Professional Documents
Culture Documents
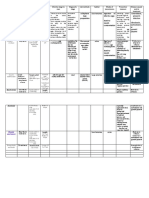
Table of Lower Genital Tract Infections: Disease Etiology Pathogenesis SSX Diagnosis Treatment
Uploaded by
Monique Angela Turingan Gangan0 ratings0% found this document useful (0 votes)
21 views3 pagesG
Original Title
L 2015
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentG
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views3 pagesTable of Lower Genital Tract Infections: Disease Etiology Pathogenesis SSX Diagnosis Treatment
Uploaded by
Monique Angela Turingan GanganG
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
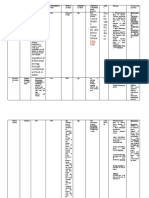
TABLE OF LOWER GENITAL TRACT INFECTIONS Prepared by: Paolo Warren (3i)
DISEASE ETIOLOGY PATHOGENESIS SSx DIAGNOSIS TREATMENT
ASx cyst + Age<40: No treatment
Obstruction of the duct
Cyst: tense, nonpainful Acute adenitis w/o abscess formation:
secondary to nonspec inflamm
Broad-spectrum antibiotics, hot Sitz bath
Bartholin’s Gland or trauma continued
Abscess: develops rapidly (2-4d), fluctuant, Sx cyst or abscess: Marsupialization, word
Infection secretion of glandular fluid
erythema, tenderness, edema, acute vulvar catheter, antibiotics (only if with cellulitis)
cystic dilation of the Bartholin’s
pain, dyspareunia, pain on walking Women age>40: excision biopsy to rule out
duct
malignancy
Eggs (nit) deposited at base of
Phthirus pubis (crab or Examination of vulva w/o
hair follicle nymph adult Kill both adult lice and eggs
pubic louse) Constant itching in the pubic area d/t allergic magnification: eggs and adult lice,
louse (dark gray) Permethrin 1% cream rinse
Sites: hairy areas of sensitization “pepper grain” feces adjacent to hair
Pediculosis Pubis Transmission: direct sexual Pyrethrins w/ piperonyl butoxide
vulva, occasionally the shaft
contact (>90% infected after Alt: Malathione 0.5% lotion
eyelids Pruritus w/in 24h after reinfection Definitive Dx: Microscopy adult louse
single exposure), may also be Ivermectin 250 ug/kg
Travels slowly and nit-containing larvae
non-sexually transmitted
Sarcoptes scabiei (itch
mite) Severe but intermittent itching
May involve hands, wrists, Kill both adult mites and eggs
Sites: widespread w/o Pruritus more intense at night Microscopy using scratch technique
breasts, vulva and buttocks Permethrin 5% cream (safe in pregnant)
Scabies predilection for hairy Papules, vesicles and (mites lack lateral claw legs but have 2
Short, “wavy” rashes in the Ivermectin 02mg/kg orally
areas Burrows (pathognomonic: twisted line on triangular hairy buds)
buttocks and interdigits Lindane 1% 1 oz lotion or 30g cream
Travels rapidly up to skin surface w/ small vesicle at one end)
2.5cm/min
Chronic localized infection
Trans: skin-skin contact, Self-limiting (for solitary lesions)
Microscopy of white waxy material
autoinoculation, fomites Flesh-colored small nodule or dome-shaped May inject local anesthetic on individual
from inside the nodule:
Molluscum Widespread infxn closely papule (1-5mm) w/ umbilicated crater at the papules to evacuate caseous material
Pox virus intracytoplasmic Molluscum bodies w/
contagiosum related to immunodeficiency center Base of papule treated w/ Ferric subsulfate
Wright or Giemsa stain
(HIV, chemo, corticosteroid Complication – superinfection (Monsel sol’n) or 85% TCA
Clinical Dx
admin) Cantharidin
Direct cervical inspection: whitish
lesions
Asymptomatic Depends on location, size and extend and
30% clinically overt macroscopic Biopsy: when unresponsive to
HPV 6 and 11 (90% of Pain, itching, tendency to bleed when friable, whether the woman is pregnant
lesions standard Tx, when condition
the causes of genital (+) odor when secondarily infected Chemical, cautery, immunologic Tx, surgery
70% subclinical, no signs of infxn accelerates during Tx, in
Condyloma warts) *RRP – recurrent respiratory papillomatosis Not 100% guarantee of cure
Trans: sexual, autoinoculation immunocompromised, if appears
acuminatum MC viral STD of the Pigmented, indurated, fixed or ulcerated Podofilox 0.5% solution or gel
Predisposing: pigmented, indurated, fixed or
vulva, vagina, rectum cauliflower-like lesions Imiquimod 5% cream
immunosuppressed, diabetic, ulcerated
and cervix Raised warty lesions 2mm-2cm, bigger Cryotherapy, Podophyllin resin,
pregnant, local trauma Microscopy: Koilocytes (perinuclear
pedunculated lesions Trichloroacetic acid
halo), Electron Micrograph: causative
agent
Clinical inspection
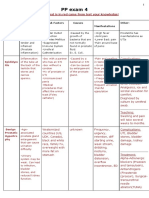
Primary Infxn: Viral culture: positive in primary infxn
Paresthesia of the vulvar skin PCR: most accurate and sensitive for
HSV1 – infection
Recurrent, incurable, highly Papule and vesicle formation HSV
above the waist, MC For non-pregnant:
contagious and one of the most Severe vulvar pain, tenderness and inguinal Western blot: most specific for
acquired genital herpes Valacyclovir
frequently encountered STD adenopathy diagnosing recurrent, unrecognized or
in women <25yo, does Acyclovir
Trans: asymptomatic shedding General malaise and fever subclinical herpes
not protect VS HSV2 Famciclovir
Genital Herpes Not a debilitating physical dse, Recurrence: Type-specific HSV serologic assay
HSV2 – infxn below (see table for complete dosing and
but may present an Related to onset of menses or emo stress ELISA and immunoblot test
the waist, offers indications)
overwhelming psych burden ASx but most are half as symptomatic as Lesion: multiple vesicles become
protection VS HSV1,
Resides in a latent phase in the primary shallow then develop as superficial
definite sexual Prevention: regular condom use, vaccine
dorsal root ganglia S2-S4 Prodrome: sacroneuralgia, vulvar burning, ulcers over a large area of the vulva
transmission
tenderness and pruritus Microscopy: Tzanck smear
Cytology: + multinucleated giant cell
Biopsy: + bag of coins
Chronic, slowly progressive,
Microscopy: Donovan bodies –
Klebsiella ulcerative, bacterial infxn of the Initially: ASx ndule w/c ulcerates (beefy red Doxycycline 100mg BID
clusters of dark-staining bacteria w/
granulomatosis – skin and subQ tissue of the ulcer w/ fresh granulation tissue) coalesce Alternatives:
Granuloma bipolar or safety-pin appearance in
Gram neg, non-motile vulva and if untreated destroys normal vulvar Ciprofloxacin 750mg BID
inguinale smears and specimen taken from the
encapsulated rod Trans: sexual & non-sexual close architecture Erythromycin base 500mg QID
(Donovanosis) ulcers
Common in tropical contact, not highly contagious, Pseudobubo – subQ involvement Azithromycin 1g PO weekly (for pregnant)
Special silver stain to identify Donovan
climates and chronic exposure is needed Secondary bacterial involvement TMP-SMZ 800mg/160mg BID
bodies
to contract the disease
DISEASE ETIOLOGY PATHOGENESIS SSx DIAGNOSIS TREATMENT
Primary: shallow painless ulcer
of the vestibule or labia,
resolves spontaneously Shallow painless ulcer
Chlamydia trachomatis Secondary: painful adenopathy Culture
– majority of cases in (bubo) in inguinal and perirectal, Painful adenopathy (bubo) Direct immunofluorescence Doxycycline 100mg BID for 21 days
Lymphogranuloma men, very disfiguring when untreated becomes “Groove Sign” NAAT of C. trachomatis of pus or Alternatives:
venereum (LGV) Sites: vulva (MC), enlarged, tender and matted aspirate from an infected node Azithromycin 1g PO once a week for 3wks
urethra, rectum, “Groove Sign” Multiple draining sinuses, fistula Complement fixation antibody titer > Erythromycin base 500mg QID for 21d
cervix Tertiary: formation of multiple Elephantiasis, multiple fistulas, stricture 1:64 is indicative of infxn
draining sinuses and fistula, formation of anal canal and rectum
extensive destruction and
secondary extensive scarring
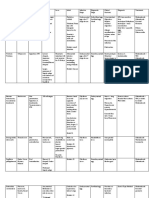
Sexually transmitted, acute,
Gram Stain: “school of fish”
ulcerative dse of the vulva
Culture of purulent material by
Haemophilus ducreyi – Genital ulcers of chancroid
Painful and tender ulcer aspiration of tender lymph nodes Azithromycin 1gm orally
highly contagious small facilitates the transmission of
Tender suppurative inguinal adenopathy Ceftriaxone 250mg IM single dose
Chancroid Gram neg rod, non- HIV
(buboes) Need to culture bec H.ducreyi is Ciprofloxacin 500mg BID for 3d
motile facultative Tissue trauma or excoriation
resistant to multiple antibiotics Erythromycin base 500mg TID for 7d
anaerobe must precede initial infxn since
Susceptibility of bacterial isolates
H.ducreyi is unable to penetrate
should be performed
and invade normal skin
Primary: solitary painless ulcer (chancre),
heals spontaneously, small ulcerated lesion
on labia majora, on Q-tip probing hard Primary, Secondary and Early Latent Phase:
nontender ulcer base, nontender nodulations Benzathine Pen G, 2.4M units IM (safe in
in the inguinal areas pregnant)
Secondary: d/t hematogenous dissem of If Penicillin-allergic / non-pregnant:
Chronic complex systemic dse the spirochetes and is a systemic dse, rashes Doxycycline 100mg BID 14d or
VDRL (Venereal Dse Research Lab) –
Patients are contagious during – red macules and papules over palms and Tetracycline 500mg PO QID 2wks
screening test
Treponema pallidum – the primary, secondary and soles; vulvar lesions – syphilitic lesion,
RPR (Rapid Plasma Reagin) – index for
anaerobic, elongated, probably the 1st yr of latent mucous patches and condyloma latum – pale Late Latent Phase: Benzathine Pen G 2.4M
response to Tx
tightly wound syphilis brown or pale pinkish gray assoc w/ painless units IM at 1 week intervals x 3 doses
Syphilis TIT (Treponema Immobilization Test)
spirochete, can Trans: sexual contact, kissing or adenopathy, slightly raised surface, flat, clean, If Penicillin-allergic / non-pregnant:
FTA-ABS (Fluorescent-labeled
penetrate skin or touching a person who has an moist from exudates, highly infectious Doxycycline 100mg BID 4 wks or
Treponema antibody absorption)
mucous membrane active lesion on the lips, oral Latent: follows secondary, positive serology Tetracycline 500mg PO QID 4wks
MHA-TP (microhemagglutination assay
cavity, breast or genitals w/o SSx of the dse
for antibodies to T.pallidum)
Oral-genital contact Tertiary: potentially destructive effects on Neurosyphilis: Aqueous crystalline Pen G
the CNS, CVS, and musculoskeletal system 18-24M units admin 3-4M units IV q4h for
Late: optic atrophy, tabes dorsalis, 10-14d
generalized paresis, aortic aneurysm, Alternative: Procaine Pen 2.4M units IM OD
gummas (areas of tissue necrosis resulting to + Probenecid 500mg PO QID for 10-14d
ischemia caused by endarteritis and
granulation tissue)) of skin and bones
Normal physiologic vaginal
Fungus (candidiasis) discharge: cervical and vaginal Nonspecific:
Protozoan epithelial cells, normal bacterial Vaginal discharge
(trichomoniasis) flora, water, electrolytes, other Superficial dyspareunia
Vaginitis
Synergistic bacterial chemicals, pH 4.0 Dysuria
infection (bacterial Normal flora: Lactobacilli, Odor
vaginosis) S.epidermidis, E.coli, Vulvar burning
diphtheroids, streptococci
Amsel’s Criteria (3 out 4 to Dx):
Homogenous vaginal discharge Metronidazole 500mg BID for 7d
Shift in vaginal flora from pH > or = 4.5 Metronidazole gel 0.75%, 5g, intravaginally
Lactobacilli-dominant to mixed amine-like odor when mixed w/ KOH OD for 5d
flora (genital microplasmas, (Whiff test) Clindamycin cream 5%, 5g intravaginally
Absence of inflammation in biopsies hence
Bacterial No causative agent has G.vaginalis, anaerobes such as Wet smear demonstrated clue cells > QHS for 7d
the term vaginosis rather than vaginitis
Vaginosis been identified Peptostreptococci, Prevoterall, 20% of the vaginal epithelial cells Alternative:
Mobiluncus) Clindamycin 300mg BID for 7d
Not classified as an STD (more Microscopy: Gold Standard Tinidazole
of sexually-associated dse only) Gram Stain: clue cells – decreased Clindamycin ovules 100g intravaginally at
number of lactobacilli (Nugent criteria HS for 3d
score 7-10)
DISEASE ETIOLOGY PATHOGENESIS SSx DIAGNOSIS TREATMENT
Trichomonas vaginalis
– unicellular,
Profuse frothy discharge w/ unpleasant odor
intracellular, Metronidazole 2g PO single dose
Erythema and edema of vulva and vagina
Trichomonas anaerobic, flagellated NSS smear / wet smear – visualization Tinidazole 2g PO single dose
Transmission: sexually Strawberry cervix and upper vagina
vaginal infection protozoan of the trichomonas organism Alternative: Metronidazole 500mg BID 7d
Vulvar pruritus
Inhabits vagina and Pregnant: Metronidazole 2g PO single dose
Dysuria
LUT, Skene’s ducts in
the female
Saprophytic organisms on the
mucosal surface of the vagina KOH (10-20%) smear – filamentous
w/c becomes opportunistic Pruritus – intense vaginal pruritus forms, mycelia, hyphae (albicans),
Produced by Intravaginal regimens:
when vaginal ecosystem is exacerbated by menses pseudohyphae (non-albicans)
ubiquitous, airborne, Butoconazole, Clotrimazole, Miconazole,
disturbed Vulvar burning
Gram positive fungus Nystatin, Tioconazole, Terconazole
Candida vaginitis Predisposing: hormonal (mens, External dysuria Culture w/ Nickerson or Saboraud
(Candida albicans /
pregnancy), depressed cell-med Dyspareunia medium – useful when KOH smear is
glabrata / tropicalis) – Oral regimens:
immunity (AIDS), DM, obesity, Shallow erosions on the labia and perineum negative or when a woman has
commensal Fluconazole 150mg in a single dose
debilitating dse, antibiotic use Plaques of white cheesy discharge recently treated herself w/ an
(Penicillin, Tetracycline, antifungal
Cephalosporins)
Ectocervicitis – HSV,
severe vaginitis
(strawberry cervix
assoc w/ T.vaginalis or
C. albicans) Hypertrophic and edematous cervix
Inflammatory process assoc w/
Mucopurulent Vaginal discharge
trauma, inflammatory systemic
cervicitis Endocervicitis – Deep dyspareunia
dse, neoplasia, infection
C.trachomatis or Post-coital bleeding
N.gonorrheae,
Bacterial vaginosis and
M.genitalium have also
been associated
Ceftriaxone 250mg IM or
NAAT (Nucleic Acid Amplification
Cefixime 400mg PO + Chlamydia therapy if
Test) – Gold Standard
N.gonorrheae – Gram not ruled out
Culture
negative diplococci Alternative:
Neisseria Localized acute infxn resulting Gram stain
Sites: epithelium of the Purulent urethral discharge w/ edema of the Spectinomycin 2g IM in a single dose or
gonorrheae to bacteremia / disseminated Enzyme immunoassay
GUT, rectum, pharynx meatus Ceftizoxime 500mg IM or Cefoxitin 2g IM +
infection infxn Nucleic Acid Hybridization Test
or the eye Probenecid 1g orally; or Cefotaxime 500mg
Microscopy – stained smear of the
IM
endocervical swab: gram neg
Azithromycin 2g + Chlamydial therapy if
intracellular diplococci
infxn not ruled out
Empiric therapy – recommended in women
at inc. risk of this common STD (age <25yo,
new or multiple sex partners, unprotected
NAAT – Gold Standard sex)
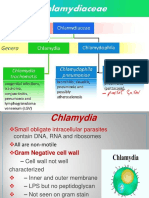
Chlamydia C.trachomatis – Cell culture Azithromycin 1g single dose
Cervical edema and ectopy with
trachomatis obligatory intracellular Microscopy: Doxycycline 100mg BID 7d
mucopurulent exudation
infection organism Direct immunofluorescence test – Alternative:
elementary bodies Erythromycin base 500mg QID for 7d
Erythromycin base 500mg QID for 7d
Ofloxacin 300mg BID for 7d
Levofloxacin 500mg for 7d
This should, in no way, replace the PowerPoint lecture slides.
Use at your own peril.
Prepared by: Paolo Warren (3i)
You might also like
- Sarcoptes Scabei Var. HumanusDocument2 pagesSarcoptes Scabei Var. HumanusZai Ra DianaNo ratings yet
- Notes on Diseases of Cattle: Cause, Symptoms and TreatmentFrom EverandNotes on Diseases of Cattle: Cause, Symptoms and TreatmentNo ratings yet
- Nplex Micro ChartDocument12 pagesNplex Micro Chartapi-26938624100% (2)
- Wuolah Free Bacteria TableDocument11 pagesWuolah Free Bacteria TableELENA FERNANDEZNo ratings yet
- NameDocument2 pagesNamekorikonglibatNo ratings yet
- Cause of AbortionDocument5 pagesCause of Abortioneutamène ramziNo ratings yet
- Gu Tract TableDocument2 pagesGu Tract TableAsela MirandaNo ratings yet
- MB Rickettsiaceae PassDocument2 pagesMB Rickettsiaceae PassJulia IshakNo ratings yet
- Identification by Microimmunofluorescence Test: AKA "Woolster's Disease" Incubation For C. Anthrax Is 1-15 DaysDocument10 pagesIdentification by Microimmunofluorescence Test: AKA "Woolster's Disease" Incubation For C. Anthrax Is 1-15 DaysizzmichikoNo ratings yet
- AAD BF Non TB Cutaneous Mycobact InfectionsDocument3 pagesAAD BF Non TB Cutaneous Mycobact Infectionskahkashanahmed065No ratings yet
- GYNE 4.02 - Lower and Upper Genital InfectionDocument12 pagesGYNE 4.02 - Lower and Upper Genital InfectionGray Snell100% (1)
- TrematodesDocument1 pageTrematodesfatima chrystelle nuñalNo ratings yet
- Sexually-Transmitted Infections and Aids Control Program Sexually Transmitted InfectionsDocument5 pagesSexually-Transmitted Infections and Aids Control Program Sexually Transmitted InfectionsShaira Abigail AninoNo ratings yet
- Gyne - Case 11 Lower Genital UTI PDFDocument2 pagesGyne - Case 11 Lower Genital UTI PDFcbac1990No ratings yet
- Tropical Fevers Table Case 2 by Rahaf AlzoubiDocument1 pageTropical Fevers Table Case 2 by Rahaf AlzoubiR. nounNo ratings yet
- Para Rationale and QuestionsDocument83 pagesPara Rationale and Questionselijah montefalcoNo ratings yet
- Mat 1Document5 pagesMat 1Shainnie IsmaelNo ratings yet
- Tinywow Communicable-Diseases 48897647 18Document1 pageTinywow Communicable-Diseases 48897647 18JULIUS CEZAR QUINAYNo ratings yet
- Dermatology Lectures JRRMMCDocument10 pagesDermatology Lectures JRRMMCGi Em100% (1)
- Ascaris Lumbricoides (Linneaus. 1758) : NEMATODES: IntestinalDocument21 pagesAscaris Lumbricoides (Linneaus. 1758) : NEMATODES: IntestinalPatricia CabisonNo ratings yet
- Infections of The Upper & Lower Genital Tract: Teresita R. Tablizo Fpogs, FpsuogDocument76 pagesInfections of The Upper & Lower Genital Tract: Teresita R. Tablizo Fpogs, FpsuogPrincess Aira Bucag CarbonelNo ratings yet
- Ectopic Phatophysiology Tentative 2Document3 pagesEctopic Phatophysiology Tentative 2Alexe Nicole BiscanteNo ratings yet
- Herpes SimpexDocument1 pageHerpes Simpexmkct111No ratings yet
- Communicable Diseases, Prevention and The Immune SystemDocument4 pagesCommunicable Diseases, Prevention and The Immune SystemTiago JamesNo ratings yet
- OrganismDocument3 pagesOrganismJoanne Alyssa Hernandez LascanoNo ratings yet
- Derm Pathology PDFDocument21 pagesDerm Pathology PDFMara MitrutNo ratings yet
- Corynebacterium Diphtheriae Listeria Monocytogenes Erysipelothrix Rhusopathiae Lactobacillus Spp. Streptomycetes Spp. Nocardia SPPDocument1 pageCorynebacterium Diphtheriae Listeria Monocytogenes Erysipelothrix Rhusopathiae Lactobacillus Spp. Streptomycetes Spp. Nocardia SPPAbcd ReyesNo ratings yet
- Nematodes Common Name Characteristic S Host Disease Produced Diagnosis MOT Location EggsDocument8 pagesNematodes Common Name Characteristic S Host Disease Produced Diagnosis MOT Location EggsGumimba, Ma. Mae JoyceNo ratings yet
- PP Exam 4: Everything That Is in Red Came From Test Your Knowledge!Document15 pagesPP Exam 4: Everything That Is in Red Came From Test Your Knowledge!netanya DoanNo ratings yet
- Approach To Eye DiseasesDocument16 pagesApproach To Eye DiseasesoliverNo ratings yet
- Intestinal-Nematodes PDFDocument3 pagesIntestinal-Nematodes PDFKrisha Marie BadilloNo ratings yet
- ARTHROPODSDocument5 pagesARTHROPODSAis AbulNo ratings yet
- Gyne Lesions TableDocument18 pagesGyne Lesions TableLynx Kee BayatingNo ratings yet
- Abscess Dr. Nasrin Sultana JuyenaDocument4 pagesAbscess Dr. Nasrin Sultana JuyenaShakil MahmodNo ratings yet
- Micro-Para Practical Exam ReviewerDocument8 pagesMicro-Para Practical Exam ReviewerRA TranceNo ratings yet
- Skin PathogensDocument4 pagesSkin PathogensEhi EdialeNo ratings yet
- (Internal) The Epidermis That Grow On The Keratin Present On TheseDocument8 pages(Internal) The Epidermis That Grow On The Keratin Present On TheseAthena Irish LastimosaNo ratings yet
- Diagnosis Other Name Causative Agent Laboratory Procedures Pathognomonic Sign (S) TreatmentDocument4 pagesDiagnosis Other Name Causative Agent Laboratory Procedures Pathognomonic Sign (S) TreatmentEllaine MilarNo ratings yet
- Communicable Diseases of Childhoo1Document3 pagesCommunicable Diseases of Childhoo1esmirikNo ratings yet
- Helminths TableDocument3 pagesHelminths TableAshikin Lee SaniNo ratings yet
- Clinical AND ADVANCE Pathology: TopicDocument7 pagesClinical AND ADVANCE Pathology: TopicNestley TiongsonNo ratings yet
- Tinywow Communicable-Diseases 48897647 20Document1 pageTinywow Communicable-Diseases 48897647 20JULIUS CEZAR QUINAYNo ratings yet
- Nemtodes BelizarioDocument7 pagesNemtodes BelizarioMarl EstradaNo ratings yet
- Terrorism Information ChartDocument15 pagesTerrorism Information ChartAsad Imran100% (1)
- Pinworm, Seatworm Enterobiasis, Pinworm InfectionDocument2 pagesPinworm, Seatworm Enterobiasis, Pinworm InfectionJoan Delos ReyesNo ratings yet
- !DRUGSTUDY CasepresssDocument6 pages!DRUGSTUDY CasepresssAchi AxxxNo ratings yet
- Cattle Diseases and ParasitesDocument6 pagesCattle Diseases and ParasitesNorman Rodriguez LlorandoNo ratings yet
- GYNE 2.01a Lower Genital Tract Infections PDFDocument12 pagesGYNE 2.01a Lower Genital Tract Infections PDFMiguel Domingo100% (1)
- Parasitology Notes: Phasmids: Species Infective Stage Diagnostic Stage Pathology/Notes Diagnosis TreatmentDocument4 pagesParasitology Notes: Phasmids: Species Infective Stage Diagnostic Stage Pathology/Notes Diagnosis TreatmentOrhan AsdfghjklNo ratings yet
- Helminths MicroDocument2 pagesHelminths MicroElena Relacion de VillenaNo ratings yet
- Flash Notes Billie-GeneticsDocument29 pagesFlash Notes Billie-GeneticsschxzerrydawnNo ratings yet
- Gram Pos, Spore Former BacilliDocument5 pagesGram Pos, Spore Former BacilliRach ReyesNo ratings yet
- Lab 4 Ascaris LumbricoidesDocument15 pagesLab 4 Ascaris LumbricoidesAAANo ratings yet
- Chapter 43: Nursing Care of A Family When A Child Has An Infectious Disorder The Infectious Process #1 Infectious Disease in ChildrenDocument20 pagesChapter 43: Nursing Care of A Family When A Child Has An Infectious Disorder The Infectious Process #1 Infectious Disease in ChildrenMark oliver Gonzales100% (1)
- Micro paraDocument2 pagesMicro parafeminaNo ratings yet
- LongDocument4 pagesLongsamakashif1No ratings yet
- S.NO. Name of Procedure Indications Contraindications Articles Required Special Considerations and Precautions 1. Non-Stress Test MaternalDocument4 pagesS.NO. Name of Procedure Indications Contraindications Articles Required Special Considerations and Precautions 1. Non-Stress Test Maternaljyoti ranaNo ratings yet
- Activity 2 CriticalDocument11 pagesActivity 2 CriticalWILJOHN DE LA CRUZNo ratings yet
- Female Genital TractDocument5 pagesFemale Genital Tractsarguss14100% (1)
- Whats New in GINA 2021 FinalDocument47 pagesWhats New in GINA 2021 FinalHeriestian eriesNo ratings yet
- Diets in Fever and AnemiaDocument6 pagesDiets in Fever and AnemiaMonique Angela Turingan GanganNo ratings yet
- Hyperlipidemias and Atherosclerosis Dr. ManaloDocument3 pagesHyperlipidemias and Atherosclerosis Dr. ManaloMonique Angela Turingan GanganNo ratings yet
- Nutrition Screening 2Document2 pagesNutrition Screening 2Monique Angela Turingan GanganNo ratings yet
- Early Nutritional InterventionDocument2 pagesEarly Nutritional InterventionMonique Angela Turingan GanganNo ratings yet
- Normal Urine Output: 30-60ml/min: Protein RequirementsDocument6 pagesNormal Urine Output: 30-60ml/min: Protein RequirementsMonique Angela Turingan GanganNo ratings yet
- Testicular Ca NCCNDocument90 pagesTesticular Ca NCCNMonique Angela Turingan GanganNo ratings yet
- Therapeutic Nutrition - Dr. ManaloDocument2 pagesTherapeutic Nutrition - Dr. ManaloMonique Angela Turingan GanganNo ratings yet
- Legal MedDocument42 pagesLegal Medaisajane_rmt100% (6)
- 2019 Bar ExamDocument7 pages2019 Bar Examnathaniel50% (2)
- Updated Covid GuidelinesDocument42 pagesUpdated Covid GuidelinesMonique Angela Turingan GanganNo ratings yet
- Legal Medicine 1 Dr. RebosaDocument1 pageLegal Medicine 1 Dr. RebosaMonique Angela Turingan GanganNo ratings yet
- Diets in Fever and AnemiaDocument6 pagesDiets in Fever and AnemiaMonique Angela Turingan GanganNo ratings yet
- Legal Medicine - ApmcDocument10 pagesLegal Medicine - ApmcMonique Angela Turingan GanganNo ratings yet
- Legal Medicine ReviewerDocument36 pagesLegal Medicine ReviewerMonique Angela Turingan Gangan100% (1)
- Respiratory DR - AntonioDocument3 pagesRespiratory DR - AntonioMonique Angela Turingan GanganNo ratings yet
- Inborn Errors of Metabolism - JjramDocument4 pagesInborn Errors of Metabolism - Jjramjezreel terreNo ratings yet
- March 5, 2014 Lactose Intolerance in Infants and Children (Dr. Ramolete)Document3 pagesMarch 5, 2014 Lactose Intolerance in Infants and Children (Dr. Ramolete)Monique Angela Turingan GanganNo ratings yet
- Inborn Errors of Metabolism - JjramDocument2 pagesInborn Errors of Metabolism - JjramMonique Angela Turingan GanganNo ratings yet
- Recommended Allowance of Preference ProteinsDocument2 pagesRecommended Allowance of Preference ProteinsMonique Angela Turingan GanganNo ratings yet
- Guidelines On The Proper Recording of Physical Examination FindingsDocument11 pagesGuidelines On The Proper Recording of Physical Examination Findingskitten garciaNo ratings yet
- UGIB Prob Sec To BPUD Vs Gastric Mass Alzheimer's DiseaseDocument7 pagesUGIB Prob Sec To BPUD Vs Gastric Mass Alzheimer's DiseaseMonique Angela Turingan GanganNo ratings yet
- Inborn Errors of Metabolism - JjramDocument2 pagesInborn Errors of Metabolism - JjramMonique Angela Turingan GanganNo ratings yet
- Inborn Errors of Metabolism - JjramDocument4 pagesInborn Errors of Metabolism - Jjramjezreel terreNo ratings yet
- Diets in Fever and AnemiaDocument4 pagesDiets in Fever and AnemiaMonique Angela Turingan GanganNo ratings yet
- Diabetes Mellitus and Therapeutic Nutrition Dr. Manalo February 19, 2014Document4 pagesDiabetes Mellitus and Therapeutic Nutrition Dr. Manalo February 19, 2014Monique Angela Turingan GanganNo ratings yet
- NUTRITION IN THE PRETERM AND SGA INFANTS/ Term Neonates/Children/Athletes-Dr. Ramolete Feb 5, 2014Document6 pagesNUTRITION IN THE PRETERM AND SGA INFANTS/ Term Neonates/Children/Athletes-Dr. Ramolete Feb 5, 2014Monique Angela Turingan GanganNo ratings yet
- Nutrition in Git Diseases - DrramDocument4 pagesNutrition in Git Diseases - DrramMonique Angela Turingan GanganNo ratings yet
- Surgical Nutrition-Dr. Cinio (Edited)Document6 pagesSurgical Nutrition-Dr. Cinio (Edited)Monique Angela Turingan GanganNo ratings yet
- 16 Rickettsiaceae Chlamydiaceae and Cell Wall Deficient Bacteria PDFDocument5 pages16 Rickettsiaceae Chlamydiaceae and Cell Wall Deficient Bacteria PDFAnne MorenoNo ratings yet
- Lesson 33Document6 pagesLesson 33Abdelraouf ElmanamaNo ratings yet
- Chlamydia SeminarDocument110 pagesChlamydia Seminarsuvarnaramesh2007100% (1)
- ChlamydiaDocument45 pagesChlamydiamnn164No ratings yet
- Case On TrachomaDocument20 pagesCase On Trachomadimple alluriNo ratings yet
- Seroepidemiology of Clamaydia TDocument8 pagesSeroepidemiology of Clamaydia TMulatuNo ratings yet
- Pharmacoepidemiology QuestionsDocument11 pagesPharmacoepidemiology Questionsallymyly88100% (1)
- Mycoplasma and CoDocument58 pagesMycoplasma and Coobed cudjoeNo ratings yet
- Last Minute Revision Points - 2018 MicrobiologyDocument27 pagesLast Minute Revision Points - 2018 MicrobiologyPremangshu GhoshalNo ratings yet
- Treatment of Chlamydia Trachomatis InfectionDocument9 pagesTreatment of Chlamydia Trachomatis InfectioneeeeewwwwwNo ratings yet
- MCI FMGE Previous Year Solved Question Paper 2005 PDFDocument32 pagesMCI FMGE Previous Year Solved Question Paper 2005 PDFRuby Bhola100% (1)
- BRS Microbiology Flash-CardsDocument500 pagesBRS Microbiology Flash-CardsAmirsalar Eslami100% (1)
- Chlamydia TrachomatisDocument3 pagesChlamydia Trachomatisexamen grupos grupos examenNo ratings yet
- STI Treatment Guidelines 2012 PDFDocument8 pagesSTI Treatment Guidelines 2012 PDFPaolo Castelblanco VelandiaNo ratings yet
- Microbiology: Atypical Bacteria: Chlamydia, Mycoplasms, LegionellaDocument4 pagesMicrobiology: Atypical Bacteria: Chlamydia, Mycoplasms, LegionellaPatricia Mae de JesusNo ratings yet
- Micro LMRP 2019Document45 pagesMicro LMRP 2019skNo ratings yet
- Chlamydia PosterDocument1 pageChlamydia PosterCharlene WongNo ratings yet
- Safety declaration-EN-03 - 2021Document8 pagesSafety declaration-EN-03 - 2021Abdalazeez AlsayedNo ratings yet
- Male Urethritis With or Without Discharge A ClinicDocument5 pagesMale Urethritis With or Without Discharge A ClinicDian FitriNo ratings yet
- Cestosis y Cestodos PDFDocument14 pagesCestosis y Cestodos PDFErnesto VersailleNo ratings yet
- Congenital and Neonatal Pneumonia PAEDIATRIC RESPIRATORY REVIEWS (2007) 8, 195-203 Michael D. NissenDocument9 pagesCongenital and Neonatal Pneumonia PAEDIATRIC RESPIRATORY REVIEWS (2007) 8, 195-203 Michael D. Nissenroggers72No ratings yet
- 2023 SONBAHAR YDS PDF SistemDocument26 pages2023 SONBAHAR YDS PDF SistemOnur Can GençNo ratings yet
- PhysioEx Exercise 12 Activity 1Document4 pagesPhysioEx Exercise 12 Activity 1t4gjzhpfjcNo ratings yet
- Final Exam MCQsDocument23 pagesFinal Exam MCQsTrang Nguyen50% (2)
- Theme 6 ChlamydiaDocument28 pagesTheme 6 ChlamydiaAmitNo ratings yet
- Module 6.1 MicrobiologyDocument18 pagesModule 6.1 MicrobiologyPNo ratings yet
- Chlamydia&Rickettsia 2023Document29 pagesChlamydia&Rickettsia 2023Alhassn NasserNo ratings yet
- Artrite REATIVAsexualmente ADQUIRIDADocument10 pagesArtrite REATIVAsexualmente ADQUIRIDAYgor AlbuquerqueNo ratings yet
- Microbial Structures and Functions MoicroorganismsDocument390 pagesMicrobial Structures and Functions MoicroorganismssamsoatsNo ratings yet
- Neonatal Pneumonia in Developing Countries: Arch. Dis. Child. Fetal Neonatal EdDocument10 pagesNeonatal Pneumonia in Developing Countries: Arch. Dis. Child. Fetal Neonatal EdadiNo ratings yet