Professional Documents
Culture Documents
Perioperative Medication Management Guideline - 2013 Feb 26
Uploaded by
Jayelle2Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Perioperative Medication Management Guideline - 2013 Feb 26
Uploaded by
Jayelle2Copyright:
Available Formats
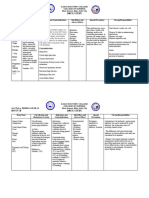
Perioperative Medication Management
Drug Hold or Continue Recommendations / Relevant Pharmaceutical Effects When to Restart
Pre-op? Post-Op
ACID SUPPRESSANTS
Antacids Hold AM of surgery Not needed during surgery. Not known to reduce the risk of acid aspiration. Restart once patient is able to tolerate
Aluminum hydroxide NG/PO intake, and symptom relief
Calcium carbonate needed.
Magnesium hydroxide
91,92
Histamine-2 receptor antagonists Continue Benefit shown in reducing the risk of acid aspiration by decreasing gastric volume contents and increasing gastric pH. -
Cimetidine – see notes*
Famotidine * Special caution with cimetidine warranted because of greater risk of drug interactions relative to other agents. Cimetidine is a weak inhibitor of multiple P450
Nizatidine enzymes. The inhibitory effect may last for days following cessation of cimetidine.
Ranitidine
91, 92
Proton pump inhibitors Continue Benefit shown in reducing the risk of acid aspiration by decreasing gastric volume contents and increasing gastric pH. -
Esomeprazole
Lansoprazole
Omeprazole
Pantoprazole
Rabeprazole
February 26, 2013 Page 1 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
ANALGESICS
Aspirin See Antiplatelets
NSAIDS (COX-1) Hold 4 – 7 days prior to surgery Reversible inhibition of platelet cyclooxygenase. Restart when risk of bleeding is
In general, NSAIDS should be stopped 4 to 7 days prior to surgery. However, minor bleeds can have serious consequences in some surgeries (e.g retinal orintracranial diminished and patient is able to tolerate
Diclofenac Hold 4 days prior to surgery surgery), and thus NSAIDS should be stopped for a minimum of 2 weeks. oral intake.
Ibuprofen The benefit of discontinuing the medication preoperatively should outweigh the risk of pain. Ensure postoperative hemostasis at
Indomethacin Although rare the most compelling reason for discontinuation of NSAIDS is the potential for renal dysfunction. surgical site is adequate.
Ketoprofen Discontinuation prior to surgery depending on half-life.
Naproxen
Sulindac Hold 7 days prior to surgery
Ref 1, 14, 57, 72
NSAIDs (COX-2) Hold a.m. of surgery Little or no effect on platelets. Post hip surgery do not restart unless
Celecoxib * see exceptions Most compelling reason for discontinuation is the potential for renal dysfunction ordered by orthopedic team.
* Exceptions: Patient is at risk for renal dysfunction
Patient is at risk for myocardial ischemia and reperfusion injury.
Do not take the morning of surgery if patient is going for hip surgery
Ref 1, 14, 57, 72
Methadone Continue For methadone maintenance program or for pain management take the dose on the day of surgery. Resume as soon as possible even if with a
Avoid fluctuation in drug level. sip of water to avoid withdrawal
symptoms / loss of tolerance.
Missed Doses: 3 Consecutive Days Missed If the patient has not received
If the usual maintenance dose is methadone 30mg or less, the usual dose may be restarted. If the usual maintenance dose is greater than 30mg then start the dose at methadone for more than 3 consecutive
30mg or up to half the usual maintenance dose. The dose can then be titrated. days the maintenance dose should be re-
Ref 55, 56 evaluated due to a rapid loss of
tolerance.
Narcotics Continue If patient takes high doses of narcotics or routinely takes a long acting preparation. Have the patient take dose on the morning of surgery. Restart once able to tolerate oral intake.
February 26, 2013 Page 2 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
ANTICOAGULANTS
Apixaban (direct Xa inhibitor) Hold prior to surgery, longer for Hold 1-2 days for minor surgery. Resume when adequate hemostasis is
patients with hepatic Hold for 3 days for neuraxial anesthesia. achieved; withdrawal of epidural
impairment No adjustment for age or renal function. catheter at least 24 hours after last dose;
resume at least 5 hours after epidural
Use aPTT or PT preop to verify catheter removal
lack of effect
Dabigatran Hold prior to surgery, longer for Patients less than 65 years of age Patients 65 years of age or greater Resume after at least 12 hours following
(direct thrombin inhibitor) patients with renal dysfunction CrCl > 50 ml/min: hold 2 days prior to day of minor surgery CrCl > 80 ml/min: hold 3 days prior to day of surgery major surgery and after at least 2 hours
neuraxial, hold for 3 days prior * extend for neuraxial following minor surgery provided there is
Use aPTT preop to verify lack of CrCl 30-50 ml/min: hold at least 4 days prior to day of surgery CrCl > 50 ml/min: hold 4 days prior to day of surgery no obvious bleeding.
Antibody fragment to dabigatran in effect * extend for neuraxial * extend for neuraxial Ensure postoperative hemostasis at
development – phase I, 2012 CrCl < 30 ml/min: hold at least 5 or more days prior to surgery CrCl 30-50 ml/min: hold 5 or more days prior to day of surgery surgical site is adequate.
* extend for neuraxial; contraindicated at < 30 * extend for neuraxial
ml/min per ACCP CrCl < 30 ml/min: 7 or more days prior to surgery
* extend for neuraxial; contraindicated at < 30
ml/min per ACCP
Heparin IV (or SQ treatment) doses > 5000 U Hold 4 to 6 hours prior to surgery If emergency surgery is required, can be reversed using protamine 1 mg per 100 unit of heparin or fresh frozen plasma.
sc bid Ref 1
Low-Molecular Weight Heparin (LMWH) Hold 12 to 24 hours prior to Depending on dosing regimen, for once daily dosing, stop LMWH 24 hours preoperatively. For every 12 hour dosing, stop LMWH 12 hours preoperatively. Resume 12 – 24 hours postoperatively
surgery Ref 1 provided there is no obvious bleeding.
Ensure postoperative hemostasis at
surgical site is adequate.
Rivaroxaban (direct Xa inhibitor) Hold at least 24 hours prior to Patients less than 65 years of age Patients 65 years of age or greater Resume when adequate hemostasis is
surgery CrCl > 30 ml/min: hold at least 1 day prior to day of surgery CrCl > 30 ml/min: hold 2 days prior to day of surgery achieved; withdrawal of epidural
neuraxial, hold for 2 days prior neuraxial, hold for at least 3 days prior catheter at least 18 hours after last dose;
Use aPTT or PT preop to verify CrCl < 30 ml/min: hold at least 2 days prior to day of surgery CrCl < 30 ml/min: no recommendation for elderly with reduced renal resume at least 6 hours after epidural
lack of effect neuraxial, hold for at least 3 days prior; function; not recommended for < 30 ml/min catheter removal
not recommended for < 30 ml/min
Warfarin Hold 5 – 7 days prior to surgery Inhibits the synthesis of vitamin K dependent clotting factors. Use Fresh Frozen Plasma if urgent reversal is required. Restart once patient is able to tolerate
Does not have to be discontinued for cataract surgery. NG/PO intake.
Evaluate risk of stroke versus bleeding. Ensure postoperative heomstasis at
Consider using heparin or LMWH to bridge gap between day of stopping and resuming warfarin. surgical site is adequate.
Ref 1
February 26, 2013 Page 3 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
ANTIPLATELETS Ref 1, 5, 11, 72
Clopidogrel Assess risk vs benefit Irreversibly inhibits platelet aggregation. For patients with recent cardiac stents (<12 months) and/or high cardiovascular risk, call cardiologist to discuss the risks of Restart when risk of bleeding is
If holding therapy is necessary, stopping (acute, if restenosis of stent would be catastrophic). diminished.
hold 7 days prior to surgery. Consider restarting as soon as possible for
Aspirin Assess risk vs benefit For patients on ASA for secondary prevention having minor procedures (e.g. minor dental, patients with a very high risk for
If holding therapy is necessary, dermatological, cataract) or at moderate to high risk for CV events should continue therapy. Chest
cardiovascular disease.
2012
hold 7 days prior to surgery Ensure postoperative hemostasis at
Patients on ASA for primary prevention or at low risk for CV events may stop ASA 7 to 10 days surgical site is adequate.
Aggrenox (Dipyridamole + ASA) Assess risk vs benefit prior to OR. Chest 2012
If holding therapy is necessary, Irreversibly inhibits platelet function - 7 to 10 days until new platelets can be generated. In high risk patients (e.g. unstable coronary syndromes or cerebrovascular
hold 7 days prior to surgery disease, percutaneous coronary intervention or stents within 12 months) it may not be feasible to stop therapy. Discuss risk with cardiologist and/or surgical team.
Ticlopidine Assess risk vs benefit
If holding therapy is necessary, Stopped due to the aspirin component of the medication.
hold 10 days prior to surgery
BIPHOSPHONATES
Alendronate Hold a.m. of surgery Alendronate: held because of strict instructions for administration. Must be taken with 6 – 8 oz of water at least 30 minutes before any food, beverage or medications in Resume once patient is able to tolerate
Etidronate the day, and patient must remain upright for a minimum of 30 minutes. oral intake (minimum 6 – 8 oz water) and
Risedronate Etidronate: held because of strict instructions for administration. Must be taken with 6 – 8 oz of water at least 2 hours before or after any food, beverage or is able to sit upright for a minimum of 30
medication. minutes.
22
No withdrawal effects and so there is no need for taper. Stopping pre-dental surgery advised but may not avoid osteonecrosis.
Ref 1, 12,22, 52
CARDIOVASCULAR DRUGS
Antiarrhythmics Continue Restart on schedule providing stable
Amiodarone hemodynamics (eg no bradycardia) and
Should be continued if the indication is a serious heart arrhythmia that causes hemodynamic instability. (eg. Sustained Ventricular Tachycardia). If clinically indicated, able to tolerate NG/PO.
Disopyramide, Flecanide, Procainamide, parenteral procainamide can be used as an alternative, if an IV formulation is required. IV form available if oral intake not
Propafenone, Quinidine, Sotalol Ref 1, 7 possible for an extended period of time.
Monitor closely if restarted, as these may
cause QT, ventricular arrhythmias
which are enhanced by changes in
electrolytes.
February 26, 2013 Page 4 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
Angiotensin Converting Enzyme (ACE) In general, continue. Associated with intra-operative hypotension. Restart once patient is hemodynamically
Inhibitors: Benazepril, Captopril, stable and able to tolerate NG/PO intake.
Cilazapril, Enalapril, Enalaprilat, In the following cases hold am of Check renal function before restarting.
Fosinopril, Lisinopril, Perindopril, surgery:
Quinapril, Ramipril, Tandolapril 1. Surgeries expecting large
blood losses.
Angiotensin II AT1 Receptor Blockers (ARBs): 2. Underlying renal dysfunction
Candesartan, Eprosartan, Irbesartan,
Losartan, Telmisartan, Valsartan
Ref 9
February 26, 2013 Page 5 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
CARDIOVASCULAR DRUGS
Antilipemic agents Hold a.m. of surgery All agents may cause perioperative muscle injury. Potential is greater when used in combination. No data on perioperative risk. No withdrawal effects and so there is Restart once patient is able to tolerate
Niacin no need for tapering. NG/PO intake, unless creatine kinase
Fibrates: Bezafibrate, Clofibrate, increases or rhabdomyolysis occurs.
Fenofibrate, Gemfibrozil
HMG CoA reductase inhibitors Continue Some pleotropic (anti-inflammatory, vasodilatory and antithrombotic effects). Growing evidence that perioperative statin therapy is safe and beneficial in reducing morbidity
Skrlin and Hou
Atorvastatin, Simvastatin and mortality in the perioperative period; with the greatest benefit in patients at higher risk for cardiovascular complications.
Pravastatin, Lovastatin, 18 19, 20
Good in-vitro data to suggest continuing treatment, limited data in non-cardiac populations. Case reports suggesting risk of rhabdomyolysis but a large
Fluvastatin 20
systematic review found only a 0.2% increased risk of CK elevations in statin-users (NNH 2,500). Potential for myopathy and rhabdomyolysis may be greater where
significant muscle damage occurs. Perioperative clinical trials showed no cases of rhabdomyolysis and the only
17
independent predictor for myopathy was length of surgery. Skrlin and Hou
Ref 17-20
Ezetimibe Hold a.m. of surgery No data on perioperative risk. No withdrawal effects and so there is no need for tapering.
Bile acid sequestrants Hold a.m. of surgery No data on perioperative risk. No withdrawal effects and so there is no need for tapering. Bile acid sequestrants bind some medications and therefore lower their
21
Cholestyramine bioavailability. As it may compromise the absorption of other medications, it is preferable to avoid in the immediate post-operative period.
Cholesipol Ref 7, 15, 21
β-Adrenergic Blocking Agents Continue β-blockers should be continued in patients undergoing surgery who are receiving them to treat cardiac conditions such as angina, symptomatic arrhythmias, Restart as soon as possible, provided
hypertension. There is a risk for withdrawal syndrome if therapy is discontinued abruptly. Abrupt discontinuation has been associated with an increased risk of peri- hemodynamically stable. If possible, no
operative infarction (OR 17.7, p = 0.003) and mortality (0% vs. 29%, p = 0.005). interruption in course of therapy.
If oral intake not possible, IV formulation can be used postoperatively. Metoprolol biovailability = 50%. Theoretical IV to PO ratio is 1:2.5. Due to a rapid maximum beta-
blockade with IV dosing, see suggested conversion below:
If < 25 mg PO convert to 2.5 mg IV q6h. If needed, increase dose by 2.5 mg IV q6h and titrate to effect
If > 25 mg PO convert to 5 mg IV q6h. If needed, increase dose by 5 mg IV q6h and titrate to effect.
Note: higher dosages such as 10-15 mg IV q4h may be required to achieve adequate beta blockade.
Ref 1, 17, 53, 54
Calcium Channel Blockers Continue No major adverse reactions reported in the perioperative period. Restart on schedule provided
No withdrawal reactions. hemodynamically stable (ie. no
Do not use short acting sublingual nifedipine to treat postoperative hypertension. bradycardia) and able to tolerate NG/PO.
For arrhythmias controlled with calcium channel blockers consider IV diltiazem or verapamil if patient unable to take NG/PO medications. Diltiazem may be preferred
since it has less negative inotropic/chronotropic effects therefore less likely to cause pulmonary edema or heart failure.
If taking long-acting formulations of diltiazem (e.g. Cardizem CD, Tiazac XC) or verapamil (e.g. Chronovera, Isoptin SR), determine daily dose, divide QID and use
immediate release formulation.
Ref 7
Digoxin Continue IV form available if oral intake not possible for an extended period of time. Restart on schedule provided
Serum levels taken perioperatively. hemodynamically stable (ie. no
A trough level should be taken 5 – 7 days after reinitiating therapy if no loading dose was given, 2 days after reinitiating therapy if a loading dose was given, and 1 – 3 bradycardia) and able to tolerate NG/PO.
weeks after reinitiating therapy if renal impairment is suspected.
Normal therapeutic range: 1.0 – 2.6 nmol/L
February 26, 2013 Page 6 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
Dosage adjustments maybe required postoperatively if problems with renal function.
Ref 1, 7, 11
CARDIOVASCULAR DRUGS
Diuretics Hold a.m. of surgery Potential for hypokalemia, intravascular volume depletion and hypotension. Monitor electrolytes and fluid status
Exception: Monitor electrolytes preoperatively. closely.
Continue if used for control of
chronic congestive heart failure.
Ref 10
Hypotensive Agents Continue In general, hypotensive agents should be given on the morning of surgery. Of note, clonidine is an central alpha-2 agonist. Abrupt cessation of central agonist may cause Restart once patient is hemodynamically
Clonidine dangerous rebound hypertension. stable and able to tolerate NG/PO intake.
If oral intake is not possible, parenteral agents such as esmolol, propranolol, hydralazine, diltiazem, nitrates are options.
When the discontinuation of clonidine is required and beta blockers are being used in combination, stop the beta blocker first to avoid unopposed alpha stimulation
which can potentiate rebound hypertension. Giving labetalol an alpha 1 and beta-adrenergic blocking agent may be useful.
Ref 1, 12, 17
Nitrates Continue Should be continued during the perioperative period if used as an antianginal to avoid compromising the stability of cardiac disease.
Isosorbide dinitrate Do not substitute with patches or ointment in the preoperative period, intraoperative transdermal absorption not reliable.
Isosorbide mononitrate If oral intake not possible postoperatively, ointment or patches can be used.
Ref 1, 7
RAAS antagonists Hold 24 hours prior to surgery Limited data. Aliskiren has a half life of 24 hours and is recommended to be withheld for 1 half life. Restart once patient is hemodynamically
Aliskiren stable and able to tolerate NG/PO intake.
Ref 95
CHOLINESTERASE INHIBITORS
Donepezil Continue May exaggerate the muscle relaxation effect of succinylcholine (inactivated by plasma cholinesterase) during anaesthesia and inhibit the effect of non-depolarizing Restart once tolerating PO/NG intake
Galantamine neuromuscular blocking agents. Restart carefully and titrate to avoid the
Rivastigmine Rivastigmine has a relatively shorter half-life. Give on morning of surgery if it coincides with patient’s usual regimen. risk of a cholinergic crisis.
Ref 72
February 26, 2013 Page 7 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
ANTICONVULSANTS
Antiepileptics Continue Risk of convulsion, hypoxia, aspiration pneumonia if withdrawn. Restart once tolerating NG/PO intake.
Gabapentin If patient unable to take oral doses postoperatively for an extended period of time then preoperative conversion to a drug with an IV form is suggested for those treated Give Phenytoin administered via the ng
Topiramate with drugs which only have an oral form. Postoperative level suggested where applicable. route 1 hour before or 2 hours after feeds
or any medications containing calcium,
Carbamazepine Normal Therapeutic Range Carbamazepine: 17 – 50 mol/L magnesium or aluminum.
Ethosuximide Normal Therapeutic Range Ethosuximide: 280 – 710 mol/L
Phenobarbital
Normal Therapeutic Range Phenobarbital: 65 – 170 mol/L
Phenytoin
Normal Therapeutic Range Phenytoin: 40 – 80 mol/L
Primidone
Normal Therapeutic Range Primidone: 20 – 25 mol/L
Valproic Acid
Normal Therapeutic Range Valproic Acid: 350 – 700 mol/L
Ref 7
February 26, 2013 Page 8 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
ANTIDEPRESSANTS
Monoamine Oxidase Inhibitors (MAO-I) In general - hold 2 weeks prior to Drug interaction with ephedrine can cause hypertensive crisis by releasing huge amounts of stored noradrenaline. Restart once tolerating NG/PO intake.
surgery. Drug interaction with meperidine, fentanyl, alfentanil, sufentanil and dextromethorphan can cause an excitatory reaction similar to serotonin syndrome.
Symptoms include agitation, headache and hemodynamic instability which can lead to pyrexia, seizure, coma and death.
Non Selective (Type A, B) Proper discontinuation of MAO-I drugs require a 2 week taper. These agents are usually used where depression is refractory to conventional treatments. Therefore the
Phenelzine Hold 10 – 14 days prior to surgery risk of relapse is a reality. Consider MAO-I safe anesthesia by avoiding drugs such as ephedrine, meperidine, fentanyl, alfentanil, and sufentanil.(not used in OR)
Hold 7 days prior to surgery
Trancypromine
Selective (Type A) Hold 2 days prior to surgery
Moclobemide Ref 1, 7, 9
Selective Serotinin Reuptake Inhibitors (SSRI) Continue Continue during the perioperative period no reports of interactions with anesthetics. Restart once tolerating NG/PO intake.
Citalopram, Fluoxetine, Withdrawal syndrome can occur after just one day of stopping therapy. Symptoms of this syndrome include dizziness, agitation, lethargy, nausea, chills, myalgias, gait
Fluvoxamine, Paroxetine, instability, shortness of breath and impaired short-term memory.
Sertraline Ref 1,7
Tricyclic antidepressants Hold a.m. of surgery Can be taken with caution during perioperative period. Restart once tolerating NG/PO intake.
Amitriptyline, Desipramine, Sympathomimetic activity of isoproterernol, phenylephrine, norepinephrine, epinephrine and amphetamines may be potentiated causing risk of hypertension and
Doxepine, Imipramine, arrhythmias.
Nortriptyline Rare adverse effects include sedation, delirium, reduced cardiac conduction and arrhythmias.
Tetracyclic agents If withholding is warranted, taper over several days due to their long half-life and potential for withdrawal syndrome.
Maprotiline,mirtazapine Ref 7, 10, 13
February 26, 2013 Page 9 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
ANTIDIABETIC AGENTS
Insulin See next column for details Depending on the severity of diabetes, daily insulin doses may be modified requiring the usage of intra-operative IV insulin infusion and supplemental SC insulin. IV Assess patient’s PO status, blood glucose
insulin infusion with supplemental SC insulin should be continued post-opertatively until the patient is able to tolerate oral intake or ng feeds. and insulin sensitivity. Usually continue
basal insulin at ½ of usual dose (e.g.
DM Type 1, Strongly consider using IV insulin infusion. Alternatively,
NPH) even if patient is NPO.
Take one quarter of total daily dose (TDD/4) every 12 hours as basal insulin (NPH type).
Individualize supplemental scale based on
Add supplemental fast-acting or rapid-acting insulin scale.
pt’s needs.
Start IV (D5W or 2/3 - 1/3) unless the patient is very hyperglycemic. (>15 mmol/L )
Patients with Type 1 Diabetes should NOT have their insulin infusion stopped due to the risk of ketoacidosis
DM Type 2, Usually treated with insulin
Take one quarter of total daily dose (TDD/4) every 12 hours as basal insulin (NPH type).
Check BG every 6 hours.
Add supplemental fast-acting or rapid-acting insulin scale
Very insulin-resistant/deficient patients (> 100 units/day) may be managed as Type 1 DM above.
Oral hypoglycemics Hold For short acting agents, hold evening and morning dose as patient will be fasting. For long acting agents (e.g. Diamicron MR, hold 24 hours prior to surgery). Resume once patient eating or tolerating
Acarbose (duration of hold depends on May need supplemental insulin PRN. Insulin supplemental scale may be required postoperatively until the patient is able to tolerate oral intake or ng feeds. NG feeds. Monitor blood glucose.
If insulin is needed for > 48 hours, start basal insulin (NPH) to promote smoother control. Start at 0.1 units/kg every 12 hours and continue supplemental q6h insulin.
Chlorpropamide, Tolbutamine half-life of drug)
Glicazide, Glyburide
Repaglinide
Pioglitazone
Rosiglitazone
Gliptins Resume postop once patient is eating and
96 96
Liraglutide Hold morning of surgery no longer experiencing nausea
Metformin Hold a.m. of surgery Lactic acidosis has rarely been associated with metformin use. Lactic acidosis is a serious and potentially avoidable complication: renal failure is a major factor Rule out renal dysfunction and patient
contributing to lactic acidosis. Other factors include sepsis, acute myocardial infarction, liver impairment and respiratory conditions leading to hypoxemia. able to tolerate oral intake or NG feeds.
Ref 1, 4
February 26, 2013 Page 10 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
ANTIPARKINSONIAN AGENTS Ref 1, 7, 9, 72
Dopaminergic agents: Levodopa/Carbidopa, Continue Restart as soon as possible post-opertatively to avoid the return of Parkinsonian symptoms. Withdrawal has been associated with symptoms similar to Neuroleptic Restart as soon as possible at the times
Levodopa/Benserzide Malignant Syndrome. Benefits of continued treatment outweighs risk of possible arrhythmias due to interaction with anaesthetic. which the medications administered prior
to stopping.
Dopamine agonists: Bromocriptine,
Pramipexole, Ropinorole
Anticholinergic agents: Benztropine,
Ethopropazine, Procyclidine,
Trihexyphenidyl
COMT Inhibitors: Entacapone Withdrawal of entacapone has been associated with a neuroleptic malignant-like syndrome. (ref: CPS 2008)
MAO Inhibitors, Selective (Type B): Selegiline
Continue May continue perioperatively, as long as MAOI-safe anaesthesia is used. At doses greater than 10mg selegiline becomes non-selective (ie: MAO-I Type A and B). Drug
Rasagiline interaction with meperidinie, fentanyl, sufentanil and alfentanil (can cause rigidity, hallucinations, fever, confusion, coma and death).
Hold 2-3 weeks prior to surgery
ANTIPSYCHOTICS
Clozapine, Chlopromazine Hold a.m. of surgery Can be continued with caution during the perioperative period. Restart once tolerating NG/PO intake.
Fluphenazine, Haloperidol Consider neuroleptic malignant syndrome if pattient develops hyperthermia, muscle rigidity and dysregulation of autonomic nervous system postoperatively. These
Olanzapine, Quetiapine symptoms are similar to malignant hyperthermia, which sometimes occur after anesthesia.
Risperidone, Thioridazine May be given to patient on a.m. of surgery in some conditions.
Ref 7
ANTI-RHEUMATIC AGENTS / GASTROINTESTINAL AGENTS
Sulfasalazine Hold a.m. of surgery In most cases holding one dose perioperatively will have minimal impact on the disease management. May continue peri-operatively if needed. Restart when tolerating oral,
Ref 73to 78 hemodynamically stable and if therapy
still indicated.
5-ASA products Hold a.m. of surgery In most cases holding one dose perioperatively will have minimal impact on the disease management. May continue peri-operatively if needed. Restart when tolerating oral and if
(ASACOL®,MESASAL®, MEZAVANT®, therapy still indicated.
SALOFALK®, PENTASA®)
Ref 73 to 78
February 26, 2013 Page 11 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
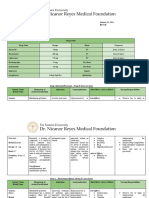
CORTICOSTEROIDS
Corticosteroids, oral 1. If Supplemental Steroid Perioperative adrenal insufficiency is an uncommon complication of surgery. Restart oral glucocortoids once tolerating
Betamethasone coverage will be given, Hold oral * Although oral budesonide bioavailability is only ~ 20%, it lowers plasma cortisol levels and can significantly alter adrenal function. Treat oral budesonide as any other NG/PO intake. Dose dependent on
93
Budesonide - see Recommendations* steroids a.m. of surgery. oral corticosteroid. previous steroid usage and postoperative
Dexamethasone 2. If Supplemental Steroid If perioperative glucocorticoid coverage is provided, it should be dependent on status.
Fludrocortisone coverage will NOT be given, 1) Surgical stress
Hydrocortisone Continue the usual oral steroids 2) Degree of HPA suppression ( which depends on the duration and dose of glucocorticoid therapy)
Methylprednisolone a.m. of surgery.
Prednisolone SHOULD STEROID COVERAGE BE PROVIDED?
Prednisone
Triancinolone MEDICAL STATUS PRENISONE DOSAGE HPA RESPONSE
Likely adequate adrenal function. No steroid coverage recommended.
Patients currently taking steroids ≤ 5 mg/day
Continue usual steroid dose perioperatively.
HPA response may be compromised. Steroid coverage recommended.
Patients currently taking steroids > 5 mg/day
See supplemental steroid coverage chart below.
Patients who stopped Likely adequate adrenal function.
≤ 5 mg/day
taking steroids < 3 months No steroid coverage recommended.
Patients who stopped HPA response may be compromised. Steroid coverage recommended.
> 5 mg/day
taking steroids < 3 months See supplemental steroid coverage chart below.
Patients who stopped HPA response likely normal.
> 5 mg/day
taking steroids > 3 months No steroid coverage recommended.
HOW MUCH SUPPLEMENTAL STEROID BE PROVIDED?
RECOMMENDED
DEGREE OF SURGICAL STRESS RECOMMENDED DURATION
CORTICOSTEROID DOSE
MINOR (ie. Inguinal hernia repair) Hydrocortisone 25 mg iv /day One dose preoperatively
Hydrocortisone 50 mg/day iv Preoperatively and taper rapidly to usual steroid
MODERATE (ie. Open cholecystectomy)
(Hydrocortisone 25mg iv q12h) dose over 1-2 days postoperatively
Hydrocortisone 100 mg/day iv Preoperatively and taper rapidly to usual steroid
SEVERE (ie proctocolectomy)
(Hydrocortisone 50mg iv q12h) dose over 2-3 days postoperatively
February 26, 2013 Page 12 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
CORTICOSTEROIDS, continued
Corticosteroids, oral, continued
COMPARATIVE PROPERTIES OF CORTICOSTEROIDS
DRUG BIOLOGIC HALF LIFE EQUIVALENT ANTI- RELATIVE MINERAL-CORTICOID POTENCY
( hr) INFLAMMATORY DOSE (mg)
BUDESONIDE 2-4 uncertain weak, relative effect uncertain
CORTISONE 8-12 25 2
HYDROCORTISONE 8-12 20 2
METHYLPREDNISOLONE 18-36 4 0
PREDNISOLONE 18-36 5 1
PREDNISONE 18-36 5 1
TRIAMCIOLONE 18-36 4 0
BETAMETHASONE 36-54 0.6 0
DEXAMETHASONE 36-54 0.75 0
FLUDROCORTISONE 12-24 10 125
Ref 58- 72
Corticosteroids, rectal
Hydrocortisone 100mg/60ml rectal Hold a.m. of surgery. If HPA As much as 30-90% can be absorbed systemically, and even greater if rectal/colon mucosa is inflamed. 30-90% of Hydrocortisone 100mg = Hydrocortisone 30mg to 90mg is
suspension suppression is likely equivalent to prednisone 7.5 -22.5mg.
Supplemental steroid coverage is
recommended
Hold a.m. of surgery
Budesonide 2mg/dose Enema Routine supplemental steroid Budesonide is a potent glucocorticosteroid with high topical potency and weak systemic effects.
coverage NOT recommended Systemic absorption is approximately 15-30%.
At recommended dose, budesonide enema causes no or minimal adrenal suppression.
Ref 58- 72
HERBALS
Echinacea Hold 7 – 14 days prior to surgery. Short-term use thought to boost immune system. Long-term use may actually suppress the immune system. Theoretical potential for problems with postoperative
wound healing and opportunistic infections.
Same as above.
Garlic Inhibits platelet aggregation. Postoperative bleeding a potential problem with the ingestion of large amounts.
Same as above.
Ginkgo Biloba Inhibits platelet aggregation (inhibition of platelet-aggregation factor). Spontaneous postoperative bleeds reported, including intracranial bleeding
Same as above.
Ginseng Inhibits platelet aggregation, possibly irreversibly. One case report of a significant drug interaction decreasing warfarin’s effect.
February 26, 2013 Page 13 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
HERBALS, continued
Ma Huang (Ephedra) Hold Immediately; Minimum 24 A potent sympathomimetic that causes an increase in blood pressure and pulse. Can cause tachycardia and arrhytmias. Effects are dose dependent. Do not restart if possible.
hrs prior to surgery. Drug interactions with other sympathomimetics e.g combination with Halothane can cause ventricular arrythmias.
Endogenous catecholamines depleted with long term use, risk for intraoperative hemodynamic instability.
Kava Hold Immediately; Minimum 24 Increase sedative effects of anaesthetic. Linked to severe liver injury.
hrs prior to surgery
Do not restart if possible.
St. John’s Wort Hold 7 – 14 days prior to surgery Induces cytochrome P-4503A4 enzymes therefore potential to affect metabolism of multiple drugs.
Valerian Taper dose a Can increase sedative effects of anesthetics. Has the potential to cause an acute benzodiazepine like withdrawal if stopped abruptly.
few weeks prior to surgery Alternative – continue use until surgery and benzodiazepines can be sued for withdrawal symptoms.
Danshen, Dong Quai Hold 7 – 14 days prior to surgery Interfere with warfarin action by prolonging clotting time.
Ginseng/Ginger/Fever Few Same as above Interfere with warfarin action by prolonging clotting time.
Other Herbals Same as above Interaction and effects unknown. Herbal products should be discontinued 7 to 14 days prior to surgery.
Ref 1, 7, 8
HORMONES AND HORMONE MODIFIERS Ref 79-90
Oral Contraceptive Pill (OCP) VTE risk dependent Whether or not to stop the oral contraceptives before surgery is a controversial issue. Estrogen interferes with the production and action of clotting factors. There is a
concern that patients taking OCPs will have a further increase in thromboembolic risk. The decision to continue or stop OCP before surgery must balance the risk of not
using OCP (ie. pregnancy, or excessive menstrual bleeding) against the risk of thromboembolism.
The incidence of VTE in young women who are non-OCP user is approximately 1-3 per 10,000 per year. Using OCP will increase the risk of VTE by 3-4 folds. The adverse
effects associated with estrogen are dose dependent.
LOW RISK If the patient is to have a low risk surgery and will soon be ambulating without any immobile extremities, consideration should be made to continue OCP since the Continue peri-operatively. DVT
Continue medical complications of an unplanned pregnancy may outweigh the risk of venous thromboembolism (VTE) prophylaxis recommended if appropriate.
HIGH RISK Recommended to discontinue if undergoing high-risk surgery. High-risk surgeries are defined as orthopedic surgery of the lower extremities and surgeries where long Continue holding for at least 2 weeks or
Hold 4 weeks prior to surgery periods of immobility are required. for duration of immobility.
Must use alternative form of contraception or progesterone only pills and ensure pregnancy status prior to OR. To be restarted with 1st day of menses.
DVT prophylaxis recommended if
appropriate.
February 26, 2013 Page 14 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
HORMONES AND HORMONE MODIFIERS Ref 79-90
Hormone Replacement Therapy (HRT) VTE risk dependent Risks and benefits of continuing or stopping HRT in the perioperative period must be assessed for individual patient. Restart when patient is fully mobile and
Estrogen dose is generally 20-25% of that contained in the oral contraceptives. Meta-analysis of 8 observational studies and 9 randomized controlled studies by Canonico able to tolerate oral intake. DVT
et. al showed a pooled odds ratio for oral estrogen for VTE = 2.4 and for transdermal estrogen = 1.2. prophylaxis recommended if appropriate.
Ref 90
LOW RISK OR TRANSDERMAL HRT Transdermal HRT is associated with less risk of VTE than oral HRT. Transdermal administration bypasses the first pass effect by the liver that may be responsible for
Continue induction of pro-clotting state. Scarabin PY et.al conducted a case-control study (n=536) which showed that transdermal HRT might be safer than oral HRT with respect
to thrombotic risk. Meta-analysis by Canonico also concludes transdermal estrogen did not confer additional VTE risks.
Ref 86, 90
HIGH RISK Recent case-control study (n=318) showed no association between peri-operative HRT use and post-operative thrombosis in patients undergoing major orthopedic
Hold 4 weeks prior to surgery surgery. Consider holding 4 weeks prior to surgery if multiple VTE risks.
Ref 81
Tamoxifen VTE risk dependent Risk of DVT and PE is approximately 2 folds. Oncologist should be consulted prior to discontinuation especially if used for breast cancer management to discuss Restart when patient is fully mobile and
risk/benefit ratio. able to tolerate oral intake. DVT
LOW RISK prophylaxis recommended if appropriate.
Hold a.m. of surgery
HIGH RISK
Hold 72 hours prior to surgery
Raloxifene VTE risk dependent A recent meta-analysis by Adomaityte et. al. evaluated the effects of raloxifene on VTE, which reports odds ratio of VTE = 1.62 in those who use raloxifene. Restart when patient is fully mobile and
Ref 89 able to tolerate oral intake. DVT
LOW RISK prophylaxis recommended if appropriate.
Hold a.m. of surgery
HIGH RISK
Hold 72 hours prior to surgery
Aromatase Inhibitors Continue Generally considered to have no increased risk of VTE Continue peri-operatively
Anastrozole (Arimidex®)
Letrozole (Femera®)
Exemestane (Aromasin®)
Megestrol (Megace®) Continue Synthetic progestin. Has weak glucocorticoid activity (few reports of adrenal suppression) Continue peri-operatively
Bicalutamide (Casodex®) Continue Non-steroidal anti-androgen. Continue peri-operatively
?finasteride?
MYASTHENIA GRAVIS AGENTS
Neostigmine Continue Withholding therapy may cause muscle weakness that would delay extubation post-op. recovery Continue peri-operatively. If oral intake
Pyridostigmine is not possible, IV form available.
Ref 7
February 26, 2013 Page 15 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
RESPIRATORY AGENTS
Inhaled Continue Administer just prior to surgery. Continue peri-operatively. Use nebulizers
For patients with asthma and chronic obstructive pulmonary dysfunction, use nebulizers postoperatively. Lung function is often affected in abdominal or thoracic if unable to use metered dose devices.
surgeries.
Beta-adrenergic agonists Extra doses may be given preoperatively to increase pulmonary function.
Anticholinergics
Corticosteroids Decreases pulmonary hyperactivity at time of endotracheal tube insertion and removal.
Ref 1, 12
Oral Restart once patient is able to tolerate
Theophylline Continue Optimize perioperative pulmonary stability. Continue despite narrow therapeutic window and high potential for drug interactions. Serum level preoperatively. Normal NG/PO intake.
Therapeutic Range: 55 – 110 mol/L.
Leukotriene Inhibitors Continue Little data. No parenteral formulations. No known interaction with anaesthetics. Continue through the morning of surgery.
Zafirlukast
Montelukast
Little data. No parenteral formulations. No known interactions with anaesthetics. Continue through the morning of surgery.
Lipoxygenase Inhibitors Continue. Ref 1
Zileutron
THYROID & ANTITHYROIDS
Levothyroxine Continue Missing 1 to 2 doses unlikely to be a problem due to its very long half-life of about 7 days. Restart once patient is able to tolerate
IV form available if patient unable to tolerate oral intake for an extremely long period of time. NG/PO intake.
Ref 1, 7
Anti-thyroid agents (for hyperthyroidism) Continue In hyperthyroid patients, thyroid storm is a major complication in the perioperative period. An overactive thyroid must be controlled. If not undergoing thyroidectomy, resume
Propylthiouracil Methimazole is preferred over propylthiouracil for long surgeries due to its long half-life and it’s once a day dosing schedule. once tolerating NG/PO intake.
Methimazole Beta blockers can be used to control symptoms of hyperthyroidism.
Ref 7
February 26, 2013 Page 16 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
IMMUNOSUPPRESSIVES / BIOLOGICS / MODULATORS
General approach to immunosuppressants / modulators: relative to most other therapies, there are few data on the perioperative risks of immunosuppressants and modulators. Primary concerns are impaired wound healing and risk of infection. There is also concern that changes in drug clearance
intra- and post-operatively will result in drug accumulation and cause drug toxicity. General considerations:
1. Consultation with the prescriber of the immunosuppressant/modulator is warranted to determine the risk of loss of disease control if the therapy is interrupted.
2. In the absence of clear evidence, weigh the individual’s risk of wound infection and impaired wound healing with loss of disease control. If the patient’s disease is under control and there is a high baseline risk of post-operative infection, this would weigh in favour of holding the drug for a
minimum of 5 half-lives preoperatively. Conversely if the patient’s disease is modestly controlled but improved on the therapy and the baseline risk of infection is low, this would weigh in favour of continuing the drug perioperatively.
3. Unless the therapy is being used as an adjunct to surgery, there is no need to administer the therapy on the day of surgery.
4. For drugs with serious adverse effect profiles, monitoring for changes in drug clearance intra- and post-operatively should be considered. If drug clearance is impaired, holding therapy post-operatively until clearance normalizes is advisable.
Azathioprine Continue Best evidence suggests azathioprine use is not an independent predictor of postoperative complications. Restart once tolerating NG/PO intake.
Can hold day of surgery to
reduce pill burden. Ref 25-29
23 24
Cyclosporine A In general, continue Few data available. Complication rates similar to tacrolimus-treated patients. but not increased perioperatively in ulcerative colitis patients. Generally continued Restart once tolerating NG/PO intake.
If elect to hold because of during the perioperative period. Ensure patient is well hydrated. Ensure proper hydration and renal
concerns with wound healing, If renal clearance is affected, monitor serum drug level. function. IV form available if oral intake
stop Sandimmune for 6 days and not possible for an extended period of
Neoral for 4 days prior to time.
surgery. Ref 23, 24
Imatinib Discuss with prescriber. If the surgery is related to the tumour, imatinib may be used deliberately throughout the perioperative period to reduce tumour burden; there are preliminary data Restart once tolerating NG/PO intake.
36
If elect to hold, stop ~ 8 days showing benefit preoperatively. Because the literature will evolve quickly, best to coordinate the decision with the patient’s oncologist. Imatinib can cause
preop (half-life of active thrombocytopenia but provided preoperative bloodwork does not indicate thrombocytopenia, there is no indication that it increases bleeding perioperatively.
metabolite = 40 hours). Ref 36
32
Methotrexate Continue. Can hold day of Data on interrupting methotrexate perioperatively weigh in favour of (consensus to) continuing through the perioperative period. Flares after stopping methotrexate Restart once tolerating NG/PO intake. If
30
surgery to reduce pill burden. would be expected to occur if methotrexate was stopped for several weeks; 1-2 days of treatment interruption would be unlikely to result in disease flares. parenteral, may resume immediately
post-operatively.
Ref 30-35
Mycophenolate Discuss with prescriber. Impairs wound healing but may be preferably to other options if an immunosuppressant must be used perioperatively. No data outside of transplantation. Moderate Restart once tolerating NG/PO intake.
If elect to hold, stop ~3 days quality data in renal transplant patients suggests an increased risk of wound infection and fascial dehiscence or incisional hernia was examined in 2,013 renal-transplant
37
preop (half-life of active patients.
metabolite = 8-16 hours). Ref 37
Rituximab Hold at least 6 months (1/2 year) Depletes B-cells. Half-life is very long with estimates ranging from 8 to 36 days. Consensus guideline for use of rituximab in Rheumatoid Arthritis recommends Rituximab re-treatment should not be
prior to surgery. discontinuing rituximab 6 months prior to surgery and if the arthritis is still well controlled at 6 months, to further postponed until B-cell counts have normalized (usually given until complete healing is
about 48 weeks). If surgery must be done within 6 months, assess need for additional antibiotic coverage and increase post-operative monitoring for infection. Ref achieved/absence of infection.
38- 40
February 26, 2013 Page 17 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
IMMUNOSUPPRESSIVES / BIOLOGICS / MODULATORS
Tacrolimus Discuss with prescriber. If elect to Few data are available. Similar rates of impaired wound healing to cyclosporine in transplant patients. Resume when staples/sutures can be
hold preoperatively, consider half- removed.
life range of 11-35 hours. Holding
7 days prior surgery would ensure
elimination.
Ref 23
TNF-alpha antagonists (adalimumab, Hold one treatment cycle prior to If conservative approach is recommended, hold one treatment
Evidence is conflicting regarding risks of anti-TNF therapy. Resume when staples/sutures can be
etanercept, infliximab) orthopedic surgery for patients cycle prior to surgery (1 week for etanercept, 6-8 weeks for infliximab and 2 weeks for removed.
with RA.
Mushtaq et al
adalimumab) Users anxious about stopping treatment perioperatively may elect to continue perioperatively. Best evidence failed to find a statistically
41
May continue treatment significant association with post-operative infection, but was associated with wound dehiscence.
perioperatively for IBD Ref 41-51
Kumar et al
patients.
MISCELLANEOUS AGENTS
Tamsulosin (FLOMAX) Hold minimum 14 days prior to Correlation between Floppy Iris Syndrome and tamsulosin during cataract surgery. Restart once tolerating NG/PO intake.
cataract surgery (earlier if Suggest stopping tamsulosin at least 14 days (earlier if possible) prior to cataract surgery in consultation with the patient’s urologist.
possible) Suggest when documenting medication history, tamsulosin should be clearly documented if the patient has taken this medication anytime up to one year prior to their
scheduled cataract surgery.
Ref 16
Lithium Hold a.m. of surgery. May prolong the effects of neuromuscular blocking agents. Restart once tolerating NG/PO intake.
At toxic levels may cause delirium, coma and arrhythmias.
If renal clearance is affected monitor serum drug level. Normal Therapeutic Range 0.4 – 1.3 mmol/L.
Ref 7
Memantine Continue NMDA Receptor Antagonist Restart once tolerating NG/PO intake.
Ref: 72
Vitamin E Hold minimum 7 days prior to Inhibits platelet aggregation. Postoperative bleeding a potential problem. Restart once able to tolerate NG/PO
surgery Ref 13 intake.
Ensure postoperative hemostais at
surgical site is adequate.
Vitamins, other Hold a.m. of surgery. Not needed on day of surgery. Restart once able to tolerate NG/PO
If considered essential and patient’s oral intake not possible for extended period of time consider IV multivitamin. intake.
Ref 1
February 26, 2013 Page 18 of 22
Drug Hold or Continue Relevant Pharmaceutical Effects / Recommendations When to Restart
Pre-op? Post-Op
Original document prepared 06/2003:M. Musing BScPhm, Lt. L.McMahon, BScPharm, L. Burry, PharmD. Reviewed by: C. Fan-Lun, P. Gill, S. Harley, H. Leung, Y. Rajmohamed, C. Zanchetta, Dr. Gordon Fox (Anesthesia), Dr. Rosa Braga-Mele (Ophthalmology), Dr. Keith Jarvi (Urology), Dr. Robin
McLeod (Surgery), Dr. Mitra Niroumand and Dr. Yash Patel (Medicine); Revised 05/2008 through 03.2010: H. Shin, L. Burry, D. Cheng, M. Musing, S. Sable, A. Wyllie. Reviewed by: M. Otremba (Medicine); R. MacLeod.
Revised and approved: Pharmacotherapy and Safe Medication Practice Committee 02/2007; 03/2010. Approved : Medical Advisory Committee 03/2010.
February 26, 2013 Page 19 of 22
References
1. Mercado DL, Petty BG. Perioperative medication managemant. Medical Clinics of North America 2003;87(1):41-57.
2. Drugs in the Peri-Operative Period: Hormonal contraceptives and hormone replacement therapy. DTB: Drug and Therapeutics Bulletin1999;37(10):78-80.
3. Oakes J, Hahn PM, Lillicrap D, Reid RL. A survey of recommendations by gynecologists in Canada regarding oral contraceptive use in the perioperative period. Am J Obstet Gynecol 2002;187(6):1539-43.
4. Jones GC, Macklin JP, Alexander WD. Contraindications to the Use of Metformin. BMJ 2003;326:4-5.
5. Merritt JC, Bhatt DL. The Efficacy and Safety of Perioperative Antiplatelet Therapy. Journal of Thrombosis and Thrombolysis 2002;13(2)97-103.
6. Noble DW, Webster J. Interrupting Drug Therapy in the Perioperative Period. Drug Safety 2002;25(7):489-495.
7. Spell NO. Stopping and Restarting Medications in the Perioperative Period. Medical Clinics of North America 2001; 85(5):1117-28.
8. Ang-Lee MK, Moss J, Yuan CS. Herbal Medicines and Perioperative Care. JAMA 2001; 286(2)208-214.
9. Smith MS, Muir H, Hall R. Perioperative Management of Drug Therapy, Clinical Considerations. Drugs 1996;51(2) 238-254.
10. Kroenke K, Gooby-Toedt D, Jackson JL. Chronic Medication in the Perioperative Period. Southern Medical Journal 1998;91(4)358-364.
11. Drugs in the Peri-Operative Period: Cardiovascular drugs. Drug and Therapeutics Bulletin 1999; 37(12)89-92.
12. Repchinsky C, eds. Compendium of Pharmaceuticals and Specialties. Toronto: Webcome Limited; Canadian Pharmacists Association; 2002.
13. McEvoy GK, eds. AHFS Drug Informaction. Bethesda: American Society of Health-System Pharmacists; 2003.
14. Murdoch J. To Bleed or Not to Bleed: the clot thickens. Pharmacy Practice 2002 June:43-46.
15. Repchinsky C, eds. Compendium of Pharmaceuticals and Specialties. Toronto: Webcome Limited; Canadian Pharmacists Association; 2005.
16. Chang DF, Campbell JR. Intraoperative Floppy Iris Syndrome Associated with Tamsulosin. J Cataract Refract Surg 2005(31):664-673.
17. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and care for Noncardiac Surgery. Circulation 2007;116:000-000.
18. Le Manach Y, Coriat P, Collard CD, Riedel B. Stain therapy within the perioperative period. Anesthesiology 2008;108(6):1141-6.
19. Poldermans D, Bax JJ, Kertai MD, et al. Statins are associated with a reduced incidence of perioperative mortality in patients undergoing major noncardiac vascular surgery. Circulation 2003;107:1848-51.
20. Kapoor AS, Kanji H, Buckingham J, Devereaux PJ, McAlister FA. Strength of evidence for perioperative use of statins to reduce cardiovascular risk: systematic review of controlled studies. BMJ, doi:10.1136/bmj.39006.531146.BE
21. Lipidil Supra Monograph, updated Nov 7, 2007.
22. Khan AA, Sandor GKB, Dore E, et al. Canadian Consensus Practice Guidelines for Bisphosphonate Associated Osteonecrosis of the Jaw. J Rheumatol 2008;35:1391-7.
23. Santangelo M, Clemente M, Spiezia S, Wound complications after kidney transplantation in nondiabetic patients. Transplant Proc. 2009;41(4):1221-3.
24. Hyde GM, Jewell DP, Kettlewell MG, Mortensen NJ. Cyclosporin for severe ulcerative colitis does not increase the rate of perioperative complications. Dis Colon Rectum 2001;44(10):1436-40.
25. Escalante A, Beardmore TD. Risk factors for early wound complications after orthopedic surgery for rheumatoid arthritis. J Rheumatol 1995;22:1844-51.
26. Kelley JT, Conn DL. Perioperative management of the rheumatic disease patient. Bulletin on the Rheumatic Disease 51(6).
27. Mahedevan U, Loftus EV, Tremaine WJ, et al. Azathioprine of 6-mercaptopurine before colectomy for ulcerative colitis is not associated with incrased postoperative complications. Inflammatory Bowel Disease 2002;8(5):311-6.
28. Colombel JF, Loftus EV, Tremaine WJ, et al. Early post-operative complications are not increased in patients with Crohn’s disease treated perioperative outcome in Crohn’s diseasetreated perioperatively with infliximab or immunosuppressive therapy. Am J Gastroenterol 2004;99:787-83.
29. Tay GS, Binion DG, Eastwood D, Otterson MF. Multivariate analysis suggests improved perioperative outcome in Crohn’s disease patients receiving immunomodulator therapy after segmental resection and/or strictureplasty. Surgery 2003;134;565-73.
30. Kremer JM, Rynes RI, Bartholomew LE. Severe flare of rheumatoid arthritis after discontinuation of long-term methotrexate therapy. Double-blind study. Am J Med 1987;82(4):781-6.
31. Pieringer H, Stuby U, Biesenbach G. The place of methotrexate perioperatively in elective orthopedic surgeries in patients with rheumatoid arthritis. Clin Rheumatol. 2008 Oct;27(10):1217-20.
32. Grennan DM, Gray J, Loudon J, Fear S. Methotrexate and early postoperative complications in patients with rheumatoid arthritis undergoing elective orthopaedic surgery. Ann Rheum Dis. 2001 Mar;60(3):214-7.
33. Bridges SL Jr, López-Méndez A, Han KH, Tracy IC, Alarcón GS. Should methotrexate be discontinued before elective orthopedic surgery in patients with rheumatoid arthritis? J Rheumatol. 1991 Jul;18(7):984-8.
34. Carpenter MT, West SG, Wogelgesang SA, Casey Jones DE. Postoperative joint infections in rheumatoid arthritis patients on methotrexate therapy. Orthopedics 1995;19(3):207-10.
35. Murata K, Yasuta T, Ito H, et al. Lack of increase in postoperative complications with low-dose methotrexate therapy in patients with rheumatoid arthritis undergoing elective orthopedic surgery. Mod Rheumatol. 2006;16(1):14-9.
36. Santos Fernandes GD, Blanke CD, Freitas D, al. Perioperative Treatment of Gastrointestinal Stromal Tumors. Oncology 2009;23(1).
37. Humar A, Ramcharan T, Denny R, et al. Are wound complications after a kidney transplant more common with modern immunosuppression? Transplantation 2001;72:1920–3.
February 26, 2013 Page 20 of 22
38. Pham T, Fautrel B, Gottenberg J-E, et al. Rituximab (MabThera) therapy and safety management. Clinical tool guide developed by the Rheumatic Diseases & Inflammation Group (Club Rhumatismes et Inflammation, CRI) of the French Society for Rheumatology (Société Française de
Rhumatologie, SFR). Joint Bone Spine 2008;75(Suppl 1):S2-99.
39. Usui M, Isaji S, Mizuno S, Sakurai H, Uemoto S. Experiences and problems pre-operative anti-CD20 monoclonal antibody infusion therapy with splenectomy and plasma exchange for ABO-incompatible living-donor liver transplantation. Clin Transplant. 2007;21(1):24-31.
40. Kawagishi N, Satoh K, Enomoto Y, et al. New strategy for ABO-incompatible living donor liver transplantation with anti-CD20 antibody. Transplant Proc. 2005;37:1205-6.
41. den Broeder AA, Creemers MCW, Fransen J, et al. Risk Factors for Surgical Site Infections and Other Complications in Elective Surgery in Patients with Rheumatoid Arthritis with Special Attention for Anti-Tumor Necrosis Factor: A Large Retrospective Study. J Rheumatol 2007;34(4):689–95.
42. Fisher CJ, Agosti JM, Opal SM, et al. Treatment of septic shock with the tumor necrosis factor receptor:Fc fusion protein. The Soluble TNF Receptor Sepsis Study Group. N Engl J Med 1996;334:1697–1702.
43. Scanzello CR, Figgie MP, Nestor BJ, Goodman SM. Perioperative Management of Medications used in the Treatment of Rheumatoid Arthritis. Hospital for Special Surgery 2006;2(2):141-7.
44. Poss R, Thornhill TS, Ewald FC, et al. Factors influencing the incidence and outcome of infection following total joint arthroplasty. Clin Orthop Relat Res 1984;182:117–26.
45. Wilson MG, Kelley K, Thornhill TS. Infection as a complication of total knee-replacement arthroplasty: risk factors and treatment in sixty-seven cases. J Bone Joint Surg Am 1990;72:878–83.
46. Bibbo C, Goldberg JW. Infectious and healing complications after elective orthopaedic foot and ankle surgery during tumor necrosis factor-alpha inhibition therapy. Foot Ankle Int 2005;25(5):331–335.
47. Ruyessen-Witrand A, Gossec L, Salliot C, et al. Complication rates of 127 surgical procedures performed in rheumatic patients receiving tumor necrosis factor alpha blockers. Clin Exp Rheumatol. 2007;25(3):430-6.
48. Giles JT, Bartlett SJ, Gelber AC, et al. Tumor necrosis factor inhibitor therapy and risk of serious postoperative orthopedic infection in Rheumatoid Arthritis. Arthritis Care Res 2006;55(2):333–337.
49. Kunitake H, Hodin R, Shellito PC, et al. Perioperative treatment with infliximab in patients with Crohn's disease and ulcerative colitis is not associated with an increased rate of postoperative complications. J Gastrointest Surg 2008;12(10):1730-6.
50. Appau KA, Fazio VW, Shen B, et al. Use of Infliximab within 3 Months of Ileocolonic Resection is Associated with Adverse Postoperative Outcomes in Crohn’s PatientsJ Gastrointest Surg 2008;12(10):1738-44.
51. Colombel JF, Loftus EV, Tremaine WJ, et al. Early postoperative complications are not increased in patients with Crohn’s Disease treated perioperatively with infliximab or immunosuppressive therapy. Am J Gastroenterol 2004;99(5):878-83.
52. Black DM, Schwartz AV, Ensrud KE, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 2006;296(24):2927-38.
53. Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 Guidelines on peri-operative cardiovascular evaluation and care for non-cardiac surgery: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol 2007;50(17):e159-
241.
54. Shammash JB, Trost JC, Gold JM, et al. Peri-operative beta-blocker withdrawal and mortality in vascular surgical patients. Am Heart Journal 2001;141(1):148-153.
55. Peng PWH, Tumber PS, Gourlay D. Review article: Perioperative pain management of patients on methadone therapy. Can J Anesth 2005;(5) 513-523
56. Isaac P, Kalvik A, Janecek E, Brands J. Methadone Maintenance: A Pharmacist’s Guide to Treatment. 2nd Edition 2004 Pg 83-84
57. Shim YH, Kersten JR. Preconditioning, anesthetics, and perioperative medication. Best Practice and Reasearch Clinical Anesthesiology 2008;(1) 151-165
58. Marik PE, Varon J. Requirement of Perioperative Stress Doses of Corticosteroids. A systemic review of literature. Arch Surg 2008;143(12):1222-1226
59. Salem et. Al. Perioperative Glucocorticoid Coverage. A reassessment 42 years after emergence of a problem. Annals of surgery 1994;219(4):416-425
60. Coursin DB, and Wood KE. Corticosteroid Supplementation for Adrenal Insufficiency. JAMA 2002;287(2):236-240
61. Mercado et.al. Perioperative medication management. Med Clin N Am 2003;87:41-57
62. Krasner AS. Glucocorticoid-Induced Adrenal Insufficiency. JAMA 1999;282(7):701
63. Nicholson et.al. Peri-Operative steroid supplementation. Anaesthesia 1998;53:1091-1104
64. Larsen: Williams Textbook of Endocrinology. 10th Edition. www. Mdconsult. Com/das/book/bod/85950831-15/663942196/1096/314html?SEQ...
65. LaRochelle G. Recovery of the hypothalamic-pituitary-adrenal (HPA) axis in patients with rheumatic disease receiving low-dose prednisone. AM J Med 1993;95(3)258-264
66. Howe CR et.al. Perioperative Medication Management for the patients with Rheumatoid Arthritis. J Am Acad Orthop Surg 2006;14:544-551
67. Wakim JH et.al. Anesthetic implications for patients receiving exogenous corticosteroids. AANA 2006;74(2):133-139
68. Baid SK and Nieman. Therapeutic doses of glucocorticoids: implications for oral medicine. Oral Disease 2006;12:436-442
69. Axelrod L. Perioperative management of patients treated with glucocorticoids. Endocrinol Metab Clin North Am 2003;32(2):367-383
70. Kelley et.al. Perioperative management of the rheumatic disease patients. Bulletin on the Rheumatic Diseases. Volume 5, number 6
71. Nagelhout J, Elisha S, waters E. Should I continue or discontinue that medication? AANA Journal February 9. Vol.77 no 1. Pg 59-73
72. Ramuscak N, Friedland M, and Otawa S. CPS: Clin-Info. Perioperative Management of Medications. 2008
73. Plosker GL. And Croom KF. Sulfasalazine: A review of its use in the management of rheumatoid arthritis. Drugs 2005;65(13):1825-1849
74. Howe CR, Gardner GC, and Kadel NJ. Perioperative Medications Management for the patient with rheumatoid Arthritis. J AmAcad Orthopp Surg 2006;14:544-551
February 26, 2013 Page 21 of 22
75. Busti AJ et al. Reviews of therapeutics: Effects of perioperative anti-inflammatory and immunodulating therapy on surgical wound healing. Pharmacotherapy 2005;25(11):1566-1591
76. Rosandich PA, Kelley JT, and Conn DL. Perioperative management of patients with rheumatoid arthritis in the era of biologic response modifiers. Current opinion in rheumatology 2004, 16:192-198
77. Hernandez C, Emer J, Robinson JK. Perioperative Management of medications for psoriasis and Psoriatic Arthritis: A review for the Dermasurgeons. Dermatol surg 2008;34:446-459
78. Kelley JT and Conn DL. Perioperative management of the Rheumatic Disease patient. Bulletin on the Rheumatic Diseases 2002 vol 51, number6.
79. Anderson FA and Spencer FA. Risk factors for Venous thromboemobolis. Cirulation 2003;107;I-9-I-16 [no comments on guidelines of continuing or discontinuing estrogen products pre-operatively]
80. Thromboemoblic Risk Factor Consensus Group. Risk of and prophylaxis for venous thromboembolism in hospital patients. BMJ 1992;305;567-574
81. Hurbanek et. Al. Postmenopausal hormone replacement and venous thromboembolism following hip and knee arthroplasty. Thromb Haemost. 2004 Agu;92(2):337-43
82. Douketis J. Hormone replacement therapy and risk for venous thromboembolism: what’s new and how do these findings influence clinical practice? Curr Opin Hematol 12:395-400.
83. Rathbun S. Venous thromboembolism in women. Vascular medicine 2008;13:255-266
84. Nagelhout J, Elisha S, waters E. Should I continue or discontinue that medication? AANA Journal February 9. Vol.77 no 1. Pg 59-73
85. Bundred NJ. The effects of aromatase inhibitors on lipids and thrombosis. British Journal of Cancer 2005;95(Supp 1):523-527
86. Scarabin PY et. al. Differential association of oral and transdermal oestrogen replacement therapy with venous thromboembolism risk. Lancet 2003;362(9391)428-432
87. Fabian CJ. The what, why and how of aromatase inhibitors: hormonal agents for treatment and prevention of breast cancer. Int J Clin Pract 2007;61(12):2051-2063
88. Bundred NJ. The effects of aromatase inhibitors on lipids and thrombosis. British Journal of Cancer 2005;93(suppl 1): S23-S27
89. Adomaityte J. Effects of raloxifene therapy on venous thromboembolism in postmenopausal women. A Meta-analysis. Thromb Haemost 2008;99(2):338-342
90. Canonico M. et al. Hormone replacement therapy and risk of venous thromboembolism in postmenopausal women: systematic review and meta-analysis. BMJ 2008;336;1227-1231
91. Memis D, Turan A, Karamanjioglu B, et al. The effect of intravenous pantoprazole and ranitidine for improving preoperative gastric fluid properties in adults undergoing elective surgery. Anesth Analg 2003;97(5):1360-3.
92. Nishina K, Mikawa K, Takao Y, et al. A comparison of rabeprazole, lansoprazole, and ranitidine for improving preoperative gastric fluid property in adults undergoing elective surgery. Anesth Analg 2000;90(3):717-21.
93. Lichtenstein GR, Bengtsson B, Lapten-White L, et al. Oral budesonide for maintenance of remission of Crohn’s disease: a pooled safety analysis. Aliment Pharmacol Ther 2009;29:643-53.
94. Auron M, Harte B, Kumar A,n and Michota F. Renin-angiotensin system antagonists in the perioperative setting: clinical consequences and recommendations for practice. Postgrad Med Journal. 2011;87(1029):472-81.
95. Perioperative disease management. The Medicine Consult Handbook. Accessed March 8, 2011. Updated May 2011. http://depts.washington.edu/medcons/handbookpdfs/diabetes2011.pdf.
February 26, 2013 Page 22 of 22
You might also like
- Pharmacokinetics in Drug Development - Problems and Challenges in Oncology, Volume 4Document335 pagesPharmacokinetics in Drug Development - Problems and Challenges in Oncology, Volume 4vergoslimaNo ratings yet
- General Pharmacology - Model Question and Answer PDFDocument9 pagesGeneral Pharmacology - Model Question and Answer PDFNirav Patel100% (1)
- Clinical Med CardsDocument26 pagesClinical Med CardsLila DanielsNo ratings yet
- Clinical Trials in Cardiology 2nd Ed PDFDocument272 pagesClinical Trials in Cardiology 2nd Ed PDFIrving H Torres LopezNo ratings yet
- Pre-Op Medication Reference SheetDocument3 pagesPre-Op Medication Reference Sheetsabbo morsNo ratings yet
- Pre Medications AnaesthesiaDocument34 pagesPre Medications AnaesthesiastadolinNo ratings yet
- Corticosteroid Guidelines PDFDocument6 pagesCorticosteroid Guidelines PDFMariskaNo ratings yet
- Guide To Clinical Audit Antibiotic Use in Urinary Tract InfectionDocument10 pagesGuide To Clinical Audit Antibiotic Use in Urinary Tract Infectionihtisham1No ratings yet
- Divalproex Sodium (Depakote ER)Document1 pageDivalproex Sodium (Depakote ER)karenmichellelecarozNo ratings yet
- Drug StudyDocument6 pagesDrug StudyJorge RabajaNo ratings yet
- Drug-Study OmeprazoleDocument1 pageDrug-Study OmeprazoleBeverly Datu71% (7)
- Drug Study Anemia PTDocument3 pagesDrug Study Anemia PTLex CatNo ratings yet
- Cyclophosphamide Doxorubicin Ver 1.1Document6 pagesCyclophosphamide Doxorubicin Ver 1.1Yudi ApriyantoNo ratings yet
- Articaine (Septocaine) : Mu-Opioid Receptors Are in A Family of G-Protein Coupled ReceptorsDocument30 pagesArticaine (Septocaine) : Mu-Opioid Receptors Are in A Family of G-Protein Coupled ReceptorsphamnhuchauphuongNo ratings yet
- Drug StudyDocument11 pagesDrug StudyKaguraNo ratings yet
- Rabbit Formulary: Inhalation AnestheticsDocument3 pagesRabbit Formulary: Inhalation AnestheticsMiriam CervantesNo ratings yet
- FatmaaaaaaaDocument20 pagesFatmaaaaaaaJoash LagareNo ratings yet
- Gantala Drug Stusy-TabhsoDocument8 pagesGantala Drug Stusy-TabhsoHey it's FerdyNo ratings yet
- Acifix: Description Drug Interactions Pharmaceutical PrecautionsDocument1 pageAcifix: Description Drug Interactions Pharmaceutical PrecautionsSaifur Rahman SuzonNo ratings yet
- Systemic: Gastric Acidity in Water q4h Pregnancy and Lactation Use With Caution in Clients With Renal ImpairmentDocument6 pagesSystemic: Gastric Acidity in Water q4h Pregnancy and Lactation Use With Caution in Clients With Renal ImpairmentVictoriaNo ratings yet
- DHM Collection-Instructions Urea-Breath-Test 201902 - UnknownDocument2 pagesDHM Collection-Instructions Urea-Breath-Test 201902 - Unknownjohn mewNo ratings yet
- Carboplatin With Pemetrexed Pembrolizumab Non Squamous Non-Small Cell Lung Cancer Protocol V1.1Document8 pagesCarboplatin With Pemetrexed Pembrolizumab Non Squamous Non-Small Cell Lung Cancer Protocol V1.1Olaru DianaNo ratings yet
- RamadandruginfoDocument1 pageRamadandruginfoNassèym ĀŕNo ratings yet
- Antihypertensive in AkiDocument16 pagesAntihypertensive in AkiChia Yin NgNo ratings yet
- Pain Sedation and Delirium Topic DiscussionDocument6 pagesPain Sedation and Delirium Topic Discussionapi-648891519No ratings yet
- 1 - New Drug Update 2015 - FINALEBDocument62 pages1 - New Drug Update 2015 - FINALEBnikhilNo ratings yet
- Drug Study SurgeryDocument1 pageDrug Study SurgerygorgeazNo ratings yet
- Name of DrugDocument6 pagesName of DrugKathleen ColinioNo ratings yet
- Propofol Drug StudyDocument3 pagesPropofol Drug Studygersalia.christiennikkiNo ratings yet
- Drug Study Kathleen Claire ColinioDocument11 pagesDrug Study Kathleen Claire ColinioKathleen ColinioNo ratings yet
- Combined Lipid HTN Neuro 2022Document7 pagesCombined Lipid HTN Neuro 2022Adina BrahaNo ratings yet
- 776 NSAIDsguidelinesDraftV2Nov09Document3 pages776 NSAIDsguidelinesDraftV2Nov09KavirNivNo ratings yet
- Patient NameDocument4 pagesPatient NameCatherine MetraNo ratings yet
- Medical TherapyDocument6 pagesMedical Therapyvinay reddyNo ratings yet
- Drug Study: Drug Indication Action Contraindication Adverse Effect Nursing Consideration Generic Name: Omeprazole 40mgDocument9 pagesDrug Study: Drug Indication Action Contraindication Adverse Effect Nursing Consideration Generic Name: Omeprazole 40mgNica SalazarNo ratings yet
- Drug TabDocument6 pagesDrug TabATEHAN BORDSNo ratings yet
- CM KG M: Ukall 14 Consolidation 2 Height Weight BSADocument2 pagesCM KG M: Ukall 14 Consolidation 2 Height Weight BSAKena BenNo ratings yet
- H N O S CH N: Indication DosageDocument2 pagesH N O S CH N: Indication DosagehelloaNo ratings yet
- Durg Profile 6396Document7 pagesDurg Profile 6396MUHAMMAD ZOHAIBNo ratings yet
- Drug Study: 10cc/1vialDocument2 pagesDrug Study: 10cc/1vialJoevence Gazo CuaresmaNo ratings yet
- Dexamethasone Deep Dive PDFDocument1 pageDexamethasone Deep Dive PDFRizky TiensNo ratings yet
- Anticoagulant Guidelines ASHDocument8 pagesAnticoagulant Guidelines ASHmandamanda31No ratings yet
- 596 Ifosfamide Etoposide Ie TherapyDocument6 pages596 Ifosfamide Etoposide Ie Therapyravindra0504090No ratings yet
- Perioperative CVS MedicationDocument3 pagesPerioperative CVS MedicationAminn Alhassan ContehNo ratings yet
- PDF Surgical Prophylaxis Poster Dec 2021Document1 pagePDF Surgical Prophylaxis Poster Dec 2021Midhun KishorNo ratings yet
- Top 5 Corticosteroids For Use in Emergency SettingsDocument4 pagesTop 5 Corticosteroids For Use in Emergency SettingsIulian Cătălin GrămadăNo ratings yet
- Pallcare Pain Medsv6 - 17 8 2015Document5 pagesPallcare Pain Medsv6 - 17 8 20159mvsr5d9hhNo ratings yet
- Advantages and Disadvantages of Oral Anticoagulants - UpToDateDocument2 pagesAdvantages and Disadvantages of Oral Anticoagulants - UpToDateMunkhjargal BatmunkhNo ratings yet
- Perioperative Medicines Management V8Document7 pagesPerioperative Medicines Management V8Waleed Ahmad.No ratings yet
- Antimicrobial Agents Mucosal Protective Agents: Amoxicillin Clarithromycin SucralfateDocument2 pagesAntimicrobial Agents Mucosal Protective Agents: Amoxicillin Clarithromycin SucralfateAlexandra AlexaNo ratings yet
- MILV8N8Document4 pagesMILV8N8garywall.ukNo ratings yet
- Drug Mechanism of Action Indication Contraindication Adverse Effect Nursing Considerations Generic NameDocument2 pagesDrug Mechanism of Action Indication Contraindication Adverse Effect Nursing Considerations Generic NameJohn Edward EscoteNo ratings yet
- Management Strategies For Primary Dysmenorrhea: 9.1 Topic OverviewDocument19 pagesManagement Strategies For Primary Dysmenorrhea: 9.1 Topic OverviewAgusdiwana SuarniNo ratings yet
- AmlodipineDocument2 pagesAmlodipineAnonymous QqyLDoW1No ratings yet
- Medical ManagementDocument3 pagesMedical ManagementMark Jefferson LunaNo ratings yet
- Rivaroxaban PresentationDocument13 pagesRivaroxaban PresentationReem El-HusseinyNo ratings yet
- KJJJDocument6 pagesKJJJMarcieNo ratings yet
- Antimicrobial Dosage Adjustments in Renal Impairment For FormularyDocument20 pagesAntimicrobial Dosage Adjustments in Renal Impairment For Formularyangkatanjuli2019No ratings yet
- TramadolDocument2 pagesTramadoldwightciderNo ratings yet
- Magumun - 3B WARDDocument13 pagesMagumun - 3B WARDFrancesca Aurea MagumunNo ratings yet
- Gastritis Ulcer Drugs Classification: Pio Ari PrasastiDocument16 pagesGastritis Ulcer Drugs Classification: Pio Ari Prasastipio ari prasastiNo ratings yet
- Chemo Protocol PermetrexedDocument4 pagesChemo Protocol PermetrexedSangireddy NarreddyNo ratings yet
- BNF Childern IritasiDocument4 pagesBNF Childern IritasiKiki Amelia MarthaNo ratings yet
- NCLEX Drugs CalculationDocument3 pagesNCLEX Drugs CalculationajhienngNo ratings yet
- Praziquantel in TurtlesDocument1 pagePraziquantel in TurtlesMara Hernández FresnilloNo ratings yet
- Aim 4 Aiims 3Document72 pagesAim 4 Aiims 3DrKunal JoshiNo ratings yet
- Module 2Document14 pagesModule 2Arnel Billy LimNo ratings yet
- Diploma in Pharmacy (Part - II) Examination Hospital & Clinical PharmacyDocument3 pagesDiploma in Pharmacy (Part - II) Examination Hospital & Clinical PharmacymifuoNo ratings yet
- S.O Lourdes AdditionalDocument4 pagesS.O Lourdes AdditionalJacques oltradeNo ratings yet
- 1-Panadol Advance 6-Panadol Sinus 2-Panadol Extra 7-Panadol Night 3-Panadol Actifast 4-Panadol Joint 5-Panadol Cold and Flu and Their TypesDocument12 pages1-Panadol Advance 6-Panadol Sinus 2-Panadol Extra 7-Panadol Night 3-Panadol Actifast 4-Panadol Joint 5-Panadol Cold and Flu and Their TypesSulaiman AlqatfNo ratings yet
- Annotated BibliographyDocument6 pagesAnnotated Bibliographyapi-451590039No ratings yet
- Jurnal SR 3Document12 pagesJurnal SR 3Zaina Khairunisa AsyaNo ratings yet
- Cancer ChemotherapyDocument79 pagesCancer ChemotherapyDanii-Boo InspiraNo ratings yet
- Butilbromuro de Hioscina Una Revisión de Su Uso en El Tratamiento de Cólicos y Dolor AbdominalDocument6 pagesButilbromuro de Hioscina Una Revisión de Su Uso en El Tratamiento de Cólicos y Dolor AbdominalalexqaNo ratings yet
- Top Pharma CompaniesDocument8 pagesTop Pharma CompaniesMichael BrownNo ratings yet
- Daftar Obat ApotekDocument4 pagesDaftar Obat ApotekSriNo ratings yet
- Flexilor RangeDocument31 pagesFlexilor RangekurutalaNo ratings yet
- Sys Review Tinea CrurisDocument3 pagesSys Review Tinea CrurisenintakrynNo ratings yet
- Neuromuscular Blocking DrugsDocument22 pagesNeuromuscular Blocking DrugsMuhammad Shahid BilalNo ratings yet
- Computer ApplicationsDocument8 pagesComputer ApplicationsHusnaNo ratings yet
- Pricelist Update Agustus 2023Document6 pagesPricelist Update Agustus 2023greenika yulendaNo ratings yet
- Amoxicillin + HydrochlorothiazideDocument1 pageAmoxicillin + HydrochlorothiazideAnonymous wmF9p2ejNo ratings yet
- Miura D Inj Leaflet PakistanDocument1 pageMiura D Inj Leaflet PakistanMuhammad Azhar SattarNo ratings yet
- Adm Resep Tipe 1 Usk 2020Document9 pagesAdm Resep Tipe 1 Usk 2020Oman TirtaNo ratings yet
- Ra FinaleDocument80 pagesRa FinaleJoanaNo ratings yet
- Drug Use in Paeds and ElderlyDocument27 pagesDrug Use in Paeds and ElderlyCuthbert Tinotenda MusarurwaNo ratings yet
- 3-SHIFT Elevated Heart RateDocument11 pages3-SHIFT Elevated Heart RateMochammad IchwanuddinNo ratings yet
- Medication Dosing For Continuous Enteral Feedings Adult Inpatient 15.09.18 New LinksDocument30 pagesMedication Dosing For Continuous Enteral Feedings Adult Inpatient 15.09.18 New LinksMarsyaNo ratings yet
- Magensium SulfateDocument2 pagesMagensium SulfateAndrea ANo ratings yet