Professional Documents
Culture Documents
HX Journal
Uploaded by
Shiela GutierrezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HX Journal
Uploaded by
Shiela GutierrezCopyright:
Available Formats
TAKING A HISTORY
How to take a complete eye history
Moureen Taking a good history not only helps you to make a diagnosis, it can also help you
Takusewanya
Ophthalmologist: to understand the impact
Mbarara Hospital,
Uganda. of the condition on the
patient and identify any
obstacles to treatment.
I
t is impossible to over-emphasise
the importance of taking a careful
history when assessing an eye
patient. Taking a good history can
ADRIANE OHANESIAN/SIGHTSAVERS
help to focus your examination
and indicate what investigations
are needed. It can also help you
to understand the impact of the
condition on the patient and
pinpoint any difficulties they may
have adhering to treatment. Make careful notes when you take a history. SOUTH SUDAN
This is also your opportunity to focus
on the patient as a person and to form a relationship of Personal and demographic data
trust, respect and mutual understanding. Ask the patient’s personal details:
• Name, for identification, filing and patient follow-up
How to structure history taking
• Address and mobile phone number, for follow-up
To ensure you don’t miss anything important, structure and to identify patients from areas with endemic
your history taking carefully. Ask about: diseases
• Personal and demographic data • Age and gender, for noting
Tip: You can use • Reason for visit or presenting complaint down and ruling out any Recording the age,
this bulleted list as a diseases associated with gender, language
checklist Copy and • History of presenting complaint and disability status
keep it where you • Past eye history different age groups and/or sex
of patients allows
can see it during • General medical history • Language you to monitor who
history taking to
• Family eye history • Disability is, and is not,
help you to stay on
• Medication history • Patient’s occupation, daily tasks coming to your eye
track and ensure clinic or hospital.
that you will not • Allergy history and hobbies.
Compare these
miss anything • Social history Understanding a patient’s figures with the
important. population to
Each of these is discussed in more detail below. occupation, daily tasks (e.g., identify groups that
looking after grandchildren) and are under-
hobbies is helpful for finding represented, e.g.,
Top tips for taking a good history out a patient’s visual needs girls with other
disabilities, and
and understanding any eye
• Introduce yourself to the patient – this creates a friendly environment. manifestations or symptoms as a
plan ways to reach
out to them.
• Respect the patient’s privacy and confidentiality while taking the history result of occupational hazards.
• Ask questions that are direct, simple and clear. Avoid using medical
terms and explain things in ordinary language as much as possible. Reason for visit/Presenting complaint
• Be a good listener. Avoid interrupting or rushing the patient. Show Ask the main reason why the patient has come to seek
them that you are listening and paying attention: make eye contact an eye examination.
as appropriate and ask if you are not sure about something they Record the main presenting symptoms in the patient’s
said. It is often useful to use open questions (e.g., how are you?) and own words and in a chronological order. The four main
closed questions (e.g., yes/no answers) to help focus the discussion. groups of symptoms are:
• Try to see things from the patient’s point of view and make an effort
to understand them and their circumstances, especially when these 1 Red, sore, painful eye or eyes (including injury to
are very different from your own. the eye)
• Be aware that patients who are older, or who have disabilities 2 Decreased distance vision in one or both eyes,
(including hearing impairment, speech difficulties or a learning whether suddenly or gradually
disability) may need a bit more time or may struggle to express 3 A reduced ability to read small print or see near
themselves. This may cause them some anxiety, so remain patient objects after the age of 40 years
and reassure them that you are there to listen. 4 Any other specific eye symptom, such as double
vision, swelling of an eyelid, watering or squint.
44 COMMUNITY EYE HEALTH JOURNAL | VOLUME 32 | NUMBER 107 | 2019
History of presenting complaint Family eye history Figure 1 Case scenarios
This is an elaboration of the presenting complaint It is important to ask the patient whether with different presenting
and provides more detail. The patient should be any other member of the family has a similar complaints
encouraged to explain their complaint in detail condition or another eye disease. This can help
and the person taking history should be a patient to establish familial predisposition of inheritable
listener. While taking a history of the presenting ocular disorders like glaucoma, retinoblastoma
complaint, it is important to have potential diagnoses or congenital eye diseases, diabetes and
in mind. For each complaint, ask about: hypertension.
CLARE GILBERT
• Onset (sudden or gradual) Medication history
• Course (how it has progressed) Ask about present and past medications for
• Duration (how long) both ocular and medical conditions. Don’t A case of age-related
• Severity overlook any medications that the patient may cataract (history of gradual
• Location (involving one or both eyes) have stopped taking some time ago. Some loss of vision)
• Any relevant associated symptoms medications are important in the etiology of
• Any similar problems in the past ocular conditions.
• Previous medical advice and any current
It is also helpful to ask whether the patient has
medication.
been able to use the medication as prescribed
Past eye history (their compliance). If a medication is ineffective,
P. VIJAYALAKSHM
Ask for detail about any previous eye problems you want to know whether the patient is
actually using the medication as prescribed, for
• History of similar eye complaints in the past. example glaucoma medications.
This is important in recurrent conditions such as A case of red eye due to
herpes simplex keratitis, allergic conjunctivitis, Using your own discretion, it is helpful to find bacterial conjunctivitis
uveitis and recurrent corneal erosions out whether access to medication prescribed is
a problem. This helps to ascertain whether cost
• History of similar complaints in the other eye
or other concerns are a potential reason for
is important in bilateral conditions such as
non-compliance. There could also be practical
uveitis, cataract
issues, such as difficulty instilling eyedrops or
MURRAY MCGAVIN
• History of past trauma to the eye may explain forgetting to do so.
occurrence of conditions such as cataract and
retinal detachment Do not forget to ask in a non-judgmental way
about traditional/herbal medication use. A case of ophthalmia
• History of eye surgery. It is important to ask neonatorum (history of
about any ocular surgery in the past such as Allergies
purulent discharge in a
cataract extraction, muscle surgery, glaucoma, or Ask about any allergies to medications or other
newborn)
retinal surgery substances.
• Other symptoms. Ask whether the patient has Social history
any other specific eye symptoms. • Smoking (amount, duration and type)
• Alcohol (amount, duration and type)
General medical history
Ask about any current and past medical conditions. Birth and immunisation history
These include conditions such as diabetes, For children, the birth history (prematurity) and
hypertension, arthiritis, HIV, asthma and eczema. immunisation status can be important.
Letter to When something goes wrong are more difficult to discern. There may be fear that
the editor Thank you so much for your courageous coverage acknowledging inadvertent harm could threaten public
health programmes that deliver substantial benefits.
of medical error in the most recent issue of the
Community
V O L U M E 3 2 • N U M B E R 1 0 6 • 2 0 19
Community Eye Health Journal. Inadvertent harm in Consequently, as described in a recent article (http://
Eye Health Journal
health care settings can be devastating for patients and bit.ly/glob-apol), apology in public health is less often
caregivers alike. Not too long ago, when I was trained the norm. We in public health can be inspired and
in medicine, disclosure of medical error and apology challenged by the progress made by eye health in
Being involved in a
medical error can be
devastating; health
workers will need
the support of senior
colleagues (p. 26).
STOCK IMAGE
When something goes wrong were discouraged because of the potential for lawsuits. acknowledging unintended harm.
in medical care
As health workers, we do everything within our power to ensure that our patients
have the best visual and clinical outcomes possible. What should we do if
something goes wrong?
Such an approach disrespected patients and morally Your remarkable coverage of this topic in the Community
harmed caregivers. It was therefore tremendously
David Yorston
Consultant
H
Ophthalmologist: ealth care is an inherently dangerous activity. We The guidance emphasises that the explanation and apology
Tennent Institute of
Eye Health Journal has done us all a great service.
give people drugs that can be poisonous and use should be delivered by a senior clinician. That person may
Ophthalmology,
Gartnavel Hospital, sharp instruments in their eyes. Sometimes, these not be at fault, but she or he is responsible for the care of
Glasgow, Scotland, activities will have harmful consequences. What should the patient. A more senior health worker may also be more
UK. we do when someone comes to harm as a result of likely to have the knowledge and experience needed in
something we have, or have not, done? order to answer the patient’s questions.
encouraging to learn that, at least in clinical eye care,
The UK’s General Medical Council – the body that sets If the apology and explanation is to be delivered by a
ethical standards for doctors in the UK – provides senior clinician, the more junior member of the team has
guidance1 that emphasises the duty of candour: the duty to inform her or his senior colleague aobut the
Indeed, this issue can serve as a model for other fields
the duty to be open and truthful with our patients. error. This can be an uncomfortable moment; therefore,
If something goes wrong, we have to tell our patients, senior staff have a duty to encourage a culture of
give them a full explanation, and apologise. reporting errors without fear of retribution.
Continues overleaf ➤
disclosure of error and apology are being practiced in
COMMUNITY EYE HEALTH JOURNAL | VOLUME 32 | NUMBER 106 | 2019 21
within health care and across global health. Thank
hospitals and clinics around the world. A recent account you for so positively advancing the conversation, with
in the Huffington Post by a gynaecologist (http://bit. extraordinary clarity and forthrightness.
ly/Huff-apology) complements your reporting and
highlights the positive impact of disclosing medical error. David Addiss
When something goes wrong in public health, or Director: Focus Area for Compassion and Ethics (FACE),
global health, offering an apology can be even more Task Force for Global Health, Decatur, USA.
difficult. Responsibility is diffuse and causal pathways Web: www.taskforce.org Email: daddiss@taskforce.org
COMMUNITY EYE HEALTH JOURNAL | VOLUME 32 | NUMBER 107 | 2019 45
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Interpretation of Wechsler Intelligence Scale For Children-Fifth Edition CanadianDocument44 pagesInterpretation of Wechsler Intelligence Scale For Children-Fifth Edition CanadianRaghu kumar VNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- RGP Lens MeasurementDocument5 pagesRGP Lens MeasurementSumon SarkarNo ratings yet
- A Handbook of Contact Lens ManagementDocument102 pagesA Handbook of Contact Lens ManagementOscar Daniel Mendez100% (2)
- Emergency Plan For Rescue From HeightsDocument9 pagesEmergency Plan For Rescue From HeightsMuhammad Shamaran AbdullahNo ratings yet
- Vitality Book (1606456525)Document57 pagesVitality Book (1606456525)Ritu ShewaniNo ratings yet
- 12 - Objective RefractionDocument11 pages12 - Objective RefractionSumon SarkarNo ratings yet
- Anomalous Retinal Correspondence - Diagnostic Tests and TherapyDocument5 pagesAnomalous Retinal Correspondence - Diagnostic Tests and TherapySumon SarkarNo ratings yet
- New Jec Patient Health and History FormDocument2 pagesNew Jec Patient Health and History FormSumon SarkarNo ratings yet
- Silo - Tips - How To Take An Ophthalmic HistoryDocument5 pagesSilo - Tips - How To Take An Ophthalmic HistorySumon SarkarNo ratings yet
- Article 2Document17 pagesArticle 2Sumon SarkarNo ratings yet
- O&A LetterDocument2 pagesO&A LetterSumon SarkarNo ratings yet
- 293 FullDocument9 pages293 FullSumon SarkarNo ratings yet
- Contact Lenses (1) - 151-156Document6 pagesContact Lenses (1) - 151-156Sumon SarkarNo ratings yet
- CCLRU GradingDocument2 pagesCCLRU GradingSumon SarkarNo ratings yet
- SynaptophoreDocument1 pageSynaptophoreSumon SarkarNo ratings yet
- Epidemiological Overview of Preventable Blindness in India-A Focus On Vitamin A Deficiency Among Pre-School Children in IndianDocument20 pagesEpidemiological Overview of Preventable Blindness in India-A Focus On Vitamin A Deficiency Among Pre-School Children in IndianSumon SarkarNo ratings yet
- Umc Meetings 6-6-2022 To 7-6-2022Document4 pagesUmc Meetings 6-6-2022 To 7-6-2022Sumon SarkarNo ratings yet
- The Importance of Epidemiology in Optometry: Oriahi, M. ODocument4 pagesThe Importance of Epidemiology in Optometry: Oriahi, M. OSumon SarkarNo ratings yet
- Phase 1 Assignment 4Document4 pagesPhase 1 Assignment 4Sumon SarkarNo ratings yet
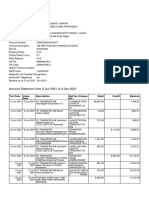
- Account Statement From 2 Jun 2021 To 2 Dec 2021: TXN Date Value Date Description Ref No./Cheque No. Debit Credit BalanceDocument9 pagesAccount Statement From 2 Jun 2021 To 2 Dec 2021: TXN Date Value Date Description Ref No./Cheque No. Debit Credit BalanceSumon SarkarNo ratings yet
- Account Statement From 1 Nov 2021 To 30 Nov 2021: TXN Date Value Date Description Ref No./Cheque No. Debit Credit BalanceDocument2 pagesAccount Statement From 1 Nov 2021 To 30 Nov 2021: TXN Date Value Date Description Ref No./Cheque No. Debit Credit BalanceSumon SarkarNo ratings yet
- National Programme For Control of Blindness: Assistant Prof., Deptt. of Community Medicine GMCH ChandigarhDocument23 pagesNational Programme For Control of Blindness: Assistant Prof., Deptt. of Community Medicine GMCH ChandigarhSumon SarkarNo ratings yet
- 21UCH-105 21UCH-105: Sr. NoDocument9 pages21UCH-105 21UCH-105: Sr. NoSumon SarkarNo ratings yet
- Lecture 9: Case-Control Studies: Mathew Reeves, BVSC, PHDDocument32 pagesLecture 9: Case-Control Studies: Mathew Reeves, BVSC, PHDSumon SarkarNo ratings yet
- Assignment 3: Units 2.1, 2.2 and 2.3 of Module 2 of The IACLE Contact Lens CourseDocument5 pagesAssignment 3: Units 2.1, 2.2 and 2.3 of Module 2 of The IACLE Contact Lens CourseSumon SarkarNo ratings yet
- National Programme For Control of Blindness & Visual ImpairmentDocument15 pagesNational Programme For Control of Blindness & Visual ImpairmentSumon SarkarNo ratings yet
- Aes 03 33Document7 pagesAes 03 33Sumon SarkarNo ratings yet
- Role of The Technician: Lynn Lawrence, CPOT, ABOC, COADocument6 pagesRole of The Technician: Lynn Lawrence, CPOT, ABOC, COASumon SarkarNo ratings yet
- India's 1 Health Management LabDocument14 pagesIndia's 1 Health Management LabAjay Kumar dasNo ratings yet
- DU Yoga National ConferenceDocument2 pagesDU Yoga National ConferenceUjjval SolankiNo ratings yet
- CH 3 4Document22 pagesCH 3 4Marie ChanNo ratings yet
- GEA Districts - 2024-03-07Document24 pagesGEA Districts - 2024-03-07Silvia RabinovichNo ratings yet
- Long Quiz 2Document5 pagesLong Quiz 2ARNEL METILLONo ratings yet
- Lucknow University IMS MBA (Marketing) Human Resource ManagementDocument12 pagesLucknow University IMS MBA (Marketing) Human Resource ManagementShadaab AlamNo ratings yet
- Penguard Topcoat: Technical Data SheetDocument4 pagesPenguard Topcoat: Technical Data SheetSafinahNo ratings yet
- Assigment Leadership Matrix Self Assessment Questionnaire Blake MoutonDocument4 pagesAssigment Leadership Matrix Self Assessment Questionnaire Blake Moutonvarun k.sNo ratings yet
- Free XXX Sex Videos Gay Men One of The Woman S FancyDocument4 pagesFree XXX Sex Videos Gay Men One of The Woman S FancyeliseheacockNo ratings yet
- CHN CHP 7Document5 pagesCHN CHP 7Charmaine Rose Inandan Triviño100% (2)
- Management of Acute Diarrhoea in ChildrenDocument26 pagesManagement of Acute Diarrhoea in ChildrenVishal ParmarNo ratings yet
- Choking ManagementDocument2 pagesChoking ManagementAllysa-raeNo ratings yet
- Great Eastern Life - Confidential Medical Certificate (Other Illnesses) - CLMLAMCODocument2 pagesGreat Eastern Life - Confidential Medical Certificate (Other Illnesses) - CLMLAMCOsimpoonNo ratings yet
- Iaqvec2023 511Document17 pagesIaqvec2023 511M. Iqbal, S.T., M.Sc M. Iqbal, S.T., M.ScNo ratings yet
- ANC ThesisDocument91 pagesANC ThesisAlemseged NegashNo ratings yet
- NCM 120 - 1st LEDocument48 pagesNCM 120 - 1st LEYo MamaNo ratings yet
- Hawassa University: Faculty of Veterinary MedicineDocument6 pagesHawassa University: Faculty of Veterinary MedicineSamuel TsigeNo ratings yet
- Child Rearing Practices Among Families in Countryside PhilippinesDocument7 pagesChild Rearing Practices Among Families in Countryside PhilippinesDina Mae TadeoNo ratings yet
- CBCP PDFDocument7 pagesCBCP PDFDarnell WoodardNo ratings yet
- Hasil Try Out Exclusive Ujikom Kebidanan 3.0Document15 pagesHasil Try Out Exclusive Ujikom Kebidanan 3.0Kaelah AjiNo ratings yet
- Adopting Reso BNCDocument2 pagesAdopting Reso BNCVin XhyneNo ratings yet
- UNHCR Brochure ENDocument36 pagesUNHCR Brochure ENamandeep kansalNo ratings yet
- (123doc) - Opthalmic-Microsurgical-Suturing-Techniques-Part-3-PpsxDocument15 pages(123doc) - Opthalmic-Microsurgical-Suturing-Techniques-Part-3-PpsxTEODORA MIHAELA PELEASANo ratings yet
- Svu Area SeatsDocument26 pagesSvu Area SeatsDevi VaraNo ratings yet
- Glioblastoma and Other Malignant GliomasDocument3 pagesGlioblastoma and Other Malignant GliomasSARANo ratings yet
- Anemia CMEDocument64 pagesAnemia CME[ qιlα ]No ratings yet