Professional Documents
Culture Documents
Spirometry Pulmonary Function Test
Uploaded by
hoohoo0 ratings0% found this document useful (0 votes)
26 views17 pagesCopyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views17 pagesSpirometry Pulmonary Function Test
Uploaded by
hoohooCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 17
SPIROMETRY
Prepared by: Rose Marie B. Lagasca, MAN
• Spirometry: A lung function test to
measure breathing capacity and how
well you breathe. You will breathe
into a device called a spirometer.
What is the role of spirometry in the diagnosis
of asthma?
• Spirometry assessments should be obtained as the primary
test to establish the asthma diagnosis. Spirometry should be
performed prior to initiating treatment in order to establish the
presence and determine the severity of baseline airway
obstruction. Optimally, the initial spirometry should also
include measurements before and after inhalation of a short-
acting bronchodilator in all patients in whom the diagnosis of
asthma is considered.
• Spirometry measures the forced vital capacity
(FVC), the maximal amount of air expired from the
point of maximal inhalation, and the forced
expiratory volume in one second (FEV1). A
reduced ratio of FEV1 to FVC, when compared
with predicted values, demonstrates the presence
of airway obstruction. Reversibility is demonstrated
by an increase of 12% and 200 mL after the
administration of a short-acting bronchodilator.
• Spirometry is a simple breathing test. It measures how much air flows in
and out of your lungs. If you have symptoms that could be a sign of
asthma—like shortness of breath—you should have a spirometry test.
• Spirometry helps diagnose and manage asthma.
• A spirometry test can confirm whether you have asthma or another
disease. And it helps your healthcare provider decide on your treatment. A
spirometry test can also show how well your treatment is working. If
follow-up spirometry tests show that your asthma is well controlled, your
treatment is working. If it shows that your asthma is not under control,
your doctor may need to change your medicine or give you more
medicine.
• When should you have a spirometry test?
• Children older than age five, and adults of any age, who have asthma-like
symptoms should have a spirometry test. The healthcare provider should
also do a physical exam and a full medical history. If the test shows that
you have asthma, your doctor should prescribe asthma medicine. Then
you should be retested four to six weeks later. If your test results improve,
your treatment is working. You may even be able to take less medicine. If
your symptoms get worse, you should have another spirometry test. If
your symptoms are controlled, you should have a test at least once every
year or two.
• How to prepare for a spirometry test
• You shouldn’t smoke one hour before a spirometry test.
You’ll also need to avoid alcohol that day as well.
Eating too large of a meal could also impact your ability
to breathe.
• Don’t wear clothing that’s so tight that it could restrict
your breathing. Your doctor may also have instructions
about whether you should avoid using inhaled breathing
medications or other medications prior to your test.
Spirometry procedure
• A spirometry test usually takes about 15 minutes and generally happens in
your doctor’s office. Here’s what happens during a spirometry procedure:
• You’ll be seated in a chair in an exam room at your doctor’s office. Your
doctor or a nurse places a clip on your nose to keep both nostrils closed.
They also place a cup-like breathing mask around your mouth.
• Your doctor or nurse next instructs you to take a deep breath in, hold your
breath for a few seconds, and then exhale as hard as you can into the
breathing mask.
• You’ll repeat this test at least three times to
make sure that your results are consistent.
Your doctor or nurse may have you repeat
the test more times if there is a lot of
variation between your test results. They’ll
take the highest value from three close test
readings and use it as your final result.
• If you have evidence of a breathing disorder, your
doctor might then give you an inhaled medication
known as a bronchodilator to open up your lungs
after the first round of tests. They’ll then ask you
to wait 15 minutes before doing another set of
measurements. Afterward, your doctor will
compare the results of the two measurements to
see whether the bronchodilator helped increase
your airflow.
• When used to monitor breathing disorders, a
spirometry test is typically done once a year
to once every two years to monitor changes
in breathing in people with well-controlled
COPD or asthma. Those with more severe
breathing problems or breathing problems
that aren’t well controlled are advised to
have more frequent spirometry tests.
Spirometry side effects
• Few complications can occur during or after a spirometry test.
You may feel a bit dizzy or have some shortness of breath
immediately after performing the test. In very rare cases, the
test may trigger severe breathing problems.
• The test requires some exertion, so it isn’t recommended if you
recently had a heart condition or have other heart problems.
Spirometry normal values and how to
read your test results
• Normal results for a spirometry test vary from person to person. They’re based
on your age, height, race, and gender. Your doctor calculates the predicted
normal value for you before you do the test. Once you’ve done the test, they look
at your test score and compare that value to the predicted value. Your result is
considered normal if your score is 80 percent or more of the predicted value.
• Spirometry measures two key factors: expiratory forced vital capacity (FVC) and
forced expiratory volume in one second (FEV1). Your doctor also looks at these
as a combined number known as the FEV1/FVC ratio. If you have obstructed
airways, the amount of air you’re able to quickly blow out of your lungs will be
reduced. This translates to a lower FEV1 and FEV1/FVC ratio.
FVC measurement
• One of the primary spirometry measurements is FVC, which is the greatest total amount of air you can
forcefully breathe out after breathing in as deeply as possible. If your FVC is lower than normal, something is
restricting your breathing.
• Normal or abnormal results are evaluated differently between adults and children:
• For children ages 5 to 18:
• Percentage of predicted FVC value Result
• 80% or greater normal
• less than 80% abnormal
Patient undergo spirometry test
References:
• 1. What is the role of spirometry in the diagnosis of asthma?
• https://www.medscape.com/answers/296301-8005/what-is-the-role-of-spir
ometry-in-the-diagnosis-of-asthma
• 2. Spirometry for Asthma
• https://www.choosingwisely.org/patient-resources/spirometry-for-asthma/
• 3. Spirometry: What to Expect and How to Interpret Your Results
• https://www.healthline.com/health/spirometry
You might also like
- Pediatric Case 5: Charlie Snow: Guided Reflection QuestionsDocument4 pagesPediatric Case 5: Charlie Snow: Guided Reflection QuestionsTancred Uy100% (3)
- Close Your MouthDocument144 pagesClose Your MouthSelvakumaran Dhandapani100% (13)
- Respiratory Care Review: An Intense Look at Respiratory Care Through Case StudiesFrom EverandRespiratory Care Review: An Intense Look at Respiratory Care Through Case StudiesNo ratings yet
- Pulmonary Function TestsDocument7 pagesPulmonary Function Testspragna novaNo ratings yet
- Pulmonary Function Test: By: Alfaro, Ruby Jane SDocument13 pagesPulmonary Function Test: By: Alfaro, Ruby Jane SgjevamNo ratings yet
- lr5 - ILHAASHINI (012021090323) - Lab 5 DoneDocument7 pageslr5 - ILHAASHINI (012021090323) - Lab 5 DoneIlhaashini krishnanNo ratings yet
- Pulmonary Function TestsDocument24 pagesPulmonary Function TestsSachin KonkaniNo ratings yet
- Spirometry For Diagnosis of CopdDocument4 pagesSpirometry For Diagnosis of CopdriasaliNo ratings yet
- Spiro Me TryDocument18 pagesSpiro Me TryAreesha ArifNo ratings yet
- Pulmonary Function TestsDocument2 pagesPulmonary Function TestsNishanth SampathNo ratings yet
- PFT Preparation and ResultsDocument3 pagesPFT Preparation and ResultsBuatlogin DoangNo ratings yet
- Respi Update 2019 SpirometryDocument48 pagesRespi Update 2019 SpirometryJashveerBedi100% (1)
- PFT Tests Measure Lung FunctionDocument19 pagesPFT Tests Measure Lung FunctionAshenafi BerhanuNo ratings yet
- Spirometry Interpretation MCAS Miramar 4-7-10Document73 pagesSpirometry Interpretation MCAS Miramar 4-7-10Henry WojtczakNo ratings yet
- TXTXDocument7 pagesTXTXHydie Mae AlcabedosNo ratings yet
- Peak Flow MetersDocument16 pagesPeak Flow Meters1048477No ratings yet
- Spirometry Instructions HandoutDocument3 pagesSpirometry Instructions HandoutJathurshika VigneswaranNo ratings yet
- Pulmonary Function TestDocument7 pagesPulmonary Function Testgurneet kourNo ratings yet
- Spiro Me Try Cheat Sheet 09Document2 pagesSpiro Me Try Cheat Sheet 09Yudha Perwira PutraNo ratings yet
- The PFT LexiconDocument3 pagesThe PFT Lexiconjmel67No ratings yet
- Pulmonary Function TestsDocument1 pagePulmonary Function Testsprecious_n143No ratings yet
- Peak Flow MeterDocument3 pagesPeak Flow MeterNicole PramonoNo ratings yet
- Spirometry: Performance and Interpretation A Guide For General PractitionersDocument15 pagesSpirometry: Performance and Interpretation A Guide For General PractitionersAgi AngloSaxonNo ratings yet
- GOLD Spirometry 2010Document59 pagesGOLD Spirometry 2010Ck Kma100% (1)
- BM Project On SpirometerDocument11 pagesBM Project On SpirometerAnushka NardeNo ratings yet
- Spirometris Con Enfoque ClínicoDocument7 pagesSpirometris Con Enfoque ClínicomariaNo ratings yet
- Pulmonary Function TestDocument13 pagesPulmonary Function TestsajjadNo ratings yet
- Peak Expiratory Flow Rate Measurements Guidelines: The Royal Free Hampstead Nhs TrustDocument14 pagesPeak Expiratory Flow Rate Measurements Guidelines: The Royal Free Hampstead Nhs TrustsivaNo ratings yet
- INTRODUCTION TO SPIROMETRY and 6MWT EditDocument8 pagesINTRODUCTION TO SPIROMETRY and 6MWT Editsai vasavi bandaruNo ratings yet
- Health Screenig ServicesDocument36 pagesHealth Screenig ServicesTarachand LalwaniNo ratings yet
- Peak Flow Meter - SpirometryDocument9 pagesPeak Flow Meter - SpirometryJoanne MayNo ratings yet
- Measure Airflow With PEFDocument3 pagesMeasure Airflow With PEFukmppdNo ratings yet
- Guidelines For Setting Up A Spirometry ServiceDocument12 pagesGuidelines For Setting Up A Spirometry ServicealiNo ratings yet
- PFT measures lung function through spirometry, diffusion testsDocument4 pagesPFT measures lung function through spirometry, diffusion testspragna novaNo ratings yet
- Week 4 - Ms1 Course Task - Cu 4 - RoveroDocument2 pagesWeek 4 - Ms1 Course Task - Cu 4 - RoveroJohnmarkLorenzanaRoveroNo ratings yet
- Understanding Spirometry: Diagnosing and Monitoring Lung DiseaseDocument68 pagesUnderstanding Spirometry: Diagnosing and Monitoring Lung Diseasex22xNo ratings yet
- Basics of SpirometryDocument15 pagesBasics of SpirometryPeter BockarieNo ratings yet
- Pulmonary Function HandoutDocument50 pagesPulmonary Function HandoutAbed SabeNo ratings yet
- History and Physical Exam For COPDDocument10 pagesHistory and Physical Exam For COPDCathy GuerreroNo ratings yet
- PEFR MetreDocument6 pagesPEFR MetreEbuwa AmadasunNo ratings yet
- Definition of Asthma: Controller) Medication Usually Prescribed inDocument5 pagesDefinition of Asthma: Controller) Medication Usually Prescribed inpiterwiselyNo ratings yet
- Diagnostic Tests & Treatments for AsthmaDocument4 pagesDiagnostic Tests & Treatments for AsthmaFrauline GagaracruzNo ratings yet
- 48 SpirometryDocument18 pages48 SpirometryZeeshan AhmadNo ratings yet
- Assessment of Respiratory FunctionDocument1 pageAssessment of Respiratory FunctionRoderick AgbuyaNo ratings yet
- Asthma - Peak Flow MeterDocument22 pagesAsthma - Peak Flow Meterapi-3729824100% (2)
- Spyrometry Flipchart PDF FinalDocument10 pagesSpyrometry Flipchart PDF FinalHiếu KiềuNo ratings yet
- Pulmonary Function Testing: Camilla Hollen, MMS, PA-C PA 530Document49 pagesPulmonary Function Testing: Camilla Hollen, MMS, PA-C PA 530KatherynSotoNo ratings yet
- Asthma by DR SarmaDocument88 pagesAsthma by DR SarmaSurbhi JoshiNo ratings yet
- COPD - Diagnostics 2 1Document8 pagesCOPD - Diagnostics 2 1Hydie Mae AlcabedosNo ratings yet
- Asthma Update: 10 Key Clinical ActivitiesDocument48 pagesAsthma Update: 10 Key Clinical ActivitiesSusie Marsick MartinNo ratings yet
- 01 05 05 Occs10080)Document7 pages01 05 05 Occs10080)IJIRAE- International Journal of Innovative Research in Advanced EngineeringNo ratings yet
- Dr. Rowshne Jahan Spirometry Presentation-1Document40 pagesDr. Rowshne Jahan Spirometry Presentation-1Shahadat Hossain BabuNo ratings yet
- Disability Evaluation Under Social Security 3.00 Respiratory Disorders - AdultDocument24 pagesDisability Evaluation Under Social Security 3.00 Respiratory Disorders - Adultsfinx100007696No ratings yet
- Why We Investigate Asthma PatientsDocument5 pagesWhy We Investigate Asthma PatientsustaztNo ratings yet
- Bronchial Asthma: Causes, Symptoms and TreatmentDocument21 pagesBronchial Asthma: Causes, Symptoms and TreatmentshaitabliganNo ratings yet
- Endoscopic Diagnosis of ChestDocument2 pagesEndoscopic Diagnosis of ChestSumith GNo ratings yet
- 2.3 علاج تنفسى د كريم (1) -٣Document11 pages2.3 علاج تنفسى د كريم (1) -٣Ahmed KadiraNo ratings yet
- GINA 2014 ShortcutDocument44 pagesGINA 2014 ShortcutKath Dellosa100% (1)
- SpirometerDocument9 pagesSpirometerMariam AladinNo ratings yet
- Top 10 Care Essentials in Ventilated PtsDocument3 pagesTop 10 Care Essentials in Ventilated PtsAdel HamadaNo ratings yet
- Aspiration Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAspiration Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Respiratory Therapy: 66 Test Questions Student Respiratory Therapists Get Wrong Every Time: (Volume 1 of 2): Now You Don't Have Too!: Respiratory Therapy Board Exam Preparation, #1From EverandRespiratory Therapy: 66 Test Questions Student Respiratory Therapists Get Wrong Every Time: (Volume 1 of 2): Now You Don't Have Too!: Respiratory Therapy Board Exam Preparation, #1No ratings yet
- CHAPTER VII (Rizal's First Homecoming)Document15 pagesCHAPTER VII (Rizal's First Homecoming)hoohooNo ratings yet
- Noli Me Tangere: Photo by José Rizal / Public DomainDocument81 pagesNoli Me Tangere: Photo by José Rizal / Public DomainhoohooNo ratings yet
- Unit VII: Nurse Informaticist RoleDocument41 pagesUnit VII: Nurse Informaticist RolehoohooNo ratings yet
- CHAPTER VII (Rizal's First Homecoming)Document15 pagesCHAPTER VII (Rizal's First Homecoming)hoohooNo ratings yet
- UNIT IX - Application of Nursing Informatics (Clinical)Document201 pagesUNIT IX - Application of Nursing Informatics (Clinical)hoohooNo ratings yet
- Noli Me Tangere: Photo by José Rizal / Public DomainDocument81 pagesNoli Me Tangere: Photo by José Rizal / Public DomainhoohooNo ratings yet
- UNIT IX - Application of Nursing Informatics (Clinical)Document201 pagesUNIT IX - Application of Nursing Informatics (Clinical)hoohooNo ratings yet
- Unit VII: Nursing Informatics LeadershipDocument38 pagesUnit VII: Nursing Informatics LeadershiphoohooNo ratings yet
- 05-06-Science, Technology and Nation Building FINDocument46 pages05-06-Science, Technology and Nation Building FINhoohooNo ratings yet
- Rizal's Second Journey AbroadDocument13 pagesRizal's Second Journey AbroadhoohooNo ratings yet
- Standard of Nursing InformaticsDocument36 pagesStandard of Nursing InformaticsRaquel Monsalve100% (1)
- CHAPTER VIII-RizalDocument26 pagesCHAPTER VIII-RizalhoohooNo ratings yet
- NSTP 2 ActivityDocument7 pagesNSTP 2 ActivityhoohooNo ratings yet
- Problems With Passenger and PowerDocument6 pagesProblems With Passenger and PowerhoohooNo ratings yet
- PROMDocument16 pagesPROMhoohooNo ratings yet
- Postpartum ComplicationsDocument16 pagesPostpartum Complicationshoohoo100% (1)
- NGT Feeding NeonateDocument58 pagesNGT Feeding NeonatehoohooNo ratings yet
- Arterial Blood Gas Analysis - Lp5.pediaDocument48 pagesArterial Blood Gas Analysis - Lp5.pediahoohooNo ratings yet
- SHOULDER-DYSTOCIA EditedDocument17 pagesSHOULDER-DYSTOCIA Editedhoohoo100% (1)
- Chapter Ix-RizalDocument9 pagesChapter Ix-RizalhoohooNo ratings yet
- Netiquette Rules and Guidelines: By: Ariel AbenojaDocument13 pagesNetiquette Rules and Guidelines: By: Ariel AbenojaRaquel MonsalveNo ratings yet
- Asthma: Prepared By: Rose Marie B. Lagasca, MANDocument39 pagesAsthma: Prepared By: Rose Marie B. Lagasca, MANhoohooNo ratings yet
- Spirometry Pulmonary Function TestDocument17 pagesSpirometry Pulmonary Function TesthoohooNo ratings yet
- PROMDocument16 pagesPROMhoohooNo ratings yet
- SHOULDER-DYSTOCIA EditedDocument17 pagesSHOULDER-DYSTOCIA Editedhoohoo100% (1)
- NGT Feeding NeonateDocument58 pagesNGT Feeding NeonatehoohooNo ratings yet
- Neb Ul IzationDocument15 pagesNeb Ul IzationhoohooNo ratings yet
- Neb Ul IzationDocument15 pagesNeb Ul IzationhoohooNo ratings yet
- Netiquette Rules and Guidelines: By: Ariel AbenojaDocument13 pagesNetiquette Rules and Guidelines: By: Ariel AbenojaRaquel MonsalveNo ratings yet
- Drug StudyDocument186 pagesDrug StudyTheresa Sombilla FacunlaNo ratings yet
- Bronchial Asthma in Children FdneDocument36 pagesBronchial Asthma in Children FdneRonit ChandNo ratings yet
- Human Respiratory System ModelDocument35 pagesHuman Respiratory System ModelCheryl LowNo ratings yet
- Anatomy and Function of the Normal Lung (39Document3 pagesAnatomy and Function of the Normal Lung (39Mangesh KetkarNo ratings yet
- Drug Study FormatDocument8 pagesDrug Study FormatKenrick BajaoNo ratings yet
- Bronchial AsthmaDocument84 pagesBronchial AsthmaNavnik NaithikNo ratings yet
- Multichannel Lung Sound Analysis For Asthma Detection PDFDocument13 pagesMultichannel Lung Sound Analysis For Asthma Detection PDFskwijayaNo ratings yet
- DESIGN OF A BREATHING SIMULATOR GENERATING ADULT AND PEDIATRIC PATTERNS MSC Thesis PDFDocument81 pagesDESIGN OF A BREATHING SIMULATOR GENERATING ADULT AND PEDIATRIC PATTERNS MSC Thesis PDFyekta8No ratings yet
- Position Your Respirator Correctly and Check The Seal To Protect Yourself From COVID-19Document1 pagePosition Your Respirator Correctly and Check The Seal To Protect Yourself From COVID-19rmruivoNo ratings yet
- Science 9: I. Directions: Multiple Choice. Read The Questions Carefully. Choose and Write The Correct Letter On YourDocument2 pagesScience 9: I. Directions: Multiple Choice. Read The Questions Carefully. Choose and Write The Correct Letter On YourJunar Alarcon100% (1)
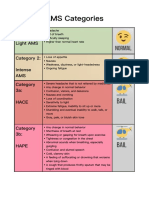
- AMS Symptoms and CategoriesDocument1 pageAMS Symptoms and CategoriesyyggvcNo ratings yet
- SAM's Drugs GuideDocument499 pagesSAM's Drugs Guideصباح عباس الساعديNo ratings yet
- Activity 1.1 Journey of A Breath of AirDocument4 pagesActivity 1.1 Journey of A Breath of AirJorjette Kate BatuNo ratings yet
- Single PDF JuneDocument6 pagesSingle PDF JuneNirav TrivediNo ratings yet
- Suma Eden D4.5 Antimicrobial Fruit and Vegetable Wash: Safety Data SheetDocument5 pagesSuma Eden D4.5 Antimicrobial Fruit and Vegetable Wash: Safety Data SheetekiyasekiNo ratings yet
- Clinical Pathway For Bronchial Asthma atDocument3 pagesClinical Pathway For Bronchial Asthma atwenda sariNo ratings yet
- Drugs Affecting The Body SystemDocument3 pagesDrugs Affecting The Body SystemKhzNo ratings yet
- Ards Concept MapDocument1 pageArds Concept Mapchristine louise bernardoNo ratings yet
- Kinesitherapy and Ultrasound in Children With Bronchial AsthmaDocument5 pagesKinesitherapy and Ultrasound in Children With Bronchial AsthmaIJAR JOURNALNo ratings yet
- CDEM 18january WebDocument24 pagesCDEM 18january WebRicardo Jonathan Ayala GarciaNo ratings yet
- Science: Mahay Integrated Secondary SchoolDocument10 pagesScience: Mahay Integrated Secondary Schoollavenia acdalNo ratings yet
- Anaphylaxis: Watch For Any One of The Following Signs of AnaphylaxisDocument1 pageAnaphylaxis: Watch For Any One of The Following Signs of AnaphylaxisBrîndușa PetruțescuNo ratings yet
- Chai xịt côn trùng Raid.PMI854Document8 pagesChai xịt côn trùng Raid.PMI854nhật minh nguyễnNo ratings yet
- Microcosmic Orbit Meditation for Reproductive HealthDocument1 pageMicrocosmic Orbit Meditation for Reproductive HealthSaimon S.M.No ratings yet
- Asma 1Document14 pagesAsma 1Dwi Yuli YantiNo ratings yet
- AEBA QUESTIONS-WPS OfficeDocument2 pagesAEBA QUESTIONS-WPS OfficeMarj Castor LisondraNo ratings yet
- Pneumonia: (Related To Copious Tracheobronchial Secretions.)Document1 pagePneumonia: (Related To Copious Tracheobronchial Secretions.)Alyssa Mae DumularNo ratings yet
- Asthma Control Test (ACT)Document5 pagesAsthma Control Test (ACT)Mutiara SundasariNo ratings yet