Professional Documents
Culture Documents
Immunomodulator Drugs2
Uploaded by
Ankita Tathe0 ratings0% found this document useful (0 votes)
11 views23 pagesOriginal Title
Immunomodulator Drugs2 - Copy
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views23 pagesImmunomodulator Drugs2
Uploaded by
Ankita TatheCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 23
Immunomodulator Drugs
Introduction
• Immunopharmacology
The study of the use of pharmacological
agents as modulators of immune response
• The principal applications:
–Immunosuppressive agents
Compounds that suppress undesirable immune
responses
–Immunostimulating agents
Drugs/microorganism/biological products that
enhance/augment immune responses
Introduction (con’t…)
• 3 major indication for immunotherapy:
– Auto immune diseases
– Primary immunodefficiency
– Organ transplantation
Table some auto immune disorders treated
with immunosuppressive therapy
Autoimmune hemolytic anemia
Myasthenia gravis
Cranial arteritis
Idiopathic thrombocytopenic purpura
Membranous glomerulonephritis
Polymyalgia rheumatica
Polymyositis
Psoriatic arthropathies
Rheumatoid arthritis
Systemic lupus erythematosus
Ulcerative colitis
Uveitis
Wegener’s granulomatosis
General Principles Of
Immunosuppresive Therapy
• Primary immune responses are more
readily inhibited than are secondary
responses
– The primary phase of the immune response
(processing, proliferation, differentiation)
more sensitive to drug action
– Unsensitized person show much less effect
General Principles (con’t…)
• Not all immune responses are equally
affected by immunosuppresive drugs
– Celullar & humoral immunity may be
affected differentially
– The different classes of immune globulin in a
humoral response may be variably affected
General Principles (con’t…)
• Beneficial effects other than
immunosuppression may result from
therapy with these drugs
– The antiinflammatory properties of certain
drug may be valuable because inflammation
often accompanies the immune response
Individual drugs used
to suppress the imune system
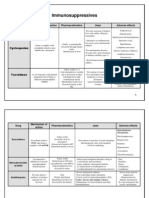
Cyclosporine
• A potent inhibitor of antibody & cell-
mediated immune responses
Immunosuppressant of choice -prevention of
transplant rejection
useful in the treatment of autoimmune
disease -RA, SLE, uveitis, IDD, psoriatik
arthropathies
Cyclosporine (con’t…)
• Mechanism of action
– Bind to cytosolic protein (cytophilin c)
complex inhibit calcineurin phosphatase
activity synthesis & release of several
cytokines
– Impairs the proliferative response of T-Cells to
antigens
– High specific to T-Cells
Cyclosporine (con’t…)
• Pharmacokinetic:
– oral absorption slowly & incompletely
– Tmax = 3 – 4 hours; t½ = 10 – 27 hours
– Metabolized by liver & excreted via bile feces
• Adverse effect:
– nephrotoxicity 75% (severe tubular necrosis
chronic interstitial nephropathy)
– Hypertension 25%
– Hypertension, hyperlipidemia
– Transient liver dysfunction
– hirsutism
Corticosteroid
• Used alone or in combinatioin with other agents in the
treatment of autoimmune disorders and for the
prevention of allograft rejection
• Although posses immunosuppressive properties, their
real value is in controlling the inflammation that can
accompany transplantation and autoimmune disorders
• All phases of the inflammatory process are affected by
these drugs
• Corticosteroid therapy alone is successful in only limited
number of autoimmune diseases, such as idiopathic
thrombocytopenia, hemolytic anemia & polymyalgia
rheumatica
Tacrolimus
• A second generation immunosuppresive agent
that has been approved for use in liver
transplantation
• 10 – 100 times more potent than cyclosporine
• A macrolide antibiotic that selectively inhibits
transcription of a specific set of lymphokine
genes in T-lymphocytes (IL-2, IL-4, IF- & bind
to cytoplasmic proteins (=cytophilins) in
lymphocyte, which are important
– For intracellular folding of proteins
– In regulating gene expression
Tacrolimus (con’t…)
• Absorption from GI is variable, extensively
metabolized in liver & excreted in urine
• The principal side effect is nephrotoxicity
Sirolimus
• Structurally related to tacrolimus
• It is approved for use as an adjunctive agent in
combination with cyclosporine for prevention of
acute renal allograft rejection
• It blocks IL-2 dependent T-cell proliferation by
inhibiting a cytoplasma serine-threonine kinase
• MOA is different from tacrolimus & cyclosporine
can immunosuppresive effect of these
drugs
Azathioprine
• a derivate of 6-mercaptopurine
• very effective as an immunosuppresive
agent and replicating cell is a target for
this action
• Mechanism of action
– Inhibit DNA synthesis & therefore suppreses
lymphocyte proliferation
Inhibits both humoral & cell-
mediated immune reponses
Azathioprine (con’t…)
• Pharmacokinetic
– Well absorbed following oral administration
– Tmax = 1 – 2 hours; t½ 5 hours
– Extensively metabolized to 6-MP and then
converted (liver, erythrocytes) to a variety of
metabolites including 6-thiouric acid
– Metabolites are excreted in the urine
Azathioprine (con’t…)
• Clinical uses :
– Related to direct immunosuppresive action &
antiinflammatory properties
– Combination with corticosteroid to inhibit
rejection of organ tranplants (kidney, liver)
– Reserved for patients who do not response to
cyclosporine + corticosteroids alone
– Autoimmune disorders mostly RA
– Wegener’s granulomatosis
Azathioprine (con’t…)
• Adverse effects
– BM suppression (leukopenia, thrombocytopenia,
both)
– GI toxicity, mild hepatotoxic
– Serious infections (due to immunosuppressive
action)
– Mutagenic & carcinogenic
Mycophenolate Mofetil
• By effectively inhibiting de novo purine
synthesis it can impair the proliferation of both
T & B-lymphocytes
• Combination with cyclosporine + corticosteroids
in the prevention of organ rejection in patient
renal & cardiac transplants
• Almost completely absorbed from GI,
metabolized (liver) to mycophenolic acid
(active), then to inactive glucuronide
• GI side effect are most common
Other cytotoxic drugs
• Cyclophosphamid (cycle specific agent)
• Methotrexate (phase specific agent)
• Chlorambucil (alkylating agent)
Antibodies
• Antiserum can used against lymphocytes
or thymocytes
• Can suppres cellular & often humoral
immunity against a variety of tissue graft
system
• Responses are variable
Antibodies (con’t…)
• Examples:
– Antithymocyte globulin
Has been used successfully alone/combination
with azathioprine + corticosteroids
– Muromonab (CD3)
For preventing rejection in kidney, liver, cardiac
and BM transplantation
– RHO(D) immunoglobulin
Human IgG that contains a high titer of antibodies
againts the Rh(D) red cell antigen
You might also like
- Handbook of Drug Interaction and the Mechanism of InteractionFrom EverandHandbook of Drug Interaction and the Mechanism of InteractionRating: 1 out of 5 stars1/5 (1)
- S-Immunomodulator DrugsDocument48 pagesS-Immunomodulator DrugsFaishal100% (2)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Immunomodulator: Dr. Hj. Rika Yuliwulandari, PHDDocument55 pagesImmunomodulator: Dr. Hj. Rika Yuliwulandari, PHDAnonymous 3ktnNjNo ratings yet
- Immunosuppressive PharmacologyDocument54 pagesImmunosuppressive PharmacologyCARSON 539No ratings yet
- Immuno Modulator SDocument62 pagesImmuno Modulator SAntony Prakash RajNo ratings yet
- ImmunopharmacologyDocument19 pagesImmunopharmacologyMaaz Uddin Siddiqui100% (1)
- Immunosuppressants: Pharmacology TeamDocument26 pagesImmunosuppressants: Pharmacology TeamZaina MasriNo ratings yet
- Immunosuppressant DrugsDocument28 pagesImmunosuppressant DrugsimnasNo ratings yet
- Immuno Far Mako Log IDocument12 pagesImmuno Far Mako Log IMia RahmawatiNo ratings yet
- S 25 Staud ImmunomodulatorsDocument41 pagesS 25 Staud ImmunomodulatorsCarlo MaxiaNo ratings yet
- Immunosuppressants Prof. Alhaider, 1431 HDocument45 pagesImmunosuppressants Prof. Alhaider, 1431 HMourian AmanNo ratings yet
- Immunopharmacology ImmunosupressantsDocument15 pagesImmunopharmacology ImmunosupressantsPraज्ञा GharpankarNo ratings yet
- Immunomodulator 2014Document56 pagesImmunomodulator 2014LeilybadryaNo ratings yet
- Immunotherapy: Prof Anura WeerasingheDocument17 pagesImmunotherapy: Prof Anura WeerasingherikarzNo ratings yet
- Immunosuppresantmbbs 190608061036Document115 pagesImmunosuppresantmbbs 190608061036syarintaadeninaNo ratings yet
- IMMUNOMODULATORSDocument44 pagesIMMUNOMODULATORSMaria khurshidNo ratings yet
- Immunosuppressants NotesDocument20 pagesImmunosuppressants NotesmadcalNo ratings yet
- Immunomodulators: Ma. Stephanie Fay S. Cagayan, MDDocument67 pagesImmunomodulators: Ma. Stephanie Fay S. Cagayan, MDFaye Cagayan100% (1)
- Drug TransplantationDocument36 pagesDrug Transplantationsajad abasewNo ratings yet
- Immunomodulators: - Nirali Thakkar (From SMT S.M.Shah Pharmacy College)Document23 pagesImmunomodulators: - Nirali Thakkar (From SMT S.M.Shah Pharmacy College)Suvojit BasakNo ratings yet
- IMmuno-modulating AgentsDocument26 pagesIMmuno-modulating AgentsRida fatimaNo ratings yet
- Powerpoint For Marking PharmacologyDocument25 pagesPowerpoint For Marking PharmacologyKennedy ShelemaniNo ratings yet
- Rheumatoid ArthritisDocument49 pagesRheumatoid ArthritisDr.U.P.Rathnakar.MD.DIH.PGDHM100% (4)
- NCM 106 Immunosuppresants 1 1Document11 pagesNCM 106 Immunosuppresants 1 1Mariella EspañaNo ratings yet
- Immunomodulators: Dr. Kaushik Mukhopadhyay Assistant Professor, Dept. of Pharmacology Esi-PgimsrDocument31 pagesImmunomodulators: Dr. Kaushik Mukhopadhyay Assistant Professor, Dept. of Pharmacology Esi-PgimsrsyarintaadeninaNo ratings yet
- Drugs For Immune SystemDocument75 pagesDrugs For Immune SystemDhonat FlashNo ratings yet
- Surgery 06 - Transplantation - 27th April 2023Document110 pagesSurgery 06 - Transplantation - 27th April 2023mannkheni209No ratings yet
- Adverse Effects of DrugsDocument62 pagesAdverse Effects of DrugsValentine MandelaNo ratings yet
- ImmunosuppressantsDocument18 pagesImmunosuppressantsomar khanNo ratings yet
- Immunosuppressant DrugsDocument6 pagesImmunosuppressant DrugsShoaib MohiuddinNo ratings yet
- Prof. - Sanjay - Khattri - Anti - Rheumatoid - DrugsDocument29 pagesProf. - Sanjay - Khattri - Anti - Rheumatoid - DrugsBe GameNo ratings yet
- Immuno-Suppressants: Dr. PrasadDocument21 pagesImmuno-Suppressants: Dr. PrasadMuskaan ZaharaNo ratings yet
- 1 ImmunosuppressantDocument10 pages1 Immunosuppressantasifhussainuol850No ratings yet
- 1 - Immuno Tables1Document4 pages1 - Immuno Tables1Urugonda VenumadhavNo ratings yet
- Immunosuppressive AgentsDocument36 pagesImmunosuppressive AgentsFlorensa Teolina NdruruNo ratings yet
- Immune System 14Document61 pagesImmune System 14Лариса ТкачеваNo ratings yet
- FACTS: There Is No Cure & Complete: Sustained Remissions Are Rare. Principles of TherapyDocument12 pagesFACTS: There Is No Cure & Complete: Sustained Remissions Are Rare. Principles of TherapyAzizan HannyNo ratings yet
- IMMUNOMODULATORS (EDocFind - Com)Document67 pagesIMMUNOMODULATORS (EDocFind - Com)sac00772006No ratings yet
- Immuno PharmacologyDocument39 pagesImmuno PharmacologyGd SuarantaNo ratings yet
- Anticancer DrugsDocument117 pagesAnticancer DrugsKishore Chandra Korada100% (2)
- Immunosuppressive Drug TherapyDocument25 pagesImmunosuppressive Drug Therapyapi-3741769100% (2)
- Suatu Substansi Baik Alamiah Maupun Sintetis Yang Dapat Membantu Mengatur Keseimbangan Sistem ImunDocument19 pagesSuatu Substansi Baik Alamiah Maupun Sintetis Yang Dapat Membantu Mengatur Keseimbangan Sistem ImunSefniSilviianaDewiNo ratings yet
- Drugs Treating ArthritisDocument38 pagesDrugs Treating ArthritisDere RawandNo ratings yet
- Antifungal - Anticancer 21Document83 pagesAntifungal - Anticancer 21DR AbidNo ratings yet
- MontelukastDocument37 pagesMontelukastdr.erdogan1074No ratings yet
- The Immunosuppression 2021Document10 pagesThe Immunosuppression 2021Muhammad AliNo ratings yet
- IMMUNOTHERAPYDocument50 pagesIMMUNOTHERAPYPandiya Raja73% (15)
- Antitubercular Drug: Dr. Deepak K GuptaDocument46 pagesAntitubercular Drug: Dr. Deepak K Guptasandeepv08No ratings yet
- Management of Rheumatoid ArthritisDocument48 pagesManagement of Rheumatoid ArthritisAlexNo ratings yet
- TransplantationpptfinalDocument57 pagesTransplantationpptfinalmilka berhaneNo ratings yet
- Hypersensitivity ReactionDocument23 pagesHypersensitivity ReactionJo CanensNo ratings yet
- Principles of Antimicrobial Therapy Part 1Document83 pagesPrinciples of Antimicrobial Therapy Part 1Carl Elexer Cuyugan Ano100% (1)
- Pharmacology IDocument202 pagesPharmacology ISalahadinNo ratings yet
- Burchum & Rosenthal: Lehne's Pharmacology For Nursing Care, 9th EditionDocument2 pagesBurchum & Rosenthal: Lehne's Pharmacology For Nursing Care, 9th Editionhockeyman1584No ratings yet
- ImunofarmakologiDocument63 pagesImunofarmakologiShafiraNo ratings yet
- Антимикробиал чбDocument71 pagesАнтимикробиал чбSangeeta SharmaNo ratings yet
- Pharmacology of Antituberculosis Drugs: DR - Datten Bangun MSC, SPFK Dept - Farmakologi & Terapeutik Fak - Kedokteran UhnDocument45 pagesPharmacology of Antituberculosis Drugs: DR - Datten Bangun MSC, SPFK Dept - Farmakologi & Terapeutik Fak - Kedokteran UhnPutri Rahmi MaharaniNo ratings yet
- Anti InfectivesDocument40 pagesAnti InfectivesIconMaicoNo ratings yet
- ImmunomodulatorsDocument8 pagesImmunomodulatorsfaisalnadeem100% (1)
- Cepheid Xpert MTB RIF Brochure CE IVD 0089 EnglishDocument4 pagesCepheid Xpert MTB RIF Brochure CE IVD 0089 EnglishMontana PrinceNo ratings yet
- Spleen Qi Defficiency SampleDocument33 pagesSpleen Qi Defficiency SampleVivek RaneNo ratings yet
- CAC Basic Guide v1.14 - 28082021Document10 pagesCAC Basic Guide v1.14 - 28082021neomunumu34567No ratings yet
- 1 InfluenzaDocument7 pages1 InfluenzaElena MoldoveanuNo ratings yet
- Oliver Wyman COVID 19 Special PrimerDocument61 pagesOliver Wyman COVID 19 Special PrimerdupaNo ratings yet
- Đề 2Document7 pagesĐề 2Gmod GopnikNo ratings yet
- Stroke ThesisDocument7 pagesStroke Thesisnavysavchenkobellevue100% (1)
- Cardio ReviewDocument25 pagesCardio ReviewHarini PrayagaNo ratings yet
- Drug Study MBDocument29 pagesDrug Study MBk4jggjtnz5No ratings yet
- WP Contentuploads201902yin Yang Qiao Yin Yang Wei Dai Mai PDFDocument240 pagesWP Contentuploads201902yin Yang Qiao Yin Yang Wei Dai Mai PDFAnissa Hamid100% (1)
- Lesson 1 Stages of Infection 2Document20 pagesLesson 1 Stages of Infection 2Delechos JaysonNo ratings yet
- Acute Coronary Syndromes Acute Coronary Syndromes OverviewDocument8 pagesAcute Coronary Syndromes Acute Coronary Syndromes Overviewمحمد زينNo ratings yet
- Peoria County Booking Sheet 09/06/15Document8 pagesPeoria County Booking Sheet 09/06/15Journal Star police documentsNo ratings yet
- First Aid & Bandaging: Maybelle B. Animas, R.N Nurse II-Imus IDocument35 pagesFirst Aid & Bandaging: Maybelle B. Animas, R.N Nurse II-Imus IJoel VelasquezNo ratings yet
- Drug Study #2Document3 pagesDrug Study #2Sarah Kaye BañoNo ratings yet
- Pharmacology For Nursing Care 6e Test BankDocument5 pagesPharmacology For Nursing Care 6e Test BankSharon Spence100% (33)
- General Medicine Past Exam QuestionsDocument61 pagesGeneral Medicine Past Exam Questionsptusha44274No ratings yet
- Look For The Drug-Drug Interaction of The Following Drugs Given and Give Nursing Considerations As You Give The Drugs TogetherDocument2 pagesLook For The Drug-Drug Interaction of The Following Drugs Given and Give Nursing Considerations As You Give The Drugs TogetherLa CartaNo ratings yet
- Ramadan Guide For DiabetesDocument9 pagesRamadan Guide For DiabetesUjwal TickooNo ratings yet
- Intervencion de Psicosis en PeruDocument9 pagesIntervencion de Psicosis en PeruLinda Ailin OchoaNo ratings yet
- Stages of Shock NCLEX ReviewDocument3 pagesStages of Shock NCLEX ReviewCamille SanguyoNo ratings yet
- HimophiliyaDocument20 pagesHimophiliyaDenuwan FernandoNo ratings yet
- Veterinary Microbiology II:: Bovine Ephemeral Fever (BEF)Document22 pagesVeterinary Microbiology II:: Bovine Ephemeral Fever (BEF)Reza Alfitra MutiaraNo ratings yet
- PRUMy Child Plus Flyer 2023 ENGDocument3 pagesPRUMy Child Plus Flyer 2023 ENGridermateNo ratings yet
- Sas 8Document5 pagesSas 8Rodesa MigarNo ratings yet
- Covid 19 and Indigenous ChildrenDocument3 pagesCovid 19 and Indigenous ChildrenJenny Vieb CaspilloNo ratings yet
- PHYSIO 1.06 ECG Interpretation DR - UbinaDocument7 pagesPHYSIO 1.06 ECG Interpretation DR - UbinapachayilstephanoseshintoNo ratings yet
- WHO 5th Edition Classification 2023Document57 pagesWHO 5th Edition Classification 2023mohamaed abbasNo ratings yet
- Polycythemia VeraDocument18 pagesPolycythemia VeraHSC UNITEDNo ratings yet
- TABLE A14 - Physical Exam Labs and Other DataDocument1 pageTABLE A14 - Physical Exam Labs and Other DataDragutin PetrićNo ratings yet