Professional Documents
Culture Documents
Transposition of Great Artery: 1. Abstract
Uploaded by
A. Fajar AprianiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Transposition of Great Artery: 1. Abstract
Uploaded by
A. Fajar AprianiCopyright:
Available Formats
TRANSPOSITION OF GREAT ARTERY
1. ABSTRACT
Transposition of the great arteries (TGA) is a congenital (present at birth) heart defect that
occurs when the large vessels that take blood away from the heart to the lungs, or to the body, are
improperly connected. Normally:
oxygen-poor (blue) blood returns to the right atrium from the body, travels to the right
ventricle, then is pumped through the pulmonary artery into the lungs where it receives
oxygen.
Oxygen-rich (red) blood returns to the left atrium from the lungs, passes into the left
ventricle, then is pumped through the aorta out to the body.
In transposition of the great arteries, the aorta is connected to the right ventricle, and the
pulmonary artery is connected to the left ventricle-the exact opposite of a normal heart's anatomy:
Oxygen-poor (blue) blood returns to the right atrium from the body, passes through the
right atrium and ventricle, then goes into the misconnected aorta back to the body.
Oxygen-rich (red) blood returns to the left atrium from the lungs, passes through the left
atrium and ventricle, then goes into the pulmonary artery and back to the lungs.
Two separate circuits are formed -- one that circulates oxygen-poor (blue) blood from the
body back to the body, and another that recirculates oxygen-rich (red) blood from the lungs back to
the lungs. Other heart defects are often associated with TGA, and actually may be necessary in order
for an infant with transposition of the great arteries to live. Openings in the wall separating the left
and right sides of the heart, called atrial septal defect or ventricular septal defect, will allow blood
from one side to mix with blood from another, creating "purple" blood with an oxygen level
somewhere between that of the oxygen-poor (blue) and the oxygen-rich (red) blood.
Babies with TGA have two separate circuits -- one that circulates oxygen-poor (blue) blood
from the body back to the body, and another that recirculates oxygen-rich (red) blood from the
lungs back to the lungs. Without an additional heart defect that allows mixing of oxygen-poor (blue)
and oxygen-rich (red) blood, such as an atrial or ventricular septal defect, infants with TGA will have
oxygen-poor (blue) blood circulating through the body, a situation that is critical. Even with an
additional defect present that allows mixing, babies with transposition of the great arteries may not
have enough oxygen in the bloodstream to meet the body's demands.
Even when a significant amount of mixing of oxygen-poor (blue) and oxygen-rich (red) blood
occurs, other problems may be present. The left ventricle, which in TGA is connected to the
pulmonary artery, is usually the stronger of the two ventricles since it normally has to generate a lot
of force to pump blood to the body. The right ventricle, connected to the aorta in TGA, is considered
the weaker of the two ventricles and may not be able to pump blood efficiently to the body. As a
result, it will enlarge under the strain.
A patent ductus arteriosus (another type of congenital heart defect) will allow mixing of
oxygen-poor (blue) and oxygen-rich (red) blood through the connection between the aorta and
pulmonary artery. The "purple" blood that results from this mixing is beneficial, providing small, if
not normal, amounts of oxygen to the body.
2. PREDISPOSITION AND EPIDEMIOLOGY
The heart is forming during the first eight weeks of fetal development. The problem occurs in
the middle of these weeks, allowing the aorta and pulmonary artery to be attached to the incorrect
chamber. Some congenital heart defects may have a genetic link, either occurring due to a defect in
a gene, a chromosome abnormality or environmental exposure, causing heart problems to occur
more often in certain families. Most of the time this heart defect occurs sporadically (by chance),
with no clear reason for its development.
The epidemiology of TGA are :
Transposition is the most common cyanotic congenital heart lesion presenting in the
neonate.
The overall annual incidence is 20-30 per 100,000 live births.
It is more common in males than females, with a ratio of about 3:1.
Transposition is rarely associated with syndromes or extracardiac malformations
Factors in the mother that may increase the risk of this condition include:
Age over 40
Alcoholism
Diabetes
Poor nutrition during pregnancy (prenatal nutrition)
Rubella or other viral illness during pregnancy
a. Frequency
Despite its overall low prevalence, transposition of the great arteries is the most common
etiology for cyanotic congenital heart disease in the newborn.
1
This lesion presents in 5-7%
of all patients with congenital heart disease. The overall annual incidence is 20-30 per
100,000 live births, and inheritance is multifactorial. Transposition of the great arteries is
isolated in 90% of patients and is rarely associated with syndromes or extracardiac
malformations. This congenital heart defect is more common in infants of diabetic mothers.
b. Mortality/Morbidity
The mortality rate in untreated patients is approximately 30% in the first week, 50% in the
first month, and 90% by the end of the first year. With improved diagnostic, medical, and
surgical techniques, the overall short-term and midterm survival rate exceeds 90%. Long-
term complications are secondary to prolonged cyanosis and include polycythemia and
hyperviscosity syndrome. These patients may develop headache, decreased exercise
tolerance, and stroke. Thrombocytopenia is common in patients with cyanotic congenital
heart disease leading to bleeding complications. Patients with a large ventricular septal
defect, a patent ductus arteriosus, or both may have an early predilection for congestive
heart failure, as pulmonary vascular resistance falls with increasing age. Heart failure may be
mitigated in those patients with left ventricular outflow tract (pulmonary) stenosis.
A small percentage (approximately 5%) of patients with transposition of the great arteries
(and often a ventricular septal defect) develop accelerated pulmonary vascular obstructive
disease and progressive cyanosis despite surgical repair or palliation. Long-term survival in
this subgroup is particularly poor.
c. Race
No racial predilection is known.
d. Sex
TGA has a 60-70% male predominance.
e. Age
Patients with TGA usually present with cyanosis in the newborn period, but clinical
manifestations and courses are influenced predominantly by the degree of intercirculatory
mixing.
3. PATHOPHYSIOLOGY
Systemic and pulmonary circulations are
completely separated. After returning to the right heart,
desaturated systemic venous blood is pumped into the
systemic circulation without being oxygenated in the
lungs; oxygenated blood entering the left heart goes back
to the lungs rather than to the rest of the body. This
anomaly is not compatible with life unless desaturated
and oxygenated blood can mix through openings at one
or more levels. The pulmonary and systemic circulations
function in parallel, rather than in series. Oxygenated
pulmonary venous blood returns to the left atrium and
left ventricle but is recirculated to the pulmonary vascular
bed via the abnormal pulmonary arterial connection to
the left ventricle. Deoxygenated systemic venous blood returns to the right atrium and right
ventricle where it is subsequently pumped to the systemic circulation, effectively bypassing the
lungs. This parallel circulatory arrangement results in a deficient oxygen supply to the tissues and an
excessive right and left ventricular workload. It is incompatible with prolonged survival unless mixing
of oxygenated and deoxygenated blood occurs at some anatomic level. The following are 3 common
anatomic sites for mixing of oxygenated and deoxygenated blood in transposition of the great
arteries: Atrial septal defect, Ventricular septal defect, and Patent Ductus Arteriosus
4. CLINICAL MANIFESTATION
a. History
Infants with transposition of the great arteries (TGA) are usually born at term, with cyanosis
apparent within hours of birth.
The clinical course and manifestations depend on the extent of intercirculatory mixing and
the presence of associated anatomic lesions.
o Transposition of the great arteries with intact ventricular septum: Prominent and
progressive cyanosis within the first 24 hours of life is the usual finding in infants.
o Transposition of the great arteries with large ventricular septal defect
Infants may not initially manifest symptoms of heart disease, although mild
cyanosis (particularly when crying) is often noted.
Signs of congestive heart failure (tachypnea, tachycardia, diaphoresis, and
failure to gain weight) may become evident over the first 3-6 weeks as
pulmonary blood flow increases.
o Transposition of the great arteries with ventricular septal defect and left ventricular
outflow tract obstruction
Infants often present with extreme cyanosis at birth, proportional to the
degree of left ventricular (pulmonary) outflow tract obstruction.
The clinical history may be similar to that of an infant with tetralogy of
Fallot.
o Transposition of the great arteries with ventricular septal defect and pulmonary
vascular obstructive disease
Progressively advancing pulmonary vascular obstructive disease can prevent
this rare subgroup of patients from developing symptoms of congestive
heart failure, despite a large ventricular septal defect.
Most often, patients present with progressive cyanosis, despite an early
successful palliative procedure.
b. Physical
Newborns with transposition of the great arteries are usually well developed, without
dysmorphic features. Physical findings at presentation depend on the presence of associated lesions.
Transposition of the great arteries with intact ventricular septum
o Infants typically present with progressive central (perioral and periorbital) cyanosis.
o Other than cyanosis, the physical examination is often unremarkable.
Transposition of the great arteries with large ventricular septal defect
o Cyanosis may be mild initially, although it is usually more apparent with stress or
crying.
o Upon presentation, infants often have an increased right ventricular impulse, a
prominent grade 3-4/6 holosystolic murmur, third heart sound, mid-diastolic
rumble, and a gallop rhythm.
o Hepatomegaly may be present.
Transposition of the great arteries with ventricular septal defect and left ventricular outflow
tract obstruction
o Cyanosis is prominent at birth, and the findings are similar to those of infants with
tetralogy of Fallot.
o A single, or narrowly split, diminished second heart sound and a grade 2-3/6 systolic
ejection murmur may be present.
o Hepatomegaly is rare.
Transposition of the great arteries with ventricular septal defect and pulmonary vascular
obstructive disease
o Progressive pulmonary vascular obstructive disease is not always evident from
physical examination findings.
o Cyanosis is usually present and can progress despite palliative therapy in the
newborn period.
o No murmur (despite the ventricular septal defect) or early short systolic ejection
sounds are heard.
o The second heart sound is often single, with increased intensity.
o In later childhood or adolescence, a high-pitched, blowing, early decrescendo
diastolic murmur of pulmonary insufficiency and a blowing apical murmur of mitral
insufficiency are evident.
5. DIAGNOSIS
A pediatric cardiologist and/or a neonatologist may be involved in your child's care. A pediatric
cardiologist specializes in the diagnosis and medical management of congenital heart defects, as well
as heart problems that may develop later in childhood. A neonatologist specializes in illnesses
affecting newborns, both premature and full-term. Cyanosis is the major indication that there is a
problem with your newborn. Your child's physician may also have heard a heart murmur during a
physical examination. A heart murmur is simply a noise caused by the turbulence of blood flowing
through the openings that allow the blood to mix.
Other diagnostic tests are needed to help with the diagnosis, and may include the following:
Chest X-ray A diagnostic test that uses invisible electromagnetic energy beams to
produce images of internal tissues, bones, and organs onto film.
In the normal anatomy, the aorta is anterior to and at the right of the pulmonary
artery . In transposition of the great arteries, the pulmonary artery is situated to the
right of its normal location and is obscured by the aorta on frontal chest radiographs.
This malposition, in association with stress-induced thymic atrophy and hyperinflated
lungs, results in the apparent narrowing of the superior mediastinum on radiographs,
the most consistent sign of transposition of the great arteries. The cardiovascular
silhouette varies from normal in the first few days after birth to enlarged and globular,
with the classic egg on a string appearance.
Electrocardiogram (ECG or EKG) A test that records the electrical activity of the heart,
shows abnormal rhythms (arrhythmias or dysrhythmias) and detects heart muscle
stress.
Echocardiogram (echo) A procedure that evaluates the structure and function of the
heart by using sound waves, recorded on an electronic sensor, that produce a moving
picture of the heart and heart valves.
Cardiac Catheterization A procedure that gives very detailed information about the
structures inside the heart. Under sedation, a small, thin, flexible tube (catheter) is
inserted into a blood vessel in the groin and guided to the inside of the heart. Blood
pressure and oxygen measurements are taken in the four chambers of the heart, as well
as in the pulmonary artery and aorta. Contrast dye is injected to more clearly visualize
the structures inside the heart.
Cardiac Magnetic Resonance Imaging (MRI) A non-invasive test that uses three-
dimensional imaging technology produced by magnets to accurately determine blood
flow and functioning of the heart as it is working.
6. TREATMENT
Specific treatment for transposition of the great arteries will be determined by physician
based on:
child's age, overall health and medical history
extent of the disease
child's tolerance for specific medications, procedures or therapies
how child's doctor expects the disease to progress
opinion or preference
The children most likely will be admitted to the intensive care unit (ICU) or special care
nursery once symptoms are noted. Initially, your child may be placed on oxygen or a ventilator to
assist his/her breathing. Intravenous (IV) medications may be given to help the heart and lungs
function more efficiently.
Other important aspects of initial treatment include the following:
A cardiac catheterization procedure can be used as a diagnostic procedure, as well as an
initial treatment procedure for some heart defects. A cardiac catheterization procedure will
usually be performed to evaluate the defect(s) and the amount of blood that is mixing.
As part of the cardiac catheterization, a procedure called a balloon atrial septostomy may be
performed to improve mixing of oxygen-rich (red) and oxygen-poor (blue) blood.
1. A special catheter with a balloon in the tip is used to create an opening in the atrial
septum (wall between the left and right atria).
2. The catheter is guided through the foramen ovale (a small opening present in the atrial
septum that closes shortly after birth) and into the left atrium.
3. The balloon is inflated.
4. The catheter is quickly pulled back through the hole, into the right atrium, enlarging the
hole, allowing blood to mix between the atria.
An intravenous medication called prostaglandin E1 is given to keep the ductus arteriosus
from closing.
All patients require antibiotic prophylaxis prior to dental and indicated surgical
procedures in order to reduce the risk of subacute bacterial endocarditis
Within the first 1 to 2 weeks of age, transposition of the great arteries is surgically repaired.
The procedure that accomplishes this is called a "switch," which roughly describes the surgical
process. The surgical correction of TGA is carried out through an incision in the middle of the chest.
The breast bone is split in the middle and spread apart to expose the heart. A heart-lung machine is
used to do the work of the heart while the heart is cooled, stopped, emptied and opened. The aorta
and pulmonary arteries are disconnected and reconnected to their proper ventricles. The coronary
arteries must be transferred to the newly positioned aorta as well, or "blue" blood will supply the
muscle of the heart. Associated holes between the chambers of the heart are closed. The heart is
then restarted as the heart-lung machine is withdrawn.
7. COMPLICATIONS
Congestive heart failure
Arrhythmias
Right ventricular dysfunction in long-term survivors
Eisenmenger's syndrome
Polycythaemia and hyperviscosity syndrome
Seizures may occur in about 5% of patients before surgery
2
Thrombocytopenia
8. PROGNOSIS
Many infants who undergo TGA surgical repair will grow and develop normally. After TGA
repair, however, infants will need to be followed periodically by a pediatric cardiologist who will
make assessments to check for any heart-related problems, which can include the following:
fast, slow or irregular heart rhythms
leaky heart valves
narrowing of one or both of the great arteries at the switch connection site(s)
narrowing of the coronary arteries at their switch connection site
The mortality rate in untreated patients is approximately 30% in the first week, 50% in the
first month, and 90% by the end of the first year.
Death is usually due to anoxia, acidosis, heart failure and complications associated with
polycythaemia, including thromboembolic events.
The overall survival rate following arterial switch operation is approximately 90% at 15 years
of age. However, exercise performance, cognitive function and quality of life may be
impaired.
Low gestational age and a high preoperative lactate are the most important predictors of
poor developmental outcome.
SOURCES :
1. Childrens Hospital Boston online : TGA
2. eMedicine Pediatrics:Cardiac Disease and Critical Care_TGA
3. http://www.wikipedia.org
4. Merck Manual Professional : Congenital Cardiovascular Anomalies_TGA
5. Medline Plus Medical Encyclopedia_TGA
6. Doctor and Patients UK_TGA
7. American Journal of Roentgenology online
You might also like
- Transposition of The Great Arteries PDFDocument6 pagesTransposition of The Great Arteries PDFSakuntalaPalanki100% (2)
- Cardio Vascular DisordersDocument62 pagesCardio Vascular DisordersUday Kumar100% (1)
- Pediatric Patent Ductus ArteriosusDocument12 pagesPediatric Patent Ductus Arteriosusabirami_murugesuNo ratings yet
- High Yield Plab TopicsDocument20 pagesHigh Yield Plab TopicsBeaulah HunidzariraNo ratings yet
- Complete Transposition of Great ArteriesDocument85 pagesComplete Transposition of Great ArteriesRahul AgrawalNo ratings yet
- Congenital Heart DiseaseDocument10 pagesCongenital Heart DiseaseMarisa PetersonNo ratings yet
- Conginital Heart DiseaseDocument19 pagesConginital Heart DiseaseSanthosh.S.UNo ratings yet
- Acyanotic Congenital Heart DiseaseDocument7 pagesAcyanotic Congenital Heart DiseaseSam Raj100% (1)
- Tiki Taka Notes Final PDFDocument104 pagesTiki Taka Notes Final PDFAditiSahak62No ratings yet
- Principles of EchocardiographyDocument3 pagesPrinciples of Echocardiographys336336anl100% (1)
- Cardiovascular Disease: Internal Medicine Board Review FlashcardsDocument55 pagesCardiovascular Disease: Internal Medicine Board Review FlashcardsJoyee BasuNo ratings yet
- Congenital Heart Diseases, A Simple Guide to these Medical ConditionsFrom EverandCongenital Heart Diseases, A Simple Guide to these Medical ConditionsNo ratings yet
- Congenital Heart Disease - Cynotic AcynoticDocument34 pagesCongenital Heart Disease - Cynotic Acynoticvruttika parmarNo ratings yet
- Introduction To High Risk PregnancyDocument13 pagesIntroduction To High Risk PregnancyMabes100% (1)
- Medical AbbreviationsDocument31 pagesMedical AbbreviationsLailaNo ratings yet
- Nursing Care Plan For Acyanotic Heart DiseaseDocument55 pagesNursing Care Plan For Acyanotic Heart DiseaseDeepikaxena John79% (14)
- Description: Congestive Heart FailureDocument22 pagesDescription: Congestive Heart FailurePinklet Arleena CubianNo ratings yet
- Transposition of Great ArteriesDocument18 pagesTransposition of Great Arteriesparmeshori100% (2)
- Cardio Vascular Disease in PregnancyDocument57 pagesCardio Vascular Disease in PregnancySanthosh.S.U0% (1)
- Martin Zenker-Noonan Syndrome and Related Disorders - A Matter of Deregulated Ras Signaling (Monographs in Human Genetics Vol 17) - S. Karger AG (Switzerland) (2009)Document178 pagesMartin Zenker-Noonan Syndrome and Related Disorders - A Matter of Deregulated Ras Signaling (Monographs in Human Genetics Vol 17) - S. Karger AG (Switzerland) (2009)Lupu AndreeaNo ratings yet
- 1.conginital Cardiac DefectsDocument39 pages1.conginital Cardiac DefectsJõsëph Jåy MîthNo ratings yet
- ERN MRCPCH 3e PDFDocument52 pagesERN MRCPCH 3e PDFrizixxxxxx80% (5)
- Tetralogy of FallotDocument31 pagesTetralogy of FallotAnditha Namira RS100% (1)
- Cardiovascular System Dr. Eman Badr 2020Document182 pagesCardiovascular System Dr. Eman Badr 2020Amina DinarNo ratings yet
- 12 - Semiotics of Cardiovascular Disorders. Semiotics of Congenital Hert Diseases in Children.Document30 pages12 - Semiotics of Cardiovascular Disorders. Semiotics of Congenital Hert Diseases in Children.Omowunmi KadriNo ratings yet
- Cyanotic Congenital Heart DiseaseDocument8 pagesCyanotic Congenital Heart DiseaseMohammed Taha Al-nuaimyNo ratings yet
- Congenital Heart Diseases.Document86 pagesCongenital Heart Diseases.Salman KhanNo ratings yet
- CVS - Session 3 - CHDDocument3 pagesCVS - Session 3 - CHDkotecha.rheaNo ratings yet
- Tetralogy of FallotDocument28 pagesTetralogy of FallotconcozNo ratings yet
- Tricuspid AtresiaDocument14 pagesTricuspid AtresiaPretty AjursNo ratings yet
- Lapkas Dian and DamboDocument34 pagesLapkas Dian and DamboDian Primadia PutriNo ratings yet
- Aruna Ramesh-Emergency...Document6 pagesAruna Ramesh-Emergency...Aishu BNo ratings yet
- Cardio Vascular DiseasesDocument34 pagesCardio Vascular DiseasesSam ParkNo ratings yet
- Tetralogy of FallotDocument7 pagesTetralogy of FallotWidelmark FarrelNo ratings yet
- Congenital Heart DefectDocument12 pagesCongenital Heart Defectsangkularosmina837No ratings yet
- Truncus Arteriosus TransletDocument11 pagesTruncus Arteriosus TransletHijaz Al-YamanNo ratings yet
- Tetralogy of FallotDocument7 pagesTetralogy of FallotAshok Kumar JangirNo ratings yet
- Transposition of The Great ArteriesDocument4 pagesTransposition of The Great ArteriesAgustria AnggraenyNo ratings yet
- Congenital Heart Disease (2011)Document17 pagesCongenital Heart Disease (2011)drheay100% (1)
- Tricuspid Atresia Heart Defect ExplainedDocument5 pagesTricuspid Atresia Heart Defect ExplainedCassyDelaRosaNo ratings yet
- Cardiovascular Dysfunction in ChildrenDocument15 pagesCardiovascular Dysfunction in ChildrenJhasseryne Orias SanchezNo ratings yet
- Congenital Heart Disease EtiologyDocument8 pagesCongenital Heart Disease EtiologykudzaimuregidubeNo ratings yet
- Transposition of Great ArteriesDocument21 pagesTransposition of Great ArteriesAlusio Navosailagi VUNIIVI100% (1)
- Heart Diseases3Document33 pagesHeart Diseases3api-3699361No ratings yet
- 41 HLHS Ma AaDocument14 pages41 HLHS Ma AaVictor PazNo ratings yet
- Tetralogy of FallotDocument3 pagesTetralogy of FallotMiLody NajeNo ratings yet
- Cayanotic Heart DiseaseDocument28 pagesCayanotic Heart DiseasesivanathanNo ratings yet
- Tetralogy of FallotDocument5 pagesTetralogy of FallotCharity OaniaNo ratings yet
- Physiology Congenital: of DiseaseDocument5 pagesPhysiology Congenital: of DiseaseFirah Triple'sNo ratings yet
- TiKa TaKa PediatricsDocument86 pagesTiKa TaKa PediatricsEmad MerganNo ratings yet
- patho1Document153 pagespatho1ademabdellaaleNo ratings yet
- What is Tetralogy of FallotDocument18 pagesWhat is Tetralogy of FallotIyah Bu-ucanNo ratings yet
- Essential Echocardiography for Congenital Heart DiseaseDocument21 pagesEssential Echocardiography for Congenital Heart Diseasedgina8800No ratings yet
- Anatomic Pathology HandbookDocument166 pagesAnatomic Pathology HandbookNeelu PrasharNo ratings yet
- Minggu 2 LP ASDDocument15 pagesMinggu 2 LP ASDMuhammad PanduNo ratings yet
- Tetralogy of FallotDocument8 pagesTetralogy of FallotHillary Faye FernandezNo ratings yet
- Ciano Tico IDocument14 pagesCiano Tico ILilik FitrianaNo ratings yet
- Understanding Tetralogy of Fallot: Causes, Symptoms and TreatmentDocument7 pagesUnderstanding Tetralogy of Fallot: Causes, Symptoms and TreatmentJoanna Bee Rose MagyawiNo ratings yet
- Transposition of The Great Arteries Article PDFDocument10 pagesTransposition of The Great Arteries Article PDFMYMANo ratings yet
- PdaDocument14 pagesPdaGeorgianaTudorNo ratings yet
- Truncus Arteriosus: Rare Heart Defect With Single Arterial TrunkDocument19 pagesTruncus Arteriosus: Rare Heart Defect With Single Arterial TrunkHijaz Al-YamanNo ratings yet
- Case Report: Atrial Septal Defect and Ventricular Septal DefectDocument28 pagesCase Report: Atrial Septal Defect and Ventricular Septal DefectDian Primadia PutriNo ratings yet
- Congenital Heart Disease Is One or More Problems With The Heart's Structure ThatDocument37 pagesCongenital Heart Disease Is One or More Problems With The Heart's Structure Thatneelimawanker chinnariNo ratings yet
- Truncus ArteriosusDocument9 pagesTruncus ArteriosusAkang KurniawanNo ratings yet
- Congenital Heart Diseases: TopicsDocument19 pagesCongenital Heart Diseases: TopicsMaheen SyedNo ratings yet
- Atrial Septal Defects ( ASD)Document30 pagesAtrial Septal Defects ( ASD)wissam salimNo ratings yet
- Tetralogy of Fallot, Agarwala 2017Document5 pagesTetralogy of Fallot, Agarwala 2017rinayondaNo ratings yet
- Common Heart DiseasesDocument5 pagesCommon Heart DiseasesShams MosaadNo ratings yet
- Test Bank For Human Diseases 8th Edition ZelmanDocument22 pagesTest Bank For Human Diseases 8th Edition Zelmandenisedanielsbkgqyzmtr100% (29)
- Presentstion No-1Document15 pagesPresentstion No-1Lally LukeNo ratings yet
- Tetralogy of Fallot: Cyanotic Congenital Heart DiseaseDocument31 pagesTetralogy of Fallot: Cyanotic Congenital Heart DiseaseJabir EspinaNo ratings yet
- Convert CSVDocument2,498 pagesConvert CSVSunnt BandiNo ratings yet
- Coarctation of AortaDocument5 pagesCoarctation of AortaktNo ratings yet
- N PDFDocument136 pagesN PDFDr-Jahanzaib GondalNo ratings yet
- Directions To Candidates Paper 1 - MedicalDocument29 pagesDirections To Candidates Paper 1 - MedicalMedicEdNo ratings yet
- PreviewpdfDocument235 pagesPreviewpdfchubura_je_rajNo ratings yet
- Noonan Syndrome - Symptoms, Causes, Treatment NORDDocument24 pagesNoonan Syndrome - Symptoms, Causes, Treatment NORDSerik AdaiNo ratings yet
- 1.case Presentation CHDDocument23 pages1.case Presentation CHDDHARM MEENANo ratings yet
- Perioperative Evaluation and Treatment in PediatricsDocument86 pagesPerioperative Evaluation and Treatment in Pediatricsmedpedshospitalist100% (2)
- Heart Murmurs: What Is A Heart Murmur?Document2 pagesHeart Murmurs: What Is A Heart Murmur?Stefan Codrin CriclevitzNo ratings yet
- Mejoras Primera Entrega y Método e InstrumentoDocument16 pagesMejoras Primera Entrega y Método e InstrumentoANDREA CAROLINA NIÑO QUINTERONo ratings yet
- Antibiotics: Use and Misuse in Pediatric Dentistry - A ReviewDocument23 pagesAntibiotics: Use and Misuse in Pediatric Dentistry - A ReviewKarishma SirimullaNo ratings yet
- IAS AneurysmDocument13 pagesIAS AneurysmE'len HamidahNo ratings yet
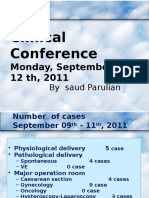
- SAUD VSD KonklinDocument91 pagesSAUD VSD KonklinDedy Tesna AmijayaNo ratings yet
- Truncus ArteriosusDocument20 pagesTruncus ArteriosusjustinahorroNo ratings yet
- Common Unit Conversion GuideDocument28 pagesCommon Unit Conversion GuideRazrin RazakNo ratings yet
- Embryology of Spinal CordDocument5 pagesEmbryology of Spinal CordSteven MatualiNo ratings yet
- مهم للمزاولةDocument13 pagesمهم للمزاولةbelal nurseNo ratings yet