Professional Documents
Culture Documents
Pallcare Pain Medsv6 - 17 8 2015
Uploaded by
9mvsr5d9hhOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pallcare Pain Medsv6 - 17 8 2015
Uploaded by
9mvsr5d9hhCopyright:
Available Formats
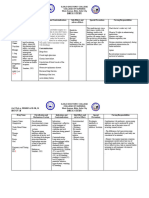
Chronic Kidney Disease and commonly used medications in Palliative Care.
Adaptation of Palliative Care drugs in Renal Failure by Yorkshire Palliative Medicine Guidelines
Group (2006) and Broadbent et al (2003).
Waiver: All efforts have been made to ensure the accuracy of these guidelines. The best information available has been used. Readers should exercise clinical judgement in the use of all medications. The authors of this guideline do not accept responsibility for its use in practice.
DRUG Action in end of METABOLITES ELIMINATION Dose/interval change in Adult Dose with Renal Failure Dose/interval HF HD NEPHRO OTHER COMMENTS
life care (A=active, (D=drug, renal failure change in renal TOXIC?
I=inactive) M=metabolites) GFR replacement Rx (Y/N)
PD
Amitriptyline (Endep) Neuropathic Pain Metabolised in the D < 5% excreted No change to normal No change to usual dose. Starting dose Not dialysed Unknown Not dialysed No "Although no dose reduction is required, a low starting dose is
liver. Main active unchanged in urine doses. 10mg nocte. Increase dose according to recommended given the likelihood of anticholinergic side
metabolite is response and tolerability. effects." (Davison & Koncicki, 2014) Contraindicated in
nortriptyline. Glaucoma, recent AMIs, arrhythmias and any degree of heart
block. Has multiple drug interactions (see The Renal Drug
Handbook (4th ed) , MIMS ). Note particularly the combination
of TCAs and SSRIs causes an increase in plasma
concentrations of TCAs by 20 % to 10 times (Palliative Care
Formulary , 5th ed, 2014). Side effects - Antihistamine effect -
sedation; Anticholinergic effect - dry mouth, blurred vision,
constipation, urinary retention.
Atropine 1% Drops Terminal Incompletely Readily absorbed from 2 drops sublingual q 2-4hrly May be used as first line as an anti-secretory agent in patients
secretions. metabolised by mucous membranes. with terminal secretions. Atropine given by injection “should be
Anticholinergic the liver About 30-50 % administered with excessive care” in patients with renal
excreted either as impairment (MIMS, 2014).
parent drug or
metabolites in the
urine.
Buprenorphine Pain Buprenorphine -3- Approximately 70 % is 10-50 ml/min No change Starting dose - 5mg patch changed Dialysed – Dialysed – Dialysed – No "Buprenorphine may be given in standard doses to patients with
(Norspan) patches management glucuronide (B3G) excreted in the faeces <10 ml/min Patches 5mg every 7 days dose as for dose as for dose as for GFR< CKD. Generally considered safe for use in CKD if monitored
– inactive. as unchanged minimum dose changed GFR< 10mls/min GFR< 10mls/min carefully." (Davison & Koncicki 2014). Buprenorphine patches
Norbuprenorphine buprenorphine. every 7 days 10mls/min are not suitable for acute pain. The Renal Drugs Handbook
. Metabolites are Injection & S/L: Reduce (4th ed) states that “it may take up to 30 hours for plasma
principally excreted in dose by 25- buprenorphine concentration to decrease by 50 % after the
the bilary system. 50%. Avoid large single …patch has been removed” and advises against giving another
Some urinary excretion doses opioid for 24 hours after the removal of the patch.
of metabolites occurs.
Buscopan (see
Hyoscine
Butylbromide)
Clonazepam (Rivotril) Benzodiazepine. 7-amino- Renal (D) <1% No dose adjustment Commence 0.25 - 0.5 mg nocte SL/sci Dose as normal No data Not dialysed No Can be used as a sublingual drops. In the terminal phase could
Uraemic jerks, clonazepam (I) unchanged required and increase according to response. renal function use Clonazepam drops sublingually or Midazalom
Restless Legs 7-acetylamino- *INCREASED RISK OF Unknown subcutaneously.
Syndrome, clonazepam (I) SEDATION IN RENAL dialysability
intractable 3-hydroxy- FAILURE
hiccups, terminal clonazepam (A)
agitation.
Codeine Pain, cough, C6G (A), 0-16 % excreted in the 20-50 - normal dose Not recommended in CKD Unlikely to be Unknown Not dialysed. No "Metabolized to morphine derivatives and known to cause
diarrhoea. Norcodeine 20-50 urine. Note active 10-20 - 75% normal dose dialysed dialysability. profound hypotension and CNS and respiratory depression.
10-20 <10 metabolites. <10 - 50% dose Not recommended in CKD". Davison & Koncicki et al (2014).
(?),Morphine (A) Note Renal Drugs Handbook (4th ed) permits doses
M3G (I)M6G (A) commencing 30mg qid in patients on dialysis and those with an
eGFR < 10.
Cyclizine Centrally acting The inactive <1% excreted No change to normal 50mg tds po/sci/ivi Unknown Unknown Unknown No Increased central sensitivity in patients with renal failure.
antiemetic metabolite is unchanged in urine doses. “Elderly patients are more susceptible to sedative and central
(antihistaminic, norcyclizine. antimuscarinic effects eg. postural hypotension, memory
antimuscarinic) impairment, extrapyramidal reactions.” (Palliative Care
Formulary, 5th ed, 2014). Not recommended in the terminal
phase.
Dexamethasone Breathlessness 65% (I) 8% unchanged GFR <10ml/min Dosing according to indication. Typical Not dialysed No data Not dialysed No "Does not require dose adjustment, but may be complicated by
Appetite eliminated in urine Normal dose tapered to commencing dose - 4mg mane. If using fluid retention" (Yorkshire Group, 2006. p.9)
Renal (D,M) minimum effective dose more than one daily dose use mane and For anorexia should consult Renal Dietician. Be aware of the
midi dosings only. significant side effects of Dexamethasone in intermediate to
long term use, including an increased susceptibility to
infections, proximal myopathy, impaired glucose tolerance,
hypertension and osteoporosis.
Duloxetine Serotonin and Extensively Less than 1% excreted Normal interval dosing Commencing dose 30mg daily. See Not dialysed Unlikely to be Not dialysed "Reduced starting dose in CKD (30mg daily) with a maximum
noradrenaline metabolised into unchanged in the (daily), but reduced dose. Other Comments section. dialysed dose of 60mg per day. Some sources …Contraindicated in
reuptake inhibitor inactive urine. uncontrolled HT due to the potential risk of hypertensive crisis
(SNRI). Painful metabolites. (The Renal Drug Handbook.) "Reduced starting dose in CKD
peripheral (30mg) with a maximum dose of 60mg per day. Some sources
neuropathy; anti- recommend avoiding in patients with a Cr/Cl of < 30 ml/minute.
depressant. Others suggest start at a very low dose and increase according
to response, with a maximum dose of 30mg daily." (Davison &
Knocicki et al, 2014).
Note: Non-steriodals not recommended in renal failure 1
Waiver: All efforts have been made to ensure the accuracy of these guidelines. The best information available has been used. Readers should exercise clinical judgement in the use of all medications. The authors of this guideline do not accept responsibility for its use in practice.
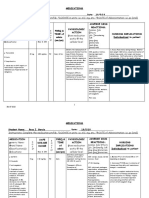
DRUG Action in end of METABOLITES ELIMINATION Dose/interval change in Adult Dose with Renal Failure Dose/interval HF HD NEPHRO OTHER COMMENTS
life care (A=active, (D=drug, renal failure change in renal TOXIC?
I=inactive) M=metabolites) GFR replacement Rx (Y/N)
PD
Fentanyl (Durogesic) Opioid Norfentalyl (I) D – 9% faecal 20-50 - normal dose Minimal commencing dose - Not dialysed Not dialysed Not dialysed No "Inactive metabolites. Most pharmacokinetic studies in CKD
patch D,M - 75% renal 10-20 - 75% normal dose 12mcg/hour patch changed every 3 use parenteral rather than transdermal fentanyl. Generally
<10 - 50% dose days. considered safe for use in CKD if monitored carefully". Davison
& Koncicki et al (2014). If converting from other opioids to
transdermal Fentanyl and vice versa be aware of the time
(approximately 16 hours) for the Fentanyl to reach steady state
when commencing a patch and to remain active after the
removal of the patch.
Gabapentin Neuropathic pain Renal (D) eliminated In dialysis patients a Minimum commencing dose - If on dialysis - Probably Dialysed Dialysed Yes Note the efficacy of Gabapentinoids (Gabapentin and
(Neurontin) Uraemic Pruritus unchanged in urine single dose after each 100mg post dialysis. Titrate does by dialysed Pregabalin) in the management of several symptoms
Restless Legs dialysis. In patients on a 100mg increments. experienced by patient with ESKD (uraemic pruritus, Restless
Syndrome conservative pathway with Legs Syndrome and painful peripheral neuropathy). Main side
eGFR < 15 a dose every If on a conservative non-dialysis pathway - effects of gabapentinoids are drowsiness, blurred vision and
second night. (a) If eGFR >50 commence 100mg tds and ataxia. Note the dosing schedule in this chart are more
titrate up by 100mg increments according
conservative than other formularies and guidelines including
to tolerability and response. See 'Other
the Palliative Care Formulary (5th ed, 2014, p 272). Also see
Comments' column.
(b) If eGFR 30-49 commence 100mg nocte
the commentary on Gabapentin dosing on pages 5 and 9 and
– 100mg bd and titrate up by 100mg Table 5 of Davison SN, Koncicki H, Brennan FP. Pain in
increments according to tolerability and Chronic Kidney Disease : A Scoping Review. Seminars in
response. See Other Comments column. Dialysis 2014;27(2): 188-204. Also note that both Gabapentin
(c) If eGFR 15-29 commence 100mg nocte and Pregabalin should be used with caution on patients with
and titrate up by 100mg increments severe congestive cardiac failure.
according to tolerability and response. See The Renal Drugs Handbook (4th ed) recommends giving
Other Comments column. dialysis patients an initial loading dose of Gabapentin 300-
(d) If eGFR < 15 commence 100mg every 400mg.
second night and titrate up by 100mg
increments according to tolerability and
response. See Other Comments column.
Glycopyrrolate Respiratory No data D = 48.5% renal No data 200-400mcg q 2 - 4 hrs sci No data No data No data No Recommended for terminal secretions in renal
(Robinul) secretions remainder unchanged Dose is titrated against effect.
(Terminal) in bile Accumulation possible
Haloperidol Agitation, Hepatic (M) mainly eliminated GFR <10ml/min or Minimal commencing dose - 0.5 mg. Not dialysed Not dialysed. Not dialysed No Elderly should use low doses to avoid extrapyramidal reactions.
(Serenace) confusion, metabolism via bile, faeces and dialysis. Begin with low Typical commencing doses for: Dose as for GFR Dose as for Dose as for GFR In CKD there is an increased CNS sensitivity and risk of
nausea, Hydroxyl- urine end of dose range and * Nausea - 0.5 mg bd <10 eGFR < 10. <10 sedation. Exacerbates Parkinson’s Disease. Can cause fatal
intractable haliperidol (A) titrate according to * Delirium - 1mg bd prolongation in QT interval if given intravenously and in higher
hiccups. response than recommended doses.
Hydromorphone Opioid H-3-G is inactive Renal(D,M) 20-50 Normal dose If opioid naïve typical commencement Unknown so Unknown so Haemodialysis No Much better tolerated than morphine. Start at low doses in
(Dilaudid) as an analgesic Metabolites renally 10-20 Reduce dose dose - 0.5 - 1mg mg q 6 hours orally (or dose as for dose as for reduces plasma CKD. “Pharmacodynamic data have shown less
but can cause excreted but inactive <10 Reduce dose 0.25 - 0.5 mg sci) GFR<10 GFR<10 concentrations of neuroexcitation compared to morphine and a greater than 65
neuroexcitation. Titrate according to pain / dyspnea. hydromorphone % reduction in pain over dosing intervals with no clinically
by about one half. significant opioid toxicity when given in low doses and
Dialysis removes monitored carefully [Davison & Koncicki et al (2014)]. Koncicki
40-55 % of the et al, 2015 concluded that "Given the changes in
pre-dialysis levels pharmacokinetics in ESRD, titration should start at low doses,
of the metabolite, with an increased dosing interval and with close monitoring for
hydromorphone-3- side effects." Note that Murtagh, 2015 expressed a more
glucuronide. cautious approach:
"It may be reasonable, given the available evidence, to use
hydromorphone carefully in mild or even moderate renal
impairment, provided doses are reduced and the dose interval
increased, and with careful monitoring and titration. In severe
renal impairment, its use
cannot be recommended however, until there is more evidence
available."
If converting from other opioids to hydromorphone and vice
versa consult opioid conversion charts or the Pain or Palliative
Care team.
Hyoscine Colicky pain, Unknown D - 50% renal Normal dose Typical commencement dose 20mg tds - Dialysed – No data Dialysed – No May be used to manage terminal secretions in patients with
Butylbromide terminal excretion qid po/sci. Maximum daily dose - dose as for dose as for GFR< CKD. No dose adjustment required.
(Buscopan) secretions, 240mg. GFR< 15mls/min 15mls/min
malignant bowel
obstruction
Hyoscine Inhibit Excessive Apohyoscine Excreted in urine, eGFR > 15 Normal dose Not recommended in the Terminal Dialysable Dialysed Dialysable No Anticholinergic - Can cause urinary retention
Hydrobromide Secretions metabolised in liver eGFR < 15 - Not Phase with ESRD Normal dose Normal dose Not recommended in the terminal phase. Uraemia causes
(s/c only 3.4% D recommended in ESKD increased permeability of the blood brain barrier to
excreted in urine in 72 (crosses blood/brain centrally acting agents. This may result in Hyoscine
hrs) barrier) hydrobromide causing paradoxical agitation. (Douglas C,
Murtagh FEM et al. Palliative Medicine 2009;23:103-110).
Note: Non-steriodals not recommended in renal failure 2
Waiver: All efforts have been made to ensure the accuracy of these guidelines. The best information available has been used. Readers should exercise clinical judgement in the use of all medications. The authors of this guideline do not accept responsibility for its use in practice.
DRUG Action in end of METABOLITES ELIMINATION Dose/interval change in Adult Dose with Renal Failure Dose/interval HF HD NEPHRO OTHER COMMENTS
life care (A=active, (D=drug, renal failure change in renal TOXIC?
I=inactive) M=metabolites) GFR replacement Rx (Y/N)
PD
Ketamine Neuropathic pain Nor-ketamine (A) About 90 % of a No change Best be used under the supervision of Unlikely to be Unknown Unknown No NMDA Receptor antagonist. Dose as per normal renal function.
dehydronor- parenteral dose of the Pain or Palliative Care teams. dialysed dialysability dose Can cause profound psychomimetic effects. To prevent
ketamine ketamine is excreted in Usual practice is to give a test dose of as for normal psychomimetic side effects best to prescribe a regular dose of
(I) the urine, mostly as 10mg sci. Monitor for any dose as for renal Haloperidol (0.5-1mg bd) concurrently. Contraindicated in
conjugates of psychomimetic effects. After two hours, normal function patients with severe hypertension and patients prone to
hydroxylated if tolerated, commence 100mg sci in a renal function psychosis.
metabolites. Less than syringe driver over 24 hours and titrate
5 % is excreted up by 100mg/ day according to efficacy
unchanged via the and side effects.
faeces and urine.
Levomepromazine Restlessness, a) sulphoxide Majority excreted in GFR 10-50 - No change Minimal dose - 6.25 mg. Typical No data No data No data Start cautiously and at low doses, and titrated according to
(Nozinam) confusion, metabolite urine as M GFR <10 ml/min - start commencement dose - 6.25 mg bd sci. response and side effects (Yorkshire Group 2006, p.8)
agitation, nausea b) glucuronides D- small amount with small dose. Doses are best adjusted according to Can be added after Midazolam for terminal agitation if
excreted unchanged in symptoms. symptoms persist (Douglas et al 2009, p.106). Increased CNS
urine and faeces sensitivity in CKD. More likely to cause sedation.
Lignocaine Difficult to Active metabolites No change Should be used under the supervision of Unlikely No data Not dialysed No Caution in prolonged infusion in renal failure-dose modification
manage accumulate the Pain or Palliative Care teams. if adverse effects. The Renal Drug Handbook (4th ed), p 558
Neuropathic pain during prolonged
infusions
Lorazepam (Ativan) Breathlessness, 70-75 % as Renal (88%) The rest GFR <10ml/min or 0.5-1mg bd-tds (sublingual or po) Unlikely to be Unknown Not dialysed No Increased CNS sensitivity in patients with CKD.
anxiety inactive is eliminated in faeces dialysis. Begin with low dialysed
glucuronide and bile. end of dose range and
metabolites. titrate according to
response
Methadone Pain (I) 2-ethylidine-1, Primarily excreted in eGFR 10-50 Normal Should be used under the supervision of Not dialysed Dialysed Not dialysed No “Primarily excreted in the faeces. Plasma concentrations are
Intractable cough 5-dimethyl- , 3- the feces. dose the Pain or Palliative Care teams. Dose as for GFR Dose as for GFR similar in CKD compared to those with normal renal function.
diphenylpyrrolidin eGFR <10 50-75% of Only recommended to be used by <10 <10 Generally considered safe to uses in CKD if monitored
e, 2-ethyl-3, 3- normal dose. (Aronoff et knowledgeable physicians (Mid-Atlantic carefully.” (Davison & Koncicki, 2014). “Risk of QT interval
diphenyl-5- al. Drug Prescribing in Renal Coalition and the Kidney End-of- prolongation especially with high doses and concomitant risk
methylpyrrolidine Renal Failure, 5th ed) Life Coalition. Clinical Algorithms to factors.” (The Renal Drug Handbook, (4th ed).
(liver) Treat Pain in Dialysis Patients. 2009.)
Both metabolites
are inactive. If eGFR 10-50 – Normal dose. If eGFR
is < 10 50-75 % of normal dose.
There are several recommended dosing
schedules. Given its metabolism - high
oral bioavailability and accumulation
with repeated dosing - it requires care
and clinical experience to use safely. If
converting from another opioid the
commencement dose is calculated
according to the current background
opioid dose. Accordingly a
commencement dose should be
individualised.
Metoclopramide Nausea, Early Metabolised in the Predominantly renal Dose as in normal renal Minimal dose 5 - 10 mg. Not dialysed Dialysed Dialysed No For GFR <20, start at low doses.
(Maxolon) satiety, Hiccups. liver. Conjugated (D,M) function. Typical commencement dose - Dose as for GFR Increased risk of extrapyramidal reactions in severe renal
metabolites are 5-10mg tds half an hour prior to meals <10 impairment. The risk of extrapyramidal side effects is dose-
inactive. related.
Midazolam Terminal agitation Alpha- Renal (D,M) 45-57% GFR 10-50 Normal dose Typical commencement dose Unlikely to be Unlikely to be Unlikely to be No Increased CNS sensitivity in CKD causing sedation. Dose
(Hypnovel) hydroxymidazola <1% as unchanged GFR <10 50% of normal 2.5 mg - 5 mg q 4 hours. Titrate dose dialysed dialysed dialysed reduction and an increased dosing interval for midazolam
m glucuronide is drug dose according to symptoms. Dose as for GFR Dose as for Dose as for GFR recommended (Douglas et al 2009, p.106)
an active <10 GFR <10 <10
metabolite and
accumulates in
ESKD.
Morphine Pain control, M3G (I) M6G (A) Renal (D,M) Not recommended in Not recommended in CKD. Not dialysed Not dialysed Morphine and its No "Rapid accumulation of active metabolites in CKD resulting in
breathlessness CKD metabolites are clinically significant opioid toxicity including sedation, confusion,
dialysed. myoclonus, and respiratory depression. Not recommended in
CKD." (Davison & Koncicki 2014)
Octreotide Malignant bowel Extensive hepatic Renal (32% Normal dose Commence with 150 mcg tds sci. Unknown Dialysed Normal dose No “In renal failure requiring dialysis… reduced elimination … may
obstruction metabolism. unchanged) Consider introducing a syringe driver Dialysed: plasma necessitate a dose reduction.” Palliative Care Formulary, 5th
over 24 hours. Maximum dose 1500 clearance ed, 2014, p 532. Potentially hazardous interaction with
mcg over 24 hours increased by cyclosporine.
around 30%.
Supplemental
dosing may be
required
Note: Non-steriodals not recommended in renal failure 3
Waiver: All efforts have been made to ensure the accuracy of these guidelines. The best information available has been used. Readers should exercise clinical judgement in the use of all medications. The authors of this guideline do not accept responsibility for its use in practice.
DRUG Action in end of METABOLITES ELIMINATION Dose/interval change in Adult Dose with Renal Failure Dose/interval HF HD NEPHRO OTHER COMMENTS
life care (A=active, (D=drug, renal failure change in renal TOXIC?
I=inactive) M=metabolites) GFR replacement Rx (Y/N)
PD
Olanzapine Management of Extensively Elimination of Plasma half-life is In CKD initial dose - 5mg daily. Not dialysed Unknown Not dialysed No Olanzapine has potentially hazardous interactions with many
delirium metabolised in the metabolites – renal (60 unchanged in CKD. dialysability classes of medications. See The Renal Drug Handbook.
liver. Major %); faecal (30 %).
metabolites are
olanzapine 10-N-
glucuronide and 4’-
N-
desmethylolanzap
ine. Metabolites
“appear to be
inactive”. (The
Renal Drug
Handbook)
Ondansetron (Zofran) Pruritus Multiple Renal Normal dose Commence 4mg prn, maximum tds. Unlikely to be Unknown Not dialysed No Ondansetron is very constipating. Consider an alternative anti-
Nausea metabolites (I) <5% unchanged in Regular dose – 4-8mg bd. dialysed emetic. Best reserved for nausea secondary to chemotherapy
urine and/or radiotherapy. Can cause a dose- dependent QT
Hepatic prolongation. Note – a systematic review found that
Ondansetron was not efficacious in the management of
uraemic pruritus. (To TH et al. J Pain Symptom Management
2012;44(5): 725-730).
Oxycodone Pain - strong Noroxycodone (A) Renal (D 19%,M 65%) In CKD oxycodone and its Endone - minimal dose 2.5mg. Unknown Dialysed Unknown No The authorities express differing views. The Palliative Care
(Endone, Oxycontin, Opioid Oxymorphone (A) Faecal (D,M) metabolites accumulate. Typical commencement doses - 2.5 mg dialysability dialysability Formulary, 5th ed, 2014 at p. 443 states that “Oxycodone is
Oxynorm) If eGFR 15-50 give 75 % tds-qid. contraindicated in renal failure and is not recommended in
of normal dose. If eGFR Oxycontin - minimal dose 5mg severe renal impairment.” A different view is expressed by two
< 15 give 50 % of normal Typical commencement dose - 5 mg bd other authorities. Davison & Koncicki, 2014 state : “There are
dose. (The Renal Drug case reports of toxicity in association with CKD yet overall
Handbook, 4th ed, 2014) consensus from the literature is that oxycodone is reasonably
safe to use in CKD if monitored carefully.” The Renal Drug
Handbook, 4th ed, 2014 recommends commencing with a
reduced dose and gradually increasing according to response.
Paracetamol Simple pain relief. Metabolised in the Renal elimination of Normal dosing interval Typical dose 1g Q6H Not dialysed Dialysed Dialysed Yes in Note is dialysed by HD but not by PD.
Antipyretic. liver. More than 80 parent drug and (q6hrly) overdose Normal doses may be used in patients with CKD.
% is metabolised metabolites.
by conjugation to Note : The editors of The Renal Drug Handbook. 4th ed, 2014
paracetamol recommend a maximum dose of 5g/day in smaller patients with
glucuronide and CKD stage 5.
paracetamol
sulphate, 10 % is
metabolised by
oxidation to N-
acetyl-p-
benzoquinoneimin
e (NAPQI) and 5
% is not
metabolised and
excreted
unchanged in the
urine.
Pregabalin (Lyrica) Neuropathic pain Undergoes Renally excreted as an With normal renal If on dialysis – commence 25 mg daily and Dialysed Dialysed 50% removal No Note the efficacy of Gabapentinoids (Gabapentin and
Uraemic Pruritus negligible unchanged drug function the dose titrate according to tolerability and after 4 hours of Pregabalin) in the management of several symptoms
Restless Legs metabolism schedule is bd response. (The Renal Drug Handbook, 4th HD experienced by patient with ESKD (uraemic pruritus, Restless
Syndrome ed). MIMS recommends giving an extra Legs Syndrome and painful peripheral neuropathy). Main side
With CKD need to adjust 25mg after each dialysis. effects of gabapentinoids are drowsiness, blurred vision and
dose – see next column. ataxia. Note the dosing schedule in these guidelines are more
If on a conservative pathway –
conservative than other formularies and guidelines including
(a) If eGFR 30-60 – commence 75 mg daily
the Palliative Care Formulary, 5th ed, 2014. Also see the
and titrate according to tolerability and
commentary on Gabapentin dosing on pages 5 and 9 and
response.
(b) If eGFR 15-29 – commence 25-50mg Table 5 of Davison SN, Koncicki H, Brennan FP. Pain in
daily and titrate according to tolerability Chronic Kidney Disease : A Scoping Review. Seminars in
and response. Dialysis 2014;27(2): 188-204. Also note that both Gabapentin
(c) If eGFR <15 – commence 25mg daily and Pregabalin should be used with caution on patients with
and titrate according to tolerability and severe congestive cardiac failure.
response. (The Renal Drug Handbook, 3rd
ed)
Risperidone Management of Metabolised in the Elimination is mainly In ESKD the clearance of The Palliative Care Formulary Unlikely to be Dialysed Dialysed No Can cause postural hypotension, deterioration in Parkinson’s
delirium liver. Major urine, some faecally. parent drug and recommends, in normal renal function, a dialysed Disease and, in the case of epilepsy, lowering of the seizure
metabolite is 9- metabolites is deceased starting dose in delirium of 1mg nocte and threshold. Risperidone has potentially hazardous interactions
hydroxy- by 60 %. prn. In the context of CKD, The Renal Drug with many classes of medications. See The Renal Drug
risperidone. Handbook recommends commencing with Handbook.
50 % of the normal dose and slowly
titrating up ie. commence with 0.5mg nocte
and prn.
Sertraline SSRI medication. Extensively “Can be used in renal failure at normal Unlikely to be No data Not dialysed Multiple drug interactions. See The Renal Drug Handbook (4th
Uraemic Pruritus, metabolised in the doses with caution.” The Renal Drug dialysed. ed), p 665.
antidepressant liver. Handbook (4th ed)
Note: Non-steriodals not recommended in renal failure 4
Waiver: All efforts have been made to ensure the accuracy of these guidelines. The best information available has been used. Readers should exercise clinical judgement in the use of all medications. The authors of this guideline do not accept responsibility for its use in practice.
DRUG Action in end of METABOLITES ELIMINATION Dose/interval change in Adult Dose with Renal Failure Dose/interval HF HD NEPHRO OTHER COMMENTS
life care (A=active, (D=drug, renal failure change in renal TOXIC?
I=inactive) M=metabolites) GFR replacement Rx (Y/N)
PD
Sodium Valproate Epilepsy. Extensively Liver (D) eGFR <10ml/min Normal Commence - 200mg bd Unknown Dialysed Not dialysed No Alter doses according to free serum levels
(Epilim) Neuropathic pain metabolised in the 5% excreted dose tapered to minimum dialysability Normal dose Increased CNS sensitivity in CKD, including greater risk of
liver, up to 60 % unchanged in urine effective dose (and blood Normal dose sedation. Palliative Care Formulary, 5th ed, 2014, at p 280
by conc) recommends “lower initial doses and slower titration may be
glucuronidation. required in renal impairment.”.
The glucuronide
metabolites are
inactive.
Tapendatol Analgesic. Has a Approximately 97 Mostly renally excreted If eGFR > 15 – normal If eGFR > 15 – normal dose; if eGFR < Probably Probably Probably No Not recommended due to limited information regarding use in
dual action – mu % of the parent in the glucuronide dose. If eGFR < 15 – not 15 – not recommended. dialysed. dialysed. dialysed. severe renal insufficiency. (Koncicki & Brennan et al, 2015).
receptor agonist drug is form. 3% is excreted recommended. The editors of The Renal Drug Handbook (4th ed) state : “Not
and noradrenaline metabolised in the unchanged in the recommended by manufacturer in severe renal impairment
re-uptake liver to inactive urine. due to lack of studies.”
inhibitor. glucuronides.
Tramadol (Tramal) Analgesia. Weak O-desmethyl- Renal (D,M) 90% If eGFR < 30 reduce If on dialysis commence 50mg bd; Unknown Dialysed Slowly dialysed No Note that the authorities recommend differing dosing regimens.
opioid; also acts tramadol Faecal(D) 10%. In dose frequency from qid maximum 100bd. dialysability Davison & Koncicki, 2014, Davison, Chambers, Ferro et al,
to enhance the (A) CKD there is a two-fold to bd. 2010, King et al, 2011, Murtagh, 2015 and the Palliative Care
inhibitory pathway. N-desmethyl- increase in the If on a conservative pathway : Formulary, 5th ed, 2014 recommend a bd dosing schedule.
tramadol elimination half-life (a) If eGFR >30 – dose as in normal The Renal Drug Handbook, 4th ed, 2014 recommends a tds
(A) renal function. dosing regimen. The extended release formulation of
(b) If eGFR 15-30 – commence 50mg Tramadol is not recommended if the Cr/Cl is < 30mls/min.
bd; maximum 100mg bd Note: uraemia lowers the seizure threshold and Tramadol may
(c) If eGFR <15 – 50mg bd (maximum). be epileptogenic in ESKD patients.
Thalidomide Uraemic Pruritus Metabolised Unlikely to be Not dialysed Unlikely to be No "Major route of elimination is non-renal therefore normal doses
resistant to other almost exclusively dialysed dialysed may be given in renal failure.” (The Renal Drug Handbook, 4th
medications. Also by non-enzymatic ed, 2014).
used in the hydrolysis. May cause unexplained hyperkalaemia. May cause peripheral
management of neuropathy. Use with caution with other medications that may
Multiple Myeloma cause peripheral neuropathy.
in certain clinical
situations.
Tranexamic acid Haemostatic None Excreted mainly eGFR < 30, once daily If eGFR is 15-30 – 15 mg/kg once daily. Unknown Unknown Unknown No Contraindicated if history of DVT/Pulmonary Emboli. One UK
agent. unchanged in the dosing. If eGFR is < 15 – not recommended. dialysability dialysability dialysability manufacturer recommends against its use in ESKD due to
urine. See Other Comments column. Dose as for GFR Dose as for Dose as for GFR accumulation and increased risk of thrombus formation.
<10 GFR <10 <10
Bibliography
Ashley C, Dunleavy A (eds). The Renal Drug Handbook. 4th ed, 2014, Radcliffe Publishing, Oxford.
Broadbent, A. Khor, K. Heaney, A. 2003. Palliation and Chronic Renal Failure: Opioid and Other Palliative Medications - Dosage Guidelines. 2003. Progress in Palliative Care 11(4), pp 183-190
Brown E et al (eds) End of Life Care in Nephrology. 2007, p.99.
Cervelli, M. The Renal Drug Reference Guide, 1st edition, 2007. Nexus Printing, Adelaide
Chambers, J. Brown, E. Germain, M. 2005. Supportive Care for the Renal Patient. Oxford University Press, UK
Chambers, J. Brown, E. Germain, M. eds 2010. Supportive Care for the Renal Patient, 2nd edition. Oxford University Press, UK
Davison S. Chambers, EJ. Ferro, CJ. Management of pain in renal failure. Chambers, J. Brown, E. Germain, M. eds 2010. Supportive Care for the Renal Patient, 2nd edition. Oxford University Press, UK
Davison S, Ferro CJ. Management of Pain in CKD. Progress in Palliative Care 2009; 17:186-195.
Davison SN, Koncicki H, Brennan FP. Pain in Chronic Kidney Disease : A Scoping Review. Seminars in Dialysis 2014;27(2): 188-204.
Department of Health. Renal NSF Team and Marie Curie Palliative Care Institute. National LCP Renal Steering Group. 2008. Guidelines for LCP Prescribing in Advanced Chronic Kidney Disease. Downloaded 4.5.09 http://www.mcpcil.org.uk/files/NationalLCPRenalsymptomcontrolguidelinesJuneprintablepdf_0.pdf
Douglas, C. Murtagh, F. Chambers, E. Howse, M. & Ellershaw, J. 2009. Symptom management for the adult patient dying with advanced chronic kidney disease: A review of the literature and development of evidence-based guidelines by a United Kingdom Expert Consensus Group. Palliative Medicine, 23, pp 103-110
Edwards, A, Yorkshire Palliative Medicine Guidelines Group. 2006. Clinical Guidelines for the use of Palliative Care Drugs in Renal Failure.
Johnson, C. 2009, Dialysis of Drugs 2009 , CKD Insights USA and Amgen Australia Pty Ltd.
King S, Forbes K, Hanks GW et al. A systematic review of the use of opioid medication for those with moderate to severe cancer pain and renal impairment : A European Palliative Care Research Collaborative opioid guidelines project. Palliative Medicine 2011; 25(5): 525-552.
Koncicki, H, Brennan F, Vinen K, Davison SN. An Approach to Pain Management in ESKD : considerations for General Management and Intradialytic Symptoms. Sem Dial 2015, Epub April 2015.
Mid-Atlantic Renal Coalition (MARC) and the Kidney End-of-Life Coalition. Clinical Algorithms to Treat Pain in Dialysis Patients . 2009
Murtagh, FEM. End-stage kidney disease. In; Cherney, NI et al. (Eds) Oxford textbook of Palliative Medicine, 5th Edition, 2015, OUP, Oxford, PP1004-1012.
Twycross R, Wilcock A, Howard P (eds) Palliative Care Formulary , 5th ed, Palliativedrugs.com, Nottingham, 2014.
Note: Non-steriodals not recommended in renal failure 5
You might also like
- Clinical Research Organization / Contract Research OrganizationDocument34 pagesClinical Research Organization / Contract Research OrganizationPHARMAIGNITENo ratings yet
- Clinical Teaching Plan Level IV First SemesterDocument12 pagesClinical Teaching Plan Level IV First SemesterMevelle Laranjo Asuncion67% (3)
- Nursing Irs Group Oet Writing Practice Test BookDocument56 pagesNursing Irs Group Oet Writing Practice Test BookMilad RostamiNo ratings yet
- Lisinopril Drug StudyDocument2 pagesLisinopril Drug StudyKristinelou Marie Reyna100% (1)
- Drug Study Omeprazole CompressDocument2 pagesDrug Study Omeprazole CompressAngelica TolledoNo ratings yet
- HospitalDocument32 pagesHospitalKaushiki Kamboj100% (1)
- Amlodipine Drug StudyDocument2 pagesAmlodipine Drug StudyAbigail Basco100% (3)
- Nifedipine Drug StudyDocument3 pagesNifedipine Drug StudyCrystal Queen MarquezNo ratings yet
- PPD's Better Pharmacy Drug Hand Book 9 Edition 2009: Marquez, Crystal Queen CDocument1 pagePPD's Better Pharmacy Drug Hand Book 9 Edition 2009: Marquez, Crystal Queen CCrystal Queen MarquezNo ratings yet
- Drug-Study OmeprazoleDocument1 pageDrug-Study OmeprazoleBeverly Datu71% (7)
- Saurashtra ListDocument200 pagesSaurashtra Listvadoliya umeshNo ratings yet
- Micardis PlusDocument2 pagesMicardis PlusKristine YoungNo ratings yet
- Generic Name:: Drug Mechanism of Action Indication Contraindication Side Effects Nursing ResponsibilitiesDocument3 pagesGeneric Name:: Drug Mechanism of Action Indication Contraindication Side Effects Nursing ResponsibilitiesALIANA KIMBERLY MALQUESTONo ratings yet
- Clonidine Trimetazidine Drug StudyDocument4 pagesClonidine Trimetazidine Drug StudyLanzen DragneelNo ratings yet
- The Final Act 1Document21 pagesThe Final Act 1yoyo1rnNo ratings yet
- Durg Profile 6396Document7 pagesDurg Profile 6396MUHAMMAD ZOHAIBNo ratings yet
- PharmacoDocument28 pagesPharmacoCy RilNo ratings yet
- CHN - Drug StudyDocument6 pagesCHN - Drug Studyjmcalvelo.518No ratings yet
- Dopamine Antagonist: Generic Name: Chemical EffectDocument2 pagesDopamine Antagonist: Generic Name: Chemical EffectMajeed AlzahraniNo ratings yet
- Fluphenazine Drug Study - DoxDocument3 pagesFluphenazine Drug Study - Doxan naNo ratings yet
- Drugstudy AnesthesiaDocument5 pagesDrugstudy AnesthesiaElisha Fleur Cambas GachoNo ratings yet
- Drug Study (First Meet - RLE)Document5 pagesDrug Study (First Meet - RLE)Pauline AñesNo ratings yet
- H2 Receptor Antagonists and LidocaineDocument14 pagesH2 Receptor Antagonists and LidocaineJoharaNo ratings yet
- Drug Study 2023 1Document17 pagesDrug Study 2023 1Precious PanganibanNo ratings yet
- DRUG STUDY FOR HYPOKALEMIA Case Study 3Document11 pagesDRUG STUDY FOR HYPOKALEMIA Case Study 3Montero, Ma. Cecilia - BSN 3-BNo ratings yet
- Drug StudyDocument1 pageDrug StudyZia CaldozaNo ratings yet
- Patient NameDocument4 pagesPatient NameCatherine MetraNo ratings yet
- Drug StudyDocument1 pageDrug StudyZia CaldozaNo ratings yet
- Mfe, Ferrous Sulfate, Calcium Drug StudyDocument3 pagesMfe, Ferrous Sulfate, Calcium Drug StudyMary Shane MoraldeNo ratings yet
- ClonidineDocument1 pageClonidineYuuki Chitose (tai-kun)No ratings yet
- Drug Study (Acetaminophen)Document1 pageDrug Study (Acetaminophen)Kian HerreraNo ratings yet
- Drug-Study 2eDocument10 pagesDrug-Study 2eaijelethdaldeavilaNo ratings yet
- Drug Name Dosage, Route, Frequency Mechanis MOF Action Indications Contraindication S Adverse Effects Nursing ResponsibilitiesDocument4 pagesDrug Name Dosage, Route, Frequency Mechanis MOF Action Indications Contraindication S Adverse Effects Nursing ResponsibilitiesJonna Mae TurquezaNo ratings yet
- Drug Studyyy 57-59Document3 pagesDrug Studyyy 57-59Real TetisoraNo ratings yet
- Tramadol, Paracetamol, Calmoseptine, B12Document5 pagesTramadol, Paracetamol, Calmoseptine, B12Denise EspinosaNo ratings yet
- Drug Study Kathleen Claire ColinioDocument11 pagesDrug Study Kathleen Claire ColinioKathleen ColinioNo ratings yet
- Drug StudyDocument2 pagesDrug StudyAlyssa Marie PepitoNo ratings yet
- Drug Study: Atropine: RecommendedDocument6 pagesDrug Study: Atropine: RecommendedShara Lailanie A. AzisNo ratings yet
- Drug Study - Colon CancerDocument4 pagesDrug Study - Colon Cancerbea pegadNo ratings yet
- Gantala Drug Stusy-TabhsoDocument8 pagesGantala Drug Stusy-TabhsoHey it's FerdyNo ratings yet
- KETOROLACDocument1 pageKETOROLACJugen Gumba Fuentes AlquizarNo ratings yet
- Drug Study Furosemide and MidazolamDocument2 pagesDrug Study Furosemide and MidazolamCuttie Anne GalangNo ratings yet
- Instructions: Complete The Medication Profile. DOSAGE in Units: I.E. ML/, MG, Etc. ROUTE of Administration: I.E. Po (Oral)Document12 pagesInstructions: Complete The Medication Profile. DOSAGE in Units: I.E. ML/, MG, Etc. ROUTE of Administration: I.E. Po (Oral)Rosa Garcia100% (1)
- Drug Study - AlfuzosinDocument1 pageDrug Study - AlfuzosinKian HerreraNo ratings yet
- Drug Study For Losartan PotassiumDocument2 pagesDrug Study For Losartan PotassiumChryst Louise SaavedraNo ratings yet
- Generic/ Brandname Indication Classification Dosage/Freq./ Route Side Effects Nursing ConsiderationDocument4 pagesGeneric/ Brandname Indication Classification Dosage/Freq./ Route Side Effects Nursing Considerationgayeng04No ratings yet
- MedicationDocument4 pagesMedicationkayalNo ratings yet
- Paracetamol DrugstudyDocument1 pageParacetamol DrugstudyMsOrangeNo ratings yet
- FerroussulfatedsDocument2 pagesFerroussulfatedsDayanaj OngNo ratings yet
- Drug Study: Sedation, Dizziness/vertigo, Headache, Hypotension Sweating, Nausea, VomitingDocument1 pageDrug Study: Sedation, Dizziness/vertigo, Headache, Hypotension Sweating, Nausea, VomitingRoland YusteNo ratings yet
- 204DS Mod1Document2 pages204DS Mod1Aally ChandraNo ratings yet
- Medication Class Mechanism of Action Dosage Range Side Effects Nursing Implications/ Teaching Generic NameDocument19 pagesMedication Class Mechanism of Action Dosage Range Side Effects Nursing Implications/ Teaching Generic NameindyaphdNo ratings yet
- Drug StudyDocument6 pagesDrug StudyLovelyNo ratings yet
- Drug StudyDocument3 pagesDrug StudyAlyssa Marie PepitoNo ratings yet
- Drug Study: Drug Indication Action Contraindication Adverse Effect Nursing Consideration Generic Name: Omeprazole 40mgDocument9 pagesDrug Study: Drug Indication Action Contraindication Adverse Effect Nursing Consideration Generic Name: Omeprazole 40mgNica SalazarNo ratings yet
- Generic:: Drug Study #1Document1 pageGeneric:: Drug Study #1Patricia Jean FaeldoneaNo ratings yet
- Tramadol Plus ParacetamolDocument2 pagesTramadol Plus ParacetamolKeir Mrls ForcadillaNo ratings yet
- Peripherally Acting Anti-Adrenergics: Generic Name: Losartan Potassium Brand Name: CozaarDocument4 pagesPeripherally Acting Anti-Adrenergics: Generic Name: Losartan Potassium Brand Name: Cozaarbea pegadNo ratings yet
- Drug Shit ShemDocument28 pagesDrug Shit ShemJoselo YasayNo ratings yet
- Drug Study ICUDocument2 pagesDrug Study ICUErryl Justine AdvinculaNo ratings yet
- Drugstudy PharmaDocument4 pagesDrugstudy PharmaKyla FerriolsNo ratings yet
- Drug Study Ranitidine TramadolDocument11 pagesDrug Study Ranitidine Tramadolaaron tabernaNo ratings yet
- Medication Action Indications Contraindications Side Effects Nursing ConsiderationsDocument6 pagesMedication Action Indications Contraindications Side Effects Nursing ConsiderationsAnne CamilleNo ratings yet
- DRUG NAME DepressionDocument3 pagesDRUG NAME DepressionLord Allen B. GomezNo ratings yet
- Draft Resolution 1.0Document3 pagesDraft Resolution 1.0Just A BoyNo ratings yet
- English Language Proficiency Requirements For Overseas Nurses and MidwivesDocument3 pagesEnglish Language Proficiency Requirements For Overseas Nurses and MidwivesFrae NavarroNo ratings yet
- Pharma 5Document4 pagesPharma 5Ночной волкNo ratings yet
- NCM 107 Day 2Document52 pagesNCM 107 Day 2joanaalpayNo ratings yet
- Dr. Archya Sengupta: ContactDocument2 pagesDr. Archya Sengupta: ContactJenefer AntoNo ratings yet
- Band and Pontic: A Modified Band and Loop Space Maintainer - Clinical InnovationDocument3 pagesBand and Pontic: A Modified Band and Loop Space Maintainer - Clinical InnovationIJAR JOURNALNo ratings yet
- Five Principles To Practice (And Live) By: Ethics SeminarDocument20 pagesFive Principles To Practice (And Live) By: Ethics SeminarindydentalsocietyNo ratings yet
- Is The Smile Line A Valid Parameter For Esthetic Evaluation A Systematic Literature ReviewDocument14 pagesIs The Smile Line A Valid Parameter For Esthetic Evaluation A Systematic Literature Reviewmaroun ghalebNo ratings yet
- Core Standards For Handling Medicines in Community Teams - Version 4 - April 17Document11 pagesCore Standards For Handling Medicines in Community Teams - Version 4 - April 17Liza GomezNo ratings yet
- Tbi PathophysiologyDocument10 pagesTbi PathophysiologysampathNo ratings yet
- Antedate Letter To PLDTDocument2 pagesAntedate Letter To PLDTR. REYESNo ratings yet
- General Nursing and MidwiferyDocument4 pagesGeneral Nursing and MidwiferyBALAJI INSTITUTENo ratings yet
- Covid VaccinatedDocument1 pageCovid Vaccinatedhlwan naingNo ratings yet
- Dr. Umashankar R: 22 Years Experience Overall (19 Years As Specialist)Document10 pagesDr. Umashankar R: 22 Years Experience Overall (19 Years As Specialist)Venkatesha SNo ratings yet
- Rps - Professional Standards For Hospital Pharmacy PDFDocument33 pagesRps - Professional Standards For Hospital Pharmacy PDFDrAmit VermaNo ratings yet
- Internal Medicine A Guide To Clinical Therapeutics by Rebecca L Attridge Monica L Miller Rebecca Moote Laurajo Ryan 0071745807Document5 pagesInternal Medicine A Guide To Clinical Therapeutics by Rebecca L Attridge Monica L Miller Rebecca Moote Laurajo Ryan 0071745807Hesbon MomanyiNo ratings yet
- Case #4 Clinical Decision Making IiDocument1 pageCase #4 Clinical Decision Making IiJoslin Roz GalileaNo ratings yet
- Annex I National Leprosy Eradication ProgrammeDocument5 pagesAnnex I National Leprosy Eradication ProgrammespmdocNo ratings yet
- Challenges For Psychiatric PatientsDocument11 pagesChallenges For Psychiatric PatientsyolandaNo ratings yet
- Ahrq 2004 PDFDocument74 pagesAhrq 2004 PDFDelly TunggalNo ratings yet
- Hizon Interview Group 2Document3 pagesHizon Interview Group 2Dan HizonNo ratings yet
- Bioethics: Beneficence / Non-MaleficenceDocument35 pagesBioethics: Beneficence / Non-MaleficenceBheru LalNo ratings yet
- Counselli NG in Hiv/Aids: Presented By-Bhawna Joshi Msc. N 2 Tear SNSRDocument30 pagesCounselli NG in Hiv/Aids: Presented By-Bhawna Joshi Msc. N 2 Tear SNSRBhawna JoshiNo ratings yet
- Isaac Munene CV-CDocument4 pagesIsaac Munene CV-CIsaac MuneneNo ratings yet
- Monthly Accomplishment ReportDocument11 pagesMonthly Accomplishment ReportAlexandria P. OrcajadaNo ratings yet