2-7 pg/mL (1.9-6.5 pmol/L)
GnRH tests) ▫ 295-300 mOsm/kg: 4-12 pg/mL (3.7-11.1 pmol/L)
• Normally,
▫ Adults: GnRH causes marked rise in LH (increments of >15 U/L) and
smaller rise in FSH (>2 U/L)
▫ Children: GnRH causes marked rise in FSH and smaller rise in FSH
ACTH Stimulation Test
• cosyntropin test or tetracosactide test
• small amount of synthetic ACTH is injected, and amount of cortisol or
aldosterone is measured
• distinguish whether the cause is adrenal (low cortisol and aldosterone
production) or pituitary (low ACTH production)
▫ cortisol should be increased by twofold to threefold within 60 minutes
▫ fasting (8 hrs)
LH Ovulation Dipstrip Urine Test
▫ - test approximately the same time each day
- reduce liquid intake two hours before testing
LH Immunoassay (EIA/IRMA)
• Mab1-LH-Mab2HRP
▫ measured using chromogenic reaction
▫ Absorbance proportional to LH concentration
• Mab1-LH-Mab2125I
Fertility test (male)
• Semen analysis
• Testosterone - 300-1100 ng/dl
• Prolactin - 7-18 ng/ml
• Luteinizing Hormone ( LH) - 2-18 mIU/ml
• Follicle Stimulating Hormone ( FSH): - 2-18 mIU/ml
• Estradiol ( Day 3): <50 pg/ml
Fertility test (female)
• FSH: measures your ovarian reserve (ovarian function)
• low levels of FSH & LH: hypogonadotropic hypogonadism
• high LH with a normal FSH level: PCOD (polycystic ovarian disease)
• high prolactin: hyperprolactinemia
• high estradiol (D3): poor ovarian reserve
• estradiol rises as follicle matures; useful for measuring follicular
activity
• mature follicles > 200-300 pg/ml of estradiol
• P >15 ng/ml about 7 days after ovulation: corpus luteum is functioning
normally
• low Day 21 P suggests the cycles was anovulatory (no egg was
produced)
Serum FSH Measurement (IRMA)
• measures the amount of follicle stimulating hormone (FSH) in blood
• Mab1-serum-Mab2125I
• used to assess and manage disorders of the endocrine glands,
including suspected infertility
• related tests: LH, PRL, testosterone, estradiol
Normal Values for serum FSH
▫ Female, menstruating:
Follicular phase: 1.4-9.9 mIU/mL (1.4-9.9 IU/L)
VILLAGRACIA, JALEN C. MT 3-YA-8 14
CC2 LEC
THYROID GLAND ● Metabolically active hormone
● also known as butterfly-shaped gland ● Produced by conversion of T4 within the liver and periphery
● consist of two lobes (one on either side of the trachea) located in ● Metabolic rate of every cell of the body
the lower part of the neck, just below the voice box (larynx) ● Encourages cellular differentiation
● The lobes are connected by a narrow band called isthmus ● Tissue growth and development
● By 11 weeks of gestation, the gland begins to produce ● Affect oxygen consumption
measurable amounts of hormone ● Calorie and vitamin/mineral metabolism
● Follicle is the fundamental structure unit of the thyroid gland ● Almost 70-80% is produced from the deiodination of T4
● 2 Types of Cells (conversion of T4 to T3 takes place in many tissue, particularly in
Follicular cell (T3 and T4) the liver and kidneys).
Parafollicular cells or C Cells (Calcitonin) ● Principal application of this hormone is in diagnosing T,
● Thyroglobulin is a glycoprotein; it acts as a preformed matrix thyrotoxicosis
containing tyrosyl groups; it is stored at the follicular colloid of the ● Better indicator of recovery from hyperthyroidism
thyroid gland ● Increased in the plasma level of T3 is the first abnormality seen in
● Controls the biosynthesis and release of thyroid hormones from hyperthyroidism
thyroglobulin
● Regulate carbohydrate, lipid, and protein metabolism Calcitonin (CT)
● Act on the CNS ● Participates in calcium homeostasis by responding to a
● Stimulate the heart hypercalcemia
● Physical growth and development ● Depresses the release of calcium from the bone
● Inhibits the bone-dissolving activity of osteoclasts
THYROID HORMONE SYNTHESIS
The Thyroid Gland - Histology CLINICAL DISORDERS OF THYROID GLAND
● Gland is composed of hollow spheres, called colloid follicles. HYPERTHYROIDISM
● Squamous epithelial cells, cuboidal cells (follicle cells) ● Excess of circulating thyroid hormones
● Colloid fills the follicle cavities. Follicle cells produce thyroglobulin ● Signs and symptoms: tachycardia, tremors, weight loss, heat
→ pro- hormone of T, and T. intolerance, and menstrual changes
● Primary hyperthyroidism: elevated T, and T4 (defects of thyroid
Thyroid Follicles gland), decreased TSH
● lodine trapping ● Secondary hyperthyroidism: increased FT4 and TSH (defects of
● Thyroid peroxidase enzyme converts lodide to lodine, attach pituitary gland)
● iodide to thyroxine
● Monoiodothyronine (MIT) and diiodothyronine (DIT) A. Thyrotoxicosis
● .Endocytosis on apical membrane ● Caused by excessive thyroid hormone in the circulation
● Lysosomal fusion and digestion ● Causes the cells to be overactive
● Release of T3 and T4 with the aid of TSH ● T3 thyrotoxicosis or Plummer's disease: FT3 is increased but FT4
normal with low TSH
THYROID HORMONE BINDING PROTEINS ● T4 thyrotoxicosis: T3 is normal or low but T increased with low
● Thyroxine Binding Protein TSH
● Transports majority of T3 (affinity for T3 is lower than T4) ● Laboratory results :
● Transports 70-75% of T4 ○ Elevated thyroid hormone serum levels
● Thyroxine Binding Pre-Albumin (transthyretin) ○ Decreased serum TSH
● Transports 15-20% of T4
● No affinity to T3 B. Grave's Disease (diffuse toxic goiter)
● Thyroxine Binding Albumin ● Autoimmune disease in which antibodies are produced that
● Transports T3 and 10% of T4 activate TSH receptor
● Features: exopthalmos (bulging eyes) and pretibial myxedema
NOTE ● Laboratory results:
● Protein bound hormones are metabolically inactive. ○ - Increased T3, T4, FT4I (Free T4 Index) and T3U
● Free hormones (FT3 and FT4) are (T3 Uptake)
● physiologically active ○ - Decreased or Normal TSH
● Protein bound hormones do not enter the cell and are considered C. Riedel's Thyroiditis
as biologically inert and functions as storage sites for circulating ● Inflammation of the gland
thyroid hormones ● Thyroid turns into woody or stone-hard mass
● Caused by: Viral infection and Bacterial infection
Thyroid Hormones
● There are two biologically active thyroid hormones: D. Subclinical Hyperthyroidism
○ - tetraiodothyronine (T4; usually called thyroxine) ● Shows no clinical symptoms but TSH level is low and FT3 and
○ - triiodothyronine (T3) FT4 are normal
● Derived from modification of tyrosine.
E. Sub-acute granulomatous/Sub- acute non-suppurative
Synthesis of thyroid hormones thyroiditis/ De Quervain thyroiditis (Painful thyroiditis)
● Active uptake of iodide into follicular cell ● Neck pain, low-grade fever and swings in thyroid function test
● Iodide-iodine - H2O2 (catalyzed by TPO) ● Thyroidal peroxidase (TPO) antibodies are absent; ESR and
● Active uptake of iodine at follicular/ colloid interface thyroglobulin test levels are elevated
● Incorporation of iodine onto tyrosine residues of thyroglobulin
● Coupling of iodinated tyrosines HYPOTHYROIDISM
● Storage of T3 and T4 ● Serum level of thyroid hormone is insufficient to provide for the
metabolic needs of the cells
Thyroxine (T4) ● Treatment with thyroid hormone replacement therapy:
● Principal secretory product Levothyroxine
● Dominant hormone produced from the thyroid gland ● Symptoms include: enlarged thyroid gland (goiter), Fatigue,
● All circulating T4 originates in the thyroid gland impairment of mental processes, loss of appetite, myxedema
● It is a good indicator of thyroid secretory rate Represents 80% of ● Causes: tissue damage and lack of dietary iodine
thyroid hormone
● Serves as the pro-hormone for T3 A. PRIMARY HYPORTHYROIDISM
● Elevated level causes inhibition of TSH secretion and vice versa ● inadequate secretion of thyroid hormones
● There is a problem with the thyroid gland itself
Triiodothyronine (T3) ● ➤ Laboratory results:
● Represents only 20% of the thyroid hormone produced from the ● decreased T3
gland ● decreased T4
VILLAGRACIA, JALEN C. MT 3-YA-8 15
CC2 LEC
● decreased free thyroxine index (FTI) decreased T3 uptake (TU), ● concentrated in the thyroid gland or excreted in the urine
increased TSH over the next few hours
● amount of iodine that goes into the thyroid gland can be
HASHIMOTO'S DISEASE (Chronic autoimmune thyroiditis) measured by a "Thyroid Uptake"
● Caused by a genetic abnormality in the immune system ● RIA for Calcitonin
● Involves massive infiltration of the thyroid gland by lymphocytes ● marker for medullary thyroid carcinoma
● Same symptoms with hypothyroidism ● Thyroid Ultrasound
● Most common cause of hypothyroidism ● use of high frequency sound waves to obtain an image of the
● Signs and symptoms: Weight loss thyroid gland and identify nodules
● • Loss of muscle mass ● - "solid" or a fluid-filled cyst
● • Hyperactivity yet quick fatigability ● - allows accurate measurement of a nodule's size
● • Insomnia ● determine if a nodule is getting smaller or is growing larger
● • Increased sweating during treatment
● • Nervousness ● Thyroid Needle Biopsy
● • Palpitations ● most reliable test to differentiate the "cold" nodule that is
● • Goiter cancer from the "cold" nodule that is benign
● Bulging ● "hot" nodules are rarely cancerous
● Causes:
● Pituitary tumors TESTS FOR THYROID EVALUATION
● Excessive TSH secretion 1. Blood tests
● Thyroid carcinoma A. TSH
● Toxic multi-nodular goiter ● Most useful test for assessing thyroid function
● All assays are capable of diagnosing primary hypothyroidism
MYXEDEMA ● 3 Generation of assays
● Peculiar non-pitting swelling of the skin
● Skin becomes infiltrated by mucopolysaccharides ● 2nd Generation
● Clinical features: "puffy" face, weight gain, slow speech, eyebrows ● 0.1 mU/L detection limits
thinned, dry and yellow skin and anemia ● Routinely used to monitor & adjust thyroid hormone
● Myxedema Coma: severe form of primary hypothyroidism replacement therapy
● Screen for hyperthyroidism & hypothyroidism
B. SECONDARY HYPOTHYROIDISM ● 3rd Generation
● Involves decrease in production of TSH leading to low serum ● 0.01 mU/L detection limits
levels of thyroid hormones ● Routinely used to monitor & adjust thyroid hormone
● Failure of the pituitary gland replacement therapy
● Laboratory results: All thyroid test values are decreased ● Screen for hyperthyroidism & hypothyroidsm
● less likely to give false-negative results
D.CONGENITAL HYPOTHYROIDISM/ CRETINISM ● More accurate distinguish between euthyroidism &
● .Defect in the development or function of the gland hyperthyroidism
● symptoms: physical and mental development of the child are ● ability to detect subclinical disease (mild degree of thyroid
retarded dysfunction due to large reciprocal change in TSH levels
● Screening test: T1 (decreased) even for small changes in Free T4
● Confirmatory test: TSH (increased)
B. Serum T4 and T3
E. SUBCLINICAL HYPOTHYROIDISM ● RIA: radioimmunoassay
● T3 and T1 are normal but TSH is 4 slightly increased ● Chemiluminometric assay
● Immunometric technique
OTHER DISORDERS OF THE THYROID ● Total T4 & T3
● Drug-induced thyroid disease ● Free T4 & T3
● Amiodarone-induced thyroid disease
○ Cardiovascular drug C. Thyroglobulin
○ High iodine content ● protein synthesized & secreted by thyroid follicular cells
○ Decreases thyroid hormone synthesis ● Pro-hormone in circulation
○ Hypothyroidal condition ● proof of presence of thyroid tissue (benign/malignant)
● Non-thyroidal illness ● ideal tumor marker for thyroid cancer
● Thyroid nodules ● patients
● Patients treated for thyroid CA:
LABORATORY ANALYSES ● undetectable thyroglobulin levels
● T3 resin uptake
- analyzes the capacity of thyroid binding globulin to bind thyroid Measurement:
hormones ● Double antibody (RIA)
- indirect measurement of the number of free binding sites on the TBG ● Enzyme-linked immunoassay (ELISA)
molecule ● Immunoradiometric assay (IRMA)
● Free thyroxine index (Ft4l) ● Immunochemiluminescent assay (ICMA)
- indirectly assesses the concentration of circulating free T4 ● Measurement depends on:
- calculated by multiplying the value of the total T4 by the percentage ○ Specificity of antibody used
value of the T3 resin uptake ○ Absence of anti thyroglobulin autoantibodies
○ Well-differentiated thyroid CA (+)
LABORATORY ANALYSES
● Thyroid antibody screens D. Thyroid autoimmunity/antibodies
● assay for the presence of thyroid-stimulating ● Thyroid stimulating antibodies (TSAB, TSI)
immunoglobulins ● TSH receptor antibodies (TRAB, TSHR-Ab)
● TRH stimulation test ● Grave's disease: antibody directed at TSH receptor
● measures pituitary TSH stores ● Chronic lymphocytic thyroiditis (Hashimoto's thyroiditis): TPO
● considered conclusive for hyperthyroidism antibodies
● Thyroid-releasing hormone is injected
● Blood sample are assayed for Thyroid-Stimulating Hormone 2. Nuclear Medicine
● TSH levels rise rapidly in a normal person Radioactive iodine
● TSH levels will not rise in a hyperthyroid patient ● Assessing metabolic activity of thyroidtissue
● lodine Uptake Scan ● Assisting in the evaluation & treatment of thyroid CA
● iodine is taken up by the thyroid gland (RAI uptake) ● Percentage of oral dose is taken by the thyroid gland
● dose of radioactive iodine on an empty stomach ● Radioactive iodine uptake
VILLAGRACIA, JALEN C. MT 3-YA-8 16
CC2 LEC
VITAMIN D
Radioactive iodine uptake ● Vitamin D shares striking similarities in origin with steroid
HIGH UPTAKE hormones
● Gland is metabolically active & producing significant amounts of ● A metabolic product of the cholesterol synthetic pathway
thyroid hormone ● Tissues involved in the synthesis: skin, liver, and kidneys
● High uptake with undetectable TSH: thyroid is acting ● Tissues it affects: gut, bone, and parathyroids
autonomously (hypothalamus pituitary- thyroid feedback system) ● De novo synthesis of vitamin D begins in the skin
● TSH surrogate (Grave's disease): ● 7-dehydrocholesterol is transformed to vitamin D3 by the action of
Immunoglobulin activates TSH ultraviolet light.
receptor= inc thyroid hormone - inc Radioactive lodine Uptake ● Vitamin D3 is biologically inert and must be further metabolized to
LOW UPTAKE the biologically active metabolite.
● Gland is metabolically inactive ● An enzyme in the liver, 25-hydroxylase, metabolizes min D3 to
25-hydroxy vitamin D.
"hot nodules" ● Serum 25-hydroxy vitamin D indicates the adequacy of vitamin D
● Take up significant radioactive iodine stores in the body.
● Unlikely thyroid CA ● An enzyme in the kidneys, renal renal 1- hydroxylase, under
● Benign regulation from PTH, completes the metabolism of vitamin D to
● Able to concentrate the active metabolite, 1,25-dihydroxy vitamin D.
"cold nodules'
● Show little or no radioactive iodine 1,25-dihydroxy Vitamin D (Active metabolite)
● Indeterminate/may be cancerous (majority are benign) ● In small intestinal:
● Malignant ○ upregulates expression of a number of genes that
● Unable to concentrate stimulate transepithelial calcium transport from the
intestinal lumen into the blood
3. Thyroid ultrasound ○ site of greatest absorption is the duodenum
● Assessment of thyroid anatomy ○ also stimulates absorption of phosphate.
● Characterization of palpable abnormalities ● In bone:
● Small size (<1cm) thyroid nodules seen ○ differentiation of osteoclast precursors to
osteoclasts
4. Fine Needle Aspiration Biopsy ○ stimulates osteoblasts to influence osteoclasts to
● Most accurate tool in evaluation of thyroid nodules mobilize bone calcium
● Identification & treatment of thyroid malignancy ○ does not directly affect mature osteoclast
● Palpation with ultrasound physiology
● Indeterminate with FNAB: surgical removal for definitive diagnosis ○ mineralization of bone
● Abnormal bone results when vitamin D is deficient or its
PARATHYROID GLAND metabolism is defective.
● ocated on or near the thyroid capsule; sometimes within the
L ● Increases blood calcium by augmenting intestinal absorption of
thyroid gland calcium. Blood calcium feeds back to parathyroid tissue and
● May also be found between the hyoid bone in the neck and affects synthesis and secretion of PTH.
mediastinum ● Direct transcriptional control over the PTH gene in the
● Smallest endocrine gland in the body parathyroids.
● Secretes parathyroid hormone (PTH): HYPERCALCEMIC ● The 1,25(OH)2D-vitamin D receptor complex binds to the
hormone. vitamin D response element upstream of the PTH gene and
downregulates PTH gene transcription.
Role of Parathyroid Hormone ● PTH stimulates production of 1,25(OH)2D, and 1,25(OH)2D,
● Prime role: to prevent hypocalcemia (regulates blood calcium) in turn, feeds back to decrease PTH secretion, all to maintain
● It preserves calcium and phosphate within the normal range blood calcium in the normal range.
● Major physiologic action is mineral homeostasis
● Involved in the metabolism of both calcium and phosphorus by Primary analytes of interest:
the kidney and bone ● -Total and lonized Calcium
● In Bone ● lonized (free) calcium is the biologically active component of
● - Increases bone resorption (breaking down) of calcium into circulating calcium (50% of circulating).
plasma ● Total calcium is being measured when calcium is measured
● In The Kidney in a serum chemistry panel.
● Increases renal reabsorption of calcium ● -Inorganic Phosphorus
● - To drive 1a-hydroxylation of 25-hydroxy vitamin D to ● retention causes a decrease in ionized calcium, leading to
produce the active metabolite of vitamin D, 1,25(OH)2D increased parathyroid hormone
(1,25-dihydroxy vitamin D) ● Parathyroid hormone
● Stimulates conversion of inactive Vitamin D to activated vitamin ● inc calcium phosphorus
D3.
● Indirectly stimulates intestinal absorption of calcium LABORATORY ANALYSES
● As calcium levels increase, PTH secretion is supressed allowing ● PTH C-terminal analysis:
urinary loss of calcium and calcium remain in bone ○ - examines the intact PTH molecule
● If calcium levels decrease, PTH is released. ○ -specific for detecting hyperparathyroidism
● PTH N-terminal analysis:
CALCITRIOL ○ measures both the whole PTH molecule
● is a form of Vitamin D that is used to treat and prevent low levels ○ amino-terminal fragments in the serum
of calcium in the blood of patients whose kidneys or parathyroid ● Nephrogenous CAMP:
glands (glands in the neck that release natural substances to ○ measures urinary portion of cAMP produced by
control the amount of calcium in the blood) are not working the kidneys
normally. ○ directly influenced by PTH and its excretion by the
renal tubules
HORMONAL CONTROL OF CALCIUM METABOLISM
● Parathyroid hormone (PTH) and vitamin D are the two hormones Analytes of secondary interest:
that play the dominant role in the regulation of calcium ● Calcitonin
homeostasis. ○ decrease calcium, inc phosphorus, counteracts
● Vitamin D - It should first be noted that vitamin D is in reality a parathyroid hormone (PTH).
hormone and, as is true of hormones in general, it is made at (a) ● -Vitamin D
site(s) different than the organs whose function it affects. ○ stimulates intestinal absorption of calcium
● -Magnesium
VILLAGRACIA, JALEN C. MT 3-YA-8 17
CC2 LEC
○ magnesium deficiency can inhibit the secretion of Secondary Hyperparathyroidism
PTH and also blunt its actions on target tissues ● Condition associated with the body's attempt to compensate for
● -Bicarbonate hypocalcemic state
○ PTH decreases bicarbonate reabsorption ● Seen in renal failure due to inexcretion of phosphorus
● Decreased calcium stimulates secretion of PTH
CLINICAL DISORDERS ● Laboratory Results:
Primary Hypoparathyroidism ○ Serum calcium is low
● - Hyposecretion of PTH ○ PTH is increased
● - Caused by: ○ Phosphorus is increased
○ surgical removal of the gland (thyroidectomy,
lymph node dissection) TERTIARY HYPERPARATHYROIDISM
○ trauma following surgery ● Autonomous PTH secretion and hypercalcemia in the setting of
○ radiotherapy directed at thyroid gland renal failure or after renal transplantation.
Laboratory results: ● prolonged stimulation of the parathyroid glands,, stimulates the
● - Low serum calcium development of parathyroid hyperplasia or adenoma similar to
● - high phosphorus that seen in primary hyperparathyroidism.
● PTH is often extremely elevated
Idiopathic Hypoparathyroidism ● Occurs with Secondary hyperparathyroidism Treated with
● Rare and hereditary parathyroidectomy
● Laboratory results:
○ -Very low serum calcium level
○ Very high phosphorus level
Pseudohypoparathyroidism
● Characterized by lack of responsiveness of renal or other organ
systems to PTH
● This results from uncoupling of the PTH receptor from adenylate
cyclase, due to a mutant stimulatory G protein (Gs).
● PTH binds its receptor but cannot activate the second messenger,
CAMP, and thus there is no response.
● Laboratory Results:
○ - Serum PTH levels are typically normal to
increased in this condition
Other Causes of Hypoparathyroidism
● Autoimmune destruction of parathyroid tissue associated with
other autoimmune diseases such as type 1 diabetes, Hashimoto's
thyroiditis, and Addison's disease.
● Mutations in the PTH gene
● Abnormal deposition of copper or aluminum in the parathyroid
glands
HYPERCALCEMIA
● Diagnosed when serum calcium levels rise
● Higher than 102 ng/L
● Sustained at level >100 mg/L
Primary Hyperparathyroidism
● most common cause of hypercalcemia in the outpatient setting
● physiologic defect lies with the parathyroid glands themselves
● autonomous nature of PTH production
● single adenoma, multiple adenomas, or hyperplasia of the
parathyroid glands.
● Laboratory Results:
○ Serum calcium is increased
○ PTH is increased
○ Phosphorus is normal to decreased
GENETIC SYNDROMES ASSOCIATED WITH PRIMARY
HYPERPARATHYROIDISM
● Multiple endocrine neoplasia, type 1 (MEN-1): This may result in
tumors of the parathyroids, pituitary, and pancreas. It results from
loss of a tumor suppressor gene that maps to human
chromosome 11.
● •Multiple endocrine neoplasia, type 2a (MEN-2a): This may result
in tumors of the parathyroids, medullary thyroid hyperplasia or
cancer, and pheochromocytoma. This results from an activating
mutation in the ret proto-oncogene, which resides on human
chromosome 10.
● Familial hyperparathyroidism: without other associated tumors.
The gene is not known but has been mapped to human
chromosome 1.
● Familial hypocalciuric hypercalcemia (FHH): result of a mutation
in the calcium sensing receptor and thus an increased "set point"
for calcium homeostasis. It is associated with mild hypercalcemia
and hyperparathyroidism, yet decreased (or low normal) urinary
calcium excretion. It is the decreased urinary calcium excretion
that distinguishes FHH from primary HPT, making this test very
valuable in distinguishing between the two
VILLAGRACIA, JALEN C. MT 3-YA-8 18
CC2 LEC
ADRENAL GLANDS CORTEX STEROIDOGENESIS
● Control of steroid hormone biosynthesis is complex, including
● Multifunctional organ that produces the steroid hormones and adrenocorticotropic hormone (ACTH) and angiotensin (Ang) II
neuropeptides essential for life ● All adrenal steroids are derived by sequential enzymatic
● Most pathologic conditions of the adrenal gland are linked by their conversion of a common substrate: cholesterol
impact on blood pressure and electrolyte balance ● Adrenal parenchymal cells accumulate and store circulating
low-density lipoproteins (LDL)
● The adrenal gland can also synthesize additional cholesterol
using acetyl-CoA, ensuring normal adrenal steroidogenesis in
patients with variable lipid disorders and in patients on
lipid-lowering agents
● Corticotropin-releasing hormone (CRH) (circadian signals, serum
cortisol, and stress)
● release of stored ACTH
● transport of free cholesterol into adrenal mitochondria
● accumulate and store circulating low-density lipoproteins (LDL)
● synthesize additional cholesterol using acetyl-CoA
● Mitochondrial membrane cytochrome P450 (CYP450) converts
Cholesterol to Pregnenolone
● After conversion, Pregnenolone is returned to the cytosol for
subsequent zonal conversion by microsomal enzymes in each
Cortex layer by F-layer enzymes and/or androgens by enzymes in the
● Corticosteroid: lipid derivatives R-layer
● 3 Zones of Cortex
1. G Zone (Zona Gomerulosa)
● - Mineralocorticoids:
● Aldosterone
2. F Zone (Zona Fasciculata)
● - Glucocorticoids: Cortisol
3. R Zone (Zona Reticularis)
Sex steroids precursor:
Dehydroepiandosteron
Medulla
Catecholamine: Tyrosine derivatives
● Norepinephrine/ Noradrenaline
● Epinephrine/Adrenaline
● Adult adrenal glands are shaped like pyramids, located just above
and medial to the kidneys in the retroperitoneal space (suprarenal
glands).
● Cortex appears yellow, the medulla is dark mahogany
● Glucocorticoids from the cortex are carried directly to the adrenal
medulla via the portal system, where they stimulate production of
epinephrine (EPI)
● Sympathetic and parasympathetic axons reach the medulla
through the cortex.
● En route, these axons release neurotransmitters (e.g.,
catecholamines, neuropeptide Y) that modulate cortex blood flow,
cell growth, and function.
● Medullary projections into the cortex have been found to contain
cells that also synthesize and release neuropeptides
● vasoactive inhibitory peptide (VIP)
● Adrenomedullin
● atrial natriuretic peptide (ANP)
G Zone
● Zona glomerulosa cells (outer 10%)
● synthesize mineralocorticoids (aldosterone) sodium retention
volume
● dec Potassium
● Acid-base homeostasis
● Low cytoplasmic-to-nuclear ratios and small nuclei with dense
chromatin with intermediate lipid inclusions.
F Zone·
● Zona fasciculata cells (middle 75%)
● synthesize glucocorticoids, (cortisol, and corticocortisone)
● critical to blood glucose homeostasis and blood pressure.
● Fasciculata cells are cords of clear cells, with a high
cytoplasmic-to-nuclear ratio and lipids laden with "foamy"
cytoplasm.
R-zone
● Zona reticularis cells (inner 10%)
● Sulfate DHEA (dehydroepiandrosterone) to DHEAS, which is the
main adrenal androgen.
● The zone is sharply demarcated with lipid-deficient cords
● of irregular, dense cells with lipofuscin deposits.
VILLAGRACIA, JALEN C. MT 3-YA-8 19
CC2 LEC
● Enhanced with high sodium diets
● Is stimulated by:
○ Angiotensin II, ACTH, Elevated Serum K+,
Progesterone, Dopamine
● ·Is inhibited by:
○ Atrial natriuretic peptide (ANP), Intracellular
calcium
○ Certain drugs: Ketoconazole, ACE inhibitors,
NSAIDS, Heparin
CORTISOL
● Synthesis: 15-20 mg/day
● Maintain blood glucose by inducing lipolysis
● and amino acid release from muscle breakdown for conversion
into glucose (gluconeogenesis) → storage as liver glycogen
Urinary cortisol metabolites
1. 17-hydroxycorticosteroid
● -utilizes phenyl hydrazine in H2SO4 + alchohol (Porter-Silber
method)
2. 17-ketogenic steroids
● -Sodium bismuthate for Norymberski reaction
-meta-dinitrobenzene for Zimmerman reaction
● Cortisol is the primary feedback regulator of ACTH- stimulated
hormone production in the adrenal cortex. ACTH generally does
not significantly impact G-layer aldosterone synthesis
● Decreased activity of any enzymes required for enzymes
biosynthesis can occur as an acquired or inherited (autosomal
recessive) trait.
● Defects that decrease production of cortisol cause increases in
ACTH and CRH secretion in an attempt to stimulate cortisol levels
and lead to adrenal hyperplasia or overproduction of androgens
PATHOLOGIC CONDITIONS
Congenital Adrenal Hyperplasia
● Inherited family of enzyme disorders
● Decreased cortisol and aldosterone production
● Clinical presentation depends on enzyme affected
● Laboratory findings:
○ Increased upstream substrates
○ Overflow across open pathways
○ Decreased products downstream
G-ZONE ● Partial defects: puberty
● Conversion of Pregnenolone to Aldosterone ● 95% 21-hydroxylase deficiency
● 15-20 mg/day ○ 17-OH progesterone & androgen buildup
● Synthesis occurs due to: ○ Cortisol decreased
● Low Aldosterone synthase activity in other zones ○ Treatment:
○ Final oxidation of Corticosterone to Aldosterone ■ Oral glucocorticoids
● Low G-cell 17a-hydroxylase activity Isolated Hypoaldosteronism
○ .Prevents substrate diversion into other pathways ● Insufficient aldosterone production
● Aldosterone secretion is regulated by: Renin-Angiotensin System ● Adrenal gland destruction
(RAS) which functions to maintain mainly sodium balance. ● Chronic heparin therapy
● Renin: proteolytic enzyme by renal cells in the juxtaglomerular ● Unilateral adrenalectomy (transient)
apparatus ● Patients with mild renal insufficiency
● Production stimulated by: ● DM with mild metabolic acidosis
○ Volume depletion ● High serum K+
○ Low filtered salt ● Low urinary K+ excretion (urine K+ < urine Na+)
○ -Sympathetic nerve stimulation ● Low reninemia
● Treatment:
ALDOSTERONE ● Florinef (synth. Mineralocorticoid)
● Increase blood pressure through volume expansion by increasing ○ Enhances salt retention, secretion of potassium &
sodium reabsorption → water retention acid
● Stimulates Hydrogen+ and Potassium+ excretion → metabolic
alkalosis with volume expansion, hypertension and hypokalemia
VILLAGRACIA, JALEN C. MT 3-YA-8 20
CC2 LEC
HYPERALDOSTERONISM ○ Bilateral adrenal hemorrhage
● Excess aldosterone production ○ Adrenoleukodystrophy
● Metabolic alkalosis ○ - Infiltrative processes
● HTN ○ - Metastasis
● Hypokalemia ● Secondary to ACTH deficiency
○ - Easy fatigability ● Glucocorticoid therapy (most common)
○ Muscle weakness (paralysis) ● Tumors
○ - Polyuria (loss of renal concentrating ability) ● Hemorrhage
○ - Palpitations ● Infiltrative processes
○ - Impaired insulin secretion ● Developmental abnormalities
○ Aldosterone suppression ● .Malignancies
● Signs & Symptoms: Weakness, Fatigue, Anorexia, Nausea,
PRIMARY ALDOSTERONISM Diarrhea, Abdominal pain
● Low Renin ● Weight loss
● Autonomous oversecretion of aldosterone ● Signs & Symptoms: Hyponatremia, Hyperkalemia,
● Diagnosis: Hypercalcemia, Prerenal azotemia, Mild metabolic acidosis
○ PA/PRA greater than 25 ● Diagnosis:
○ Low plasma renin that fails to increase with ● - Low baseline cortisol levels (8AM, supine)
volume depletion ● - Elevated ACTH >200 pg/mL
○ High aldosterone that fails to decrease with saline ● · Random Cortisol >20 ug/dL
or angiotensin inhibition ● - Cosyntropin (synthetic stimulator of cortisol/ aldosterone)
stimulation tests
SECONDARY ALDOSTERONISM ● Metyrapone test - Block 11B- hydroxylase
● Elevated Renin ● Insulin tolerance test -gold standard for secondary and tertiary
● RAS-activated aldosterone secretion hypocorticolism.
PSEUDOALDOSTERONISM
● Liddle's syndrome
○ -increase epithelial sodium channel
● Bartter's syndrome
○ -bumetanide-sensitive Chloride channel mutation
● - Gitelman's syndrome
○ Thiazide-sensitive transporter mutation
HYPERCORTISOLISM
● Overproduction of CRH & ACTH secretion
○ Immune (suppression, poor healing)
○ Dermatologic (thin, friable tissue, wide purple
striae)
○ Vascular (vessel fragility, ecchymoses)
○ Metabolic (hyperglycemia & insulin resistance)
○ Bone (loss)
● Adrenal glucocorticoid effects
○ Adipose (increased fat with redistribution to upper
back and central locations buffalo hump.
○ Muscle (wasting, weakness, heart failure)
Diagnosis Algorithm ○ Neurologic(neuropathy)
● Urinary potassium excretion ○ Renal (edema, HTN, calciuria)
○ - >30 mEq/day: suggestive of hyperaldosteronism
○ <30 mEq/day: renal K+ retention (diuretic use & Cushing's Syndrome
GIT loss) ● . Excess glucocorticoid production
● Upright PA/PRA ratio ● Hypercortisolism
○ Overnight fluid deprivation (PRA) ● Prolonged exogenous steroid use
○ *Volume expansion (2L normal saline in 4h: ● Most common causes:
normally supresses aldosterone) ○ ACTH-secreting pituitary adenoma
○ PA/PRA ration: >25 (1'Aldosteronism) ○ Autonomous Cortisol production from adrenal
ACTH tumor (ACTH suppressed)
● - ACTH & Cortisol: highest early in the morning (8am) ○ Excess ACTH or CRH production (usually
● - ACTH & Cortisol: lowest at night (10pm-12am) malignant)
● - ACTH pulse amplitude: rises between 2-4am Cushing's Syndrome Diagnosis
● - ACTH suppressed: Elevated glucocorticoids 1. Document Cortisol excess
● - ACTH peaks ● - Random plasma cortisol: of little value for the diagnosis of
○ Protein-rich meals Cushing's syndrome
○ ADH & CRH stimulation ● Baseline AM cortisol: have no diagnostic value
○ Hypoglycemia: ADH & CRH stimulation ● Urine free cortisol
○ Acute stress ○ Increased once Corticosteroid Binding Globulin is
saturated
Adrenal insufficiency: Addison's Disease ○ 24-hour urine free cortisol (Tandem Mass
● • Low cortisol: Hypocortisolism Spectroscopy): most sensitive & specific
● Primary adrenal problem: destruction of 90% of the adrenal gland 2. Determine if Diurnal Rhythm is Lost
cortex ● Late night values remain high
○ - Autoimmune adrenalitis (70%) ● - Plasma cortisol (highest 6-8am) (lower 10pm-12am)
○ - Fungal diseases ● Single midnight cortisol (>7.5ug/dL)=100% specific
○ - HIV infection
○ - Tuberculosis
VILLAGRACIA, JALEN C. MT 3-YA-8 21
CC2 LEC
● Single salivary cortisol level (11pm) with 8am salivary cortisol after ● EPI is transported into secretory vesicles by vesicle monoamine
overnight dexamethasone suppresion (1mg)=100% specific & transporters (VMAT) in pheochromocytes
92% sensitive
● Midnight (12am) values <1.3ng/mL (RIA) Urine & Plasma Catecholamine Measurements
● Midnight (12am) values >1.5 ng/mL (Competitive-protein binding) ● Catecholamine are:
3. Determine Loss of Normal Cortisol ○ Hydrophilic
● Suppression by Dexamethasone ○ Circulate in low levels (50% albumin-bound) -
● Dexamethasone acts as exogenous cortisol substitute Short half-lives (seconds to 2 minutes)
● Supress ACTH production of pituitary gland (N) ○ Produce wide, rapidly fluctuating levels
● Supress Cortisol production of adrenal gland (N)
● Screen patients for overproduction of cortisol Causes of Sympathetic Hyperactivity
● Autonomous dysfunctions
Androgen excess ● Panic attacks (emotions)
● Ambiguous genitalia in infant girls ● Pheochromocytoma (catecholamine- producing tumor)
● Precocious puberty in children ● Stress response:
● Short stature ○ - Hypoglycemia
● Virilization in boys ○ - Injury
○ Penile enlargement ○ - Infarction
○ - Androgen-dependent hair growth ○ - Infection
○ - 2' sexual char. ○ - Psychosis
● Virilization in girls ○ - Seizures
○ Hirsutism
○ - Acne Causes of Sympathetic Hyperactivity
○ - Clitorimegaly ● Drugs:
● Virilization in women. ○ Decongestants
○ - Infertility ○ Appetite suppressors
○ - Masculinizing effects ○ Stimulants
○ - Hirsutism ○ Bronchodilators
○ - Acne ○ MAO inhibitors
○ Male-pattern baldness ○ Thyroid hormone
○ Menstrual irregularities ○ Cortisol
● In Men ○ Nicotine withrawal
○ Inhibits gonadotropins release by pituitary ○ Short-acting sympathetiic antagonists
○ Lowers testicular testosterone production ○ ·Clonidine & Propranolol
● Virilization in men ○ Tyramine intake
● Infertility
● Feminizing effects
● Hypogonadal symptoms
○ Loss of muscle mass
○ Decreased hair growth
○ Decreased testes size
ADRENAL MEDULLA
● Composed primarily by chromaffin cells that secrete
catecholamines
Medullary Hormones
● Norepinephrine (Primary amine) - produced by sympathetic
ganglia
○ Highest concentration id found in brain
○ neurotransmitter in both CNS and SNS
● Epinephrine (Adrenaline, Secondary amine) - Most abundant
medullary hormone
○ Produced from norepinephrine, comes only from
adrenal
○ "Fight or flight hormone", released in response to
physiologic injuries or psychological threats (stress
and anxiety)
● · Dopamine
○ Cathecolamine produced in the body by the
decarboxylation of 3,4-dihydroxyphenylalanine
(DOPA)
○ Major intact cathecolamine present in urine
Medullary Catecholamine Release
● STIMULATION - Catecholamine release -
(STIMULATION→Transmitting messages via efferent axons)
● Medulla functions as an atypical sympathetic ganglion
● Catecholamines serve as 1st responders to stress in seconds
(cortisol takes 20 mins)
○ Promotes fight-or-flight response
○ Increases cardiac output & blood pressure
○ Diverts blood toward muscle & brain
○ Mobilizes fuel from storage
Biosynthesis & Storage of Catecholamines
● Medulla chromaffin cells
● Norepinephrine (NE) passively diffuse into the cytosol
● NE is coverted into Epinephrine (EPI) by Phenylethanolamine
N-methyltransferase (PNMT) {Cortisol dependent:↑Cortisol=1EPI}
VILLAGRACIA, JALEN C. MT 3-YA-8 22
You might also like
- Advanced Pharmaceutical analysisFrom EverandAdvanced Pharmaceutical analysisRating: 4.5 out of 5 stars4.5/5 (2)
- FLUIDS AND ELECTROLYTES UpdatedDocument8 pagesFLUIDS AND ELECTROLYTES UpdatedSJane FeriaNo ratings yet
- ภาพถ่ายหน้าจอ 2564-11-26 เวลา 11.17.04Document59 pagesภาพถ่ายหน้าจอ 2564-11-26 เวลา 11.17.04CHULEEMAT KAEWDANGNo ratings yet
- Kuliah S2 Dasar Air-ElekDocument38 pagesKuliah S2 Dasar Air-ElekViany RehansyahNo ratings yet
- Fluids ElectrolytesDocument2 pagesFluids ElectrolytesYuet Chin LowNo ratings yet
- 00 Renal FabsDocument9 pages00 Renal FabsAngelica AlayonNo ratings yet
- Intravenous Fluid Prescribing: Patient Safety FirstDocument27 pagesIntravenous Fluid Prescribing: Patient Safety FirstMuhammed SamiNo ratings yet
- L8-IV FluidsDocument41 pagesL8-IV FluidsKrishna RajakumarNo ratings yet
- Renal Physiology ReviewDocument7 pagesRenal Physiology ReviewHOD AnesthesiaNo ratings yet
- Electrolytes To Phosphorus PPTsDocument99 pagesElectrolytes To Phosphorus PPTsMarvin SimbulanNo ratings yet
- Fisiologi 1 - Introducton Renal PhysiolgyDocument5 pagesFisiologi 1 - Introducton Renal PhysiolgyHachi Nini Shop IINo ratings yet
- Fluid ResuscitationDocument23 pagesFluid ResuscitationDunstan Abel SambatangNo ratings yet
- Lecture 21 - Fluid & Electrolyte Balance1 - 16 Oct 2006Document35 pagesLecture 21 - Fluid & Electrolyte Balance1 - 16 Oct 2006api-3703352No ratings yet
- Fluid & Electrolytes: DR Win Min OoDocument55 pagesFluid & Electrolytes: DR Win Min OoBiomedical Science MyanmarNo ratings yet
- Correos Electrónicos 1. Optimizacion Cardiovascular, FluidosDocument29 pagesCorreos Electrónicos 1. Optimizacion Cardiovascular, FluidosKaren PMNo ratings yet
- Supplementary Information To Chapter 30: Overview of Electrolyte BalanceDocument11 pagesSupplementary Information To Chapter 30: Overview of Electrolyte BalanceAaron JoseNo ratings yet
- Hyponatremia: ElectrolytesDocument5 pagesHyponatremia: ElectrolytesCyreen Jill Aliling100% (1)
- Fluid Therapy: Presenter: Chew Zi Qi Supervisor: Dr. Tan KWDocument43 pagesFluid Therapy: Presenter: Chew Zi Qi Supervisor: Dr. Tan KWaslanNo ratings yet
- Trastornos HidroelectroliticosDocument45 pagesTrastornos HidroelectroliticosIván Mesias PachasNo ratings yet
- T09-Physiology 3Document26 pagesT09-Physiology 3Mohammad AlomariNo ratings yet
- CC2 - Electrolytes and Inorganic IonsDocument4 pagesCC2 - Electrolytes and Inorganic Ionsjohnjoseph.ermitanoNo ratings yet
- Electrolytes ACID BASE BALANCEDocument11 pagesElectrolytes ACID BASE BALANCEimbendo.cvtNo ratings yet
- IV Fluid Therapy SeminarDocument29 pagesIV Fluid Therapy Seminarعمر احمد شاكرNo ratings yet
- Fluids PDFDocument26 pagesFluids PDFLeogalvez BedanoNo ratings yet
- Mtap - Aubf Review NotesDocument8 pagesMtap - Aubf Review NotesMoira Pauline LibroraniaNo ratings yet
- CC 2 - ElecDocument4 pagesCC 2 - Elecjohnjoseph.ermitanoNo ratings yet
- Correcting Electrolyte Em@ ED (Buckley) - ACEP 08Document57 pagesCorrecting Electrolyte Em@ ED (Buckley) - ACEP 08drnado_82No ratings yet
- LS607 Module 7 Renal PhysiologyDocument24 pagesLS607 Module 7 Renal PhysiologyasmaaalmesaifriNo ratings yet
- DiureticsDocument29 pagesDiureticsdeepak askarNo ratings yet
- NephrologyDocument34 pagesNephrologyDebayan KhanNo ratings yet
- Diuretics TableDocument6 pagesDiuretics TableVie TNo ratings yet
- Terapi Cairan Pada AnakDocument48 pagesTerapi Cairan Pada AnakAstri Novia RizqiNo ratings yet
- Electrolytes Water Balance PH Balance Trace MetalsDocument21 pagesElectrolytes Water Balance PH Balance Trace MetalsJohn Kevin Carl SaligumbaNo ratings yet
- NCMB 312Document7 pagesNCMB 312ENJELAH RAIKA NEYRANo ratings yet
- Disorders of SodiumDocument38 pagesDisorders of SodiumMuhammad FaizanNo ratings yet
- Fluid TherapyDocument36 pagesFluid TherapyAmin MasromNo ratings yet
- Sodium Potassium Imbalances MedsurgDocument5 pagesSodium Potassium Imbalances Medsurgchi kNo ratings yet
- Water and Sodium 2024 PDFDocument61 pagesWater and Sodium 2024 PDFMpho MosehlaNo ratings yet
- Week 7 Fluid Volume Imbalances: SoluteDocument8 pagesWeek 7 Fluid Volume Imbalances: SoluteMaica LectanaNo ratings yet
- A&P - 3. Renal Physiology (12p)Document12 pagesA&P - 3. Renal Physiology (12p)AbrahamWongCheeHongNo ratings yet
- Summary 1Document133 pagesSummary 1Miss LindiweNo ratings yet
- Sodium and Potassium DisordersDocument7 pagesSodium and Potassium DisordersShia LevyNo ratings yet
- The Heart and Circulatory System and The Kidney 2Document28 pagesThe Heart and Circulatory System and The Kidney 2Izzuddin AhmadNo ratings yet
- 1 Fluid and ElectrolyteDocument51 pages1 Fluid and ElectrolyteSanjiv SharmaNo ratings yet
- (MED - LE5) 05 - Approach To Common Water and Electrolyte Problems (v1)Document20 pages(MED - LE5) 05 - Approach To Common Water and Electrolyte Problems (v1)evizak9253No ratings yet
- Fluid and Electrolytes: Balance and DisturbanceDocument47 pagesFluid and Electrolytes: Balance and DisturbanceSavanna ChambersNo ratings yet
- Electrolytes, Trace Elements and VitaminsDocument67 pagesElectrolytes, Trace Elements and VitaminsFatima MendozaNo ratings yet
- LP3 NCM 112 Electrolytes2021 UpdatedDocument57 pagesLP3 NCM 112 Electrolytes2021 UpdatedJade CentinoNo ratings yet
- Electrolyte Disorders - 1Document29 pagesElectrolyte Disorders - 1sanketh bhat.sNo ratings yet
- 1 Fluid and ElectrolyteDocument51 pages1 Fluid and ElectrolyteSanjiv SharmaNo ratings yet
- Electrolyte AbnormalitiesDocument74 pagesElectrolyte Abnormalitiesbluecrush1No ratings yet
- (CC Lab) Sodium and PotassiumDocument8 pages(CC Lab) Sodium and PotassiumDennisse San JoseNo ratings yet
- Hyponatremia in DCLDDocument27 pagesHyponatremia in DCLDGowtham KrishnaNo ratings yet
- Electrolyte Imbalance ArcherDocument111 pagesElectrolyte Imbalance ArcherDanica Chiara Motia100% (2)
- (PH166) 11 ElectrolytesDocument10 pages(PH166) 11 ElectrolytesRosshlein Marian YangsonNo ratings yet
- Balda Electrolyte DisbalanceDocument33 pagesBalda Electrolyte DisbalanceBaldandorj KhavalkhaanNo ratings yet
- HD B Braun For CNN TakersDocument6 pagesHD B Braun For CNN TakersWhimsey CipresNo ratings yet
- Obat-Obat KardiovaskulerDocument50 pagesObat-Obat KardiovaskulerMuhammad IqbalNo ratings yet
- FluidelectrolytebalanceDocument87 pagesFluidelectrolytebalancePavi MuruganathanNo ratings yet
- Topic 10 Management of QualityDocument19 pagesTopic 10 Management of QualityMary Kaye Yvonne OtillaNo ratings yet
- Topic 9 - Location Planning and AnalysisDocument10 pagesTopic 9 - Location Planning and AnalysisMary Kaye Yvonne OtillaNo ratings yet
- Laboratory MathDocument13 pagesLaboratory MathMary Kaye Yvonne OtillaNo ratings yet
- VILLALONDocument1 pageVILLALONMary Kaye Yvonne OtillaNo ratings yet
- Villalon ApplicationDocument1 pageVillalon ApplicationMary Kaye Yvonne OtillaNo ratings yet
- Topic 12 - Occupational Safety and Health StandardsDocument9 pagesTopic 12 - Occupational Safety and Health StandardsMary Kaye Yvonne OtillaNo ratings yet
- Lecture1 and 2 Introduction To Pathology Cellular Injury Death Adaptation Inflammation and RepairDocument96 pagesLecture1 and 2 Introduction To Pathology Cellular Injury Death Adaptation Inflammation and RepairMary Kaye Yvonne OtillaNo ratings yet
- Biopsy and Autopsy: Lecture#4Document44 pagesBiopsy and Autopsy: Lecture#4Mary Kaye Yvonne OtillaNo ratings yet
- EndocrineDocument4 pagesEndocrineMary Kaye Yvonne OtillaNo ratings yet
- ImseDocument18 pagesImseMary Kaye Yvonne OtillaNo ratings yet
- ABO Blood Group SystemDocument56 pagesABO Blood Group SystemMary Kaye Yvonne OtillaNo ratings yet
- Imhm321 Week 4 Lecture - Abo Subgroups and DiscrepanciesDocument59 pagesImhm321 Week 4 Lecture - Abo Subgroups and DiscrepanciesConsigliereNo ratings yet
- OTILLADocument2 pagesOTILLAMary Kaye Yvonne OtillaNo ratings yet
- HPCTDocument1 pageHPCTMary Kaye Yvonne OtillaNo ratings yet
- Megaloblastic AnemiaDocument3 pagesMegaloblastic AnemiaMary Kaye Yvonne OtillaNo ratings yet
- MONOLOGUEDocument1 pageMONOLOGUEMary Kaye Yvonne OtillaNo ratings yet
- EnteroDocument10 pagesEnteroMary Kaye Yvonne OtillaNo ratings yet
- WBC Morphologic DefectDocument10 pagesWBC Morphologic DefectMary Kaye Yvonne OtillaNo ratings yet
- NORMOCYTICDocument2 pagesNORMOCYTICMary Kaye Yvonne OtillaNo ratings yet
- LIVERDocument8 pagesLIVERMary Kaye Yvonne OtillaNo ratings yet
- Week 7 LabDocument2 pagesWeek 7 LabMary Kaye Yvonne OtillaNo ratings yet
- Forms of HemoglobinDocument4 pagesForms of HemoglobinMary Kaye Yvonne OtillaNo ratings yet
- LEUKEMIA, MPDs & MDSsDocument11 pagesLEUKEMIA, MPDs & MDSsMary Kaye Yvonne OtillaNo ratings yet
- Kantian - Utilitarianism: Villalon, Royette Phol A. 02-04-22 EthicsDocument1 pageKantian - Utilitarianism: Villalon, Royette Phol A. 02-04-22 EthicsMary Kaye Yvonne OtillaNo ratings yet
- GOC & EAS CPP-II - PMDDocument14 pagesGOC & EAS CPP-II - PMDVansh sareenNo ratings yet
- ASAP2Document119 pagesASAP2hacvuaNo ratings yet
- Checklists For Quality Control For RCC WorkDocument4 pagesChecklists For Quality Control For RCC Workwaimaung100% (1)
- Lehmann Et Al 2013 PDFDocument13 pagesLehmann Et Al 2013 PDFJack HamiltonNo ratings yet
- KEIYU NDT Ultrasonic TransducerDocument6 pagesKEIYU NDT Ultrasonic TransducersrgokuNo ratings yet
- Gen Nav WeOneDocument272 pagesGen Nav WeOnecaptvivekNo ratings yet
- Ptical Oxygen Sensor: ATA HeetDocument14 pagesPtical Oxygen Sensor: ATA HeetZoran ConstantinescuNo ratings yet
- Grain SizeDocument30 pagesGrain SizeRex SabersonNo ratings yet
- Achidram, Ashwamedham & KatakamDocument228 pagesAchidram, Ashwamedham & KatakamSubhash Sharma100% (9)
- Tutorial 4 JawapanDocument6 pagesTutorial 4 JawapanlimNo ratings yet
- Data Communication: By:Eng - Alaa I.HaniyDocument8 pagesData Communication: By:Eng - Alaa I.Haniypömo cNo ratings yet
- APN-002 Protection and Control DevicesDocument10 pagesAPN-002 Protection and Control DevicesYusron MuhammadNo ratings yet
- Basic Principles of Radiology: Bachtiar MurtalaDocument75 pagesBasic Principles of Radiology: Bachtiar MurtalaMargaretha SonoNo ratings yet
- Landscape Products: Technical GuideDocument124 pagesLandscape Products: Technical Guidegabbo24No ratings yet
- ABM11 BussMath Q1 Wk3 ProportionsDocument12 pagesABM11 BussMath Q1 Wk3 ProportionsArchimedes Arvie Garcia100% (1)
- Soil Mechanics: Triaxial Stress Measurement Test (Uu-Cu-Cd Tests)Document3 pagesSoil Mechanics: Triaxial Stress Measurement Test (Uu-Cu-Cd Tests)Opu DebnathNo ratings yet
- IISER Aptitude Test 17th Sept 2021Document22 pagesIISER Aptitude Test 17th Sept 2021Muskaan KathuriaNo ratings yet
- s10763 017 9799 1 PDFDocument19 pagess10763 017 9799 1 PDFJoy PascoNo ratings yet
- 06 Strengthening MechanismsDocument63 pages06 Strengthening MechanismsMURALIGOCAM_29070605100% (1)
- Implementation of Integrated OBD-II Connector Whith External NetworkDocument7 pagesImplementation of Integrated OBD-II Connector Whith External NetworkKelvin PárragaNo ratings yet
- Training Manual A 319/320/321: ATA 30 Ice and Rain ProtectionDocument46 pagesTraining Manual A 319/320/321: ATA 30 Ice and Rain ProtectionHansraj Kayda100% (1)
- K Type Thermocouple Extension Cable KXYY (1-50) Pairs X 1.5 MM 300 VDocument1 pageK Type Thermocouple Extension Cable KXYY (1-50) Pairs X 1.5 MM 300 VArthurNo ratings yet
- Psychological, Social and Environmental BarriersDocument12 pagesPsychological, Social and Environmental BarrierssaifNo ratings yet
- The Best Itext Questions On StackoverflowDocument361 pagesThe Best Itext Questions On Stackoverflowadaf8850% (2)
- Lab ReportDocument4 pagesLab ReportSyafiq MTNo ratings yet
- FG Wilson AtsDocument5 pagesFG Wilson AtsErwan Shidiq FathoniNo ratings yet
- Gauss Contest: Grade 7Document4 pagesGauss Contest: Grade 7irwan syahNo ratings yet
- 7.RP.A2a - Determine Proportional RelationshipsDocument12 pages7.RP.A2a - Determine Proportional Relationshipsicka830% (1)
- Microprocessors and Digital ICs For Control of Power Electronics and DrivesDocument79 pagesMicroprocessors and Digital ICs For Control of Power Electronics and DrivesTianmingyuNo ratings yet
- Info Sphere Information Analyzer - Methodology and Best PracticesDocument127 pagesInfo Sphere Information Analyzer - Methodology and Best PracticesRoshava KratunaNo ratings yet
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (1)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 4.5 out of 5 stars4.5/5 (2)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingFrom EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingRating: 4 out of 5 stars4/5 (3)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthFrom EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthRating: 4 out of 5 stars4/5 (6)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarFrom EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarRating: 5 out of 5 stars5/5 (351)
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouFrom EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNo ratings yet
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyFrom EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyNo ratings yet
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainFrom EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainRating: 3.5 out of 5 stars3.5/5 (38)
- Molecules of Emotion: Why You Feel the Way You FeelFrom EverandMolecules of Emotion: Why You Feel the Way You FeelRating: 4 out of 5 stars4/5 (128)
- Keto Friendly Recipes: Easy Keto For Busy PeopleFrom EverandKeto Friendly Recipes: Easy Keto For Busy PeopleRating: 3.5 out of 5 stars3.5/5 (2)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsFrom EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsRating: 4 out of 5 stars4/5 (49)
- How Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseFrom EverandHow Not to Die by Michael Greger MD, Gene Stone - Book Summary: Discover the Foods Scientifically Proven to Prevent and Reverse DiseaseRating: 4.5 out of 5 stars4.5/5 (84)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- The End of Craving: Recovering the Lost Wisdom of Eating WellFrom EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellRating: 4.5 out of 5 stars4.5/5 (81)
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomFrom EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomRating: 4 out of 5 stars4/5 (1)
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthFrom EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthNo ratings yet
- The Whole Body Reset: Your Weight-Loss Plan for a Flat Belly, Optimum Health & a Body You'll Love at Midlife and BeyondFrom EverandThe Whole Body Reset: Your Weight-Loss Plan for a Flat Belly, Optimum Health & a Body You'll Love at Midlife and BeyondRating: 4.5 out of 5 stars4.5/5 (28)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeFrom EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeRating: 5 out of 5 stars5/5 (1)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisFrom EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisRating: 3 out of 5 stars3/5 (2)
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodFrom EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodNo ratings yet
- Ultrametabolism: The Simple Plan for Automatic Weight LossFrom EverandUltrametabolism: The Simple Plan for Automatic Weight LossRating: 4.5 out of 5 stars4.5/5 (28)