Professional Documents
Culture Documents
BB - Unit6ABO and H Blood Groups
Uploaded by
Charmaine Corpuz GranilOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BB - Unit6ABO and H Blood Groups
Uploaded by
Charmaine Corpuz GranilCopyright:
Available Formats
ABO and H Blood
Groups
Terry Kotrla, MS,
MT(ASCP)BB
2010
History
Discovered in 1900 by Karl Landsteiner
and remains the most important blood
group system
Mixed blood of colleagues (serum from
one, cells from another) together
Discovered A, B and O
His student discovered AB in 1902
Landsteiners Rule
Reciprocal antibodies are consistently and
predictably present in the sera of normal
people whose rbcs lack the corresponding
antigen(s)
He was awarded the Nobel Prize in
Physiology or Medicine in 1930 for his
work
Landsteiners Rule
Red Cell membrane structure
Surface of the RBC consists of a bilipid
membrane in which large protein
molecules are embedded.
Composed of phosholipids which are both
hydrophilic (heads) and hydrophobic
(tails).
Red Blood Cell Membrane
Red Blood Cell Membrane
Red Blood Cell Membrane
External surface of RBC membrane is coated
with a diverse array of glycoproteins, complex
carbohydrates, and lipoproteins, imparting
antigenic structure to the membrane.
A and B Antigens
Inheritance follows Mendelian genetics
Frequency in white population: group O
45%, group A 40%, group B 11% and
group AB 4%.
Frequencies differ in selected populations and
ethnic groups
Group B higher in Black and Asian
populations
A and B Antigens
Not fully developed at birth, fewer copies
of the antigen on the cells.
Antigens detectable as early as 5 weeks
after conception
Human typing sera may give weaker, or
very rarely negative, reactions
Biochemistry of A, B, H Antigens
ABO antigens are located on RBCs, lymphs,
platelets, tissue cells, bone marrow and solid
organs.
Inheritance results in expression.
Antigens ARE NOT direct products of the genes.
Genes code for TRANSFERASE which causes
transfer of monosaccharide molecule onto a
precursor substance on the RBC.
H Gene
Codes for the production of fucosyl transferase that catalyzes the
addition of L-fucose,the immunodominant structure of H antigen.
Two slightly different structures, known as the type 1 and type 2
precursor chains.
The H gene and its allele h are inherited independently of the allelic
A, B and O genes
H antigen only person is group O.
Once L-fucose added A and B gene specified products can be add
their sugars.
A Gene
Codes for production of a galactosaminyl
transferase that effects the addition of N-
acetyl-galactosamine to the preformed H-
bearing chains.
B Gene
Codes for production of a galactosyl
transferase that effects the addition of D-
galactose to the same H-bearing structure.
A, B and H
A, B and H
Immunodominant structure of the H
antigen is L-fucose person is group O
Immunodominant structure of A antigen N-
acetyl-galactosamine person is group A
Immunodominant structure of the B
antigen, D-galactose- person is group B
Bombay (O
h
)
If L-fucose is added H, A and B cannot be added.
Individual may inherit A or B genes but without H the
immunodominant sugars CANNOT be added.
Must be homozygous for h, which is an amorph, with no
detectable product, similar to d.
A Bombay individual has genotype hh but WILL type as
Group O.
Can only be determined by family studies or testing with
lectins
Bombay
The H System
Two genes: H and h
H 99.9%>
H <0.%
Leads to production of H antigen precursor
molecule for A and B antigens.
Ulex europaeus = anti-H
Not all H is converted to A or B, varies among
the blood groups.
Memorize: 0>A
2
>B>A
2
B>A
1
>A
1
B
H Antibodies
H-like antigens are found in nature.
Anti-H occasionally detected in A
1
, A
1
B
and rarely in B individuals and will cause
false positive in the REVERSE reaction.
So little H on cells may form anti-H
Relatively weak
Almost always reacts at RT
Considered clinically insignificant
H Antibodies
May cause an ABO discrepancy
Anti-A Anti-B A
1
cells B Cells Interp
4+ 0 1+ 4+
4+ 0 1+ 1+
H Antibodies
In contrast persons of the rare Oh (hh)
phenotype (have no A, B or H antigens on their
RBCs) form a potent clinically significant anti
H which reacts well over a wide thermal range
and with all RBCs except those of other O
people.
Anti-A Anti-B A1 Cell B Cell O Cell
0 0 4+ 4+ 4+
O
h
Phenotype (Bombay)
Occurs when two hh genes are inherited
at the Hh locus.
Possess normal A or B genes (if they were
inherited) but unable to express.
Must have H on red cell membrane
Can transmit A or B gene to offspring
Term Bombay used since first
discovered in Bombay, India
O
h
Phenotype (Bombay)
Symbol O
h
denotes this phenotype
RBCs not agglutinated by anti-A, -B or A,B
Serum/plasma agglutinates A and B cells
Not recognized until serum tested against group
O cells and causes strong agglutination.
Have anti-A, -B, -A,B and H
Can only be transfused with Bombay blood <0.01%
O
h
Phenotype (Bombay)
Confirmatory testing
Anti-H lectin (Ulex europaeus) negative
Agglutination of A, B, AB and O cells
Serum/plasma will not agglutinate Oh cells.
Secretor Genes
A, B and H antigens may be present in
fluids.
Controlled by Se and se, secretor genes.
Need only one copy of the Se gene.
The gene se is an amorph.
Not linked to ABO locus, inherited
independently
Secretor Genes
Persons who have A, B and/or H in secretions
are called secretors
Blood Group Substance in Secretions
A A and H
B B and H
AB A, B and H
O H
Secretor Genes
Secretor studies helpful in defining weak
subgroups or resolving genetic make up of
individuals with unusual blood group
80% of Caucasians are secretors
20% are non-secretors
Subgroups of A (A
1
and A
2
)
Subgroups of A are phenotypes that differ
from others of the same ABO group with
respect to the
amount of A antigen carried on RBCs, and,
in secretors, present in the saliva.
Variant gene produces a weaker than
normal red cell antigen
Subgroups of A (A
1
and A
2
)
Different levels of expression of A (or B)
on RBCs are classified into subgroups
80% of group A individuals are A1
Approximately 20% are A2
Transferase produced by A2 gene differs
from that produced by A1, less efficient in
converting H chains to A
Subgroups of A
Difference Between A
1
and A
2
A
1
has more A and less H antigen on the
cell.
A
2
has less A and more H antigen
Cannot be detected serologically
A
2
can produce anti- A
2
qualitative
difference?
Lectins
Naturally occurring materials (usually
plant) that react specifically with blood
group antigens.
Dolichos biflorus anti-A
1
Will agglutinate A
1
red blood cells
Will not agglutinate A
2
red blood cells
Anti-A
1
1-8% of A2 and 22-35% of A2B people will
have anti-A1
Causes ABO discrepancy reverse type
Incompatible crossmatch if donor A1
NOT clinically significant unless reactive at
37C or AHG.
Clinically significant ability to cause red
cell destruction donor blood or hemolytic
disease of the fetus and newborn.
Subgroups of A weaker than A2
Occur infrequently, characterized by
decreasing numbers of A antigens
Less than 1% of total A gene pool
Classification of Weak A Subgroups
Strength of agglutination when tested with:
Anti-A1 lectin
Anti-A,B
Anti-H lectin
Presence of anti-A1
Presence of A and H in secretions
Subgroups of A
Subgroups of A weaker than A2 (Ael, Aint,
A3, Ax, Am, etc) are seen only infrequently
NOTE: A3 is characterized by mixed field
agglutination.
Subgroups of B
Less common than subgroups of A
Criteria resembles that used for A subgroups
Usually detected based on forward type, reverse
type correctly
Do not make anti-B as commonly
NOTE: B3 characterized by mixed field
agglutination
Antibodies to A and B
Landsteiner individuals do not form antibodies
against antigens on their own cells.
Naturally ocurring is a misnomer
Antibody production stimulated by substances in the
environment similar to blood group antigens
Simply implies antibody production NOT due to actual
exposure to red blood cells
Allows both serum/plasma and red cells to
determine ABO type check/balance system
Development of anti-A and anti-B
Antibody production first few months of life
Babies cannot be reversed typed:
Antibodies present in baby from mom
Are not born with antibodies, detectable at 3 to 6
months of age
Once produced remain constant until elderly
Complete absence of ABO antibodies
exceedingly rare
Anti-A,B
Group O have THREE ABO antibodies:
anti-A, -B and A,B
may react more strongly than anti-A and
anti-B with some weak A or B subgroups
use anti-A,B to test group O donors
used to type babies, antigens not being
well-developed at birth
Antibody Characteristics
React best at room temperature.
Agglutinate saline suspended red cells, no
additional reagents are necessary
May produce hemolysis in vivo and in vitro
Routine Testing For ABO Group
Forward -Test known anti-serum with
unknown patient cells (antigens)
Reverse Test unknown serum (antibody)
with known A and B antigens (cells0
MUST MATCH
ABO Discrepancies
Discrepancy between forward and reverse
Helpful observations
Strength of reaction: forward 4+ if antigen present,
reverse 2-4+.
Unexpected negative in reverse
Unexpected positive in forward OR reverse
Must delay transfusion until resolved
emergency give out O RBCs and appropriate D
type
ABO Discrepancies
Errors divided into two categories
Technical
Sample
Results in false positives and negatives
Sample errors divided into rbc and serum
ABO Discrepancy Technical False Negative
Failure to add serum or antiserum to a test.
Failure to identify hemolysis as a positive reaction.
Not using the appropriate serum (or reagent) to cell ratio.
Improper centrifugation.
Incubation of tests at temperatures above 20-25 C.
Use of inactive reagents.
Failure to interpret or record test results correctly.
ABO Discrepancy Technical False Positive
Over centrifugation
Use of contaminated reagent antibodies,
RBCs or saline
Use of dirty glassware
Incorrect interpretation or recording of
results
Problems Associated With Testing RBC
Sample from recently transfused or bone marrow
transplant patient
ABO subgroup or weakened antigens due to disease
such as leukemia
Abnormal proteins or Whartons jelly
Increased A or B blood group substances inhibit reaction
false negative
Antibodies to dyes in forward reagents
Cold autoagglutinins patient cells may spontaneously
agglutinate
Problems Associated with Serum
Weak or negative due to patients condition or IV fluids
Fibrin clots
Rouleaux
High levels abnormal proteins
Unexpected antibodies
Antibodies to reagent chmicials
Negative or weak reactions in infants < 6 months
Bone marrow transplant ABO non-identical donor
Transfused with non-ABO identical plasma products
Resolving ABO Discrepancies
REPEAT THE TEST
Patient group A with agglutination of A1 cells
test patient cells with anti-A1 and patient
serum/plasma with A2 cells
MOST COMMONLY encountered discrepancy.
Example testing to prove A2 with anti-A1
Anti-A Anti-A1 A1 cells A2 cells
4+ 0 1-2+ 0
Resolving ABO Discrepancies
Incubate reverse at RT for 15-30 minutes
if false negative suspected.
Can incubate at 4C but MUST run autocontrol
Decreased antibody most frequent cause of
false negative in reverse
Wash patient and reagent RBCs
Obtain a new sample
ABO Discrepancies
Test against group O adult, group O cord and
auto-control to detect cold agglutinins
Cold agglutinin = anti-I, adult cells have I, cord
cells have little or no I at birth.
Adult O cells Cord O cells Auto=control
4+ 0/1+ 4+
Acquired B Phenotype - B (A)
Forward = AB, reaction with anti-B weak
Serum contains anti-B
Phenomena associated with
colon or rectal cancer
Gram negative sepsis
Intestinal obstruction
Increased detection with monclonal anti-B
Acquired B
Bacteria (E. coli) have a deacetylating
enzyme that effects the A sugar.
Group A
individual
N-acetyl galactosamine
Acquired
B
Phenotype
Bacterial enzyme
removes acetyl group
Galactosamine
now resembles
D-galactose (found
in Group B)
Mixed Field Agglutination
Sample has TWO distinct cell populations
A or B patient transfused with group O
D pos transfused with D neg OR D neg
transfused with D pos
BMT with different ABO type
A3 or B3 subgroups
Chimerism - rarest
Mixed Field Agglutination
Transfusion Practice
Provide serologically compatible blood.
Whole blood must be ABO identical - has RBCs
AND plasma
For Red Blood Cells the donor must lack the
ABO antigen to which the patient has antibodies.
Group O is the universal donor.
Group AB is the universal recipient.
Donor products such as FFP and Platelet
concentrates must lack ABO antibodies to
recipient RBCs.
AB is the universal donor
Group O is the universal recipient
Grouping
Forward Reverse
Missing/Weak Extra Mixed Field Missing/Weak Extra
A/B Subgroup
Disease
(cancer)
Acquired B
B(A) Phenotype
O Transfusion
Bone Marrow
Transplant
Young
Elderly
Immunocompromised
Cold
Autoantibody
Anti-A
1
Rouleaux
Cold
Alloantibody
Rouleaux
May cause all + reactions
Lets practice !
Example 1
Anti-A Anti-B A1 Cells B Cells
3+ 0 0 1+
Problem:
Causes:
Resolution:
Example 2
Anti-A Anti-B A1 Cells B Cells
3+ 1+ 0 4+
Problem:
Causes:
Resolution:
Example 3
Anti-A Anti-B A1 Cells B Cells
2+ 0+ 1+ 4+
Problem:
Causes:
Resolution:
Example 4
Anti-A Anti-B A1 Cells B Cells
0 0 0 3+
Problem:
Causes:
Resolution:
Example 4
Anti-A,B
Patient RBC 1+
Probably a subgroup of A (A
x
)
if the result was negative (0), adsorption or elution
studies with anti-A could be performed (these will
help determine what A antigens)
Example 5
Anti-A Anti-B A1 Cells B Cells
0 2+mf 3+ 0
Problem:
Causes:
Resolution:
Example 6
Anti-A Anti-B A1 Cells B Cells
4+ 4+ 0 1+
Problem:
Causes:
Resolution:
Example 7
Anti-A Anti-B A1 Cells B Cells
0 0 0 0
Problem:
Causes:
Resolution:
Example 6
Screening
Cells
(I and II)
Autocontrol
(AC)
Conclusion
Patient
Serum 1
Pos Neg Cold
alloantibody
Patient
Serum 2
Pos Pos Cold
autoantibody
if alloantibody antibody ID techniques
if autoantibody special procedures (minicold panel, prewarming techniques
Visit!
http://faculty.matcmadison.edu/mljensen/BloodBank/lectures/abo_blood_group_system.htm
http://drpeterjdadamo.com/wiki/wiki.pl/Lewis_Blood_Group
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Signed RBSN Guidelines (Central Luzon)Document19 pagesSigned RBSN Guidelines (Central Luzon)Charmaine Corpuz GranilNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Compatibility TestingDocument36 pagesCompatibility TestingCharmaine Corpuz Granil100% (1)
- Atlas Human Anatomy Ciba NetterDocument641 pagesAtlas Human Anatomy Ciba Netterxxxx79% (28)
- Gram Positive Cocci Sem 1 1Document45 pagesGram Positive Cocci Sem 1 1Charmaine Corpuz Granil100% (1)
- NBME 24 TopicsDocument5 pagesNBME 24 TopicsSteele FisherNo ratings yet
- Atlas Of: Human Body Ultrasound ScanningDocument575 pagesAtlas Of: Human Body Ultrasound ScanningGARY WILLIAMS CORTEZ PEREZNo ratings yet
- Infectious Disease NotesDocument19 pagesInfectious Disease Notesshwetlana rampureNo ratings yet
- ENTEROBACTERIACEAEDocument40 pagesENTEROBACTERIACEAECharmaine Corpuz GranilNo ratings yet
- Hospital Blood Transfusion Committee ReportDocument3 pagesHospital Blood Transfusion Committee ReportCharmaine Corpuz Granil0% (1)
- Human Body Systems Lesson Plan 3Document3 pagesHuman Body Systems Lesson Plan 3api-338430889100% (1)
- Specimen Preparation: Grossing and Sectioning: Manuelito A. Madrid, MD, FPSPDocument30 pagesSpecimen Preparation: Grossing and Sectioning: Manuelito A. Madrid, MD, FPSPCharmaine Corpuz Granil100% (2)
- Mcq Exams Ent 3rd Edition الهيئة السعوديةDocument162 pagesMcq Exams Ent 3rd Edition الهيئة السعوديةHamada Hassan Alloq100% (1)
- TNCT Q4 Module5Document22 pagesTNCT Q4 Module5Glenn Mendez100% (1)
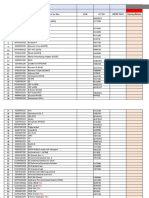
- COBAS 6000: E601 Reagent Inventory MONTH/YEAR: - AUGUST 2020Document3 pagesCOBAS 6000: E601 Reagent Inventory MONTH/YEAR: - AUGUST 2020Charmaine Corpuz GranilNo ratings yet
- Laboratory Department Tracking Sheet OriginalDocument124 pagesLaboratory Department Tracking Sheet OriginalCharmaine Corpuz GranilNo ratings yet
- COBAS 6000: C501 Reagent Inventory MONTH/YEARDocument3 pagesCOBAS 6000: C501 Reagent Inventory MONTH/YEARCharmaine Corpuz GranilNo ratings yet
- Custom Tailored Email: CGFNS ID Number: 7455589 Order Number: 3368466 User Name: CharmaineDocument1 pageCustom Tailored Email: CGFNS ID Number: 7455589 Order Number: 3368466 User Name: CharmaineCharmaine Corpuz GranilNo ratings yet
- Table of BenefitsDocument3 pagesTable of BenefitsCharmaine Corpuz GranilNo ratings yet
- Job Description: JOB TITLE: Laboratory TechnicianDocument3 pagesJob Description: JOB TITLE: Laboratory TechnicianCharmaine Corpuz GranilNo ratings yet
- COBAS 6000: E601 Reagent Inventory MONTH/YEARDocument2 pagesCOBAS 6000: E601 Reagent Inventory MONTH/YEARCharmaine Corpuz GranilNo ratings yet
- Salary Transfer Form: Employee Name: Staff ID Number: Designation: Date of Joining: Facility Name: Passport NumberDocument1 pageSalary Transfer Form: Employee Name: Staff ID Number: Designation: Date of Joining: Facility Name: Passport NumberCharmaine Corpuz GranilNo ratings yet
- DMH Blood Safety IndicatorDocument7 pagesDMH Blood Safety IndicatorCharmaine Corpuz GranilNo ratings yet
- Gram Negative Cocci-Sem 1.Document21 pagesGram Negative Cocci-Sem 1.Charmaine Corpuz GranilNo ratings yet
- Act No.2 Question # 3-4. With ReferenceDocument2 pagesAct No.2 Question # 3-4. With ReferenceCharmaine Corpuz GranilNo ratings yet
- HYPERTRICHOSISDocument11 pagesHYPERTRICHOSISCharmaine Corpuz GranilNo ratings yet
- Immunology and SerologyDocument4 pagesImmunology and SerologyCharmaine Corpuz GranilNo ratings yet
- Gram Positive Cocci - Sem 1Document45 pagesGram Positive Cocci - Sem 1Charmaine Corpuz GranilNo ratings yet
- Rizal InSunny Spain ) )Document31 pagesRizal InSunny Spain ) )Charmaine Corpuz GranilNo ratings yet
- Central Luzon Doctors HospitalDocument3 pagesCentral Luzon Doctors HospitalCharmaine Corpuz GranilNo ratings yet
- Significance of The StudyDocument2 pagesSignificance of The StudyCharmaine Corpuz Granil83% (6)
- Endometriosis & AdenomyosisDocument54 pagesEndometriosis & AdenomyosisKapil StaleyNo ratings yet
- Gills vs. LungsDocument1 pageGills vs. Lungsmartinscottwalker1178100% (2)
- Canine Demodecosis and Babesiosis - Bambang Pontjo-INDONESIADocument14 pagesCanine Demodecosis and Babesiosis - Bambang Pontjo-INDONESIAIkhwanul KhairiaNo ratings yet
- Frog DissectionDocument4 pagesFrog Dissection2110038No ratings yet
- LAW246 Lecture Notes 4Document3 pagesLAW246 Lecture Notes 4Lita ptr projectNo ratings yet
- Bavituximab MOA BrochureDocument3 pagesBavituximab MOA BrochureinternetforumuserNo ratings yet
- Patologi Sistem Pencernaan Hati Sesi 1aDocument36 pagesPatologi Sistem Pencernaan Hati Sesi 1adewinurfadilahNo ratings yet
- DX Procedure & Nursing ResponsibilityDocument3 pagesDX Procedure & Nursing ResponsibilityGwyneth SantiagoNo ratings yet
- Relevant Equine Renal Anatomy, Physiology and Mechanisms of AKI ReviewDocument12 pagesRelevant Equine Renal Anatomy, Physiology and Mechanisms of AKI ReviewMarilú ValdepeñaNo ratings yet
- Sporogenous TissueDocument4 pagesSporogenous TissueJewel SajiNo ratings yet
- Bio270 Tutorial Week 10Document2 pagesBio270 Tutorial Week 10Mirza KarmilaNo ratings yet
- Pharyngitis SiccaDocument3 pagesPharyngitis SiccaEdris SharifiNo ratings yet
- PhysioEx Exercise 3 Activity 7Document5 pagesPhysioEx Exercise 3 Activity 7Alesandra Campo Sanmartín100% (1)
- Pathologyofdiseasesof Geriatricexoticmammals: Drury R. Reavill,, Denise M. ImaiDocument34 pagesPathologyofdiseasesof Geriatricexoticmammals: Drury R. Reavill,, Denise M. ImaiRaquel MotaNo ratings yet
- Oncologic Nursing: Naming of CancerDocument7 pagesOncologic Nursing: Naming of CancerDianne MaeNo ratings yet
- 16 Immune System Review SheetDocument2 pages16 Immune System Review Sheetjohn gusmanNo ratings yet
- Medical Terminolog1Document25 pagesMedical Terminolog1Jullia SollezaNo ratings yet
- Year 10 DPP Biology Term 3 Exam RevisionDocument8 pagesYear 10 DPP Biology Term 3 Exam RevisionPoojit VenugopalaNo ratings yet
- Int J Lab Hematology - 2021 - Kitchen - International Council For Standardization in Haematology ICSH Recommendations ForDocument12 pagesInt J Lab Hematology - 2021 - Kitchen - International Council For Standardization in Haematology ICSH Recommendations ForLaboratorium RS BELLANo ratings yet
- Class 5 Science Classwork 091020Document3 pagesClass 5 Science Classwork 091020Rakesh AgarwalNo ratings yet
- A Case of Giant Pleomorphic Adenoma of The Parotid GlandDocument3 pagesA Case of Giant Pleomorphic Adenoma of The Parotid GlandmitaNo ratings yet
- Model Answers: Chapter 13 Homeostasis and The Human Urinary SystemDocument3 pagesModel Answers: Chapter 13 Homeostasis and The Human Urinary Systemsyed aliNo ratings yet
- Anatomy LandmarkDocument31 pagesAnatomy LandmarkWildan Humairah33% (3)