Professional Documents
Culture Documents
A Competing Risk Approach With Censoring To Estimate The Probability of Death of HIV/AIDS Patients On Antiretroviral Therapy in The Presence of Covariates
Uploaded by
SEP-PublisherOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Competing Risk Approach With Censoring To Estimate The Probability of Death of HIV/AIDS Patients On Antiretroviral Therapy in The Presence of Covariates
Uploaded by
SEP-PublisherCopyright:
Available Formats
Statistics Research Letters (SRL) Volume 3, 2014
www.srl-journal.org
A Competing Risk Approach with Censoring
to Estimate the Probability of Death of
HIV/AIDS Patients on Antiretroviral Therapy
in the Presence of Covariates
Gurprit Grover1, Prafulla Kumar Swain1*, Vajala Ravi
Department of Statistics, University of Delhi, Delhi-110007, India
prafulla86@gmail.com
Abstract
Tuberculosis, the most common opportunistic infection and
leading cause of death among HIV/AIDS infected
individuals in India, greatly influences the morbidity and
mortality of HIV infections. But the widespread use of
Antiretroviral Therapy (ART) has led to remarkably decrease
in the death rates of HIV/AIDS infected patients. The main
objective of this paper is to estimate probability of death of
HIV/AIDS patients on ART due to Opportunistic infection
Tuberculosis in the presence of various competing risks viz,
Diarrhea, Other infections and Unknown/unspecified cause.
Also we have assessed the effects of prognostic factors on
HIV/AIDS cause specific deaths, compared with the death
from other competing risks, and exploring leading cause of
death among HIV/AIDS patients on Antiretroviral Therapy.
Cause specific hazard, subdistribution hazard model and
flexible parametric proportional hazard model have been
used to assess the effect of covariates on cumulative
incidence function (CIF).
Keywords
AIDS; Competing Risks; Cumulative Incidence Function;
Subdistribution Hazard and Flexible Parametric Model
Introduction
The wider access to Antiretroviral Therapy (ART) has
resulted in a decline of the number of people dying
due to AIDS related causes (NACO report 2010-11). It
has greatly changed the mortality profile for HIV
infected individuals. In this changing scenario, death
of an HIV/AIDS patient is caused by any opportunistic
infection prevalent in the population but not by virus
itself. As we know AIDS is a syndrome which breaks
down the immune system of the body and becomes
susceptible to wide variety of opportunistic infections.
It is known that Tuberculosis is the most pronounced
opportunistic
infection
among
HIV
infected
individuals in India (Grover et al. 2012, Takalkar et
al.2012, Srirangaraj and Venkatesha 2011, Grover and
Shivraj 2004). Tuberculosis accounts for 20-25 percent
of death among people living with HIV/AIDS (NACO
report 2010-11). The main focus of this paper is on
estimating the probability of death of AIDS patients on
ART due to the opportunistic infection Tuberculosis
(TB), in the presence of other competing risks viz.
Diarrhea, Other infection and unknown causes.
Lau et al. (2007) used a competing risk model to
quantify the cause specific mortality of non-AIDS as
well as AIDS related causes before and after HAART.
Afolabi et al.(2012) linked migration with AIDS/TB by
investigating how the migrants risk of dying from
other causes compete with their risk of dying of
AIDS/TB. Bonnet et al.(2005) compared patients who
died of other causes with patients who died with
opportunistic infections in the HAART era in France.
Yan et al.(2000), Del Amo et al.(2006), Tahira P. Alves
et al. (2010), Pacheco et al. (2010) have used competing
risk theory to model HIV/AIDS population.
Grover et al.(2012) estimated the probability of death
of AIDS patients in the presence of competing risks for
complete data and in the absence of covariates. This
work is a further extension of their work by
considering censoring and covariates. Cumulative
Incidence Function (CIF) has been used to estimate
probability of death and cause specific hazard,
subdistribution hazard and flexible parametric model
have been applied to assess the covariate effects on CIF.
Competing risks are frequently encountered in
survival analysis. It arises when a failure can result
from one of several causes and one cause precludes the
others. It alters the probability of occurrence of other
event. For example, a HIV/AIDS patient who is at risk
of dying from tuberculosis, he/she is also at risk of
www.srl-journal.org
dying due to causes like diarrhea or other infection.
Several authors have attempted to study competing
risks theory and the estimation of cumulative
incidence function of an event of interest. Prentice et al.
(1978) discussed likelihood inference to examine the
effect of prognostic factors on the event of interest in
the presence of competing risk events. Pepe and More
(1993) described various probability models for
summarizing competing risk data. Recently Klein and
Moeschberger (2003), Pintilie (2006, 2011), Klein (2010)
reviewed some basic statistical methods for analyzing
the competing risk data.
In competing risk scenario, it has been evinced that the
complement of the non parametric Kaplan-Meier
estimate (1-KM) fails as an estimate of cumulative
probability of failure due to the cause of event of
interest, since the Kaplan-Meier estimate depends on
the hazard of failure from the event of interest alone,
without taking into account other causes of failure
( Pepe and More 1993, Lin 1997, Gooley et al. 1999).
The cumulative Incidence Function (CIF), which
partitions the probability of failure into probability
corresponding to each competing event at any point in
time, the overall (1-KM) estimate is equal to the sum of
the CIFs for each type of event. The cumulative
incidence function will give the proportion of patients
at any time who have died from a particular cause.
There are two important approaches widely used to
assess the covariate effects on a cumulative incidence
function i.e Cause specific hazard and Subdistribution
hazard model. The cause specific hazard measures the
instantaneous failure rate due to one cause at a time. In
cause specific hazard model, the effect of the
investigated covariates on the other competing risk
event(s) is ignored. So there is no direct connection
between the regression coefficients and incidence
events, and also this approach assumes that the
competing events are independent to each other and is
difficult to evaluate the covariate effect on the
incidence function directly.
Fine and Gray (1999) developed a Subdistribution
hazard model approach; in this approach the covariate
effects on the cumulative failure probability due to one
risk can be measured directly, in the presence of other
competing risks. In this model, the regression
coefficients are monotonously linked to the cumulative
incidence function and occurrence of competing events
has an influence on the coefficients (Haller et al. 2013).
Recently, the flexible parametric model is used as an
alternative to Cox proportional hazard model
Statistics Research Letters (SRL) Volume 3, 2014
especially if the proportionality assumption is violated.
The parametric models have the advantage of directly
estimating cause specific hazard rates in the model as
well as handling non proportional hazards with ease.
Royston and Parmar (2002) developed the use of the
flexible parametric model to obtain both the cause
specific hazards and the cumulative incidence function
in a competing risks framework. The smooth estimates
for cause specific hazard and CIF can be obtained by
using the restricted cubic splines on log cumulative
hazard.
Material and Methods
Methods Used:
Cumulative Incidence Function (CIF) has been used to
estimate probability of death due to competing risk as
an alternative to 1-Kaplan-Meier estimator. Cause
specific hazard model and subdistribution hazard
model have been used in this competing risk analysis
to assess the covariate effects on cause specific hazard.
Also flexible parametric hazard model has been
employed to determine the significance of covariates.
The results obtained from these three methods are then
compared.
Cumulative Incidence Function (CIF):
The cumulative incidence function Fk(t), is probability
of failure due to cause k before a given time t. It is
defined as
Fk(t) = P( T t, K= k )
(1.1)
Where T and K are the random variables representing
the time to the first observed event and the cause of
event respectively. In the absence of competing risks,
the cumulative incidence function is equal to 1- S(t),
where S(t) is the survival function, which can be
derived by the Kaplan- Meier estimator. In the
presence of competing risks the cumulative incidence
function for cause k can be estimated as
=:
Fk(t)
(1.2)
() (1)
where S(t) is the estimator for the overall survivor
function at time t including all types of event and ti
denotes the ith ordered event time. k is the cause
specific hazard rate, which can be estimated by
(ti) =
where dki is the number of deaths from cause k at time
ti and ni is the risk set at time ti , i.e. the number of
patients who are not censored and have not died from
any cause up to time ti.
In other words, the cumulative incidence function Fk(t),
Statistics Research Letters (SRL) Volume 3, 2014
www.srl-journal.org
gives the proportion of patients at time t who have
died from cause k accounting for the fact that patient
can die from other causes as well
Fk(t) = 0 () ()
(1.3)
hk is the cause specific hazard, X is the covariate vector
and S is the overall survival function. Here we assume
that the event of interest is death of AIDS patient due
to the opportunistic infection TB (indexed 1), in the
presence of competing risks diarrhea, other infection
and unknown causes indexed as 2, 3 and 4 respectively,
the model is depicted in figure 1.
Deaths due to Competing Risks
Tuberculosis
Diarrhea
Other Infections
Unknown/Unspecified
HIV/AIDS
Patients on
ART
FIGURE 1 COMPETING RISKS MODEL FOR HIV/AIDS PATIENTS
ON ART.
Cause Specific Hazard:
Without loss of generality, a cause specific hazard
function hk(t) at time t, (Prentice et al.,1978) is defined
as
hk(t) = lim0
The overall hazard of failure is the sum of all the cause
specific hazards. i.e h(t) = hk(t)
In other words hk(t: x) the instantaneous failure rate
due to cause k at time t given X, where X is the
covariate vector, is given by
hk(t: x) = h0k(t) exp(=1 ) k= 1, 2, 3, 4 (1.4)
The corresponding partial likelihood function is given
by
exp(k Xj)
() exp(k X(l) )
Fine and Gray (1999) proposed a regression model that
directly links the regression coefficients with the
cumulative incidence function in a competing risk
analysis. The subdistribution hazard hks(t), is the
instantaneous risk of dying from a particular cause k
in an infinitesimal small time interval t given that the
subject experienced no event until time t or
experienced an event other than k before time t;
hsk(t)=lim0
=
f*k(t) =
()
( <+ ,= > ( ))
1 ()
Fk(t)
()
()+ ()
(1.6)
(1.5)
Where R(tjk) denotes the risk set at time tj in the
presence of cause k.
A cause specific hazard model estimates the covariates
effect on the instantaneous probability of death from a
specific cause k, and it treats death from competing
risks as censored observations. Since the cumulative
incidence function for cause k depends not only on the
hazard associated with cause k, but also on
are the subdistribution cumulative
incidence, subsurvivor, and subdensity function
respectively. Since the cause specific hazard approach
does not reflect the covariate effects on the cumulative
incidence function. Therefore the subdistribution
hazard due to cause k is given by
h*sk(t/X)=
k= 1, 2, 3, 4
Where T be the survival time and K be the cause of
death (k=1, 2, 3, 4 ), indexes TB (as the event of
interest), Diarrhea, Other Infections and Unknown
causes
L(k)=
Subdistribution Hazard Model:
where F*k(t) = P(T < t, K=k), S*k(t) = P( T > t, K=k) and
Alive/ Censored
( <+ , = )
the hazards of all other causes. Therefore the
interpretation of results obtained by this model needs
utmost care and cannot extend to cumulative incidence
function.
(1(/))
=>F*k(t/X)=1-exp[-0 () ]
(1.7)
It is shown that there is a direct link between subdistribution hazard and Cumulative Incidence
Function, from which the proportional subdistribution hazard model is then
h*k(t/ x) = h*0k(t) exp('kX)
(1.8)
where h (t) denotes the subdistribution baseline
hazard function.
*0k
This method takes into account other events and does
not make any assumptions about their independence
between the event time and censoring distribution.
Both cause specific hazard and subdistribution hazard
model use partial likelihood approaches for estimation
of parameters. However, the difference between cause
specific hazard and subdistribution hazard model lies
in the risk set (Lau et al.2009). For cause specific
hazard, hk(t/ x), the risk set decreases at each time
point at which there is an event from another cause.
For the subdistribution hazard, h*k(t/ x) , a patient who
has an event from another cause remains in the risk set.
Flexible Parametric Proportional Hazard Model:
The flexible parametric model was first proposed by
Royston and Parmar (2002) for use with censored
9
www.srl-journal.org
Statistics Research Letters (SRL) Volume 3, 2014
survival data. Since Weibull model is the most
common parametric survival model having both
proportional hazards as well as accelerated failure
time model interpretations, therefore we have
considered the log cumulative hazard form of a
Weibull model. For a Weibull distribution the survival
function is
S(t) = exp( )
(1.9)
Transforming this to the log cumulative hazard scale,
we get
ln H(t)= ln[-ln(S(t))]
ln H(t)= ln() + ln(t)
This is a linear function of log time, now adding
covariates X in this model, we have
ln[H(t/X)] = ln() + ln(t) +X
(1.10)
Where are the covariate coefficients, however, rather
than assuming linearity with ln(t), apply flexible
parametric approach which uses the restricted cubic
splines for ln(t), (Hinchliffe and Lambert (2013)).
The baseline log cumulative hazard in a proportional
hazard model incorporates the restricted cubic spline
function of S( ln(t)/ , n0) with knot location n0, and
covariates X, and can be written as
ln[ H(t/X)] = S( ln(t)/ , n0 ) +X
(1.11)
Covariate effects can be interpreted as log hazard
ratios under the assumption of proportional hazards.
The survival and hazard function can be obtained
through a transformation of the model parameters.
S(t/ X) = exp (- exp(ln [H(t/X)] ))
h(t/X)=
S( ln(t)/ ,n0 )
exp(ln[H(t/X)])
(1.12)
One of the main advantages of the flexible parametric
approach is the ease with which time dependent
effects can be fitted. A detailed description of restricted
cubic splines is explained in appendix.
Data Sources:
The study population included 1101 adult (>18 years
age) HIV/AIDS patients who were undergoing
Antiretroviral Therapy in the ART centre of Dr. Ram
Manohar Lohia Hospital, New Delhi, India, during the
period April 2004 to November 2009, and were
followed up through the ART routine register records
till December 2010. Out of 1101 patients 119 patients
died at the end of the study. Since the outcome
variable of interest is the cause of death therefore data
related to death due to various specific causes viz,
Tuberculosis, Diarrhea, Other infections and
Unknown/Unspecified cause were collected. Other
10
infections include hepatitis B, hepatitis C, Oral
Candidiasis, Pneumocystis Carinii Pneumonia (PCP),
Herpes Zoster etc. And the other baseline information
such as age, sex, last available CD4 count, mode of
transmission, weight and hemoglobin were also noted
down. These variables were entered into the model as
categorical variablesAge (35yrs/>35yrs), Sex (male/
female), CD4 cell count (350cells/mm3/>350 cells/mm3),
MOT (sexual/others) and continuous variablesHemoglobin and Weight. The category sexual of the
covariate MOT included both Homosexual and
Heterosexual transmissions and the category other
included Injecting Drug Users (IDU) and Unknowns.
Patients who were alive at the end of the study period,
were treated as right censored. The software packages
survival/cmprsk/timereg in R and STATA (version 12.0)
have been used to perform the statistical analyses.
TABLE 1 DESCRIPTIVE STATISTICS
Variables
Age
Sex
Mode of
Transmission
(MOT)
CD4+ cell
Status
Category (Code)
35 years (0)
< 35 years (1)
Male (0)
Female (1)
N=1101
403
698
732
369
Percent
36.6
63.4
66.5
33.5
Sexual (1)
767
69.7
Others (0)
350 (0)
<350 (1)
Alive (0)
Death (1)
334
526
575
982
119
30.3
47.7
52.3
89.2
10.8
Opportunistic
Tuberculosis (1)
39
Infections
Diarrhea (2)
24
Other Infections (3)
29
Unknown /Unspecified (4)
27
Hemoglobin
11.001.88 Mean SD
Weight
50.2310.67 Mean SD
Age (in years)
34.608.14 Mean SD
CD4+ count
354.80197.10 Mean SD
32.78
20.17
24.37
22.68
Result
Table 1 contains the descriptive statistics of the study,
out of 1101 patients, 66.5% were males and 33.5% were
females. The majority of patients 63.4% were less than
35 years at the time of enrolment. The predominant
mode of HIV transmission was sexual route, which
included both homo- and hetro- sexual transmission,
767 (69.7%) were sexually transmitted patients and the
remaining 334 patents were transmitted by others
mode. 575 (52.3%) patients had CD4 cell count less
than 350 cells/mm3. The mean age at diagnosis was
34.60( 8.14) years whereas the mean CD4 cell count of
last available record was 354.80 ( 197.10) cells/mm3.
At the end of study period 119 (10.8%) patients died.
Statistics Research Letters (SRL) Volume 3, 2014
www.srl-journal.org
The majority of deaths occurred due to tuberculosis,
accounting for 32.78% of total deaths, followed by
other infection 24.37%, unknown cause 22.68% and
diarrhea 20.17%. The mean CD4 count of patients who
died due to cause tuberculosis, diarrhea, other infection
and unknown cause were 96.83(76.48), 93.78(76.75),
96.54(77.70) and 96.52(77.40) cells/mm3 respectively.
We have applied cause specific hazard and
subdistribution hazard model to obtain the cumulative
incidence of death due to causes tuberculosis, diarrhea,
other infections and unknown causes. The hazard
ratios are given in Table 2. The result shows that the
two models are quite close to each other but different
for cause specific deaths. Both cause specific and
subdistribution hazard model show that the
prognostic factors sex, CD4 count, hemoglobin and
weight are statistically significant (P-value <0.000) for
patients who have died due to cause tuberculosis.
Males had higher risk of death due to tuberculosis as
compared to their female counterpart. Patients with
CD4 count less than 350 cells/mm3 had 7.57 and 6.18
times more hazard of death due to tuberculosis as
compared to patients with CD4 count more than 350
cells/mm3 in the cause specific and subdistribution
hazard models respectively, [ HR= 7.57, 95% CI (2.67,
21.41), HR= 6.18, 95% CI(2.16, 17.63)].
CD4 count, weight and hemoglobin have a significant
effect on the patients who died due to diarrhea. The
lower CD4 count patients whose death occurred due to
diarrhea had 3.38 times higher hazard than those who
had a CD4 count less than 350 cells/mm3. According to
cause specific and subdistribution hazard model an
increase in weight per kg is found to be strongly
associated with the survival of HIV/AIDS patients.
Hemoglobin is found to be a significant factor for the
probability of death due to any cause in the cause
specific model (P-value <0.000), however, it is not
found to be significant in subdistribution model for the
probability of death due to cause diarrhea and other
infections. This is due to the fact that the effect of a
covariate on the cumulative incidence for one cause
does not depend only on the effect of the covariate on
the cause specific hazard for the corresponding cause,
but also on the respective effect on the cause specific
hazard functions for all other causes as well as on the
baseline hazard functions. CD4 count is also found to
be a significant marker for the patients whose cause of
death is unknown/ unspecified.
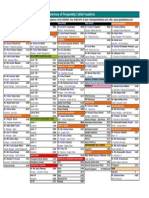
TABLE 2 RESULTS OF CAUSE SPECIFIC HAZARD MODEL AND SUBDISTRIBUTION HAZARD MODEL
Parameters
Tuberculosis
Age
-0.152
Sex
-1.999
CD4 cell count
2.024
Mode of Transmission
0.422
Hemoglobin
-0.357
Weight
-0.088
Diarrhea
Age
-0.382
Sex
-0.930
CD4 cell count
1.407
Mode of Transmission
0.252
Hemoglobin
-0.242
Weight
-0.138
Other Infections
Age
-0.285
Sex
-1.006
CD4 cell count
1.660
Mode of Transmission
0.330
Hemoglobin
-0.245
Weight
-0.068
Unknown/unspecified
Age
-0.291
Sex
-0.743
CD4 cell count
2.032
Mode of Transmission -0.101
Hemoglobin
-0.330
Weight
-0.039
Cause specific Hazard Model
Std.Error
HR
95% CI
P-value
Subdistribution Hazard Model
Std.Error
HR
95% CI
P-value
0.332
0.493
0.530
0.398
0.086
0.019
0.858
0.135
7.575
1.525
0.699
0.915
(0.45, 1.64)
(0.05, 0.35)
(2.67, 21.41)
(0.69, 3.33)
(0.59, 0.82)
(0.88, 0.95)
0.647
<0.000
<0.000
0.289
<0.000
<0.000
-0.122
-1.883
1.821
0.442
-0.303
-0.073
0.329
0.506
0.535
0.404
0.087
0.021
0.885
0.152
6.180
1.555
0.738
0.930
(0.46,1.68)
(0.05,0.41)
(2.16,17.63)
(0.70,3.43)
(0.62,0.87)
(0.89,0.97)
0.710
<0.000
<0.000
0.270
<0.000
<0.000
0.420
0.452
0.554
0.505
0.108
0.026
0.681
0.394
4.086
1.287
0.784
0.870
(0.29,1.55)
(0.16,0.95)
(1.37,12.12)
(0.47,3.46)
(0.63,0.97)
(0.82,0.91)
0.362
<0.039
<0.011
0.616
<0.025
<0.000
-0.406
-0.761
1.220
0.248
-0.165
-0.127
0.428
0.434
0.560
0.510
0.108
0.022
0.666
0.467
3.389
1.282
0.848
0.880
(0.28,1.54)
(0.19,1.09)
(1.13,10.16)
(0.47,3.48)
(0.68,1.04)
(0.84,0.92)
0.340
0.080
<0.029
0.630
0.130
<0.000
0.380
0.455
0.541
0.460
0.099
0.022
0.751
0.365
5.263
1.391
0.782
0.933
(0.35,1.58)
(0.14,0.89)
(1.82,15.21)
(0.56,3.43)
(0.64,0.95)
(0.89,0.97)
0.452
<0.027
<0.002
0.473
<0.013
<0.002
-0.289
-0.863
1.562
0.324
-0.206
-0.060
0.392
0.426
0.542
0.474
0.113
0.027
0.749
0.422
4.768
1.384
0.813
0.942
(0.34,1.61)
(0.18,0.97)
(1.62,13.97)
(0.54,3.50)
(0.65,1.01)
(0.89,0.99)
0.460
<0.043
<0.004
0.490
0.070
<0.028
0.395
0.463
0.614
0.425
0.103
0.021
0.747
0.475
7.634
0.903
0.718
0.961
(0.34,1.62)
(0.19,1.18)
(2.29,25.44)
(0.39,2.07)
(0.58,0.87)
(0.92,1.01)
0.461
0.109
<0.000
0.811
<0.001
0.074
-0.226
-0.571
1.874
-0.087
-0.261
-0.028
0.381
0.413
0.603
0.433
0.090
0.019
0.797
0.565
6.517
0.916
0.770
0.972
(0.37,1.68)
(0.25,1.27)
(1.99,21.26)
(0.39,2.14)
(0.64,0.91)
(0.93,1.01)
0.550
0.170
<0.001
0.840
<0.003
0.140
11
www.srl-journal.org
Statistics Research Letters (SRL) Volume 3, 2014
TABLE 3 RESULTS OF FLEXIBLE PARAMETRIC PROPORTIONAL HAZARD MODEL
Parameters
Tuberculosis
Age
Sex
CD4 cell count
Mode of Transmission
Hemoglobin
Weight
Diarrhea
Age
Sex
CD4 cell count
Mode of Transmission
Hemoglobin
Weight
Other Infections
Age
Sex
CD4 cell count
Mode of Transmission
Hemoglobin
Weight
Unknown/unspecified
Age
Sex
CD4 cell count
Mode of Transmission
Hemoglobin
Weight
Flexible Parametric Proportional Hazard Model
HR
95% CI
Std.Error
P-value
-0.209
-2.030
2.080
0.556
-0.372
-0.096
0.301
0.473
0.530
0.396
0.085
0.019
0.811
0.131
8.004
1.743
0.689
0.908
(0.42, 1.56)
(0.04, 0.34)
(2.82, 22.64)
(0.79, 3.82)
(0.58, 0.81)
(0.87, 0.95)
0.531
<0.000
<0.000
0.165
<0.000
<0.000
-0.453
-0.968
1.480
0.385
-0.272
-0.144
0.401
0.432
0.544
0.504
0.081
0.020
0.635
0.379
4.392
1.469
0.762
0.865
(0.27, 1.45)
(0.15, 0.92)
(1.47, 12.93)
(0.54, 3.97)
(0.61, 0.94)
(0.82, 0.91)
0.284
<0.030
<0.007
0.448
<0.013
<0.000
-0.542
-3.310
4.012
2.060
-0.643
-0.153
0.378
0.412
0.540
0.455
0.082
0.011
0.581
0.036
55.257
7.845
0.525
0.858
(0.21, 1.43)
(0.01, 0.47)
(12.89, 144.23)
(0.97, 24.89)
(0.36, 0.95)
(0.46, 0.98)
0.401
<0.024
<0.004
0.330
<0.009
<0.002
-0.324
-0.775
2.060
0.019
-0.346
-0.045
0.380
0.412
0.601
0.412
0.080
0.018
0.723
0.461
7.845
1.019
0.707
0.953
(0.33, 1.57)
(0.18, 1.14)
(2.35, 26.04)
(0.44, 2.35)
(0.57, 0.86)
(0.91, 0.99)
0.413
0.094
<0.000
0.964
<0.000
<0.042
Number of Deaths
Deaths due to various opportunistic infections
45
40
35
30
25
20
15
10
5
0
FIGURE 2 NUMBER OF DEATHS OCCURRED DUE TO VARIOUS OPPORTUNISTIC INFECTIONS
Table 3 shows the hazard ratios and its confidence
interval obtained from flexible parametric hazard
model. The estimates obtained by flexible parametric
hazards model are similar to the cause specific and
subdistribution hazards model. Male shows an
increased risk of death due to tuberculosis, diarrhea
and other infections as compared to their female
12
counterparts. CD4 count, hemoglobin and weight are
found to be statistically significant factors for all
specified risks of death. Tuberculosis shows a higher
incidence among the causes of death of HIV/AIDS
patients (shown in figure 3). Figure 5 depicts that
males have a slightly higher incidence of death than
females irrespective of causes of death, and patients with
Statistics Research Letters (SRL) Volume 3, 2014
www.srl-journal.org
Cumulative Incidence Function
0.04
0.035
0.03
0.025
Tuberculosis
0.02
Diarrhea
0.015
Other Infections
0.01
Unknown
0.005
0
0
20
40
60
Time in Month
FIGURE 3 CUMULATIVE INCIDENCE FUNCTIONS FOR TUBERCULOSIS, DIARRHEA, OTHER INFECTIONS AND UNKNOWN
CAUSE OF DEATH OF HIV/AIDS PATIENTS
Diarrhea
1.0
1.0
Tuberculosis
0.8
CD4>350 cells/mm3
CD4<= 350cells/mm3
0.0
0.0
0.2
0.2
0.4
0.4
CIF
CIF
0.6
0.6
0.8
CD4>350 cells/mm3
CD4<= 350cells/mm3
10
20
30
40
50
60
70
10
20
30
Months
50
60
70
50
60
70
Months
Unknown/Unspecified cause
1.0
1.0
Other Infections
40
0.8
CD4>350 cells/mm3
CD4<= 350cells/mm3
0.0
0.0
0.2
0.2
0.4
0.4
CIF
CIF
0.6
0.6
0.8
CD4>350 cells/mm3
CD4<= 350cells/mm3
10
20
30
40
Months
50
60
70
10
20
30
40
Months
FIGURE 4 ESTIMATED CUMULATIVE INCIDENCE FUNCTIONS FOR TUBERCULOSIS, DIARRHEA, OTHER INFECTIONS AND
UNKNOWN/ UNSPECIFIED CAUSES OF DEATHS OF HIV/AIDS PATIENTS BY CD4 CELL COUNT USING CAUSE
SPECIFIC HAZARD MODELS.
13
www.srl-journal.org
Statistics Research Letters (SRL) Volume 3, 2014
Diarrhea
1.0
1.0
Tuberculosis
0.6
0.8
Male
Female
0.4
0.0
0.0
0.2
0.2
0.4
CIF
CIF
0.6
0.8
Male
Female
10
20
30
40
50
60
70
10
20
40
30
Months
50
60
70
50
60
70
Months
Unknown/Unspecified cause
1.0
1.0
Other Infections
0.8
Male
Female
0.0
0.0
0.2
0.2
0.4
0.4
CIF
CIF
0.6
0.6
0.8
Male
Female
10
20
30
40
50
60
70
Months
10
20
30
40
Months
FIGURE 5 ESTIMATED CUMULATIVE INCIDENCE FUNCTIONS FOR TUBERCULOSIS, DIARRHEA, OTHER INFECTIONS AND
UNKNOWN/ UNSPECIFIED CAUSES OF DEATHS OF HIV/AIDS PATIENTS BY SEX USING CAUSE SPECIFIC HAZARD MODELS.
CD4 less than 350 cells/mm3 have also a higher
incidence of death than the patients with CD4 greater
than or equal to 350 cells/mm3 (shown in figure 4). We
have checked the proportionality assumption by using
Schoenfeld residuals (not shown here), and it indicates
no evidence against the departure from this
assumption for all specific causes of death.
Discussion
The result demonstrates the differences in estimates
obtained by the cause specific, subdistribution hazard
model and flexible parametric model. Our analysis
shows that the three models yield similar results with
regard to the effect of covariates. The most common
opportunistic infection cause of death among
HIV/AIDS patients is found to be tuberculosis, which
is corroborated with earlier studies of India (Grover et
14
al. 2012, Takalkar et al.2012, Srirangaraj and
Venkatesha 2011, and Ghate et al,. 2009). The effects of
prognostic factors have been assessed using cause
specific hazard model, subdistribution hazard model
and flexible parametric hazard model. CD4 cells count
is found to be an important marker for HIV/AIDS
patients by all the methods. Over six times higher
cause specific and sudistribution hazard ratios for
tuberculosis deaths are found for patients with lower
CD4 cell count compared to the patients with higher
CD4 cell count, whereas hazard ratios for diarrhea and
other infections deaths are comparatively smaller. This
effect can also be seen in the results of flexible
parametric model approach. Consistent with literature
of Ghate et al.2009, the risk of developing tuberculosis
and oral candidiasis is more than 10 times greater at
CD4 count less than 200 cells/mm3 as compared to CD4
Statistics Research Letters (SRL) Volume 3, 2014
count of more than 350/mm3. The results of cause
specific and sudistribution hazard model are found to
be similar. However, the factor hemoglobin is found to
be significant for diarrhea and other infections death
by cause specific hazard model but non-significant in
subdistribution hazard analysis, which is consistent
with the findings of Beyersmann et al,.2007.
As stated by Haller et al., 2013; these results should be
interpreted carefully, because in the cause specific
hazard model, the effect of the competing event(s) is
not considered, so a higher cause specific hazard is
necessarily translated into a higher cumulative
incidence function. In the subdistribution hazard
model, the covariates are directly linked to the
cumulative incidence function of the event of interest.
Hence it is possible that an observed effect of a
covariate on the event of interest is caused by an effect
on a competing event, which might lead to biological
implausible results. Although the three models show
similar hazard ratios with respect to covariates, but the
choice of model should be driven by the scientific
question. Our findings reveal that the flexible
parametric approach has a slightly lower standard
error than the cause specific and subdistribution
hazard models. So the flexible parametric model is
recommended as a viable approach in competing risk
analysis. A sensitivity analysis is required for further
conformity.
Therefore the implication of our finding might be
prudent on the part of treatment and care providers to
target early detection of opportunistic infection and
prompt action should be taken to reduce morbidity
and improve quality of life of HIV/AIDS infected
people. Emphasis needs to be given to the early
diagnosis and management of tuberculosis in HIV
infected individuals.
There are some limitations in our study; and we have
analyzed only one ART centre data, therefore a strict
generalization of our findings at national level would
require utmost care and further conformity of multi
centric analysis. Another significant drawback is the
independence assumption of competing risks i.e
patients having both tuberculosis and diarrhea are not
included in the study.
ACKNOWLEDGMENTS
This work was supported by grants to first author
under R and D programme of University of Delhi,
India. We thanked the reviewers for their constructive
and valuable comments.
www.srl-journal.org
Appendix
Splines are flexible mathematical functions defined by
piecewise polynomials, with some constraints to
ensure that the overall curve is smooth. The points at
which polynomials join are called knots. In order to
obtain a smooth function the regression splines are
forced to have continuous first and second derivatives.
For restricted cubic splines a further restriction forces
the splines to be linear before the first knot and after
the final knot. A restricted cubic spline function of
S( ln(t)/ , n0 ) with N knots can be fit by creating N-1
derived variables. For knots n0, n1,nN, and
parameters 0, 1, N-1,can be written as
S( ln(t)/ , n0 ) = 0+ 1z1+ 2z2+ + N-1zN-1
The derived variables z1, z2, zN-1 are calculated as
follows
z1 = ln(t)
zj = (ln(t)- nj )+3 - j( ln(t)- n1)+3 (1- j) (ln(t) -nN)+3
1, 2, N-1
where j =
j=
and (u)+ = u if u> 0, 0 otherwise. Thus
a model with N knots for the baseline log cumulative
hazard uses N-1 degrees of freedom.
REFERENCES
Afolabi .S, Bocqier.P, Kahn.K and Collinson.M (2012), A
competing Risk approach to studying AIDS/TB mortality
consequences of migration in rural South Africa, PPA
conference paper.
Beyersmann J, Dettenkofer M, Bertz H, and Schumacher M
(2007), A competing risks analysis of bloodstream
infection
after
stem
cell
transplantation
using
subdistribution hazards and cause specific hazards,
Statistics in Medicine, 26; 5360-5369
Bonnet. F, Lewden C, and May.T et al.(2005), Opportunistic
infections as causes of death in HIV-infected patients in
the HAART era in France. Scand J Infect Dis, 37(6-7); 4827
Del Amo J, Perez-Hoyos S and Moreno A. et al.(2006),
Trends in AIDS and mortality in HIV infected subjects
with hemophilia from 1985 to 2003; the competing risks
for death between AIDS and liver disease,
J Acquir
Immune Defic Syndr , 41(5), 624-31
Fine J.P and Gray R.J(1999), A proportional hazards model
for the subdistribution of a competing Risk, Journal of
the American Statistical Association, 94; 496-509
15
www.srl-journal.org
Statistics Research Letters (SRL) Volume 3, 2014
Ghate M, Despande S, and Tripathy .S et al. (2009), Incidence
of common opportunistic infections in HIV- infected
Med, 16; 901-910
National Aids Control Organization (NACO),
Annual
individuals in Pune, India: analysis by stages of
Report, 2011-12. Available at http://www.nacoom;org
immunosuppression
upload/Publication/Annual%20Report/NACO_AR_Eng%
represented
by
CD4
counts.
International journal of infectious diseases, 13; e1-e8
(Accessed on 8th July 2012).
Gooley T.A, Leisenring W, and Crowley J. et al.(1999),
Pacheco A.G, Tuboi S.H, and May S.B et al.(2010) Temporal
Estimation of failure probabilities in the presence of
changes in causes of death among HIV infected patients
competing risks: new representation of old estimators,
in the HAART era in Rio-de Janeiro, Brazil, 51(5); 624-
Stats in Med, 18(6); 695-706.
630
Grover.G and Shivraj.S.O (2004) Survival pattern of reported
HIV infected individuals in the city of Delhi (India), J
conditional
Commun Dis, 36(2); 83-92.
competing risks failure time data, Stat Med, 12; 737-751
Grover.G, Gadpayle A.K and Varshney M.K (2012), On the
estimation of probability of death of AIDS patients in the
presence of competing risks, Aligarh Journal of Statistics,
32;69-83
Risk regression models an overview, Lifetime Data
Analysis, 19; 33-58
(2006,
2011),
curves
Competing
in
risks;
summarizing
a
practical
perspective, Wiley,
Prentice.R, Kalbfleisch.J and Peterson A. et al. (1978) The
of
risks, Biometrics, 34; 541-554
Royston P and Parmar M .K.B (2002), Flexible parametric
proportional hazards and proportional odds models for
Hinchliffe. S.R and Lambert.P.C (2013), Flexible parametric
modeling
Pintilie.M
probability
analysis of failure times in the presence of competing
Haller B, Schmidt G, and Ulm.K (2013), Applying Competing
cause
specific
hazards
to
estimate
cumulative incidence functions, BMC Medical Research
Methodology, 13.
censored survival data, with application to prognostic
modeling and estimation of treatment effects, Stats Med,
21; 2175-2197
Srirangaraj.S
Klein J.P (2007), Competing risks. WIREs Comput Stat, 2;
333-339
and
Venkatesha.
D.(2011),
Opportunistic
Infections in relation to antiretroviral status among AIDS
patients from south India.Indian J Med Microbiol, 29;
Klein J.P. and Moeschberger M.L.(2003), Survival analysistechniques for censored and truncated data . Springer ,
New York
395-400
Tahira P. Alves, Hulgan T, and Wu.P et al. (2010), Race,
kidney disease progression , and mortality risk in HIV
Lau B, Gange S.J and Moore R.D (2007), Risk of Non-AIDS-
infected persons, Clin J Am Soc Nephrol, 5; 2269-2275
Related Mortality May Exceed Risk of AIDS Related
Takalkar A.A, Saiprasad G.S, Prasad. V.G, Madhekar N.S
Mortality among Individuals Enrolling into Care with
(2012), Study of Opportunistic Infections in HIV
CD4+ Counts greater than 200 cells/mm3 , J Acquir
Seropositive patients Admitted to Community Care
Immune Defic Syndr, 44; 179-187.
Centre (CCC), KIMS Narketpally. Biomedical Research ,
Lau. B, Cole. S.R and Gange.S.J(2009), Competing risk
regression
models
for
epidemiologic data, Am J
Epidemiol, 170; 244-256
Lin DY.(1997), Non parametric inference for cumulative
incidence functions in competing risks studies, Stats in
16
Pepe.M.S and More.M (1993), Kaplan-Meier, marginal or
23(1); 139-142
Yan Y, Moore R.D and Hoover D.R.(2000), Competing risk
adjustment reduces overestimation of opportunistic
infection rates in AIDS, Journal of Clinical Epidemiology,
53;817-822
You might also like
- FWR008Document5 pagesFWR008sreejith2786No ratings yet
- Contact Characteristics of Metallic Materials in Conditions of Heavy Loading by Friction or by Electric CurrentDocument7 pagesContact Characteristics of Metallic Materials in Conditions of Heavy Loading by Friction or by Electric CurrentSEP-PublisherNo ratings yet
- Influence of Aluminum Oxide Nanofibers Reinforcing Polyethylene Coating On The Abrasive WearDocument13 pagesInfluence of Aluminum Oxide Nanofibers Reinforcing Polyethylene Coating On The Abrasive WearSEP-PublisherNo ratings yet
- Improving of Motor and Tractor's Reliability by The Use of Metalorganic Lubricant AdditivesDocument5 pagesImproving of Motor and Tractor's Reliability by The Use of Metalorganic Lubricant AdditivesSEP-PublisherNo ratings yet
- Microstructural Development in Friction Welded Aluminum Alloy With Different Alumina Specimen GeometriesDocument7 pagesMicrostructural Development in Friction Welded Aluminum Alloy With Different Alumina Specimen GeometriesSEP-PublisherNo ratings yet
- Microstructure and Wear Properties of Laser Clad NiCrBSi-MoS2 CoatingDocument5 pagesMicrostructure and Wear Properties of Laser Clad NiCrBSi-MoS2 CoatingSEP-PublisherNo ratings yet
- Effect of Slip Velocity On The Performance of A Magnetic Fluid Based Squeeze Film in Porous Rough Infinitely Long Parallel PlatesDocument11 pagesEffect of Slip Velocity On The Performance of A Magnetic Fluid Based Squeeze Film in Porous Rough Infinitely Long Parallel PlatesSEP-PublisherNo ratings yet
- Experimental Investigation of Friction Coefficient and Wear Rate of Stainless Steel 202 Sliding Against Smooth and Rough Stainless Steel 304 Couter-FacesDocument8 pagesExperimental Investigation of Friction Coefficient and Wear Rate of Stainless Steel 202 Sliding Against Smooth and Rough Stainless Steel 304 Couter-FacesSEP-PublisherNo ratings yet
- Mindfulness and Happiness: The Empirical FoundationDocument7 pagesMindfulness and Happiness: The Empirical FoundationSEP-PublisherNo ratings yet
- Reaction Between Polyol-Esters and Phosphate Esters in The Presence of Metal CarbidesDocument9 pagesReaction Between Polyol-Esters and Phosphate Esters in The Presence of Metal CarbidesSEP-PublisherNo ratings yet
- Device For Checking The Surface Finish of Substrates by Tribometry MethodDocument5 pagesDevice For Checking The Surface Finish of Substrates by Tribometry MethodSEP-PublisherNo ratings yet
- Enhancing Wear Resistance of En45 Spring Steel Using Cryogenic TreatmentDocument6 pagesEnhancing Wear Resistance of En45 Spring Steel Using Cryogenic TreatmentSEP-PublisherNo ratings yet
- Mill's Critique of Bentham's UtilitarianismDocument9 pagesMill's Critique of Bentham's UtilitarianismSEP-PublisherNo ratings yet
- Delightful: The Saturation Spirit Energy DistributionDocument4 pagesDelightful: The Saturation Spirit Energy DistributionSEP-PublisherNo ratings yet
- Quantum Meditation: The Self-Spirit ProjectionDocument8 pagesQuantum Meditation: The Self-Spirit ProjectionSEP-PublisherNo ratings yet
- Enhanced Causation For DesignDocument14 pagesEnhanced Causation For DesignSEP-PublisherNo ratings yet
- Ontology-Based Testing System For Evaluation of Student's KnowledgeDocument8 pagesOntology-Based Testing System For Evaluation of Student's KnowledgeSEP-PublisherNo ratings yet
- Cold Mind: The Released Suffering StabilityDocument3 pagesCold Mind: The Released Suffering StabilitySEP-PublisherNo ratings yet
- Isage: A Virtual Philosopher System For Learning Traditional Chinese PhilosophyDocument8 pagesIsage: A Virtual Philosopher System For Learning Traditional Chinese PhilosophySEP-PublisherNo ratings yet
- Social Conflicts in Virtual Reality of Computer GamesDocument5 pagesSocial Conflicts in Virtual Reality of Computer GamesSEP-PublisherNo ratings yet
- Architectural Images in Buddhist Scriptures, Buddhism Truth and Oriental Spirit WorldDocument5 pagesArchitectural Images in Buddhist Scriptures, Buddhism Truth and Oriental Spirit WorldSEP-PublisherNo ratings yet
- Technological Mediation of Ontologies: The Need For Tools To Help Designers in Materializing EthicsDocument9 pagesTechnological Mediation of Ontologies: The Need For Tools To Help Designers in Materializing EthicsSEP-PublisherNo ratings yet
- A Tentative Study On The View of Marxist Philosophy of Human NatureDocument4 pagesA Tentative Study On The View of Marxist Philosophy of Human NatureSEP-PublisherNo ratings yet
- Legal Distinctions Between Clinical Research and Clinical Investigation:Lessons From A Professional Misconduct TrialDocument4 pagesLegal Distinctions Between Clinical Research and Clinical Investigation:Lessons From A Professional Misconduct TrialSEP-PublisherNo ratings yet
- Metaphysics of AdvertisingDocument10 pagesMetaphysics of AdvertisingSEP-PublisherNo ratings yet
- Computational Fluid Dynamics Based Design of Sump of A Hydraulic Pumping System-CFD Based Design of SumpDocument6 pagesComputational Fluid Dynamics Based Design of Sump of A Hydraulic Pumping System-CFD Based Design of SumpSEP-PublisherNo ratings yet
- Damage Structures Modal Analysis Virtual Flexibility Matrix (VFM) IdentificationDocument10 pagesDamage Structures Modal Analysis Virtual Flexibility Matrix (VFM) IdentificationSEP-PublisherNo ratings yet
- The Effect of Boundary Conditions On The Natural Vibration Characteristics of Deep-Hole Bulkhead GateDocument8 pagesThe Effect of Boundary Conditions On The Natural Vibration Characteristics of Deep-Hole Bulkhead GateSEP-PublisherNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Bio-Tank Guidelines for Indian RailwayDocument51 pagesBio-Tank Guidelines for Indian Railwayravi100% (2)
- Montgomery County Ten Year Comprehensive Water Supply and Sewerage Systems Plan (2003)Document228 pagesMontgomery County Ten Year Comprehensive Water Supply and Sewerage Systems Plan (2003)rebolavNo ratings yet
- General Specifications: Detail ADocument1 pageGeneral Specifications: Detail AJeniel PascualNo ratings yet
- Nursing Diagnosis TemplateDocument6 pagesNursing Diagnosis Templatesdk6972No ratings yet
- Request Baha Alert PPMPDocument3 pagesRequest Baha Alert PPMPLö Räine AñascoNo ratings yet
- Analisis Dampak Reklamasi Teluk Banten Terhadap Kondisi Lingkungan Dan Sosial EkonomiDocument10 pagesAnalisis Dampak Reklamasi Teluk Banten Terhadap Kondisi Lingkungan Dan Sosial EkonomiSYIFA ABIYU SAGITA 08211840000099No ratings yet
- Dimensional Data: For Valves and ActuatorsDocument52 pagesDimensional Data: For Valves and ActuatorsPaulNo ratings yet
- HVDC BasicDocument36 pagesHVDC BasicAshok KumarNo ratings yet
- Antenna LecDocument31 pagesAntenna Lecjosesag518No ratings yet
- New Microsoft Excel WorksheetDocument4 pagesNew Microsoft Excel WorksheetRaheel Neo AhmadNo ratings yet
- PDS in Paschim MidnaporeDocument12 pagesPDS in Paschim Midnaporesupriyo9277No ratings yet
- Haematology Notes - 3rd EdDocument100 pagesHaematology Notes - 3rd EdSally Brit100% (1)
- Parasitology Lecture Hosts, Symbiosis & TransmissionDocument10 pagesParasitology Lecture Hosts, Symbiosis & TransmissionPatricia Ann JoseNo ratings yet
- Hypertension Protocol Mukta VatiDocument18 pagesHypertension Protocol Mukta VatiDr. Avnish UpadhyayNo ratings yet
- Alternate Mekton Zeta Weapon CreationDocument7 pagesAlternate Mekton Zeta Weapon CreationJavi BuenoNo ratings yet
- December - Cost of Goods Sold (Journal)Document14 pagesDecember - Cost of Goods Sold (Journal)kuro hanabusaNo ratings yet
- Wastewater Treatment Plant Design PDFDocument68 pagesWastewater Treatment Plant Design PDFmostafa1alaahobaNo ratings yet
- Forest Fire Detection and Guiding Animals To A Safe Area by Using Sensor Networks and SoundDocument4 pagesForest Fire Detection and Guiding Animals To A Safe Area by Using Sensor Networks and SoundAnonymous 6iFFjEpzYjNo ratings yet
- 1 Colmac DX Ammonia Piping Handbook 4th EdDocument64 pages1 Colmac DX Ammonia Piping Handbook 4th EdAlbertoNo ratings yet
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocument1 pageDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoNo ratings yet
- Formularium ApotekDocument12 pagesFormularium ApotekNurul Evi kurniatiNo ratings yet
- The Ultimate Safari (A Short Story)Document20 pagesThe Ultimate Safari (A Short Story)David AlcasidNo ratings yet
- G10 Bio CellsDocument6 pagesG10 Bio CellsswacaneNo ratings yet
- ItilDocument11 pagesItilNarendar P100% (2)
- Ucg200 12Document3 pagesUcg200 12ArielNo ratings yet
- 8-26-16 Police ReportDocument14 pages8-26-16 Police ReportNoah StubbsNo ratings yet
- IMCI Chart 2014 EditionDocument80 pagesIMCI Chart 2014 EditionHarold DiasanaNo ratings yet
- Aging and Elderly IQDocument2 pagesAging and Elderly IQ317537891No ratings yet
- UMR Introduction 2023Document110 pagesUMR Introduction 2023tu reves mon filsNo ratings yet
- Schneider Electric PowerPact H-, J-, and L-Frame Circuit Breakers PDFDocument3 pagesSchneider Electric PowerPact H-, J-, and L-Frame Circuit Breakers PDFAnonymous dH3DIEtzNo ratings yet