Professional Documents
Culture Documents
3C3 Subgroup1 M11 PT1
Uploaded by
ENKELI VALDECANTOSOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
3C3 Subgroup1 M11 PT1
Uploaded by
ENKELI VALDECANTOSCopyright:
Available Formats
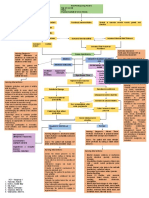
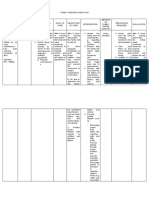
Legend
Risk/Predisposing Factors
Risk Factors
•Age (47 yrs old)
•Stress
Pathophysiology
•Physical Inactivity (8 hours of work)
Signs and Symptoms
Nursing diagnosis,
goals, & interventions Defects in renal sodium homeostasis Functional, vasoconstriction Defects in vascular smooth muscle growth and structure
Medications
Inadequate sodium excretion
Diagnostic/Laboratory
Tests Sodium and Water retention
Increased Plasma and ECF volume Increased Vascular activity Increased Vascular Wall Thickness
Increased Cardiac
Output Increased Total Peripheral
Resistance
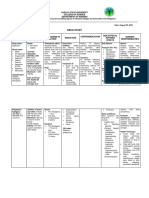
NURSING DIAGNOSIS
Nursing Diagnosis: Acute pain r/t increased BP as
Primary Hypertension evidenced by discomfort
Activity intolerance r/t
weakness as evidenced by
reports of dizziness Dizziness Discomfort: Headache and Nape Goals: The patient will participate in
and weakness of the body pain activities that reduce the pain.
Weakness of the body Acetaminophen, Naproxen
Goals: The patient will
participate in necessary sodium Nursing Interventions:
desired activities and the
Vestibular suppressant Laboratory/Diagnostic Tests: Acknowledge and accept
patient will use identified
drugs (Diazepam, • Urinalysis the client’s pain.
techniques to enhance
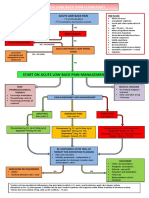
meclizine) Hypertensive Crisis • Blood Chemistry •Obtain client’s/SO’s
activity tolerance.
• 12-lead ECG assessment of pain to
• Creatinine Clearance include location,
Rapid increased vascular • Renin Levels characteristics, onset,
Nursing Interventions: resistance • 24-hour urine protein duration, frequency, quality,
Establish guidelines and goals of activity intensity.
with the patient •Provide comfort measures
Endothelial Damage Spontaneous natriuresis (e.g., touch, repositioning,
•Ascertain ability to move about and
degree of assistance necessary or use of use of heat or cold packs,
equipment to determine current status and nurse’s presence), quiet
Intravascular volume depletion
needs associated with participation in environment, and calm
needed activities. Increased Endothelial activities to promote
permeability nonpharmacological pain
•Increase exercise/activity levels gradually; Increased in vasoconstrictors
teach methods to conserve energy management.
•Plan care to carefully balance rest periods Dec. in vasodilators, nitric •Instruct in and encourage
with activities to reduce fatigue oxide, prostacyclin use of relaxation
•Provide positive atmosphere, while Further increase in blood techniques, such as focused
acknowledging the difficulty of the situation pressure breathing, imaging,
Platelet and fibrin intimal CDs/tapes (e.g., “white”
for the client. H proliferation
•Encourage client to maintain positive noise, music, instructional)
attitude; suggest use of relaxation to distract attention and
techniques, such as visualization or guided Severe blood pressure reduce tension.
imagery, as appropriate, to enhance sense elevation •Encourage diversional
of well-being. activities (e.g., TV/radio,
•Encourage participation in recreation, socialization with others).
social activities, and hobbies appropriate Elevated BP 220/150 mm Syncope •Establish collaborative
for situation. Hg approach for pain
management based on
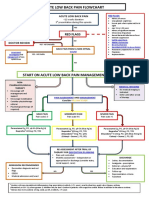
Nursing Diagnosis: Altered Tissue client’s understanding about
Nursing Diagnosis: Decreased cardiac Perfusion r/t decrease in peripheral blood and acceptance of available
Beta blockers
output r/t altered contractility evidenced circulation AEB syncope and elevated BP. treatment options
(Metoprolol, Propranolol)
by elevated BP •Administer analgesics, as
Goals: The patient will show effective indicated
ACE inhibitors
Goals: The patient will maintain BP tissue perfusion by having a stable blood
(captopril, ramipril)
within individually acceptable range. pressure.
Angiotensin 2 receptor
blockers Nursing Interventions:
(Losartan, Valsartan) Nursing Interventions:
Check the blood pressure in the
morning before eating or taking any • Monitor changes suddenly or continuous
medication and in the evening mental disorders (anxiety, confusion,
•Keep client on bed rest in a position of lethargy).
comfort • Observation of pallor, cyanosis, striped, skin
•Administer oxygen via mask or cold / humid, record peripheral pulse
ventilator if needed strength.
•Provide a peaceful environment to • Assess Homan's sign (pain in the calf with
promote adequate rest dorsiflexion), erythema, edema.
•Encourage the patient to perform self- • Encourage leg exercises active / passive.
care activities • Monitor breathing.
•Collaborate with nutritionist for diet • Assess GI function, note; anorexia,
restrictions decreased bowel sounds, nausea /
3C3 – Subgroup 1 •Educate the patient about the s/s and vomiting, abdominal distension,
1. Florentino, Robelle report any changes constipation.
2. Gomez, Khallae May •Give information about positive signs of • Monitor input and changes in urine output.
3. Sia, Angel improvement, such as normal BP • Prevent injury (nonskid socks, doesn’t walk
4. Tabora, Kurt Raidel •Encourage the patient to engage in without assistance, bed in the lowest locked
5. Urayanza, Nikka Ira regular exercise position, necessary items within reach, call
6. Valdecantos, Enkeli S. bell within reach, side rails up x3)
You might also like
- ShitDocument1 pageShitENKELI VALDECANTOSNo ratings yet
- Naproxen Drug StudyDocument4 pagesNaproxen Drug StudyTimz GatdulaNo ratings yet
- Case Study CvaDocument33 pagesCase Study CvaArmand Bong Santiago100% (1)
- LosartanDocument2 pagesLosartanVina Jane P Laurel89% (9)
- Drug StudyDocument6 pagesDrug StudyGeraldine Gallaron - CasipongNo ratings yet
- Kelompok 1 - Kelas B - Nursing English IIDocument7 pagesKelompok 1 - Kelas B - Nursing English IINazimatul FitriyahNo ratings yet
- Beriso Drug StudyDocument5 pagesBeriso Drug StudyKasandra Dawn Moquia BerisoNo ratings yet
- Nifedepine Drug StudyDocument1 pageNifedepine Drug StudyMa. Sheenadel ZamudioNo ratings yet
- AmlodipineDocument2 pagesAmlodipineVina Jane P Laurel92% (12)
- AmlodipineDocument2 pagesAmlodipineCj LowryNo ratings yet
- Drug Study - ParacetamolDocument2 pagesDrug Study - ParacetamolNE TdrNo ratings yet
- Decreased Cardiac Output NCPDocument2 pagesDecreased Cardiac Output NCPmicah1318100% (2)
- COLCHICINEDocument4 pagesCOLCHICINEMitch GonzalesNo ratings yet
- Nursing Care Plan: Case ScenarioDocument14 pagesNursing Care Plan: Case ScenarioShelvin Jules LayvaNo ratings yet
- Emergency DrugsDocument16 pagesEmergency DrugsDavid Hines LopezNo ratings yet
- Acute Low Back Pain Flowchart March 2016Document1 pageAcute Low Back Pain Flowchart March 2016Alfiya HasnaNo ratings yet
- Methadone HCLDocument2 pagesMethadone HCLtiffanald50% (2)
- College of Nursing and Midwifery: Mabini Colleges Daet, Camarines NorteDocument10 pagesCollege of Nursing and Midwifery: Mabini Colleges Daet, Camarines NorteMa. Sheenadel ZamudioNo ratings yet
- Nursing Care Plan of A Patient With Ebola Virus DiseaseDocument3 pagesNursing Care Plan of A Patient With Ebola Virus DiseaseJam100% (1)
- Clinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzDocument31 pagesClinical Therapeutics Oral Revalida Review Notes: CASE 1: Dr. Abraham Daniel C. CruzNoreenNo ratings yet
- Acute Low Back Pain Flowchart January 2017Document1 pageAcute Low Back Pain Flowchart January 20171234chocoNo ratings yet
- ParacetamolDocument2 pagesParacetamolAnreezahy GnoihcNo ratings yet
- Evangelista Drug-StudyDocument15 pagesEvangelista Drug-Studydinglasanerica57No ratings yet
- CPG Bite StingsDocument10 pagesCPG Bite StingsMarvin M PulaoNo ratings yet
- College of Nursing and Midwifery: Mabini Colleges Daet, Camarines NorteDocument1 pageCollege of Nursing and Midwifery: Mabini Colleges Daet, Camarines NorteMa. Sheenadel ZamudioNo ratings yet
- Case Presentation Station 3B Drug Study ClinidineDocument6 pagesCase Presentation Station 3B Drug Study ClinidinehahahahaaaaaaaNo ratings yet
- Cabildo, Grandville Mia M.-Tahbso CaseDocument8 pagesCabildo, Grandville Mia M.-Tahbso CaseEarl Joseph DezaNo ratings yet
- Epo DrugstudyDocument3 pagesEpo DrugstudyKhatlen BagaresNo ratings yet
- Lidocaine and Bupivacaine Local AnesthesiaDocument2 pagesLidocaine and Bupivacaine Local AnesthesiaEmer NicolasNo ratings yet
- Drugstudy Fourniers GangreneDocument13 pagesDrugstudy Fourniers GangrenemarinordNo ratings yet
- Estoya, Gen Paulo C. - BPH NCP - NCM 112 LecDocument3 pagesEstoya, Gen Paulo C. - BPH NCP - NCM 112 LecGen Paulo EstoyaNo ratings yet
- MARQUEZ Acetaminophen DSDocument3 pagesMARQUEZ Acetaminophen DSMacy MarquezNo ratings yet
- Week 2 Individual AssignmentDocument1 pageWeek 2 Individual AssignmentPaul SahagunNo ratings yet
- Nitrates Drug StudyDocument4 pagesNitrates Drug StudyNikael Patun-ogNo ratings yet
- Make A Drug Study On The Medications Given To JaneDocument2 pagesMake A Drug Study On The Medications Given To JaneYoko Mae YanoNo ratings yet
- Femur FractureDocument19 pagesFemur FractureMadx VNo ratings yet
- MetherginDocument2 pagesMetherginOtan Cuison100% (1)
- 5 Drug StudyDocument5 pages5 Drug StudyAbijah Leris SarmientoNo ratings yet
- Drug Study YyyDocument7 pagesDrug Study YyyIanjoyce OlivarNo ratings yet
- Sample (Concept Map)Document1 pageSample (Concept Map)NMDNMSSDNo ratings yet
- Pain Dr. HenryDocument36 pagesPain Dr. Henryreagan setiawanNo ratings yet
- NaproxenDocument2 pagesNaproxenDeinielle Magdangal RomeroNo ratings yet
- Acute PainDocument1 pageAcute Painnursing concept mapsNo ratings yet
- Drug Study NifedipineDocument3 pagesDrug Study NifedipineJanzelvine Lee MontenegroNo ratings yet
- NEURODISORDERSDocument24 pagesNEURODISORDERSMiden AlbanoNo ratings yet
- Drug StudyDocument49 pagesDrug StudyLexa Moreene Cu�adoNo ratings yet
- Assessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermDocument4 pagesAssessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermGensen Cu RoxasNo ratings yet
- Neuromuscular Junction Blocking AgentsDocument9 pagesNeuromuscular Junction Blocking AgentsSyvNo ratings yet
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial InfarctionjamieboyRN88% (8)
- Assignment 3Document5 pagesAssignment 3Samantha PargadNo ratings yet
- Ketorolac 2Document1 pageKetorolac 2Ma. Sheenadel ZamudioNo ratings yet
- Bonilla Drug Study 2 20Document9 pagesBonilla Drug Study 2 20YLA KATRINA BONILLANo ratings yet
- Drug Study (Aspirin, in Enalapril Maleate, Tramadol, AmlodipineDocument10 pagesDrug Study (Aspirin, in Enalapril Maleate, Tramadol, AmlodipineFlauros Ryu Jabien100% (1)
- DrugstudyDocument2 pagesDrugstudyacissej_o3No ratings yet
- Combinepdf 3Document95 pagesCombinepdf 3paruNo ratings yet
- NCP DengueDocument3 pagesNCP DengueNecy Tessa C. AcostaNo ratings yet
- Peripheral Receptor Targets for Analgesia: Novel Approaches to Pain ManagementFrom EverandPeripheral Receptor Targets for Analgesia: Novel Approaches to Pain ManagementNo ratings yet
- Fast Facts: Perioperative Pain: Effective management has numerous benefitsFrom EverandFast Facts: Perioperative Pain: Effective management has numerous benefitsNo ratings yet
- Interventional Radiology of the Spine: Image-Guided Pain TherapyFrom EverandInterventional Radiology of the Spine: Image-Guided Pain TherapyJ. Kevin McGrawNo ratings yet
- Pain Free 1-2-3: A Proven Program for Eliminating Chronic Pain NowFrom EverandPain Free 1-2-3: A Proven Program for Eliminating Chronic Pain NowRating: 1 out of 5 stars1/5 (1)
- Cardiovascular Disorders: Concept: Oxygen DebtDocument15 pagesCardiovascular Disorders: Concept: Oxygen DebtENKELI VALDECANTOSNo ratings yet
- Family Nursing Care During The COVID-19 Pandemic: Conference PaperDocument6 pagesFamily Nursing Care During The COVID-19 Pandemic: Conference PaperENKELI VALDECANTOSNo ratings yet
- Valdecantos Oral Revalida SLEDocument1 pageValdecantos Oral Revalida SLEENKELI VALDECANTOSNo ratings yet
- Lower RespiratoryDocument35 pagesLower RespiratoryENKELI VALDECANTOSNo ratings yet
- 1 Family Data Base AssessmentDocument15 pages1 Family Data Base AssessmentENKELI VALDECANTOSNo ratings yet
- COPD and Lung CancerDocument42 pagesCOPD and Lung CancerENKELI VALDECANTOSNo ratings yet
- Family Nursing Care Plan: Partially AchievedDocument3 pagesFamily Nursing Care Plan: Partially AchievedENKELI VALDECANTOSNo ratings yet
- Valdecantos3c3 m2 Post Task RleDocument15 pagesValdecantos3c3 m2 Post Task RleENKELI VALDECANTOSNo ratings yet
- Valdecantos M3 Pre TaskDocument1 pageValdecantos M3 Pre TaskENKELI VALDECANTOSNo ratings yet
- Quiz #3 - Interactive Communication Simulator Exercise (Triad Group 1)Document2 pagesQuiz #3 - Interactive Communication Simulator Exercise (Triad Group 1)ENKELI VALDECANTOSNo ratings yet
- Upper RespiratoryDocument37 pagesUpper RespiratoryENKELI VALDECANTOSNo ratings yet
- Acid Normal Base: HG, and HCO3 25 Mmol/l. What Does This Mean?Document3 pagesAcid Normal Base: HG, and HCO3 25 Mmol/l. What Does This Mean?ENKELI VALDECANTOSNo ratings yet
- Communal LandDocument17 pagesCommunal Landermias dersehNo ratings yet
- NEW Curriculum Vitae Marking Scheme (Jan 2022)Document2 pagesNEW Curriculum Vitae Marking Scheme (Jan 2022)TONo ratings yet
- Invoice 2 PDFDocument1 pageInvoice 2 PDFPurva TiwariNo ratings yet
- Justification of StorytellingDocument3 pagesJustification of StorytellingJoanne Lian Li FangNo ratings yet
- Microbiology & ImmunologyDocument24 pagesMicrobiology & ImmunologyKumuthaa ShroomNo ratings yet
- Collaborating With China Forestry Higher EducationDocument20 pagesCollaborating With China Forestry Higher EducationjuanbvNo ratings yet
- Albatross Academy BrochureDocument4 pagesAlbatross Academy BrochureBhavesh KriplaniNo ratings yet
- 2 The Therapeutic Nurse-Client RelationshipDocument30 pages2 The Therapeutic Nurse-Client Relationshipsri endriyaniNo ratings yet
- De-Stijl ArchitectureDocument25 pagesDe-Stijl Architecturedplpthk1502No ratings yet
- NCOB Solidarity Report FINAL PDFDocument135 pagesNCOB Solidarity Report FINAL PDFRes2001No ratings yet
- InglesDocument5 pagesInglesDavid Quiñones PoloNo ratings yet
- Sample Construction BOQDocument2 pagesSample Construction BOQbcss.labNo ratings yet
- 4th Competency Mapping (Final)Document11 pages4th Competency Mapping (Final)Mitz JazNo ratings yet
- Kontrak Jangka PanjangDocument26 pagesKontrak Jangka Panjanganon_800888083No ratings yet
- Be Esd MCQDocument13 pagesBe Esd MCQsuhaskakade0075745No ratings yet
- Case Study Questions: Group NameDocument9 pagesCase Study Questions: Group NameVersha RaniNo ratings yet
- Factors Affecting The Interest of Accounting Students in Career SelectionDocument12 pagesFactors Affecting The Interest of Accounting Students in Career SelectionRazel VistalNo ratings yet
- Ipophl LTFRB Lto Mdppa MoaDocument5 pagesIpophl LTFRB Lto Mdppa MoaMra LappayNo ratings yet
- 01 Overview of StatisticsDocument33 pages01 Overview of StatisticsJohn Lewis SuguitanNo ratings yet
- 5 Coolest Pinoy Inventions You HavenDocument6 pages5 Coolest Pinoy Inventions You HavenChiela BagnesNo ratings yet
- The Family Code of The Philippines: Title Ix Parental AuthorityDocument4 pagesThe Family Code of The Philippines: Title Ix Parental AuthorityMarc Eric Redondo100% (1)
- Tramway Timog PackageDocument2 pagesTramway Timog PackageYzang SisonNo ratings yet
- Purpose: Using NCPA For Passive ChecksDocument10 pagesPurpose: Using NCPA For Passive ChecksMarco ParodiNo ratings yet
- Electro-Diesels v6Document14 pagesElectro-Diesels v6Nuh AinuhaNo ratings yet
- Brown Skin Girl - BeyonceDocument1 pageBrown Skin Girl - BeyonceveritoNo ratings yet
- PCC 1.3.6Document3 pagesPCC 1.3.6usama buttNo ratings yet
- Soutache & Bead EmbroideryDocument97 pagesSoutache & Bead EmbroiderySissy1124100% (2)
- Kali Hanuman Vani HanumanjiDocument11 pagesKali Hanuman Vani HanumanjiDharmendrasinh AtaliaNo ratings yet
- Sikhism-Struggle of Gurus Against Mughal Empire of IndiaDocument45 pagesSikhism-Struggle of Gurus Against Mughal Empire of IndiaBruno AquinoNo ratings yet
- Acp 113 (Ah) Call Sign Book PDFDocument224 pagesAcp 113 (Ah) Call Sign Book PDF王大明No ratings yet