Professional Documents
Culture Documents
CNS Tumor Map 2020 Full
Uploaded by
Alves de MeloOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CNS Tumor Map 2020 Full
Uploaded by
Alves de MeloCopyright:
Available Formats
= Low grade
CNS TUMOR MAP, 2020 REVISION WITH 2016 WHO
E = EGBs = Enhancing b = BRAF alteration * Tumor summaries below may not necessarily state the formal WHO Prepared by C. Krishnan, MD
= Grade III preferred terminology, in the name of brevity. Ref: WHO Tumors of the CNS
= Seizures = Cyst+mural nodule i = IDH1/2 mutation
LEGEND
(4th rev 2020)
DESIGNATIONS AND MOLECULAR INTEGRATION
= Grade IV # Not all CNS tumors are described here. Specifically, this chart will not
R = Rosenthals = Calcifications o = 1p/19q co-del = Ungraded address meningiomas, CNS lymphomas or mesenchymal tumors.
INFANT HIGH-GRADE GLIOMA I ANGIOCENTRIC GLIOMA ASTROBLASTOMA II PLEOMORPHIC XANTHOASTROCYTOMA III GLIOBLASTOMA, EPITHELIOID GLIOBLASTOMA (IDH MUT) GLIOBLASTOMA (IDH WT)
Usually embryonal “PNET-like” histology. Subtly infiltrative, spindle cell tumor with elongated Well defined tumor arranged in radial “rosettes” with Cellular tumor with epithelioid cells, sometimes lipidized Infiltrative tumor with epithelioid eosinophilic cells +/- Infiltrative glial tumor with: hypercellularity, mitoses, Infiltrative glial tumor with: hypercellularity,
cells radially arranged around vessels - akin to broad bases. Prominent vascular hyalinization. Can have and vascular proliferation. Less pronounced necrosis. mitoses, pseudopalisading necrosis and vascular
MX
MX
Sometimes papillary, rosetted or spindled growth with multinucleation & nuclear inclusions. Frequent rhabdoid change. May have lipidzed cells, ala PXA. Zonal
MX
MX
MX
MX
MX
patterns. Occasionally lower-grade glial pattern. E ependymomatous rosettes papillary like formation. Occasional necrosis. perivascular lymphocytes and reticulin. necrosis and +/- MV proliferation. E Often arising from lower grade glioma proliferation. Small cell var = minimal atypia
E
POS (if mutated): ALK1, panNTRK, ROS1 POS: GFAP, MYB, EMA (dot-like) POS: GFAP (var), S100, Ki67 (<20%), Ker (var) POS: GFAP, BRAF V600E, MAP2 (var), CD34 (var) POS: S100, GFAP (patchy), EMA/CK (focal), BRAF POS: GFAP, IDH1 R132H, p53 POS: GFAP, IDH1 R132H, p53, S100, focal INI-1 loss
R R
IHC
IHC
IHC
IHC
IHC
IHC
IHC
NEG: retained INI1/BRG1 NEG:Ki67 (<5%), Synap, p53, IDH1 NEG: IDH1 NEG: p16 null (usually), IDH1 NEG: H3K27M, CK5/6, retained INI1/BRG1 NEG: H3K27M, ATRX, IDH1 (if alternative mutation) NEG: H3K27M, CK5/6
HGG pattern: ALK / ROS / NTRK / MET alterations IDH1 wildtype. BRAF V600E (50%) IDH1 R132X mutated or IDH2 R172K mutated IDH1 wildtype, TERT promoter mut., EGFR alterations
MYB (6q23) alterations or rearrangements aCGH: gains of 19 and 20q
MOL
MOL
MOL
BRAF mut (80%), CDKN2A del (60%)
MOL
MOL
MOL
MOL
LGG pattern: ALK alterations only No H3K27M or SMARCB1/B4 mutations Additionally: TP53 mut, ATRX mut, MGMT hypermeth (esp in small cell var.), TP53 mut
Usually don’t have H3K27M or BRAF mutations Ependymoma, pilomyxoid astrocytoma, astroblastoma Malignant var: anaplastic, >5 mites, palisading necr. Grade 3 = >5 mitoses & necrosis | Epithelioid GBM Related to anaplastic PXA or may arise from Gr2PXA IDH-wt GBM, IDH-mut anaplastic astro Epithelioid GBM, Oligodendroglioma (small cell var)
DDX
DDX
i
DDX
DDX
DDX
DDX
DDX
b i i
S
U PEDIATRIC LOW-GRADE GLIOMA, ALK
FUSION I
DESMOPLASTIC INFANTILE
ASTRO/GANGLIO
I DNET
Glioneuronal tumor with oligo-like cells in vertical
?I PLNTY I PAPILLARY GLIONEURONAL TUMOR
Low-grade biphasic glioneuronal tumor arranged in
P
Glial tumor with piloid cells, set among prominent
MX
Glial or glio-neuronal tumor with moderate rows, mucoid microcysts and “floating” neurons. pseudopapillae surrounding hyalinzed vessels. Intervening
MX
MX
Triphasic tumor: glial cyst wall, desmoplastic vasculature and heavy calcification
cellularity and mild atypia. High-grade Can have distinct glioma areas & separate FCD (IIIa) ganglionic cells with neuropil.
MX
embryonal mural nodule +/- ganglion cell
MX
R
versions also exist. component.
Oligo-like: POS: S100, OLIG2, CD34 (focal) POS: Synap, CD34 (strong) POS: GFAP and S100 (glial); OLIG2 (var), Synap
IHC
IHC
IHC
NEG: GFAP (in oligo-like), IDH1 NEG: Cga, IDH1, GFAP (mostly) , Ki67 usu low NEG: CgA
POS: GFAP, Alk,
A
POS GFAP, reticulin fibres, Synap (neurons),
IHC
IHC
NEG: Ki67 (very low) desmin (rare)
i FGFR2-CTNNA3 fusions
MOL
BRAF mut (30%), Chr 5 and 7 gains (30%) SLC44A1-PRKCA fusion in most
MOL
MOL
T
Alk-fusions: PPP1CB-Alk and rare other Rare aneuploidy. Rare BRAF V600E mutations.
MOL
MOL
partners No BRAF-fusions or TP53 mutations Pilocytic astrocytoma, DNET, ganglioglioma
o
DDX
Pilocytic astro, oligodendroglioma, ganglioglioma Ependymoma, AVM
DDX
DDX
i II III II III EXTRAVENTRICULAR NEUROCYTOMA
E PLNTY, Ganglioglioma ASTROCYTOMA OLIGODENDROGLIOMA II
DDX
Embryonal tumors, ganglioglioma, pilocytic astro
DDX
Cellular astrocytic, fibrilar neoplasm with mild to moderate Infiltrating gliomas with round, “fried-egg” cells in Round cell neurocytic tumor with prominent
N intralesional vessels and pseudorosettes.
MX
nuclear atypia, angulated nuclei + hyperchromasia. No necrosis delicate chicken-wire vasculature background. Grade 3
MX
MX
DICER1-ASSOCIATED CNS SARCOMA allowed. = Incr. mitoses + Microvasc prolif + necrosis Oligo-like with occasional gangliod differentiation.
GANGLIOGLIOMA
I
T CNS EMBRYONAL TUMORS, GENETICALLY High-grade spindle cell neoplasm with PPB-like
III
Disorganized, variably cellular lesion with glial and neuronal POS: GFAP, TP53, IDHR132H (80%) POS: IDHR132H (90%), ATRX (retained), S100, OLIG2 POS: Synap
IHC
IHC
IHC
NEG: Cga, IDH1, GFAP (mostly) , Ki67 usu low
MX
component. Look for binucleated and dysplastic neurons. NEG: ATRX (loss) NEG: GFAP (mostly)
MX
pattern, eosinophilic globules and ~ rhabdo cells.
O DEFINED Perivascular lymphocytes.
POS: Desmin (focal), nyogenin (focal) (80%) IDH1/2 mut & TP53 mut + ATRX mut
o IDH1/2 mut + co-del 1p/19q | Often: CIC & TERT mut. o Rarely co-del 1p/19q. FGFR1-TACC1 fusions
E
MOL
MOL
MOL
POS (Neuron): MAP2, Synap, BRAF V600E, CD34 Never IDH1/2 mutation or BRAF V600E mutation
MGMT promoter methylation (50%) NEG: mutations in ATRX or TP53
IHC
R
IHC
Many genetically defined embryonal tumors look similar to one NEG: GFAP, Olig2, Synap, INI1 (retained) Rarely: H3K27M in non-infiltrative, temporal cases
another: Oligodendroglioma, DNET, ganglioglioma, PGNT
i Grade 3 = Hypercellular + increased mitoses Neurocytoma, clear cell ependymoma, DNET, Pilocytic
DDX
DDX
DDX
Bi-allelic DICER1 mutations BRAF V600E (~50%), BRAF fusions (rarely)
i i i
MOL
MOL
I
NO IDH1/2 mutations (excludes this diagnosis)
1. CNS NB-FOXR2: Resembles CNS neuroblastoma, ganglionic nodules
Embryonal tumors, GBM, AT/RT
DDX
DNET, Oligodendroglioma, co-existing FCD (type IIIb)
DDX
b
A
2. CNS HGNET-MN1: Solid + pseudopapillary tumor, resembles
MX
astroblastoma
L
3. CNS HGNET-EFT-CIC: Can resemble EWS ATYPICAL TERATOID/RHABDOID TUMOR EMBRYONAL TUMOR WITH MULTILAYERED
4. CNS HGNET-BCOR: Glial looking w/ rosettes or ependymoma-like ROSETTES
5. CNS HGG-ALK/ROS/NTRK Supratentorial > infratentorial & midline Cerebellar > Midline/Posterior fossa.
Polyphenotypic, hypercellular embryonal tumor with
II EPENDYMOMA (SUPRATENTORIAL)
MX
Embryonal tumor with layered rosettes and islands of
MX
rhabdoid and ocasional anaplastic cells. nucleus free neuropil
Can be papillary or clear cell morphology. Clear cell =
CNS NB-FOXR2: Olig2, Synaptophysin, GFAP POS: LIN28 (strong & diffuse), Synap (neuropil) III arranged in cellular groups with perinuclear halos, focal
MX
POS: INI1 or BRG1 (aberrant loss), GFAP (foca)
IHC
IHC
CNS HGNET-MN1: GFAP NEG: INI1 (retained), GFAP perivascular rosettes.
CNS HGNET-EFT-CIC: NUT1 SMARCB1 > SMARCA4 alterations. Mut >> deletions POS: FOXJ1, GFAP, S100, EMA (dot-like)
IHC
IHC
C19MC-altered
MOL
In SP-RELA: Cyclin-D1, L1CAM, p16 null
MOL
33% germline
CNS HGNET-BCOR: GFAP, B-cat (nuc), BCOR
ST-EPN-RELA: C11orf95-RELA fusion, Chromothripsis
MOL
All embryonal tumors in children
DDX
Embryonal tumors, anaplastic ependymoma, CPC
DDX
CNS HGG-ALK/ROS/NTRK: ALK1, ROS1, NTRK ST-EPN-YAP1: YAP1 fusions
Oligodendroglioma, neurocytoma, hemangioblastoma
DDX
PINEOCYTOMA PINEAL PARENCHYMAL TUMOR OF
PAPILLARY TUMOR OF PINEAL REGION
PINEOBLASTOMA ? II I ? II INTERMEDIATE DIFFERENTIATION
H3G34R mut
CNS NB-FOXR2: Intrachromosomal rearrangement, FOXR2 upreg.
More often
Embryonal, hypercellular tumor of pineal region ? III Biphasic solid and papillary tumor with Moderately cellular round cell tumor growing in
? III
Two patterns: Diffuse neurocytoma-like and
CNS HGNET-MN1: Various fusion partners ependymoma-like pattern, hyalinized vessels and sheets and multilayered (pineocytomatous) lobulated/nested pattern w/ distinct vessels. More
MX
MX
MX
with focal rosette formation. Often invasive and
MX
occasional PAS+ cytoplasmic globules neuropil rosettes, set among rich vasculature. cellular and occasional dysplastic gangloid cells.
CNS HGNET-EFT-CIC: CIC-NUTM1 fusion disseminated.
MOL
CNS HGNET-BCOR: BCOR ITD exon 15 DIFFUSE MIDLINE HIGH-GRADE GLIOMA, H3K27M POS: Synap (var), NF (focal), CgA (focal) POS: Keratins (AE1/3, CAM5/2, CK18), GFAP (var) POS: Synap, NF, MAP2 (var), CgA (var) POS: Synap, NF, CgA (var)
IHC
IHC
IHC
IHC
M
NEG: INI1 & BRG1 (retained) NEG: NF, Syanp (focal), CgA (focal) NEG: GFAP, S100 NEG: GFAP, S100, NeuN
CNS HGG-ALK/ROS/NTRK: Various fusion partners across all
E
Infiltrative tumor involving midline nuclei or brainstem.
I
Monomorphic tumor cells with variable morphology RB1 deletion, DICER1 mutation
MOL
MX
aCGH: del 10, + 4. PTEN alteration occasional No relevant diagnostic molecular genetic profile aCGH: gains of 4q, 12q and loss of 22
MOL
MOL
MOL
resembling pilocytic astro to GBM.
R
D
All embryonal tumors of childhood, AT/RT
DDX
DDX
Ependymoma, Germ cell tumor, Metastasis PPTID, EV neurocytoma, Germinoma Pineoblastoma, Germinoma,
DDX
DDX
POS: GFAP (var), H3K27M, OLIG2, MAP2
IHC
NEG: retained INI1/BRG1, CGA, ATRX, OLIG2
LI H3K27M mutation (midline), H3G34R (hemispheric) i
N
MOL
PILOMYXOID ASTROCYTOMA TP53 (50%), PDGRFA amp. PILOCYTIC ASTROCYTOMA
I
Astrocytic tumor with elongated processes, biphasic
E Piloid astrocytic tumor with subtle angiocentric growth, Related to anaplastic PXA or may arise from Gr2PXA density, microcysts and occasional multinucleation. Low ANAPLASTIC ASTROCYTOMA WITH
DDX
MX
myxoid background & microcysts.
E PILOID FEATURES
MX
mitoses. +/- Vasc prolif, Leptomening. spread
Variable mitotic activity. +/- Pilocytic-like areas
Cellular, moderately pleomorphic infiltrative tumor
I
POS: GFAP, ~OLIG2, BRAF (hemispheric)
with pilocytic morphology, vascular proliferation
IHC
MX
POS: GFAP, S100, ~CD34, Ki67 (up to 20% labeling)
R
NEG: p53, IDH1/2
R and focal areas of necrosis.
N
IHC
NEG: BRAF V600E, H3K27M Posterior fossa; KIAA1549-BRAF fusion
MOL
F
Cortex/Midline: BRAF mut, FGFR1 (5%), NTRK (~5%)
E POS: GFAP
IHC
Rarely can have BRAF rearrangement NEG: ATRX (loss), IDH1, H3K27M
MOL
R Pilomyxoid (no EGBs/ Rs), Oligodendo., DNET
DDX
b Defined by methylation studies. Characteristic:
A
MOL
DDX
Pilocytic astrocytoma, Angiocentric glioma NF1/BRAF alterations + del ATRX + del CDKN2A
T MEDULLOBLASTOMA EPENDYMOMA (PF) Pilocytic astrocytoma, IDH-wt GBM
DDX
II i
E Embryonal tumor with variable nodules of neuronal
Monomorphic glioma arranged in rosettes with ?I DYSPLASTIC CEREBELLAR GANGLIOCYTOMA
III CEREBELLAR LIPONEUROCYTOMA
N perivascular anuclear zones. Can have dense Expansion of molecular and internal granule layers
II
MX
MX
differentiation. Cerebellum and 4th ventricle
cellularity, focal necrosis and hemorrhage with variably sized ganglionic cells that preserves
MX
T overall architecture. Cerebellar version of neurocytoma with prominent
MX
POS: Synap, MAP2, p53, B-Cat (WNT),, GAB1 (SHH) POS: FOXJ1, GFAP, S100, EMA (dot-like) neoplastic adipocyte-like component.
O
IHC
IHC
NEG: GFAP, INI1 (retained) H3K27me3: Lost in EPN-A, Retained in EPN-B POS: Syna
IHC
NEG: PTEN (loss in adult cases) POS: Synap, NeuN, MAP2, GFAP (focal)
R
IHC
4 molecular groups: PF-EPN-A: Few copy # changes, CpG-me + NEG: Ki67 (usu <10%)
MOL
WNT - Older children, some adults. PF-EPN-B:Chromosomal instability, Cpg-me - Adult: PTEN mutations (Cowden syndrome)
I
TP53 mutation (20%),
MOL
SHH - Often hemispheric & Desmoplastic/EN. TP53 Children: no PTEN mutations
MOL
MOL
mut confers worse prognosis No BRAF or IDH mutations
A
Choroid plexus tumor, Medulloblastoma, Metastasis
DDX
G3/4 - Infants/children. Large/anaplasia & MYC amp
DDX
Ganglioglioma, Glioneuronal tumors Astrocytomas, lipid-rich SFT?
DDX
i
L
B I
MYXOPAPILLARY EPENDYMOMA
II EPENDYMOMA (SPINAL CORD)
R & ?II
Typically found in distal spinal cord. Radially arranged
tumor cells in papillary / balloon arrangement around III
Often Tanycytic morphology: Monomorphic glioma in
A
MX
spinal cord growing as spindle cell fascicles with
MX
myxoid substance. elongated nuclei. Rosettes typically subtle.
I C POS: GFAP, S100, CD99, Ker AE1/3 POS: FOXJ1, GFAP, S100, EMA (dot-like)
IHC
IHC
NEG: CK5/6, CK7, CK20, EMA, Ki67 (<1%) NEG:
N O Whole chromosome aneuploidy Frequent NF2 mutations, del Chr 22
S R
MOL
MOL
MYCN amplification (more aggressive variant)
T D Metastatic papillary tumors (adult), Chordoma Pilocytic astrocytoma, Schwannoma, Met.
DDX
DDX
E
M
V I CHOROID PLEXUS TUMOR MYXOID GLIONEURONAL TUMOR DIFFUSE LEPTOMENINGEAL TUMOR CENTRAL NEUROCYTOMA SUBEPENDYMOMA
CHOROID PLEXUS CARCINOMA I SUBEPENDYMAL GIANT CELL TUMOR I ROSETTE FORMING GLIONEURONAL TUMOR
I II CHORDOID GLIOMA OF 3RD VENTRICLE
E II Intraventricular round cell neurocytic tumor with
N Malignant intraventricular tumor w/ sheet-like II Papillary tumor with delicate fronds with crowded
cuboidal cells. Atypical = >2/10 mits + incr.
Circumscribed glio-neuronal tumor with large
gemistocyic or ganglion-type cells. Mitoses, tumor
DNET-like tumor arising in septum
E
Oligodendroglial-like tumor with predominant
leptomeningeal growth pattern and lesser
Biphasic solid-cystic, tumor: neurocytic rosettes
and piloid astrocytic components. Neurocytic
prominent intralesional vessels and pseudorosettes.
Ventricular tumor. Clusters of small nuclei
arranged in fibrillar matrix with occasional
Solid neoplasm w/ cords and nests of epithelioid
tumor cells. Lymphoplasmacytic infiltrates present.
MX
MX
MX
MX
MX
MX
MX
growth, focal papillary formation, necrosis and brain pellucidum > lateral ventricles.
MX
T
Anaplastic cytology = “atypical central
invasion. Usu freq. Mitoses. cellularity, pleomoprh., solid growth and/or necrosis. lymphocytes and hyalinized vessels present. ganglion cell / neuropil component
R rosettes surround neuropil core. b microcysts. Rarely forming rosettes. Mucinous stroma common. Rarely fibrotic.
R
MX
R
Myxoid stroma, microcysts and neurocytoma”.
R POS: CK7, p53 (50%) POS: CK7, TTR, S100 (var) POS: GFAP, S100, Synap (var), NeuN (var) rosette-formations. POS: OLIG2, MAP2, S100, GFAP (focally) POS: Neurocytic = Synap, MAP2; Glial = GFAP POS: Synap, NeuN, MAP2 POS: GFAP POS: GFAP, TTF-1, CD34, Ker (var), S100 (var)
IHC
IHC
IHC
IHC
IHC
IHC
IHC
IHC
NEG: EMA, NeuN, IDH1
I NEG: S100, TTR, EMA, INI1 (Retained) NEG: CK20, EMA (weak) NEG: CD34 NEG: BRAF V600E, IDH1/2 NEG: Cga, GFAP, Ki67 usu <2%. If >2% = “atypical” NEG: EMA, Ki67 (<1%) NEG: P53 (weak), Synapto, IDH1
POS: OLIG2, MAP2, S100, GFAP (focal)
i
IHC
C TSC1 and TSC2 mutations common NEG: CD34, NeuN, IDH1 KIAA-BRAF fusion (75%), del 1p (50%), rare FGFR1 mut, PIK3CA mut in some aCGH: 11q13 and 9p21 losses.
MOL
Germline TP53 mut (40%) aCGH: hyperdiploidy. MGMT promoter methylation aCGH: copy # alterations, MYCN amplification Not really relevant
MOL
MOL
MOL
MOL
MOL
MOL
MOL
60% sporadic, 40% TS syndromic 1p/19q del. No BRAF V600E or IDH1/2. No BRAF alterations or IDH1/2 mutations No TP53 mutations
L
DDX
E
Defined by PDGFRA K385I/L mutation Oligodendroglioma, Pilocytic astro, PXA
b i
MOL
Anaplastic ependymoma, Embryonal tumors CP carcinoma, Endolymphatic sac tumor, Metastasis Ganglioglioma, PXA (if not obviously near ventricle) Pilocytic astro, neurocytoma, Oligodendroglioma Ependymoma, Pineocytoma Ependymoma variants Metastasis, Chordoma.
DDX
DDX
DDX
DDX
DDX
DDX
DDX
o o
S
0 - 24 months 2- 20 years 20-50 years > 50 years
You might also like
- VolvoTD70 Service Manual EngineDocument110 pagesVolvoTD70 Service Manual EngineHeikki Alakontiola87% (47)
- Load Considerations and Design Based Residual HazardsDocument1 pageLoad Considerations and Design Based Residual HazardssabeerNo ratings yet
- Application Form For Nationals Csec 2018 and InstructionsDocument7 pagesApplication Form For Nationals Csec 2018 and InstructionsCassidy ChaitramNo ratings yet
- Instant Assessments for Data Tracking, Grade 3: MathFrom EverandInstant Assessments for Data Tracking, Grade 3: MathRating: 5 out of 5 stars5/5 (2)
- DAPHNE GREASE MP NO.2Document8 pagesDAPHNE GREASE MP NO.2sanusi.pdkmNo ratings yet
- Father Dámaso: María Clara Quotes in Noli Me TangereDocument11 pagesFather Dámaso: María Clara Quotes in Noli Me TangereSilver ArgentNo ratings yet
- Heat LoadDocument41 pagesHeat LoadpanyamnrNo ratings yet
- Level 3 General Arrangement Plan: A B C D E F G Suspended Slab NotesDocument1 pageLevel 3 General Arrangement Plan: A B C D E F G Suspended Slab NotesSubhekshya ShresthaNo ratings yet
- PVH Ambulance Worksheet For EMR - VeterinaryDocument1 pagePVH Ambulance Worksheet For EMR - VeterinaryMercedes Araujo SolarNo ratings yet
- Lecture 11 SlidesDocument15 pagesLecture 11 SlidesDanishNo ratings yet
- Mapping On Sheet S2-10 - 03-23-2021Document1 pageMapping On Sheet S2-10 - 03-23-2021gv Sathishkumar KumarNo ratings yet
- Distribution Board Internal Wiring-ModelDocument1 pageDistribution Board Internal Wiring-ModelGarlapati TrinadhNo ratings yet
- Type A1 First Floor CSD Sign Off - Submittal #174Document2 pagesType A1 First Floor CSD Sign Off - Submittal #174nuraishah zulkifliNo ratings yet
- RILEM TC QFS Quasibrittle Fracture Scaling and Size Effect'-Final ReportDocument22 pagesRILEM TC QFS Quasibrittle Fracture Scaling and Size Effect'-Final ReportsonalisarayNo ratings yet
- Warning: Wiring DiagramDocument3 pagesWarning: Wiring DiagramEnmanuel J AriasNo ratings yet
- Summary Training HESDocument8 pagesSummary Training HESyeremia 75No ratings yet
- Precautionary Boil Water AdvisoryDocument9 pagesPrecautionary Boil Water AdvisoryWXYZ-TV Channel 7 DetroitNo ratings yet
- Bus Shelter India (Made From Scrap-Steel+aluminium+rubber+plastic)Document2 pagesBus Shelter India (Made From Scrap-Steel+aluminium+rubber+plastic)vanshaj mehtaNo ratings yet
- Major993502x12.2pscslab V5 Approve P12Document1 pageMajor993502x12.2pscslab V5 Approve P12rushi123No ratings yet
- Shop materials for confidential plumbing projectDocument1 pageShop materials for confidential plumbing projectJohn SmitNo ratings yet
- Delaware SussexDocument1 pageDelaware SussexIgor SemenovNo ratings yet
- Material Point Method: Theory and Applica3onsDocument35 pagesMaterial Point Method: Theory and Applica3onsyin hoe ongNo ratings yet
- ELElDocument1 pageELElALEENA ASLAMNo ratings yet
- Phasing PlanDocument1 pagePhasing PlanNEWS CENTER MaineNo ratings yet
- Crazy For Christmas: Bert AppermontDocument10 pagesCrazy For Christmas: Bert Appermontsofia canoNo ratings yet
- PEDWPRTS771025A1 - Main Compressor B Train 1 - 5Document1 pagePEDWPRTS771025A1 - Main Compressor B Train 1 - 5macielNo ratings yet
- 21057423-Cs-csd-5000-0040 Weighing Scale Control Room Structural and Foundation Detail Drawing Rev.0Document1 page21057423-Cs-csd-5000-0040 Weighing Scale Control Room Structural and Foundation Detail Drawing Rev.0arjunNo ratings yet
- Ampeg Pf500 Main Power Supply 2034544-01-c02-SchDocument2 pagesAmpeg Pf500 Main Power Supply 2034544-01-c02-SchManuel CoutoNo ratings yet
- STCT-ILV-SHC-PL-AD03-REV24-AD3-4 cd2Document1 pageSTCT-ILV-SHC-PL-AD03-REV24-AD3-4 cd2Giancarlo Manrique VillarrealNo ratings yet
- Shop Materials Confidential Use OnlyDocument1 pageShop Materials Confidential Use OnlyAlam MD SazidNo ratings yet
- Isometric View Lifting Detail: NotesDocument2 pagesIsometric View Lifting Detail: NotesRajveer SinghNo ratings yet
- Instrument Reference Chart v4Document2 pagesInstrument Reference Chart v4Rosie Chase100% (6)
- Orchestration Ranges PDFDocument2 pagesOrchestration Ranges PDFzeuta1100% (1)
- Amphi TheatreDocument1 pageAmphi TheatreanzaniNo ratings yet
- Manhole Dimensions D B: 7' X 7' Square Concrete NO. 3 Manhole StandardDocument1 pageManhole Dimensions D B: 7' X 7' Square Concrete NO. 3 Manhole StandardAlinda Gupta AbhroNo ratings yet
- See, See, The Word Is IncarnateDocument20 pagesSee, See, The Word Is IncarnateLopezNo ratings yet
- C536400001v00e2 - Facility Plot Plan Isf Site Plan PDFDocument1 pageC536400001v00e2 - Facility Plot Plan Isf Site Plan PDFmostafa essamNo ratings yet
- STR BnderDocument6 pagesSTR Bnderhemanthkumar67008No ratings yet
- Lower Ground Floor Slab R/F Detail Restaurant Building (C3, C4 Block)Document1 pageLower Ground Floor Slab R/F Detail Restaurant Building (C3, C4 Block)Sampath S. WickramanayakaNo ratings yet
- RFI 225 Back-Up DCE ResponseDocument3 pagesRFI 225 Back-Up DCE ResponsePurushotam TapariyaNo ratings yet
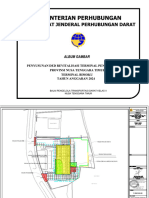
- 1 DED Peningkatan Revitalisasi Terminal Tipe A BimokuDocument52 pages1 DED Peningkatan Revitalisasi Terminal Tipe A BimokuHakim fauziNo ratings yet
- Interconnection Diagram XL-200 - 110V PDFDocument1 pageInterconnection Diagram XL-200 - 110V PDFOluas OlivNo ratings yet
- Investor FlyerDocument2 pagesInvestor FlyerffxNo ratings yet
- OB Containment LayoutDocument1 pageOB Containment LayoutShahul HameedNo ratings yet
- Kafd A1 111 Comn BF1 XXXXX SHP Arc Asb 00023Document1 pageKafd A1 111 Comn BF1 XXXXX SHP Arc Asb 00023YazNo ratings yet
- CRISTO DE LA PRESENTACION Clarinete 1ºDocument1 pageCRISTO DE LA PRESENTACION Clarinete 1ºJAIMENo ratings yet
- DMH5Document1 pageDMH5Keyvin dela CruzNo ratings yet
- General Arrangement of PilingDocument8 pagesGeneral Arrangement of PilingPNo ratings yet
- Drawing 2.Document1 pageDrawing 2.tiyaniNo ratings yet
- Red-Line Ne 2311000024 - FiberDocument1 pageRed-Line Ne 2311000024 - FiberMohamed F. AbdullahNo ratings yet
- Kanawat Zoning MapDocument1 pageKanawat Zoning MapLOKUT LocapNo ratings yet
- StandardDocument1 pageStandardAyesha jabeenNo ratings yet
- ReleaseNote - FileList of X441MAR - 2009 - X64 - V1.00Document7 pagesReleaseNote - FileList of X441MAR - 2009 - X64 - V1.00Johanis.WNo ratings yet
- R02i16 Wsu XX ZZ DWG ST 33012 PDFDocument1 pageR02i16 Wsu XX ZZ DWG ST 33012 PDFSanjay LohodasanNo ratings yet
- A B J N Q: Semi - Basement Floor Plan - Overall PlanDocument6 pagesA B J N Q: Semi - Basement Floor Plan - Overall PlanKevin LowNo ratings yet
- S19091 DIB NASJV PK1 MOS IFC A AAR 04 GF 00 0000 02 ReplyDocument1 pageS19091 DIB NASJV PK1 MOS IFC A AAR 04 GF 00 0000 02 ReplyMohammed Aleem UddinNo ratings yet
- HSE Standard Guidelines for Injury Treatment Register Doc 08.05Document1 pageHSE Standard Guidelines for Injury Treatment Register Doc 08.05dalNo ratings yet
- 08.05 Injury Record RegisterDocument1 page08.05 Injury Record RegisterdalNo ratings yet
- Date Name Nature of Injury Cause of Injury DR Referred To / Days OffDocument1 pageDate Name Nature of Injury Cause of Injury DR Referred To / Days OffdalNo ratings yet
- Instant Assessments for Data Tracking, Grade 2: MathFrom EverandInstant Assessments for Data Tracking, Grade 2: MathNo ratings yet
- Instant Assessments for Data Tracking, Grade 1: Language ArtsFrom EverandInstant Assessments for Data Tracking, Grade 1: Language ArtsNo ratings yet
- Anatomia Del TalloDocument24 pagesAnatomia Del TallofrancyNo ratings yet
- Dissection Manual Karl StorzDocument80 pagesDissection Manual Karl StorzazadutNo ratings yet
- Operative Compared With Nonoperative Treatment of A Thoracolumbar Burst Fracture Without Neurological DeficitDocument9 pagesOperative Compared With Nonoperative Treatment of A Thoracolumbar Burst Fracture Without Neurological DeficitAlves de MeloNo ratings yet
- Bohl 2017Document12 pagesBohl 2017Alves de MeloNo ratings yet
- Protocolo HsaeDocument19 pagesProtocolo HsaeAlves de MeloNo ratings yet
- What's Here?: 5 LevelsDocument3 pagesWhat's Here?: 5 LevelsTamara Anita LimaNo ratings yet
- Aula 4 - Vancouver Style How To Cite ReferencesDocument16 pagesAula 4 - Vancouver Style How To Cite ReferencesAlves de MeloNo ratings yet
- Exame Do RNDocument7 pagesExame Do RNAlves de MeloNo ratings yet
- ABI D Arapiraca JVUDocument5 pagesABI D Arapiraca JVUAlves de MeloNo ratings yet
- How Are You Today? What's Your Name? What Old Are You? Do You Have Any Brothers or Sisters? Where Are You From?Document12 pagesHow Are You Today? What's Your Name? What Old Are You? Do You Have Any Brothers or Sisters? Where Are You From?Alves de MeloNo ratings yet
- UK-India Coffee Market ReportDocument27 pagesUK-India Coffee Market ReportNikhil MunjalNo ratings yet
- 3edited My Class Note 1 On Blood BankDocument46 pages3edited My Class Note 1 On Blood BankmatewosNo ratings yet
- How to Give a Woman the Most Powerful OrgasmDocument10 pagesHow to Give a Woman the Most Powerful OrgasmFederico Ceferino BrizuelaNo ratings yet
- GatesDocument188 pagesGatesMilos LIcko Bash RandjelovicNo ratings yet
- AISC Design Guide 27 - Structural Stainless SteelDocument159 pagesAISC Design Guide 27 - Structural Stainless SteelCarlos Eduardo Rodriguez100% (1)
- Applications of Proton Exchange Membrane Fuel CellDocument20 pagesApplications of Proton Exchange Membrane Fuel CellRiri SasyNo ratings yet
- The Impact of ProstitutionDocument6 pagesThe Impact of ProstitutionLea TanNo ratings yet
- Module 6 - Accounting Cycle 1 - Recording Business Transactions and Accounting For Service Entities - Part BDocument29 pagesModule 6 - Accounting Cycle 1 - Recording Business Transactions and Accounting For Service Entities - Part BAbelNo ratings yet
- MBR-STP Design Features PDFDocument7 pagesMBR-STP Design Features PDFManjunath HrmNo ratings yet
- MEP Design ConsultancyDocument54 pagesMEP Design ConsultancyIshan Ranganath67% (3)
- Chemical Reactions and Equations: Multiple Choice QuestionsDocument8 pagesChemical Reactions and Equations: Multiple Choice QuestionsSahana karpagamNo ratings yet
- Roofing Section Guide for QCS 2014Document5 pagesRoofing Section Guide for QCS 2014Galfarqatar MEPNo ratings yet
- Importance of That Identified Strength in The OrganizationDocument2 pagesImportance of That Identified Strength in The OrganizationClarissa TeodoroNo ratings yet
- Cessna 208 (B) Caravan I T.T.R.Document7 pagesCessna 208 (B) Caravan I T.T.R.Junior Mebude SimbaNo ratings yet
- Alkana-1Document61 pagesAlkana-1ayundhaNo ratings yet
- Mental HealthDocument146 pagesMental HealthAnggraeni Beti Dwi LestariNo ratings yet
- AcetophenoneDocument3 pagesAcetophenonepriteshpatNo ratings yet
- Census of India 2011 Village and Town Level Data for Purba Champaran District, BiharDocument368 pagesCensus of India 2011 Village and Town Level Data for Purba Champaran District, BiharRahul SharmaNo ratings yet
- Dokumen - Tips Daewoo Service Manual Instrument Cluster Matiz-2023Document23 pagesDokumen - Tips Daewoo Service Manual Instrument Cluster Matiz-2023urexalg AlgériaNo ratings yet
- 17 Subcon RequirementsDocument38 pages17 Subcon RequirementsMohammed MinhajNo ratings yet
- Sri Venkateswara Caterers Tiffin MenuDocument4 pagesSri Venkateswara Caterers Tiffin MenuJPDGLNo ratings yet
- Toxicological Effects of Extracts of The Leaves of Scoparia Dulcis On The Brain ofDocument5 pagesToxicological Effects of Extracts of The Leaves of Scoparia Dulcis On The Brain ofFrancis AbuludeNo ratings yet
- Smoke & Ventilation CalculationsDocument7 pagesSmoke & Ventilation CalculationsZine ModelsNo ratings yet
- 10 DNA Testing Myths Busted, and Other Favorite Posts: by Blaine T. BettingerDocument11 pages10 DNA Testing Myths Busted, and Other Favorite Posts: by Blaine T. BettingerSexy888No ratings yet
- Sixth CommandmentDocument26 pagesSixth CommandmentJewel Anne RentumaNo ratings yet
- Dengue Fever in The PhilippinesDocument27 pagesDengue Fever in The PhilippinesDale Marie RenomeronNo ratings yet
- Quality Operating Process: Manual of Operations Care of PatientsDocument4 pagesQuality Operating Process: Manual of Operations Care of PatientsPrabhat KumarNo ratings yet