Professional Documents
Culture Documents
Chapter - 12
Chapter - 12
Uploaded by
eat spongeCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter - 12
Chapter - 12
Uploaded by
eat spongeCopyright:
Available Formats
Pharmacology for Canadian Pharmacy
Technicians
First Canadian Edition
Chapter 12
Drugs for Seizures
Copyright © 2017 Pearson Canada Inc. 12 - 1
Learning Outcomes (1 of 2)
LO1: Compare and contrast the terms epilepsy, seizures, and
convulsions.
LO2: Recognize the possible causes of seizures.
LO3: Relate the signs and symptoms of specific types of
seizures.
LO4: Describe the pharmacological management of acute
seizures and epilepsy.
Learning Outcomes (2 of 2)
LO5: Explain the importance of patient drug compliance in
the pharmacotherapy of epilepsy and seizures.
LO6: For each of the drug classes, know representative drug
examples and explain their mechanisms of drug action,
primary actions, and important adverse effects.
LO7: Categorize the drugs used in the treatment of seizures
on the basis of their classifications and mechanisms of
action.
Core Concept 12.1
All convulsions are seizures, but not all seizures are convulsions.
Seizure
• A disturbance of electrical activity in the brain
• Caused by abnormal neuronal discharges
Seizure and Convulsion
• Not synonymous
• Convulsions
• Involuntary, violent spasms of the large skeletal muscles of the face, neck,
arms, and legs
• Some seizures involve convulsions, others do not
Core Concept 12.2
Many causes of seizure activity are known; a few are not.
Causes of Seizure Activity (1 of 2)
A symptom of an underlying disorder
• Infectious diseases
• meningitis, encephalitis
• Trauma
• physical or chemical trauma
• Metabolic disorders
• hypoglycemia, hyponatremia, water intoxication
Causes of Seizure Activity (2 of 2)
• Vascular diseases
• Respiratory hypoxia
• Carbon monoxide poisoning
• Cerebral vascular accidents
• Shock, Cardiac dysrhythmias
• Pediatric disorders
• Febrile seizure
• Neoplastic disease
Core Concept 12.3
Epileptic seizures are typically identified as partial, generalized, or
special epileptic syndromes.
Types of Seizures (1 of 3)
Partial (focal) seizures
• Limited portion of the brain
• Simple partial seizures
• Small, limited focus
• Complex partial seizures
• Involve sensory, motor, or autonomic symptoms
• Some degree of altered or impaired consciousness
• Can be proceeded by an aura
Types of Seizures (2 of 3)
Generalized seizures
• Entire brain on both sides
• Absence seizures
• Last for few seconds only, staring common sign
• Atonic seizures
• episodes are very short
• stumbling and falling for no apparent reason.
Types of Seizures (3 of 3)
Tonic-clonic seizures (grand mal seizures)
• Most common type of seizure
• Intense muscle contractions indicate the tonic phase
and apnea
• The clonic phase is characterized by alternating
contraction and relaxation of muscles
• The seizure usually lasts 1 to 2 minutes, after which
the patient becomes drowsy, disoriented, and sleeps
deeply
Special Epileptic Syndromes (1 of 3)
Febrile seizures
• Tonic-clonic motor activity lasting for 1 to 2 minutes
• Rapid return of consciousness
• Caused by rapid rise in body temperature
• 3-month to 5-year age group
Special Epileptic Syndromes (2 of 3)
Status epilepticus
• Medical emergency
• Repeated occurrence of a seizure
• Hypoxia may develop
• Hypoglycemia, acidosis, and hypothermia
• Can cause brain damage and ultimately death
Special Epileptic Syndromes (3 of 3)
Management of status epilepticus
• Treatment involves the IV administration of antiseizure medications
• During seizure activity, steps must be taken to make sure to maintain
airway
Core Concept 12.4
Effective seizure management involves strict adherence to drug therapy.
Antiseizure Pharmacology
• Dependent on patient presentation, medical history, and associated
pathologies
• Effective therapy usually obtained with one drug
• Seizures can occur due to drug cessation, discontinuation should
occur over many weeks
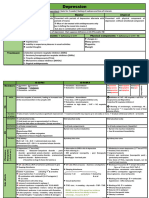
Table 12.1 Suggested Drugs for the Management of Specific
Types of Seizures
Blank Blank Generalized Seizures Blank Special
Partial
Blank Seizures Absence Tonic–clonic Myoclonic
Drugs That Potentiate GABA Blank Blank Blank Blank
clobazam (Frisium) ✓ ✓ ✓ ✓
gabapentin (Neurontin) ✓ Blank Blank Blank
phenobarbital (Luminal) ✓ Blank Blank Blank
primidone (Mysoline) ✓ Blank ✓ Blank
topiramate (Topamax) ✓ ✓ ✓ ✓
Copyright © 2017 Pearson Canada Inc. 12 - 19
[Table 12.1 Continued]
Blank Blank Generalized Seizures Blank Special
Partial
Blank Seizures Absence Tonic–clonic Myoclonic
Hydantoin and Related Drugs Blank Blank Blank Blank
carbamazepine (Tegretol) ✓ Blank ✓ Blank
lamotrigine (Lamictal) ✓ ✓ ✓ ✓
levetiracetam (Keppra) ✓ ✓ ✓ ✓
oxcarbazepine (Trileptal) ✓ Blank Blank Blank
phenytoin (Dilantin) ✓ Blank ✓ Blank
valproic acid (Depakene) ✓ ✓ ✓ ✓
Succinimides Blank Blank Blank Blank
ethosuximide (Zarontin) Blank ✓ Blank Blank
Adapted from Gray, J. (2014). Therapeutic Choices. Ottawa, ON: Canadian Pharmacists Association. Copyright Canadian
Pharmacists Association, www.etherapeutics.ca.
Copyright © 2017 Pearson Canada Inc. 12 - 20
Core Concept 12.5
Antiseizure pharmacotherapy is directed at controlling the movement of
electrolytes across neuronal membranes or affecting neurotransmitter
balance.
Goal and Action
• Suppress neuronal activity just enough to prevent abnormal or
repetitive firing
• Three general mechanisms by which antiseizure drugs work:
• Stimulating an influx of chloride ions, neurotransmitter gamma-aminobutyric
acid (GABA)
• Delaying an influx of sodium ions
• Delaying an influx of calcium ions
Core Concept 12.6
By increasing the effects of gamma-aminobutyric acid (GABA) in the
brain, drugs reduce a wide range of seizure types.
GABA (1 of 2)
• Primary inhibitory neurotransmitter
• Suppress the firing of neurons
• Barbiturates, benzodiazepens, and some others reduce seizure
activity by augmenting the action of GABA
• GABA related drugs usually used in conjunction with other medication
GABA (2 of 2)
Core Concept 12.7
Hydantoin and related drugs are effective in treating partial seizures and
tonic–clonic seizures.
Hydantoins
• Dampen CNS activity
• Delay the influx of sodium ions across neuronal
membranes
• Sodium channels are not blocked, just made to be less
sensitive to decrease the likelihood for an action
potential
• Drugs in this group may also affect the threshold of
neuronal firing:
• They may interfere with transduction of the excitatory
neurotransmitter glutamate.
First-Line Drugs (1 of 2)
• Dilantin (phenytoin)
• The oldest and most commonly prescribed antiseizure
medication
• First-line drugs in the treatment of status epilepticus
• Phenytoin-related drugs have a mechanism similar to
that of the hydantoins
First-Line Drugs (2 of 2)
• Examples:
• Carbamazepine (Tegretol), oxcarbazepine (Trileptal), and
valproic acid (Depakene, Depakote), and Lamotrigine
Core Concept 12.8
Succinimides are used to treat absence seizures.
Succinimides
• Affect calcium influx at neurotransmitters, hormones,
and membranes
• Calcium is fundamental in neuronal transmission
• Delay influx thereby increasing the electrical
threshold and reducing the probability of an action
potential
• Example: Zarontin (ethosuximide)
Table 12.2 Key Drugs to Treat Seizures
Classification Generic Name Original Brand Name
Barbiturate phenobarbital Phenobarb
Blank primidone Myosoline
Benzodiazepine clobazam Frisium
Gamma-aminobutyric acid (GABA) gabapentin Neurontin
derivative
Hydantoin-like carbamazepine Tegretol, Tegretol CR
Blank divalproex Epival
Blank oxcarbazepine Trileptal
Blank valproic acid Depakene
Hydantoin phenytoin Dilantin
Miscellaneous type lamotrigine Lamictal
Blank levetiracetam Keppra
Blank topiramate Topamax
Succinimide ethosuximide Zarontin
Copyright © 2017 Pearson Canada Inc. 12 - 32
Summary
• Seizures are uncontrolled neuronal brain discharges,
whose reasons are not all known
• Seizures categorized as partial, generalized, or special
epileptic syndromes
• Seizure management involves pharmacotherapy to
control the movement of electrolytes thereby
increasing the electrical threshold
• Mechanisms involve, chloride ions (GABA),
desensitization to sodium channels, and blocking of
calcium channels
You might also like
- Seizure & Epilepsy PDFDocument11 pagesSeizure & Epilepsy PDFbencleese100% (1)
- Anti ConvulsantDocument42 pagesAnti ConvulsantAkmal SafwanNo ratings yet
- CNSDocument102 pagesCNSNoriko MatsumotoNo ratings yet
- Systemic PharmacologyDocument37 pagesSystemic PharmacologyMoNiruzzaman MoNirNo ratings yet
- Farmakologi Dari Obat EpilepsiDocument82 pagesFarmakologi Dari Obat EpilepsiDion SaputraNo ratings yet
- Anticonvulsants 2Document1 pageAnticonvulsants 2Taif Salim100% (1)
- Sedative HypnoticDocument60 pagesSedative HypnoticNeeraj KumarNo ratings yet
- Drug StudyDocument4 pagesDrug StudyDean Angelo BarrientosNo ratings yet
- Extra Pyramidal Symptoms AdvanceDocument5 pagesExtra Pyramidal Symptoms AdvanceMr. Psycho Sam100% (2)
- CNS DrugsDocument57 pagesCNS DrugsHussein Al-jmrawiNo ratings yet
- Pharmacology and Venipuncture (Prelim)Document14 pagesPharmacology and Venipuncture (Prelim)Shan Angelie SarmientoNo ratings yet
- Common Drugs in MI DepartmentDocument43 pagesCommon Drugs in MI DepartmentNur IzzaidahNo ratings yet
- Pharmacology of Drugs Used in Movement Disorders: Christian WaeberDocument34 pagesPharmacology of Drugs Used in Movement Disorders: Christian WaeberciaranNo ratings yet
- Farmacologia Das Drogas Ansiolà TicasDocument65 pagesFarmacologia Das Drogas Ansiolà TicasEduarda StumpfNo ratings yet
- Conventional Antiepileptic Drugs: Presented by Dr. Mehnaz MahmoodaDocument41 pagesConventional Antiepileptic Drugs: Presented by Dr. Mehnaz MahmoodaMehediNo ratings yet
- Neurology - TremorDocument1 pageNeurology - TremorvaleriaNo ratings yet
- Untitlednf Fli DJ Ig Tu JDocument30 pagesUntitlednf Fli DJ Ig Tu JBEST OF BESTNo ratings yet
- AntihistaminesDocument36 pagesAntihistaminesAli ElattarNo ratings yet
- Anti-Epileptic DrugsDocument7 pagesAnti-Epileptic DrugsSampada ghodkiNo ratings yet
- Chapter - 5 Ph. Chemistry Drug Acting On CNSDocument40 pagesChapter - 5 Ph. Chemistry Drug Acting On CNSArpan DhungelNo ratings yet
- Anti Psychotic CNS EacDocument33 pagesAnti Psychotic CNS EacPavan chowdaryNo ratings yet
- ParkinsonDocument30 pagesParkinsonRebecca HarsNo ratings yet
- Lecture 11 Sedative-Hypnotic and Anti-Anxiety AgentsDocument32 pagesLecture 11 Sedative-Hypnotic and Anti-Anxiety AgentsHafsa ShakilNo ratings yet
- Antiepileptic DrugsDocument63 pagesAntiepileptic Drugsvpd100% (1)
- Anxiolytic DrugsDocument60 pagesAnxiolytic Drugsneleh grayNo ratings yet
- Antipsychotic Agents and Their Use in SchizophreniaDocument24 pagesAntipsychotic Agents and Their Use in SchizophreniaJV CustodioNo ratings yet
- Geriatri at GlanceDocument29 pagesGeriatri at GlanceHarli RaivonNo ratings yet
- Pharmacodynamics How Drugs WorkDocument21 pagesPharmacodynamics How Drugs WorkWen SilverNo ratings yet
- CNS PNS DrugsDocument29 pagesCNS PNS DrugsMadel A. AlberioNo ratings yet
- Benzodiazepines Rational UseDocument25 pagesBenzodiazepines Rational UseMila PetrovicNo ratings yet
- SeizuresDocument3 pagesSeizuresShairaNo ratings yet
- CAE #11 - PsychiatryDocument51 pagesCAE #11 - PsychiatryMariam ShenoudaNo ratings yet
- Epilepsy Is Due To Sudden, Excessive Depolarization Of: Some or All Cerebral NeuronsDocument19 pagesEpilepsy Is Due To Sudden, Excessive Depolarization Of: Some or All Cerebral NeuronsMourian AmanNo ratings yet
- Drugs For Anxiety and InsomniaDocument10 pagesDrugs For Anxiety and InsomniaApple MaeNo ratings yet
- Drugs That Act On The CNSDocument27 pagesDrugs That Act On The CNSnur rachmad afandiNo ratings yet
- SchizopDocument43 pagesSchizopapi-548578435No ratings yet
- Psycho Pharmacology - FinalDocument145 pagesPsycho Pharmacology - FinalKane CruzNo ratings yet
- Epileptic Drugs by DR DinaDocument39 pagesEpileptic Drugs by DR DinaseraNo ratings yet
- MEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionDocument1 pageMEDICAL SURGICAL NURSING ASSESSMENT AND MANAGEMENT OF CLINICAL PROBLEMS 9th EditionMeryPinkihanNo ratings yet
- Antiseizures DrugsDocument27 pagesAntiseizures DrugsIrene Zae MwandotoNo ratings yet
- An Xy Olitics HypnoticsDocument59 pagesAn Xy Olitics Hypnoticsneleh grayNo ratings yet
- Antiepileptic Drug: Presented by Prerna Surana Yukta Mehta Sarfa MalickDocument65 pagesAntiepileptic Drug: Presented by Prerna Surana Yukta Mehta Sarfa Malick33 Momin SarahNo ratings yet
- The Hitchhiker's Guide To Clinical Pharmacology: Pharmacodynamics: How Drugs WorkDocument23 pagesThe Hitchhiker's Guide To Clinical Pharmacology: Pharmacodynamics: How Drugs WorkMylz MendozaNo ratings yet
- Bimbel Ukmppd FarmakoDocument92 pagesBimbel Ukmppd FarmakoJavier AntaresNo ratings yet
- 1 - PharmacologyDocument18 pages1 - PharmacologyLuidgi MichelNo ratings yet
- Pharmacology: Drugs That Affect The: Nervous SystemDocument84 pagesPharmacology: Drugs That Affect The: Nervous SystemSameh Saber100% (1)
- Lecture Material - Sedative-Hypnotic DrugsDocument13 pagesLecture Material - Sedative-Hypnotic DrugsДилара КилшибаеваNo ratings yet
- Antiepileptic Drugs (Aed) : R. Anita. IndriyantiDocument36 pagesAntiepileptic Drugs (Aed) : R. Anita. Indriyantiandisti2323No ratings yet
- Therapeutic Reviews: Antipsychotics AHFS 28:16.08.04Document10 pagesTherapeutic Reviews: Antipsychotics AHFS 28:16.08.04Milton Kaspo Sagoya IIINo ratings yet
- Anti Seizure Drugs 07Document27 pagesAnti Seizure Drugs 07ashokvishnoi29pNo ratings yet
- LECT-5B - Patient Case and MISCDocument31 pagesLECT-5B - Patient Case and MISCnonaNo ratings yet
- PsychopharmacologyDocument59 pagesPsychopharmacologyrushnaNo ratings yet
- Bipolar Disorder SlidesDocument61 pagesBipolar Disorder Slidesapi-663471551No ratings yet
- Risperidone: Generic Name: ClassificationsDocument9 pagesRisperidone: Generic Name: ClassificationsColeen Mae CamaristaNo ratings yet
- Cmpi MidtermDocument185 pagesCmpi MidtermAubrey MadelaineNo ratings yet
- Antipsychotics: Mary A. Wittler and Eric J. LavonasDocument5 pagesAntipsychotics: Mary A. Wittler and Eric J. LavonasSNo ratings yet
- PSYCHIATRIcsDocument11 pagesPSYCHIATRIcssaraNo ratings yet
- By Duy Thai, 1997: Diffuse Out of Nerve Terminal and Act On COMPT in External TissuesDocument5 pagesBy Duy Thai, 1997: Diffuse Out of Nerve Terminal and Act On COMPT in External Tissuesravi2likeNo ratings yet
- AntidepressantsDocument4 pagesAntidepressantsAhmed MansourNo ratings yet
- Kode Diagnosa PRBDocument9 pagesKode Diagnosa PRBpuskesmas sobangNo ratings yet
- Chapter 426 - Seizures and Epilepsy: Susan S. SpencerDocument35 pagesChapter 426 - Seizures and Epilepsy: Susan S. Spencerenriquelima19No ratings yet
- Epilepsy Board Quick Review.2014.2nd Ed - Jerome Engel, JR PDFDocument209 pagesEpilepsy Board Quick Review.2014.2nd Ed - Jerome Engel, JR PDFMeriam OuertaniNo ratings yet
- Epilepsia - 2022 - Hirsch - ILAE Definition of The Idiopathic Generalized Epilepsy Syndromes Position Statement by TheDocument25 pagesEpilepsia - 2022 - Hirsch - ILAE Definition of The Idiopathic Generalized Epilepsy Syndromes Position Statement by TheIngrid RivadeneiraNo ratings yet
- StudentsguidetoEpilepsySecondEdition AcompletepublicDocument46 pagesStudentsguidetoEpilepsySecondEdition AcompletepublicRamo EdumNo ratings yet
- National Epilepsy Consensus Guideline Society of Neurologists of Bangladesh 1Document130 pagesNational Epilepsy Consensus Guideline Society of Neurologists of Bangladesh 1Kutu MiaNo ratings yet
- ILAE Classification of Seizures and Epilepsy - UpToDateDocument13 pagesILAE Classification of Seizures and Epilepsy - UpToDateKrissia SalvadorNo ratings yet
- Epilepsia - 2022 - Wirrell - Methodology For Classification and Definition of Epilepsy Syndromes With List of Syndromes - 1Document16 pagesEpilepsia - 2022 - Wirrell - Methodology For Classification and Definition of Epilepsy Syndromes With List of Syndromes - 1Neurologie PediatricaNo ratings yet
- Typical Absence Seizures and Their Treatment: Current TopicDocument5 pagesTypical Absence Seizures and Their Treatment: Current TopicAndika Eriza PutraNo ratings yet
- International League Against Epilepsy Classification and Definition of Epilepsy Syndromes With Onset in Childhood Position Paper by The ILAE Task Force On Nosology and DefinitionsDocument45 pagesInternational League Against Epilepsy Classification and Definition of Epilepsy Syndromes With Onset in Childhood Position Paper by The ILAE Task Force On Nosology and DefinitionsEduardo Rios DuboisNo ratings yet
- Icd NaDocument41 pagesIcd NaTia NingNo ratings yet
- Epilepsia - 2022 - Specchio - International League Against Epilepsy Classification and Definition of Epilepsy SyndromesDocument45 pagesEpilepsia - 2022 - Specchio - International League Against Epilepsy Classification and Definition of Epilepsy SyndromesIngrid RivadeneiraNo ratings yet
- Kode Diagnosa PRBDocument21 pagesKode Diagnosa PRBRahmat GzNo ratings yet
- Seizures and Epilepsy LectureDocument7 pagesSeizures and Epilepsy LecturekiaraNo ratings yet
- Genetic Epilepsy SyndromesDocument24 pagesGenetic Epilepsy SyndromesAnali Durán CorderoNo ratings yet
- Absence Seizures in Children: QuestionsDocument7 pagesAbsence Seizures in Children: QuestionsAliss OñaNo ratings yet
- Clinical NeurologyDocument288 pagesClinical NeurologyWeronika Tomaszczuk-KłakNo ratings yet
- Handbook of Pediatric Epilepsy: David C. DredgeDocument256 pagesHandbook of Pediatric Epilepsy: David C. DredgeDiana HereldNo ratings yet
- Epilepsy Syndromes in Children - UpToDateDocument26 pagesEpilepsy Syndromes in Children - UpToDatecapt_zoeNo ratings yet
- EpiInChi2eBySheJWal PDFDocument529 pagesEpiInChi2eBySheJWal PDFAryan Singh100% (1)
- Idiopathic Generalised Epilepsies: January 2010Document7 pagesIdiopathic Generalised Epilepsies: January 2010PryslalalaNo ratings yet
- Diagnosa PRBDocument12 pagesDiagnosa PRBSAEHANNo ratings yet
- Epilepsia - 2022 - Riney - International League Against Epilepsy Classification and Definition of Epilepsy Syndromes WithDocument33 pagesEpilepsia - 2022 - Riney - International League Against Epilepsy Classification and Definition of Epilepsy Syndromes WithEccololiNo ratings yet
- Wa0008.Document8 pagesWa0008.Dany MorBenNo ratings yet
- Treatment in Epileptic Encephalopathy With ESES and Landau-Kleffner SyndromeDocument6 pagesTreatment in Epileptic Encephalopathy With ESES and Landau-Kleffner SyndromeDaniela TapiaNo ratings yet
- Neuropsychiatry - EpilepsyDocument139 pagesNeuropsychiatry - EpilepsySangkaran KumarNo ratings yet
- Childhood Epilepsy: An Update On Diagnosis and Management: January 2015Document18 pagesChildhood Epilepsy: An Update On Diagnosis and Management: January 2015Berto PengNo ratings yet
- Book Matter - AtlasOf EpilepsiesDocument55 pagesBook Matter - AtlasOf EpilepsiesDhamara AdhityaNo ratings yet
- Absans, MiklonikDocument11 pagesAbsans, MiklonikrendyNo ratings yet