Professional Documents
Culture Documents
Ana Uri
Uploaded by
STEM-G.04 Kiarrah Katrina Botin0 ratings0% found this document useful (0 votes)
8 views3 pagesThe urinary system works to eliminate waste from the body through urine. It regulates water balance, electrolytes, acid-base balance, and blood pressure. The kidneys contain nephrons which filter blood to form urine. Filtration occurs in the glomerulus, and reabsorption and secretion occur along the renal tubule as urine is formed and collected to exit through the ureters, bladder, and urethra. The urinary system works with hormones to precisely regulate water and electrolyte balance in the body.
Original Description:
Original Title
Ana Uri.docx
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe urinary system works to eliminate waste from the body through urine. It regulates water balance, electrolytes, acid-base balance, and blood pressure. The kidneys contain nephrons which filter blood to form urine. Filtration occurs in the glomerulus, and reabsorption and secretion occur along the renal tubule as urine is formed and collected to exit through the ureters, bladder, and urethra. The urinary system works with hormones to precisely regulate water and electrolyte balance in the body.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views3 pagesAna Uri
Uploaded by
STEM-G.04 Kiarrah Katrina BotinThe urinary system works to eliminate waste from the body through urine. It regulates water balance, electrolytes, acid-base balance, and blood pressure. The kidneys contain nephrons which filter blood to form urine. Filtration occurs in the glomerulus, and reabsorption and secretion occur along the renal tubule as urine is formed and collected to exit through the ureters, bladder, and urethra. The urinary system works with hormones to precisely regulate water and electrolyte balance in the body.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
The Urinary System ● Capillaries are covered with podocytes from the renal
Functions of the Urinary System tubule
● Elimination of waste products ● The glomerulus sits within a glomerular capsule (the first
− Nitrogenous wastes part of the renal tubule)
− Toxins ● Enclosed by Bowman’s capsule
− Drugs
● Regulate aspects of homeostasis
− Water balance Renal Tubule
− Electrolytes ● Glomerular (Bowman’s) capsule
− Acid-base balance in the blood ● Proximal convoluted tubule (PCT)
− Blood pressure ● Loop of Henle
− Red blood cell production (erythropoietin) ● Distal convoluted tubule (DCT)
− Activation of vitamin D
Types of Nephrons
Organs of the Urinary system ● Cortical nephrons – more common
● Kidneys − Located entirely in the renal cortex
● Ureters − Includes most nephrons
● Urinary bladder – hypogastric region ● Juxtamedullary nephrons
● Urethra – outlet of urine − Found at the boundary of the cortex and medulla
− Loop of Henle in the renal medulla
Location of the Kidneys
● Against the dorsal body wall Peritubular Capillaries
● At the level of T12 to L3 ● Arise from efferent arteriole of the glomerulus
● The right kidney is slightly lower than the left ● Normal, low pressure capillaries
● Attached to ureters, renal blood vessels, and nerves at ● Attached to a venule
renal hilus- a medial indentation ● Cling close to the renal tubule
● Atop each kidney is an adrenal gland ● Reabsorb some substances from collecting tubes
Coverings of the Kidneys Urine Formation Processes
● Renal capsule ● Filtration – glomerular
− Surrounds each kidney − Glomerulus and Bowman’s capsule
● Adipose capsule ● Reabsorption – tubular
− Surrounds the kidney − PCT, renal tubule, peritubular capillaries
− Provides protection to the kidney ● Secretion – tubular
− Helps keep the kidney in its correct location
Filtration
Regions of the Kidney ● Nonselective passive process
● Renal cortex – outer region ● Water and solutes smaller than proteins are forced
● Renal medulla – inside the cortex through capillary walls
● Renal pelvis – inner collecting tube ● Blood cells cannot pass out to the capillaries
● Filtrate is collected in the glomerular capsule and leaves
Kidney Structures via the renal tubule
● Medullary pyramids – triangular regions of tissue in the
medulla Reabsorption
● Renal columns – extensions of cortex-like material inward ● The peritubular capillaries reabsorb several materials
● Calyces – cup-shaped structures that funnel urine − Some water − Amino acids
towards the renal pelvis − Glucose − Ions
Blood Flow in the Kidneys ● Some reabsorption is passive, most is active
aorta → renal artery → segmental artery → lobar artery → ● Most reabsorption occurs in the PCT
interlobar artery → arcuate artery → interlobular artery → afferent ● Materials not reabsorbed
arteriole → glomerulus (capillaries) → efferent arteriole → − Nitrogenous waste products − Creatinine
peritubular capillaries → interlobular vein → arcuate vein → − Excess water − Urea
interlobar vein → renal vein → inferior vena cava − Uric acid
Nephrons
● The structural and functional units of the kidneys Secretion – Reabsorption in Reverse
● Responsible for forming urine ● Some materials move from the peritubular capillaries
● Main structures of the nephrons into the renal tubules
− Glomerulus − Hydrogen and potassium ions and Creatinine
− Renal tubule ● Materials left in the renal tubule move toward the ureter
Glomerulus – filtering ability Flow of Urine
● A specialized capillary bed Medullary pyramid → minor calyx → major calyx →renal
● Attached to arterioles on both sides (maintains high pelvis → ureter → urinary bladder → urethra
pressure)
− Large afferent arteriole Characteristics of Urine Used for Medical Diagnosis
− Narrow efferent arteriole
● Colored somewhat yellow due to the pigment urochrome Distribution of Body Fluid
(from the destruction of hemoglobin) ● Intracellular fluid (inside cells)
● Sterile ● Extracellular fluid (outside cells)
● Slightly aromatic − Interstitial fluid
● Normal pH of around 6 − Blood plasma
● Specific gravity of 1.001 to 1.035
− Pyuria – fat cells (UTI)
− Glycosuria – diabetic The Link between Water and Salt
− Bacteriuria – UTI ● Changes in electrolyte balance causes water to move
− Bilirubinuria – hepatitis from one compartment to another
− Proteinuria – pregnant women ● Alters blood volume and blood pressure
− Hemoglobinuria – exaggerated RBC ● Can impair the activity of cells
− Hematuria – kidney stones or trauma
Maintaining Water Balance
Ureters ● Water intake must equal water output
● Slender tubes attaching the kidney to the bladder ● Sources for water intake
− Continuous with the renal pelvis − Ingested foods and fluids
− Enter the posterior aspect of the bladder − Water produced from metabolic processes
● Peristalsis aids gravity in urine transport ● Sources for water output
− Vaporization out of the lungs
Urinary Bladder − Lost in perspiration
● Temporarily stores urine − Leaves the body in the feces
● Trigone – three openings − Urine production
− Two from the ureters ● Dilute urine is produced if water intake is excessive
− One to the urethra ● Less urine (concentrated) is produced if large amounts of
● Wall water are lost
− Three layers of smooth muscle (detrusor muscle) ● Proper concentrations of various electrolytes must be
− Mucosa made of transitional epithelium present
− Walls are thick and folded in an empty bladder
− Bladder can expand significantly without increasing Regulation of Water and Electrolyte Reabsorption
internal pressure ● Regulation is primarily by hormones
− Antidiuretic hormone (ADH) prevents excessive
Urethra water loss in urine
● Thin-walled tube that carries urine from the bladder to − Aldosterone regulates sodium ion content of
the outside of the body by peristalsis extracellular fluid (blood volume ↑ pressure ↑)
● Release of urine is controlled by two sphincters ● Triggered by the renin-angiotensin-aldosterone
− Internal urethral sphincter (involuntary) mechanism
− External urethral sphincter (voluntary) ● Vasoconstriction
● Peripheral assistance ↑ blood pressure ↑
Urethra Gender Differences
● Length Maintaining Acid-Base Balance in Blood
− Females – 3–4 cm (1 inch) ● Blood pH must remain between 7.35 and 7.45 to
− Males – 20 cm (8 inches) maintain homeostasis
● Location − Alkalosis – pH above 7.45
− Females – along wall of the vagina − Acidosis – pH below 7.35
− Males – through the prostate and penis ● Most ions originate as byproducts of cellular metabolism
● Function ● Most acid-base balance is maintained by the kidneys
− Females – only carries urine ● Other acid-base controlling systems
− Males – carries urine; passageway for sperm cells − Blood buffers
− Respiration
Micturition (Voiding) Blood Buffers
● Both sphincter muscles must open to allow voiding ● Molecules react to prevent dramatic changes in hydrogen
− The internal urethral sphincter is relaxed after ion (H+) concentrations
stretching of the bladder − Bind to H+ when pH drops
− Activation is from an impulse sent to the spinal cord − Release H+ when pH rises
and then back via the pelvic splanchnic nerves ● Three major chemical buffer systems
− The external urethral sphincter must be voluntarily − Bicarbonate buffer system
relaxed − Phosphate buffer system
Maintaining Water Balance − Protein buffer system
● Normal amount of water in the human body
− Young adult females – 50% The Bicarbonate Buffer System
− Young adult males – 60% ● Mixture of carbonic acid (H2CO3) and sodium bicarbonate
− Babies – 75% (NaHCO3)
− Old age – 45% ● Bicarbonate ions (HCO3–) react with) strong acids to
● Water is necessary for many body functions and levels change them to weak acids
must be maintained ● Carbonic acid dissociates in the presence of a strong base
to form a weak base and water
Respiratory System Controls of Acid-Base Balance
● Carbon dioxide in the blood is converted to bicarbonate
ion and transported in the plasma
● Increases in hydrogen ion concentration produces more
carbonic acid
● Excess hydrogen ion can be blown off with the release of
carbon dioxide from the lungs
● Respiratory rate can rise and fall depending on changing
blood pH
Renal Mechanisms of Acid-Base Balance
● Excrete bicarbonate ions if needed
● Conserve or generate new bicarbonate ions if needed
● Urine pH varies from 4.5 to 8.0
Developmental Aspects of the Urinary System
● Functional kidneys are developed by the third month
● Urinary system of a newborn
− Bladder is small
− Urine cannot be concentrated
● Control of the voluntary urethral sphincter does not start
until age 18 months
● Urinary infections are the only common problems before
old age
Aging and the Urinary System
● There is a progressive decline in urinary function
● The bladder shrinks with aging
● Urinary retention is common in males
You might also like
- Kidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandKidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Anaphy FinalDocument22 pagesAnaphy FinalMa Sofiya Yazmin OroñaNo ratings yet
- Chapter 15 - URINARY SYSTEM PDFDocument8 pagesChapter 15 - URINARY SYSTEM PDFRishelle Mae Miñoza PilonesNo ratings yet
- Lymphatics and Lymph Circulation: Physiology and PathologyFrom EverandLymphatics and Lymph Circulation: Physiology and PathologyRating: 4 out of 5 stars4/5 (1)
- Excretory Products & Their Elimination PowernotesDocument2 pagesExcretory Products & Their Elimination PowernotesSushmit SrivastavaNo ratings yet
- UrologyDocument28 pagesUrologybuzz QNo ratings yet
- Bio 208 Urinary SystemDocument121 pagesBio 208 Urinary SystemNazir RabiuNo ratings yet
- 1.1 Renal Physiology 1Document8 pages1.1 Renal Physiology 1Carmela MarianoNo ratings yet
- Lecture 11 - Urinary SystemDocument64 pagesLecture 11 - Urinary SystemmaecabauatanNo ratings yet
- Anatomy and Physiology RenalDocument5 pagesAnatomy and Physiology RenalMaryGeneville Opeña AbitNo ratings yet
- Urinary System: BS-Radiologic Technology 2-1Document47 pagesUrinary System: BS-Radiologic Technology 2-1Julia Stefanel PerezNo ratings yet
- VII - Urinary SystemDocument2 pagesVII - Urinary SystemGael QuingNo ratings yet
- Excretory SystemDocument3 pagesExcretory Systemden mNo ratings yet
- Histology of The Urinary SystemDocument116 pagesHistology of The Urinary SystemSandra OnceNo ratings yet
- Urinary System PearsonsDocument13 pagesUrinary System Pearsonsblando.shaneNo ratings yet
- Urinary SystemDocument3 pagesUrinary Systemshanelhello1No ratings yet
- Urinary System Ch.18Document3 pagesUrinary System Ch.18Bulda, Princess Kaye R.No ratings yet
- The Urinary System Functions of The Urinary System: © 2018 Pearson Education, Ltd. 1Document13 pagesThe Urinary System Functions of The Urinary System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- Lecture 8 Urinary SystemDocument46 pagesLecture 8 Urinary SystemKang MonNo ratings yet
- ANAPHY Urinary System ReviewerDocument11 pagesANAPHY Urinary System ReviewerMARIDEN AYSONNo ratings yet
- Analysis of Urine & Body Fluids Lecture - : Sison The Kidney AnatomyDocument7 pagesAnalysis of Urine & Body Fluids Lecture - : Sison The Kidney AnatomyCherry BlossomNo ratings yet
- The Urinary System Functions of The Urinary System: © 2018 Pearson Education, Inc. 1Document13 pagesThe Urinary System Functions of The Urinary System: © 2018 Pearson Education, Inc. 1Stef FieNo ratings yet
- The Urinary SystemDocument34 pagesThe Urinary Systemaarti HingeNo ratings yet
- Urinary SystemDocument3 pagesUrinary SystemJake SimNo ratings yet
- Urogenital Guide Notes PDFDocument26 pagesUrogenital Guide Notes PDFJoryn LimNo ratings yet
- SEHH2234 2021 S2 Ch16 Urinary System StudentsDocument58 pagesSEHH2234 2021 S2 Ch16 Urinary System Studentsmiki leeNo ratings yet
- Renal PhysiologyDocument73 pagesRenal PhysiologyYosief DemissieNo ratings yet
- 2 - Renal PhysiologyDocument8 pages2 - Renal PhysiologyKunware TropaNo ratings yet
- KIDNEYDocument3 pagesKIDNEYBaJo GarnaceNo ratings yet
- Urinary SystemDocument32 pagesUrinary SystemDr Anais AsimNo ratings yet
- Urinary SystemDocument55 pagesUrinary SystemChristian UdaundoNo ratings yet
- Urinary System (Renal System) : Arba Pramundita RamadaniDocument36 pagesUrinary System (Renal System) : Arba Pramundita RamadaniReeds Riko Renjer RivaiNo ratings yet
- Urinary SystemDocument99 pagesUrinary SystemHarshika KDGNo ratings yet
- Urinary SystemDocument40 pagesUrinary SystemAlyssa AlferezNo ratings yet
- Urinary SystemDocument10 pagesUrinary SystemAly HannahNo ratings yet
- RenalSystem Part 1 (Spring2020)Document49 pagesRenalSystem Part 1 (Spring2020)Sahil ParikhNo ratings yet
- Urinary SystemDocument36 pagesUrinary SystemguintogeorgetteNo ratings yet
- Happ Finals Week 16-2Document7 pagesHapp Finals Week 16-2qt potatoNo ratings yet
- The Urinary System: William J. Babler, PH.DDocument30 pagesThe Urinary System: William J. Babler, PH.DMary-GraceScalesNo ratings yet
- Urinary SystemDocument34 pagesUrinary SystemJULIANNE ANACTANo ratings yet
- KidneyDocument85 pagesKidneyIshita SinghNo ratings yet
- Anatomy and Physiology of Urinary SystemDocument53 pagesAnatomy and Physiology of Urinary SystemArathy KalathingalNo ratings yet
- Physiology OF Renal SYSTEMDocument24 pagesPhysiology OF Renal SYSTEMsam bossaNo ratings yet
- Chapter 11 - ExcretionDocument46 pagesChapter 11 - Excretionapi-372850875% (4)
- UrogenitalDocument36 pagesUrogenitalCharlene Chin SeeNo ratings yet
- Kidneys and ExcretionDocument28 pagesKidneys and ExcretionD-Cristen OrlandoNo ratings yet
- ExcertionDocument39 pagesExcertionMuhammad UsmanNo ratings yet
- QUIAMBAO - Urinary System Reviewer - AnaPhy LecDocument8 pagesQUIAMBAO - Urinary System Reviewer - AnaPhy LecqlouisamarieNo ratings yet
- Chapter 15 The Urinary SystemDocument18 pagesChapter 15 The Urinary SystemYeshia InocencioNo ratings yet
- Excretion and KidneysDocument39 pagesExcretion and KidneyselizabethNo ratings yet
- The Urinary SystemDocument32 pagesThe Urinary SystemriniambarwatiNo ratings yet
- The Urinary System: DR RNGT Amin Samiasih, SKP - Msi.MedDocument36 pagesThe Urinary System: DR RNGT Amin Samiasih, SKP - Msi.MedSura MaduNo ratings yet
- 14 Drugs Acting On The Renal SystemDocument8 pages14 Drugs Acting On The Renal SystemCristine Claire ArasNo ratings yet
- The Urinary SystemDocument66 pagesThe Urinary Systemapi-26587879No ratings yet
- BIOL 174 - Anatomy and Physiology II Ms. C. Myers Thursday 8 April 2010Document59 pagesBIOL 174 - Anatomy and Physiology II Ms. C. Myers Thursday 8 April 2010miss_clio4502No ratings yet
- Chapter 12 - Excretory SystemsDocument57 pagesChapter 12 - Excretory Systemsnokate konkoorNo ratings yet
- ANAPHY LEC Urinary System Page 1: TH RDDocument6 pagesANAPHY LEC Urinary System Page 1: TH RDMarjorie ViescaNo ratings yet
- Chapter 18 Anaphy TransesDocument5 pagesChapter 18 Anaphy TransesHoly HaeinNo ratings yet
- Ana DigesDocument2 pagesAna DigesSTEM-G.04 Kiarrah Katrina BotinNo ratings yet
- Location: BDO Plaza Calderon: Pedro Gil Branch, Vesta, Sta Ana, Metro Manila, Philippines. Coordinates: 14.58122, 121.01151 Street ViewDocument10 pagesLocation: BDO Plaza Calderon: Pedro Gil Branch, Vesta, Sta Ana, Metro Manila, Philippines. Coordinates: 14.58122, 121.01151 Street ViewSTEM-G.04 Kiarrah Katrina BotinNo ratings yet
- Medical Terminlogy Body Planes SectionsDocument75 pagesMedical Terminlogy Body Planes SectionsSTEM-G.04 Kiarrah Katrina BotinNo ratings yet
- Local Government Is A Type of Governing Body of A Country's Specific State or ProvinceDocument2 pagesLocal Government Is A Type of Governing Body of A Country's Specific State or ProvinceSTEM-G.04 Kiarrah Katrina BotinNo ratings yet
- Group 2 ManilaDocument42 pagesGroup 2 ManilaSTEM-G.04 Kiarrah Katrina BotinNo ratings yet
- RomuloMa - Faye BAPT-12 ManilaStudies-1Document5 pagesRomuloMa - Faye BAPT-12 ManilaStudies-1STEM-G.04 Kiarrah Katrina BotinNo ratings yet
- Philosophical ViewsDocument2 pagesPhilosophical ViewsSTEM-G.04 Kiarrah Katrina BotinNo ratings yet
- Members and ShareholdersDocument6 pagesMembers and ShareholdersSTEM-G.04 Kiarrah Katrina BotinNo ratings yet
- Sabapathy 2014Document15 pagesSabapathy 2014Trina ViskhawatNo ratings yet
- Endocrine Glands Are Glands of TheDocument9 pagesEndocrine Glands Are Glands of ThextinebadzNo ratings yet
- Planilha Classificação Qualis 2017-2018 - TabelaDocument460 pagesPlanilha Classificação Qualis 2017-2018 - TabelaThiago EtcNo ratings yet
- Lecture 1 BiophysicsDocument22 pagesLecture 1 Biophysicsmaxwell amponsahNo ratings yet
- Qt.2 Summative Test 1 & 2Document5 pagesQt.2 Summative Test 1 & 2Susan Salvador100% (1)
- B.V Raju Institute of Technology: Department of Physical EducationDocument24 pagesB.V Raju Institute of Technology: Department of Physical EducationNarsimharaju RVNo ratings yet
- Anxiety: Insights Into Signs, Symptoms, Etiology, Pathophysiology, and TreatmentDocument13 pagesAnxiety: Insights Into Signs, Symptoms, Etiology, Pathophysiology, and TreatmentMichael Judika Deardo PurbaNo ratings yet
- Nitrogen FixationDocument6 pagesNitrogen FixationSaziya QuadriNo ratings yet
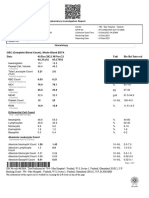
- Date 01/dec/2021 04:33AM 30/nov/21 05:17PM Unit Bio Ref IntervalDocument2 pagesDate 01/dec/2021 04:33AM 30/nov/21 05:17PM Unit Bio Ref IntervalSaurabh PuriNo ratings yet
- Udgam School For Children: SCIENCE-Worksheet No. 4Document4 pagesUdgam School For Children: SCIENCE-Worksheet No. 4YASHVI MODINo ratings yet
- Aqa 6811 W MS Jun05Document6 pagesAqa 6811 W MS Jun05AQA Biology AEANo ratings yet
- NIA AA Revised Clinical Criteria AAIC 2023Document39 pagesNIA AA Revised Clinical Criteria AAIC 2023Ana Cecília RizzuttiNo ratings yet
- Ch07b Ehap LectDocument43 pagesCh07b Ehap LectMONIQUE R. MINISTERIONo ratings yet
- Chapter 17 Notes Summary Biopsychology PDFDocument11 pagesChapter 17 Notes Summary Biopsychology PDFjo cheungNo ratings yet
- Biology 2nd Lab Report (Onion Cell)Document4 pagesBiology 2nd Lab Report (Onion Cell)Johanna Haludilu88% (16)
- Kumar Verma: Lab NoDocument3 pagesKumar Verma: Lab NoSamar SinghNo ratings yet
- Enriched Advanced Ecology Notes 2020Document62 pagesEnriched Advanced Ecology Notes 2020aditi.ugandaNo ratings yet
- Biology Class: 11 Unit: 1Document8 pagesBiology Class: 11 Unit: 1samiNo ratings yet
- AOSpine Manual Thoracic Spine AnatomyDocument18 pagesAOSpine Manual Thoracic Spine AnatomySebastián MorenoNo ratings yet
- Trial SPM SBP 2010 Biology Marking SchemeDocument29 pagesTrial SPM SBP 2010 Biology Marking SchememarwaniNo ratings yet
- Pengaruh Pemberian Ekstrak Daun Salam (Eugenia Polyantha) TERHADAP KADAR TRIGLISERIDA Serum Tikus Jantan Galur Wistar HiperlipidemiaDocument16 pagesPengaruh Pemberian Ekstrak Daun Salam (Eugenia Polyantha) TERHADAP KADAR TRIGLISERIDA Serum Tikus Jantan Galur Wistar HiperlipidemiaIbnu FajarNo ratings yet
- Mallea Et Al. (2019 Classical Conditioning)Document16 pagesMallea Et Al. (2019 Classical Conditioning)Sebastian Chacon0% (1)
- Biology All Chapters Concept AnswersDocument37 pagesBiology All Chapters Concept Answerscazmi AndirahmanNo ratings yet
- Kimberly M. Tsan - The Fool's JourneyDocument26 pagesKimberly M. Tsan - The Fool's Journeyfabio passavantiNo ratings yet
- Sehs2.1 WorkbookDocument4 pagesSehs2.1 Workbookemily khievNo ratings yet
- GSSE Pathology NotesDocument120 pagesGSSE Pathology NotesEmilyNo ratings yet
- Photosynthesis (Handouts)Document5 pagesPhotosynthesis (Handouts)Jelea MagallanesNo ratings yet
- The Human Body: An Orientation: © 2018 Pearson Education, IncDocument59 pagesThe Human Body: An Orientation: © 2018 Pearson Education, IncShana AquinoNo ratings yet
- Plants Make Food CBSE Class 4 WorksheetDocument4 pagesPlants Make Food CBSE Class 4 WorksheetrupikaNo ratings yet
- Science7 Q2 Mod4 EggsAreWhiteLemonsAreYellowLikeMeAndYouTheyreMadeOfCellsToo V3.1 TessOKDocument34 pagesScience7 Q2 Mod4 EggsAreWhiteLemonsAreYellowLikeMeAndYouTheyreMadeOfCellsToo V3.1 TessOKEspher Macabitas100% (6)
- Return of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseFrom EverandReturn of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseRating: 4.5 out of 5 stars4.5/5 (52)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4.5 out of 5 stars4.5/5 (6)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessFrom Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessRating: 4 out of 5 stars4/5 (33)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceFrom EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceRating: 4.5 out of 5 stars4.5/5 (517)
- The Rise and Fall of the Dinosaurs: A New History of a Lost WorldFrom EverandThe Rise and Fall of the Dinosaurs: A New History of a Lost WorldRating: 4 out of 5 stars4/5 (597)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (393)
- Tales from Both Sides of the Brain: A Life in NeuroscienceFrom EverandTales from Both Sides of the Brain: A Life in NeuroscienceRating: 3 out of 5 stars3/5 (18)
- Buddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomFrom EverandBuddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomRating: 4 out of 5 stars4/5 (216)
- Seven and a Half Lessons About the BrainFrom EverandSeven and a Half Lessons About the BrainRating: 4 out of 5 stars4/5 (111)
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesFrom EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesRating: 4.5 out of 5 stars4.5/5 (397)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedFrom EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedRating: 4 out of 5 stars4/5 (11)
- Good Without God: What a Billion Nonreligious People Do BelieveFrom EverandGood Without God: What a Billion Nonreligious People Do BelieveRating: 4 out of 5 stars4/5 (66)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionFrom EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionRating: 4 out of 5 stars4/5 (812)
- Human: The Science Behind What Makes Your Brain UniqueFrom EverandHuman: The Science Behind What Makes Your Brain UniqueRating: 3.5 out of 5 stars3.5/5 (38)
- Lymph & Longevity: The Untapped Secret to HealthFrom EverandLymph & Longevity: The Untapped Secret to HealthRating: 4.5 out of 5 stars4.5/5 (13)
- The Lives of Bees: The Untold Story of the Honey Bee in the WildFrom EverandThe Lives of Bees: The Untold Story of the Honey Bee in the WildRating: 4.5 out of 5 stars4.5/5 (44)
- Who's in Charge?: Free Will and the Science of the BrainFrom EverandWho's in Charge?: Free Will and the Science of the BrainRating: 4 out of 5 stars4/5 (65)
- Darwin's Doubt: The Explosive Origin of Animal Life and the Case for Intelligent DesignFrom EverandDarwin's Doubt: The Explosive Origin of Animal Life and the Case for Intelligent DesignRating: 4.5 out of 5 stars4.5/5 (39)
- Fast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperFrom EverandFast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperRating: 4.5 out of 5 stars4.5/5 (16)
- The Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindFrom EverandThe Consciousness Instinct: Unraveling the Mystery of How the Brain Makes the MindRating: 4.5 out of 5 stars4.5/5 (93)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (411)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorFrom EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorNo ratings yet