Professional Documents
Culture Documents
Occipital Nerve Blockade in Chronic Cluster
Uploaded by
Toni DOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Occipital Nerve Blockade in Chronic Cluster
Uploaded by
Toni DCopyright:
Available Formats
doi:10.1111/j.1468-2982.2007.01424.
Occipital nerve blockade in chronic cluster headache patients
and functional connectivity between trigeminal and
occipital nerves
V Busch1, W Jakob1, T Juergens1, W Schulte-Mattler1, H Kaube2 & A May1,3
1
Department of Neurology, University of Regensburg, Regensburg, Germany, 2Headache Group, Institute of Neurology, London, UK and
3
Department of Systems Neuroscience, University of Hamburg, Hamburg, Germany
Busch V, Jakob W, Juergens T, Schulte-Mattler W, Kaube H & May A. Occipital
nerve blockade in chronic cluster headache patients and functional connectivity
between trigeminal and occipital nerves. Cephalalgia 2007; 27:1206–1214.
London. ISSN 0333-1024
Headache syndromes often involve occipital and neck symptoms, suggesting a
functional connectivity between nociceptive trigeminal and cervical afferents.
Although reports regarding effective occipital nerve blockades in cluster head-
ache exist, the reason for the improvement of the clinical symptoms is not
known. Using occipital nerve blockade and nociceptive blink reflexes, we were
able to demonstrate functional connectivity between trigeminal and occipital
nerves in healthy volunteers. The R2 components of the nociceptive blink reflex
and the clinical outcome in 15 chronic cluster headache patients were examined
before and after unilateral nerve blockade of the greater occipital nerve with 5 ml
prilocain (1%) on the headache side. In contrast to recent placebo-controlled
studies, only nine of the 15 cluster patients reported some minor improvement
in their headache. Six patients did not report any clinical change. Exclusively on
the injection side, the R2 response areas decreased and R2 latencies increased
significantly after the nerve blockade. These neurophysiological and clinical data
provide further evidence for functional connectivity between cervical and
trigeminal nerves in humans. The trigeminocervical complex does not seem to be
primarily facilitated in cluster headache, suggesting a more centrally located
pathology of the disease. However, the significant changes of trigeminal function
as a consequence of inhibition of the greater occipital nerve were not mirrored
by a significant clinical effect, suggesting that the clinical improvement of
occipital nerve blockades is not due to a direct inhibitory effect on trigeminal
transmission. 䊐Cluster headache, nociceptive blink reflex, occipital nerve block,
trigeminal nerve
Arne May, MD, Assistant Professor of Neurology, Department of Systems
Neuroscience, University of Hamburg, Martinistr. 52, D-22046 Hamburg, Germany.
Tel. + 040 4 2803 9189, fax + 040 4 2803 9955, e-mail a.may@uke.uni-hamburg.de
Received 15 August 2006, accepted 26 May 2007
pain, stiffness or tenderness, suggesting participa-
Introduction tion of trigeminal and cervical innervation in
Patients suffering from primary headache syn- central pain processing mechanisms in these disor-
dromes with typically frontal symptoms, such as ders (1). The most likely mechanism for this obser-
migraine, tension-type headache or cluster head- vation is ‘referred pain’ originating from structures
ache (CH), often complain of accompanying neck in the neck and projecting to facial areas and vice
1206 © Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
Occipital nerve blockade in CCH patients 1207
versa at the level of second-order neurons in the the usual treatment options. A further aim was to
brainstem, which receive convergent input from test whether the clinical outcome—in the case of
both trigeminal and cervical territories (2–4). Based a successful result—correlated with changes of
on findings from experimental studies, electrical trigeminal transmission, which would imply a
stimulation of the greater occipital nerve (GON) in modulatory role of the cervical innervation in these
animals has indeed been shown to have a facilitat- patients. We therefore examined with the same
ing effect on dural nociceptive stimulation (5–7), design as tested in healthy volunteers (8) the noci-
suggesting the subsequent induction of central ceptive blink reflex responses before and after GON
sensitization on second-order neurons receiving blockade in a group of 15 CCH patients.
cervical and trigeminal input.
We have recently shown that a reduction of
sensory cervical input in humans inhibits the noci- Subjects and methods
ceptive transmission from the first division of the
trigeminal nerve in healthy volunteers (8). Specifi- Subjects
cally, we found a decrease of the nociceptive blink
Fifteen patients (14 men, one woman, age
reflex responses and an increase of the R2 latencies
23–64 years, mean 40 years) with active CCH
following GON blockade with Prilocain. These
according to the criteria of the International Head-
findings support the hypothesis of functional con-
ache Society (20) were studied before and after
nectivity between trigeminal and cervical afferent
occipital nerve blockade ipsilateral to the headache
pathways in humans (9).
side. The clinical and demographic characteristics
Several studies have suggested that pain relief in
are shown in Table 1. All patients were otherwise
migraine, cervicogenic headache and CH can be
healthy, but had been suffering from daily CH
achieved by local injections of steroids, local anaes-
attacks for many years, despite several preventative
thetics, or a mixture of both in the area of the GON
treatments. None had suffered an attack within the
(10–15). However, the reason for the improvement
last 4 h prior to the first measurement taken outside
of clinical symptoms after occipital nerve blockade
of an attack.
in primary headache patients is unknown. Several
Written, informed consent was obtained from all
hypotheses have been suggested, including inhibi-
patients and the study was approved by the Ethics
tion of central pain-processing mechanisms at
Committee of the University of Regensburg.
the brainstem level, a systemic steriod effect and
placebo effects.
CH is an excruciatingly painful primary head-
Design
ache syndrome, characterized by attacks of severe,
unilateral pain in the orbital, supraorbital and tem- The response areas (AUC) and the latencies of the
poral areas, lasting from 15 to 180 min, recurring up R2 components of the nociceptive blink reflexes and
to eight times daily and accompanied by ipsilateral thresholds for sensory and pain perception were
autonomic symptoms (16). One in 10 subjects pre- measured in 15 CCH patients. This was followed by
sents the chronic form (CCH), in which remissions recordings of the nociceptive blink reflexes as
are absent for at least 1 year or last <1 month. A described below. Occipital nerve blocks were per-
significant proportion of CCH subjects are refrac- formed by injecting 5 ml of a local anaesthetic
tory to any pharmacological therapy and thus (Prilocain 1%; Astra Zeneca, Wedel, Germany) in
remain dramatically disabled (17). Blockade of the the region of the GON ipsilateral to the headache
GON using suboccipital injections of steroids or side (11 right, four left). The GON was located in
local anaesthetics (or a combination of both) on the the nuchal line halfway between the mastoid
pain side is therefore justified before resorting to process and the occipital protuberance, as described
surgical procedures, as side-effects are rare (14, 18, (8). Successful blockade was confirmed by testing
19). sensory perception with a cotton swab. Finally,
In general, the success of any procedure or treat- measurements of the nociceptive blink reflexes were
ment for episodic CH has to be judged with great repeated. The time interval between the two record-
caution, as the natural course of the disease is a ings was approximately 20 min. Patients were
temporary remission. The purpose of this study asked about the clinical outcome following the
was to assess the clinical effect of a single cervical nerve blockade and about head pain and CH
cutaneous nerve blockade with local anaesthetics attacks on the evening of the same day, 1 day and
alone in otherwise chronic CH patients resistant to 1 week after the procedure.
© Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
1208
Table 1 The clinical and demographic characteristics of 15 chronic cluster headache patients
Clinical outcome
V Busch et al.
Attacks On the day 1 week
N Age, years Gender Side Medication usually One day after GON after GON
1 53 M r – 4 No attacks for 3 days Better night sleep (lasting 4 No changes
nights)
2 27 M r – 5–6 One night without attacks, otherwise no changes No changes
3 35 M l Verapamil 3 ¥ 160 mg 4–5 No changes No changes
4 45 M r Verapamil 3 ¥ 160 mg 3–5 No attacks for the rest of the day No changes
No interval headache for 3 days
5 64 M r Verapamil 3 ¥ 160 mg 2 No changes No changes
6 26 F l – 3–4 Feeling of ‘lightness’ No changes
No attack on the same, and only one on next day
7 57 M r Verapamil 3 ¥ 160 mg 1–6 No changes No changes
Lithiumcarbonate 450 mg
8 40 Verapamil 3 ¥ 240 mg 4 Feeling of ‘lightness’ No changes
Attacks less intensive for about 1 week
No attacks until next day
9 53 M l Verapamil 3 ¥ 240 mg 5–6 No autonomic symptoms for 3 days No changes
Otherwise no changes
10 46 M r Verapamil 420 mg 5 No changes
Facial hyposthesia (~4 days)
11 35 M r – 2–3 Feeling of ‘lightness’ No changes
No attacks until next day
12 33 M l Verapamil 3 ¥ 160 mg 1–6 Feeling of ‘lightness’ No changes
Lithiumcarbonate 450 mg No attacks until next day
13 43 M r Lithium 2 ¥ 400 mg 1–4 No changes No changes
14 27 M r – 3 No changes No changes
15 23 M r Verapamil 3 ¥ 160 mg 4–6 No changes No changes
Lithiumcarbonate 450 mg
r, Right side; l, left side; M, male; F, female. Medication and attacks per day. Clinical outcome refers to the number of usual attacks (before the nerve blockade).
© Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
Occipital nerve blockade in CCH patients 1209
Electrophysiology Results
To study trigeminal nociception and transmission,
Electrophysiology
the nociceptive blink reflex was elicited with a
custom-built planar concentric electrode with a Results are presented in mean and standard
stimulation area of approximately 20 mm2 (21). It deviations.
was placed on both sides of the forehead, 10 mm
above the entry zone of the supraorbital nerve.
Preblockade
Stimulus pulse width was 500 ms. Surface electrodes
In chronic CH patients the initial R2 latencies (in
were placed infraorbitally below both eyes and at
ms) on the injection/headache side were not sig-
the root of the nose (22). Recording bandwidth was
nificantly different from the non-injection/non-
50–2500 Hz. The patient’s individual threshold for
headache side (34.5 ⫾ 3.9 vs. 35.3 ⫾ 3.4, P = 0.453).
sensory detection (Ie) and pin prick like pain
Similarly, the R2 response AUC (in mVms) on the
(Ip) were determined by applying two series of
injection/headache side before the blockade did not
electrical pulses with increasing and decreasing
differ from the non-injection/non-headache side
stimulus intensities using stepwise increments
(5786 ⫾ 2604 vs. 5620 ⫾ 1907, P = 0.694) (Fig. 1a,b).
of 0.1 mA. Nociceptive blink reflexes were elicited
At baseline, patients with CCH showed no signifi-
with stimulus intensities of 1.5 times the
cant differences regarding the R2 onset latencies
individual Ip at interstimulus intervals of 15–17 s
or the R2 response areas compared with healthy
(pseudorandomized).
controls (8).
The study was blinded in terms of the injection/
headache side to the researcher who collected the
blink reflex data. Post blockade
The first sweep from each recording block of six In comparing measurements from before and after
sweeps was discarded to avoid contamination with the nerve blockade, significantly decreased AUC
EMG responses due to startle responses. From aver- and increased latencies of the R2 components were
ages of five single stimuli, the AUC and the laten- found in the patients exclusively on the injection
cies were calculated offline after demeaning and side. Inclusion of thresholds for sensory and pin
rectification of the raw EMG signal. AUC were prick-like pain perception did not explain more of
calculated between 30 and 90 ms (23). The values the variance. Correlations between thresholds and
given are the means of four blocks of five single R2 latencies/R2 response areas before and after the
stimuli administered on each side. nerve blockade were not significant in patients or in
PC-based, off-line analysis was done with controls. The thresholds were therefore not consid-
custom-written software using Matlab 5.1 (Math- ered in the final model (Table 2).
works, Natick, MA, USA). Performing post hoc analyses, a significant
increase of R2 latencies (before 34.5 ⫾ 3.9, after
38.9 ⫾ 3.3; P = 0.001) and a significant decrease
Statistics
of R2 response areas (before 5786 ⫾ 2604, after
R2 latencies and R2 AUC of the nociceptive blink 4046 ⫾ 2067; P = 0. < 001) were found on the
reflex recordings and perception and pin prick-like injection/headache side. On the non-injection/
pain thresholds of the 15 CH patients were proved non-headache side, neither the latencies (before
for normal distribution by Kolmogorov–Smirnov 35.3 ⫾ 3.1, after 36.4 ⫾ 3.9; P = 0.297) nor the AUC
tests and by q–q plots. Repeated measures ANOVA (before 5620 ⫾ 1907, after 4842 ⫾ 2979; P = 0.153)
was used to assess the effect of GON injections with were changed significantly, although there was a
‘TIME’ (before vs. after the nerve blockade) and tendency towards longer R2 onset latencies and
‘SIDE’ (headache vs. non-headache side) as within- decreased AUC after the nerve block on the head-
subject factors. Post hoc group differences between ache side (Fig. 1a,b).
headache side vs. non-headache side of the initial Thresholds for sensory and pin prick-like pain
R2 responses (baseline) were assessed with Stu- perception are shown in Table 3. Thresholds of
dent’s t-test. In an additional analysis, thresholds pin prick-like pain perception were significantly
for sensory and pin prick-like pain perception were increased on the headache compared with the non-
tested as dynamic covariates. Correlations were headache side (1.43 ⫾ 0.33 vs. 1.23 ⫾ 0.29, t = 4.61,
tested with Pearson’s product moment coefficients. P < 0.001) and with healthy controls (8). This differ-
The level of significance was set at P < 0.05. ence continued after the blockade (1.39 ⫾ 0.27 vs.
© Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
1210 V Busch et al.
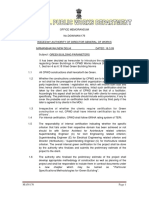
a
Injection/headache side Non-injection/non-headache side
8000 8000
7000 7000
6000 6000
R2 AUC (µVms)
R2 AUC (µVms)
*
5000 5000
*
4000 4000
3000 3000
2000 Ipsilateral 2000 Ipsilateral
1000 Contralateral 1000 Contralateral
Baseline After blockade Baseline After blockade
Injection/headache side Non-injection/non-headache side
45 45
44 44
43 43
*
42 * 42
41 41
R2 latencies (ms)
R2 latencies (ms)
40 40
39 39
38 38
37 37
36 36
35 35
34 34
33 33
32 Ipsilateral 32 Ipsilateral
31 31
30 Contralateral 30 Contralateral
Baseline After blockade Baseline After blockade
Figure 1 Error bars represent the ipsilateral and contralateral R2 areas under the curve (a) and latencies (b) of nociceptive
blink reflexes as means with 95% confidence interval before and after the occipital nerve blockade in 15 chronic cluster
headache patients. *Significant at P < 0.01.
Table 2 Analysis of variance for repeated measures (General linear model)
R2 latencies (ms) R2 response areas (AUC) (mV)
Ipsilateral Contralateral Ipsilateral Contralateral
Factor F P F P F P F P
SIDE 0.23 NS (0.64) 0.01 NS (0.93) 0.59 NS (0.46) 0.18 NS (0.69)
TIME 7.95 0.02 5.22 NS (0.06) 6.94 0.02 6.53 0.03
SIDE ¥ TIME 7.48 0.03 6.26 0.04 7.01 0.02 6.23 0.03
Within-subject factors = ‘side’ (headache side/non-headache side) and ‘time’ (before and after the occipital nerve blockade).
F-values and P-values are shown for ipsi- and contralateral reflex responses. Degrees of freedom (hypothesis/error) were 1/14
for all measurements.
© Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
Occipital nerve blockade in CCH patients 1211
Table 3 t-test comparison of thresholds before and after the greater occipital nerve blockade
Headache/injection side Non-headache/non-injection side
Before After P Before After P
Perception:
sensory 0.54 ⫾ 0.21 0.58 ⫾ 0.19 NS (0.36) 0.53 ⫾ 0.12 0.55 ⫾ 0.29 NS (0.47)
(pin prick-like) pain 1.43 ⫾ 0.33 1.39 ⫾ 0.27 NS (0.35) 1.23 ⫾ 0.18 1.20 ⫾ 0.27 NS (0.49)
Values are means with standard deviations for patients. Comparisons before and after the injection are done with Student’s
t-tests for injection side and for non-injection side. The injection side in patients was the side of their headache.
1.20 ⫾ 0.27, t = 3.59, P < 0.01). However, there was No major adverse events were observed after the
no significant change of these thresholds after the nerve block, but one patient reported hypoaesthesia
occipital nerve blockade on both sides (Table 3). of all three trigeminal divisions of the ipsilateral
Thresholds for sensory perception showed no face lasting for about 4 days. None of the other
initial differences between headache and non- patients complained of any facial sensory loss.
headache side in our patients and no changes after
the nerve blockade on both sides (Table 3).
Discussion
Clinical outcome Clinical effect
After the nerve blockade, all patients experienced After occipital nerve blockade, nine of 15 patients
complete sensory loss in the posterior scalp lasting with CCH presented some general improvement,
between 2 and 11 h (mean 4 h). but only to a small degree, including one patient
Detailed information about the clinical outcome with reduced autonomic symptoms and one with
is given in Table 1. Because of our primarily neu- an arrested interval headache for about 3 days after
rophysiological approach, data regarding the clini- the nerve block. Taking a possible placebo effect
cal outcome are only descriptive. Generally, nine into account (24), the specific effect size of the
out of 15 patients reported some improvement of treatment in our study was even smaller.
the headache attacks, but only to a minor degree. In other studies, the clinical effect of GON block-
Seven patients reported no attacks for the rest of the ades has been reported higher (12) and in the only
day, one patient for the following 3 days. One day placebo-controlled trial so far, a single suboccipital
after the blockade, only one patient continued to steroid injection completely suppressed attacks in
keep pain free, whereas the remaining 14 patients >80% of CH patients (14). However, most of these
experienced the same number of attacks as before patients were episodic cluster patients. Further-
the blockade. One week after the nerve blockade, more, in all these studies, cortisone or a mixture of
no therapeutical benefit was reported. The pain cortisone and local anaesthetics were used. There-
intensity of single attacks was also reduced in four fore, the data cannot answer the question, whether
patients, but these changes were not statistically the steroid is acting systemically and whether the
analysed, e.g. using rating scales. suboccipital injection site does not provide any
One patient was completely pain free for 3 days advantage (19). Our results are in accordance with
after the occipital nerve block. Two patients expe- those of Anthony, who found that suboccipital
rienced a significant reduction in the intensity and injections of local anaesthetic alone have neither a
frequency of their attacks for 2 days. Four patients beneficial nor harmful effect on CH attacks (18).
reported a feeling of ‘light-headedness’ and did not The absence of a uniform clinical reaction in our
have any attacks for the rest of the day. One patient patients may in part be explained by anatomical
reported complete cessation of his interval head- and physiological variations of the main course of
aches, which is a feature in some patients. One the GON between the midline and the nerve along
patient, although still suffering from pain attacks, the intermastoid line (25). However, all of our
observed no autonomic symptoms for 3 days patients experienced anaesthesia in the GON area.
during his acute cluster attack. The remaining six Moreover, the mean reduction of R2 response areas
patients did not report any clinical changes follow- and increase in R2 onset latencies were significant,
ing the nerve block. suggesting a sufficient nerve block.
© Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
1212 V Busch et al.
(31–33), the inhibition of thresholds may be an
Electrophysiology
impairment of descending pain control systems.
Following the injection, a significant decrease of The nociceptive blink reflex is known to be oligo-
the ipsi- and contralateral nociceptive blink reflex synaptic and poorly influenced by (supratentorial)
R2 areas and an increase of the ipsi- and contralat- descending pathways. This could be the explana-
eral R2 latencies exclusively on the side of the tion for our observation of decreased pin prick-like
nerve block were found. This altered trigeminal perception on the headache side but the same reflex
transmission provides evidence for the existence of response regarding AUC integral and latencies
functional connectivity between the occipital and compared with the non-headache side in our cluster
trigeminal nerve structures, not only in healthy patients. Other studies have reported a decrease in
volunteers (8), but also in CH patients, a finding pain thresholds (31, 34). Interestingly, one patient
which has been suggested in experimental studies reported the absence of autonomic symptoms for
(2, 26). The similar results in patients and controls several days after the nerve blockade, though his
suggest a general ‘cross-talk’ between the two headache was not clinically meaningfully reduced.
afferent nerve territories, which is independent This may be explained by the anatomical pathways
of an underlying diagnosis of a primary CH of parasympathetic fibres passing from the superior
syndrome. salivatory nucleus via the greater petrosal nerve to
At baseline, the patients with CCH showed no the sphenopalatine ganglion, which mediates the
significant differences regarding R2 onset latencies parasympathetic features associated with trigemi-
or R2 response areas compared with healthy con- nally mediated pain (35). Previous studies on symp-
trols (8). This suggests that there is no facilitation of tomatic headaches involving cervical innervation
trigeminal nociceptive transmission in the nucleus have also reported cranial autonomic symptoms
caudalis in patients with CCH outside the acute resembling CH (36, 37). In one case report, an
attack. Additionally, there was no correlation aneurysm of the basilar artery was reported to have
between clinical and electrophysiological outcome caused a cluster-like headache in a female patient.
in the cluster patients. Among those who reported Both the pain and the autonomic features were
clinical improvement after the occipital nerve block- significantly reduced after the angiographic coiling
ade, no particular changes in blink reflex responses of the aneurysm, providing evidence for some
could be found. Our data suggest therefore that the ‘cross-talk’ between the cervical and the trigeminal
physiological ‘trigemino-cervical cross-talk’ as such sensory/nociceptive/parasympathetic systems in
does not play a pivotal role in the clinical manifes- the trigeminocervical complex (38).
tation (frequency or duration of attacks) of CH. In It is noteworthy that one patient reported a facial
view of the positive effects of occipital stimulation hypoaesthesia of all three trigeminal branches,
in CH patients (27), it is remarkable that one patient lasting for 3 days after the GON blockade on the
described a cessation of his constant background ipsilateral side. This observation is similar to the
headache, which is known to occur in some patients case report (39), providing further clinical evidence
with CCH (8). In view of these results, it seems for a cervico–trigeminal interaction (37).
unlikely that the therapeutic effect of a mixture of In summary, our neurophysiological and clinical
steroids or local anaesthetics (18) is solely due to data provide further evidence for the existence of
direct inhibition of occipital input. functional connectivity between the sensory occipi-
The pain thresholds at baseline were higher in tal segments and the ophthalmic branch of the
our cluster patients ipsilateral to the headache com- trigeminal nociceptive system in humans. This
pared with the non-headache side and compared cross-talk is independent of whether the subjects
with both sides of healthy controls (8). Our data are suffer from CH or are healthy controls. The trigemi-
in agreement with the literature concerning signifi- nocervical complex does not seem to be facilitated
cant increases in thermal threshold on the pain side in CH, suggesting a more centrally located pathol-
of cluster patients (28). New data from QST studies ogy of the disease. The impressive changes of
in cluster patients have shown either impaired (29) trigeminal function due to cervical inhibition are
or increased thermal thresholds for warmth and not mirrored by a significant clinical effect of an
thermal sensory limen in cluster patients regardless occipital injection of local anaesthetics alone, sug-
whether they were inside or outside the bout (30). gesting that the clinical improvement in some cases
An increase of pin prick-like threshold does not is not due to a direct inhibitory effect on the
necessarily mean an inhibition of the trigemino- trigeminal transmission. In refractory CH patients,
cervical circuit itself. As discussed in the literature who failed to respond to occipital nerve blockade,
© Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
Occipital nerve blockade in CCH patients 1213
it may be necessary to block the more proximal C2 15 Gawel MJ, Rothbart PJ. Occipital nerve block in the
nerve roots, to use longer acting anaesthetics (40) or management of headache and cervical pain. Cephalalgia
to use local cortisone injections (11, 18, 41). 1992; 12:9–13.
16 Headache Classification Committee of the International
Headache Society. Classification and diagnostic criteria
Acknowledgements for headache disorders, cranial neuralgias and facial pain.
Cephalalgia 1988; 8:1–96.
The authors thank Tina Schneider for technical support. The 17 May A. Cluster headache: pathogenesis, diagnosis, and
study was supported by a University grant (ReForM-A) to management. Lancet 2005; 366 (9488):843–55.
V.B. 18 Anthony M. Arrest of attacks of cluster headache by local
steroid injections of the occipital nerve. In: Clifford Rose
References F, editor. Migraine: clinical and research advances. Basel:
Karger, 1985:168–73.
1 Silberstein SD. Tension-type headaches. Headache 1994; 19 Bigo A, Delrieu F, Bousser MG. [Treatment of vascular
34:S2–7. pain of the face by methylprednisolone injection into the
2 Bartsch T, Goadsby PJ. Stimulation of the greater occipital area of the greater occipital nerve: 16 cases]. Rev Neurol
nerve induces increased central excitability of dural affer- 1989; 145:160–2.
ent input. Brain 2002; 125:1496–509. 20 Headache Classification Committee of the International
3 Goadsby PJ, Knight YE, Hoskin KL. Stimulation of the Headache Society. Classification and diagnostic criteria
greater occipital nerve increases metabolic activity in the for headache disorders, cranial neuralgias and facial pain.
trigeminal nucleus caudalis and cervical dorsal horn of Cephalalgia 2004; 24 (Suppl. 1):1–160.
the cat. Pain 1997; 73:23–8. 21 Kaube H, Katsarava Z, Kaufer T, Diener H, Ellrich J. A
4 Kerr FW. Central relationships of trigeminal and cervical new method to increase nociception specificity of the
primary affernets in the spinal cord and medulla. Brain human blink reflex. Clin Neurophysiol 2000; 111:413–6.
Res 1972; 43:561–72. 22 Kimura J. Electrodiagnosis in diseases of nerve and
5 Hu J, Sessle BJ, Raboisson P, Dallel R, Woda A. Stimula- muscle, 3rd edn. Oxford: Oxford University Press, 2001.
tion of craniofacial muscle afferents induces prolonged 23 Ellrich J, Treede RD. Characterization of blink reflex
facilitatory effects in trigeminal nociceptive brain-stem interneurons by activation of diffuse noxious inhibitory
neurones. Pain 1992; 48:53–60. controls in man. Brain Res 1998; 803:161–8.
6 Hu J, Vernon H, Tatourian I. Changes in neck electromyo- 24 Nilsson Remahl AI, Ansjon R, Lind F, Waldenlind E.
graphy associated with meningeal noxious stimulation. Hyperbaric oxygen treatment of active cluster headache:
J Manipulative Physiol Ther 1995; 18:577–81. a double-blind placebo-controlled cross-over study.
7 Bartsch T, Goadsby PJ. Increased responses in trigemi- Cephalalgia 2002; 22:730–9.
nocervical nociceptive neurons to cervical input after 25 Becser N, Bovim G, Sjaastad O. Extracranial nerves in
stimulation of the dura mater. Brain 2003; 126:1801–13. the posterior part of the head. Anatomic variations
8 Busch V, Jakob W, Juergens T, Schulte-Mattler W, Kaube and their possible clinical significance. Spine 1998;
H, May A. Functional connectivity between trigeminal 23:1435–41.
and occipital nerves revealed by occipital nerve blockade 26 Bogduk N. Headache in the neck. In: Goadsby PJ, editor.
and nociceptive blink reflexes. Cephalalgia 2006; 26:50–5. Headache. Blue books of practical neurology. Boston:
9 Busch V, Frese A, Bartsch T. [The trigemino-cervical Butterworth-Heinemann, 1997:369–81.
complex. Integration of peripheral and central pain 27 Matharu MS, Bartsch T, Ward N, Frackowiak J, Weiner R,
mechanisms in primary headache syndromes]. Schmerz Goadsby PJ. Central neuromodulation in chronic
2004; 18:404–10. migraine patients with suboccipital stimulatiors: a PET
10 Inan N, Ceyhan A, Inan L, Kavaklloglu O, Alptekin A, study. Brain 2004; 127:220–30.
Unal N. C2/C3 nerve blocks and greater occipital nerve 28 Becser N, Bovim G, Sjaastad O. Thermal sensitivity in
block in cervicogenic headache treatment. Funct Neurol unilateral headaches. Cephalalgia 1998; 18:675–83; discus-
2001; 16:239–43. sion 657.
11 Caputi CA, Firetto V. Therapeutic blockade of greater 29 Ellrich J, Ristic D, Yekta SS. Impaired thermal perception
occipital and supraorbital nerves in migraine patients. in cluster headache. J Neurol 2006; 253:1292–9.
Headache 1997; 37:174–9. 30 Ladda J, Straube A, Forderreuther S, Krause P, Eggert T.
12 Peres MF, Stiles MA, Siow HC, Rozen TD, Young WB, Quantitative sensory testing in cluster headache:
Silberstein SD. Greater occipital nerve blockade for increased sensory thresholds. Cephalalgia 2006; 26:1043–
cluster headache. Cephalalgia 2002; 22:520–2. 50.
13 Bovim G, Berg R, Dale LG. Cervicogenic headache: anes- 31 Bono G, Antonaci F, Sandrini G, Pucci E, Rossi F, Nappi
thetic blockades of cervical nerves (C2–C5) and facet joint G. Pain pressure threshold in cluster headache patients.
(C2/C3). Pain 1992; 49:315–20. Cephalalgia 1996; 16:62–6; discussion 3–4.
14 Ambrosini A, Vandenheede M, Rossi P, Aloj F, Sauli E, 32 Hardebo JE. The involvement of trigeminal substance P
Pierelli F, Schoenen J. Suboccipital injection with a neurons in cluster headache. An hypothesis. Headache
mixture of rapid- and long-acting steroids in cluster 1984; 24:294–304.
headache: a double-blind placebo-controlled study. Pain 33 Moskowitz MA. The neurobiology of vascular head pain.
2005; 118:92–6. Ann Neurol 1984; 16:157–68.
© Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
1214 V Busch et al.
34 Nappi G, Sandrini G, Alfonsi E, Cecchini AP, Micieli G, anaesthesia and dysaesthesia to cold stimuli. J Neurol
Moglia A. Impaired circadian rhythmicity of nociceptive Neurosurg Psychiatry 1999; 66:397–400.
reflex threshold in cluster headache. Headache 2002; 38 Giffin NJ. Basilar artery aneurysm with autonomic
42:125–31. features: an interesting pathophysiological problem. J
35 Gottselig R, Messlinger K. Noxious chemical stimulation Neurol Neurosurg Psychiatry 2001; 71:805–8.
of rat facial mucosa increases intracranial blood flow 39 Kinney MA, Wilson JL, Carmichael SW, De Ruyter ML,
through a trigemino-parasympathetic reflex—an experi- Fulgham JR. Prolonged facial hypesthesia resulting from
mental model for vascular dysfunctions in cluster head- greater occipital nerve block. Clin Anat 2003; 16:362–5.
ache. Cephalalgia 2004; 24:206–14. 40 Anthony M. Cervicogenic headache: prevalence and
36 Kuritzky A. Cluster headache-like pain caused by an response to local steroid therapy. Clin Exp Rheumatol
upper cervical meningioma. Cephalalgia 1984; 4:185–6. 2000; 18 (2 Suppl. 19):S59–64.
37 de la Sayette V, Schaeffer S, Coskun O, Leproux F, Defer 41 Saadah HA, Taylor FB. Sustained headache syndrome
G. Cluster headache-like attack as an opening symptom associated with tender occipital nerve zones. Headache
of a unilateral infarction of the cervical cord: persistent 1987; 27:201–5.
© Blackwell Publishing Ltd Cephalalgia, 2007, 27, 1206–1214
You might also like
- Jurnal Reading Saraf ALGIDocument6 pagesJurnal Reading Saraf ALGIMuhammad Al GifariNo ratings yet
- Peripheralneuromodulation Fortreatmentofchronic MigraineheadacheDocument4 pagesPeripheralneuromodulation Fortreatmentofchronic MigraineheadacheCorin Boice TelloNo ratings yet
- Gray 2014Document10 pagesGray 2014Nada MachichNo ratings yet
- 2013 Trriger Point ECOM + TMO en Cefalea CervicogenicaDocument9 pages2013 Trriger Point ECOM + TMO en Cefalea CervicogenicaPablo Cuevas SaldivarNo ratings yet
- UseofDr tansChineseBalanceAcupuncture Medicalacupuncture04 16Document10 pagesUseofDr tansChineseBalanceAcupuncture Medicalacupuncture04 16Marlon ManaliliNo ratings yet
- The Effect of Prednisolone On Sequelae in Bell's PalsyDocument5 pagesThe Effect of Prednisolone On Sequelae in Bell's Palsyrara fifiNo ratings yet
- A Case of Occipital NeuralgiaDocument20 pagesA Case of Occipital NeuralgiaLakNo ratings yet
- Hypothalamus and Amygdala Response To Acupuncture StimuliDocument13 pagesHypothalamus and Amygdala Response To Acupuncture StimuliAnibal CisternasNo ratings yet
- Motor cortex stimulation relieves neuropathic facial painDocument5 pagesMotor cortex stimulation relieves neuropathic facial painmoiNo ratings yet
- França (2018) Brain StimulationDocument12 pagesFrança (2018) Brain StimulationAna paula CamargoNo ratings yet
- Deep Brain Stimulation of Posterior Hypothalamic Area For Cluster Headache: A Retrospective Case SeriesDocument5 pagesDeep Brain Stimulation of Posterior Hypothalamic Area For Cluster Headache: A Retrospective Case SeriesegyzellahsNo ratings yet
- Treatment of Medically Intractable Cluster Headache by Occipital Nerve Stimulation: Long-Term Follow-Up of Eight PatientsDocument8 pagesTreatment of Medically Intractable Cluster Headache by Occipital Nerve Stimulation: Long-Term Follow-Up of Eight PatientsareteusNo ratings yet
- Clinical Efficacy of The Mulligan Maneuver For Cervicogenic Headache RCTDocument11 pagesClinical Efficacy of The Mulligan Maneuver For Cervicogenic Headache RCTDavid FehertyNo ratings yet
- J Clinph 2013 03 031Document7 pagesJ Clinph 2013 03 031Andres Rojas JerezNo ratings yet
- Interventional Techniques for Headache ReliefDocument11 pagesInterventional Techniques for Headache ReliefareteusNo ratings yet
- Estimulación Nervio VagoDocument12 pagesEstimulación Nervio VagoMiguel A. RojasNo ratings yet
- NIH Public Access: Author ManuscriptDocument12 pagesNIH Public Access: Author ManuscriptcasNo ratings yet
- The Mechanism of Neurofeedback Training For TreatmDocument14 pagesThe Mechanism of Neurofeedback Training For TreatmcornelteusdeaNo ratings yet
- 2017 Edvinsson The Trigeminovascular PathwayDocument9 pages2017 Edvinsson The Trigeminovascular PathwayCollin SandersonNo ratings yet
- Advances in Diagnosis, Classification, Pathophysiology and Mannagement of Trigeminal Neuralgia PDFDocument13 pagesAdvances in Diagnosis, Classification, Pathophysiology and Mannagement of Trigeminal Neuralgia PDFSergio A SalgadoNo ratings yet
- Neurological MCQDocument4 pagesNeurological MCQAnonymous hF5zAdvwCC100% (1)
- 1983 - Partial Infraorbital Nerve Ligation As A Model of Trigeminal Nerve Injury in The Mouse Behavioral, NDocument13 pages1983 - Partial Infraorbital Nerve Ligation As A Model of Trigeminal Nerve Injury in The Mouse Behavioral, NNarawut Paka7eprotNo ratings yet
- 1 s2.0 S1341321X18304598 MainDocument3 pages1 s2.0 S1341321X18304598 MainEduardo RodriguezNo ratings yet
- TTH Journal 4 PDFDocument5 pagesTTH Journal 4 PDFRumah Kost Kontrakan AntapaniNo ratings yet
- 127 - Case Report - Complicanza Iniezione Faccette CervicaliDocument3 pages127 - Case Report - Complicanza Iniezione Faccette CervicaliMarco PeroliNo ratings yet
- Edvin S Son 1994Document8 pagesEdvin S Son 1994ProfNo ratings yet
- 30 Years of Vagus NerveDocument5 pages30 Years of Vagus NerveErnesto Ochoa MonroyNo ratings yet
- A Neuroscience Perspective of Physical Treatment of Headache and Neck PainDocument7 pagesA Neuroscience Perspective of Physical Treatment of Headache and Neck PainOcha24 TupamahuNo ratings yet
- Vestibular Neuritis Affects Both Superior and Inferior Vestibular NervesDocument10 pagesVestibular Neuritis Affects Both Superior and Inferior Vestibular NervesSabina BădilăNo ratings yet
- DOR_FENOL_Chemical-Ablation-of-Genicular-Nerve-with-Phenol-for-Pain-Relief-in-Patients-with-Knee-Osteoarthritis-A-Prospective-Study_compressedDocument7 pagesDOR_FENOL_Chemical-Ablation-of-Genicular-Nerve-with-Phenol-for-Pain-Relief-in-Patients-with-Knee-Osteoarthritis-A-Prospective-Study_compressedGustavo FredericoNo ratings yet
- 10 1016@j Clinph 2019 04 615Document2 pages10 1016@j Clinph 2019 04 615danie.arti01No ratings yet
- J JBMT 2014 01 001Document10 pagesJ JBMT 2014 01 001yoverNo ratings yet
- CTS PDFDocument6 pagesCTS PDFBiola DwikoNo ratings yet
- Watson Et Al. (2012) - Head Pain Referral During Examination of The Neck in Migraine and Tension-Type HeadacheDocument10 pagesWatson Et Al. (2012) - Head Pain Referral During Examination of The Neck in Migraine and Tension-Type HeadacheTom StevensNo ratings yet
- Cervicogenic Headache Diagnosis and Treatment BogdukDocument10 pagesCervicogenic Headache Diagnosis and Treatment BogdukYoan PereiraNo ratings yet
- Euroscience: Molecular, Cellular and Circuit Basis of Cholinergic Modulation of PainDocument14 pagesEuroscience: Molecular, Cellular and Circuit Basis of Cholinergic Modulation of PainPriyabrata HalderNo ratings yet
- Cerebrolysin: A Multi-Target Drug For Recovery After Stroke: Expert Review of NeurotherapeuticsDocument17 pagesCerebrolysin: A Multi-Target Drug For Recovery After Stroke: Expert Review of NeurotherapeuticsAlina DorceaNo ratings yet
- Astrocytes in Chronic Pain and ItchDocument19 pagesAstrocytes in Chronic Pain and ItchMerly JHNo ratings yet
- 2014 24 H Mov SacadicosDocument11 pages2014 24 H Mov SacadicosIda Ho Rosell RodríguezNo ratings yet
- Surgical Management of Occipital Neuralgia A Systematic Review of The LiteratureDocument10 pagesSurgical Management of Occipital Neuralgia A Systematic Review of The Literatureosobucox1967No ratings yet
- Neurom Tec at the Neur Inter - 2017 - Linderoth - Conventional and Novel Spinal Stimulation Algorithms HypotheticalDocument9 pagesNeurom Tec at the Neur Inter - 2017 - Linderoth - Conventional and Novel Spinal Stimulation Algorithms Hypotheticalsannorberto8No ratings yet
- Use of Dr. Tans Chinese Balance AcupunctDocument9 pagesUse of Dr. Tans Chinese Balance AcupunctrendaoNo ratings yet
- Brain Injury After Cardiac Arrest - From Prognostication of Comatose Patients To RehabilitationDocument12 pagesBrain Injury After Cardiac Arrest - From Prognostication of Comatose Patients To RehabilitationHabib G. Moutran BarrosoNo ratings yet
- Descending Control Mechanisms in Chronic PainDocument7 pagesDescending Control Mechanisms in Chronic PainpedroNo ratings yet
- Clinical Neurology and Neurosurgery: SciencedirectDocument5 pagesClinical Neurology and Neurosurgery: SciencedirectareteusNo ratings yet
- Cervicogenic HeadacheDocument8 pagesCervicogenic HeadacheEmma KopcikasNo ratings yet
- Psico CirugiaDocument24 pagesPsico CirugiaJuliana MartinezNo ratings yet
- Pemicu 1: Blok Sistem Saraf Dan KejiwaanDocument50 pagesPemicu 1: Blok Sistem Saraf Dan KejiwaancecilliacynthiaNo ratings yet
- Encephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningDocument9 pagesEncephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningRoberto SoehartonoNo ratings yet
- Corrientes InterferencialesDocument9 pagesCorrientes InterferencialesLeticia RiveraNo ratings yet
- Migraine PathophysiologyDocument10 pagesMigraine PathophysiologytalithananNo ratings yet
- Head - Neck PainDocument8 pagesHead - Neck PainAnonymous yy8In96j0rNo ratings yet
- Peripheral Nerve Stimulation PH Neuralgia Li 2015Document3 pagesPeripheral Nerve Stimulation PH Neuralgia Li 2015fajarrudy qimindraNo ratings yet
- The Eight Cervical Nerves and Its Role in TinnitusDocument6 pagesThe Eight Cervical Nerves and Its Role in TinnitusMáté BoaNo ratings yet
- High-resolution ultrasound predicts outcomes in Bell's palsyDocument5 pagesHigh-resolution ultrasound predicts outcomes in Bell's palsyAzmi FananyNo ratings yet
- Neuralgias of The Head: Occipital Neuralgia: ReviewDocument10 pagesNeuralgias of The Head: Occipital Neuralgia: ReviewLuthfia PrasetiaNo ratings yet
- AN C F P: EW Lassification For Acial AINDocument4 pagesAN C F P: EW Lassification For Acial AINAkmal Niam FirdausiNo ratings yet
- Acupuntura y Kinesio Taping para El Manejo Agudo de La Parálisis de Bell. Reporte de Un Caso.Document5 pagesAcupuntura y Kinesio Taping para El Manejo Agudo de La Parálisis de Bell. Reporte de Un Caso.Francisco AlbarracinNo ratings yet
- Dowd 2017 Basal GangliaDocument9 pagesDowd 2017 Basal Gangliasingle_ladyNo ratings yet
- CNS Regeneration: Basic Science and Clinical AdvancesFrom EverandCNS Regeneration: Basic Science and Clinical AdvancesJeffrey KordowerNo ratings yet
- Intra-Spinal Microstimulation PDFDocument5 pagesIntra-Spinal Microstimulation PDFToni DNo ratings yet
- Effects of Physical Therapy On Pain PDFDocument5 pagesEffects of Physical Therapy On Pain PDFToni DNo ratings yet
- Lower Limb Involvement in Spinal Function PDFDocument1 pageLower Limb Involvement in Spinal Function PDFToni DNo ratings yet
- What Is Important Management of Pain PDFDocument12 pagesWhat Is Important Management of Pain PDFToni DNo ratings yet
- Toward A Multimodal Framework of Brainstem Pain-Modulation Circuits in MigraineDocument3 pagesToward A Multimodal Framework of Brainstem Pain-Modulation Circuits in MigraineToni DNo ratings yet
- Occipital Nerve Blockade in Chronic ClusterDocument9 pagesOccipital Nerve Blockade in Chronic ClusterToni DNo ratings yet
- What Is Important Management of Pain PDFDocument12 pagesWhat Is Important Management of Pain PDFToni DNo ratings yet
- A Rat Chronic Pain Model of Spinal Cord PDFDocument9 pagesA Rat Chronic Pain Model of Spinal Cord PDFToni DNo ratings yet
- The Efficacy of Pain Neuroscience EducationDocument25 pagesThe Efficacy of Pain Neuroscience EducationToni DNo ratings yet
- Pain Neuroscience Education StateDocument17 pagesPain Neuroscience Education StateToni DNo ratings yet
- Pain Neuroscience Education and ExerciseDocument6 pagesPain Neuroscience Education and ExerciseToni DNo ratings yet
- Systematic Review and Meta-Analysis of Pain PDFDocument34 pagesSystematic Review and Meta-Analysis of Pain PDFToni DNo ratings yet
- Characteristics of Cognitive Functions PDFDocument5 pagesCharacteristics of Cognitive Functions PDFToni DNo ratings yet
- Pain Neuroscience Education and ExerciseDocument6 pagesPain Neuroscience Education and ExerciseToni DNo ratings yet
- The Efficacy of Pain Neuroscience EducationDocument25 pagesThe Efficacy of Pain Neuroscience EducationToni DNo ratings yet
- Occipital Nerve Blockade in Chronic ClusterDocument9 pagesOccipital Nerve Blockade in Chronic ClusterToni DNo ratings yet
- Pain Neuroscience Education and ExerciseDocument6 pagesPain Neuroscience Education and ExerciseToni DNo ratings yet
- Systematic Review and Meta-Analysis of Pain PDFDocument34 pagesSystematic Review and Meta-Analysis of Pain PDFToni DNo ratings yet
- The Pterygopalatine Ganglion and its Role in Pain SyndromesDocument14 pagesThe Pterygopalatine Ganglion and its Role in Pain SyndromesToni DNo ratings yet
- Clinical Training at TANUVAS by M. Murshidul AhsanDocument3 pagesClinical Training at TANUVAS by M. Murshidul AhsanmurshidvetNo ratings yet
- Soumya Mary 1 Year MSC (N)Document24 pagesSoumya Mary 1 Year MSC (N)Salman HabeebNo ratings yet
- ISO 13485:2012 Certified PDO Thread LiftingDocument8 pagesISO 13485:2012 Certified PDO Thread Liftinghuyenthanh1807No ratings yet
- HealthcareDocument15 pagesHealthcareSumit DaniNo ratings yet
- Ferlin PDFDocument1 pageFerlin PDFRomeo ReyesNo ratings yet
- Pancreatita MetabolicaDocument4 pagesPancreatita MetabolicaRoxana EnachescuNo ratings yet
- Create SOAP Notes Using Medical TerminologyDocument4 pagesCreate SOAP Notes Using Medical TerminologyLatora Gardner Boswell100% (3)
- Essay History Online CounsellingDocument5 pagesEssay History Online CounsellingSky WilliamsNo ratings yet
- Course Material Part-2Document224 pagesCourse Material Part-2pranav_joshi_32No ratings yet
- Jurisprudence and EthicsDocument22 pagesJurisprudence and EthicsRozamae Magnanao100% (1)
- Parasitology Lecture 15 - Liver Flukes and Lung FlukeDocument4 pagesParasitology Lecture 15 - Liver Flukes and Lung Flukemiguel cuevasNo ratings yet
- Perception of Students On The Health Services of The School ClinicDocument2 pagesPerception of Students On The Health Services of The School ClinicMary BiscochoNo ratings yet
- Ensure Recipe BookDocument28 pagesEnsure Recipe BookansshakiNo ratings yet
- Biscuits For Breakfast: Empty Calories For The Hungry Poor by Maheen MirzaDocument5 pagesBiscuits For Breakfast: Empty Calories For The Hungry Poor by Maheen MirzaSubhadeep GhoshNo ratings yet
- Water Quality Classification of Quitinday Underground RiverDocument55 pagesWater Quality Classification of Quitinday Underground RiverRose Dane Escobedo DiestaNo ratings yet
- Pour Plate TechniqueDocument10 pagesPour Plate TechniqueGitanti Rohmanda HolaholaNo ratings yet
- 2010-2011 Uwc Maastricht Welcome GuideDocument27 pages2010-2011 Uwc Maastricht Welcome Guidegap09No ratings yet
- CPWD Green Building Guidelines MemoDocument19 pagesCPWD Green Building Guidelines Memonakul4491_88890127No ratings yet
- KeithBodger - IBD Registry - BSG - 2017 - Revised - Share PDFDocument47 pagesKeithBodger - IBD Registry - BSG - 2017 - Revised - Share PDFcfmunro65No ratings yet
- FilgrastimDocument3 pagesFilgrastimapi-3797941No ratings yet
- Assertive Training and Self-EsteemDocument3 pagesAssertive Training and Self-EsteemKuldeep singhNo ratings yet
- UTP Field Trip ReportDocument8 pagesUTP Field Trip Reportdcros88No ratings yet
- Scores FinalDocument71 pagesScores FinalLakshay Chanana100% (6)
- Development of "Mang Kepweng's Lab": A Mobile Android Information On Herbal PlantsDocument160 pagesDevelopment of "Mang Kepweng's Lab": A Mobile Android Information On Herbal PlantsMac John Teves Poblete100% (3)
- التكفل بأطفال طيف التوحد العلاج التربوي للأطفال المصابين بالتوحد وصعوبات التواصل (Teacch) أنموذجا تحليل لدراسات سابقةDocument13 pagesالتكفل بأطفال طيف التوحد العلاج التربوي للأطفال المصابين بالتوحد وصعوبات التواصل (Teacch) أنموذجا تحليل لدراسات سابقةasmamam07No ratings yet
- Intro To Guidance and CounsellingDocument38 pagesIntro To Guidance and Counsellingolaoluwa adedayoNo ratings yet
- The Musculoskeletal System: Structure and Movement in 38 CharactersDocument30 pagesThe Musculoskeletal System: Structure and Movement in 38 CharactersJosee50% (2)
- Lesson Plan - Unit 2 ReadingDocument9 pagesLesson Plan - Unit 2 ReadingHuyền TrangNo ratings yet
- Hypertrophic ScarsDocument13 pagesHypertrophic ScarsNovita NingtyasNo ratings yet
- 5618B Pertrach AdultDocument1 page5618B Pertrach AdultWilsonSantiagoNo ratings yet