Professional Documents
Culture Documents
Management of ENT Emergencies: Simon Lloyd Consultant ENT Surgeon Central Manchester NHS Foundation Trust
Uploaded by
Dzulkifli I. DotutinggiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Management of ENT Emergencies: Simon Lloyd Consultant ENT Surgeon Central Manchester NHS Foundation Trust
Uploaded by
Dzulkifli I. DotutinggiCopyright:
Available Formats
Management of ENT
Emergencies
Simon Lloyd
Consultant ENT Surgeon
Central Manchester NHS Foundation Trust
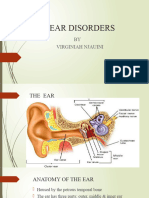
Facial palsy
Anatomy
Sensory
Taste
Posterior ear canal
Autonomic
Parasympathetic to:
Lacrimal gland
Submandibular gland
Sublingual gland
Motor
Facial expression
Stapedius
Posterior belly of digastric
Aetiology
Huge differential
Congenital
Neurological eg. Moebius syndrome
Traumatic eg. Forceps
Acquired
Idiopathic eg. Bells palsy
Traumatic eg. Temporal bone fracture
Iatrogenic eg. Surgery
Infection eg. Acute otitis media, malignant otitis media,
Ramsey Hunt syndrome
Neoplastic eg. Parotid malignancy
Examination
Facial nerve grading (House Brackmann)
Other cranial nerves
Tympanic membrane/pinna for vesicles
Parotid/mouth
Assessment
House Brackmann Grading (I to VI)
I = Normal
II = Normal at rest, mild weakness on active
movement
III= Good eye closure
V = Some tone
VI= No movement
Eyes open Eyes closed
Facial Palsy
52 year old lady
Rapid onset left facial
weakness
Left facial numbness
No ear symptoms
Otherwise fit and well
Grade III weakness
No other abnormalities
Bells Palsy
Idiopathic (probably viral Herpes simplex)
Acute unilateral facial palsy (peripheral)
Occasionally other cranial nerve palsies eg. Trigeminal
Resolves within 3 months in 80% of cases
10% recur (including contralateral)
Higher incidence in diabetes
Treatment
Eye Care (lubrication)
Oral steroids
No evidence for benefit from antivirals
Sullivan et al. New England Journal of Medicine 2007
Who to refer
Additional findings (Cr. Nerves, lumps)
No improvement at 3 weeks
Incomplete recovery
Concerns
Sudden Hearing Loss
Normal TM with sudden hearing loss
Aetiology unknown
Viral
Vascular
Rarely acoustic neuroma, perilymph leak
May be unsteady or vertiginous
Sudden Hearing Loss
Management
Refer urgently
Treatment options
Oral steroid
Antiviral
No evidence for efficacy
Carbogen
No evidence for efficacy
Intratympanic steroid
Weak evidence for efficacy
Allergic response to BIPP
Acute Otalgia with normal TM
Complications of
Otitis Media
Mastoiditis
Facial palsy
Labyrinthitis
Meningitis
Intracranial abscess
Lateral sinus thrombosis
- Long term
Tympanosclerosis
Tympanic membrane perforation
Ossicular damage
Acute Mastoiditis
History of acute otitis media
Infection spreads to mastoid
Post-auricular abscess
Treatment
Grommet
Cortical mastoidectomy
Complications acute otitis media
mastoiditis
Intracerebral Abscess
Diagnosis
High index of suspicion
Headache
Reduced conscious level
Fever
Seizures
Requires drainage
Ring enhancement
with contract
enhanced CT
Lateral Sinus Thrombosis
Diagnosis
High index of suspicion
Headache
Decreased conscious level
Ataxia
Seizures
Treatment
Anticoagulation
?thrombectomy
Filling defect
on MRA
Epistaxis
Anatomy
Aetiology
Usually idiopathic
? atherosclerotic vessels
Predisposing factors
Anticoagulants
Hypertension
Trauma eg. Digital, fractured nose
Nasal vestibulitis eg. Staphlococcal
Topical treatment eg. Nasal steroids
Rare
HHT
Neoplasia
Septal perforation
Epistaxis First Aid
Conservative Management
Pinch soft part of nose
Lean forward and breathe
through mouth
Ten minutes
Protect yourself
Gown
Gloves
Mask
Treatment
Identifiable Vessel
Nasal cautery
Examine nose
Identify vessel
Apply 1 in 10,000
adrenaline and
1%lignocaine on
cotton wool pledget
Silver nitrate cautery
of vessel
Silver nitrate cautery
Treatment
No Identifiable Vessel
Nasal packing
Merocel
Rapidrhino
BIPP packing
Rapid Rhino
BIPP Packing
Treatment
Ongoing bleeding
Re-check vital signs
IV access +/- fluids
Check clotting
Posterior packing
Brighton baloon
Foley catheter and BIPP
pack
Surgical Intervention
Septoplasty
Sphenopalatine artery ligation
Anterior ethmoid artery ligation
Maxillary artery ligation
External carotid artery ligation
Management Algorithm
Nose bleed
Digital
pressure
Bleeding stops:
discharge with
relevant information
Ongoing bleeding
Nasal preparation
Visualise bleeding point
Able to
visualise
Cauterise
Cautery fails
Unable to
visualise
Packing
Packing fails
Surgery
Nasal Vestibulitis
Paediatric
Digital trauma
Cautery vs Naseptin
Equal efficacy
Bactroban tastes horrible ? Prevents digital trauma
Fractured nose
Fractured nose
Ask about
Epistaxis
CSF
Diplopia on upward gaze
Infraorbital parasthesia
Shape change
Nasal obstruction
Fractured nose
Examination
Nasal bones crepitus, shape
Infraorbital parasthesia
Orbital rims
Septum for haematoma
No need for X ray unless
medicolegal
Fractured nose
Management
If no complicating factors and nose straight leave
alone.
If orbital fracture or septal haematoma refer
immediately
If shape change with no complicating factors refer to
ENT about five days post injury
Nose should be reduced within 2 weeks for
best chance of good result
Complications of Sinusitis
Intracranial complications
Brain Abscess
Meningitis
Orbital complications
Periorbital cellulitis
Periorbital abscess
Orbital abscess
Potts puffy tumour
Periorbital Cellulitis and Abscess
Unwell
Pyrexia
Eye closes
Erythema
Chemosis
Colour vision goes off
first
Refer urgently
Periorbital Cellulitis
Treatment
Nose
Topical decongestants
Ephidrine
Otravine
Systemic
IV antibiotics
CT imaging to exclude
periorbital abscess
Foreign Bodies
Material
Paper, beads, watch batteries
etc.
Unilateral rhinorrhoea is a
foreign body until proved
otherwise
Treatment
Wrap up child
Assistant hold head
Remove
Complications of Tonsillitis
Peritonsillar abscess
Symptoms
Pain becomes more unilateral
Often referred otalgia
Trismus (therefore difficult to get a good look)
Drooling
Systemically unwell with pyrexia
Normally big tender upper deep cervical node
Refer
Complications of tonsillitis
Peritonsillar abscess (quinsy)
Peritonsillar abscess
Treatment
Incision and drainage (needle/blade)
Intravenous penicillin and metronidazole
First quinsy and previous history of
tonsillitis recommend tonsillectomy
First quinsy with no prior tonsillitis
historyverbal warning
Stridor
Harsh, high-pitched sound indicative of airway obstruction.
Inspiratory Supraglottic or Glottic
Biphasic Subglottic or Extrathoracic Trachea
Expiratory Intrathoracic Trachea
NB. Stertor High upper airway obstruction
Stridor - Assessment
What level ??
History What sort of stridor
How severe ??
Accessory muscles
Tracheal tug / Recession in children
Pulse
pCO
2
Retention
Does the airway need securing ??
Severe OR patient getting tired.
Causes
Children
Infection
Bacterial eg. Epiglottitis
Viral eg. Croup
Foreign body
Adults
Infection
Supraglottitis
Neoplasia
Squamous cell carcinoma
Stridor -management
SIT PATIENT UP
OXYGEN
RE-HYDRATION (i.v.)
STEROIDS (Nebulised, i.v. or oral)
ADRENALINE NEBULISER
HELIOX Helium / oxygen mixture
ANTI-BIOTICS
AIRWAY INTERVENTION
Intubation
Bronchoscopy
Tracheostomy
Croup vs Epiglottitis
Croup Epiglottitis
Age 1-3years 3-6 years
Duration URTI (days) Short(hours)
Clinical Viral Unwell*
Stridor Loud Quiet
* Decreased concious level, circumoral palor, rapid deterioration.
Airway Foreign Bodies
RIGHT main bronchus (more vertical)
May get air trapping, distal to FB.
Monophonic wheeze (asthma POLYphonic)
High index of suspicion - REFER
Rigid bronchoscope
Bronchoscope and camera being used to assess the airway in a child with a
tracheostomy
You might also like
- Nclex New FINALDocument266 pagesNclex New FINALNadim Khalid100% (1)
- Adenotonsillitis NewDocument100 pagesAdenotonsillitis NewDrravikumar Bhandari100% (1)
- URTDDocument61 pagesURTDfcgabasanNo ratings yet
- ENT - UnitDocument63 pagesENT - Unitsuganthi rajesh kannaNo ratings yet
- Common Ent EmergenciesDocument65 pagesCommon Ent EmergenciesferaNo ratings yet
- BHN Kuliah Traumatology English Class QP-2003 BaruDocument168 pagesBHN Kuliah Traumatology English Class QP-2003 BaruazifadewiatasyaNo ratings yet
- Ear Nose and Throat 2Document34 pagesEar Nose and Throat 2api-195799092No ratings yet
- Ent Med RevisionDocument41 pagesEnt Med RevisionswamysamsonNo ratings yet
- Common Diseases of PharynxDocument72 pagesCommon Diseases of PharynxPinak DeNo ratings yet
- Otitis MediaDocument67 pagesOtitis MediaFurqan MirzaNo ratings yet
- Ent For General PracticeDocument46 pagesEnt For General PracticefenixaNo ratings yet
- Laryngitis, Laryngeal Paralysis, DDX of Stridor, StertorDocument44 pagesLaryngitis, Laryngeal Paralysis, DDX of Stridor, StertorDurand S. KhadkaNo ratings yet
- LIMITLESS PEDIATRICS BY DR NAVEEN - DAY 4 (Green)Document56 pagesLIMITLESS PEDIATRICS BY DR NAVEEN - DAY 4 (Green)Biplav SinghNo ratings yet
- EntDocument128 pagesEntNaila Omer100% (1)
- Acute Suppurative Otitis MediaDocument24 pagesAcute Suppurative Otitis MediaDr Tipu SultanNo ratings yet
- Davao Medical School Foundation: Chris Robinson D. Laganao, MD, DPBO-HNSDocument48 pagesDavao Medical School Foundation: Chris Robinson D. Laganao, MD, DPBO-HNSVasiliás PrawinNo ratings yet
- Respiratory Emergencies in PediatricsDocument49 pagesRespiratory Emergencies in PediatricsMuhammed BarznjiNo ratings yet
- Kitty ActonDocument25 pagesKitty ActonSarina PromthongNo ratings yet
- Common Ent Emergencies 24126Document64 pagesCommon Ent Emergencies 24126Krittin NaravejsakulNo ratings yet
- Anatomy Head Neck EMRCS MCQDocument23 pagesAnatomy Head Neck EMRCS MCQTowhid HasanNo ratings yet
- Diseases of Pharynx and Larynx 150406135136 Conversion Gate01Document68 pagesDiseases of Pharynx and Larynx 150406135136 Conversion Gate01dr. EndahNo ratings yet
- IVRSDocument61 pagesIVRSAndrew ChinchillaNo ratings yet
- Ears&MouthDocument76 pagesEars&Mouthrichelley08No ratings yet
- Ryan Martin Ko, M.DDocument54 pagesRyan Martin Ko, M.DDhaval Makwana100% (2)
- Otitis Media: Prepared By: - Priyanka ThapaDocument38 pagesOtitis Media: Prepared By: - Priyanka ThapaKalo kajiNo ratings yet
- TonsillitisDocument7 pagesTonsillitisjuicyprunesNo ratings yet
- Online Learning ModuleDocument38 pagesOnline Learning ModuleMani SainiNo ratings yet
- Tonsillectomy 200829131303Document102 pagesTonsillectomy 200829131303deptanaesaiimsgkpNo ratings yet
- Otitis Media With Effusion: Shixun Zhong PH.DDocument31 pagesOtitis Media With Effusion: Shixun Zhong PH.DsuciNo ratings yet
- Otitis MediaDocument98 pagesOtitis MediaLody Lean CruzNo ratings yet
- Adenoid Hypertrophy Adenoidectomy Cesar GarciaDocument56 pagesAdenoid Hypertrophy Adenoidectomy Cesar GarciaIemima RotunduNo ratings yet
- Upper Airway InfectionDocument47 pagesUpper Airway Infectionjm_john0% (1)
- BHN Kuliah TraumatologyDocument130 pagesBHN Kuliah TraumatologySinta Dewi AdityaniNo ratings yet
- Anesthesia For Maxillofacial ProcedureDocument90 pagesAnesthesia For Maxillofacial ProcedureAnirban Roy100% (1)
- Review For ENT (2008 Batch)Document9 pagesReview For ENT (2008 Batch)HaslinNo ratings yet
- Parts: Nose Throat Pharynx LarynxDocument47 pagesParts: Nose Throat Pharynx LarynxRANJIT GOGOINo ratings yet
- Nasal Obstruction: Meng JuanDocument36 pagesNasal Obstruction: Meng JuanReshma VasuNo ratings yet
- Upper Airway Obstruction & Infection: PediatricDocument71 pagesUpper Airway Obstruction & Infection: PediatricLuke RosenczweigNo ratings yet
- OtitisanDocument54 pagesOtitisanmagreaNo ratings yet
- Eye and Ear DisordersDocument14 pagesEye and Ear Disorderslemesa abdisaNo ratings yet
- Diagnosis of Ent Disorders You Make The CallDocument137 pagesDiagnosis of Ent Disorders You Make The Callsaifsaffa2No ratings yet
- EntDocument36 pagesEntArya ChoudhuryNo ratings yet
- Concept Map FinaleDocument31 pagesConcept Map FinaleDeVineNo ratings yet
- Tons Slides 2003 1105 PDFDocument44 pagesTons Slides 2003 1105 PDFmasterhen1No ratings yet
- Disorders of EarDocument17 pagesDisorders of EarharpreetNo ratings yet
- SinusitisDocument23 pagesSinusitisMumin Alamin AllaminNo ratings yet
- ENT Emergency PresentationDocument135 pagesENT Emergency PresentationshahiruddinNo ratings yet
- 18 Head and NeckDocument23 pages18 Head and NeckMahmoud AbuAwadNo ratings yet
- Serous Otitis MediaDocument22 pagesSerous Otitis MediaChandra BhanNo ratings yet
- ENT Emergency: James Paul O'NeillDocument43 pagesENT Emergency: James Paul O'NeillkylieverNo ratings yet
- Upper Airway InfectionsDocument5 pagesUpper Airway InfectionsPhilline MacapagalNo ratings yet
- Lecture 2 Ent.Document70 pagesLecture 2 Ent.kiprotich weldonNo ratings yet
- ENT SGD 1 Clinical History and ENT Physical ExaminationDocument51 pagesENT SGD 1 Clinical History and ENT Physical ExaminationEmerson QuimbaNo ratings yet
- 12 Congenital Lesions of Larynx and Evaluation of StridorDocument77 pages12 Congenital Lesions of Larynx and Evaluation of StridorAbhishek ShahNo ratings yet
- ENTDocument51 pagesENTBryan Paul Ramirez100% (1)
- Upper Respiratory Tract Infections 2Document87 pagesUpper Respiratory Tract Infections 2wellYONGNo ratings yet
- Drugs and Substance AbuseDocument75 pagesDrugs and Substance Abuseseline sherylNo ratings yet
- Ent Eye Osce Totes - YJDocument31 pagesEnt Eye Osce Totes - YJanon_373532435No ratings yet
- Infeksi Telinga: Rizka Dany AfinaDocument63 pagesInfeksi Telinga: Rizka Dany AfinaRizka Dany AfinaNo ratings yet
- DTSCH Arztebl Int-115 0012 PDFDocument15 pagesDTSCH Arztebl Int-115 0012 PDFliseinsaniNo ratings yet
- Making Success: The StandardDocument17 pagesMaking Success: The StandardsalsomanoNo ratings yet
- BleedingDocument14 pagesBleedingRhomizal MazaliNo ratings yet
- Child's NosebleedsDocument29 pagesChild's Nosebleedsgalihmd07No ratings yet
- 14 Talking About Sickness and SymptomsDocument9 pages14 Talking About Sickness and SymptomsAdin SukamtoNo ratings yet
- Key To ENT Diagnosis by Tashfeen NasiraDocument10 pagesKey To ENT Diagnosis by Tashfeen Nasirashreyamuragi9No ratings yet
- 111 - Contact PrecautionsDocument115 pages111 - Contact PrecautionsOlgaKNo ratings yet
- Enhanced Reading Intervention Program For Junior High School StudentsDocument36 pagesEnhanced Reading Intervention Program For Junior High School StudentsEditor IJTSRDNo ratings yet
- P.E 9 Week 6 Activity Sheets Q 3.final 2Document4 pagesP.E 9 Week 6 Activity Sheets Q 3.final 2NathanielNo ratings yet
- Epistaxis 1Document2 pagesEpistaxis 1Muhammad Azhar BasyirNo ratings yet
- ATROVENTDocument25 pagesATROVENTNúñez AlejandroNo ratings yet
- American Journal of Emergency MedicineDocument4 pagesAmerican Journal of Emergency MedicineAnonymous 4qjMN06rHsNo ratings yet
- ExamDocument43 pagesExamFoxtrot NursingNo ratings yet
- Packing ReviewDocument16 pagesPacking ReviewChandrasekaryas2010No ratings yet
- Basic Medical Arabic EnglishDocument10 pagesBasic Medical Arabic EnglishLuisMunozD'Santos100% (3)
- Barotac Nuevo National Comprehensive High SchoolDocument2 pagesBarotac Nuevo National Comprehensive High SchoolVon AlexisNo ratings yet
- Updates On The Management of EpistaxisDocument9 pagesUpdates On The Management of EpistaxisIlham NoeryosanNo ratings yet
- English Reading Passage JhsDocument3 pagesEnglish Reading Passage JhsEve MacerenNo ratings yet
- Nosebleed PDFDocument4 pagesNosebleed PDFgsundar8173No ratings yet
- Sas 4 Cabahug, Victoria Mae IDocument4 pagesSas 4 Cabahug, Victoria Mae Ibekbekk cabahugNo ratings yet
- Set BDocument25 pagesSet BImraan KhanNo ratings yet
- Nasal Septal HematomaDocument12 pagesNasal Septal HematomaNoor Al Zahraa AliNo ratings yet
- Grade 4 Reading PassagesDocument43 pagesGrade 4 Reading PassagesCherry MaeNo ratings yet
- Primary Hospital (Catering Exclusive)Document40 pagesPrimary Hospital (Catering Exclusive)Jonas AsiaNo ratings yet
- Assessing Head, Face and NeckDocument112 pagesAssessing Head, Face and NeckHyacinth Jane Dela PeñaNo ratings yet
- Soap 1Document4 pagesSoap 1api-248360288No ratings yet
- Reading Comprehension PracticeDocument6 pagesReading Comprehension PracticeAngelica 01No ratings yet
- Embolisation in ENTDocument9 pagesEmbolisation in ENTsudheer joelNo ratings yet
- MS 21Document10 pagesMS 21karenkaren09No ratings yet