Professional Documents
Culture Documents
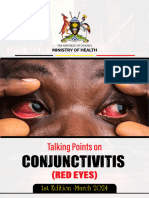
Conjunctivitis (Inflammation of The Eye)
Uploaded by
Jzia Dadie0 ratings0% found this document useful (0 votes)
28 views3 pagesConjunctivitis, or inflammation of the eye, has many causes including bacterial, viral, allergic, and chemical irritants. Symptoms vary depending on the cause but often include redness, irritation, watery or pus-like discharge. Treatment involves antibiotics for bacterial infections, lubricants for viral infections, and antihistamines or other medications to address the specific cause. Good hygiene practices can help prevent the spread of contagious forms of conjunctivitis.
Original Description:
Original Title
Conjunctivitis
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentConjunctivitis, or inflammation of the eye, has many causes including bacterial, viral, allergic, and chemical irritants. Symptoms vary depending on the cause but often include redness, irritation, watery or pus-like discharge. Treatment involves antibiotics for bacterial infections, lubricants for viral infections, and antihistamines or other medications to address the specific cause. Good hygiene practices can help prevent the spread of contagious forms of conjunctivitis.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
28 views3 pagesConjunctivitis (Inflammation of The Eye)
Uploaded by
Jzia DadieConjunctivitis, or inflammation of the eye, has many causes including bacterial, viral, allergic, and chemical irritants. Symptoms vary depending on the cause but often include redness, irritation, watery or pus-like discharge. Treatment involves antibiotics for bacterial infections, lubricants for viral infections, and antihistamines or other medications to address the specific cause. Good hygiene practices can help prevent the spread of contagious forms of conjunctivitis.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Conjunctivitis (inflammation of the eye)
Reviewed by Dr Caroline McEwan, consultant ophthalmologist, Dr Whye Onn Ho, specialist registrar and Dr Una O' Colmain, specialist
registrar
What is conjunctivitis?
Inflammation is seen as reddish change
in the periphery of the eye often
accompanied by a pus-like discharge.
Conjunctivitis is an inflammation of the conjunctiva, which is the mucous membrane covering the white of the eyes and the inner side of the
eyelids.
It usually affects both eyes at the same time – although it may start in one eye and spread to the other after a day or two. It may be
asymmetrical, affecting one eye more than the other.
There are many causes and the treatment will depend upon the cause.
Conjunctivitis is a common eye condition. It's not serious, but it can be uncomfortable and irritating.
What causes conjunctivitis?
There are five different kinds of conjunctivitis, each with its own cause.
Bacterial conjunctivitis
Bacterial conjunctivitis is an infection caused by bacteria, such as staphylococci, streptococci or haemophilus. These organisms may come
from the patient's own skin or upper respiratory tract or they may be caught from another person with conjunctivitis.
Viral conjunctivitis
Viral conjunctivitis is often associated with the common cold. This may be caused by a virus called 'adenovirus'. This type of conjunctivitis
can spread rapidly between people and may cause an epidemic of conjunctivitis.
Chlamydial conjunctivitis
This type of conjunctivitis is caused by an organism called Chlamydia trachomatis. This organism may also affect other parts of the body and
can cause the sexually transmitted infection chlamydia.
Allergic conjunctivitis
Allergic conjunctivitis is common in people who have other signs of allergic disease, such as hay fever, asthma and eczema. The
conjunctivitis is often caused by antigens like pollen, dust mites or cosmetics.
Reactive conjunctivitis – chemical or irritant conjunctivitis
Some people are susceptible to chemicals in swimming pools or to smoke or fumes, and this can cause an irritation of the conjunctiva with
discomfort, redness and watering. In such cases these irritants should be avoided.
What are the symptoms of conjunctivitis?
Bacterial conjunctivitis
This is a condition that affects both eyes. The eyes will usually feel gritty and irritated with a sticky discharge. The eyelids may be stuck
together particularly in the mornings, and there may be discharge or crusting on the eyelashes.
Viral conjunctivitis
The eyes are red and there may be a watery discharge.
Often the eyelids are very swollen and even the conjunctiva on the white of the eye may be swollen, creating a glassy appearance.
The eyes are uncomfortable, and there may also be the generalised symptoms of a cold. Sometimes there are tender lymph nodes (swollen
glands) around the ear or the neck.
This type of conjunctivitis may also spread to affect the cornea (keratitis), and it may persist for several weeks and cause hazy vision.
Chlamydial conjunctivitis
One or both eyes will be red with a sticky discharge and, sometimes, swollen eyelids. The cornea may also be involved in this condition.
Allergic conjunctivitis
Allergic conjunctivitis is usually associated with intense itching of the eyes.
There may be a stringy discharge and the eyes are usually intermittently red. This may occur at particular times of the year, for instance
during spring and summer when there is a lot of pollen in the air.
Conjunctivitis in young children
Small children may be susceptible to infective conjunctivitis, and they may develop severe forms of the condition because of poor immune
defences.
This is particularly the case in babies, and conjunctivitis in an infant aged less than one month old is a notifiable disease in the UK.
This type of conjunctivitis (ophthalmia neonatorum) may be due to an infection that has been contracted during the passage through the
mother’s birth canal and may include the sexually transmitted infections, such as gonococcal or chlamydialinfection.
Small babies may develop conjunctivitis from other types of infection, but swabs should always be taken in order that appropriate treatment
can be given.
Small babies often have poorly developed tear drainage passages (a condition known as nasolacrimal duct obstruction).
These children are susceptible to watering eyes and they may intermittently become sticky, but this is usually not serious and most of the
time this settles down with no treatment.
How is conjunctivitis treated?
Bacterial conjunctivitis
This is usually treated with broad spectrum antibiotic drops or ointment, (egchloramphenicol or fusidic acid).
The eyes should also be cleaned with cotton wool soaked in cooled boiled water to remove any crusts or stickiness.
For bacterial conjunctivitis, research evidence shows that while 64 per cent of cases will clear on their own within five days, antibiotic eye
medication does lead to increased cure rates and earlier remission.
Viral conjunctivitis
There is no effective treatment for viral conjunctivitis. But the eyes may be made more comfortable by using a lubricant ointment such
as Lacri-Lube.
Cold compresses on the eyes and tablets, such as paracetamol andibuprofen, can help the symptoms.
As this is a highly contagious condition, it's important to ensure that a strict code of hygiene is adhered to, such as hand and face washing
and no sharing of face towels.
Close contact with other people, eg at school, is not recommended for the first one to two weeks to help prevent spread of the infection.
This condition may go on for a prolonged time and in some instances corticosteroid drops have been advocated although these should only
be given under the strict supervision of a doctor specialising in eye disease (ophthalmologist).
Chlamydia conjunctivitis
Treatment is with chlorotetracycline ointment to both eyes and tetracycline tablets in order to ensure that infection elsewhere is controlled.
Children cannot be treated with tetracycline tablets, and erythromycin is usually used for them.
Because of the possible infection of other mucous membranes any associated sexually transmitted infection should be identified and both
the patient and their partners must be treated.
Conjunctivitis in infants
This needs to be taken very seriously.
Specimens are taken from the sticky discharge and such children must be seen by an ophthalmologist.
Treatment is given depending on the underlying cause of the conjunctivitis, based on results of the swabs from the laboratory.
Allergic conjunctivitis
This can be treated using topical antihistamine drops.
Drops, such as sodium cromoglicate (eg Opticrom eye drops), can be used to prevent the allergic response and they need to be used for
many weeks in order to give any result.
Corticosteroid drops are occasionally used, but should only be used under the supervision of an ophthalmologist.
The main treatment should be identifying what is triggering off the allergic response and removing this source of allergen.
What is Trachoma?
Trachoma is a form of conjunctivitis that is common in the developing world, particularly in parts of Africa and Asia.
It's exacerbated by a lack of clean water because it's spread by contact with other infected people and by flies.
Trachoma is one of the world’s greatest causes of blindness because long-standing infection develops and causes scarring of the eyelids
and eyes.
The most effective treatment is to provide a clean supply of water that allows good hygiene.
Antibiotics are also effective in treating the infection in the short term, but recurrent re-infection from within communities causes more
damage.
How does the doctor make the diagnosis?
Conjunctivitis can usually be diagnosed and treated by your GP.
The doctor will usually diagnose the condition based on examination of your eyes and the history that you give.
Sometimes, a swab has to be taken from the eye – especially if there is no improvement on standard treatment.
In some cases that are severe or do not respond to treatment, you may need to see an eye specialist (ophthalmologist).
What should I pay particular attention to?
If there is any worsening of the symptoms despite treatment or if the vision deteriorates, a further consultation with your doctor should be
requested even if treatment is being carried out.
If you wear contact lenses and develop symptoms of conjunctivitis, it's important to see your doctor. People who wear contact lenses can
develop a serious infection of the cornea which requires specialist treatment.
What can be done to avoid conjunctivitis?
Good hygiene of hands and face is important. There should be no sharing of face towels, especially if someone has conjunctivitis.
Conjunctivitis can spread from one eye to the other, especially when you rub your eyes. Pus and crust should be removed by bathing the eye
with lukewarm salt water, which can also lessen the symptoms.
Use disposable tissues when you dry the eyes and throw them away after use. This will limit the contamination. Dispose of any antibiotic eye
drops after the treatment is over.
People who suffer from conjunctivitis should have a special towel that only they use.
It is sensible to never share eye make up or eye drops with another person.
How does conjunctivitis usually progress?
Even if left untreated, most forms of conjunctivitis will gradually get better on their own in a few weeks. Allergic conjunctivitis usually
continues while there's exposure to the aggravating agent.
With appropriate treatment, the eyes are usually more comfortable within a few days, although cases of adenoviral infection may cause
problems for some weeks.
Other people also read:
Allergy: get advice on what other things provoke attacks.
Cataracts: how does the doctor make a diagnosis?
Chlamydia infections: what complications can it cause?
Hay fever and allergic perennial rhinitis: what medicine can you take?
References
Sheikh A, Hurwitz B, Cave J. Antibiotics for acute bacterial conjunctivitis. Cochrane Library. Issue 3, 1999.
Based on a text by Per Lykke Gregersen, consultant
Last updated 03.02.2011
You might also like
- Quantum Techniques Client ManualDocument42 pagesQuantum Techniques Client ManualVeres Beatrix100% (4)
- Common Eye DiseasesDocument54 pagesCommon Eye Diseaseskyro draxNo ratings yet
- Enema Instructional BookletDocument34 pagesEnema Instructional Bookletmumtean cosminNo ratings yet
- Nasogastric Gastrostomy Tube Feedling Guidelines v1.4Document45 pagesNasogastric Gastrostomy Tube Feedling Guidelines v1.4bandarascbNo ratings yet
- ABC of Red EyeDocument5 pagesABC of Red Eyeakmar887No ratings yet
- CASE STUDY - ConjunctivitisDocument9 pagesCASE STUDY - ConjunctivitisAngela CancinoNo ratings yet
- BLEPHARITISDocument25 pagesBLEPHARITISSrijana MahatoNo ratings yet
- PLAB 2 Notes Part 2Document565 pagesPLAB 2 Notes Part 2Anonymous YqCxXQ6wF5No ratings yet
- ConjunctivitisDocument5 pagesConjunctivitisAmrit Preet KaurNo ratings yet
- Red Eyes (Conjunctivitis), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandRed Eyes (Conjunctivitis), A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Health Talk TopicsDocument3 pagesHealth Talk Topicsvarshasharma0562% (13)
- Unit Plan (3) Child Health NursingDocument5 pagesUnit Plan (3) Child Health Nursinggill priyaNo ratings yet
- ConjunctivitisDocument4 pagesConjunctivitisCrisMartAgullanaNo ratings yet
- Sore Eyes (Conjunctivitis/Pink Eyes)Document21 pagesSore Eyes (Conjunctivitis/Pink Eyes)Diana MaeNo ratings yet
- CONJUNCTIVITISDocument8 pagesCONJUNCTIVITISWàrìs Ràfìqùé ßàlòçhNo ratings yet
- College of Medicine and Health SciencesDocument17 pagesCollege of Medicine and Health SciencesJean De La Paix MugwanezaNo ratings yet
- ConjunctivitisDocument3 pagesConjunctivitisFaye DacsNo ratings yet
- Case PresentationDocument11 pagesCase PresentationJOhn DiCeNo ratings yet
- MICRO BIOLOGY ConjunctivitisDocument5 pagesMICRO BIOLOGY Conjunctivitisbabyko143444No ratings yet
- Eye & Ear - Eye - Conjunctivitis - PharmaPedia - PharmaGatesDocument9 pagesEye & Ear - Eye - Conjunctivitis - PharmaPedia - PharmaGatesIslam FawzyNo ratings yet
- ConjunctivitisDocument19 pagesConjunctivitiskatrina_velasco_1No ratings yet
- Conjunctivitis and Hearing Loss: Submitted By: Pamo, JoshuaDocument13 pagesConjunctivitis and Hearing Loss: Submitted By: Pamo, Joshuachazney casianoNo ratings yet
- Eye InfectionsDocument16 pagesEye InfectionsrodericpalanasNo ratings yet
- Eye Infection and Blepharitis by MHSNDocument18 pagesEye Infection and Blepharitis by MHSNMhsn0% (1)
- Conjunctivitis Nursing ManagementDocument3 pagesConjunctivitis Nursing Managementflex gyNo ratings yet
- Conjunctivitis On The Rise - Causes, Symptoms, Prevention, and TreatmentDocument2 pagesConjunctivitis On The Rise - Causes, Symptoms, Prevention, and TreatmentKamatNo ratings yet
- Conjunctivitis 1Document28 pagesConjunctivitis 1Nrs Sani Sule MashiNo ratings yet
- Corneal UlcerDocument35 pagesCorneal UlcerMary Mae Bercacio BuellaNo ratings yet
- Academic Essay On Sterile and Infectious KeratitisDocument3 pagesAcademic Essay On Sterile and Infectious KeratitisAneelaMalikNo ratings yet
- Conjunctivitis Pink EyeDocument2 pagesConjunctivitis Pink EyeVeeNo ratings yet
- H3e8g OczbiDocument7 pagesH3e8g OczbiShumaila AzamNo ratings yet
- Conjunctivitis 03Document4 pagesConjunctivitis 03Carmii CastorNo ratings yet
- ConjunctivitisDocument2 pagesConjunctivitist304pkNo ratings yet
- ASCIA PCC Allergic Conjunctivitis 2015Document4 pagesASCIA PCC Allergic Conjunctivitis 2015LuqnieReitaNo ratings yet
- Bacterial and Viral Conjunctivitis: What Is Conjunctivitis? TreatmentDocument2 pagesBacterial and Viral Conjunctivitis: What Is Conjunctivitis? TreatmentElrach CorpNo ratings yet
- Conjunctivitis - AAFPDocument23 pagesConjunctivitis - AAFP21613284No ratings yet
- Conjunctivitis (Pink Eye)Document15 pagesConjunctivitis (Pink Eye)MD TristanNo ratings yet
- A Corneal Ulcer Is An Open Sore On The CorneaDocument3 pagesA Corneal Ulcer Is An Open Sore On The CorneaDhillon DillingerNo ratings yet
- Prevention of Red EyeDocument1 pagePrevention of Red EyeMaxcer AdNo ratings yet
- CONJUNCTIVITISDocument7 pagesCONJUNCTIVITISogwal andrewictynetNo ratings yet
- Pink Eye (Conjunctivitis) : When To See A DoctorDocument4 pagesPink Eye (Conjunctivitis) : When To See A DoctorMohammed Shamiul ShahidNo ratings yet
- CONJUNCTIVITISDocument2 pagesCONJUNCTIVITIScpborneoNo ratings yet
- What Is KeratitisDocument6 pagesWhat Is KeratitisFebrinaNo ratings yet
- Talking Points Conjunctivitis (RED EYES) - 21st March 2024Document5 pagesTalking Points Conjunctivitis (RED EYES) - 21st March 2024sabellanabimanya9No ratings yet
- Conjunctivitis - Dita LSDocument17 pagesConjunctivitis - Dita LSMeNo ratings yet
- ConjunctivitisDocument14 pagesConjunctivitisSharmila gafoor.14-ANo ratings yet
- Conjunctivitis UpToDateDocument21 pagesConjunctivitis UpToDateRosejane MagauayNo ratings yet
- ConjunctivitisDocument1 pageConjunctivitisIbrahim QariNo ratings yet
- Eye Emergency: DR Abdelmoniem SaeedDocument63 pagesEye Emergency: DR Abdelmoniem SaeedYousef Al-AmeenNo ratings yet
- Allergic Conjunctivitis: Ascia Information For Patients, Consumers and CarersDocument4 pagesAllergic Conjunctivitis: Ascia Information For Patients, Consumers and CarersElrach CorpNo ratings yet
- Conjunctivitis 2016 - 1Document2 pagesConjunctivitis 2016 - 1Rida RahayuNo ratings yet
- Conjunctivitis 1385 PILDocument2 pagesConjunctivitis 1385 PILMicius91No ratings yet
- Dieses of ConjunctivitisDocument2 pagesDieses of ConjunctivitisSiMS learnOnlineNo ratings yet
- Bacteria PowerpointDocument21 pagesBacteria PowerpointOpubo BrownNo ratings yet
- Conjunctivitis (Bacterial and Viral)Document2 pagesConjunctivitis (Bacterial and Viral)Abhay SagarNo ratings yet
- Viral Conjunctivitis: Daniel Solano Craig N. CzyzDocument6 pagesViral Conjunctivitis: Daniel Solano Craig N. CzyzJavier BarretoNo ratings yet
- Conjunctivity (RED EYES) Talking Points - 2024 - 1Document5 pagesConjunctivity (RED EYES) Talking Points - 2024 - 1Odiit StephenNo ratings yet
- Eyelid Disorders: Ii. ChalazionDocument62 pagesEyelid Disorders: Ii. ChalazionFreeburn SimunchembuNo ratings yet
- Apollo247-Eye FluDocument1 pageApollo247-Eye Flujonifow730No ratings yet
- Author: Section Editor: Deputy EditorDocument20 pagesAuthor: Section Editor: Deputy EditorEvy Alvionita YurnaNo ratings yet
- Conjunctivitis by Asma GulDocument36 pagesConjunctivitis by Asma GulAbdul SamadNo ratings yet
- Sore EyesDocument2 pagesSore EyescpborneoNo ratings yet
- Contact Lens-Associated Microbial KeratitisDocument39 pagesContact Lens-Associated Microbial Keratitisณัช เกษมNo ratings yet
- BlepharitisDocument2 pagesBlepharitisPranay SriNo ratings yet
- MS Eye and Vision DisordersDocument78 pagesMS Eye and Vision DisordersAntoinette Sallan NopiaNo ratings yet
- Cystic Fibrosis: Meet The Client: Debbie BakerDocument8 pagesCystic Fibrosis: Meet The Client: Debbie BakerJasjit Singh100% (1)
- HEALTH 8 3rd 4thDocument5 pagesHEALTH 8 3rd 4thBrian CorpuzNo ratings yet
- (Antonella Surbone MD, PHD, FACP (Auth.), Antonell (B-Ok - Org) 2Document525 pages(Antonella Surbone MD, PHD, FACP (Auth.), Antonell (B-Ok - Org) 2Anonymous YdFUaW6fBNo ratings yet
- BudesonideDocument2 pagesBudesonideLouie James Velasco OstreaNo ratings yet
- Pharmacoeconomics - Part IIIDocument29 pagesPharmacoeconomics - Part IIISima JabbariNo ratings yet
- 1 - Indications For Removal of TeethDocument7 pages1 - Indications For Removal of TeethLama NahedNo ratings yet
- Management of A Case of Ventricular Bigeminy UsingDocument2 pagesManagement of A Case of Ventricular Bigeminy UsingAlfian AlfianNo ratings yet
- 2UDocument47 pages2Uucnursingcesdev2008100% (3)
- Brochure Medicine PDFDocument12 pagesBrochure Medicine PDFJacklineNo ratings yet
- Pedia ReportDocument4 pagesPedia ReportBeda MalecdanNo ratings yet
- Nerium OleanderDocument20 pagesNerium OleanderGeneizzel GotuatoNo ratings yet
- Meyer Et Al 2001Document38 pagesMeyer Et Al 2001MIANo ratings yet
- 2013-11-20 Metlit Meta-Analysis Critical Appraisal Partini P. TrihonoDocument64 pages2013-11-20 Metlit Meta-Analysis Critical Appraisal Partini P. TrihonoHanumNo ratings yet
- NCRP Report 155 AapmDocument266 pagesNCRP Report 155 AapmFISICO CADAVIDNo ratings yet
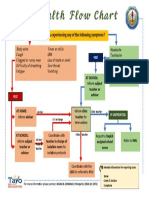
- Health Flow ChartDocument1 pageHealth Flow ChartAlex Cainoy JrNo ratings yet
- National Health AccountsDocument4 pagesNational Health AccountsMyat MinNo ratings yet
- 65 Interview Questions For Nurses.13Document3 pages65 Interview Questions For Nurses.13natalieshirleyNo ratings yet
- Zoonotic Potentiality of Protozoa: Assignment Subject: ParasitologyDocument7 pagesZoonotic Potentiality of Protozoa: Assignment Subject: ParasitologyArushi PatiyalNo ratings yet
- Lemos 2016Document32 pagesLemos 2016wendyjemmy8gmailcomNo ratings yet
- Actinomycetes Staining MethodsDocument14 pagesActinomycetes Staining MethodsvikasNo ratings yet
- Medical Reimbursement Claim FormDocument2 pagesMedical Reimbursement Claim FormHimanshu JainNo ratings yet
- Nnaca Sop 302Document6 pagesNnaca Sop 302Thusitha LakpriyaNo ratings yet
- Contagious Bovine PyelonephritisDocument26 pagesContagious Bovine PyelonephritisMuhammad Hamza AlviNo ratings yet
- Arnica Montana - FayazuddinDocument13 pagesArnica Montana - FayazuddinMohammad AtaNo ratings yet