Professional Documents
Culture Documents
APF Handouts
Uploaded by
JaysellePuguonTabije0 ratings0% found this document useful (0 votes)
5 views2 pagesOriginal Title
APF-handouts.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views2 pagesAPF Handouts
Uploaded by
JaysellePuguonTabijeCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
ACUTE PULMONARY FAILURE
(Community acquired pneumonia)
ACUTE PULMONARY FAILURE
Acute respiratory failure occurs when fluid builds up in the air sacs in your lungs.
When that happens, your lungs can't release oxygen into your blood. In turn,
your organs can't get enough oxygen-rich blood to function.
Community acquired pneumonia
.
In community-acquired pneumonia (CAP), you get infected in a community
setting. It doesn’t happen in a hospital, nursing home, or other healthcare center.
Community-acquired pneumonia (CAP) is one of the most common infectious
diseases and is an important cause of mortality and morbidity worldwide.
Typical bacterial pathogens that cause CAP include:
o Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella
catarrhalis.
Pneumonias caused by chlamydia and mycoplasma are often clinically
indistinguishable from other pneumonias.
Symptoms and signs are :
o fever, cough, sputum production, pleuritic chest pain, dyspnea,
tachypnea, and tachycardia.
Diagnosis is based on clinical presentation
o Chest x-ray
o Consideration of alternative diagnoses (eg, heart failure, pulmonary
embolism)
o Sometimes identification of pathogen
Treatment
o Risk stratification for determination of site of care
o Antibiotics
o Antibiotic therapy is the mainstay of treatment for community-acquired
pneumonia. Appropriate treatment involves starting empiric antibiotics
as soon as possible, preferably ≤8 hours after presentation.
o Antivirals for influenza or varicella
o Supportive measures
Prognosis is excellent for relatively young or healthy patients, but many
pneumonias, especially when caused by S. pneumoniae, Legionella,
Staphylococcus aureus, or influenza virus, are serious or even fatal in older,
sicker patients.
Nursing Interventions:
o Assess respiratory symptoms.
Symptoms of fever, chills, or night sweats in a patient should be reported
immediately to the nurse as these can be signs of bacterial pneumonia.
o Assess clinical manifestations.
Respiratory assessment should further identify clinical manifestations
such as pleuritic pain, bradycardia, tachypnea, and fatigue, use of
accessory muscles for breathing, coughing, and purulent sputum.
o Physical assessment.
Assess the changes in temperature and pulse; amount, odor, and color of
secretions; frequency and severity of cough; degree of tachypnea or
shortness of breath; and changes in the chest x-ray findings.
o Assessment in elderly patients.
Assess elderly patients for altered mental status, dehydration, unusual
behavior, excessive fatigue, and concomitant heart failure.
o Instruct patient and family about the cause of pneumonia, management of
symptoms, signs, and symptoms, and the need for follow-up.
o Instruct patient about the factors that may have contributed to the
development of the disease.
o Nursing Priorities
o Maintain/improve respiratory function.
o Prevent complications.
o Support recuperative process.
o Provide information about disease process, prognosis, and treatment.
You might also like
- Acute Pulmonary Failure: Symptoms and Signs AreDocument2 pagesAcute Pulmonary Failure: Symptoms and Signs AreJaysellePuguonTabijeNo ratings yet
- Classification: Community-Acquired PneumoniaDocument15 pagesClassification: Community-Acquired PneumoniaHASLINDANo ratings yet
- Group 2 Community Acquired PneumoniaDocument24 pagesGroup 2 Community Acquired PneumoniaalyanadayritNo ratings yet
- Cap PDFDocument23 pagesCap PDFriyaNo ratings yet
- Clinical PresentationDocument54 pagesClinical PresentationSêrâphîm HâdíNo ratings yet
- MCPDP, June, 2023 PneumoniaDocument22 pagesMCPDP, June, 2023 Pneumonianafisaabdulmalik882No ratings yet
- Munity Acquired PneumoniaDocument4 pagesMunity Acquired PneumoniaDIVEN SolvonNo ratings yet
- Pneumonia: - Is An Infection of One or Both Lungs Which Is Usually Caused by BacteriaDocument10 pagesPneumonia: - Is An Infection of One or Both Lungs Which Is Usually Caused by Bacteriajdvea12No ratings yet
- Literature Review 3 TopicDocument27 pagesLiterature Review 3 TopicBharathi Sneha PeriasamyNo ratings yet
- Pneumonia: Related Diagnostic TestsDocument2 pagesPneumonia: Related Diagnostic TestsBenj VillanuevaNo ratings yet
- Lower Respiratory Tract InfectionDocument21 pagesLower Respiratory Tract InfectionJohn Vincent Dy OcampoNo ratings yet
- Inflammation of The LungsDocument5 pagesInflammation of The LungsNikka MarieNo ratings yet
- PneumoniaDocument16 pagesPneumoniaMelissa David100% (1)
- Lect 8 Pneumonia PDFDocument68 pagesLect 8 Pneumonia PDFRaghad AbdullaNo ratings yet
- Pneumonia Is An Inflammation of The Lungs Caused by An Infection. It Is Also Called Pneumonitis orDocument6 pagesPneumonia Is An Inflammation of The Lungs Caused by An Infection. It Is Also Called Pneumonitis orOtrebron BatisanNo ratings yet
- Respiratory Viruses: Organisms Causing PneumoniaDocument17 pagesRespiratory Viruses: Organisms Causing PneumoniaSherree HayesNo ratings yet
- Chemotherapy ComplicationDocument21 pagesChemotherapy ComplicationDr ZakaryaNo ratings yet
- Approach To The Patient With Cough and Hemoptysis 15 11 13Document34 pagesApproach To The Patient With Cough and Hemoptysis 15 11 13Sanchit PeriwalNo ratings yet
- Chapter 27 - Lower Respiratory ProblemsDocument10 pagesChapter 27 - Lower Respiratory Problemsjosie teehNo ratings yet
- Pneumonia - Marzo, Cecille Joyce D. (BSN4A-1)Document24 pagesPneumonia - Marzo, Cecille Joyce D. (BSN4A-1)Marzo, Cecille JoyceNo ratings yet
- PneumoniaDocument8 pagesPneumoniaCostescu ClaudiaNo ratings yet
- Pneumonia Is An: ClinicalDocument13 pagesPneumonia Is An: ClinicaldfgsfsfssdNo ratings yet
- W1 L2 PneumoniaDocument57 pagesW1 L2 PneumoniaAnas FikriNo ratings yet
- Pneumonia Is Caused by VirusesDocument6 pagesPneumonia Is Caused by VirusesrayshahNo ratings yet
- Pneumonia 3Document8 pagesPneumonia 3janinecasilenNo ratings yet
- REQ - PneumoniaDocument6 pagesREQ - PneumoniaAira AgolongNo ratings yet
- 3 PneumoniaDocument17 pages3 PneumoniaMohamed Na3eemNo ratings yet
- Nursing Management 1Document8 pagesNursing Management 1Melai AvilaNo ratings yet
- Physical Education 12 Pneumonia: To Be Reported By: Alawi, Lhamiah M. Casano, Diana Elizabeth C. Kinoshita, Ryou GDocument19 pagesPhysical Education 12 Pneumonia: To Be Reported By: Alawi, Lhamiah M. Casano, Diana Elizabeth C. Kinoshita, Ryou GRyou KinoshitaNo ratings yet
- By: Anghel Ștefan (6A) Prisacariu Arina (6A) Robu Amalia (6A) Ștefan Valentina (6A)Document21 pagesBy: Anghel Ștefan (6A) Prisacariu Arina (6A) Robu Amalia (6A) Ștefan Valentina (6A)Mihnea PriNo ratings yet
- Cap MRDocument4 pagesCap MRKit BarcelonaNo ratings yet
- Dr. Sana Bashir DPT, MS-CPPTDocument46 pagesDr. Sana Bashir DPT, MS-CPPTbkdfiesefll100% (1)
- Pleurisy WordDocument17 pagesPleurisy WordThoby MlelwaNo ratings yet
- Jurnal Bahasa InggrisDocument12 pagesJurnal Bahasa InggrisVanessa Angelica SitepuNo ratings yet
- NURSING CARE PLAN PneumoniaDocument38 pagesNURSING CARE PLAN PneumoniaLuna JadeNo ratings yet
- 3.pulmonary Alterations - Part 2Document37 pages3.pulmonary Alterations - Part 2Rawan AlotaibiNo ratings yet
- Pneumonia PPT NewDocument22 pagesPneumonia PPT NewOsuri MapitigamaNo ratings yet
- Respiratorydisease 170426125838Document69 pagesRespiratorydisease 170426125838Hayder MaqsadNo ratings yet
- Pneumonia by Kamran UOSargodhaDocument19 pagesPneumonia by Kamran UOSargodhaZeshan Haider Kazmi100% (3)
- Pneumonia: Pneumococcus. A Serious Complication of Pneumonia, Pneumococcal Meningitis, Is AssociatedDocument7 pagesPneumonia: Pneumococcus. A Serious Complication of Pneumonia, Pneumococcal Meningitis, Is AssociatedHannah YtacNo ratings yet
- Central Academy: Biology ProjectDocument12 pagesCentral Academy: Biology ProjectMastbleNo ratings yet
- Acute Upper Respiratory Infection (AURI)Document58 pagesAcute Upper Respiratory Infection (AURI)api-19916399No ratings yet
- Physical Education 12 Pneumonia: To Be Reported By: Alawi, Lhamiah M. Casano, Diana Elizabeth C. Kinoshita, Ryou GDocument21 pagesPhysical Education 12 Pneumonia: To Be Reported By: Alawi, Lhamiah M. Casano, Diana Elizabeth C. Kinoshita, Ryou GRyou KinoshitaNo ratings yet
- Pneumonia 150514133315 Lva1 App6892Document34 pagesPneumonia 150514133315 Lva1 App6892SadiaNo ratings yet
- Pneumonia: Tammy Wichman MD Assistant Professor of Medicine Pulmonary-Critical Care Creighton University Medical CenterDocument80 pagesPneumonia: Tammy Wichman MD Assistant Professor of Medicine Pulmonary-Critical Care Creighton University Medical CenterKartika RezkyNo ratings yet
- PneumoniaDocument27 pagesPneumoniamohammedghassan53No ratings yet
- PneumoniaDocument50 pagesPneumoniaannududi378556No ratings yet
- Readings CAP MRDocument28 pagesReadings CAP MRleijustinesNo ratings yet
- PneumoniaDocument14 pagesPneumoniaDrashti Dewani100% (1)
- Pneumonia AnswersDocument5 pagesPneumonia AnswersColeen Mae CamaristaNo ratings yet
- Diagnosa Banding PneumoniaDocument7 pagesDiagnosa Banding PneumoniaLuphly TaluvtaNo ratings yet
- PneumoniaDocument13 pagesPneumoniaZakaria FarahNo ratings yet
- AsthmaDocument31 pagesAsthmakenmanikeseNo ratings yet
- Pneumonia PDFDocument68 pagesPneumonia PDFfatiniNo ratings yet
- Pharmacotherapy of PneumoniaDocument56 pagesPharmacotherapy of Pneumoniahoneylemon.co100% (1)
- PBLDocument7 pagesPBLRobelNo ratings yet
- Case Study Cap NCM 118Document29 pagesCase Study Cap NCM 118Marie Kelsey Acena MacaraigNo ratings yet
- Pneumonia: Episode OverviewDocument9 pagesPneumonia: Episode Overviewsamfarmer333No ratings yet
- Evaluationandtreatmentof Chroniccough: Genji Terasaki,, Douglas S. PaauwDocument13 pagesEvaluationandtreatmentof Chroniccough: Genji Terasaki,, Douglas S. PaauwRSU DUTA MULYANo ratings yet
- Table 55.: Percentage According To The Type of Seminar/TrainingDocument6 pagesTable 55.: Percentage According To The Type of Seminar/TrainingJaysellePuguonTabijeNo ratings yet
- C. Expense BudgetDocument2 pagesC. Expense BudgetJaysellePuguonTabijeNo ratings yet
- Generic Name: Indications: Adverse EffectsDocument6 pagesGeneric Name: Indications: Adverse EffectsJaysellePuguonTabijeNo ratings yet
- Ent ExamDocument8 pagesEnt ExamJaysellePuguonTabijeNo ratings yet
- Drug Study: Tabije, Arvie Jayselle P. Marbella, IvyDocument15 pagesDrug Study: Tabije, Arvie Jayselle P. Marbella, IvyJaysellePuguonTabijeNo ratings yet
- Pathophysiology of Alzheimers DiseaseDocument2 pagesPathophysiology of Alzheimers DiseaseJaysellePuguonTabijeNo ratings yet
- Tang Nang EnglishDocument7 pagesTang Nang EnglishJaysellePuguonTabijeNo ratings yet
- Jet BookshopDocument3 pagesJet BookshopJaysellePuguonTabijeNo ratings yet
- Mr. Alinger: Mr. Hamza Mr. Marco Mr. Ken Mr. DanielDocument4 pagesMr. Alinger: Mr. Hamza Mr. Marco Mr. Ken Mr. DanielJaysellePuguonTabijeNo ratings yet
- Tabije Drug Study (L07)Document8 pagesTabije Drug Study (L07)JaysellePuguonTabijeNo ratings yet
- KattabaDocument4 pagesKattabaJaysellePuguonTabijeNo ratings yet
- TABIJEact 5Document1 pageTABIJEact 5JaysellePuguonTabijeNo ratings yet
- Tabije, Arvie Jayselle PDocument8 pagesTabije, Arvie Jayselle PJaysellePuguonTabijeNo ratings yet
- TABIJEdiagnosticDocument2 pagesTABIJEdiagnosticJaysellePuguonTabijeNo ratings yet
- Tables CommunityDocument21 pagesTables CommunityJaysellePuguonTabijeNo ratings yet
- TABIJEact 7Document1 pageTABIJEact 7JaysellePuguonTabijeNo ratings yet
- Bio DataDocument2 pagesBio DataJaysellePuguonTabijeNo ratings yet
- Table 8Document1 pageTable 8JaysellePuguonTabijeNo ratings yet
- Pathophysiology of Heart FailureDocument2 pagesPathophysiology of Heart FailureJaysellePuguonTabijeNo ratings yet
- Educating The Next Generation of Nurses To Be Innovators and Change AgentsDocument3 pagesEducating The Next Generation of Nurses To Be Innovators and Change AgentsJaysellePuguonTabijeNo ratings yet
- 50 QuestionsDocument15 pages50 QuestionsJaysellePuguonTabijeNo ratings yet
- Tabije MciDocument3 pagesTabije MciJaysellePuguonTabijeNo ratings yet
- The 4 ADocument3 pagesThe 4 AJaysellePuguonTabijeNo ratings yet
- Jet BookshopDocument3 pagesJet BookshopJaysellePuguonTabijeNo ratings yet
- 50 QuestionsDocument15 pages50 QuestionsJaysellePuguonTabijeNo ratings yet
- Surgical Ward ExamDocument8 pagesSurgical Ward ExamJaysellePuguonTabijeNo ratings yet
- Activity 2 EdnDocument3 pagesActivity 2 EdnJaysellePuguonTabijeNo ratings yet
- Tomay Puj Drivers Level of Awareness To OHSDocument1 pageTomay Puj Drivers Level of Awareness To OHSJaysellePuguonTabijeNo ratings yet
- Bio DataDocument2 pagesBio DataJaysellePuguonTabijeNo ratings yet
- Important Information About Your Online DirectoryDocument17 pagesImportant Information About Your Online Directoryc__bNo ratings yet
- Designing Reliable Practices For IV Push Medication Use Handout PDFDocument17 pagesDesigning Reliable Practices For IV Push Medication Use Handout PDFalejandromfunes1749No ratings yet
- Incident ReportDocument3 pagesIncident Reportthuynh12No ratings yet
- Ch18 Zinke3e Short Section 5Document23 pagesCh18 Zinke3e Short Section 5HaNo ratings yet
- Autism PaperDocument5 pagesAutism PaperMaggie NielsenNo ratings yet
- Dr. Yoyos - Acute Cervical Injury FinalDocument30 pagesDr. Yoyos - Acute Cervical Injury FinalRsud Malinau Ppk BludNo ratings yet
- Oral Exam: Answers NCC Group HQ B': Health and HygieneDocument3 pagesOral Exam: Answers NCC Group HQ B': Health and HygieneAnshul BarthwalNo ratings yet
- Causes of Upper Gastrointestinal Bleeding in Adults UpToDateDocument37 pagesCauses of Upper Gastrointestinal Bleeding in Adults UpToDateJodene Rose RojasNo ratings yet
- Unit I (Hypertension) Part 1Document77 pagesUnit I (Hypertension) Part 1RUSSEL JAN ROJASNo ratings yet
- Case Study Childhood OverweightDocument6 pagesCase Study Childhood Overweightmaalaka100% (1)
- Hospital La Comunidad de Santa Rosa: Chapter I: Problem and Its SettingsDocument15 pagesHospital La Comunidad de Santa Rosa: Chapter I: Problem and Its SettingsMeynard MagsinoNo ratings yet
- Hubungan Pelaksanaan Screening Test Menelan Dengan Kejadian Disfagia Pada Pasien Baru Yang Menderita Stroke AkutDocument7 pagesHubungan Pelaksanaan Screening Test Menelan Dengan Kejadian Disfagia Pada Pasien Baru Yang Menderita Stroke AkutmaydamayNo ratings yet
- Immunomodulation - DR TuliDocument6 pagesImmunomodulation - DR TuliPankaj VatsaNo ratings yet
- Demncia Frontotemporal ContinumDocument25 pagesDemncia Frontotemporal ContinumcositaamorNo ratings yet
- Quiz Results: NURS 502 Med / Surg Cardiovascular System Correct Answers: 7Document7 pagesQuiz Results: NURS 502 Med / Surg Cardiovascular System Correct Answers: 7Moshi LoveNo ratings yet
- Occular Manifestations in Systemic DiseaseDocument42 pagesOccular Manifestations in Systemic DiseasekhalidNo ratings yet
- Reproductive SystemDocument56 pagesReproductive SystemRochelle Ann CunananNo ratings yet
- Foot JournalDocument13 pagesFoot Journalay100% (1)
- Pain Management in AnimalsDocument184 pagesPain Management in Animalsssarbovan100% (1)
- Simulation Based Training For Anaesthesia ResidentsDocument8 pagesSimulation Based Training For Anaesthesia ResidentsSajal SahaNo ratings yet
- Comparison and Contrast Rizka Ananda Bin Ladi A1B219074Document2 pagesComparison and Contrast Rizka Ananda Bin Ladi A1B219074Rizka AnandaNo ratings yet
- Cuong Vong - Resume - RevisedDocument2 pagesCuong Vong - Resume - Revisedapi-300295160No ratings yet
- Introduction To PathologyDocument40 pagesIntroduction To PathologyJugun HayatNo ratings yet
- Hospital DietsDocument451 pagesHospital DietsErika Anne Mercado Cadawan100% (1)
- CcrnexamhandbookDocument42 pagesCcrnexamhandbookSpam SpazzamNo ratings yet
- Trauma and Stressor Related DisordersDocument5 pagesTrauma and Stressor Related DisordersVillarino, Ian C.No ratings yet
- Drug Study - FractureDocument4 pagesDrug Study - FractureMark Zedrix MediarioNo ratings yet
- Question Papers of BHUDocument13 pagesQuestion Papers of BHUgyogi1989No ratings yet
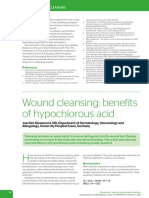
- Wound Cleansing: Benefits of Hypochlorous AcidDocument5 pagesWound Cleansing: Benefits of Hypochlorous Acidlps DiamondNo ratings yet
- Interdisciplinary Interface Between Fixed Prosthodontics and PeriodonticsDocument23 pagesInterdisciplinary Interface Between Fixed Prosthodontics and Periodonticsaziz20070% (1)