Professional Documents
Culture Documents
Incorporates NICE Bacterial Meningitis and Meningococcal Septicaemia Guideline CG102. Distributed in Partnership With NICE
Uploaded by
LilisOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Incorporates NICE Bacterial Meningitis and Meningococcal Septicaemia Guideline CG102. Distributed in Partnership With NICE
Uploaded by
LilisCopyright:
Available Formats
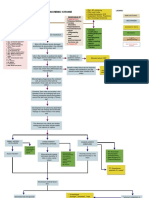
Management of Bacterial Meningitis in Children and Young People BM1 Diagnostic and other laboratory tests:
Take bloods for Blood gas (bicarb, base deficit), Lactate, Glucose, FBC,
U&E, Ca++, Mg++, PO4, Clotting, CRP, Blood cultures, Whole blood
Incorporates NICE Bacterial Meningitis and Meningococcal Septicaemia Guideline CG102. Distributed in partnership with NICE (EDTA) for PCR, X-match. Take Throat swab. If limited blood volume,
Edition 2A prioritise blood gas, lactate, glucose, electrolytes, FBC, clotting.
Meningococcal Symptoms and signs of bacterial meningitis?
Disease Algorithm BM2 Contraindications to Lumbar Puncture
YES Endorsed by
www.meningitis.org Clinical or radiological signs of raised intracranial pressure
Check airway, breathing and circulation; gain vascular access
Shock
After convulsions until stabilised
YES Coagulation abnormalities
Signs of raised intracranial pressure (RICP) or shock? - Clotting study results (if obtained) outside the normal range
NO - Platelet count below 100 x 109/L
- on Anticoagulant therapy
Perform diagnostic tests BM1 Correct any dehydration Local superficial infection at LP site
Respiratory insufficiency.
NO Perform Lumbar Puncture Perform delayed LP in children with suspected bacterial meningitis
Contraindication to Lumbar Puncture? BM2 when contraindications no longer present
Do not await CSF results before starting antibiotics
Empiric antibiotics for suspected meningitis YES BM3 Contraindications to Ceftriaxone
IV Cefotaxime + either Amoxicillin or Ampicillin Premature neonates with corrected gestational age < 41 weeks and
<3 months old?
(can replace Cefotaxime with Ceftriaxone if no other neonates <1 month old, particularly those with jaundice,
contraindication BM3) YES NO hypoalbuminaemia, or acidosis; or receiving concomitant treatment
DO NOT DELAY ANTIBIOTICS Empiric antibiotics for suspected meningitis with intravenous calcium.
IV Ceftriaxone unless contraindicated BM3
Add Vancomycin if recently overseas, or prolonged or multiple antibiotic exposure within last 3 months. DO NOT DELAY ANTIBIOTICS
BM4 Indications for CT scan in children with suspected bacterial
meningitis
NO CT scan cannot reliably detect raised intracranial pressure. This should
LP results available?
be assessed clinically.
YES Perform a CT scan to detect other intracranial pathologies if GCS ≤8 or
focal neurological signs in the absence of an explanation for the clinical
NO Lumbar puncture suggests meningitis? features.
In neonates (<28 days old), ≥ 20 cells/µl In older children > 5 cells/µl or > 1 neutrophil/µl Do not delay treatment to undertake a CT scan.
(if lower cell count, still consider bacterial meningitis if other symptoms and signs suggest the diagnosis especially in neonates). Clinically stabilise the child before CT scanning.
Consult a paediatric intensivist, anaesthetist, or intensivist.
YES
NICE Fever in under
BM5 Indications for tracheal intubation and mechanical ventilation
5s guideline CG160 Consider TB meningitis If raised CSF WCC and risk factors for TB. If TB meningitis in differential diagnosis
www.nice.org.uk/ refer to NICE TB NG33 for appropriate antibiotic treatment Threatened or actual loss of airway patency (e.g. GCS <9, response to
guidance/cg160 pain only).
Consider Herpes simplex meningoencephalitis. If HSV in differential diagnosis give Aciclovir. Need for any form of assisted ventilation e.g. bag–mask ventilation.
Clinical observation of increased work of breathing
Hypoventilation or Apnoea
Steroids: Dexamethasone 0.15 mg/kg to a max dose of 10 mg, qds x 4 days for children ≥ 3 months old IF ≤ 12h from first antibiotics and LP shows: Features of respiratory failure, including
frankly purulent CSF CSF WCC > 1000/µl raised CSF WCC and protein > 1 g/L bacteria on Gram stain. - Irregular respiration (e.g. Cheyne–Stokes breathing)
Steroids should not be used in developing countries. - Hypoxia (saturation <94% in air, PaO2 < 13 kPa or 97.5mmHg),
If TB meningitis in the differential diagnosis, refer to NICE NG33 before administering steroids. hypercapnoea (PaCO2 > 6 kPa or 45 mmHg)
Continuing shock following 40ml/kg of resuscitation fluid
Signs of raised intracranial pressure
Impaired mental status
Reduced or fluctuating conscious level or focal neurological signs? BM4 YES
Perform CT Scan - GCS drop of ≥ 3, or score <9, or fluctuation in conscious level
- Moribund state
NO Control of intractable seizures
Need for Stabilisation for brain imaging or for transfer to PICU.
Full-volume maintenance fluids: enteral feeds if tolerated or isotonic IV fluids e.g. 0.9% Saline or 0.9% Saline with 5% Glucose Should be undertaken by a health professional with expertise in
Do not restrict fluids unless there is evidence of increased anti-diuretic hormone secretion or RICP paediatric airway management, Consult PICU. (See MD4)
Monitor fluid administration, urine output, electrolytes and blood glucose
See Meningococcal Disease Algorithm to treat seizures.
BM6 Repeat LP in neonates after starting treatment if:
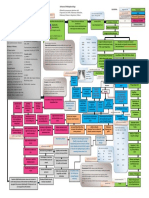
Antibiotics for confirmed meningitis persistent or re-emergent fever, new clinical findings (especially
Meningococcus: IV Ceftriaxone for 7 days neurological findings), deteriorating clinical condition, or persistently
H influenzae: IV Ceftriaxone for 10 days abnormal inflammatory markers
Close monitoring for signs of Raised ICP, Shock & repeated review
S pneumoniae: IV Ceftriaxone for 14 days, add
Go to Meningococcal Disease Algorithm if signs are found and consult a paediatric intensivist, anaesthetist, or intensivist BM7
Vancomycin if resistant strain. Long-term management: Before discharge consider need for after
Perform delayed LP if no longer contraindicated BM2
care, discuss potential long-term effects with parents, arrange hearing
Group B Strep: IV Cefotaxime for ≥ 14 days If LP contraindicated, perform delayed LP when no longer contraindications.
test. Refer children with severe or profound deafness for cochlear
L monocytogenes: IV Amoxicillin or Ampicillin for
implant assessment ASAP. Use MRF discharge checklist
21 days in total, plus IV Gentamicin for at least http://www.meningitis.org/assets/x/55764. Provide ‘Your Guide’ and
the first 7 days YES NO direct to meningitis support organisations www.meningitis.org/recovery
Gram-negative bacilli: IV Cefotaxime for
Specific pathogen identified? Antibiotics for unconfirmed meningitis
or www.meningitisnow.org/recovery. Offer further care on discharge as
≥ 21 days (unless alternative directed by local needed. Paediatrician to review child with results of their hearing test 4-6
antimicrobial resistance patterns or specific weeks after discharge from hospital considering all potential morbidities
sensitivities) <3 months old? and offer referral. Inform GP, health visitor or school nurse.
Unless directed otherwise by antibiotic sensitivities.
Duration may be dictated by clinical response – IV Cefotaxime (or Ceftriaxone unless contraindicated BM3 ) YES NO IV Ceftriaxone for Based on NICE CG102 www.nice.org.uk/guidance/CG102
discuss with infectious disease specialist. + either Amoxicillin or Ampicillin IV for ≥ 14 days. ≥10 days. Authors AJ Pollard (GDG chair), A Cloke, SN Faust, L Glennie, C Haines, PT Heath, JS Kroll,
M Levin, I Maconochie, S McQueen, P Monk, S Nadel, N Ninis, MP Richardson, MJ Thompson,
AP Thomson, D Turner.
Notify public health, prophylaxis see MD11 on Meningococcal disease algorithm; Long-term management BM7 Further copies from www.meningitis.org or 080 88003344. © Meningitis Research Foundation 08/18
A charity registered in England and Wales no 1091105 and in Scotland no SC037586.
You might also like
- Pericarditis Vs Mi: Internal Medicine: CvsDocument6 pagesPericarditis Vs Mi: Internal Medicine: CvsRojales FrancisNo ratings yet
- Ancient Norse RunesDocument19 pagesAncient Norse Runess_avgerNo ratings yet
- Pediatric Surgery Handbook For Residents and Medical Students (2017)Document428 pagesPediatric Surgery Handbook For Residents and Medical Students (2017)Oana Stefania Pintilii100% (1)
- Simple Note On Medical ApproachDocument7 pagesSimple Note On Medical ApproachSyaidatul NadwaNo ratings yet
- Family Safety HandbookDocument12 pagesFamily Safety HandbookAdib_dokterNo ratings yet
- Palmistry ExpertiseDocument65 pagesPalmistry ExpertisePawan AgrawalNo ratings yet
- Saint PatrickDocument1 pageSaint PatrickAnalía Cimolai0% (1)
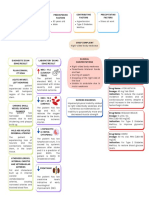
- Acute Ischemic Stroke Concept MapDocument6 pagesAcute Ischemic Stroke Concept MapMoonyeen Jann Casera Balic100% (2)
- Eurocode 7 Section 7 Pile FoundationsDocument20 pagesEurocode 7 Section 7 Pile FoundationsHoNo ratings yet
- Pathophysiology of Acute Renal FailureDocument1 pagePathophysiology of Acute Renal FailureAina HaravataNo ratings yet
- List of Documents ISO 45001 Documentation Toolkit enDocument2 pagesList of Documents ISO 45001 Documentation Toolkit enCiciaSalatin100% (1)
- Mis C Clinical GuidelineDocument9 pagesMis C Clinical GuidelineasyqarNo ratings yet
- Drug StudyDocument30 pagesDrug StudyClaire MachicaNo ratings yet
- PATENT DUCTUS ARTERIOSUS Concept MapDocument2 pagesPATENT DUCTUS ARTERIOSUS Concept MapErika CadawanNo ratings yet
- Advanced Pathophysiology of Respiratory Failure and Other Underlying Resp Diseases With LegendDocument1 pageAdvanced Pathophysiology of Respiratory Failure and Other Underlying Resp Diseases With LegendTeanu Jose Gabrillo TamayoNo ratings yet
- Nursing Care Plan For HELLP SyndromeDocument17 pagesNursing Care Plan For HELLP SyndromeRosemarie Carpio75% (4)
- Simplified Modified Compression Field Theory For Calculating Shear Strength of Reinforced Concrete ElementsDocument11 pagesSimplified Modified Compression Field Theory For Calculating Shear Strength of Reinforced Concrete ElementsTooma David100% (1)
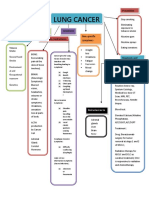
- Concept Map LungDocument1 pageConcept Map LungThea Eya FayeNo ratings yet
- Colloquia Latina D Ooge PDFDocument104 pagesColloquia Latina D Ooge PDFHadaixx100% (1)
- Skill Checklist Applying An Extremity RestraintDocument2 pagesSkill Checklist Applying An Extremity RestraintAsep BageurNo ratings yet
- Metoprolol Drug StudyDocument4 pagesMetoprolol Drug StudyCrisha Ann Billones BacutaNo ratings yet
- 2nd - NCPDocument3 pages2nd - NCPjoidaNo ratings yet
- Acute Coronary Syndrome Workup Approach Considerations, Electrocardiography, Measurement of CK-MB LevelsDocument1 pageAcute Coronary Syndrome Workup Approach Considerations, Electrocardiography, Measurement of CK-MB LevelsfeaghNo ratings yet
- Name and Classification of DrugDocument3 pagesName and Classification of DrugAnicas, Ralph Joshua V.No ratings yet
- Feb DTRDocument3 pagesFeb DTRFeb NamiaNo ratings yet
- MIS-C: Clinic-Diagnostic/Dispo Recs For Multisystem Inflammatory Syndrome in ChildrenDocument8 pagesMIS-C: Clinic-Diagnostic/Dispo Recs For Multisystem Inflammatory Syndrome in ChildrenJosselle Sempio CalientaNo ratings yet
- Pediatric Shock StatesDocument32 pagesPediatric Shock StatessavasNo ratings yet
- Khorsand 2023 Not All Shock States Are Created EqualDocument25 pagesKhorsand 2023 Not All Shock States Are Created EqualLê Huy HoàngNo ratings yet
- 11 - Management Post Operative Low Cardiac Output SyndromeDocument46 pages11 - Management Post Operative Low Cardiac Output SyndromeNat SNo ratings yet
- AGLIAM, Dwight Jeremy D. BSN Ii-Intl GRP B 10/15/2018Document3 pagesAGLIAM, Dwight Jeremy D. BSN Ii-Intl GRP B 10/15/2018Dwight Jeremy DeVera AgliamNo ratings yet
- Onco ImDocument2 pagesOnco ImAlexandra BascoNo ratings yet
- RUG Tudy: Medicatio N Action Indication Contraindication Adverse Effects Nursing Considerati ONDocument4 pagesRUG Tudy: Medicatio N Action Indication Contraindication Adverse Effects Nursing Considerati ONGiselle EstoquiaNo ratings yet
- Name of Drug Dosage, Route, and Frequency Drug Action Indication Contraindication Adverse Effects Nursing ConsiderationsDocument3 pagesName of Drug Dosage, Route, and Frequency Drug Action Indication Contraindication Adverse Effects Nursing ConsiderationsAngelou MortosNo ratings yet
- Septic Shock For SiteDocument3 pagesSeptic Shock For Siteمحمد زينNo ratings yet
- Why LAMA Is Fundamental Treatment For COPD: Rudi DermawanDocument29 pagesWhy LAMA Is Fundamental Treatment For COPD: Rudi DermawanwitwiiwNo ratings yet
- Diagnostic Test and Laboratory TestDocument7 pagesDiagnostic Test and Laboratory TestampalNo ratings yet
- 3Document1 page3Ayesha Mae Baniaga DoctoleroNo ratings yet
- Ineffective Cerebral Tissue PerfusionDocument4 pagesIneffective Cerebral Tissue PerfusionLeticia ElricNo ratings yet
- Categorize The Treatment Options For Patients With Existing Medical ConditionDocument3 pagesCategorize The Treatment Options For Patients With Existing Medical ConditionMicah LatosaNo ratings yet
- Second Degree Av Block Type 1 (Mobitz I or Wenckebach)Document1 pageSecond Degree Av Block Type 1 (Mobitz I or Wenckebach)christine louise bernardoNo ratings yet
- Pediatric Shock (PICUCOURSE)Document40 pagesPediatric Shock (PICUCOURSE)surasuarezlopezNo ratings yet
- Surgery FADocument170 pagesSurgery FArafeekwalid551No ratings yet
- Co AmoxyclavDocument2 pagesCo AmoxyclavHaneulNo ratings yet
- Pediatric Shock: Dr. Lilia Dewiyanti, Spa, MsimedDocument40 pagesPediatric Shock: Dr. Lilia Dewiyanti, Spa, MsimedLa Ode RinaldiNo ratings yet
- Labs:: Pulmonary Renal Syndromes (PRS) Diffuse Alveolar HemorrhageDocument1 pageLabs:: Pulmonary Renal Syndromes (PRS) Diffuse Alveolar HemorrhageRonald MoralesNo ratings yet
- CeftriaxoneDocument3 pagesCeftriaxonejiloNo ratings yet
- Shock States in ChildrenDocument37 pagesShock States in ChildrenjuanitaNo ratings yet
- 8-Ecg in CovidsDocument35 pages8-Ecg in CovidsyandraNo ratings yet
- Pathophysiology of AllDocument1 pagePathophysiology of AllBGHMC PEDIAHONo ratings yet
- PathophysiologyDocument1 pagePathophysiologyArt Lemuel LotereñaNo ratings yet
- Case Chest Pain and DyspneaDocument1 pageCase Chest Pain and DyspneaVineeNo ratings yet
- Celecoxib Drug Study WWW RNpedia ComDocument3 pagesCelecoxib Drug Study WWW RNpedia ComAngelou MortosNo ratings yet
- Dopamine HydrochlorideDocument1 pageDopamine HydrochlorideJoannes SanchezNo ratings yet
- Estados de ChoqueDocument25 pagesEstados de ChoqueKarina Moreno PalacioNo ratings yet
- Bagian Ilmu Kesehatan Anak FK UNSRAT/ RSU. Prof. Dr. R.D. Kandou-ManadoDocument29 pagesBagian Ilmu Kesehatan Anak FK UNSRAT/ RSU. Prof. Dr. R.D. Kandou-ManadoAmarantoNo ratings yet
- Drug Study (Print3copiesDocument8 pagesDrug Study (Print3copiesPhylum ChordataNo ratings yet
- Pulmonary Edema: Mycobacterium Tuberculosis Patient BackgroundDocument1 pagePulmonary Edema: Mycobacterium Tuberculosis Patient BackgroundAubrey RecierdoNo ratings yet
- Drug Study Emergency DrugsDocument6 pagesDrug Study Emergency DrugsJhessa Curie PitaganNo ratings yet
- MIB 3 AnnotatedDocument78 pagesMIB 3 AnnotatedShekhar NandalNo ratings yet
- Fluid and Electrolyte ImbalanceDocument18 pagesFluid and Electrolyte ImbalanceKaren PiliNo ratings yet
- Shock in Covid PatientDocument21 pagesShock in Covid PatientGHALEB A. AlmekhlafiNo ratings yet
- 2019 LAMA For COPDDocument25 pages2019 LAMA For COPDdonnyNo ratings yet
- Updates On Pulmonary HypertensionDocument39 pagesUpdates On Pulmonary HypertensionZurlin DwirostantinNo ratings yet
- Jantung - Acute Heart FailureDocument32 pagesJantung - Acute Heart FailurefaradibaNo ratings yet
- Dilantin (Phenytoin) : Drug Classification Actions Side Effects ConsiderationsDocument4 pagesDilantin (Phenytoin) : Drug Classification Actions Side Effects ConsiderationsbreehaireNo ratings yet
- Cardiac Care and COVID-19: Perspectives in Medical PracticeFrom EverandCardiac Care and COVID-19: Perspectives in Medical PracticeNo ratings yet
- Insulin Degludec PDFDocument19 pagesInsulin Degludec PDFLilisNo ratings yet
- Steiner2010 PDFDocument14 pagesSteiner2010 PDFLilisNo ratings yet
- Gestational AgeDocument7 pagesGestational AgeLilisNo ratings yet
- Denver II, Dev DelDocument11 pagesDenver II, Dev DelLilisNo ratings yet
- ZILLENIALSDocument1 pageZILLENIALSakhilNo ratings yet
- Everyday2 M8 S2 Student GrammarDocument2 pagesEveryday2 M8 S2 Student GrammarIvan MQNo ratings yet
- Test 1Document15 pagesTest 1Ngọc ÁnhNo ratings yet
- M M M MMMMMMMMMMMMMMMMM MMMMMM MMMM MMMMMMMMM MMMMMMMMMMMMMMMMMM M M ! MM MMM"MM M MMM#MMMM M MMDocument8 pagesM M M MMMMMMMMMMMMMMMMM MMMMMM MMMM MMMMMMMMM MMMMMMMMMMMMMMMMMM M M ! MM MMM"MM M MMM#MMMM M MMcool_vjk4b9No ratings yet
- Cambodia V ThailandDocument22 pagesCambodia V ThailandMaria QadirNo ratings yet
- Favour Emmanuel - Resume - Data AnalystDocument3 pagesFavour Emmanuel - Resume - Data AnalystEmmanuel FavourNo ratings yet
- Guidelines On Cadastral (2017 Edition Final)Document29 pagesGuidelines On Cadastral (2017 Edition Final)Olaitan RasheedNo ratings yet
- Leadership and FollowershipDocument10 pagesLeadership and FollowershipLawrence ConananNo ratings yet
- Coop Conference Proceeding (21-22aug 2022)Document585 pagesCoop Conference Proceeding (21-22aug 2022)oliviahuda75No ratings yet
- VLD 6000 AIS Airborne Transponder PDFDocument2 pagesVLD 6000 AIS Airborne Transponder PDFShin Ami IgamiNo ratings yet
- Alargamiento Del Complejo Gastronemio SoleoDocument8 pagesAlargamiento Del Complejo Gastronemio SoleoC Martin TraumatoNo ratings yet
- EC6802 Wireless Networks Important PART-A &B Questions With AnswersDocument21 pagesEC6802 Wireless Networks Important PART-A &B Questions With AnswersohmshankarNo ratings yet
- Chemistry Test 11 Chap 1-5Document2 pagesChemistry Test 11 Chap 1-5Sabitra RudraNo ratings yet
- Punk Science - Inside The Mind of GodDocument3 pagesPunk Science - Inside The Mind of GodRobert Garcia0% (2)
- Sampel Cylinder 1 (MS-01-177) R0Document6 pagesSampel Cylinder 1 (MS-01-177) R0herysyam1980No ratings yet
- Impact TestDocument11 pagesImpact TestMohsin AbbasNo ratings yet
- Compresor Atlas Copco GA30Document16 pagesCompresor Atlas Copco GA30Florin Maria Chirila100% (1)
- Parts of Speech (Updated) - 1Document33 pagesParts of Speech (Updated) - 1Ramzan MemonNo ratings yet
- uC-GUI UserDocument920 pagesuC-GUI Userpmih1No ratings yet