Professional Documents
Culture Documents
Pharmaceutical Sciences: Frequency of Pre-Analytical Phase Errors in A Clinical Chemistry Laboratory
Uploaded by
Ayesha MehmoodOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmaceutical Sciences: Frequency of Pre-Analytical Phase Errors in A Clinical Chemistry Laboratory
Uploaded by
Ayesha MehmoodCopyright:
Available Formats
IAJPS 2019, 06 (05), 8906-8909 Muhammad Zubair et al ISSN 2349-7750
CODEN [USA]: IAJPBB ISSN: 2349-7750
INDO AMERICAN JOURNAL OF
PHARMACEUTICAL SCIENCES
http://doi.org/10.5281/zenodo.2667728
Available online at: http://www.iajps.com Research Article
FREQUENCY OF PRE-ANALYTICAL PHASE ERRORS IN A
CLINICAL CHEMISTRY LABORATORY
1
Dr Muhammad Zubair, 2Dr Ahmed Raza, 3Dr Tahir Mahmood
1
PGR, Department of Chemical Pathalogy Chughtai Lab Lahore, 2Quaide Azam Medical College
Bahawalpur, 3Demonstrator Physiology at Sahara Medical College Narowal.
Article Received: March 2019 Accepted: April 2019 Published: May 2019
Abstract:
Objective:To find out the leading cause of pre analytical error in a clinical chemistry laboratory.
Duration and place: This study was conducted in clinical chemistry laboratory at Chughtai Lab Lahore over a period
of 1 year from January 2018 to December 2018.
Method:It was a retrospective study which had been carried out to find out the frequency of various factors affecting
the preanalytical phase of total laboratory testing. Data were gathered by the help of laboratory technologist who
were register data of rejections, and causes for rejections of all the samples which were sent to clinical chemistry
laboratory for analysis.
Results: Of the 518765 tubes received during the data collection period, 1792 samples were found unsuitable for
further processing. This accounted for 0.34% of all samples collected n the laboratory. Rejections arose as a result
of the following reasons: 1256(0.24%) specimens had hemolysis ; 147(0.03%) had insufficient sample quantity,
389(0.07%) had compromised or unsatisfactory results.
Conclusion: Of all the samples received in the lab, the overall percentage of rejection is 0.34%.
Corresponding author:
Dr. Muhammad Zubair, QR code
PGR, Department of Chemical Pathalogy Chughtai Lab Lahore.
Please cite this article in press Muhammad Zubair et al., Frequency Of Pre-Analytical Phase Errors In A Clinical
Chemistry Laboratory., Indo Am. J. P. Sci, 2019; 06(05).
www.iajps.com Page 8906
IAJPS 2019, 06 (05), 8906-8909 Muhammad Zubair et al ISSN 2349-7750
INTRODUCTION: process and the effectiveness of its policies and
Laboratory medicine quality can be defined as the procedures.Quality assurance is a component of total
provision of confirmation that the report which is quality management and deal with all the three phase
delivered to patient or clinician is accurate and reliable of laboratory testing pre analytical,analytical and post
and which is helpful for the making of clinical decision analytical.
and effective patient care [1]. The generation of any
laboratory test involves various important steps like, The rationale of this study was to enumerate and
Ordering of test from physician, specimen collection, analyze the frequency of different preanalytical errors
identification ,transportation ,separation or that occur during sample processing in the clinical
preparation, analysis ,reporting and provision of chemistry and immunology laboratory so that we can
results.The errors in these various steps of lab testing improve those areas which leads to sample rejection in
constitute the total laboratory errors which can be our laboratory set up.
further divided in to three components : pre analytical
,analytical, post analytical [2]. Pre analytical errors are MATERIAL AND METHOD:
those errors which occur before the analysis of the The study was conducted in the department of clinical
specimen and account for 65- 70% total laboratory chemistry and immunology of chughtai institute of
errors. The most commonly reported types of pre- pathology from January 2018 to December 2018.The
analytical error are: a) wrong or missing clinical chemistry department equipped with state of
identification, b) haemolysed, clotted, and insufficient the art equipment like, Architect CI 8200, Alinity
samples, c) inappropriate containers, f) inappropriate CI,Liasion XL, immulite XPr 2000,Helios,Blue dot
blood to anticoagulant ratio, and g) inappropriate driver, Alegria,cobas e411.
transport and storage condition [3,4].
The data collection procedure involved review of
Analytical errors are those errors which occur during blood samples received from the main head office
the analysis of the specimens on the analyzer and reception as well as from collection points of
account for 15 to 20 % laboratory error. There is a laboratory situated at various cities. Venous blood
great reduction in these errors over a couple of years samples are considered unsuitable according to the
due to standardization of analytic techniques, increase following accepted criteria: quantity not sufficient,
stability of reagents, advance instrumentation, wrong or missing patient identification, inappropriate
innovation in information technology, quality control specimen container, visible hemolysis after
and quality assurance methods. centrifugation, lipemic or turbid samples.
Post analytical phase errors are those errors which are RESULTS:
caused by interruption in result transmission from A total of 518765 specimens were received over the
analyser to laboratory information system, course of one year in department of clinical chemistry
transcription related errors, incorrect interpretation. and immunology from head office reception as well as
Total quality management program monitor and from various collection points of the laboratory which
evaluate the ongoing and overall quality of total testing are situated at various cities of Pakistan.
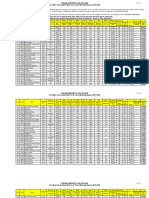
Frequency of various pre analytical errors
Total number of specimens 518765
Total number of samples rejected 1792(0.34%)
Total number of samples Hemolyzed 1256(0.24%)
Total number of samples Quantity not sufficient 147(0.03%)
Total number of samples Compromised or 389(0.07%)
unsatisfactory results(wrong container,EDTA
contamination, inappropriate time for sampling
A total of 1792 specimens had been rejected on the ,EDTA contamination ,turbidity of specimen
basis of our specimen rejection criteria.Most common ,inappropriate time of sampling and account for
cause of specimen rejection was hemolyzed specimen rejection of 389 specimens.Only 147 specimens were
which account rejection of 1256 specimen over a rejected on the basis of insufficiency of sample volume
period of one year.Secondly the specimen which were in our laboratory. Percentage of all errors in table1:
rejected were those which have wrong container
www.iajps.com Page 8907
IAJPS 2019, 06 (05), 8906-8909 Muhammad Zubair et al ISSN 2349-7750
DISCUSSION: Another factor leading to rejection of blood samples in
During the last few decades, laboratory medicine had our study was insufficient blood volume. Every
been revolutionized by transformation of laboratory analytical process requires a fixed volume of
diagnostics from manual, cumbersome testing serum/plasma for analysis. The main reasons behind
methods to fully automated science, ensuring accuracy this error are ignorance of the phlebotomists, difficult
and speedy analysis. However, the laboratory cannot sampling as in pediatric patients, patients with chronic,
function in isolation. It is dependent upon other debilitating diseases, and patients on chemotherapy
departments, mainly the clinical division for properly whose thin veins are difficult to localize.
filled requisition slips and samples for analysis.
Evidence indicate that accuracy and reliability in test These data are comparable to those provided by other
can not achieved by only improving the analytical investigators, which confirm that problems directly
phase but The phases before the sample reaches the related to specimen collection are the main cause of
laboratory (preanalytical) and the phase after the preanalytical errors, especially hemolyzed, clotted,
sample is analyzed (post-analytical) are equally insufficient, and incorrect samples. [6] [8].
important. The pre analytical phase is accompanied by
many short comings ranging from contamination of With the exclusive use of vacutainers, the frequency of
specimens due to non following the proper order of errors found in our study is 1.5%. It is clear from the
draw and lack of awareness of the staff about ideal above discussion that incorrect phlebotomy practices
phlebotomy procedures. The health care provider must are the main reason behind preanalytical errors. The
be more diligent in applying scientific knowledge to reason for incorrect phlebotomy practice includes lack
reduce the errors in this pre analytical phase. of awareness or possibly a heavy workload. This is the
reason phlebotomy has been considered a separate
According to one study conducted by Plebani and area of improvement for medical technicians in
Carraro the highest frequency of errors result from developed countries. Those of us in developing nations
problems in the preanalytical or post-analytical must adopt a similar approach toward phlebotomy and
phases. Hemolysis accounted for the majority of initiate steps for the inculcation of ideal phlebotomy
rejections in our study. There are lot of factors which practices among health care workers.
leads to hemolysis of specimens like blood is forced
through a fine needle, shaking the tubes vigorously, CONCLUSION:
and centrifuging the specimens before clotting is com- The concept of total quality management encompasses
plete.4 Red top tube without any preservative should all the steps involved in sample processing, beginning
not be shaken after the sample has been collected, and from test ordering to the final interpretation of results
plasma tubes should be gently inverted a few times so by the clinicians to reduce or eliminate the errors that
the anticoagulant mixes with the blood. In another may arise during the various steps. The promotion of
study by Jay and colleagues, the majority of ideal phlebotomy practices and sample transport
hemolyzed samples (>95%) could be attributed to in procedures is a pre-requisite for the efficacy of
vitro processes resulting from incorrect sampling laboratory functioning. The dependence on accurate
procedure or transportation errors. Hemolysis leads to laboratory results for diagnostics makes it mandatory
the extravasation of intracellular contents into the for labs to ensure accountability and accuracy of
plasma, leading to false high values of potassium and results to negate incorrect diagnosis as a consequence
intracellular enzymes such as ALT and LDH. It also of faulty reporting. A practice of keeping a record of
leads to delay in reporting of results due to the need the errors at all stages of analysis and then devising
for fresh specimens for processing the request. corrective strategies for their prevention can gradually
free a laboratory from such errors. Adoption of quality
To overcome the errors in pre analytical phase , we control in all the phases and not merely the analytical
have developed standard operating procedures (SOPs) processes and regular appraisal and audits is necessary
for the different steps involved in ideal laboratory to safeguard patient interests and deliver our services
operations and ethics. Regular training and awareness to society.
sessions of phlebotomist and specimen transporters are
conducted at regular interval by quality management REFERENCES:
department. The samples are thereby transported to 1. Bonini P, Plebani M, Ceriotti F, et al. Errors in
our laboratory from the collection center by our staff laboratory medicine. Clin Chem. 2002;48:691–
following the basic precautions that must be adhered 698.
to during transportation. 2. Lippi G, Blanckaert N, Bonini P, et al. Causes,
consequences, detection and prevention of
www.iajps.com Page 8908
IAJPS 2019, 06 (05), 8906-8909 Muhammad Zubair et al ISSN 2349-7750
identification errors in laboratory diagnostics. 9. Green SF. The cost of poor blood specimen
Clin Chem Lab Med. 2009;47:143–153. quality and errors in preanalytical processes. Clin
3. Romero A, Munoz M, Ramos JR, et al. Biochem. 2013;46(13):1175-1179
Identification of preanalytical mistakes in the stat 10. Plebani M. Exploring the iceberg of errors in
section of the clinical laboratory. Clin Chem Lab laboratory medicine. Clin Chim Acta.
Med. 2005;43:974–975. 2009;404(1):16-23.
4. Carraro P, Plebani M. Errors in a stat laboratory: 11. Plebani M. Errors in clinical laboratories or errors
Types and frequencies 10 years later. Clin Chem. in laboratory medicine? Clin Chem Lab Med.
2007;53:1338–1342. 2006;44(6):750-759.
5. Bonini P, Plebani M, Ceriotti F, Rubboli F. Errors 12. Plebani M. Laboratory errors: How to improve
in laboratory medicine. Clin Chem 2002;48:691- pre- and post-analytical phases Biochemia
8. Medica. 2007;17(1):5-9.
6. Young DS. Effects of preanalytical variables on 13. Chawla R, Goswami B, Tayal D, et al.
clinical laboratory tests. 3rd ed. Washington, DC: Identification of the types of preanalytical errors
AACCPress, 2007 in the clinical chemistry laboratory: 1-year study
7. Plebani M, Sciacovelli L, Aita A, Chiozza ML. at G.B. Pant Hospital. LabMedicine. 2010;41:89-
Harmonization of pre-analytical quality 92.
indicators. Biochem Med 2014;24:105-13. 14. Lippi G, Bonelli P, Rossi R, et al. Development of
8. Hawkins R. Managing the pre- and post-analytical a preanalytical errors recording software.
phases of the total testing process. Ann Lab Med. Biochem Med. 2010;20:90-95.
2012;32(1):5-16.
www.iajps.com Page 8909
You might also like
- Accurate Results in the Clinical Laboratory: A Guide to Error Detection and CorrectionFrom EverandAccurate Results in the Clinical Laboratory: A Guide to Error Detection and CorrectionRating: 5 out of 5 stars5/5 (1)
- Cipero & Guaracara River Water Quality Site VisitsDocument76 pagesCipero & Guaracara River Water Quality Site VisitsBrandon Atwell79% (29)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 8 Parts of Speech PRINTDocument16 pages8 Parts of Speech PRINTNabila Nasser100% (2)
- Russian and US Mind Control Technology Psychotronic WarDocument123 pagesRussian and US Mind Control Technology Psychotronic WardropsyNo ratings yet
- Three Years' Experience of Quality Monitoring Program On Pre-Analytical Errors in ChinaDocument7 pagesThree Years' Experience of Quality Monitoring Program On Pre-Analytical Errors in ChinaCenyiqanita NurqanitaNo ratings yet
- Biomed 24 3 376Document7 pagesBiomed 24 3 376adrianaNo ratings yet
- Mistakes in A Stat Laboratory: Types and Frequency: Clinical Chemistry September 1997Document5 pagesMistakes in A Stat Laboratory: Types and Frequency: Clinical Chemistry September 1997Othman MaaiNo ratings yet
- Muestras No Conformes en Fase PreanaliticaDocument7 pagesMuestras No Conformes en Fase PreanaliticaYaquelin VelasquezNo ratings yet
- TAT Pre AnalitikDocument6 pagesTAT Pre AnalitikPOKJA PPNo ratings yet
- JLP 10 237Document4 pagesJLP 10 237Nur Muhammad IsmatullohNo ratings yet
- Tube Validation - Dr. Tester AshavaidDocument87 pagesTube Validation - Dr. Tester Ashavaidgonteng sadyogaNo ratings yet
- Review Article: Pre-Analytical Phase in Clinical Chemistry LaboratoryDocument8 pagesReview Article: Pre-Analytical Phase in Clinical Chemistry Laboratorymuthia aninditaNo ratings yet
- The Economic Impact of Poor Blood Sample QualityDocument10 pagesThe Economic Impact of Poor Blood Sample QualityGökhanNo ratings yet
- Najms 6 224Document5 pagesNajms 6 224fioravantipamela1321No ratings yet
- Original Papers: Specimen Rejection in Laboratory Medicine: Necessary For Patient Safety?Document9 pagesOriginal Papers: Specimen Rejection in Laboratory Medicine: Necessary For Patient Safety?KKay LaminNo ratings yet
- Role of Nursing Personnel in Laboratory Testing: August 2018Document6 pagesRole of Nursing Personnel in Laboratory Testing: August 2018John Alexander Hurtado ParraNo ratings yet
- Annalof Nursing PrimarycareDocument6 pagesAnnalof Nursing PrimarycarefatmanajehNo ratings yet
- Preanalytical Errors in The Clinical Laboratory and How To Minimize ThemDocument3 pagesPreanalytical Errors in The Clinical Laboratory and How To Minimize ThemTeguh PerdanaNo ratings yet
- 58635 Ce(Ad) f(is) Pf1(Aka Ss) Pfa(Ss) Pn(Ss)Document4 pages58635 Ce(Ad) f(is) Pf1(Aka Ss) Pfa(Ss) Pn(Ss)marvel ecstasyNo ratings yet
- Critical Value ReportingDocument7 pagesCritical Value Reportingjorguey100% (1)
- Bertholf2017 Chapter LaboratoryStructureAndFunctionDocument23 pagesBertholf2017 Chapter LaboratoryStructureAndFunctionci8084102No ratings yet
- Errores en La Fase PreanalíticaDocument4 pagesErrores en La Fase PreanalíticaYaquelin VelasquezNo ratings yet
- Errors Beyond the Lab: Understanding Errors in the Total Testing ProcessDocument10 pagesErrors Beyond the Lab: Understanding Errors in the Total Testing ProcessDiegoMaradónNo ratings yet
- Clinical Laboratory Tests - Which, Why, and What Do The Results Mean? - LaboratorDocument34 pagesClinical Laboratory Tests - Which, Why, and What Do The Results Mean? - LaboratorGeorgeNo ratings yet
- Quality Assurance in The Preanalytical PhaseDocument21 pagesQuality Assurance in The Preanalytical PhaseDaniel Huachani CoripunaNo ratings yet
- A Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayDocument7 pagesA Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayRobert MaynardNo ratings yet
- Delta Checks in The Clinical Laboratory 2019Document24 pagesDelta Checks in The Clinical Laboratory 2019birlikteyizNo ratings yet
- Analysis of Laboratory Critical Value Reporting at A Large Academic Medical CenterDocument7 pagesAnalysis of Laboratory Critical Value Reporting at A Large Academic Medical CenterLevi GasparNo ratings yet
- 2.JHKIMLS Paper 2018 - Watson WongDocument21 pages2.JHKIMLS Paper 2018 - Watson Wongfysi mackNo ratings yet
- Pre-Analytical VariationDocument5 pagesPre-Analytical VariationREMAN ALINGASANo ratings yet
- Rato - Quality of Specimen NotesDocument5 pagesRato - Quality of Specimen NotesAileen SacayNo ratings yet
- External Quality Assurance of Molecular Analysis of Haemochromatosis Gene MutationsDocument4 pagesExternal Quality Assurance of Molecular Analysis of Haemochromatosis Gene MutationssumardiNo ratings yet
- Plebani 2006Document10 pagesPlebani 2006ami190No ratings yet
- IMLT Content Guideline - 10.09Document6 pagesIMLT Content Guideline - 10.09Shaun BradleyNo ratings yet
- 6th Charles Merieux Conference 2019 Pre Post Analytical Errors in HematologyDocument7 pages6th Charles Merieux Conference 2019 Pre Post Analytical Errors in HematologyYaser MNo ratings yet
- Clinical Consequences of Specimen RejectionDocument6 pagesClinical Consequences of Specimen RejectionadrianaNo ratings yet
- Laboratory Test InappropriatenessDocument14 pagesLaboratory Test InappropriatenessomaromranNo ratings yet
- Evaluation & Control of Pre Analytical Errors in Required Quality Variables of Clinical Lab ServicesDocument18 pagesEvaluation & Control of Pre Analytical Errors in Required Quality Variables of Clinical Lab ServicesIOSRjournalNo ratings yet
- Running Head: Sample Errors Analysis 1Document10 pagesRunning Head: Sample Errors Analysis 1api-543686548No ratings yet
- EFLM WG Preanalytical Phase Opinion Paper Local Validation of Blood Collection Tubes in Clinical LaboratoriesDocument7 pagesEFLM WG Preanalytical Phase Opinion Paper Local Validation of Blood Collection Tubes in Clinical LaboratoriesSiskawati SuparminNo ratings yet
- Laboratory Investigations HospitalDocument14 pagesLaboratory Investigations HospitalgegeNo ratings yet
- A Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayDocument4 pagesA Review of Medical Errors in Laboratory Diagnostics and Where We Are TodayShahid HussainNo ratings yet
- ASSIGNMENTDocument7 pagesASSIGNMENTBENJAMIN MAWUENYEGAHNo ratings yet
- Int J Lab Hematology - 2021 - Kitchen - International Council For Standardisation in Haematology ICSH Recommendations ForDocument10 pagesInt J Lab Hematology - 2021 - Kitchen - International Council For Standardisation in Haematology ICSH Recommendations ForWidi MarsandaNo ratings yet
- ObjectivesDocument3 pagesObjectivesLiel YapNo ratings yet
- Chapter 1 Variation Errors and Quality in The Clinical Laboratory 2013 Accurate Results in The Clinical LaboratoryDocument8 pagesChapter 1 Variation Errors and Quality in The Clinical Laboratory 2013 Accurate Results in The Clinical LaboratoryCristina GaidargiNo ratings yet
- Errors in Laboratory Testing: Reducing Mistakes Throughout the Total Testing ProcessDocument11 pagesErrors in Laboratory Testing: Reducing Mistakes Throughout the Total Testing ProcessShahid HussainNo ratings yet
- Lippi 2018Document10 pagesLippi 2018Vax StoNo ratings yet
- Lot-To-Lot Variation and Verification - cclm-2022-1126Document8 pagesLot-To-Lot Variation and Verification - cclm-2022-1126Georgiana Daniela DragomirNo ratings yet
- Clinical BiochemistryDocument25 pagesClinical Biochemistrymirzafahad82005No ratings yet
- Laboratory ServicesDocument43 pagesLaboratory ServiceskanikaNo ratings yet
- Quality Control in HistopathologyDocument30 pagesQuality Control in HistopathologyMuhammad Jamiu Bello78% (9)
- Serum Indices Brochure 2019Document28 pagesSerum Indices Brochure 2019constanzanazarethNo ratings yet
- JOURNAL Errors in Clinical Laboratories or Errors in LaboratoryDocument11 pagesJOURNAL Errors in Clinical Laboratories or Errors in LaboratoryVincent ReyesNo ratings yet
- Arpa.2014 0161 CPDocument6 pagesArpa.2014 0161 CPShabbir HussainNo ratings yet
- Nikolac N Et Al - CSMBLM Recommendations For Phlebotomy-Korr 0Document13 pagesNikolac N Et Al - CSMBLM Recommendations For Phlebotomy-Korr 0servicio kendalNo ratings yet
- Clinical Laboratory Quality Practices When Hemolysis OccursDocument6 pagesClinical Laboratory Quality Practices When Hemolysis OccursFelia AkasehNo ratings yet
- Quality Assurance in Microbiology LabsDocument6 pagesQuality Assurance in Microbiology LabsgiuseppegnrNo ratings yet
- Quality assurance key to accurate lab resultsDocument6 pagesQuality assurance key to accurate lab resultsrizkiyah prabawantiNo ratings yet
- Biochem - Med 22 3 342 9Document10 pagesBiochem - Med 22 3 342 9Rute RibeiroNo ratings yet
- 2425 Manuscript 9209 1 10 20190501Document6 pages2425 Manuscript 9209 1 10 20190501Phuong LeNo ratings yet
- Study of Pre Analytical Errors in A Medium Sized Pathology LaboratoryDocument6 pagesStudy of Pre Analytical Errors in A Medium Sized Pathology Laboratorysandeep raiNo ratings yet
- The Impact of Repeat-Testing of Common Chemistry Analytes at Critical ConcentrationsDocument7 pagesThe Impact of Repeat-Testing of Common Chemistry Analytes at Critical Concentrationsmy accountNo ratings yet
- Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is SuspectedDocument19 pagesClinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is SuspectedgustixNo ratings yet
- UntitledDocument236 pagesUntitledAyesha MehmoodNo ratings yet
- UntitledDocument336 pagesUntitledAyesha Mehmood83% (6)
- UntitledDocument351 pagesUntitledAyesha MehmoodNo ratings yet
- Schedule A AAA Membership FormDocument3 pagesSchedule A AAA Membership FormAyesha MehmoodNo ratings yet
- English Language Worksheet I: Parts of SpeechDocument13 pagesEnglish Language Worksheet I: Parts of SpeechAyesha MehmoodNo ratings yet
- Superhero Nouns WorksheetDocument1 pageSuperhero Nouns WorksheetAyesha MehmoodNo ratings yet
- Cadet College Jhelum Application FormDocument1 pageCadet College Jhelum Application FormAyesha Mehmood0% (1)
- First Merit List A 2017-2018Document4 pagesFirst Merit List A 2017-2018zohaib hassan ShahNo ratings yet
- Four Types of SentencesDocument2 pagesFour Types of SentencesMay Phoo Mon100% (1)
- Does Ramadan fasting increase peptic ulcer perforations? (39 charactersDocument5 pagesDoes Ramadan fasting increase peptic ulcer perforations? (39 charactersAyesha MehmoodNo ratings yet
- Monsoon Outlook-JAS2020Document1 pageMonsoon Outlook-JAS2020Ayesha MehmoodNo ratings yet
- 4thMeritList FSC Morning2018Document2 pages4thMeritList FSC Morning2018Shakeel ArifNo ratings yet
- 9first Merit List 05 Year Program 2019Document9 pages9first Merit List 05 Year Program 2019Shahram AbbasNo ratings yet
- Chughtai Lab COVID-19 Test Patient Detail (sample form/样表)Document1 pageChughtai Lab COVID-19 Test Patient Detail (sample form/样表)Ayesha MehmoodNo ratings yet
- DEVICESDocument47 pagesDEVICESAyesha MehmoodNo ratings yet
- Get Chughtai Lab Lahore Test Reports OnlineDocument4 pagesGet Chughtai Lab Lahore Test Reports OnlineAyesha MehmoodNo ratings yet
- Medicine Practical Send Up 39th Mbbs PDFDocument24 pagesMedicine Practical Send Up 39th Mbbs PDFAyesha MehmoodNo ratings yet
- Medicine II MCQs Send Up 2014Document4 pagesMedicine II MCQs Send Up 2014Ayesha MehmoodNo ratings yet
- Medicine Practical Send Up 39th Mbbs PDFDocument24 pagesMedicine Practical Send Up 39th Mbbs PDFAyesha MehmoodNo ratings yet
- DEVICESDocument47 pagesDEVICESAyesha MehmoodNo ratings yet
- DEVICESDocument47 pagesDEVICESAyesha MehmoodNo ratings yet
- Burns Guide: Causes, Types, TreatmentDocument4 pagesBurns Guide: Causes, Types, TreatmentMartin KoaNo ratings yet
- STERILE PARENTERAL FORMULATIONSDocument85 pagesSTERILE PARENTERAL FORMULATIONSShalimashalu100% (1)
- CA IC 130LF 14 00 01 en ArxDocument8 pagesCA IC 130LF 14 00 01 en ArxRendy EksaNo ratings yet
- Annex 6: Guidance On Good Manufacturing Practices (GMP) : Inspection ReportDocument5 pagesAnnex 6: Guidance On Good Manufacturing Practices (GMP) : Inspection Reportumarn1582No ratings yet
- Coping Strategies of Athletes for Competitive AnxietyDocument13 pagesCoping Strategies of Athletes for Competitive AnxietyHONEY JEAN ESPENORIONo ratings yet
- Bailey SafeMedPharmacyTechnicianDocument10 pagesBailey SafeMedPharmacyTechnicianRazak AbdullahNo ratings yet
- High Yield Surgery Compatible VersionDocument77 pagesHigh Yield Surgery Compatible Version17kimpNo ratings yet
- CyberneticsDocument3 pagesCyberneticsTanya ChawdaNo ratings yet
- Lean GuideDocument155 pagesLean GuideSujoy Kar100% (1)
- Hydrogen Sulphide Safety Around RigDocument14 pagesHydrogen Sulphide Safety Around RigmohammedNo ratings yet
- Admin of Meds Prof GuidanceDocument8 pagesAdmin of Meds Prof GuidanceStacyNo ratings yet
- Summary of key provisions in the Domestic Workers ActDocument46 pagesSummary of key provisions in the Domestic Workers ActPaul Christopher PinedaNo ratings yet
- Inflammation - The Silent Killer - Terra Health EssentialsDocument6 pagesInflammation - The Silent Killer - Terra Health EssentialshighlanderoneNo ratings yet
- Igem ListDocument9 pagesIgem ListMilad YadollahiNo ratings yet
- MKWD Lwua Adb Package 2 AnnexesDocument199 pagesMKWD Lwua Adb Package 2 AnnexesRoland AnaumNo ratings yet
- Water QualityDocument41 pagesWater QualityPaschal MazikuNo ratings yet
- Label, Procedure, AdvertisementDocument6 pagesLabel, Procedure, AdvertisementActrissia Aprilla SandhyNo ratings yet
- Acute Diverticulitis-GcpDocument85 pagesAcute Diverticulitis-Gcpkuro hanabusaNo ratings yet
- Hospital Administrative Assistant Resume-A4Document2 pagesHospital Administrative Assistant Resume-A4Philip V AlexNo ratings yet
- GHQ 2Document8 pagesGHQ 2miji_ggNo ratings yet
- Functional Test and Weight Verification of BalancesDocument5 pagesFunctional Test and Weight Verification of BalancesMartellRNo ratings yet
- AA PamphletDocument52 pagesAA PamphletCarmen UleiaNo ratings yet
- 4th Quarter CAPSTONEDocument30 pages4th Quarter CAPSTONEWallace RamosNo ratings yet
- HO#1.1 Caring For The BodyDocument7 pagesHO#1.1 Caring For The BodyGemma CanlapanNo ratings yet
- KOICA-Yonsei Master's Program in Infectious Disease ControlDocument28 pagesKOICA-Yonsei Master's Program in Infectious Disease ControlBIDAN KSANo ratings yet
- Msds Coal PDFDocument4 pagesMsds Coal PDFGuntur Wijaya100% (1)
- Alvarez 2015Document18 pagesAlvarez 2015Clara RodriguesNo ratings yet
- The Perspective of Vat Concessions Regime in Tanzania PDFDocument32 pagesThe Perspective of Vat Concessions Regime in Tanzania PDFHandley Mafwenga SimbaNo ratings yet