Professional Documents
Culture Documents
Ineffective Breathing Pattern Related To Shortness of Breath Possible Evidence by Cues
Uploaded by
Louie Parilla0 ratings0% found this document useful (0 votes)
39 views7 pagesOriginal Title
NCP-DIABETES M
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
39 views7 pagesIneffective Breathing Pattern Related To Shortness of Breath Possible Evidence by Cues
Uploaded by
Louie ParillaCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 7
BAP
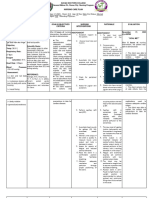
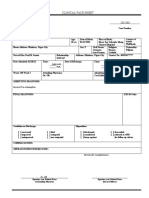
CUES NURSING NURSING NURSING RATIONALE EVALUATION
DIAGNOSIS OBJECTIVE INTERVENTION
Subjective: Ineffective Breathing After 8 hours of - Establish - To gain the •After how many
“Jak makaanges nga pattern related to nursing intervention. Rapport trust of the hours of nursing
nasyaat ading” as shortness of breath The patient will - Monitor Vital patient intervention the client
verbalized by the possible evidence by display blood signs - Indicators of will be able to
patient. cues. pressure within her - Assess the adequacy of verbalize decrease of
normal range patients systematic pain from 8/10 to
Objective: physical perfusion, 3/10
- Restlessness condition fluid/blood, •Clients blood
- Weak looking - Observe non- needs, and pressure is below
- Shallow verbal cues of developing 160/100mmHg
breathing pain such as complications •After how many
Vital Signs: holds body, - To determine hours of nursing
BP: 160/100 facial the severity of intervention the client
PR: 89 expression the pain will able to report
RR: 20 - Assist patient - Supported absence of pain.
TEMP: 36.7 to patient to
comfortable comfortable
position, such position such
as supporting as high
upper fowler’s
extremities position.
with pillows.
BAP
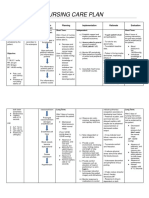
CUES NURSING NURSING NURSING RATIONALE EVALUATION
DIAGNOSIS OBJECTIVE INTERVENTION
S: Patient reports of Risk for decreased After 4 hours of -Measure BP in both -Serial measurements After 4 hours of
cold clammy skin, Cardiac Output as nursing intervention arms. Take three using correct nursing intervention
chills and dizziness. evidenced by altered the patient will readings, 3 to 5 equipment the patient
O: afterload. demonstrate stable minutes apart while provide a more demonstrates stable
BP: 200/120 mmHg cardiac rhythm, rate the client is at rest, complete cardiac rhythm, rate
PR: 112 bpm and BP within normal then sitting, and then picture of vascular and BP within normal
TEMP: 37.1*C range of 120/80 standing for initial involvement and range of 120/80.
O2SAT: 96% evaluation. Use scope of
correct cuff size and problem. Progressive
accurate technique. diastolic readings
Take note of above
elevations in systolic 120 mm Hg are
as well as diastolic considered
readings. first accelerated, then
malignant (very
-Observe skin color, severe).
moisture, Systolic hypertension
temperature, and also
capillary refill time. is an established risk
factor
-Observe for for cerebrovascular
dependent and disease and ischemic
generalized edema. heart
self-care activities as disease even when
needed. diastolic pressure is
not
-Provide calm, restful elevated. In younger
surroundings, clients
minimize with normal systolic
environmental readings, elevated
activity and noise. diastolic
Consider limiting the numbers may
number of visitors or indicate
BAP
length of visitation. prehypertension.
-Maintain activity -Presence of pallor;
restrictions (such as cool, moist skin; and
bedrest or chair rest) delayed capillary
during crisis refill time may be
situations and due
schedule periods of to peripheral
uninterrupted rest; vasoconstriction or
assist client with reflect cardiac
self-care activities as decompensation and
needed. decreased output.
-Provide comfort -May indicate onset
measures, such as of heart or kidney
back and neck failure.
massage or elevation
of head. -Helps reduce
sympathetic
-Instruct in relaxation stimulation and
techniques, guided promotes relaxation.
imagery, and
distractions, if the -Reduces physical
client is interested stress and tension that
and able to affect BP and the
participate. course of
-Monitor response to hypertension.
medications that
control BP. -Decreases
discomfort and may
COLLABORATIVE: reduce sympathetic
Administered stimulation.
medications as
ordered. -Can reduce stressful
stimuli and produce a
calming effect,
BAP
thereby reducing BP.
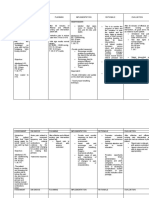
CUES NURSING NURSING NURSING RATIONALE EVALUATION
DIAGNOSIS OBJECTIVE INTERVENTION
- Blood glucose Risk for unstable SHORT TERM: INDEPENDENT: ● Hypertension is The Client verbalized
level of glucose The Client will ● Report BP of commonly associated self-care actions to
269mg/dL level related to verbalize more than 160 with diabetes. Control take if blood glucose
- Inadequate adherence self-care actions to mm Hg of is too high or too low
blood glucose of diabetes take if (systolic). BP prevents coronary a week from the date
medication management blood glucose is too Administer artery disease, stroke, of care.
management plan as evidenced by high hypertensive as retinopathy, and LONG TERM:
- Inadequate inadequate blood or too low a week prescribed. nephropathy. The client maintained
glucose glucose and blood from the ● Assess for signs ● Hyperglycemia fasting blood glucose
monitoring glucose date of care. of results level of 105 mg/dL, 1
level of 269mg/dL LONG TERM: hyperglycemia when there is an hour after the meal a
The client will ● Assess inadequate amount of level of 155 mg/dL,
maintain medications insulin to glucose. and 2 hour pc level of
fasting blood glucose taken regularly. Excess 130 mg/dL
level ● Monitor blood glucose in the blood goals during
of 105 mg/dL, 1 hour glucose levels as creates an osmotic each patient
BAP
after fasting and effect visit.
the meal a level of postprandial that results in increased
155 levels. thirst (polydipsia),
mg/dL, and 2 hour pc ● Assess feet for hunger
level temperature, (polyphagia), and
of 130 mg/dL pulses, color, increased urination
and sensation. (polyuria). The patient
● Assist the may also report
patient in nonspecific symptoms
identifying of
eating patterns fatigue and blurred
that need to be vision.
modified. ● A lot of drugs can
● Review the cause
progress toward fluctuations in blood
DEPENDENT: glucose as a side effect.
● Administer basal Beta-blockers,
and prandial corticosteroids, thiazide
insulin, as diuretics, estrogen,
ordered by the isoniazid, lithium, and
physician. phenytoin can cause
COLLABORATION: hyperglycemia. Regular
● Refer to a use of salicylates,
registered disopyramide, insulin,
dietitian for sulfonylurea agents,
individualized and
diet instruction pentamidine can cause
hypoglycemia.
Normal fasting blood
glucose for an adult is
70
to 105 mg/dL. Critical
values for
hypoglycemia
are less than 40 to 50
BAP
mg/dL. Critical values
for
hyperglycemia are
greater
than 400 mg/dL.
● This is to monitor
peripheral perfusion
and
neuropathy.
● This information
provides
the basis for
individualized dietary
instruction related to
the
clinical condition that
contributes to
fluctuation
in blood glucose levels.
● Patient involvement
in the
treatment plan
enhances
adherence to treatment
plan
● Adherence to the
therapeutic regimen
promotes tissue
perfusion.
Keeping glucose in the
normal range slows
progression of
microvascular disease.
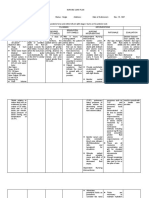
DEPENDENT:
● An individualized
meal
BAP
plan depends on the
patient’s body, weight,
blood glucose values,
activity patterns, and
specific clinical
condition.
Modifications in the
patient’s food intake
will
contribute stabilization
of
blood glucose levels.
COLLABORATION:
● Specific exercises
can be
prescribed based on
any
physical limitations the
patient may have.
You might also like
- CT 11 - HPNDocument12 pagesCT 11 - HPNLycah RotoneNo ratings yet
- Hypertension Related To Faulty Eating Habits As Evidence My Blood Pressure of 13080.Document2 pagesHypertension Related To Faulty Eating Habits As Evidence My Blood Pressure of 13080.Senyorita KHayeNo ratings yet
- Readiness For Enhanced Health ManagementDocument6 pagesReadiness For Enhanced Health ManagementJIMENEZ, TRISHA MARIE D.No ratings yet
- PositionDocument23 pagesPositionCharlene RojasNo ratings yet
- Nursing Care Plan for Hypertension PatientDocument2 pagesNursing Care Plan for Hypertension PatientfahadNo ratings yet
- NCP HyperthermiaDocument2 pagesNCP HyperthermiaKirby ContaoiNo ratings yet
- Managing Pain and Mobility for a Postpartum PatientDocument3 pagesManaging Pain and Mobility for a Postpartum PatientGuillao LensNo ratings yet
- Nursing Care Plan For HypertensionDocument4 pagesNursing Care Plan For HypertensionKathleen Dimacali100% (2)
- Ncp Sgh DianaDocument2 pagesNcp Sgh Dianadaniloabautista44No ratings yet
- Managing Shortness of Breath in Rheumatic Heart DiseaseDocument3 pagesManaging Shortness of Breath in Rheumatic Heart DiseaseGail NamangdanNo ratings yet
- Community Health Nursing and Pharmacology Course Task #4Document3 pagesCommunity Health Nursing and Pharmacology Course Task #4Michelle Angela AlombroNo ratings yet
- Bernadas NCPDocument3 pagesBernadas NCPBernadas, Jhon Kristopher C.No ratings yet
- NCP KateDor NewDocument6 pagesNCP KateDor NewSteffi GolezNo ratings yet
- Decreased Cardiac OutputDocument5 pagesDecreased Cardiac Outputshuang81No ratings yet
- Case:: Bleeding Without PainDocument3 pagesCase:: Bleeding Without PainDarwin QuirimitNo ratings yet
- Cues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale EvaluationDocument2 pagesCues Nursing Diagnosis Analysis Goals & Objectives Intervention Rationale EvaluationMiggy SikatNo ratings yet
- Draft HTN 1 PDFDocument8 pagesDraft HTN 1 PDFAko ay Wala poNo ratings yet
- Nursing Care Plan for Acute Chest PainDocument3 pagesNursing Care Plan for Acute Chest PainMelDred Cajes BolandoNo ratings yet
- Nursing Care Plan For HELLP SyndromeDocument17 pagesNursing Care Plan For HELLP SyndromeRosemarie Carpio75% (4)
- Nursing Care Plan: St. Anthony's College San Jose, Antique Nursing Department Name: M.L.HDocument3 pagesNursing Care Plan: St. Anthony's College San Jose, Antique Nursing Department Name: M.L.HNicolne LorraineNo ratings yet
- NCP - Delivery RoomDocument8 pagesNCP - Delivery RoomAUBREY MARIE . GUERRERONo ratings yet
- NCP SGHDocument2 pagesNCP SGHdaniloabautista44No ratings yet
- Caro NCPDocument17 pagesCaro NCPAbegail PolicarpioNo ratings yet
- Assessing and Managing Cerebral Perfusion IssuesDocument3 pagesAssessing and Managing Cerebral Perfusion IssuesMicaela CrisostomoNo ratings yet
- Iloilo Doctors' College College of Nursing: West Avenue, Molo, Iloilo CityDocument2 pagesIloilo Doctors' College College of Nursing: West Avenue, Molo, Iloilo CityAudrie Allyson GabalesNo ratings yet
- NCP Chest PainDocument2 pagesNCP Chest PainCG Patron BamboNo ratings yet
- Group 1 - VITALS SIGNS and INTERVENTIONSDocument19 pagesGroup 1 - VITALS SIGNS and INTERVENTIONSTrishNo ratings yet
- Nursing Care Plan for Postpartum HemorrhageDocument4 pagesNursing Care Plan for Postpartum HemorrhageEliza PejanNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale Evaluation Subjective: IndependentDocument3 pagesAssessment Diagnosis Planning Implementation Rationale Evaluation Subjective: IndependentKoulene GuimbanganNo ratings yet
- Nursing Care Plan: Acute PainDocument4 pagesNursing Care Plan: Acute PainEvet VaxbmNo ratings yet
- Medical Diagnosis: Acute Myocardial Infarction: A 66-Year-Old Male August 13, 2005 10 PM ER Unit Possible MIDocument1 pageMedical Diagnosis: Acute Myocardial Infarction: A 66-Year-Old Male August 13, 2005 10 PM ER Unit Possible MIBadri AlthubaityNo ratings yet
- NCP - Preeclampsia (A)Document6 pagesNCP - Preeclampsia (A)Ronel ResurricionNo ratings yet
- NCP Chest PainDocument2 pagesNCP Chest PainLinsae Troy50% (2)
- ASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoDocument1 pageASSESSMENT S: "Nanghihina Ako, Hindi Ko Magawa Yung Mga GustoCherie MayNo ratings yet
- Assessment 2003Document3 pagesAssessment 2003Senyorita KHayeNo ratings yet
- Drug Study And NCP OutlineDocument3 pagesDrug Study And NCP Outlinerobertvaliente471No ratings yet
- Scientific Explanation of Expected Outcomes and InterventionsDocument4 pagesScientific Explanation of Expected Outcomes and InterventionsGensen Cu RoxasNo ratings yet
- NCP & DSDocument4 pagesNCP & DSKyla Marie TejadaNo ratings yet
- Nursing Care Plan For HypertensionDocument5 pagesNursing Care Plan For HypertensionJessy MalloNo ratings yet
- NCP #1 Ineffective Cerebral Tissue PerfusionDocument4 pagesNCP #1 Ineffective Cerebral Tissue PerfusionsteffiNo ratings yet
- Subjective: " " Sto: Diagnostics: Sto:Goal MET: VitalDocument3 pagesSubjective: " " Sto: Diagnostics: Sto:Goal MET: VitalKarl KiwisNo ratings yet
- Adrian G. Mallar BSN 2 Focus: Chest Pain Nursing Care Plan - Rheumatic Heart DiseaseDocument3 pagesAdrian G. Mallar BSN 2 Focus: Chest Pain Nursing Care Plan - Rheumatic Heart DiseaseFarzana AfrinNo ratings yet
- NURSING CARE PLAN FOR CHEST PAIN AND VOMITINGDocument2 pagesNURSING CARE PLAN FOR CHEST PAIN AND VOMITINGApril Kate BanagodosNo ratings yet
- Nursing Care Plan For Subarachnoid HemorrhagicDocument2 pagesNursing Care Plan For Subarachnoid HemorrhagicAshram Smart100% (1)
- Nursing Care Plan For Subarachnoid HemorrhagicDocument2 pagesNursing Care Plan For Subarachnoid HemorrhagicAshram Smart0% (1)
- Nursing Care Plan Related To Pospartum HemmorhageDocument5 pagesNursing Care Plan Related To Pospartum HemmorhageAsmin BalahNo ratings yet
- Nursing Care Plan Format X1Document3 pagesNursing Care Plan Format X1Ramiel ChristopherNo ratings yet
- Activity 5Document4 pagesActivity 5AngieNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument5 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationBiway RegalaNo ratings yet
- NCP FormatDocument4 pagesNCP FormatCoreen Kaye TanNo ratings yet
- Marcos Er NCPDocument1 pageMarcos Er NCPAssasination ClassroomNo ratings yet
- Geria Day 2 NCP 2Document5 pagesGeria Day 2 NCP 2karl davidNo ratings yet
- N U R S I N G Care Plan For AterosclerosiDocument2 pagesN U R S I N G Care Plan For AterosclerosiRoxy TofyNo ratings yet
- Angiography (Cardiac Catherization) : Patient Teaching/preparationDocument2 pagesAngiography (Cardiac Catherization) : Patient Teaching/preparationpsyNo ratings yet
- Retained PlacentaDocument22 pagesRetained PlacentaLeander Isabelle NoolNo ratings yet
- Assessing and Treating Impending Thyroid StormDocument4 pagesAssessing and Treating Impending Thyroid StormRenie SerranoNo ratings yet
- Nursing Care Plan for Mr. Hulu's Fluid Volume DeficitDocument4 pagesNursing Care Plan for Mr. Hulu's Fluid Volume DeficitMariel GamaloNo ratings yet
- Heart of the Field "Refresher & Nha Certification Quick Notes"From EverandHeart of the Field "Refresher & Nha Certification Quick Notes"No ratings yet
- Nursing EssayDocument1 pageNursing EssayLouie ParillaNo ratings yet
- Endotracheal Intubation Learning MaterialDocument8 pagesEndotracheal Intubation Learning MaterialLouie ParillaNo ratings yet
- NCP Risk For Electrolyte ImbalanceDocument3 pagesNCP Risk For Electrolyte ImbalanceLouie ParillaNo ratings yet
- Clinical Face Sheet: Category of PatientDocument21 pagesClinical Face Sheet: Category of PatientLouie ParillaNo ratings yet
- VACCINEDocument1 pageVACCINELouie ParillaNo ratings yet
- Mental HealthDocument1 pageMental HealthLouie ParillaNo ratings yet
- Malignant Bowel ObsDocument2 pagesMalignant Bowel ObsLouie ParillaNo ratings yet
- Diagnosis Bowel ObstructionDocument1 pageDiagnosis Bowel ObstructionLouie ParillaNo ratings yet
- SCENARIODocument2 pagesSCENARIOLouie ParillaNo ratings yet
- Nephrectomy: The Advantages of Laparoscopic Surgery IncludeDocument5 pagesNephrectomy: The Advantages of Laparoscopic Surgery IncludeLouie ParillaNo ratings yet
- Bowel ObstructionDocument2 pagesBowel ObstructionLouie ParillaNo ratings yet
- Disaster ManagementDocument1 pageDisaster ManagementLouie ParillaNo ratings yet
- MANAGEMENTDocument4 pagesMANAGEMENTLouie ParillaNo ratings yet
- Bowel ObstructionDocument1 pageBowel ObstructionLouie ParillaNo ratings yet
- Covid EssayDocument1 pageCovid EssayLouie ParillaNo ratings yet
- COLONDocument2 pagesCOLONLouie ParillaNo ratings yet
- Anatomy and Physiology According to Organism LevelDocument2 pagesAnatomy and Physiology According to Organism LevelLouie ParillaNo ratings yet
- StressDocument1 pageStressLouie ParillaNo ratings yet
- Myths About CovidDocument1 pageMyths About CovidLouie ParillaNo ratings yet
- DRUG STUDY - wARDDocument9 pagesDRUG STUDY - wARDLouie ParillaNo ratings yet
- Pathophysiology: Interstitial FiltrationDocument3 pagesPathophysiology: Interstitial FiltrationLouie ParillaNo ratings yet
- HISTORYDocument1 pageHISTORYLouie ParillaNo ratings yet
- Genital WartsDocument2 pagesGenital WartsLouie ParillaNo ratings yet
- Assignment HistoryDocument5 pagesAssignment HistoryLouie ParillaNo ratings yet
- NAT 1stDocument1 pageNAT 1stLouie ParillaNo ratings yet
- Anatomy and Physiology Female ReproductiveDocument2 pagesAnatomy and Physiology Female ReproductiveLouie ParillaNo ratings yet
- HivDocument1 pageHivLouie ParillaNo ratings yet
- DocumentDocument2 pagesDocumentLouie ParillaNo ratings yet
- Med CardsDocument2 pagesMed CardsLouie ParillaNo ratings yet
- Essay On FriendsDocument1 pageEssay On FriendsLouie ParillaNo ratings yet
- KROK 2 1 профиль (315 Q 2004-2005)Document54 pagesKROK 2 1 профиль (315 Q 2004-2005)Ali ZeeshanNo ratings yet
- SPDX311 LEC - 03 ElectrocardiographyDocument6 pagesSPDX311 LEC - 03 Electrocardiographywootzu1No ratings yet
- Reduce Ami- TctmdDocument4 pagesReduce Ami- Tctmdlakshminivas PingaliNo ratings yet
- Portal HypertensionDocument18 pagesPortal Hypertensionsara82vetNo ratings yet
- CSDocument74 pagesCSSimina ÎntunericNo ratings yet
- Local Anesthetics - Blockers K+ Channel Blockers Ca2+ Channel BlockersDocument4 pagesLocal Anesthetics - Blockers K+ Channel Blockers Ca2+ Channel Blockersmed testNo ratings yet
- The ESC Handbook of Cardiovascular Rehabilitation 2020Document225 pagesThe ESC Handbook of Cardiovascular Rehabilitation 2020Daboin ZambranoNo ratings yet
- Acyanotic Congenital Heart DiseaseDocument7 pagesAcyanotic Congenital Heart DiseaseSam Raj100% (1)
- Koran Pasien PJT LT4 2 Feb 2023Document9 pagesKoran Pasien PJT LT4 2 Feb 2023maspul lamuruprintNo ratings yet
- Written Report Coronary Heart DiseaseDocument5 pagesWritten Report Coronary Heart DiseaseJade WushuNo ratings yet
- Vital Sign AssessmentDocument48 pagesVital Sign Assessmentapi-271649833No ratings yet
- Infectious Diseases of The HeartDocument84 pagesInfectious Diseases of The HeartHarold DiasanaNo ratings yet
- The Prognostic Value of Exercise Capacity: A Review of The LiteratureDocument9 pagesThe Prognostic Value of Exercise Capacity: A Review of The Literaturekelika anamikaNo ratings yet
- Embryology Cardiovascular System For WebDocument22 pagesEmbryology Cardiovascular System For WebMiyoko HatushiNo ratings yet
- TutorialDocument18 pagesTutorialEllya Syahfitri 2108125983No ratings yet
- Building A Clinical Cardiothoracic Surgical Program: A Multi-Institutional ModelDocument4 pagesBuilding A Clinical Cardiothoracic Surgical Program: A Multi-Institutional Modelnouha jhiderNo ratings yet
- Materi DR Rita Zahara NewDocument31 pagesMateri DR Rita Zahara NewIrfanNo ratings yet
- Cordis Case Study PDFDocument29 pagesCordis Case Study PDFsingh242No ratings yet
- Bio Case Study 2Document21 pagesBio Case Study 2unknownNo ratings yet
- Cardiomyopathy: Restrictive Heart DiseaseDocument18 pagesCardiomyopathy: Restrictive Heart DiseaseMitch GabuyaNo ratings yet
- 1) Vasoplegia During Cardiac Surgery Current Concepts and Management 2010Document5 pages1) Vasoplegia During Cardiac Surgery Current Concepts and Management 2010Carolina QuirogaNo ratings yet
- Cardiac Arrythmias in The ED Menbeu Edited From AnaDocument106 pagesCardiac Arrythmias in The ED Menbeu Edited From AnaTemesgen Geleta100% (1)
- Freebie Bundle-50 Pages. PDFDocument63 pagesFreebie Bundle-50 Pages. PDFMaria Conchita Traya100% (1)
- ECG Cookbook: Answer DiagnosisDocument2 pagesECG Cookbook: Answer DiagnosisShayma ShamoNo ratings yet
- Anatomy and PhysiologyDocument6 pagesAnatomy and PhysiologyJulianne B. Dela CruzNo ratings yet
- Coarctation of AortaDocument19 pagesCoarctation of AortaMustafa SayedNo ratings yet
- Antihypertensive Drug LongDocument21 pagesAntihypertensive Drug Longa.muhsinNo ratings yet
- Goals and Objectives of ICU-1Document3 pagesGoals and Objectives of ICU-1Jack GuccioneNo ratings yet
- Chapter 28 Treatment of HypertensionDocument11 pagesChapter 28 Treatment of HypertensionMark Johnuel DuavisNo ratings yet
- Article - CVD Cardiac Arrest - Bls AclsDocument2 pagesArticle - CVD Cardiac Arrest - Bls AclsAkhosh SomarajanNo ratings yet