Professional Documents
Culture Documents
Pedia Lecture
Uploaded by
Dustin RamosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pedia Lecture
Uploaded by
Dustin RamosCopyright:
Available Formats
PEDIA LECTURE
HIGH RISK NEWBORN
Problems related to:
1) Maturity
2) Birthweight
Premature - liveborn infants delivered
Intended Learning Outcome
before 37 weeks from the 1st day of the last
At the end of this session, the students will mentrual period
be able to:
Low bithweight - birthweight of 2,500 g or
1) Distinguish problems related to maturity less
and gestational weight
Premature - liveborn infants delivered
2) Apply appropriate nursing concepts and before 37 weeks from the 1st day of the last
actions to a high-risk infant mentrual period
3) Apply ethical reasoning and decision- Low birthweight - birthweight of 2,500 g or
making processes to address situations of less is due to prematurity, poor intrauterine
ethical distress and moral dilemmas. growth also called SGA or both
Overview of Perinatal and Neonatal Very Low birthweight - birthweight less
Mortality in the Philippines than 1,500 gram
Neonatal - a newborn infant or is a child Extremely Low birthweight - birthweight
less than 28 days of age. less than 1,000 gram
Perinatal - pertaining to the period Age of Viability- 24 weeks of gestation
immediately before and after birth
Characteristics
Neonatal/InfantMortality Rate -
Posture - hypotonic, partially flexed
17.968/1,000 live births (2022)
(frog like posture) - assume
18.392/1,000 live births (2021) extended posture due to poor
muscle tone
Skin - thin, gelatinous, shiny and
excessive pink with abundant lanugo
Very littel vernix edema may be
present
Breast nodules are small or absent
(<5mm)
Subcutaenous fat is deficient
Deep sole creases are often not
present in preterm baby
Neonatal Mortality Rate is highest during
the first 24 hours of life and overall accounts
for 65% of all infant deaths (deaths before 1
year of age)
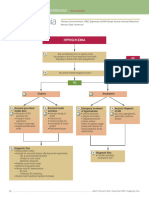
HEMATOLOGIC
-Anemia (early or late onset)
-Hyperbilirubinemia-indirect
-Subcutaneous, organ (liver, adrenal)
hemorrhage
-Disseminated intravascular coagulopathy
-Vitamin K deficiency.
-Hydrops-immune or nonimmune
GASTROINTESTINAL
-Poor gastrointestinal function-poor motility
-Necrotizing enterocolitis.
-Hyperbilirubinemia-direct and indirect
-Congenital anomalies producing
polyhydramnios.
-Spontaneous gastrointestinal isolated
perforation
METABOLIC-ENDOCRINE
-Hypocalcemia
-Hypoglycemia
-Hyperglycemia
-Late metabolic acidosis
-Hypothermia
-Euthyroid but low-thyroxin status
CENTRAL NERVOUS SYSTEM
-Intraventricular hemorrhage
-Periventricular leukomalacia
-Hypoxic-ischemic encephalopathy
Neonatal Problems Associated with Premature -Seizures
Infants -Retinopathy of prematurity
-Deafness
-Hypotonia
RESPIRATORY
-Congenital malformations
-respiratory distress syndrome (hyaline
-Kernicterus (bilirubin encephalopathy)
membrane disease)
-Drug (narcotic) withdrawal
-Bronchopulmonary dysplasia
-Pneumothorax, pneumomediastinum;
RENAL
interstitial emphysema Congenital pneumonia
-Hyponatremia
-Pulmonary hypoplasia
-Hypernatremia
-Pulmonary hemorrhage
-Hyperkalemia
-Apnea
-Renal tubular acidosis
-Renal glycosuria
CARDIOVASCULAR
-Edema
-Patent ductus arteriosus
-Hypotension
OTHER
-Hypertension
Infections (congenital, perinatal, nosocomial:
-Bradycardia (with apnea)
bacterial, viral, fungal, protozoal)
-Congenital malformations
Intrauterine Growth Retardation
Fetal growth restriction (FGR) - is said to
be present in those babies whose birth Prognosis
weight is below the 10th percentile of In most cases, infants with IUGR ultimately have
the average for the gestational age.
good outcomes, with a reported mortality rate
It can occur in preterm, term or post
of only 0,2 to 1 percent. These infants often
term babies.
Intrauterine growth restriction - it is a exhibit fast catch-up growth in the first three
clinical definition and SGA is a statistical months of life and attaining normal growth
definition. curves by one year of age.
Clinical Features of IUGR baby Journal review.
All SGA babies are IUGR but all IUGR • Intrauterine Growth Restriction: Antenatal
babies are not SGA
and Postnatal Aspects
Loose skin folds in buttocks region
Decrease subcutaneous fat
Peeling of skin • Deepak Sharma, Sweta Shastri, and Pradeep
Small abdomen Sharma
Thin umbilical cord Published by:- PUBMED, 2016
Old man like appearance Abstract
Factors Often Associated with Intrauterine Intrauterine growth restriction (IUGR), a
Growth Restriction condition that occurs due to various
reasons, is an important cause of fetal
FETAL and neonatal morbidity and mortality. It
-Chromosomal disorders (e.g., autosomal has been defined as a rate of fetal
trisomies) growth that is less than normal in light
-Chronic fetal infections (e.g., cytomegalic of the growth potential of that specific
inclusion disease, congenital rubella, syphilis) infant.
-Congenital anomalies-syndrome complexes
Usually, IUGR and small for gestational
Irradiation
age (SGA) are used interchangeably in
-Multiple gestation
literature, even though there exist
-Pancreatic hypoplasia minute differences between them. SGA
-Insulin deficiency has been defined as having birth weight
-Insulin-like growth factor type I deficiency less than two standard deviations below
the mean or less than the 10th
PLACENTAL percentile of a population-specific birth
weight for specific gestational age.
-Decreased placental weight or cellularity, or
both
These infants have many acute neonatal
-Decrease in surface area problems that include perinatal
-Villous placentitis (bacterial, viral, parasitic) asphyxia, hypothermia, hypoglycemia,
-Infarction and polycythemia. The likely long-term
-Tumor (chorioangioma, hydatidiform mole) complications that are prone to develop
-Placental separation when IUGR infants grow up includes
-Twin transfusion syndrome growth retardation, major and subtle
neurodevelopmental handicaps, and
MATERNAL
developmental origin of health and
-Toxemia disease. In this review, we have covered
-Hypertension or renal disease, or both various antenatal and postnatal aspects
-Hypoxemia (high altitude, cyanotic cardiac or of IUGR.
pulmonary disease)
-Malnutrition or chronic illness
-Sickle cell anemia
Nursing Management for Premature Babies
-Drugs (narcotics, alcohol, cigarettes, cocaine,
antimetabolites)
Protect the airway Cardiorespiratory Monitoring
Suction mouth and nostril after delivery Continuous monitoring of heart rate,
of the infant. respiratory rate, and oxygen saturation
Keep airway open. Prompt intervention in case of apnea or
bradycardia events.
Respiratory Support
Administer oxygen therapy as needed. Developmental Support
Monitoring respiratory rate and effort Providing a quiet and low-stimulation
Providing assistance with mechanical environment to minimize stress.
ventilation if required Encourage skin-to-skin contact between
Ensuring proper positioning to optimize baby and parents to promote bonding
respiratory function. and emotional well-being.
Temperature Regulation: Parenteral Involvement and Education
Placing premature infants in incubators Educating parents about their baby’s
or warmers to maintain a stable body condition and care needs
temperature. Encouraging parental involvement in
Monitoring temperature regularly to care activities, when appropriate
prevent hypothermia. Providing emotional support to parents
during what can be a challenging time.
Feeding Support
Breast feeding is of the at most Follow-up Care
importance, not only for the proper Coordinating follow-up appointments
nourishment but also for the protection and care after discharge
against infection which provides for the Monitoring growth and development
low-birth-weight baby. milestones
Initiating and monitoring enteral Providing resources and support for
feeding through a tube if the baby is parents to navigate the challenges of
unable to suck effectively. caring for premature infants at home.
Gradually introduce oral feedings as the
baby’s sucking and swallowing abilities Collaboration with Multidisciplinary Team
improve. Working closely with neonatologists,
Monitoring for signs of feeding pediatricians, respiratory therapists,
intolerance or complications. dietitians, and other healthcare
professionals to ensure comprehensive
Infection Prevention care.
Implementing strict hygiene protocols
to prevent infections.
Administering antibiotics as prescribed Post-Term Infants (Postmature babies)
Monitoring for signs of infection, such
Born after 42 weeks of gestation, as
as changes in vital signs or appearance
calculated from the mother LMP,
regardless of weight at birth
Cardiorespiratory Monitoring
When delivery is delayed 3 weeks or
Continuous monitoring of heart rate,
respiratory rate, and oxygen saturation more before term, mortality
Prompt intervention in case of apnea or significantly increases three times
bradycardia events. that of a control group of infants
born at term
Neurologic Monitoring Average incidence is about 3-12%
Regular assessment of neurologic (10%)
status, including responsiveness and Many suspected post-term
reflexes pregnancies/post-term births are
Monitoring for signs of intraventricular wrongly dated
hemorrhage (IVH) or other neurologic The case is unknown. Factors
complications associated with post-maturity include
anencephaly and trisomy 16-18.
Characteristics of post-term infants
Decrease the amount of tissue
mass, particularly subcutaneous fat
The skin may hang loosely on the
extremities and is often dry and
peeling
The fingernails and toenails are long
and lanugo is present
The nails and umbilical cord may be Other Problems in GDM
stained with meconium
More alert and wide-eyed 1. Hypoglycemia, hypocalcemia
Meconium aspiration syndrome is 2. Increased incidence of births
manifested by fetal hypoxia defects-TGA
Respiratory distress may develop at 3. RDS
delivery 4. Hyperbilirubinemia
5. Polycythemia
Nursing Management of Post-Term infant 6. Birth trauma
1. Manage meconium aspiration
syndrome.
Suction the infant's mouth and nares CASE 1
while the head is on the perineum
A baby girl at 39 weeks AOG was delivered
and before the first breath is taken to
via normal spontaneous delivery with a BW
prevent aspiration of meconium that
of 3kg and BL of 50cm. Can you give me
is in the airway.
the apgar score of this patient?
Once the infant is dry on the
warmer, intubate (if needed)Perform With your APGAR Score assessment, what
chest physiotherapy with suctioning should immediate care be provided for that
to remove excess meconium and patient?
secretions
Provide supplemental oxygen and CASE 2
respiratory support as needed
A baby boy 32 weeks AOG was delivered
2. Obtain serial blood glucose
via normal spontaneous delivery with a BW
measurement
of 1.8kg and BL of 45cm. APGAR score
3. Provide early feeding to prevent
was 5 and 7. Plot the weight of gestation.
hypoglycemia, if not contraindicated
by respiratory status. Wat is your initial nursing management of
4. Maintain skin integrity the patient? Give your answer
Keep skin clear and dry chronologically.
Avoid the use of powders, creams,
and lotions CASE 3
Large Gestation Age A baby boy at 40 weeks AOG was delivered
via cessarian section with a BW of 3.33kg
Birthweight >90th percentile for their and BL of 53cm. What is the APGAR score?
gestational age
What is the Ballard score?
Birthweight >2SD from mean weight for
gestation
You might also like
- NCM 109 A Physiologic Problems of The NBDocument3 pagesNCM 109 A Physiologic Problems of The NBmaryelle conejarNo ratings yet
- NCM 109 A Physiologic Problems of The NBDocument3 pagesNCM 109 A Physiologic Problems of The NBmaryelle conejarNo ratings yet
- 04 Pediatri Spotleri 2020Document104 pages04 Pediatri Spotleri 2020Osama E. ShamsNo ratings yet
- Cornell's Note 4Document5 pagesCornell's Note 4Angel BriboneriaNo ratings yet
- Approach To Neonate With Low Birth WeightDocument40 pagesApproach To Neonate With Low Birth Weightnirajan khanalNo ratings yet
- Approach To Neonatal JaundiceDocument73 pagesApproach To Neonatal JaundiceG Venkatesh50% (2)
- Complications of PrematurityDocument22 pagesComplications of Prematurityipad jojNo ratings yet
- Common Neonatal Conditions - Supplementary MaterialDocument25 pagesCommon Neonatal Conditions - Supplementary MaterialayunisallehNo ratings yet
- Neonatal Hyperbilirubemia: (Jaundice in Neonates)Document13 pagesNeonatal Hyperbilirubemia: (Jaundice in Neonates)Hendrix Antonni AmanteNo ratings yet
- Pediatrics NCM 109Document26 pagesPediatrics NCM 109Gezabelle SalveNo ratings yet
- (PESERTA) PEDIATRI 2 - MANTAP Februari 2017 PDFDocument157 pages(PESERTA) PEDIATRI 2 - MANTAP Februari 2017 PDFmarcelinaNo ratings yet
- Common Newborn Problems (2) C1Document39 pagesCommon Newborn Problems (2) C1ZmNo ratings yet
- Pedia at Risk Lecture 1Document10 pagesPedia at Risk Lecture 1Katelinne DabucolNo ratings yet
- Newborn ConditionsDocument80 pagesNewborn ConditionsrigasanaorayNo ratings yet
- Gestational Diabetes Mellitus - : One Disease Two Lives at StakeDocument31 pagesGestational Diabetes Mellitus - : One Disease Two Lives at StakeSadia YousafNo ratings yet
- Module No. Date: Topic:: Cues/Questions/ Keywords Notes Preterm InfantDocument10 pagesModule No. Date: Topic:: Cues/Questions/ Keywords Notes Preterm Infantanon ymousNo ratings yet
- Final Neonatal JaundiceDocument47 pagesFinal Neonatal JaundiceArati JhaNo ratings yet
- NCM 109 Lesson 1 NewDocument47 pagesNCM 109 Lesson 1 NewWeeaboo Franz VlogsNo ratings yet
- Neonatal JaundiceDocument11 pagesNeonatal JaundiceImAlien OrGodNo ratings yet
- Fetal Growth DisordersDocument3 pagesFetal Growth DisordersBess RompalNo ratings yet
- ANAK (Full Permission)Document167 pagesANAK (Full Permission)anggyNo ratings yet
- NCM 109 Prelims ReviewerDocument2 pagesNCM 109 Prelims ReviewerReyna Chame GarcinezNo ratings yet
- PediatricsDocument321 pagesPediatricsJulian GalindoNo ratings yet
- Hypoglycemia - Schermerhorn, ThomasDocument2 pagesHypoglycemia - Schermerhorn, ThomasJuanMartínezNo ratings yet
- Infant of A Diabetic MotherDocument20 pagesInfant of A Diabetic MotherElvisNo ratings yet
- Pediatrics: Raafi Ul Basheer ZargarDocument15 pagesPediatrics: Raafi Ul Basheer ZargarRaafi Ul Basheer ZargarNo ratings yet
- Neonatal Seizures: - Dr.C.S.N.VittalDocument23 pagesNeonatal Seizures: - Dr.C.S.N.VittalRidanna HartateanaNo ratings yet
- Hypoglycemia in Children: Childhood Beyond The NewbornDocument10 pagesHypoglycemia in Children: Childhood Beyond The NewbornCiendy ShintyaNo ratings yet
- MCN ReviewerDocument4 pagesMCN ReviewerMaria Arabella LanacaNo ratings yet
- Newborn ComplicationsDocument45 pagesNewborn ComplicationsWayne GretzkyNo ratings yet
- Pedia (Abnormal) - LectureDocument2 pagesPedia (Abnormal) - LectureD A M N E R ANo ratings yet
- Gestational Diabetes MellitusDocument31 pagesGestational Diabetes MellitusLidya BintangNo ratings yet
- Neonatologi SMT 7Document39 pagesNeonatologi SMT 7Zulfikar RamadhanNo ratings yet
- 01 - Premature Infants and RDSDocument82 pages01 - Premature Infants and RDSprabhat kumarNo ratings yet
- Neonatal SeizuresDocument6 pagesNeonatal SeizuresClaraAmeliaNo ratings yet
- MCN NotesDocument5 pagesMCN NoteskistlerNo ratings yet
- ObesityDocument42 pagesObesityARUN PAULNo ratings yet
- Pediatri 2Document165 pagesPediatri 2YUYUM100% (2)
- DR Hodan Ahmed, Department of Pediatrics and Child Health, Amoud Medical School, AUDocument33 pagesDR Hodan Ahmed, Department of Pediatrics and Child Health, Amoud Medical School, AUMuradNo ratings yet
- DM & Thyroid Disease During PregnancyDocument24 pagesDM & Thyroid Disease During Pregnancybodyb2714No ratings yet
- Maternal and Child Lec Reviewer 1 8Document10 pagesMaternal and Child Lec Reviewer 1 8Keziah Marie Chua Santa-AnaNo ratings yet
- Pregnancy at Risk NCM 109Document3 pagesPregnancy at Risk NCM 109kaycelyn jimenez100% (1)
- OBII - 16 Postterm Pregnancy - PDF Version 1Document6 pagesOBII - 16 Postterm Pregnancy - PDF Version 1Felina CabadingNo ratings yet
- HyperbilirubinemiaDocument32 pagesHyperbilirubinemiav.stephenson headNo ratings yet
- Intra Uteri Growt RetradationDocument44 pagesIntra Uteri Growt RetradationFikriBelikeNo ratings yet
- Classification of Newborn, - 130319150346Document45 pagesClassification of Newborn, - 130319150346Ez Ball100% (1)
- ? - PEDIA PRELIMS Lessons 1 and 2Document8 pages? - PEDIA PRELIMS Lessons 1 and 2ysabel.mendozaNo ratings yet
- Intrauterine Growth RestrictionDocument40 pagesIntrauterine Growth RestrictionnusriniNo ratings yet
- PrematurityDocument66 pagesPrematurityJolmajas JoharNo ratings yet
- OG NoteDocument207 pagesOG NoteДипак СешадриNo ratings yet
- Gestational 1Document8 pagesGestational 1RoseAngelyne VicenteNo ratings yet
- Neonatal Seizures: Postgraduate Dept of PediatricsDocument42 pagesNeonatal Seizures: Postgraduate Dept of PediatricsG VenkateshNo ratings yet
- Care of High Risk Newborn - ChaboyDocument9 pagesCare of High Risk Newborn - Chaboychfalguera0% (1)
- Neonatal Jaundice Cme 3Document56 pagesNeonatal Jaundice Cme 3Arief NorddinNo ratings yet
- JAUNDICE ReportDocument33 pagesJAUNDICE ReportMirzi CuisonNo ratings yet
- Issue End of LifeDocument28 pagesIssue End of LifeYURISDHA AFRIZALNo ratings yet
- MCPDocument3 pagesMCPChelsea CuevasNo ratings yet
- Kernicterus, (Bilirubin Encephalopathy) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandKernicterus, (Bilirubin Encephalopathy) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- 287-Article Text-507-1-10-20200728Document22 pages287-Article Text-507-1-10-20200728TOOBA KANWALNo ratings yet
- 1.2. PTI Insurance Benefits - English VersionDocument23 pages1.2. PTI Insurance Benefits - English VersionĐào Duy PhiNo ratings yet
- Personal Injury Litigation CourseDocument10 pagesPersonal Injury Litigation CourseMelissa HanoomansinghNo ratings yet
- HospitalDocument20 pagesHospitalSparsh SharmaNo ratings yet
- Implementing Hospital RPP 2-19-15pdfDocument94 pagesImplementing Hospital RPP 2-19-15pdfamparokarrilloNo ratings yet
- 2020 Greenhills Hostage Crisis Lea 3 ReportDocument4 pages2020 Greenhills Hostage Crisis Lea 3 ReportMary Grace PagurayanNo ratings yet
- Keratoconus Oet ReadingDocument6 pagesKeratoconus Oet Readingrkishore362No ratings yet
- Central Venous Pressure (CVP)Document3 pagesCentral Venous Pressure (CVP)Raul DoctoNo ratings yet
- Correct Myth and Fallacies About NonDocument2 pagesCorrect Myth and Fallacies About NonRhuj's DiaryNo ratings yet
- E Tech Consultant (Introduction Profile)Document10 pagesE Tech Consultant (Introduction Profile)E Tech ConsultantNo ratings yet
- Epocast 1628 BDocument10 pagesEpocast 1628 BNICKYNo ratings yet
- Dcs - Chccsm005 - Task 1 Questions.v1.192401Document24 pagesDcs - Chccsm005 - Task 1 Questions.v1.192401Manaw100% (3)
- Reading Test 3Document10 pagesReading Test 3Tuyết NhưNo ratings yet
- MIDTERM Community Nursing 2Document24 pagesMIDTERM Community Nursing 2Will Garcia100% (2)
- PerDev Module 5Document14 pagesPerDev Module 5mailNo ratings yet
- GCC Healthcare and Pharmaceutical Sector ReportDocument48 pagesGCC Healthcare and Pharmaceutical Sector ReportParamjot Singh100% (1)
- Cel2103 Writing Portfolio Task 3Document5 pagesCel2103 Writing Portfolio Task 3Muhammad Raimi AyobNo ratings yet
- Gaggers and Its ManagementDocument58 pagesGaggers and Its ManagementAwani GuptaNo ratings yet
- Fabius Plus XLDocument44 pagesFabius Plus XLAlter DiegoNo ratings yet
- Chlamydia/Gonorrhea Testing at TOPADocument1 pageChlamydia/Gonorrhea Testing at TOPATOPA DiagnosticsNo ratings yet
- Broth For BifidobacteriumDocument2 pagesBroth For BifidobacteriumAhnaph RafinNo ratings yet
- A. Findings: Wade, 410 U.S. 113 (1973), That Prohibit and Criminalize Abortion Unless TheDocument18 pagesA. Findings: Wade, 410 U.S. 113 (1973), That Prohibit and Criminalize Abortion Unless TheThe TexanNo ratings yet
- Case Report PtosisDocument4 pagesCase Report PtosisALYA MAULIDANo ratings yet
- Asexual and Sexual ReproductionDocument9 pagesAsexual and Sexual ReproductionJerome DimaanoNo ratings yet
- HRS - Integrated - Contract - and - Handbook - v2 - 2020 - UpdateDocument6 pagesHRS - Integrated - Contract - and - Handbook - v2 - 2020 - UpdateCamilo ZapataNo ratings yet
- SDG Progress Report Special EditionDocument43 pagesSDG Progress Report Special EditionSatya VNo ratings yet
- The Procedure: Cleaning ValidationDocument4 pagesThe Procedure: Cleaning ValidationYousif100% (1)
- Las Pe10 Day1 Week1 DonnaDocument4 pagesLas Pe10 Day1 Week1 DonnaBadeth AblaoNo ratings yet
- Efektivitas Aromaterapi Lemon Untuk Mengatasi Emesis GravidarumDocument8 pagesEfektivitas Aromaterapi Lemon Untuk Mengatasi Emesis Gravidarumsri yulinar pakuNo ratings yet
- MCQ 23Document10 pagesMCQ 23Old driverNo ratings yet