Professional Documents
Culture Documents
NCP KateDor New
Uploaded by
Steffi GolezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP KateDor New
Uploaded by
Steffi GolezCopyright:
Available Formats
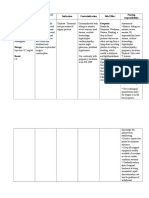
Jugo, Kate Guillan A.
Lavadia, Dorothy Rose D.
ASSESSMEN NURSING
PLANNING DIAGNOSTICS RATIONALE INTERVENTION RATIONALE EVALUATION
T DIAGNOSIS
Subjective: Cardiogenic Short term: 1. 12-lead 1. Detect the Independent: Short term:
Occupation: Shock related After 8 hours of ECG electrical 1. Monitor blood 1. Alteration in blood After 8 hours of
electrician to Tachy- nursing activity of the pressure, apical pulse, pressure and differences nursing intervention,
Unconsciou arrhythmia intervention, the heart and peripheral pulses. in equality, rate, and the patient:
s w/ labored patient will: measure the regularity of pulses are Manifested
breathing Manifest timing and indicative of the effect of normal cardiac
Erythemato normal duration of altered cardiac output on rhythm as
us face cardiac each electrical systemic/peripheral evidenced by a
Singed rhythm as phase in your circulation. normal 12-lead
eyebrows, evidenced by heartbeat. 2. Monitor vitals signs. 2. Although not all ECG reading
eyelashes a normal 12- 2. To record the Assess adequacy of dysrhythmias are life- Was free from
and hair lead ECG 2. Holter heart's activity cardiac output/ tissue threatening, immediate signs of
Thick white reading monitor as one goes perfusion, noting treatment may be cardiogenic
leathery Be free from about their significant variations in required to terminate shock.
eschar on signs of routine for a BP/pulse rate equality, dysrhythmia in the
the whole cardiogenic long period of respirations, changes in presence of alterations in Long term:
upper shock. time. skin color/temperature, cardiac output and tissue After 3 weeks of
extremities 3. Measure level of perfusion. nursing intervention,
Blisters on Long term: 3. Blood amounts of consciousness/sensoriu the patient:
anterior After 3 weeks chemistry certain m, and urine output Maintained
chest and of nursing test chemicals in a during episodes of adequate cardiac
neck intervention, the sample of dysrhythmias. output as
patient will: blood, 3. Investigate reports of 3. Reasons for chest pain evidenced by BP
Nausea
Maintain especially chest pain, are variable and depend and pulse within
adequate serum documenting location, on underlying cause. normal range,
Objective:
cardiac potassium, duration, intensity (0- However, chest pain may adequate urinary
HR: 142
output as calcium, 10 scale), and indicate ischemia due to output, palpable
bpm
evidenced by magnesium relieving/ aggravating altered electrical pulses of equal
BP: 80/50 and sodium. factors. Note nonverbal conduction, decrease
BP and pulse quality, normal
Hgb: 20 g/dl 4. Records the pain cues (e.g. facial myocardial perfusion, or
within normal level of
Hct: 52% 4. Electrocardi electrical grimacing, crying). increased oxygen need.
range, consciousness
Na: 150 ogram activity of your 4. Be prepared to initiate 4. Development of life-
adequate Displayed
mEq/L; urinary heart via cardiopulmonary threatening dysrhythmias absence of
126mEq/L output, electrodes resuscitation (CPR) as requires prompt dysrhythmias.
K: 3.2 attached to indicated. intervention to prevent
mEq/L; palpable your skin. If ischemic damage/death. Displayed no
6 mEq/L pulses of you have 5. Prepare for procedures: 5. Arterial lines are placed recurrence of
Pain: 10/10 equal quality, damaged heart Arterial Line or for invasive cardiogenic shock
Decreased normal level muscle, Central Line hemodynamic Restored
urine output of electric Placement, Gather all monitoring. They can sufficient cardiac
consciousnes problems or supplies, Ensure measure MAP, but can output to the
s fluid buildup consent is obtained by also measure other tissues.
Display around your provider, Explain hemodynamic values
absence of heart, it won't procedure to such as CO/CI, SVR, SV,
dysrhythmias. conduct patient/family, Prep etc. when using a
Display no electrical fluids or tubing, Ensure FloTrac machine.
recurrence of impulses all monitoring Central lines are
cardiogenic normally. equipment is available placed for administration
shock 5. Cardiac 5. To check the Intubation Notify of fluids and medications
Restore Catheterizati amount of Respiratory Therapist as well as hemodynamic
sufficient on blood your and Charge Nurse for monitoring of CVP,
cardiac heart is support, Suction and CO/CI, and SVR. Patients
output to the pumping with Ambu Bag at the with cardiogenic shock
tissues. each beat bedside, Gather may also receive a
(cardiac supplies, Ensure all Pulmonary Artery
output). monitoring equipment catheter (also called a
is available, Surgical Swan-Ganz catheter) for
Intervention, Follow more detailed invasive
facility procedures, hemodynamic
Remove all personal monitoring.
clothes, jewelry, etc., Patients whose airway
Ensure informed and/or ventilation has
consent is obtained by been compromised due to
provider, Facilitate ↓ LOC or pulmonary
transport edema may need to be
intubated and placed on a
ventilator.
Patients may need to
be taken to the OR to
repair the injury or
internal bleeding that
caused the hypovolemia
in the first place.
Informed consent
MUST be obtained by the
provider. You can explain
procedures to
patients/family, but the
provider must give the
reason, risks, benefits,
etc. and obtain the
informed consent.
Dependent: 1. Dysrhythmias are
1. Give the drug as generally treated
indicated such as symptomatically
intropic agents and
anti-dysrhythmias. You might be given
Inotropic Agents medications to improve
your heart function, such
as epinephrine
(Levophed) or dopamine,
until other treatments
start to work.
For systemic
Epinephrine (0.05- vasoconstriction and to
0.5mcg/kg/min) address tachycardia and
hypotension
2. For homeostasis and
2. Administer IV fluids as future administration of
ordered. emergency drugs.
3. Increases amount of
3. Administer oxygen available for
supplemental oxygen myocardial uptake,
as indicated. which decreases
irritability caused by
hypoxia.
Collaborative:
1. Monitor 1. Hemodynamic
Hemodynamics: MAP, measurements will tell us
CVP, CO, SVR, VO2 the severity of the shock
and how well the patient
is responding to
treatment.
MAP = Mean Arterial
Pressure - this is the
average pressure within
the arteries. It can be
calculated with a non-
invasive blood pressure,
but is more accurate
when measured by an
Arterial Line.
Decompensated shock
will show a decreasing
MAP below 60 mmHg
CVP = Central Venous
Pressure. This measures
Preload. In a patient with
cardiogenic shock, it will
be high (>12 mmHg).
The goal would be to see
this number return closer
to normal, but ultimately
the CO measurement is
more important.
CO = Cardiac Output. In
cardiogenic shock, the
overall CO takes the
biggest hit. The body
cannot compensate. The
goal of therapy is to
increase cardiac output,
so it needs to be
monitored closely. This
is assessed using a
FloTrac or Pulmonary
Artery catheter.
SVR = Systemic
Vascular Resistance.
This measures afterload.
We will expect this to be
high because of the
body’s attempts to
compensate through
vasoconstriction. If
treatment is effective, we
will see this number
return back down to
normal. Dobutamine can
also help to decrease this
number through
vasodilation.
VO2 Oxygen
consumption - the rate at
which oxygen is taken up
into the tissues. In
cardiogenic shock, we
will see this number
decrease significantly
because the tissues are
not getting the oxygen
they need. This is a
classic sign of
cardiogenic shock versus
heart failure (normal
2. Monitor and refer VO2)
laboratory results: 2.
Electrolytes
Imbalance of
electrolytes, such as
potassium, and
calcium adversely
affects cardiac rhythm
Drug levels and contractility.
Reveal therapeutic/
toxic level of
prescription
medications or street
drugs that may affect/
contribute to presence
3. Insert and maintain IV of dysrhythmias.
access. 3. Patent access line may be
required for
administration of
4. Prepare for the emergency drugs.
instillation of 4. Anticipation for possible
cardioversion machine occurrence of emergency
or defibrillator. cardiac dysrhythmias that
may lead to shock.
References:
Blood chemistry tests - Canadian Cancer Society. (n.d.). Retrieved from http://www.cancer.ca/en/cancer-information/diagnosis-and-treatment/tests-and-procedures/blood-
chemistry-tests/?region=on
Common Tests for Arrhythmia. (n.d.). Retrieved from https://www.heart.org/en/health-topics/arrhythmia/symptoms-diagnosis--monitoring-of-arrhythmia/common-tests-for-
arrhythmia.
Electrical Injuries in Emergency Medicine Clinical Presentation. (2018, September 04). Retrieved from https://emedicine.medscape.com/article/770179-clinical#b2.
Heart arrhythmia. (2017, December 27). Retrieved from https://www.mayoclinic.org/diseases-conditions/heart-arrhythmia/diagnosis-treatment/drc-20350674.
Nursing Care Plan for Heart Rhythm Disorders: Arrhythmia. (n.d.). Retrieved from http://nanda-diagnosis.blogspot.com/2015/04/nursing-care-plan-for-heart-rhythm.html.
Ventricular Dysrhythmias | Nursing Central. (n.d.). Retrieved from https://nursing.unboundmedicine.com/nursingcentral/view/Diseases-and-
Disorders/73741/all/Ventricular_Dysrhythmias.
You might also like
- Drug StudyDocument4 pagesDrug StudyXio PauNo ratings yet
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananNo ratings yet
- Duty Drug Study'sDocument7 pagesDuty Drug Study'sGrape JuiceNo ratings yet
- Atropine SulfateDocument1 pageAtropine SulfateTrishaaMayolNo ratings yet
- EsmololDocument2 pagesEsmololtherock316_995149No ratings yet
- Drug Study InsulinDocument2 pagesDrug Study InsulinGrant Kenneth Dumo AmigableNo ratings yet
- Vitamin KDocument2 pagesVitamin KMuvs RazonNo ratings yet
- ClonidineDocument2 pagesClonidineFlora Angeli PastoresNo ratings yet
- Atenolol Drug Study WWW RNpedia ComDocument3 pagesAtenolol Drug Study WWW RNpedia ComYuuki Chitose (tai-kun)No ratings yet
- BETAXOLOLDocument2 pagesBETAXOLOLjulieNo ratings yet
- Drug Study ON Atropine Sulfate: Maa Tripura College of Nursing, Jhabua (M.P.)Document3 pagesDrug Study ON Atropine Sulfate: Maa Tripura College of Nursing, Jhabua (M.P.)amitNo ratings yet
- Generic Name: Brand Name: Pletal: Pharmacologic Class: Pharmacokinetics General Indications Contraindications BeforeDocument2 pagesGeneric Name: Brand Name: Pletal: Pharmacologic Class: Pharmacokinetics General Indications Contraindications Beforeart_mutantNo ratings yet
- DioxelDocument1 pageDioxelJosselle Sempio CalientaNo ratings yet
- Drug Study ICUDocument5 pagesDrug Study ICUEcko MoawiaNo ratings yet
- Dutasteride 0.5mg + Tamsulosin HCL 0.4mg (Duodart)Document19 pagesDutasteride 0.5mg + Tamsulosin HCL 0.4mg (Duodart)ddandan_2No ratings yet
- Drug StudyDocument9 pagesDrug StudyJonica CamposNo ratings yet
- "Nahadlok Naman Ko Sa Akong Gipambati, Ning-Undang Ko Sakong Work As QHSE and Training Manager, Nagdecide Ko Muuli Sa Pilipinas. Pag-Uli Nako Last Week, Ginabati Nako Mura Ko Makulbaan" AsDocument4 pages"Nahadlok Naman Ko Sa Akong Gipambati, Ning-Undang Ko Sakong Work As QHSE and Training Manager, Nagdecide Ko Muuli Sa Pilipinas. Pag-Uli Nako Last Week, Ginabati Nako Mura Ko Makulbaan" Ashanna caballoNo ratings yet
- DRUG LactuloseDocument1 pageDRUG LactuloseJona Phie Domingo MonteroNo ratings yet
- Calcium Gluconate Drug StudyDocument4 pagesCalcium Gluconate Drug StudyAngelou Joefred CongresoNo ratings yet
- Drug - Htm#description.: Reference: Submitted By: Date Submitted: Submitted ToDocument2 pagesDrug - Htm#description.: Reference: Submitted By: Date Submitted: Submitted ToSHEILA MAE SACLOTNo ratings yet
- 66 Drug AnaDocument3 pages66 Drug AnaAlexa RoqueNo ratings yet
- F. Case Study Thesis-Drug Study (Revised)Document5 pagesF. Case Study Thesis-Drug Study (Revised)Lopirts NiganiNo ratings yet
- Drug StudyDocument17 pagesDrug StudyTherese ArellanoNo ratings yet
- Tramadol (Dolcet)Document1 pageTramadol (Dolcet)Beverly Ann de LeonNo ratings yet
- NafarinDocument2 pagesNafarinianecunar100% (2)
- Chronic Renal Failure Nursing Care PlanDocument6 pagesChronic Renal Failure Nursing Care PlanRuva Oscass JimmyNo ratings yet
- Amlodipine CPDocument2 pagesAmlodipine CPRose EchevarriaNo ratings yet
- Apixaban 5 PDFDocument2 pagesApixaban 5 PDFWanie Al-basriNo ratings yet
- Drug SDocument2 pagesDrug SJane CasiquinNo ratings yet
- Cefipime HCL (AXERA)Document2 pagesCefipime HCL (AXERA)Kristine YoungNo ratings yet
- SeroquelDocument2 pagesSeroqueldanaNo ratings yet
- IrbesartanDocument3 pagesIrbesartanapi-3797941No ratings yet
- Drug Study - OB WardDocument8 pagesDrug Study - OB WardCheska YsabelleNo ratings yet
- Drug Study ProglinDocument2 pagesDrug Study ProglinChris Denver BancaleNo ratings yet
- Final Magnesium SulfateDocument3 pagesFinal Magnesium SulfateGwyn RosalesNo ratings yet
- MultivitaminDocument1 pageMultivitaminAdrianne BazoNo ratings yet
- LacipilDocument2 pagesLacipilianecunarNo ratings yet
- Nursing Care Plan NCP Group 3 Fatigue ..Document2 pagesNursing Care Plan NCP Group 3 Fatigue ..Aerron Severus Secano ShuldbergNo ratings yet
- Drug AnalysisDocument3 pagesDrug AnalysisAnn Aquino100% (1)
- ApidraDocument4 pagesApidraRobert Ivan AgujarNo ratings yet
- Activated CharcoalDocument1 pageActivated CharcoalSupreeth PrasadNo ratings yet
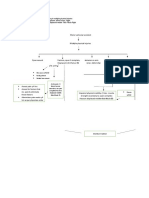
- Concept MapDocument2 pagesConcept Mapjunifer laynoNo ratings yet
- 9 Ketamine Drug StudyDocument7 pages9 Ketamine Drug Studyshadow gonzalezNo ratings yet
- Drug StudyDocument7 pagesDrug StudyHerwincayeNo ratings yet
- ItoprideDocument2 pagesItoprideLesValenzuelaNo ratings yet
- Sine CodDocument2 pagesSine CodshayneNo ratings yet
- IsoketDocument2 pagesIsoketJaessa FelicianoNo ratings yet
- 13 Areas of AssessmentDocument2 pages13 Areas of AssessmentCrystal Queen MarquezNo ratings yet
- Neurological Assessment Monitoring Sheet: C O M ADocument2 pagesNeurological Assessment Monitoring Sheet: C O M AAina HaravataNo ratings yet
- College of Nursing: Cebu Normal UniversityDocument3 pagesCollege of Nursing: Cebu Normal UniversityShiva TorinsNo ratings yet
- DRUG STUDY LevetiracetamDocument3 pagesDRUG STUDY LevetiracetamMaria Althea NajorraNo ratings yet
- Drug Study Cushing's SyndromeDocument5 pagesDrug Study Cushing's SyndromeSelena MarieNo ratings yet
- Decreased Cardiac OutputDocument4 pagesDecreased Cardiac OutputRenie SerranoNo ratings yet
- Decreased Cardiac OutputDocument3 pagesDecreased Cardiac OutputRizalyn QuindipanNo ratings yet
- Jake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersDocument8 pagesJake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersJake Yvan DizonNo ratings yet
- Bernadas NCPDocument3 pagesBernadas NCPBernadas, Jhon Kristopher C.No ratings yet
- NCP CardioDocument10 pagesNCP CardioCharles LigonNo ratings yet
- NCM 118 - Rle: College of Nursing 1 Semester AY 2021-2022Document4 pagesNCM 118 - Rle: College of Nursing 1 Semester AY 2021-2022cammel ramosNo ratings yet
- NCP Decreased Cardiac OutputDocument2 pagesNCP Decreased Cardiac OutputYamete KudasaiNo ratings yet
- Nursing Care Plan For HELLP SyndromeDocument17 pagesNursing Care Plan For HELLP SyndromeRosemarie Carpio75% (4)
- Ligon Joven NCP-1Document7 pagesLigon Joven NCP-1Steffi GolezNo ratings yet
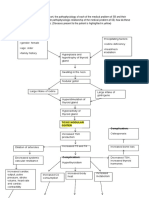
- Pathophysiology Number 3 and 4 4Document7 pagesPathophysiology Number 3 and 4 4Steffi GolezNo ratings yet
- Good Research PracticeDocument6 pagesGood Research PracticeSteffi GolezNo ratings yet
- Transformative Reflection CaDocument2 pagesTransformative Reflection CaSteffi GolezNo ratings yet
- NCP Case Analysis GastritisDocument7 pagesNCP Case Analysis GastritisSteffi GolezNo ratings yet
- Monthly Delcarmen BiblioDocument4 pagesMonthly Delcarmen BibliosteffiNo ratings yet
- Drug Ana RamDocument8 pagesDrug Ana RamSteffi GolezNo ratings yet
- (OT3L) ReflexesDocument4 pages(OT3L) ReflexesSteffi GolezNo ratings yet
- John Q EssayDocument1 pageJohn Q EssaySteffi GolezNo ratings yet
- Bio 308 Outline 21Document2 pagesBio 308 Outline 21Metehan KaraNo ratings yet
- Australasian Emergency Care: Jeremy Pallas, John-Paul SmilesDocument3 pagesAustralasian Emergency Care: Jeremy Pallas, John-Paul Smileszaenal abidinNo ratings yet
- Anidem Hw1Document2 pagesAnidem Hw1John Cromwell A. MedinaNo ratings yet
- Test Bank For Human Biology 15th Edition Sylvia Mader and Michael WindelspechtDocument21 pagesTest Bank For Human Biology 15th Edition Sylvia Mader and Michael Windelspechtjohnsmithysekamonit100% (23)
- Nursing Care Plan: Fahad Saad Alenzi 381007055 MA 60 HypertensionDocument2 pagesNursing Care Plan: Fahad Saad Alenzi 381007055 MA 60 HypertensionfahadNo ratings yet
- Photosynthesis WorksheetDocument2 pagesPhotosynthesis WorksheetYhannai FerronNo ratings yet
- Grade 10 Life Processes Part 1 Notes 2021-22Document4 pagesGrade 10 Life Processes Part 1 Notes 2021-22JAVED KHANNo ratings yet
- The Immune System - Test QuestionsDocument4 pagesThe Immune System - Test QuestionsflorinNo ratings yet
- Isotonic BeveragesDocument7 pagesIsotonic BeveragesAa 1989100% (1)
- Microbiology An Introduction 12th Edition Tortora Solutions Manual 1Document16 pagesMicrobiology An Introduction 12th Edition Tortora Solutions Manual 1robert100% (53)
- Dyspnea and CoughDocument70 pagesDyspnea and CoughLatha SukumarNo ratings yet
- Ebook Anesthesia Secrets 6Th Edition PDF Full Chapter PDFDocument67 pagesEbook Anesthesia Secrets 6Th Edition PDF Full Chapter PDFwendy.johnson850100% (28)
- JAtin ProjectDocument9 pagesJAtin ProjectAnonymousNo ratings yet
- Asthma FinalDocument71 pagesAsthma FinalVariya HemangiNo ratings yet
- Drug Study Ob WardDocument7 pagesDrug Study Ob WardKc DichosoNo ratings yet
- Breathing QuestionsDocument21 pagesBreathing QuestionsJosephine Charles HoNo ratings yet
- Technical Publication: H48651FE Direction KTI106019-100 Revision 4Document316 pagesTechnical Publication: H48651FE Direction KTI106019-100 Revision 4Tatiana Dayana BautistaNo ratings yet
- Levels of Structural Organization FinalDocument1 pageLevels of Structural Organization Finalmaxine janorasNo ratings yet
- Peringkat Borg Dari Pengerahan Persepsi: ObjektifDocument4 pagesPeringkat Borg Dari Pengerahan Persepsi: ObjektifMutmainnah MunirNo ratings yet
- ARDS QuizDocument6 pagesARDS QuizMeliza BancolitaNo ratings yet
- Metabolic Pathways Study Guide MyDocument12 pagesMetabolic Pathways Study Guide Myapi-521781723No ratings yet
- Blood GroupDocument1 pageBlood GroupgpsriramNo ratings yet
- Hubungan Jenis Packed Red Cell (PRC) Yang Ditransfusikan Dengan Reaksi Transfusi Febrile NonDocument5 pagesHubungan Jenis Packed Red Cell (PRC) Yang Ditransfusikan Dengan Reaksi Transfusi Febrile NonazizahNo ratings yet
- Organization of The Human BodyDocument8 pagesOrganization of The Human BodyAly HannahNo ratings yet
- Excretory Products and Their EliminationDocument6 pagesExcretory Products and Their Eliminationkanth3012No ratings yet
- Capstone Project 1Document13 pagesCapstone Project 1Pushpal BanerjeeNo ratings yet
- Connective Tissue ReportDocument7 pagesConnective Tissue ReportJess MCDNo ratings yet
- BIO 12 EX 6 BLOOD PRESSURE WorksheetDocument9 pagesBIO 12 EX 6 BLOOD PRESSURE WorksheetAnonymous TPCRxkw0jNo ratings yet
- Phinma - University of PangasinanDocument2 pagesPhinma - University of PangasinanRonnie De Vera IINo ratings yet
- Properties of Cardiac Muscle and Conducting SystemsDocument38 pagesProperties of Cardiac Muscle and Conducting Systemsnirilib100% (4)