Professional Documents
Culture Documents
Carotid
Uploaded by
Ans FitriOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Carotid
Uploaded by
Ans FitriCopyright:
Available Formats
ORIGINAL ARTICLE
Western Trauma Association Critical Decisions in Trauma: Screening for and Treatment of Blunt Cerebrovascular Injuries
Walter L. Bif, MD, C. Clay Cothren, MD, Ernest E. Moore, MD, Rosemary Kozar, MD, Christine Cocanour, MD, James W. Davis, MD, Robert C. McIntyre, Jr., MD, Michael A. West, MD, PhD, and Frederick A. Moore, MD
Key Words: Blunt trauma, Carotid artery injury, Vertebral artery injury, Carotid dissection, Vertebral dissection, Computed tomographic angiography, Arteriography, Heparin, Antiplatelet therapy, Stroke, Stent, Blunt cerebrovascular injury. (J Trauma. 2009;67: 1150 1153)
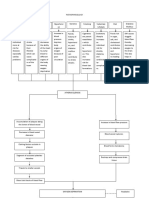
his is a recommended management algorithm from the Western Trauma Association addressing the diagnostic evaluation and management of blunt cerebrovascular injuries (BCVI) in adult patients. Because there are no published prospective randomized clinical trials that have generated class I data, the recommendations herein are based on published observational studies and expert opinion of Western Trauma Association members. The algorithm (Fig. 1) and accompanying comments represent a safe and sensible approach that could be followed at most trauma centers. We recognize that there will be patient, personnel, institutional, and situational factors that may warrant or require deviation from the recommended algorithm. We encourage institutions to use this guideline to formulate their own local protocols.
The algorithm contains letters at decision points; the corresponding paragraphs in the text elaborate on the thought process and cite the pertinent literature. The annotated algorithm is intended to (a) serve as a quick bedside reference for clinicians; (b) foster more detailed patient care protocols that will allow for prospective data collection and analysis to identify best practices; and (c) generate research projects to answer specic questions concerning decision making in the management of adults with BCVI.
HISTORICAL PERSPECTIVE
Blunt carotid injury (BCI) and blunt vertebral injury, collectively known as BCVI, have historically been considered rare, but potentially devastating, events. Early multicenter reviews collectively reported BCI-related mortality rates of 23%, with 48% of survivors suffering permanent severe neurologic sequelae.1 4 In these reviews, the collective incidence of BCI was noted to be 0.1% among blunt trauma victims admitted to trauma centers. In the latter part of the 1990s, with awareness heightened by the landmark series from Memphis,5 the reported incidence of BCI increased to 0.24% 0.4%.57 The Denver group conrmed that many injuries were clinically occult8 and instituted liberal screening of asymptomatic patients in the mid1990s.9 Screening for BCVI has now become widespread, and several centers have reported an incidence of BCVI exceeding 1% of blunt trauma admissions.10 15
Submitted for publication February 17, 2009. Accepted for publication September 17, 2009. Copyright 2009 by Lippincott Williams & Wilkins From the Department of Surgery (W.L.B., C.C.C., E.E.M.), Denver Health Medical Center, Denver, Colorado; Department of Surgery (R.K.), University of Texas Health Science Center at Houston, Houston, Texas; Department of Surgery (C.C.), University of California Davis Sacramento, California; Department of Surgery (J.W.D.), UCSF/Fresno, Fresno, California; Department of Surgery (R.C.M.), University of Colorado Health Sciences Center, Denver, Colorado; Department of Surgery (M.W.), San Francisco General Hospital, San Francisco, California; and Department of Surgery (F.A.M.), The Methodist Hospital, Houston, Texas. The Western Trauma Association (WTA) develops algorithms to provide guidance and recommendations for particular practice areas, but does not establish the standard of care. The WTA develops algorithms based on the evidence available in the literature and the expert opinion of the task force in the recent timeframe of the publication. The WTA considers use of the algorithm to be voluntary. The ultimate determination regarding its application is to be made by the treating physician and health care professionals with full consideration of the individual patients clinical status as well as available institutional resources and is not intended to take the place of health care providers judgment in diagnosing and treating particular patients. Presented at the 39th Annual Scientic Meeting of the Western Trauma Association, February 2228, 2009, Crested Butte, Colorado. Address for reprints: Walter L. Bif, MD, Department of Surgery, MC 0206, 777 Bannock Street, Denver, CO 80204-4507; email: walter.bif@dhha.org. DOI: 10.1097/TA.0b013e3181c1c1d6
ANNOTATED TEXT FOR ALGORITHM
A. Trauma patients with any of the following signs or symptoms should be considered to have BCVI until proven otherwise: arterial hemorrhage from neck, mouth, nose, ears; large or expanding cervical hematoma; cervical bruit in a patient younger than 50 years; focal or lateralizing neurologic decit, including hemiparesis, transient ischemic attack, Horners syndrome, oculosympathetic paresis, or vertebrobasilar insufciency; evidence of cerebral infarction on computed tomography (CT) or magnetic resonance imaging (MRI) scan; or neurologic decit that is incongruous with CT or MRI ndings. Any of these ndings should prompt emergent diagnostic evaluation and interventions directed at hemorrhage control or stroke management. B. Although it has been suggested that screening of asymptomatic patients is futile,16 18 there is evidence that stroke rates are signicantly lower in treated patients when
1150
The Journal of TRAUMA Injury, Infection, and Critical Care Volume 67, Number 6, December 2009
The Journal of TRAUMA Injury, Infection, and Critical Care Volume 67, Number 6, December 2009
WTA Blunt Cerebrovascular Injuries
Diagnosis and Management of Blunt Cerebrovascular Injuries
Signs/Symptoms of BCVI
Arterial hemorrhage from neck/nose/mouth (?OR) Expanding cervical hematoma Cervical bruit in pt < 50 yrs old Focal neurologic defect: TIA, hemiparesis, vertebrobasilar symptoms, Horners Syndrome Stroke on CT or MRI Neurologic deficit inconsistent with head CT Equivocal Finding or High Clinical Suspicion Yes Emergent
D
Arteriogramc
16-Slice CTAa
Positive Grade I-IV Injuryc
C
Negative
Stopb
No Risk Factors for BCVI
High energy transfer mechanism associated with: Displaced mid-face fracture (LeFort II or III) Basilar skull fracture with carotid canal involvement CHI consistent with DAI and GCS < 6 Cervical vertebral body or transverse foramen fracture, subluxation, or ligamentous injury at any level; any fracture at C1-C3 Near hanging with anoxia Clothesline type injury or seat belt abrasion with significant swelling, pain, or altered MS.
Grade V Injuryd
E
Antithrombotic Therapy: Heparin (PTT 40-50 sec)
e
F
Endovascular Treatment
B
Yes Urgent
Repeat 16-Slice CTA in 7-10 days
Injury Healed?
Yes
Discontinue Antithrombotics
No
H I
a b
Consider stenting for severe luminal narrowing or expanding pseudoaneurysmf Antiplatelet rx for 3 months and re-imageg
No
STOP
CT angiography with multidetector-row CT, 16-channel or higher. If fewer than 16 channels, interpret CTA with caution. If Signs/Symptoms or high clinical suspicion and (-)CTA, consider arteriogram as the gold standard For positive arteriogram, follow treatment algorithm as per 16-slice CTA results (E and F) d If Grade II-V injury is surgically accessible and patient has not suffered completed stroke, pursue operative repair e Heparin is preferred in the acute setting, as it is reversible and may be more efficacious than antiplatelet drugs f Stenting should be performed with caution, and appropriate antithrombotic therapy administered concurrently g Aspirin alone (75-150 mg daily) is adequate and should be considered lifelong as its risk profile is superior to coumadin
c
Figure 1. Algorithm for the diagnosis and management of blunt cerebrovascular injuries in adults.
compared with untreated patients.11,12,19 Moreover, the Denver group has demonstrated that screening and treatment of BCVI is cost effective.20 Identication of a high-risk group for screening has been debated in the literature. The fundamental mechanisms of internal carotid artery injury include (a) cervical hyperextension or hyperexion with rotation, stretching the internal carotid artery over the lateral articular processes of cervical vertebral bodies C1C3; (b) direct cervical trauma; (c) intraoral trauma; and (d) basilar skull fracture involving the carotid canal.21,22 The vertebral artery is most commonly injured from C-spine injuries, especially subluxations and fractures of the foramen transversarium.23 Analyses of screening have identied the following list of high-risk factors for BCVI:9 (a) an injury mechanism compatible with severe cervical hyperextension with rotation or hyperexion; (b) Lefort II or III midface fractures; (c) basilar skull fracture involving the carotid canal; (d) closed head injury consistent with diffuse axonal injury with Glasgow Coma Scale score 6; (e) cervical vertebral body or transverse foramen fracture, subluxation, or ligamentous injury at any level, or any
2009 Lippincott Williams & Wilkins
fracture at the level of C1C3; (f) near-hanging resulting in cerebral anoxia; or (g) seat belt or other clothesline-type injury with signicant cervical pain, swelling, or altered mental status. With the improved accuracy of noninvasive screening modalities, there is a tendency to liberalize screening in an attempt to capture all injuries, rather than restricting screening to groups with the highest risk.24 26 Broadened screening guidelines may include combined thoracic and cervical or cranial injuries, but there have not been any large-scale analyses to determine the yield of such protocols. C. Four-vessel biplanar cerebral arteriography (ART) has been considered the gold standard for diagnosis of BCVI. Unfortunately, it is invasive and resource intensive, and its risks include complications related to catheter insertion (12% hematoma; arterial pseudoaneurysm), contrast administration (12% renal dysfunction; allergic reaction), and stroke (1%).11 Duplex ultrasonography is widely used for imaging the extracranial carotid arteries. However, because of its technical limitations and poor sensitivity in clinical trials, there is virtually no role for ultrasonography for BCVI screening.3,27 Similarly, with
1151
Bif et al.
The Journal of TRAUMA Injury, Infection, and Critical Care Volume 67, Number 6, December 2009
its documented poor sensitivity and specicity for BCVI,12,28 magnetic resonance angiography is not considered a standard screening test for BCVI. In contrast, CT angiography (CTA) has emerged as the preferred screening test for BCVI. Although the accuracy of earlygeneration CTA was poor,12,28 it was improved with multidetector-row (4- and 8-slice) CTA.29,30 Sixteen-slice CTA has been adopted by a number of centers and seems to reliably identify clinically signicant BCVI.15,26 Three published studies have evaluated the accuracy of 16-slice CTA compared with ART. Eastman et al.14 reported 100% sensitivity of 16-slice CTA for carotid and 96% sensitivity for vertebral artery injuries. Utter et al.29 performed ART on a subset (30%) of their patients with normal CTA and initially found that CTA missed seven BCVI among 82 patients, for a negative predictive value of 92%. However, retrospective review of the CTA images found that the injuries were evident in six of the seven patients, and that the seventh patients abnormality was most likely not traumatic in origin. Malhotra et al.31 have offered a note of caution, reporting 43% false-positive and 9% false-negative rates for CTA. However, as in the series of Utter et al.,29 the inaccuracy of CTA seemed to be related in large part to the radiologists inexperience, as all of the missed BCVI occurred in the rst half of the study period. Thus, it seems that 16-slice (or more) CTA is reliable for screening for clinically signicant BCVI, but that the accuracy diminishes with fewer detector rows. If CTA is not available, ART is the gold standard. If ART is not available, it is recommended that an institutional clinical practice guideline be outlined that considers transfer to a trauma center for patients at high risk. In the setting of a symptomatic patient and normal noninvasive screening study, ART is recommended to denitively exclude injury. D. A relatively high false-positive rate suggests that CTA may be oversensitive. However, ART may be warranted in the setting of high clinical suspicion and a normal CTA to denitively exclude an injury. E. The primary management strategies for BCVI include observation, surgical repair, antithrombotic drugs, and endovascular therapy. In determining the treatment for an individual, the location and grade of the injury (Table 1) as well as symptomatology must all be considered.32 Given the high morbidity and mortality rates historically associated with untreated BCVI, observation should not be chosen unless there are contraindications to alternative
F.
G.
H.
TABLE 1. Blunt Carotid and Vertebral Arterial Injury Grading Scale32
Injury Grade I II III IV V Description Luminal irregularity or dissection with 25% luminal narrowing Dissection or intramural hematoma with 25% luminal narrowing, intraluminal thrombus, or raised intimal ap Pseudoaneurysm Occlusion Transection with free extravasation
I.
strategies. Currently, surgical therapy for BCVI is limited. Grade I injuries are associated with a low enough stroke risk that surgical repair is not justied. Repair is warranted in higher-grade injuries, but surgical access is often precluded by involvement of the carotid artery at the base of the skull.11 Consequently, nonsurgical management is the rst-line treatment of BCVI. There are no published prospective randomized studies comparing treatment strategies; management recommendations are made based on retrospective analyses of patients managed per institutional protocols. Early reports recommended systemic anticoagulation with heparin (no bolus; 10 U/kg/h to target partial thromboplastin time 40 50 s), demonstrating improved neurologic outcomes among symptomatic patients and stroke prevention among asymptomatic patients.5,11,12 A few retrospective, uncontrolled case series,3335 as well as more recent large reports from Memphis19 and Denver36 suggest that systemic heparinization and antiplatelet therapy (clopidogrel 75 mg daily or aspirin 325 mg daily) are equally efcacious in stroke prevention. In the absence of controlled data, systemic heparin may be preferred among patients with neurologic symptoms and in those who have no contraindications. The Memphis data5 demonstrate systemic heparinizations clear efcacy in improving neurologic outcomes among symptomatic patients. Furthermore, although statistical signicance was not achieved, the large series in Denver11 suggests that heparin may be superior to antiplatelet therapy in stroke prevention (p 0.07) and in neurologic improvement after ischemic insult (p 0.15). Grade V injuries are associated with high mortality and mandate immediate attempts at control. Urgent surgical repair is indicated for accessible lesions, but the majority is inaccessible and require endovascular techniques.11,32 A follow-up imaging study is recommended 7 days to 10 days after injury or for any change in neurologic status. Follow-up imaging led to a change in therapy in 65% of grade I and 51% of grade II injuries and helped plan therapy for grade III injuries.11 In the setting of progressive severe vessel narrowing or pseudoaneurysm enlargement, stents have been deployed in an effort to maintain vascular patency.11,32 A review of the Denver experience found a 17% incidence of stent-related complications and 45% occlusion rate, suggesting that risks exceed benets.37 On the other hand, the Memphis group19 reported a good safety and patency record. It is clear that controlled trials are needed, caution should be used during stent deployment to avoid dislodging unstable thrombus, and poststent antithrombotic therapy is critical. It is not advisable to deploy stents within the rst several days after injury. It has been recommended that patients receive long-term antithrombotic therapy,11,12 but the optimal drug and duration have not been studied. In the absence of documented healing of the vessel, it is reasonable to provide some treatment, as stroke has been reported as long as 14 years after injury. Coumadin was recommended in early series,11,12 but with the apparent efcacy of antiplatelet therapy in the early period, it seems that long-term antiplatelet therapy is preferable to warfarin for its safety and
2009 Lippincott Williams & Wilkins
1152
The Journal of TRAUMA Injury, Infection, and Critical Care Volume 67, Number 6, December 2009
WTA Blunt Cerebrovascular Injuries
cost prole. Aspirin and clopidogrel have different mechanisms of action; in addition, some individuals are resistant to the effects of one or both drugs. Several studies have evaluated the safety and efcacy of dual antiplatelet therapy (aspirin combined with clopidogrel) in a number of clinical situations. Dual therapy is indicated in the setting of acute coronary syndromes and percutaneous coronary interventions, with or without stent placement. On the other hand, it is not recommended in patients who have had a stroke or transient ischemic attack, based on increased bleeding risk and the lack of benet or increase in mortality.38 More studies are necessary to determine the risk:benet of dual therapy in BCVI. Lifelong antiplatelet therapy is recommended if the lesion persists. Aspirin is currently the agent of choice, but newer agents with reversible effects may be preferable in the future. Platelet mapping may one day assist in choice of drug and dose. REFERENCES
1. Davis JW, Holbrook TL, Hoyt DB, Mackersie RC, Field TO, Jr., Shackford SR. Blunt carotid artery dissection: incidence, associated injuries, screening, and treatment. J Trauma. 1990;30:1514 1517. 2. Martin RF, Eldrup-Jorgensen J, Clark DE, Bredenberg CE. Blunt trauma to the carotid arteries. J Vasc Surg. 1991;14:789 795. 3. Cogbill TH, Moore EE, Meissner M, et al. The spectrum of blunt injury to the carotid artery: a multicenter perspective. J Trauma. 1994;37:473479. 4. Ramadan F, Rutledge R, Oller D, Howell P, Baker C, Keagy B. Carotid artery trauma: a review of contemporary trauma center experiences. J Vasc Surg. 1995;21:46 54. 5. Fabian TC, Patton JH, Jr., Croce MA, Minard G, Kudsk KA, Pritchard FE. Blunt carotid injury: importance of early diagnosis and anticoagulant therapy. Ann Surg. 1996;223:513525. 6. Parikh AA, Luchette FA, Valente JF, et al. Blunt carotid artery injuries. J Am Coll Surg. 1997;185:80 86. 7. Berne JD, Norwood SH, McAuley CE, Vallina VL, Creath RG, McLarty J. The high morbidity of blunt cerebrovascular injury in an unscreened population: more evidence of the need for mandatory screening protocols. J Am Coll Surg. 2001;192:314 321. 8. Prall JA, Brega KE, Coldwell DM, Breeze RE. Incidence of unsuspected blunt carotid artery injury. Neurosurgery. 1998;42:495 499. 9. Bif WL, Moore EE, Ryu RK, et al. The unrecognized epidemic of blunt carotid arterial injuries: early diagnosis improves neurologic outcome. Ann Surg. 1998;228:462 470. 10. Kerwin AJ, Bynoe RP, Murray J, et al. Liberalized screening for blunt carotid and vertebral artery injuries is justied. J Trauma. 2001;51:308314. 11. Bif WL, Ray CE, Jr., Moore EE, et al. Treatment-related outcomes from blunt cerebrovascular injuries: the importance of routine follow-up arteriography. Ann Surg. 2002;235:699 707. 12. Miller PR, Fabian TC, Croce MA, et al. Prospective screening for blunt cerebrovascular injuries: analysis of diagnostic modalities and outcomes. Ann Surg. 2002;236:386 395. 13. Schneidereit NP, Simons R, Nicolau S, et al. Utility of screening for blunt vascular neck injuries with computed tomographic angiography. J Trauma. 2006;60:209 216. 14. Eastman AL, Chason DP, Perez CL, McAnulty AL, Minei JP. Computed tomographic angiography for the diagnosis of blunt cervical vascular injury: is it ready for primetime? J Trauma. 2006;60:925929. 15. Berne JD, Reuland KS, Villarreal DH, McGovern TM, Rowe SA, Norwood SH. Sixteen-slice multi-detector computed tomographic angiography improves the accuracy of screening for blunt cerebrovascular injury. J Trauma. 2006;60:1204 1209. 16. Carrillo EH, Osborne DL, Spain DA, Miller FB, Senler SO, Richardson
17. 18.
19.
20. 21. 22. 23. 24. 25. 26.
27.
28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38.
JD. Blunt carotid artery injuries: difculties with the diagnosis prior to neurologic event. J Trauma. 1999;46:1120 1125. Mayberry JC, Brown CV, Mullins RJ, Velmahos GC. Blunt carotid artery injury: the futility of aggressive screening and diagnosis. Arch Surg. 2004;139:609 613. Spaniolas K, Velmahos GC, Alam HB, de Moya M, Tabbara M, Sailhamer E. Does improved detection of blunt vertebral artery injuries lead to improved outcomes? Analysis of the National Trauma Data Bank. World J Surg. 2008;32:2190 2194. Edwards NM, Fabian TC, Claridge JA, Timmons SD, Fischer PE, Croce MA. Antithrombotic therapy and endovascular stents are effective treatment for blunt carotid injuries: results from longterm followup. J Am Coll Surg. 2007;204:10071015. Cothren CC, Moore EE, Ray CE, Jr., et al. Screening for blunt cerebrovascular injuries is cost-effective. Am J Surg. 2005;190:845 849. Crissey MM, Bernstein EF. Delayed presentation of carotid intimal tear following blunt craniocervical trauma. Surgery. 1974;75:543549. Zelenock GB, Kazmers A, Whitehouse WM, Jr., et al. Extracranial internal carotid artery dissections: noniatrogenic traumatic lesions. Arch Surg. 1982;117:425 430. Bif WL, Moore EE, Elliott JP, et al. The devastating potential of blunt vertebral arterial injuries. Ann Surg. 2000;231:672 681. Bif WL, Moore EE, Offner PJ, et al. Optimizing screening for blunt cerebrovascular injuries. Am J Surg. 1999;178:517522. Cothren CC, Moore EE, Bif WL, et al. Cervical spine fracture patterns predictive of blunt vertebral artery injury. J Trauma. 2003;55:811 813. Bif WL, Egglin T, Benedetto B, Gibbs F, Ciof WG. Sixteen-slice computed tomographic angiography is a reliable noninvasive screening test for clinically signicant blunt cerebrovascular injuries. J Trauma. 2006;60:745751. Mutze S, Rademacher G, Matthes G, Hosten N, Stengel D. Blunt cerebrovascular injury in patients with blunt multiple trauma: diagnostic accuracy of duplex Doppler US and early CT angiography. Radiology. 2005;237:884 892. Bif WL, Ray CE, Jr., Moore EE, Mestek M, Johnson JL, Burch JM. Noninvasive diagnosis of blunt cerebrovascular injuries: a preliminary report. J Trauma. 2002;53:850 856. Utter GH, Hollingworth W, Hallam DK, Jarvik JG, Jurkovich GJ. Sixteen-slice CT angiography in patients with suspected blunt carotid and vertebral artery injuries. J Am Coll Surg. 2006;203:838 848. Bub LD, Hollingworth W, Jarvik JG, Hallam DK. Screening for blunt cerebrovascular injury: evaluating the accuracy of multidetector computed tomographic angiography. J Trauma. 2005;59:691 697. Malhotra AK, Camacho M, Ivatury RR, et al. Computed tomographic angiography for the diagnosis of blunt carotid/vertebral artery injury: a note of caution. Ann Surg. 2007;246:632 643. Bif WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Burch JM. Blunt carotid arterial injuries: implications of a new grading scale. J Trauma. 1999;47:845 853. Colella JJ, Diamond DL. Blunt carotid artery injury: reassessing the role of anticoagulation. Am Surg. 1996;62:212217. Eachempati SR, Vaslef SN, Sebastian MW, Reed RL, II. Blunt vascular injuries of the head and neck: is heparinization necessary? J Trauma. 1998;45:9971004. Wahl WL, Brandt MM, Thompson BG, Taheri PA, Greeneld LJ. Antiplatelet therapy: an alternative to heparin for blunt carotid injury. J Trauma. 2002;52:896 901. Cothren CC, Moore EE, Bif WL, et al. Anticoagulation is the gold standard therapy for blunt carotid injuries to reduce stroke rate. Arch Surg. 2004;139:540 546. Cothren CC, Moore EE, Ray CE, Jr., et al. Carotid artery stents for blunt cerebrovascular injury: risks exceed benets. Arch Surg. 2005;140:480 486. Hermosillo AJ, Spinler SA. Aspirin, clopidogrel, and warfarin: is the combination appropriate and effective or inappropriate and too dangerous? Ann Pharmocother. 2008;42:790 805.
2009 Lippincott Williams & Wilkins
1153
You might also like
- Management of Blunt and Penetrating Neck TraumaDocument15 pagesManagement of Blunt and Penetrating Neck TraumaJuan Jose SarastiNo ratings yet
- Trauma CERVICAL-Radiol Clin N.A.2012Document14 pagesTrauma CERVICAL-Radiol Clin N.A.2012Pepe pepe pepeNo ratings yet
- 2015 - Improving Outcomes PolitraumaDocument18 pages2015 - Improving Outcomes PolitraumaPepe pepe pepeNo ratings yet
- Imaging in Peripheral Arterial Disease: Clinical and Research ApplicationsFrom EverandImaging in Peripheral Arterial Disease: Clinical and Research ApplicationsNo ratings yet
- Soal MCQ Dari EJVESDocument4 pagesSoal MCQ Dari EJVESAnonymous 7I3ns1zTCNo ratings yet
- NASCETDocument9 pagesNASCETektosNo ratings yet
- Computing and Visualization for Intravascular Imaging and Computer-Assisted StentingFrom EverandComputing and Visualization for Intravascular Imaging and Computer-Assisted StentingSimone BaloccoNo ratings yet
- The Devastating Potential of Blunt Vertebral Arterial InjuriesDocument10 pagesThe Devastating Potential of Blunt Vertebral Arterial InjuriesAndrew BourasNo ratings yet
- Blunt Cerebrovascular Injuries - Advances in Screening, Imaging, and Management TrendsDocument9 pagesBlunt Cerebrovascular Injuries - Advances in Screening, Imaging, and Management TrendsJuliana Mendoza MantillaNo ratings yet
- Clinical Issues: Blunt Cardiac TraumaDocument5 pagesClinical Issues: Blunt Cardiac Traumacharlietuna1No ratings yet
- Metastatic Spine Disease: A Guide to Diagnosis and ManagementFrom EverandMetastatic Spine Disease: A Guide to Diagnosis and ManagementRex A. W. MarcoNo ratings yet
- Piis1078588400911705 PDFDocument4 pagesPiis1078588400911705 PDFnilsNo ratings yet
- Diseccion Aortica Acguda CronicaDocument10 pagesDiseccion Aortica Acguda Cronicaarturo garciaNo ratings yet
- Jurnal Diagnostik ADocument8 pagesJurnal Diagnostik AImtina AhdaNo ratings yet
- Acs 03 03 234Document13 pagesAcs 03 03 234IwanNo ratings yet
- Malformacion Venosa PDFDocument6 pagesMalformacion Venosa PDFBarbara Helen StanleyNo ratings yet
- Estudio de Endarterectomía CarotídeaDocument9 pagesEstudio de Endarterectomía CarotídeaErnest Pardo RubioNo ratings yet
- Clinical Handbook of Cardiac ElectrophysiologyFrom EverandClinical Handbook of Cardiac ElectrophysiologyBenedict M. GloverNo ratings yet
- J NeuroIntervent Surg 2013 González Neurintsurg 2013 010715Document7 pagesJ NeuroIntervent Surg 2013 González Neurintsurg 2013 010715Rogério HitsugayaNo ratings yet
- The Pattern and Prevalence of Vertebral Artery Injury in Patients With Cervical Spine FracturesDocument4 pagesThe Pattern and Prevalence of Vertebral Artery Injury in Patients With Cervical Spine FracturesFrontiersNo ratings yet
- Trauma Medular - Cervical Trauma ColumnaDocument28 pagesTrauma Medular - Cervical Trauma ColumnayustinjulianavNo ratings yet
- Multiple Choice QuestionsDocument3 pagesMultiple Choice QuestionsMahmoud ElsabbaghNo ratings yet
- Atlas of Coronary Intravascular Optical Coherence TomographyFrom EverandAtlas of Coronary Intravascular Optical Coherence TomographyNo ratings yet
- Femur Fractures Should Not Be Considered Distracting Injuries For CervicalDocument6 pagesFemur Fractures Should Not Be Considered Distracting Injuries For CervicalnellyNo ratings yet
- Brown 2018Document14 pagesBrown 2018Cinthya Añazco RomeroNo ratings yet
- Journal Reading Decompressive Craniectomy For EDHDocument10 pagesJournal Reading Decompressive Craniectomy For EDHmasyfuqNo ratings yet
- Tolias CM, Choksey M 1996 - Significance - of - Sudden - Agonizing - HeadacheDocument12 pagesTolias CM, Choksey M 1996 - Significance - of - Sudden - Agonizing - HeadachemunchisolichokseyNo ratings yet
- Spontaneous Vertebral Artery Dissection: Report of 16 Cases: Original ArticleDocument7 pagesSpontaneous Vertebral Artery Dissection: Report of 16 Cases: Original ArticleAyu Yoniko CimplukNo ratings yet
- 12 Strokes: A Case-based Guide to Acute Ischemic Stroke ManagementFrom Everand12 Strokes: A Case-based Guide to Acute Ischemic Stroke ManagementFerdinand K. HuiNo ratings yet
- V23I2 05 FREE DrChouhan PDFDocument7 pagesV23I2 05 FREE DrChouhan PDFBimo PramestaNo ratings yet
- Multiple Choice QuestionsDocument3 pagesMultiple Choice QuestionsSushibalaNo ratings yet
- Intervesnsi Stroke 1Document9 pagesIntervesnsi Stroke 1Zilbran BerontaxNo ratings yet
- Antikoagulan JurnalDocument5 pagesAntikoagulan JurnalansyemomoleNo ratings yet
- Flaherty 2016Document6 pagesFlaherty 2016Diornald MogiNo ratings yet
- ESC Hot Line: European Heart Journal (2015) 36, 3359-3367 Doi:10.1093/eurheartj/ehv444Document9 pagesESC Hot Line: European Heart Journal (2015) 36, 3359-3367 Doi:10.1093/eurheartj/ehv444maranzazuuNo ratings yet
- A New Classification of Head Injury Based OnDocument7 pagesA New Classification of Head Injury Based OnJejem Marandra EmkamasNo ratings yet
- Dural Venous Sinus Thrombosis in Patients Presenting With Blunt Traumatic Brain Injuries and Skull Fractures - A Systematic Review and Meta-AnalysisDocument14 pagesDural Venous Sinus Thrombosis in Patients Presenting With Blunt Traumatic Brain Injuries and Skull Fractures - A Systematic Review and Meta-Analysisclaudio RivasNo ratings yet
- Ferro 2008Document8 pagesFerro 2008Carlos RiquelmeNo ratings yet
- Damage Control Resuscitation: Identification and Treatment of Life-Threatening HemorrhageFrom EverandDamage Control Resuscitation: Identification and Treatment of Life-Threatening HemorrhagePhilip C. SpinellaNo ratings yet
- Cervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?Document4 pagesCervical Angiograms in Cervical Spine Trauma Patients 5 Years After The Data: Has Practice Changed?edi_wsNo ratings yet
- Guideline Carotida 2011Document31 pagesGuideline Carotida 2011Marco Antonio KoffNo ratings yet
- Rectal Cancer: International Perspectives on Multimodality ManagementFrom EverandRectal Cancer: International Perspectives on Multimodality ManagementBrian G. CzitoNo ratings yet
- Chinese Journal of TraumatologyDocument5 pagesChinese Journal of Traumatologybulan hasanNo ratings yet
- Pan Nucci 2011Document8 pagesPan Nucci 2011Ana I. NevarezNo ratings yet
- Diagnosis and Treatment of Thoracic Outlet SyndromeDocument114 pagesDiagnosis and Treatment of Thoracic Outlet SyndromeCharles Mitchell100% (1)
- Society For Vascular Surgery Clinical Practice 2022 Guidelines For Management of Extracranial Cerebrovascular DiseaseDocument19 pagesSociety For Vascular Surgery Clinical Practice 2022 Guidelines For Management of Extracranial Cerebrovascular DiseaseLaura G.QNo ratings yet
- Radiologic Management of Pelvic Ring FracturesDocument95 pagesRadiologic Management of Pelvic Ring FracturesAlan Covarrubias RdgzNo ratings yet
- Broderick 2015Document4 pagesBroderick 2015Jimmy SilverhandNo ratings yet
- 030 - EIJ D 23 00749 - GalassiDocument11 pages030 - EIJ D 23 00749 - GalassiBagus CarterNo ratings yet
- Lower Extremity Fasciotomy Indications and TechniqDocument11 pagesLower Extremity Fasciotomy Indications and TechniqbbkdabdfaNo ratings yet
- Spot Sign Predict Hematoma ExpansionDocument7 pagesSpot Sign Predict Hematoma ExpansionRonny RahadiNo ratings yet
- Superior Vena Cava Syndrome - EM ClinicsDocument13 pagesSuperior Vena Cava Syndrome - EM ClinicsFuji Seprinur HidayatNo ratings yet
- Evaluation and Management of Acute Vascular Trauma: Gloria M.M. Salazar, MD, and T. Gregory Walker, MDDocument15 pagesEvaluation and Management of Acute Vascular Trauma: Gloria M.M. Salazar, MD, and T. Gregory Walker, MDfranciscoreynaNo ratings yet
- Spleen AnatomyDocument5 pagesSpleen AnatomyChlarissa WahabNo ratings yet
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeDocument7 pages(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroNo ratings yet
- Journal NeuroDocument6 pagesJournal NeuroBetari DhiraNo ratings yet
- Risk Factors For Ischemic Stroke Post Bone FractureDocument11 pagesRisk Factors For Ischemic Stroke Post Bone FractureFerina Mega SilviaNo ratings yet
- Legend Characteristics: Folklore: Long Middle School WebquestsDocument1 pageLegend Characteristics: Folklore: Long Middle School WebquestsAns FitriNo ratings yet
- Intramuscular Versus Intravenous Benzodiazepines For Prehospital Treatment of Status EpilepticusDocument9 pagesIntramuscular Versus Intravenous Benzodiazepines For Prehospital Treatment of Status EpilepticusAns FitriNo ratings yet
- 2011 ITP Pocket GuideDocument8 pages2011 ITP Pocket GuidevtNo ratings yet
- Intramuscular Versus Intravenous Benzodiazepines For Prehospital Treatment of Status EpilepticusDocument9 pagesIntramuscular Versus Intravenous Benzodiazepines For Prehospital Treatment of Status EpilepticusAns FitriNo ratings yet
- Intramuscular Versus Intravenous Benzodiazepines For Prehospital Treatment of Status EpilepticusDocument9 pagesIntramuscular Versus Intravenous Benzodiazepines For Prehospital Treatment of Status EpilepticusAns FitriNo ratings yet
- Lamp IranDocument8 pagesLamp IranAns FitriNo ratings yet
- 125 130 BunnagDocument6 pages125 130 BunnagAns FitriNo ratings yet
- Research Article: Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based StudyDocument13 pagesResearch Article: Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based StudyAns FitriNo ratings yet
- ITP BJH 2003Document23 pagesITP BJH 2003Mohammad IrfanNo ratings yet
- ITP BJH 2003Document23 pagesITP BJH 2003Mohammad IrfanNo ratings yet
- Presentation On ITPDocument23 pagesPresentation On ITPAns FitriNo ratings yet
- Prevent Mosquito Production in Your Septic TankDocument1 pagePrevent Mosquito Production in Your Septic TankAns FitriNo ratings yet
- Research Article: Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based StudyDocument13 pagesResearch Article: Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based StudyAns FitriNo ratings yet
- "I Saw Red": Morning Report March 6, 2006 Nita MohantyDocument30 pages"I Saw Red": Morning Report March 6, 2006 Nita MohantyAns FitriNo ratings yet
- ITP BJH 2003Document23 pagesITP BJH 2003Mohammad IrfanNo ratings yet
- Research Article: Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based StudyDocument13 pagesResearch Article: Comorbidities of Idiopathic Thrombocytopenic Purpura: A Population-Based StudyAns FitriNo ratings yet
- CarotidDocument4 pagesCarotidAns FitriNo ratings yet
- TB Paru klp6Document10 pagesTB Paru klp6qiejaniebieNo ratings yet
- 2151 - InCAP Studies of Kwashiorkor and MarasmusDocument8 pages2151 - InCAP Studies of Kwashiorkor and MarasmusAns FitriNo ratings yet
- My English Workbook!: Semester 1Document21 pagesMy English Workbook!: Semester 1Ans FitriNo ratings yet
- Legend Characteristics: Folklore: Long Middle School WebquestsDocument1 pageLegend Characteristics: Folklore: Long Middle School WebquestsAns FitriNo ratings yet
- Bsaic Live SupportDocument28 pagesBsaic Live SupportAns FitriNo ratings yet
- Eni PurwaniDocument9 pagesEni PurwaniRahmiDiffiliantiNo ratings yet
- Tabel Syok Bagus BngetDocument2 pagesTabel Syok Bagus BngetMega Silfia ZulfiNo ratings yet
- Soal UKDI 15 Mei 2010Document16 pagesSoal UKDI 15 Mei 2010cyelzNo ratings yet
- Intramuscular Versus Intravenous Benzodiazepines For Prehospital Treatment of Status EpilepticusDocument11 pagesIntramuscular Versus Intravenous Benzodiazepines For Prehospital Treatment of Status EpilepticusAns FitriNo ratings yet
- Theorist 2Document42 pagesTheorist 2api-33845373888% (8)
- Contoh Soal Bahasa InggrisDocument3 pagesContoh Soal Bahasa InggrisMilkha OktariyantiNo ratings yet
- Urostomy Guide - American Cancer SocietyDocument19 pagesUrostomy Guide - American Cancer SocietyDipa HandraNo ratings yet
- P2W1 Post Test MS Rle 8Document7 pagesP2W1 Post Test MS Rle 8Angel YN Patricio FlorentinoNo ratings yet
- Lymphomyosot Aids Conventional Therapy in Diabetic Peripherial Neuropathy 2003Document8 pagesLymphomyosot Aids Conventional Therapy in Diabetic Peripherial Neuropathy 2003Dr. Nancy MalikNo ratings yet
- Sany Truck Crane Stc250s5 Parts BookDocument22 pagesSany Truck Crane Stc250s5 Parts Bookrobertflynn180290sdg100% (61)
- Pelepasan Polimer LangerDocument7 pagesPelepasan Polimer LangerUntia Kartika Sari RamadhaniNo ratings yet
- Rudin 1975Document450 pagesRudin 1975Alexander WilkielNo ratings yet
- D&D Homebrew SpellsDocument6 pagesD&D Homebrew SpellsLeandro CotNo ratings yet
- Hardy Weinberg Calculation1Document8 pagesHardy Weinberg Calculation1Rishikaphriya Rauichandran100% (1)
- Concept of Poultry Insurance Schemes in India - Poultry ShortsDocument12 pagesConcept of Poultry Insurance Schemes in India - Poultry ShortsAbhishek SharmaNo ratings yet
- Haloperidol: Brand Name: HaldolDocument15 pagesHaloperidol: Brand Name: Haldolteguh aminNo ratings yet
- PsychequestionsDocument23 pagesPsychequestionsGeorgette Noquera CubayNo ratings yet
- Daftar Diagnosis Penyakit Dengan Gejala AfpDocument1 pageDaftar Diagnosis Penyakit Dengan Gejala Afpnurlaila asmaraniNo ratings yet
- Acyclovir DoseDocument3 pagesAcyclovir DoseRojik GamaNo ratings yet
- GONORRHEADocument8 pagesGONORRHEAFlorenceNo ratings yet
- Pathophysiology Tia VS CvaDocument6 pagesPathophysiology Tia VS CvaRobby Nur Zam ZamNo ratings yet
- MTF, Sba-Gmt202: (Ne Osa)Document5 pagesMTF, Sba-Gmt202: (Ne Osa)Zahra HussainNo ratings yet
- Science: Modified Strategic Intervention MaterialsDocument28 pagesScience: Modified Strategic Intervention Materialskotarobrother23No ratings yet
- Dry Fermented Seafood: Properties, Nutritional Values, Microbial Safety of Selected Starter Culture. NameDocument35 pagesDry Fermented Seafood: Properties, Nutritional Values, Microbial Safety of Selected Starter Culture. NamefidelisNo ratings yet
- Acute Lymphoblastic Leukemia Review 2017 PDFDocument12 pagesAcute Lymphoblastic Leukemia Review 2017 PDFOsiithaa CañaszNo ratings yet
- AudiologistDocument5 pagesAudiologistm afiq fahmiNo ratings yet
- IDC Program Certification Updates RICT 11152023Document22 pagesIDC Program Certification Updates RICT 11152023Geliza RecedeNo ratings yet
- Basic Care & Comfort Nclex RN UwDocument10 pagesBasic Care & Comfort Nclex RN Uwgwen scribd100% (1)
- Pharmacology Viva QuestionsDocument24 pagesPharmacology Viva QuestionsMinhaz Islam100% (1)
- The Seven Basic ChakrasDocument4 pagesThe Seven Basic ChakrasAlesha Rose100% (1)
- Oral Health Care Industry in IndiaDocument3 pagesOral Health Care Industry in IndiaSaranya KRNo ratings yet
- NCP PainDocument4 pagesNCP PainFlauros Ryu JabienNo ratings yet
- Destroy Negative Thoughts!Document107 pagesDestroy Negative Thoughts!yeabsira semuNo ratings yet
- 2009 HSC Exam BiologyDocument34 pages2009 HSC Exam Biologyeducator56100% (1)