Professional Documents
Culture Documents
4 Arterial, Central Venous, and Pulmonary Artery Catheters
Uploaded by
Toujours ÁmeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
4 Arterial, Central Venous, and Pulmonary Artery Catheters
Uploaded by
Toujours ÁmeCopyright:
Available Formats
PART
PART I CRITICAL CARE PROCEDURES, MONITORING, AND PHARMACOLOGY I
CHAPTER
Chapter 4
Arterial, Central Venous, and
4
Arterial, Central Venous, and Pulmonary Artery Catheters
Pulmonary Artery Catheters
Jean-Louis Vincent
Four potential indications for insertion of an arter-
Arterial Catheters
ial catheter for measurement of arterial pressure are
What Do They Offer?
Access recognized:
Complications 1. Hypotensive states associated with (a risk of) altered
Central Venous Catheters tissue perfusion. Hypotension that is resistant to fluid
What Do They Offer?
administration requires the administration of vasopres-
Access
Complications
sor agents, and invasive measurement of arterial pres-
sure then becomes absolutely necessary to titrate this
Pulmonary Artery Catheters
What Do They Offer? form of therapy. Norepinephrine and dopamine are the
Complications vasopressor agents most commonly used in this setting.
Technical Limitations A mean arterial pressure of 65 to 70 mm Hg usually is
Applications: Diagnosis versus Monitoring targeted, but this level should be modified as indicated
Effects of Interventions by the clinical scenario; in particular, elderly patients
Clinical Indications for Pulmonary Artery Catheter with atherosclerotic disease may require higher levels
Insertion
than young individuals with normal arteries.
Pulmonary Artery Occlusion Pressure and Partial
Occlusion 2. Vasodilator therapy. Vasodilating therapy is a mainstay
Does the Use of a Pulmonary Artery Catheter Improve in the management of heart failure, because it can
Outcome? increase cardiac output. Nitrates and hydralazine
usually are used for this purpose. Close monitoring
of arterial pressure is essential to avoid excessive
hypotension.
3. Severely hypertensive states. Extreme hypertension
may result in organ impairment, especially of the brain
ARTERIAL CATHETERS and the heart. Sodium nitroprusside or calcium entry
blockers usually are used to lower arterial pressure,
What Do They Offer? and careful, accurate monitoring is essential to titrate
The placement of an arterial catheter permits (1) reliable
the antihypertensive therapy.
and continuous monitoring of arterial pressure and (2)
4. Induction of hypertension. Hypertension sometimes
repeated blood sampling. Analysis of the arterial pulse
is induced in patients with neurologic diseases. Severe
pressure curve also may have other applications, includ-
cerebral edema with intracranial hypertension, in par-
ing assessment of fluid responsiveness and estimation of
ticular, requires vasopressor support to maintain cere-
cardiac output. The appearance of arterial pressure waves
bral perfusion pressure (the gradient between the mean
will vary according to the site at which the artery is
arterial pressure and the intracranial pressure); like-
sampled. As the arterial pressure wave is conducted away
wise, hypertension may be used to treat or prevent the
from the heart, three effects are observed: the wave
development of vasospasm secondary to subarachnoid
appears narrower; the dicrotic notch becomes smaller; and
hemorrhage, as part of the so-called triple-H therapy
the perceived systolic and pulse pressures rise and the
(hypertension, hypervolemia, hemodilution). Norepi-
perceived diastolic pressure falls.
nephrine usually is used for this purpose.
Arterial Pressure Measurement
The optimal range of arterial pressure depends on indi- Fluid Responsiveness
vidual patient characteristics, on underlying diseases, Variations in arterial pressure during positive-pressure
and also on treatment. Hence, it is impossible to give an ventilation have been used as a measure of fluid respon-
optimal range of arterial pressure that is applicable in all siveness. The transient increases in intrathoracic pressure
patients. When arterial pressure needs to be evaluated influence venous return in patients who are likely to
accurately, oscillometric measurements become unreli- respond to fluid administration. This fluctuation in ven-
able,1 and insertion of an arterial catheter is indicated. tricular filling will translate into fluctuations in arterial
53
Ch004-A04841.indd 53 9/13/2007 9:57:25 AM
PART
I
SPV
CRITICAL CARE PROCEDURES, MONITORING, AND PHARMACOLOGY
Arterial
Pressure
A Caliber of the artery
large small
⌬Down ⌬Up
Figure 4-2. Schematic representation of an arterial pressure
tracing showing that the pulse pressure increases as arterial
size decreases.
B C
Figure 4-1. The systolic pressure variation (SPV) is the concern about infection.4 Use of other sites, such as the
difference between the maximum and the minimum systolic brachial or the axillary artery or even the dorsalis pedis
blood pressures during one ventilatory cycle (A). The SPV is artery,5 can be considered. An important point to keep in
the sum of the ∆Down (B) and the ∆Up (C). (From Perel A,
mind is that the pulse pressure increases from the core to
Pizov R, Cotev S: Systolic blood pressure variation is a
sensitive indicator of hypovolemia in ventilated dogs the periphery. In other words, the systolic pressure is over-
subjected to graded hemorrhage. Anesthesiology estimated in smaller arteries (Fig. 4-2). Hence, it may be
1987;67:498.) better to rely more on mean than on systolic or diastolic
pressures.
pressure a few beats later. Accordingly, the greater the Complications
degree of systolic arterial pressure, or pulse pressure, The most feared complication with use of arterial cathe-
variation during the respiratory cycle, the greater will be ters is ischemia. With any suspicion of ischemia, the
the increase in cardiac output in response to fluid admin- catheter must be removed immediately. Allen’s test, to
istration (Fig. 4-1). However, this observation is valid pri- determine occlusive arterial lesions distal to the wrist, is
marily in patients without spontaneous respiratory unreliable and is no longer widely used. The accidental
movements and without significant arrhythmias, and only disconnection of arterial lines can be associated with
when a sufficient tidal volume is applied.2,3 severe hemorrhage and even exsanguination. Infectious
complications are rare.
Cardiac Output Assessment
The pulse contour analysis also can serve to estimate
cardiac output less invasively than with the pulmonary CENTRAL VENOUS CATHETERS
artery catheter (PAC). Because the only determinants of
arterial pressure are the stroke volume and the resistance What Do They Offer?
and compliance factors of the blood and arteries, analysis The central venous catheter can facilitate fluid administra-
of the pulse contour trace can help to monitor cardiac tion. It also allows measurement of the central venous
output over time. This can be done with regular calibra- pressure (CVP) and enables access to central venous blood
tions whenever changes in vascular tone or blood volume for sampling.
occur, or even in the absence of calibration. These mea-
surements are still approximations, so further technologi- Fluid Administration
cal developments can be expected to improve accuracy. The large-bore central venous catheter allows fluids to be
administered fast and reliably in the presence of acute
Blood Sampling hemorrhage. Placement of a central catheter is therefore
The presence of an arterial catheter can greatly facilitate essential in patients with hemorrhage due to polytrauma
blood sampling, especially in terms of enabling easy access or with other forms of acute bleeding. It also allows irritat-
to the circulation for regular monitoring of blood gases, ing or hypertonic fluids to be administered, such as
such as may be required in severe respiratory failure or parenteral solutions, potassium-enriched solutions, and
with acute metabolic alterations. Sensors can measure some therapeutic agents. Central venous lines also can be
blood gases continuously, but widespread use of such convenient in patients who need prolonged intrave-
sensors is limited by their cost. nous therapy when peripheral venous access becomes
problematic.
Access
For placement of arterial catheters, usually the radial Measurement of Central Venous Pressure
artery is used. The femoral artery can be easily cannulated CVP is identical to right atrial pressure (RAP) (in the
and gives a better signal, but presence of a femoral cath- absence of vena cava obstruction) and to right ventricular
eter interferes more with patient mobility and warrants (RV) end diastolic pressure (in the absence of tricuspid
54
Ch004-A04841.indd 54 9/13/2007 9:57:26 AM
CHAPTER
4
regurgitation). It is thus equivalent to the right-sided not uncommon, but hematoma formation usually is
filling pressure. CVP is determined by the interaction of without major consequences. Bedside ultrasonography
Arterial, Central Venous, and Pulmonary Artery Catheters
cardiac function and venous return, which is itself deter- can help guide the introduction of the catheter into the
mined by the blood volume and the compliance charac- vein. Excessive advancement of a long catheter in a
teristics of the venous system. Hence, an elevated CVP small patient can result in arrhythmias; such arrhythmias
can reflect an increase in blood volume as well as an have been described with advancement of the catheter
impairment in cardiac function. Because the CVP evalu- tip into the right ventricle, but this problem can be identi-
ates the right-sided filling pressures, CVP can be increased fied by the presence of an RV trace on the monitor
in the presence of pulmonary hypertension, even if left display.
ventricular (LV) function is normal. The normal value in Catheter-related infections constitute the major long-
healthy persons is very low, not exceeding 5 mm Hg. Thus, term complication. Adherence to basic hygiene guidelines
the CVP value may not be much lower than normal in can decrease the incidence of catheter-related sepsis.
the presence of hypovolemia. In general, a CVP below Triple-lumen catheters may be associated with a higher
10 mm Hg can be considered to indicate that the patient incidence of catheter-related infection,10 primarily as a
is more likely to respond to fluid resuscitation, but excep- result of increased catheter manipulation. The use of anti-
tions to this rule exist. A high CVP suggests a certain microbial-coated catheters may decrease the risk of infec-
blood volume but does not guarantee sufficient LV tions11 but is associated with the threat of development
filling. of resistant organisms.12 Routine replacement of catheters
Clinically, CVP can be assessed by evaluation of the after 3 to 7 days is not recommended.13
degree of jugular distention6 or liver enlargement. A single
CVP measurement is not very useful and is not a good
indicator of a positive response to fluids; an increase in PULMONARY ARTERY CATHETERS
CVP without a concurrent increase in cardiac output is
not only useless but also harmful, because it will lead to What Do They Offer?
increased edema formation. PACs allow collection of data on right atrial, pulmonary
artery, and pulmonary artery occlusive pressures (Fig. 4-
Access to Blood in Superior Vena Cava 3); flow (cardiac output); and oxygenation (mixed venous
Measuring the central venous oxygen saturation (ScvO2) oxygen saturation).
is a surrogate for measurement of the true mixed venous
oxygen saturation (SvO2). ScvO2 can be obtained either Pressures
intermittently (by withdrawal of blood samples) or con-
tinuously (with the use of a catheter equipped with fiber- Right Atrial Pressure
optic fibers). This approach may be particularly helpful in As indicated earlier, the RAP is identical to the CVP in
the early resuscitation of the patient with severe sepsis the vast majority of cases.
and septic shock, as part of so-called “early goal-directed
therapy.”7 Pulmonary Artery Occlusion Pressure
When the balloon on the catheter is inflated, it causes an
Trace Analysis obstruction (becomes wedged) in a small branch of the
Analysis of the CVP waveform can provide some interest- pulmonary artery, interrupting the flow of blood locally
ing information. In particular, a large y descent indicates (but blood flow continues normally in the rest of the pul-
a restrictive cardiac state, but not all restrictive patterns monary circulation), so that (assuming the absence of an
are associated with this finding. abnormal obstacle), a continuous column of blood is
present between the tip of the PAC and the left atrium.
Access This pulmonary artery occlusion pressure (PAOP), or pul-
The central venous catheter generally is introduced via monary artery wedge pressure (PAWP), generally reflects
the internal jugular vein; the subclavian vein also can be the left atrial pressure well. Nevertheless, a number of
used, although the risk of pneumothorax may be some- steps must be taken to ensure the adequacy of the
what higher with this route. The introduction of a femoral measurement.
catheter through the abdominal inferior vena cava to the A first question is whether the PAOP reflects the pres-
right atrium can yield reliable CVP measurements.8 The sure in the pulmonary veins and not the alveolar pressure.
use of femoral catheters, however, is associated with a The tip of the catheter should be in a West zone III posi-
greater risk of infections and thrombophlebitis.9 tion, where a continuous column of blood exists between
the catheter tip and the left atrium (Fig. 4-4). These con-
Complications siderations are less important with fluid optimization
Complications of central venous catheterization are and with today’s lower positive end-expiratory pressures
related primarily to puncture of the central vein: Hemo- (PEEP).
thorax can be life-threatening, especially in the presence To exclude a possible influence of airway pressure on
of severe respiratory failure. In the presence of unilateral PAOP readings, the changes in PAOP can simply be com-
pathology, the catheter must be introduced on the affected pared with the changes in pulmonary artery pressure
side. Arterial puncture resulting in a local hematoma is (PAP) during the respiratory cycle. If PAOP reflects the
55
Ch004-A04841.indd 55 9/13/2007 9:57:26 AM
PART
I
A Right Atrium B Right Ventricle C Pulmonary Artery D Pulmonary
Capillary Wedge
CRITICAL CARE PROCEDURES, MONITORING, AND PHARMACOLOGY
ECG
Pressure, mm Hg
30 2
3
20
1 a v
4 x y
10
ac v 6
x y
0 5
1 sec
Figure 4-3. Pressure waveforms. A, The normal right atrial (RA) tracing. The a wave is the RA pressure rise resulting from atrial
contraction and follows the P wave of the electrocardiogram (ECG). On simultaneous ECG and RA tracings it usually occurs at
the beginning of the QRS complex. The c wave, caused by closure of the tricuspid valve, follows the a wave and is coincident
with the beginning of ventricular systole. Atrial relaxation (x descent) is followed by a passive rise in RA pressure resulting from
atrial filling during ventricular systole and occurs during the T wave of the simultaneously recorded ECG. The y descent reflects
the opening of the tricuspid valve and passive atrial emptying. B, The normal right ventricular (RV) tracing. The sharp rise in RV
pressure (1) is due to isometric contraction and is followed by a rapid pressure decrease (2) as blood is ejected through the
pulmonary valve. This rapid ejection is followed by a phase of more reduced pressure decrease, which is often reflected in
a small step in the downslope of the RV pressure waveform (3). The subsequent sharp decline in RV pressure (4) occurs as
a result of isometric relaxation, and is noted once the RV pressure falls below the pulmonary artery (PA) pressure (with
consequent closure of the pulmonary valve). As RV pressure falls below RA pressure, the tricuspid valve opens, and passive
refilling (5) of the right ventricle occurs, followed by atrial contraction, causing a biphasic wave of ventricular filling to appear
on the RV tracing (6). C, The normal pulmonary arterial waveform. A pulmonary artery systolic elevation is caused by ejection
of blood from the right ventricle, followed by a decline in pressure as RV pressure falls. As RV pressure falls below pulmonary
artery pressure, the pulmonary valve closes, which causes a momentary rise in the declining pulmonary artery pressure. This is
the dicrotic notch characteristic of the pulmonary arterial (and also the systemic arterial) waveform. The pulmonary artery
systolic wave usually occurs in synchrony with the T wave of the ECG. Pulmonary artery diastolic pressure (PADP) does not fall
below RA pressure and therefore is higher than right ventricular end diastolic pressure (RVEDP): it is an approximation to left
ventricular end diastolic pressure (LVEDP). D, The normal pulmonary artery occlusion pressure (PAOP) waveform. The waveform
of the PCWP is subject to the same mechanical variables as the RA waveform, but because of the damping that occurs through
the pulmonary circulation, the waves and descents often are less distinct. Similarly, the mechanical events are recorded later in
the cardiac cycle, as seen on the ECG. Thus, the a wave is not seen until after the QRS complex, and the v wave occurs after
the T wave of the ECG. The PCWP is a closer approximation to LVEDP than is PADP. (From Grossman W: Cardiac
catheterization. In Braunwald E [ed]: Heart Disease: A Textbook of Cardiovascular Medicine, 3rd ed. Philadelphia, Saunders,
1992.)
pressure within the pulmonary veins, these changes should limitations. Simple disconnection of the respirator to
be identical, because the pulmonary artery and vein measure PAOP after obtaining an equilibration state is
should be subjected to identical changes in intrathoracic not recommended, because the measured PAOP will not
pressures. If, on the other hand, the catheter tip is not in represent the real value when PEEP is applied. A better
a West zone III, the changes in PAOP will be more signifi- method consists of measuring the lowest (nadir) PAOP
cant than the changes in PAP. In these latter conditions, within seconds after a very transient disconnection from
either fluid administration or some reduction in the PEEP the ventilator, to identify the true transmural pressure
level may abolish the differences. before a new equilibrium is reached.14 Such a maneuver
The next question is whether the measured pressure is suppresses the high intrathoracic pressure and eliminates
truly a transmural pressure—that is, the pressure differ- the influence of the extramural pressure, but the values
ence between the vascular structures and the environ- obtained may not be valid in the presence of intrinsic
mental structures. In other words, will changes in PEEP. Other methods have been suggested, some rela-
surrounding intrathoracic pressures influence the pres- tively sophisticated15 and others more simple, involving
sures measured? In the case of intrathoracic pressures, the subtraction of approximately one third of the PEEP level
changes in pleural pressure are particularly relevant. from the measured PAOP, for example. The question is
Hence, all measurements should be performed at end- whether this is really so important, because absolute
expiration, when the pleural pressure is closest to zero. A PAOP values are not very helpful.
marked fall in intrapleural pressure, as with a Mueller In respiratory failure, PAOP does not represent true
maneuver (forced inspiration against resistance), may dra- capillary pressure, which may be somewhat higher. The
matically increase the transmural pressures. A more true capillary pressure may be estimated from the mea-
common problem in the intensive care unit (ICU) is the surement of the intersection point of the rapid and slow
increase in pleural pressure due to positive-pressure ven- pressure decay curves recorded after a rapid interruption
tilation, sometimes with high PEEP levels. of the blood flow; such measurements of capillary pres-
One method of combating this problem could be to sure are possible from the pressure trace. This pressure is
subtract the esophageal pressure from the measured well correlated with extravascular lung water in animal
PAOP, but this approach has a number of technologic experiments. The need to know these values is question-
56
Ch004-A04841.indd 56 9/13/2007 9:57:26 AM
CHAPTER
4
rather, PAOP is a direct determinant of edema formation
in the lungs. The key principle is to keep the PAOP as low
Arterial, Central Venous, and Pulmonary Artery Catheters
as possible, provided that all of the other organs are
I happy.
PA>Pa>Pv
Zone 1
Pulmonary Artery Pressures
Normally the pulmonary vasculature is a low-resistance
circuit, so that the diastolic PAP should be equal to or
II Pa>PA>Pv only slightly higher than the PAOP. An increased pressure
Zone 2 gradient between the diastolic PAP and the PAOP
indicates active primary pulmonary hypertension related
to pulmonary vascular changes (hypoxia) or diseases
(primary pulmonary artery hypertension). Pulmonary
Pa>Pv>PA hypertension may result in RV dilation with septal shifts
III
Zone 3
that may compromise LV function.
Cardiac Output
The reference method for measurement of cardiac output
is use of the Fick equation; however, this is difficult to
Figure 4-4. The position of the pulmonary artery catheter tip apply in practice. The indicator dilution technique has
in relation to the zones of the theoretical lung model been used instead. Indocyanine green clearance has been
described by West. For pulmonary artery occlusion pressure used for many years, but this method is time-consuming
(PAOP) to be a valid estimate of “left heart” filling pressure, a and quite difficult to perform. The thermodilution tech-
continuous column of blood must exist between the catheter
nique developed by Ganz is a convenient technique
tip and the left atrium. In zones I and II, pulmonary
vasculature is either totally or partially compressed by the which today allows the almost continuous measurement
intra-alveolar pressure, and measurements of PAOP will be of cardiac output. The presence of tricuspid insufficiency
misleading. PA, alveolar pressure; Pa, pulmonary artery is the major limitation to this technique.
pressure; Pv, pulmonary venous pressure. (From Marini JJ: More recently, other techniques, including the transpul-
Respiratory Medicine and Intensive Care for the House Officer. monary technique proposed by PiCCO (Munich, Germany)
Baltimore, Williams & Wilkins, 1991.) and the lithium dilution technique proposed by LiDCO
(London), have been developed, but they are somewhat
able, however, because the primary goal remains to keep less precise.
these hydrostatic pressures as low as possible while main- The thermodilution technique estimates cardiac output
taining adequate cardiac output. over several cardiac cycles, whereas other techniques
PAOP may not adequately reflect LV end diastolic pres- including those based on pulse contour analysis, may
sure. It may be lower in patients with aortic regurgitation assess beat-to-beat variations. These may be useful to
or higher in the presence of significant tachycardia or estimate the influence of changes in intrathoracic pres-
mitral valve disease. LV end diastolic pressure may not sures on the stroke volume variation, an estimate of fluid
even accurately predict LV end diastolic volume. This was responsiveness.
already demonstrated many years ago with radionuclide
techniques.16 Preload is more directly defined as the end Right Ventricular Volumes
diastolic volume. A stiff, noncompliant ventricle can result The use of a modified PAC equipped with a fast response
in a relatively high end diastolic pressure for a given end thermistor also allows evaluation of the right ventricular
diastolic volume. An evaluation of end diastolic volumes ejection fraction (RVEF) (Fig. 4-5). With knowledge of the
can be obtained less invasively with echocardiographic stroke volume, it becomes easy to calculate the end sys-
techniques. Likewise, the use of transthoracic thermodilu- tolic and end diastolic volumes. This measurement can be
tion techniques allows the estimation of intrathoracic particularly useful in the presence of RV failure, but this
blood volume and global end diastolic volumes. However, also is a situation in which the measurement is least reli-
these assessments of end diastolic volumes do not give able: tricuspid regurgitation secondary to pulmonary
additional information about the likelihood of fluid hypertension.
responsiveness.
In sum, then, a given level of cardiac filling pressures Mixed Venous Oxygen Saturation
does not provide much information about fluid respon- SvO2 represents the balance between oxygen consump-
siveness, but monitoring can be very helpful to guide a tion and oxygen supply. According to the Fick equation:
fluid challenge.17 During fluid administration, the goal is
VO2 = cardiac output × (CaO2 − CvO2)
to obtain a significant increase in cardiac output (by
the Frank-Starling mechanism) with the least increment where VO2 is oxygen uptake and CaO2 and CvO2 are the
in cardiac filling pressures, in order to minimize the arterial and venous oxygen content, respectively. If the
risk of edema formation. The goal is not to keep the dissolved oxygen in the blood is neglected for the pur-
cardiac filling pressures within predefined arbitrary limits; poses of calculation, then
57
Ch004-A04841.indd 57 9/13/2007 9:57:26 AM
PART
I
Stroke Pressure
Volume
CRITICAL CARE PROCEDURES, MONITORING, AND PHARMACOLOGY
EF Dysfunction
Failure
Closing
End-Diastolic Volume Pressure
Figure 4-5. Ventricular function curve depicting the difference
between ventricular dysfunction (decrease in the ventricular
ejection fraction [EF] but preservation of stroke volume) and
Flow
ventricular failure (defined as the inability of the heart to
pump enough flow). The EF, the ratio between stroke volume Figure 4-6. Relationship between pressure and blood flow,
and end diastolic volume, is represented by the dashed lines; illustrating the limitations in the calculation of the vascular
it is decreased in all cases. resistance. Note that the line defining that relationship does
not go through the origin, since the pressure is not zero in
the absence of blood flow.
VO2 = cardiac output × Hb (SaO2 − SvO2) × C
is not a good reflection of vasomotor tone in the pulmo-
and
nary vasculature. Pulmonary hemodynamics are therefore
SvO2 = SaO2 − (VO2/cardiac output × Hb × C) best assessed by altering blood flow to better evaluate this
relationship (Fig. 4-6).
Accordingly, a decrease in SvO2 can reflect either a
Calculation of systemic vascular resistance (SVR) is not
decrease in SaO2 (hypoxemia), anemia, or a relative inad-
very helpful either. It is better to base clinical decisions
equacy of cardiac output in relation to the oxygen demand
on primary variables. Simply stated, a relatively high
of the tissues.
cardiac output in relation to arterial pressure reflects a
SvO2 can be measured continuously using catheters
low SVR state, whereas a relatively low cardiac output
equipped with fiberoptic fibers, and measurements are
reflects a high SVR state.
helpful to guide therapy. ScvO2 has been proposed as a
surrogate for SvO2, but the relationship between ScvO2 Ventricular Stroke Work The work developed by the
and SvO2 is rather vague. Indeed, the ScvO2 is lower than ventricles is determined by the ventricular work as derived
SvO2 in healthy conditions (as a result of the low O2 from the product of flow and the pressure generated. The
extraction by the kidneys) but is higher than SvO2 in criti- relationship between stroke work and the respective filling
cally ill patients (because of relative increase in O2 extrac- pressure represents a better assessment of contractility
tion in the kidneys and in the gut).18 Moreover, O2 than does the stroke volume. LV stroke work index
extraction is high in the coronary circulation, and this is (LVSWI) can be calculated using the equation
missed in the measurement of ScvO2. LVSWI = SI(MAP − PAOP) × 0.0136
Derived Variables where SI represents the stroke work index.
Hemodynamic assessment can include a number of Oxygen-Derived Variables Oxygen transport can be
derived variables, including resistance, ventricular stroke assessed as the product of cardiac output and the arterial
work, oxygen transport, oxygen consumption, and venous oxygen content, according to the equation
admixture, as described next.
DO2 = cardiac output × CaO2
Resistance In steady-flow conditions, Ohm’s law indi- = cardiac output × ([Hb] × SaO2 × 1.39) +
cates that resistance is the ratio between the pressure drop 0.0031 × PaO2
and the flow in the system. In the pulmonary circulation, Calculations of this variable benefit from combining
the inflow pressure would be the mean PAP and the measurements of cardiac output, Hb, and SaO2 but have
outflow pressure would be PAOP; for the systemic circula- the limitation that the corresponding oxygen demand is
tion, these would be the MAP and the CVP, respectively. unknown. Some studies suggested that maintaining supra-
In either case, flow would be cardiac output. This approach normal DO2 in the perioperative period or early after
is limited, however, by the fact that the extrapolated inter- trauma may result in better outcomes.
cept of the PAP–cardiac output relationship represents the Oxygen consumption also can be calculated from the
average closing pressure of the small pulmonary arteri- product of cardiac output and the arteriovenous oxygen
oles, and the slope represents the upstream arterial resis- difference, according to the formula
tance. Accordingly, the increased PAP in pulmonary
hypertension can be explained by both an increase in VO2 = cardiac output × (CaO2 − CvO2)
pulmonary vascular closing pressure and an increase in where CvO2 is calculated in the same way as for CaO2,
vascular tone, and pulmonary vascular resistance (PVR) using the SvO2 instead of the SaO2.
58
Ch004-A04841.indd 58 9/13/2007 9:57:26 AM
CHAPTER
4
The difficulty is in evaluating the oxygen requirements common but usually are without major consequence,
(or the oxygen demand) of the body. VO2 assessment may except in moribund patients. It has been suggested that
Arterial, Central Venous, and Pulmonary Artery Catheters
perhaps be useful to evaluate the caloric need of the criti- lidocaine should be given prophylactically in predisposed
cally ill patient. patients, but this usually is not necessary. Likewise, com-
The calculation of oxygen extraction is accomplished plete atrioventricular block may develop in patients with
by determining the ratio of VO2 to DO2, or, in a simplified left bundle branch block, but this is exceptional. Knot
way: formation will be rare if the catheter is advanced carefully
and if its presence in the pulmonary artery is confirmed
O2ER = VO2/DO2 = (CaO2 − CvO2)/CaO2
before further advancement into the right ventricle. In
= (SaO2 − SvO2)Hb/SaO2 × Hb
particular, care should be taken not to advance the cath-
= (SaO2 − SvO2)/SaO2
eter by more than 30 to 35 cm into the right ventricle.
Accordingly, when SaO2 is close to 100%, in the absence Thrombotic complications have become rare with the
of hypoxemia, O2ER mirrors SvO2. Its calculation can development of heparin-coated catheters. The appearance
be useful in the presence of hypoxemia, when SaO2 is of an infiltrate beyond the tip of the PAC on the chest film
decreased. Also, the relationship between cardiac output should suggest an evolving thrombotic event, which
and O2ER can be helpful to compare the central and the should lead to consideration of the withdrawal of the
peripheral components of oxygen delivery (Fig. 4-7). This catheter. Endothelial lesions have been found at autopsy,
relationship is independent of Hb, so that it can be helpful but their clinical relevance is doubtful. Endocarditis is
to evaluate the cardiovascular status in the presence of very rare. Valvular damage may occur as a result of
anemia.19 improper handling of the catheter (in particular, its with-
drawal with the balloon still inflated). Catheter-related
Venous Admixture Venous admixture can be calculated
infections remain a risk, but they do not seem to be any
by the Berggren equation:
more common than with central venous catheters.
Cc ′o2 − Cao2 Pulmonary artery rupture is the most feared complica-
Qs Qt =
Cc ′o2 − Cvo2 tion: Although it is exceptionally rare, it is associated with
a high mortality rate. The usual cause is overinflating
in which Qs is shunt flow, Qt is total pulmonary blood the balloon in the presence of resistance to inflation, par-
flow, and Cc′O2 represents the capillary oxygen content ticularly in the presence of preexisting PAH; other, less
(assuming an oxygen saturation of 100%). This may help common causes are shown in Figure 4-8. The cardinal sign
to assess the effects of various interventions (PEEP or of rupture is the development of hemoptysis. The reaction
other respiratory conditions, administration of vasoactive to this event should not be to pull out the catheter entirely,
agents) on pulmonary hemodynamics. but rather to withdraw it slightly and then inflate the
balloon. If the hemorrhage does not stop, a thoracotomy
Complications may be necessary to repair the PA.
Complications of pulmonary artery catheterization can be
divided into seven categories as listed in Box 4-1. Many
of these can be prevented, and most are relatively Technical Limitations
uncommon. Invasive measurements of pressures are based on fluid-
Complications of venous access are the same as for the filled systems with disposable transducers. The transducer
insertion of a central venous catheter. Arrhythmias are includes a deformable membrane with a Wheatstone
bridge modifying the electrical resistance and, corre-
Cardiac Index, L/min/m2 spondingly, the intensity of a current. Reliability is ensured
6 by the excellent linearity between the pressure signal and
the electrical signal generated by the transducer, in a
5 A
4 Box 4-1
B
3 Complications of Pulmonary Artery
C Catheter Insertion
2 D
■ Complicated vascular access (pneumothorax, hema-
1 toma)
■ Arrhythmias (e.g., heart block, ventricular tachy-
0 cardia/fibrillation)
0 5 10 15 20 25 30 35 40 45 50 ■ Catheter knotting
O2 Extraction, % ■ Pulmonary thrombosis and infarction
Figure 4-7. Diagram illustrating the relationship between ■ Endothelial or valvular damage
cardiac index and O2 extraction. Four typical examples are ■ Colonization and bacteremia
given: hyperkinetic state (A), anemia (B), low cardiac output ■ Pulmonary artery rupture
state (C), and profound anesthesia (D).
59
Ch004-A04841.indd 59 9/13/2007 9:57:27 AM
PART
I Figure 4-8. Possible
mechanisms of pulmonary
CRITICAL CARE PROCEDURES, MONITORING, AND PHARMACOLOGY
artery rupture (other than the
most common cause,
overinflating the balloon in
Tip perforation the presence of resistance to
inflation). (From Barash PG,
Nardi D, Hammond G, et al:
Occlusion of catheter tip Catheter-induced pulmonary
by overdistended balloon artery perforation.
Mechanisms, management,
and modifications. J Thorac
Cardiovasc Surg 1981;82:5.)
Tip propelled by
eccentric balloon
Balloon perforation
Small branch
range of frequency values largely exceeding the range of connectors, may decrease the resonant frequency,
frequencies found in the human body. resulting in “whipped” traces. Likewise, the presence
Reliability is less secure in the intermediary system of bubbles must be carefully avoided. Transient flushing
made of tubes and stopcocks along the extent of the pres- should be followed by an abrupt return of the pressure
sure system. These can modify the morphology of the trace to its actual value.
trace, resulting in damping. Motion artifacts can further
complicate th e tracings. The presence of air bubbles also Applications: Diagnosis versus Monitoring
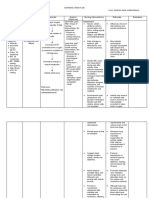
may alter the signal. Use of fluid-filled catheters to Today the PAC is more useful in guiding therapy rather
measure pressures provides reliable estimates of mean than in identifying abnormalities, this latter role having
vascular pressures. largely been taken over by noninvasive, mainly echocar-
Three steps must be followed to guarantee reliable diographic techniques (Table 4-1). In the past, analysis of
measurements: waveforms was used—for example, the abnormal V waves
of mitral regurgitation. Likewise, an increase of all pres-
1. The first step is appropriate zeroing. This is accom-
sures to identical levels should suggest pericardial tam-
plished by opening the transducer to atmospheric pres-
ponade. These findings should still alert the clinician to
sure (taken as the zero value). All pressures must be
possible abnormalities, but echocardiographic techniques
measured with reference to an arbitrary reference
have largely replaced the use of the PAC for identifying
point. This zero reference pressure level should ideally
valvular disease. The use of echocardiographic techniques
be where it is least influenced by location on the body.
for monitoring, however, is hampered by the difficulty of
In humans, it is thought to be at the level of the right
keeping the probe in the esophagus for prolonged periods
atrium, so the reference level usually is placed in the
of time, and results are very operator dependent.
mid-chest (mid-axillary) position at the level of the
To illustrate the need to integrate different variables,
fourth intercostal space. In healthy persons, the CVP
rather than focusing on just one variable, some suggested
referred to that region does not change with supine
applications follow:
versus upright position. An alternative reference is
5 cm vertically below the sternal angle. Obviously, ■ Interpretation of a cardiac output value: It is impor-
errors in zeroing are relatively more important for tant to consider the four determinants of cardiac output
measurements of cardiac filling pressures than for arte- (Fig. 4-9). Interpretation should start by considering
rial pressure measurements, because the errors are the stroke volume (cardiac output divided by heart
quantitatively identical but proportionally greater. rate), and relating this to an index of ventricular filling
2. The second step is calibration, which is now done auto- (PAOP) and an index of ventricular afterload (arterial
matically by today’s electronic systems. and pulmonary artery pressures); an inotropic agent
3. The third step is ensuring the good quality of the trace. should be added only when preload and afterload have
Shaking the catheter should result in large pressure been optimized.
variations on the screen. A damped system will under- ■ Fluid status: Low cardiac filling pressures may be
estimate systolic pressures. The liquid column should normal or reflect hypovolemia. It is the measurement
be continuous, without air bubbles in the system. of cardiac output and SvO2 that will help determine
Excessive tubing length, or multiple stopcocks and fluid needs. Indeed, hypovolemia typically is
60
Ch004-A04841.indd 60 9/13/2007 9:57:27 AM
CHAPTER
4
Table 4-1. Pulmonary Artery (PA) Catheterization versus Echocardiographic
Arterial, Central Venous, and Pulmonary Artery Catheters
Techniques for Management of Selected Disorders: Relative Value
PA Catheterization Echocardiography
Disorder Diagnosis Monitoring Diagnosis Monitoring
Tamponade + ++ +++ +
Hypovolemia ++ +++ ++ +
Valvular disease + ++ +++ +
Heart failure ++ +++ ++ +
Right ventricular failure ++ +++ +++ ++
Septic shock + +++ + +
Preload SvO2 low
Heart Rate
SaO2 low SaO2 normal
(hypoxemia)
Increased O2 extraction
Contractility
Afterload CO high CO low
Figure 4-9. The four determinants of cardiac output.
Hemoglobin PAOP high PAOP low
associated with a low cardiac output and a low SvO2
(Fig. 4-10). By contrast, hypervolemia in the presence
Normal Low Heart failure Hypovolemia
of normal cardiac function will be manifested by high (anemia)
cardiac filling pressures associated with a relatively
high cardiac output and normal or high SvO2. Elevated VO2
■ Hemodynamic versus nonhemodynamic pulmonary (exercise, stress, anxiety)
edema: The distinction between hemodynamic and Figure 4-10. Interpretation of a low SvO2 (mixed venous
nonhemodynamic types of lung edema no longer oxygen saturation). CO, cardiac output; PAOP, pulmonary
requires pulmonary artery catheterization; the clinical artery occlusion pressure; SaO2, arterial oxygen saturation;
history and less invasive (e.g., echocardiographic) mea- VO2, oxygen uptake.
surements usually are sufficient to separate the two.
Nevertheless, invasive hemodynamic monitoring can
RAP > PAOP
reveal that patients thought to meet only the acute
lung injury/acute respiratory distress syndrome (ALI/
ARDS) criteria sometimes have unexpectedly high Cardiac Output
PAOP.20 Adequate Inadequate
■ RV dysfunction versus failure: A reverse gradient (adequate SvO2) (low SvO2)
between RAP and PAOP (i.e., a higher RAP than
PAOP) indicates RV dysfunction or failure and usually RV Dysfunction RV Failure
is secondary to pulmonary hypertension, as will be
immediately apparent from the measurements of pul- Pulm. Art. P.
+ Inhaled NO?
monary artery pressures. RV dysfunction is manifested PGE1?
Normal Increased
by RV dilation (and thus a decrease in RVEF) with no
limitation on cardiac output. This is the most common Nothing
Diuretics? Arterial Pressure
situation in patients with ARDS, who usually maintain
a hyper-kinetic state. Rather, RV failure refers to a state Low Normal
in which cardiac output is no longer sustained at ade- Dobutamine
quate levels.21 These different entities are illustrated in Vasopressors Vasodilators
Figure 4-11.
Figure 4-11. Interpretation of a reversed gradient between
■ LV dysfunction versus failure: Here the gradient
the right atrial pressure (RAP) and the pulmonary artery
between PAOP and RAP will be higher than the typical occlusion pressure (PAOP). NO, nitric oxide; PEG1,
3 to 5 mm Hg. As with the right ventricle, in LV dys- prostaglandin E1; RV, right ventricular; SvO2, mixed venous
function the ventricular volumes may increase (so the oxygen saturation.
61
Ch004-A04841.indd 61 9/13/2007 9:57:27 AM
PART
I
ejection fraction will decrease), but the cardiac output ■ Dynamic assessment of cardiac function in specific
may be simultaneously preserved; such a situation may conditions: The best example is that of the patient who
CRITICAL CARE PROCEDURES, MONITORING, AND PHARMACOLOGY
exist in septic shock. LV failure is more common and is is difficult to wean from mechanical ventilation, possi-
manifested by a decrease in cardiac output and SvO2. bly owing in part to cardiac dysfunction.
Effects of Interventions Pulmonary Artery Occlusion Pressure and
■ Fluid challenge: A fluid challenge technique is indi- Partial Occlusion
cated whenever the benefit of fluid administration is Partial occlusion of the pulmonary artery in the presence
in doubt.17 Ideally, fluid administration will result in of pulmonary hypertension may be difficult to recognize
increases in cardiac output and tissue perfusion without and can lead to significant overestimation of the pulmo-
major increases in cardiac filling. An increase in PAOP nary artery occlusion pressure, denoted Ppao on Figure
in the absence of a significant change in cardiac output 4-12. A useful clue to partial occlusion is occurrence of a
and SvO2 indicates that fluid administration will only substantial increase in the Ppao without a concomitant
result in an increased risk of edema and should be change in the pulmonary artery diastolic pressure, denoted
discontinued. Ppad on the figure. If the Ppad − Ppao gradient is normal
■ Inotropic agents: The use of inotropes aims to increase and the underlying disease process would predict increased
cardiac output and possibly decrease PAOP. Lack of an pulmonary vascular resistance, partial occlusion should be
increase in cardiac output after administration of a suspected. Partial occlusion may occur if a catheter is
β1 inotropic agent indicates a desensitization of the either too proximal or too distal in the pulmonary artery,
β-adrenergic receptors and is associated with a worse and appropriate repositioning may be corrective. The best
prognosis.22 Ppao may be obtained in some circumstances by further
■ Vasopressors: The use of pure vasoconstrictors is advancing the catheter with the balloon fully inflated and
expected to increase arterial pressure but also cardiac at other times by retracting the catheter to the original
filling pressures. An excessive increase in cardiac filling pulmonary artery position and attempting to occlude with
pressures with use of such an agent suggests the need 1.0 to 1.2 mL of air, instead of full inflation. It is impera-
for addition of an inotropic agent (e.g., dobutamine). tive never to inflate against resistance. Figures 4-12 and
■ Vasodilators: The administration of vasodilators may 4-13 offer further information on diagnosis and manage-
rapidly reduce arterial pressure, so that continuous ment of partial occlusion.
arterial pressure monitoring is usually indicated. More-
over, a reduction in vascular tone in the presence of Does the Use of a Pulmonary Artery
hypovolemia may reduce venous return and thus Catheter Improve Outcome?
cardiac output. The use of the PAC has been challenged on the basis that
it has not been shown to improve outcomes.20,23-25 An
improvement in outcome, however, has not been demon-
Clinical Indications for Pulmonary Artery strated with other monitoring techniques. Moreover, a
Catheter Insertion number of studies have indicated that the use of the PAC
The improvement in noninvasive diagnostic techniques
can influence therapy.26 If use of a PAC does not result in
means that today the PAC is used primarily for monitor-
ing. Potential indications include the following:
Normal Ppad – Ppao Partial wedge
■ Circulatory shock, including the need for vasopressor
Pressure
agents: The PAC can be used to help guide fluid chal-
lenges and titrate inotropic agents. Shock due to hypo-
volemia (as in polytrauma or with other forms of
massive bleeding) does not require insertion of a PAC,
because management of such patients generally is quite
straightforward.
■ RV failure: The PAC can be used to monitor pulmonary
Increased Ppad – Ppao Partial wedge
artery pressures, the gradient between RAP and PAOP,
cardiac output, and SvO2.
Pressure
■ Acute respiratory failure due to pulmonary edema:
Whether lung edema is hemodynamic or nonhemody-
namic, the strategy should be to keep the hydrostatic
pressures as low as possible, but this requires measure-
ments of cardiac output and SvO2 to make sure the Figure 4-12. Schematic depiction of partial occlusion when
systemic circulation is not compromised the gradient between the pulmonary artery diastolic pressure
■ Complex fluid management in the presence of impend- (Ppad) and the pulmonary artery occlusion pressure (Ppao) is
normal (top) or is increased (bottom). Arrow denotes balloon
ing renal failure: Sometimes it is difficult to evaluate inflation. (From Leatherman JW, Shapiro RS: Overestimation
the fluid status in oliguric patients, in whom hypovol- of pulmonary artery occlusion pressure in pulmonary
emia may compromise renal function but hypervol- hypertension due to partial occlusion. Crit Care Med
emia obviously must be avoided. 2003;31:93-97.)
62
Ch004-A04841.indd 62 9/13/2007 9:57:28 AM
CHAPTER
4
(34) Sp02 96 PERB 0.2
Arterial, Central Venous, and Pulmonary Artery Catheters
1.5 cc 1.0 cc
Ppa Partial Ppao 苲 24 Best Ppao 苲 10
60 60
40 40
20 20
0 0
Figure 4-13. Partial pulmonary artery occlusion pressure (Ppao) measured when 1.5 cc of air was used to inflate the catheter
balloon (left graph); a much lower Ppao was obtained with a 1.0-cc inflation (right graph). Review of the chest roentgenogram
revealed that the catheter tip was too peripheral, so it was withdrawn to a more proximal location. Ppa, pulmonary artery
pressure. See text for definition of partial and best Ppao values. Scale in mm Hg. (From Leatherman JW, Shapiro RS:
Overestimation of pulmonary artery occlusion pressure in pulmonary hypertension due to partial occlusion. Crit Care Med
2003;31:93-97.)
Table 4-2. Components and Common Errors in KEY POINTS
Hemodynamic Monitoring
■ No simple guidelines for monitoring are available or
Component Common Errors applicable in all cases; monitoring should be tailored
to each patient’s needs.
1. Measure ■ Catheter misplacement
■ Errors in pressure measurements ■ Each variable, taken individually, has limitations and
■ No consideration of SvO2 is subject to error and difficulty in interpretation.
Variables should be combined and integrated to
2. Interpret ■ Interpretation of cardiac output without provide a global picture of the clinical situation.
consideration of SvO2
■ Neglect of PAP/PAOP gradient ■ A monitoring technique cannot improve outcome by
■ Neglect of inversed RAP/PAOP gradient itself; each of the three components of monitoring is
important with any monitoring technique:
3. Apply ■ Treating as if the data were not available
Accurate collection of data
■ Giving diuretics for a high PAOP without
other consideration Interpretation of the data
Application of the information obtained
PAP, pulmonary artery pressure; PAOP, pulmonary artery occlusion
pressure; RAP, right atrial pressure; SvO2, mixed venous oxygen ■ Cardiac output is an adaptive value that must
saturation. constantly adjust to the oxygen requirements of the
organs.
better outcomes, important and challenging questions ■ Separation of the four determinants of cardiac
arise about the beneficial effects of many therapeutic inter- output—heart rate, contractility, preload, and
ventions in the ICU. Some evidence suggests that the use afterload—is useful to consider the various
interventions that can be used to increase it.
of the PAC may improve outcomes in the most severely ill
subsets of critically ill patients.27,28 Errors in measurements ■ Measurements of mixed venous oxygen saturation
from the PAC were identified many years ago,29 and (i.e., SvO2) are essential to interpret cardiac output
measurements.
another consideration is the considerable interobserver
variability in interpretation of PAC tracings.30 In using a ■ The relationship between cardiac filling pressures and
volumes is relatively weak. Pressure measurements are
PAC, it is important to respect the three successive steps
important, however, because pressures (rather than
(Table 4-2): to take adequate and full measurements; to
volumes) are the primary determinant of edema
interpret the results correctly; and to apply the gathered formation.
information for the patient’s benefit. Unfortunately, poten-
■ The calculation of derived variables, such as vascular
tial errors are associated with each step. Some of these
resistances, ventricular work, and oxygen-derived
issues can be addressed with better teaching and improved variables, is of limited usefulness.
basic knowledge of hemodynamics and basic physiology.
63
Ch004-A04841.indd 63 9/13/2007 9:57:28 AM
PART
I
REFERENCES
CRITICAL CARE PROCEDURES, MONITORING, AND PHARMACOLOGY
1. Bur A, Hirschl MM, Herkner H, et al: impregnated central venous catheters. 22. Rhodes A, Lamb FJ, Malagon I, et al:
Accuracy of oscillometric blood pressure Catheter Study Group. N Engl J Med A prospective study of the use of a
measurement according to the relation 1999;340:1-8. dobutamine stress test to identify
between cuff size and upper-arm 12. Tambe SM, Sampath L, Modak SM: outcome in patients with sepsis, severe
circumference in critically ill patients. In vitro evaluation of the risk sepsis, or septic shock. Crit Care Med
Crit Care Med 2000;28:371-376. of developing bacterial resistance 1999;27:2361-2366.
2. De Backer D, Heenen S, Piagnerelli M, to antiseptics and antibiotics 23. Sakr Y, Vincent JL, Reinhart K, et al: Use
et al: Pulse pressure variations to predict used in medical devices. J of the pulmonary artery catheter is not
fluid responsiveness: Influence of tidal Antimicrob Chemother 2001;47: associated with worse outcome in the
volume. Intensive Care Med 589-598. intensive care unit. Chest 2005;128:
2005;31:517-523. 13. O’Grady NP, Alexander M, Dellinger EP, 2722-2731.
3. Heenen S, De Backer D, Vincent JL: et al: Guidelines for the prevention of 24. Harvey S, Harrison DA, Singer M, et al:
How can the response to volume intravascular catheter–related infections. Assessment of the clinical effectiveness
expansion in patients with spontaneous Infect Control Hosp Epidemiol of pulmonary artery catheters in
respiratory movements be predicted? 2002;23:759-769. management of patients in intensive
Crit Care 2006;10:R102. 14. Pinsky MR, Vincent JL, De Smet JM: care (PAC-Man): A randomised
4. Lorente L, Santacreu R, Martin MM, et al: Estimating left ventricular filling controlled trial. Lancet 2005;366:
Arterial catheter-related infection of pressure during positive end-expiratory 472-477.
2,949 catheters. Crit Care 2006;10:R83. pressure in humans. Am Rev Respir Dis 25. Rhodes A, Cusack RJ, Newman PJ, et al:
5. Martin C, Saux P, Papazian L, et al: 1991;143:25-31. A randomised, controlled trial of the
Long-term arterial cannulation in ICU 15. Teboul JL, Pinsky MR, Mercat A, et al: pulmonary artery catheter in critically ill
patients using the radial artery or Estimating cardiac filling pressure in patients. Intensive Care Med
dorsalis pedis artery. Chest 2001;119: mechanically ventilated patients with 2002;28:256-264.
901-906. hyperinflation. Crit Care Med 26. Mimoz O, Rauss A, Rekik N, et al:
6. Cook DJ, Simel DL: The rational clinical 2000;28:3631-3636. Pulmonary artery catheterization in
examination. Does this patient have 16. Calvin JE, Driedger AA, Sibbald WJ: critically ill patients: A prospective
abnormal central venous pressure? Does the pulmonary capillary wedge analysis of outcome changes associated
JAMA 1996;275:630-634. pressure predict left ventricular preload with catheter-prompted changes in
7. Rivers E, Nguyen B, Havstad S, et al: in critically ill patients? Crit Care Med therapy. Crit Care Med 1994;22:
Early goal-directed therapy in the 1981;9:437-443. 573-579.
treatment of severe sepsis and septic 17. Vincent JL, Weil MH: Fluid challenge 27. Chittock DR, Dhingra VK, Ronco JJ,
shock. N Engl J Med 2001;345: revisited. Crit Care Med 2006;34: et al: Severity of illness and risk of death
1368-1377. 1333-1337. associated with pulmonary artery
8. Joynt GM, Gomersall CD, Buckley TA, 18. Varpula M, Karlsson S, Ruokonen E, catheter use. Crit Care Med 2004;32:
et al: Comparison of intrathoracic and et al: Mixed venous oxygen saturation 911-915.
intra-abdominal measurements of cannot be estimated by central venous 28. Friese RS, Shafi S, Gentilello LM:
central venous pressure. Lancet oxygen saturation in septic shock. Pulmonary artery catheter use is
1996;347:1155-1157. Intensive Care Med 2006;32: associated with reduced mortality in
9. Merrer J, De Jonghe B, Golliot F, et al: 1336-1343. severely injured patients: A National
Complications of femoral and 19. Yalavatti GS, De Backer D, Vincent JL: Trauma Data Bank analysis of 53,312
subclavian venous catheterization in The assessment of cardiac index in patients. Crit Care Med 2006;34:
critically ill patients: A randomized anemic patients. Chest 2000;118: 1597-1601.
controlled trial. JAMA 2001;286: 782-787. 29. Morris AH, Chapman RH, Gardner RM:
700-707. 20. Wheeler AP, Bernard GR, Thompson BT, Frequency of wedge pressure errors
10. Zurcher M, Tramer MR, Walder B: et al: Pulmonary-artery versus central in the ICU. Crit Care Med 1985;13:
Colonization and bloodstream infection venous catheter to guide treatment of 705-708.
with single- versus multi-lumen central acute lung injury. N Engl J Med 30. Al Kharrat T, Zarich S, Amoateng-
venous catheters: A quantitative 2006;354:2213-2224. Adjepong Y, et al: Analysis of observer
systematic review. Anesth Analg 21. Vincent JL: Is ARDS usually associated variability in measurement of
2004;99:177-182. with right ventricular dysfunction or pulmonary artery occlusion pressures.
11. Darouiche RO, Raad II, Heard SO, et al: failure? Intensive Care Med Am J Respir Crit Care Med 1999;160:
A comparison of two antimicrobial- 1995;21:195-196. 415-420.
64
Ch004-A04841.indd 64 9/13/2007 9:57:29 AM
You might also like
- Immediate Life Support for healthcare Practitioners: A Step-By-Step GuideFrom EverandImmediate Life Support for healthcare Practitioners: A Step-By-Step GuideNo ratings yet
- Pharmacological Treatment of ArrhytmiaDocument6 pagesPharmacological Treatment of ArrhytmiaLućia-Simona Perić ExOalđeNo ratings yet
- 001 Chapter 6 Hemodynamic MonitoringDocument18 pages001 Chapter 6 Hemodynamic MonitoringMahesh Boopathy100% (2)
- Approach To Ventricular ArrhythmiasDocument18 pagesApproach To Ventricular ArrhythmiasDavid CruzNo ratings yet
- Cardiac DiseasesDocument47 pagesCardiac DiseasesismailcemNo ratings yet
- 6 Alterations On Tissue Perfusion Poleno Serrano TajalaDocument18 pages6 Alterations On Tissue Perfusion Poleno Serrano TajalaSophia A. GoNo ratings yet
- Invasive Monitoring in The Intensive Care UnitDocument6 pagesInvasive Monitoring in The Intensive Care UnitArjunNo ratings yet
- ArritmiasDocument12 pagesArritmiasJorgeNo ratings yet
- Sullivan 2015Document11 pagesSullivan 2015Karoline Pascoal Ilidio PeruchiNo ratings yet
- 00 - Physiologic Monitoring Systems, Cardiac CatheterizationDocument17 pages00 - Physiologic Monitoring Systems, Cardiac Catheterizationhabitar.unitpacNo ratings yet
- Chapter 80Document7 pagesChapter 80annisarachmaNo ratings yet
- Cardiac Arrhythmias in The Critically Ill Adult ADocument13 pagesCardiac Arrhythmias in The Critically Ill Adult AAlia SandoQaNo ratings yet
- Perioperative Implications of Pericardial Effusions and Cardiac TamponadeDocument9 pagesPerioperative Implications of Pericardial Effusions and Cardiac TamponadeMarielou CoutinhoNo ratings yet
- Management of Perioperative ArrhythmiasDocument15 pagesManagement of Perioperative Arrhythmiaszuraini_mdnoorNo ratings yet
- Pre-Operative Assessment/ Monitoring: Arif Hussain Demonstrator Anesthesia Ipms-KmuDocument20 pagesPre-Operative Assessment/ Monitoring: Arif Hussain Demonstrator Anesthesia Ipms-Kmuayub khanNo ratings yet
- Management of Perioperative Arrhythmias: PathogenesisDocument15 pagesManagement of Perioperative Arrhythmias: PathogenesisSudar Pecinta ParawaliNo ratings yet
- (NCM 410-M) Trans 1 - Altered Tissue PerfusionDocument6 pages(NCM 410-M) Trans 1 - Altered Tissue PerfusionANDREA JUSTINE CARDEÑONo ratings yet
- Hypertension GigiDocument10 pagesHypertension GigiAhamefula ChinazaNo ratings yet
- 1 s2.0 S0736467906006445 PDFDocument7 pages1 s2.0 S0736467906006445 PDFDiego Fernando Escobar GarciaNo ratings yet
- Penatalaksanaan Hipertensi EmergensiDocument6 pagesPenatalaksanaan Hipertensi Emergensiain17001No ratings yet
- Case Study of Atherosclerosis 1. Risk Factors of AtherosclerosisDocument5 pagesCase Study of Atherosclerosis 1. Risk Factors of AtherosclerosisCarly Beth Caparida LangerasNo ratings yet
- Soal Kasus HipertensiDocument3 pagesSoal Kasus HipertensiAlya NamiraNo ratings yet
- Cardiac Arrest and CardiopulmonaryDocument14 pagesCardiac Arrest and CardiopulmonaryCarlos UrquijoNo ratings yet
- Principles of Cardiac Anaesthesia: Learning ObjectivesDocument5 pagesPrinciples of Cardiac Anaesthesia: Learning ObjectivesFitri AmaliahNo ratings yet
- 2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and ChildDocument3 pages2.1. Pharmacological Therapeutics. 2.2. Basic Cardiac Life Support (BCLS) and Advanced Cardiac Life Support (ACLS) in Neonates and Childclint xavier odangoNo ratings yet
- Edwards Hemodynamic Monitoring For COVID Critically Ill PatientsDocument3 pagesEdwards Hemodynamic Monitoring For COVID Critically Ill PatientsblanquishemNo ratings yet
- touchCARDIO EJAE 7.1 pp04-11Document8 pagestouchCARDIO EJAE 7.1 pp04-11Carlos Navarro alonsoNo ratings yet
- NCP Risk For Decreased CO 1 PDFDocument2 pagesNCP Risk For Decreased CO 1 PDFdubsNo ratings yet
- Review Article: Management of Cardiac Tamponade After Cardiac SurgeryDocument10 pagesReview Article: Management of Cardiac Tamponade After Cardiac SurgeryJanuar Alfred PoliNo ratings yet
- Journal Reading Transcatheter Aortic Valve Replacement Under Monitored Anesthesia Care Versus General Anesthesia With IntubationDocument23 pagesJournal Reading Transcatheter Aortic Valve Replacement Under Monitored Anesthesia Care Versus General Anesthesia With IntubationTomy SandriyaNo ratings yet
- Anaesthesia Critical Care & Pain Medicine: EditorialDocument3 pagesAnaesthesia Critical Care & Pain Medicine: EditorialCarlos QuirogaNo ratings yet
- Capitulo IIDocument18 pagesCapitulo IIKJ IkhwanNo ratings yet
- Cateteres Arteriaes, Central y Arteria PulmonarDocument13 pagesCateteres Arteriaes, Central y Arteria PulmonarmmsNo ratings yet
- Vas OpressorDocument41 pagesVas Opressorstevanus handrawanNo ratings yet
- 272 F 80 e 4 BF 329 Ca 1 Fee 2Document16 pages272 F 80 e 4 BF 329 Ca 1 Fee 2api-684047665No ratings yet
- Shivani ShrivastavaDocument1 pageShivani ShrivastavaShivani ShrivastavaNo ratings yet
- 8 - Cardiovascular Sys - 2012 - Elsevier S Integrated Review Pharmacology SeconDocument27 pages8 - Cardiovascular Sys - 2012 - Elsevier S Integrated Review Pharmacology SeconCecilia GrayebNo ratings yet
- Cardiac Content WyattDocument90 pagesCardiac Content WyattAnni BarbaNo ratings yet
- Anesthesia For Intracranial Aneurysm Case FileDocument3 pagesAnesthesia For Intracranial Aneurysm Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Evaluation of Supraventricular TachycardiaDocument11 pagesEvaluation of Supraventricular TachycardiaJazmín Alejandra AGNo ratings yet
- Termodiluicao PulmonarDocument7 pagesTermodiluicao PulmonarKarina ResendeNo ratings yet
- POSTER - CASE REPORT Ver.2 Ventricular Tachycardia Storm and Unstable Ventricular Tachycardia in A 48-Years-Old Man Following A Non-ST Elevation Myocardial InfarctionDocument1 pagePOSTER - CASE REPORT Ver.2 Ventricular Tachycardia Storm and Unstable Ventricular Tachycardia in A 48-Years-Old Man Following A Non-ST Elevation Myocardial InfarctionRJMNo ratings yet
- TheElectrophysiologyStudy Gillingham I 2018 BJCN 135Document9 pagesTheElectrophysiologyStudy Gillingham I 2018 BJCN 135asif aliNo ratings yet
- Risk For Decreased Cardiac Output NCPDocument2 pagesRisk For Decreased Cardiac Output NCPMae Denn LabordoNo ratings yet
- AnnCardAnaesth19 Maret 2017 12Document10 pagesAnnCardAnaesth19 Maret 2017 12Henny Apriani ARNo ratings yet
- Angiography (Cardiac Catherization) : Patient Teaching/preparationDocument2 pagesAngiography (Cardiac Catherization) : Patient Teaching/preparationpsyNo ratings yet
- STH 19 - Day 2 - Track 1 - Session 2 - Watson - Hypertension - SNDocument18 pagesSTH 19 - Day 2 - Track 1 - Session 2 - Watson - Hypertension - SNiqra uroojNo ratings yet
- Peri-Operative Cardiac Arrhythmias - Part 1Document14 pagesPeri-Operative Cardiac Arrhythmias - Part 1jhonjrodriNo ratings yet
- 01 Cir 45 1 231 PDFDocument14 pages01 Cir 45 1 231 PDFFahmiNo ratings yet
- Cardiac Catheterization and MonitoringDocument25 pagesCardiac Catheterization and MonitoringReyna Mee AhiyasNo ratings yet
- NCPDocument4 pagesNCPNurhaifa MocademaNo ratings yet
- Arterial CatheterizationDocument2 pagesArterial CatheterizationZoran BuchevNo ratings yet
- Central Venous Access - 2019 (Gen, Ind-Contr)Document6 pagesCentral Venous Access - 2019 (Gen, Ind-Contr)Carlos NoronaNo ratings yet
- Antiarrhythmic Drugs and Anaesthesia 1Document9 pagesAntiarrhythmic Drugs and Anaesthesia 1CamiloRadaNo ratings yet
- Valvular Heart Disease To TW FinalDocument13 pagesValvular Heart Disease To TW FinalMohammed ElSayedNo ratings yet
- BF03259831Document21 pagesBF03259831Punnaphat Tinnaphop DaraswangNo ratings yet
- Invasive Hemodynamic Monitoring in The Cardiac Intensive Care UnitDocument12 pagesInvasive Hemodynamic Monitoring in The Cardiac Intensive Care Unitqe202300No ratings yet
- Anaesthesia in Dogs and Cats With Cardiac DiseaseDocument19 pagesAnaesthesia in Dogs and Cats With Cardiac DiseaseALEJANDRA MADRIGALNo ratings yet
- 25 Cardiovascular DiseaseDocument35 pages25 Cardiovascular DiseaseBramantyo NugrosNo ratings yet
- Ecocardiografia Monitoreo Hemodinamico en Critico..Document12 pagesEcocardiografia Monitoreo Hemodinamico en Critico..cositaamorNo ratings yet
- Ultrasound of Optic Nerve Sheath Diameter and Stroke OutcomesDocument9 pagesUltrasound of Optic Nerve Sheath Diameter and Stroke OutcomesToujours ÁmeNo ratings yet
- 353Document51 pages353AdamilzaryFikryNo ratings yet
- Fenobarbital en Tratamiento de Estatus SuprareflactarioDocument7 pagesFenobarbital en Tratamiento de Estatus SuprareflactarioToujours ÁmeNo ratings yet
- s41572 019 0118 8Document22 pagess41572 019 0118 8Annisa LazuardyNo ratings yet
- Epilepsy Guideline ST Epilepticus Children N Adult 2016Document14 pagesEpilepsy Guideline ST Epilepticus Children N Adult 2016Desi ChiloupChaNo ratings yet
- KETAMINA en NeuroDocument7 pagesKETAMINA en NeuroToujours ÁmeNo ratings yet
- 10 1164@rccm 201703-0548ST-1Document11 pages10 1164@rccm 201703-0548ST-1dogui0071No ratings yet
- 2007 Guideline For Management of Outpatient Chronic Obstructive Pulmonary Disease-Department of Veterans Affairs-Department of DefenseDocument11 pages2007 Guideline For Management of Outpatient Chronic Obstructive Pulmonary Disease-Department of Veterans Affairs-Department of DefenseToujours ÁmeNo ratings yet
- 29789983: Principles of Fluid Management and Stewardship in Septic Shock It Is Time To Consider The Four Ds and The Four Phases of Fluid TherapyDocument16 pages29789983: Principles of Fluid Management and Stewardship in Septic Shock It Is Time To Consider The Four Ds and The Four Phases of Fluid TherapyRaul LaraNo ratings yet
- Exacerbacion de EPOCDocument9 pagesExacerbacion de EPOCAlejandra FuentesNo ratings yet
- 2013 Sepsis GuidelinesDocument58 pages2013 Sepsis GuidelinesMuhd Azam100% (1)
- Epoc Vad 2007Document138 pagesEpoc Vad 2007Luz Estefany Huaman MachacaNo ratings yet
- Teorias Dela Patogenesis de Encefalopatia Hepatica 2012 The ClinicsDocument20 pagesTeorias Dela Patogenesis de Encefalopatia Hepatica 2012 The ClinicsToujours ÁmeNo ratings yet
- Bacterial Meningitidis1Document19 pagesBacterial Meningitidis1Toujours ÁmeNo ratings yet
- Usmle Step 1Document57 pagesUsmle Step 1zeal7777100% (1)
- Standard Baru Kriteria Diabetes 2010Document51 pagesStandard Baru Kriteria Diabetes 2010Tina MultazamiNo ratings yet
- First Aid Management For Common Life Threatening ConditionsDocument38 pagesFirst Aid Management For Common Life Threatening ConditionsBSN 2 - Sasis, Rusmaryte C.No ratings yet
- Pre-Hospital Assessment Sheet: Triage ScoreDocument2 pagesPre-Hospital Assessment Sheet: Triage Scoreratna purwitasariNo ratings yet
- Burns ReviewerDocument12 pagesBurns ReviewerMaverick LimNo ratings yet
- Section 8.1 - Homeostasis: Sbi4U Ms. FranklinDocument15 pagesSection 8.1 - Homeostasis: Sbi4U Ms. FranklinSidemen For LifeNo ratings yet
- Clinic Think FinalDocument6 pagesClinic Think FinalTop MusicNo ratings yet
- Zuku Visual Flashnotes Blood Gas EvalDocument10 pagesZuku Visual Flashnotes Blood Gas EvalvetthamilNo ratings yet
- A Soft Total Artificial Heart-First Concept Evaluation OnDocument11 pagesA Soft Total Artificial Heart-First Concept Evaluation OnSeyit Hamza ÇavgaNo ratings yet
- Deteksi Pre-Hospital StrokeDocument17 pagesDeteksi Pre-Hospital StrokeDocApizzNo ratings yet
- Pneumothorax: - Hitesh Rohit (3 Year B.P.T.)Document22 pagesPneumothorax: - Hitesh Rohit (3 Year B.P.T.)Hitesh RohitNo ratings yet
- Drug Study-DobutamineDocument2 pagesDrug Study-DobutamineCyril Joy N. FernandoNo ratings yet
- G2015 Adult Tachycardia PDFDocument1 pageG2015 Adult Tachycardia PDFibbs91No ratings yet
- Hemodynamic MonitoringDocument9 pagesHemodynamic MonitoringHernando CastrillónNo ratings yet
- Ynna Daria - Chicken Heart LabDocument7 pagesYnna Daria - Chicken Heart LabYnna DariaNo ratings yet
- NCPDocument2 pagesNCPNiño LuceroNo ratings yet
- Cs2-782021-Atika School-5172016 - Biology Paper 2 Marking Scheme Form4Document5 pagesCs2-782021-Atika School-5172016 - Biology Paper 2 Marking Scheme Form4bosirejanet526No ratings yet
- Headache in ChildrenDocument34 pagesHeadache in Childrensai saiNo ratings yet
- Concept 3 Notes - Endocrine System For StudentsDocument14 pagesConcept 3 Notes - Endocrine System For StudentsKaranNo ratings yet
- NCP LupusDocument5 pagesNCP LupusMarwin OditaNo ratings yet
- ZGMzZGE3ODAzZjU0ZjEyNjBkOTI2ZDg1YjAwZDY1OGQ2NzM4MDY5Yg PDFDocument137 pagesZGMzZGE3ODAzZjU0ZjEyNjBkOTI2ZDg1YjAwZDY1OGQ2NzM4MDY5Yg PDFdedyNo ratings yet
- Case-Based Discussion: BY: DAFFA JOKO N W (30101507415) Advisor: Dr. Saugi Abduh, Sp. PD., KKV, FinasimDocument71 pagesCase-Based Discussion: BY: DAFFA JOKO N W (30101507415) Advisor: Dr. Saugi Abduh, Sp. PD., KKV, FinasimAmanullah RayenNo ratings yet
- NCM 112-Mod3Document19 pagesNCM 112-Mod3Samantha BolanteNo ratings yet
- Human BIology PhysioEX Assignment 1Document2 pagesHuman BIology PhysioEX Assignment 1Peilu GanNo ratings yet
- NCM 118 Nursing Care PlansDocument15 pagesNCM 118 Nursing Care PlansElle LibalibNo ratings yet
- CardiomyopathiesDocument9 pagesCardiomyopathiesSaurabh BhandariNo ratings yet
- Regulation of Organic Metabolism and Energy Balance: Multiple Choice QuestionsDocument30 pagesRegulation of Organic Metabolism and Energy Balance: Multiple Choice QuestionswanderagroNo ratings yet
- (MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)Document11 pages(MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)NoreenNo ratings yet
- Modafinil For Excessive Sleepiness Associated With Shift-Work Sleep DisorderDocument11 pagesModafinil For Excessive Sleepiness Associated With Shift-Work Sleep DisorderbertouwNo ratings yet
- WEEK 5 Management of Patients With Fluids and ElectrolytesDocument89 pagesWEEK 5 Management of Patients With Fluids and ElectrolytesErica P. ManlunasNo ratings yet
- Thrombolysis For Acute Myocardial Infarction: Clinical Cardiology: New FrontiersDocument15 pagesThrombolysis For Acute Myocardial Infarction: Clinical Cardiology: New FrontiersBinod KumarNo ratings yet
- Hypovolemic ShockDocument25 pagesHypovolemic ShockManushi HenadeeraNo ratings yet