Professional Documents
Culture Documents
Lippincott's PEDIATRIC2 ANSWERS
Uploaded by
NursyNurseOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lippincott's PEDIATRIC2 ANSWERS
Uploaded by
NursyNurseCopyright:
Available Formats
The Child with Respiratory Health Problems 203
Managing Care Quality and Safety Answers, Rationales, and Test
61. A charge nurse is making assignments for Taking Strategies
a group of children on a pediatric unit. The nurse
should avoid assigning the same nurse to care for The answers and rationales for each question follow
a 2-year-old with respiratory syncytial virus below, along with keys ( ) to the client need
(RSV) and: (CN) and cognitive level (CL) for each question. Use
■ 1. An 18-month-old with RSV. these keys to further develop your test-taking skills.
■ 2. A 9-year-old 8 hours post-appendectomy. For additional information about test-taking skills
■ 3. A 1-year-old with a heart defect. and strategies for answering questions, refer to pages
■ 4. A 6-year-old with sickle cell crisis. 10–21, and pages 25–26 in Part 1 of this book.
62. The nurse is preparing to administer the last
dose of ceftriaxone (Rocephin) before discharge to a
1-year-old but finds the I.V. has occluded. The nurse The Client with Tonsillitis
should:
■ 1. Restart the I.V. 1. 4. If the child does not stick out his tongue so
■ 2. Administer the medication intramuscularly. the nurse can visualize the throat, it is appropriate
■ 3. Arrange for early discharge. to use a tongue blade. Having the child participate
■ 4. Contact the prescriber to request an order by holding the tongue blade while the nurse guides
change. it to facilitate visualization of the throat is appropri-
63. A nurse administers ranitidine (Zantac) ate technique. It is not useful to remove the tongue
instead of cetirizine (Zyrtec) to an 8-year-old with blade or have the child hold it because the nurse
asthma. The client has suffered no adverse effects. will need to use the tongue blade to depress the
The nurse tells the charge nurse of the incident but tongue. It is preferable to engage the child’s coopera-
fears disciplinary action from reporting the error. tion before asking the parent to restrain the child.
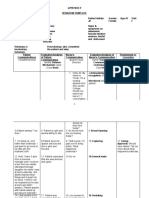
The charge nurse should tell the nurse: CN: Physiological adaptation; CL: Analyze
■ 1. “If you do not report the error, I will have to.”
■ 2. “Reporting the error helps to identify system 2. 4. When preparing a child for a procedure the
problems to improve client safety.” nurse should use neutral words, focus on sensory
■ 3. “Notify the client’s physician to see if she experiences, and emphasize the positive aspects at
wants this reported.” the end. Being reunited with parents and having an
■ 4. “This is not a serious mistake so reporting it ice pop would be considered pleasurable events.
will not affect your position.” Children this age fear bodily harm. To reduced anxi-
ety, the nurse should use the word “fixed” instead
64. A 12-year-old with cystic fibrosis is being of “removed” to describe what is being done to the
treated in the hospital for pneumonia. The physi- tonsils. Using the terms “put to sleep” and “I.V.”
cian is calling in a telephone order for ampicillin. may be threatening. Additionally, directing a play
The nurse should do which of the following? Select experience to focus on I.V. insertion may be counter-
all that apply. productive as the child may have little recollection
■ 1. Ask the unit clerk to listen on the speaker of this aspect of the procedure.
phone with the nurse and write down the
order. CN: Psychosocial adaptation;
■ 2. Ask the physician to come to the hospital and CL: Synthesize
write the order on the chart. 3. 2. The most appropriate outcome for a nurs-
■ 3. Repeat the order to the physician. ing diagnosis of Risk for perioperative-positioning
■ 4. Ask the physician to confirm that the order is injury related to the surgical procedure would be
correct as understood by the nurse. that the child remains NPO for the designated period
■ 5. Ask the nursing supervisor to cosign the tele- of time before surgery, thereby minimizing the risk
phone order as transcribed by the nurse. of aspiration during the surgery. Ability to tell about
the surgery and demonstrating an understanding of
the procedure are appropriate outcomes for a nursing
diagnosis of Deficient knowledge. Knowing that the
parents will not leave is associated with a nursing
diagnosis of Anxiety or Fear related to separation
from support systems or an unfamiliar environment.
CN: Reduction of risk potential;
CL: Synthesize
Billings_Part 2_Chap 2_Test 2.indd 203 8/7/2010 9:58:50 AM
204 The Nursing Care of Children
4. 1. After a tonsillectomy and adenoidectomy, to drain the eustachian tubes, but it would not clear
drooling bright red blood is considered an early the infection. Repeating the same antibiotic that
sign of hemorrhage. Often, because of discomfort didn’t clear the infection during the first course of
in the throat, children tend to avoid swallowing; treatment would probably not be helpful if taken for
instead, they drool. Frequent swallowing would also another 10 days. Myringotomy tubes are not indi-
be an indication of hemorrhage because the child cated with just one ear infection.
attempts to clear the airway of blood by swallowing. CN: Health promotion and maintenance;
Secretions may be slightly blood-tinged because of CL: Synthesize
a small amount of oozing after surgery. However,
bright red secretions indicate bleeding. A pulse rate 9. 1. Toddlers should be approached slowly,
of 95 bpm is within the normal range for a 5-year- because they are wary of strangers and need time
old child, as is a blood pressure of 95/56 mm Hg. to get used to someone they do not know. The best
A small amount of blood that is partially digested, approach is to ignore them initially and to focus on
and therefore dark brown, is often present in post- talking to the parents. The child will likely resist
operative emesis. being held by a stranger, so the nurse should not
pick up or hold the child until the child indicates a
CN: Reduction of risk potential; readiness to be approached or the mother indicates
CL: Analyze that it is okay.
5. 3. For the first few days after a tonsillectomy CN: Health promotion and maintenance;
and adenoidectomy, liquids and soft foods are best CL: Synthesize
tolerated by the child while the throat is sore. Chil-
dren typically do not chew their food thoroughly, 10. 1. Placing ear plugs in the ears will prevent
and solid foods are to be avoided because they are contaminated bathwater from entering the middle
difficult to swallow. Although meat loaf would be ear through the tympanostomy tube and causing
considered a soft food, uncooked carrots would not an infection. Blowing the nose forcibly during a
be. Pork is frequently difficult to chew. Foods that cold causes organisms to ascend through the eusta-
have sharp edges, such as potato chips, are con- chian tube, possibly leading to otitis media. It is not
traindicated because they are hard to chew and may necessary to administer antibiotics continuously to
cause more throat discomfort. a child with a tympanostomy tube. Antibiotics are
appropriate only when an ear infection is present.
CN: Basic care and comfort; CL: Evaluate Drainage from the ear may be a sign of middle ear
6. 3. The risk of hemorrhage from a tonsillec- infection and should be reported to the health care
tomy is greatest when the tissue begins sloughing provider.
and the scabs fall off. This typically happens CN: Reduction of risk potential;
7 to 10 days after a tonsillectomy. CL: Create
CN: Safety and infection control;
CL: Apply
The Client with Foreign
Body Aspiration
The Client with Otitis Media
11. 4. Crackers, because they crumble and eas-
7. 2. When a person is taking amoxicillin as ily dissolve, are not commonly aspirated. Because
well as an oral contraceptive it renders the contra- children commonly eat popcorn hulls or pieces that
ceptive less effective. Because pregnancy can occur have not popped, popcorn can be easily aspirated.
in such a situation, the nurse should advise the cli- Toddlers frequently do not chew their food well,
ent to use additional means of birth control during making raw vegetables a commonly aspirated food.
the time she is taking the antibiotic. There are no Round candy is often difficult to chew and comes in
risks associated with the concurrent use of amoxicil- large pieces, making it easily aspirated.
lin and antacids, vitamins, or food.
CN: Health promotion and maintenance;
CN: Psychosocial adaptation; CL: Apply CL: Evaluate
8. 4. Treatment of otitis media involves antibi- 12. 1. Young children have specific reactions to
otic therapy for 10 days and then a follow-up check separation and hospitalization. In the protest stage,
of the ears by the health care provider. If the infec- the toddler physically and verbally attacks anyone
tion is not cleared, the health care provider will who attempts to provide care. Here, the child is
restart the client on another antibiotic. The bulging fussing and crying and visibly pushes the nurse
tympanic membrane and continued pain suggest away. In the despair stage, the toddler becomes
that an infection remains. A decongestant may help withdrawn and obviously depressed (e.g., not
Billings_Part 2_Chap 2_Test 2.indd 204 8/7/2010 9:58:51 AM
The Child with Respiratory Health Problems 205
engaging in play activities and sleeping more than 16. 2. Swimming is appropriate for this child
usual). Regression is a return to a developmentally because it requires controlled breathing, assists
earlier phase because of stress or crisis (e.g., a tod- in maintaining cardiac health, enhances skeletal
dler who could feed himself before this event is not muscle strength, and promotes ventilation and
doing so now). Denial or detachment occurs if the perfusion. Stop-and-start activities, such as soccer,
toddler’s stay in the hospital without the parent is track, and gymnastics, commonly trigger symptoms
prolonged because the toddler settles in to the hos- in asthmatic clients.
pital life and denies the parents’ existence (e.g., not
reacting when the parents come to visit). CN: Health promotion and maintenance;
CL: Synthesize
CN: Psychosocial adaptation;
CL: Analyze 17. 3. The child who is experiencing an asthma
attack typically demonstrates wheezing on expira-
13. 4. The three cardinal signs indicating that a tion initially. This results from air moving through
child is truly choking and requires immediate life- narrowed airways secondary to bronchoconstriction.
saving interventions include inability to speak, blue The child’s expiratory phase is normally longer than
color (cyanosis), and collapse. Vomiting does not the inspiratory phase. Expiration is passive as the
occur while a child is unable to breathe. Once the diaphragm relaxes. During an asthma attack, secre-
object is dislodged, however, vomiting may occur. tions are thick and are not usually expelled until
Gasping, a sudden intake of air, indicates that the the bronchioles are more relaxed. At the beginning
child is still able to inhale. When a child is choking, of an asthma attack the cough will be tight but not
air is not being exchanged, so gagging will not occur. productive. Fever is not always present unless there
CN: Reduction of risk potential; is an infection that may have triggered the attack.
CL: Evaluate CN: Physiological adaptation;
CL: Analyze
The Client with Asthma 18. 1, 2, 4, 6. Coughing, especially at night and
in the absence of an infection, is a common symp-
tom of asthma. Early signs of respiratory distress
14. 3. Intercostal retractions indicate an increase include restlessness, tachypnea, tachycardia, and
in respiratory effort, which is a sign of respiratory
diaphoresis. Other signs also include hypertension,
distress. During an asthma attack, secretions are
nasal flaring, grunting, wheezing, and intercostal
thick, the cough is tight, and respiration is difficult
retractions. A heart rate of 95 bpm is normal for a
(and shortness of breath may occur). If mucous
toddler. Malaise typically does not indicate respira-
secretions are copious but thin, the client can
tory distress.
expectorate them, which indicates an improvement
in the condition. If the cough is productive it means CN: Physiological adaptation;
the bronchospasms and the inflammation have been CL: Analyze
resolved to the extent that the mucus can be expec-
torated. A respiratory rate of 20 breaths/minute
19. 2. The peak flow of 180 L/minute is in the
yellow zone, or 50% to 80% of the child’s personal
would be considered normal and no intervention
best. This means that the child’s asthma is not well
would be needed.
controlled, thereby necessitating the use of a short-
CN: Physiological adaptation; acting beta2-agonist medication to relieve the bron-
CL: Analyze chospasm. A peak flow reading greater than 80% of
the child’s personal best (in this case, 220 L/minute
15. 3. The therapeutic level of theophylline is or better) would indicate that the child’s asthma
10 to 20 mcg/m. A toxic level of theophylline
is in the green zone or under good control. A peak
can cause vomiting, irritability, headache, and
flow reading in the red zone, or less than 50% of the
tachycardia. Oral rehydration may be helpful if the
child’s personal best (135 L/minute or less), would
vomiting had created enough of a fluid volume deficit
require notification of the health care provider or a
to elevate the heart rate, but this is unlikely since the
trip to the emergency department. Cromolyn sodium
client has an I.V. Allergic reactions to ampicillin usu-
(Intal) is not used for short-term treatment of acute
ally include rash, urticaria, respiratory distress, and
bronchospasm. It is used as part of a long-term
hypotension, not tachycardia and vomiting. Although
therapy regimen to help desensitize mast cells and
the child’s heart rate could indicate hypoxia, none of
thereby help to prevent symptoms.
the other signs indicate a need for oxygen.
CN: Reduction of risk potential;
CN: Pharmacological and parenteral
CL: Evaluate
therapies; CL: Synthesize
Billings_Part 2_Chap 2_Test 2.indd 205 8/7/2010 9:58:52 AM
206 The Nursing Care of Children
20. 3. Complaints of chest pain in children and the limitations imposed by the illness. They also
adolescents are rarely cardiac. With a history of need to learn how to manage exacerbations and then
asthma, the most likely cause of the chest pain is resume as normal a life as possible. Trying to keep
related to the asthma. Therefore, the nurse should the child happy at all costs is inappropriate and
check the adolescent’s peak flow reading to evalu- can lead to the child’s never learning how to accept
ate the status of the air flow. Calling the adolescent’s responsibility for behavior and get along with oth-
parent would be appropriate, but this would be ers. Although minimizing the child’s risk for expo-
done after the nurse obtains the peak flow reading sure to infections is important, the child needs to be
and additional assessment data. Having the adoles- with his or her peers to ensure appropriate growth
cent lie down may be an option, but more data need and development. Children with a chronic illness
to be collected to help establish a possible cause. need to be involved in their care so that they can
Because the adolescent has not experienced any learn to manage it. Some parents tend to overprotect
asthma problems for a long time, it would be inap- their child with a chronic illness. This overprotec-
propriate for the nurse to administer a short-acting tiveness may cause a child to have an exaggerated
bronchodilator at this time. feeling of importance or later, as an adolescent, to
rebel against the overprotectiveness and the parents.
CN: Reduction of risk potential;
CL: Synthesize CN: Psychosocial adaptation;
CL: Evaluate
21. 3. Because persistent coughing may indicate
an asthma attack and a 7-year-old child would be 24. 4. Physical activities are beneficial to asth-
able to provide only minimal history information, it matic children, physically and psychosocially. Most
would be important to obtain information from the children with asthma can engage in school and
parent. Although determining the child’s heart rate sports activities that are geared to the child’s condi-
is an important part of the assessment, it would be tion and within the limits imposed by the disease.
done after the history is obtained. More information The coach and other team members need to be
needs to be obtained before giving the child a nebu- aware of the child’s condition and know what to do
lizer treatment. Although it may be necessary for the in case an attack occurs. Those children who have
parent to come and pick up the child, a thorough exercise-induced asthma usually use a short-acting
assessment including history information should be bronchodilator before exercising.
obtained first. CN: Health promotion and maintenance;
CN: Reduction of risk potential; CL: Apply
CL: Synthesize
22. 1. To help reduce allergic triggers in the The Client with Cystic Fibrosis and
home, the nurse should recommend that the humid-
ity level be kept between 50% and 60%. Doing so Bronchopneumonia
keeps the air moist and comfortable for breathing.
When air is dry, the risk for respiratory infections 25. 2. The child must take the pancreatic enzyme
increase. Too high a level of humidity increases supplement with meals and snacks to help absorb
the risk for mold growth. Typically, the child with nutrients so he can grow and develop normally. In
asthma should sleep in the top bunk bed to mini- cystic fibrosis, the normally liquid mucus is tena-
mize the risk of exposure to dust mites. The risk cious and blocks three digestive enzymes from
of exposure to dust mites increases when the child entering the duodenum and digesting essential
sleeps in the bottom bunk bed because dust mites nutrients. Without the supplemental pancreatic
fall from the top bed, settling in the bottom bed. enzyme, the child will have voluminous, foul, fatty
Scented sprays should be avoided because they stools due to the undigested nutrients and may
may trigger an asthmatic episode. Ideally, carpet- experience developmental delays due to malnutri-
ing should be avoided in the home if the child has tion. Dehydration is not a problem related to cystic
asthma. However, if it is present, carpeting in the fibrosis. The pancreatic enzymes have no effect on
child’s room should be vacuumed often, possibly the viscosity of the tenacious mucus. Diarrhea is
daily, to remove dust mites and dust particles. not caused by failing to take the pancreatic enzyme
supplement.
CN: Reduction of risk potential;
CL: Create CN: Pharmacological and parenteral
therapies; CL: Apply
23. 3. Positive adjustment to a chronic condition
requires placing the child’s illness in its proper 26. 3. Clients with cystic fibrosis commonly
perspective. Children with asthma need to be die from respiratory problems. The mucus in the
treated as normally as possible within the scope of lungs is tenacious and difficult to expel, leading to
lung infections and interference with oxygen and
Billings_Part 2_Chap 2_Test 2.indd 206 8/7/2010 9:58:52 AM
The Child with Respiratory Health Problems 207
carbon dioxide exchange. The client will likely need 30. 4. CF affects the exocrine glands. Mucus is
supplemental oxygen and respiratory treatments to thick and tenacious, sticking to the walls of the
maintain adequate gas exchange, as identified by pancreatic and bile ducts and eventually caus-
the oximeter reading. The child will be on bed rest ing obstruction. Because of the difficulty with
due to respiratory distress. However, although blood digestion and absorption, a high-calorie, high-
gases will probably be ordered, the oximeter read- protein, high-carbohydrate, moderate-fat diet is
ings will be used to determine oxygen deficit and indicated.
are, therefore, more of a priority. A diet high in calo-
ries, proteins, and vitamins with pancreatic granules CN: Physiological adaptation; CL: Apply
added to all foods ingested will increase nutrient 31. 2. In children with CF, poor digestion and
absorption, and help the malnutrition; however, this absorption of foods, especially fats, results in fre-
intervention is not the priority at this time. Insert- quent bowel movements that are bulky, large,
ing an I.V. to administer antibiotics is important, and foul-smelling. The stools also contain
and can be done after ensuring adequate respiratory abnormally large quantities of fat, which is called
function. steatorrhea. An adolescent experiencing good
CN: Physiological adaptation; control of the disease would describe soft stools
CL: Synthesize with little odor. Stool described as loose with
bits of food indicates diarrhea. Stool described
27. 2. Fried scallops are high in fat, and fats are as hard with streaks of blood may indicate
difficult for a client with cystic fibrosis to digest; constipation.
scallops are also not commonly preferred by most
children. Clients with cystic fibrosis commonly lack CN: Physiological adaptation;
calories and protein because their bodies do not CL: Analyze
absorb nutrients. Nutrients are not absorbed because 32. 2. The child’s favorite doll would be a
tenacious mucus blocks key digestive enzymes from good choice of toys. The doll provides support
entering the digestive system. Thus, a diet rich in and is familiar to the child. Although a 3-year-
proteins and carbohydrates is essential for these old may enjoy puzzles, a 100-piece jigsaw puzzle
clients. Roasted chicken and an egg omelet are high is too complicated for an ill 3-year-old child. In
in protein and help with growth and development. view of the child’s lung pathology, a fuzzy stuffed
The milk shake is high in carbohydrate and protein. animal would not be advised because of its poten-
CN: Health promotion and maintenance; tial as a reservoir for dust and bacteria, possibly
CL: Apply predisposing the child to additional respira-
tory problems. Scissors, paper, and paste are not
28. 1. Monitoring intake and output is the most appropriate for a 3-year-old unless the child is
important nursing action when administering an supervised closely.
aminoglycoside, such as gentamicin, because a
decrease in output is an early sign of renal dam- CN: Health promotion and maintenance;
age. Daily weight monitoring is not indicated when CL: Create
the client is receiving an aminoglycoside. Con- 33. 1. CF is characterized by a dysfunction in
stipation and bleeding are not adverse effects of the body’s mucus-producing exocrine glands. The
aminoglycosides. mucus secretions are thick and sticky rather than
CN: Pharmacological and parenteral thin and slippery. The mucus obstructs the bronchi,
therapies; CL: Synthesize bronchioles, and pancreatic ducts. Mucus plugs in
the pancreatic ducts can prevent pancreatic diges-
29. 2. Postural drainage, which aids in mobi- tive enzymes from reaching the small intestine,
lizing the thick, tenacious secretions commonly resulting in poor digestion and poor absorption of
associated with CF, is usually performed before various food nutrients. Fibrous cysts do not form
meals to avoid the possibility of vomiting or regur- in various organs. Cystic fibrosis is an autosomal
gitating food. Although the child with CF needs recessive inherited disorder and does not involve
frequent rest periods, this is not an important factor any reaction to the formation of antibodies against
in scheduling postural drainage. However, the nurse streptococcus.
would not want to interrupt the child’s rest period
to perform the treatment. Inhalation treatments CN: Physiological adaptation;
are usually given before postural drainage to help CL: Evaluate
loosen secretions. 34. 1. After treatment, the client outcome
CN: Reduction of risk potential; would be that respiratory status would be within
CL: Apply normal limits, as evidenced by a respiratory rate
and rhythm within expected range. Absence of
Billings_Part 2_Chap 2_Test 2.indd 207 8/7/2010 9:58:53 AM
208 The Nursing Care of Children
chills and fever, although related to an underlying associated with a higher incidence of SIDS. SIDS
problem causing the respiratory problem (e.g., the occurs with higher frequency in families where
infection), do not specifically relate to the respira- a child in the family has already died of SIDS,
tory problem of ineffective airway clearance. The but the age of the parents has not been shown to
child’s ability to engage in age-related activities contribute to SIDS. A respiratory infection such as
may provide some evidence of improved respira- pneumonia has not been shown to cause a higher
tory status. However, this outcome criterion is incidence of SIDS.
more directly related to a nursing diagnosis of
CN: Health promotion and maintenance;
Activity intolerance. Although the child’s abil-
CL: Analyze
ity to tolerate his or her usual diet may indirectly
relate to respiratory function, this outcome is more 38. 3. Because this is an especially disturbing
specifically related to a nursing diagnosis of Imbal- and upsetting time for the parents, they must be
anced nutrition: Less than body requirements, approached in a sensitive manner. Asking what the
which may or may not be related to the child’s infant looked like when found allows the parents to
respiratory status. verbalize what they saw and felt, thereby helping
to minimize their feelings of guilt without implying
CN: Physiological adaptation;
any blame, neglect, wrongdoing, or abuse. Asking if
CL: Evaluate
the child was wrapped in a blanket or lying on his
35. 1. Swimming would be the most appropri- stomach, or when the parents last checked on the
ate suggestion because it coordinates breathing and infant, implies that the parents did something wrong
movement of all muscle groups and can be done on or failed in their care of the infant, thus blaming
an individual basis or as a team sport. Because track them for the event.
events, baseball, and javelin throwing usually are
CN: Physiological adaptation;
performed outdoors, the child would be breathing
CL: Analyze
in large amounts of dust and dirt, which would be
irritating to her mucous membranes and pulmo- 39. 4. The community health nurse should visit
nary system. The strenuous activity and increased as soon after the death as possible, because the
energy expenditure associated with track events, in parents may need help to deal with the sudden,
conjunction with the dust and possible heat, would unexpected death of their infant. Parents often have
play a role in placing the child at risk for an upper a great deal of guilt in these situations and need to
respiratory tract infection and compromising her express their feelings to someone who can provide
respiratory function. counseling.
CN: Health promotion and maintenance; CN: Psychosocial adaptation;
CL: Synthesize CL: Synthesize
40. 1. The goal of the second home visit is to
help the parents express their feelings more openly.
The Client with Sudden Infant Many parents are reluctant to express their grief
Death Syndrome and need help. The goal of the first visit is to help
the parents understand the disease and what hap-
36. 1, 3, 4. Exposure to environmental tobacco pened. The first visit also provides time to help
increases the risk for SIDS. Sleeping on the back and the parents understand that they are not to blame.
breast-feeding both decrease the risk of SIDS. The Although it is important to assess the impact of
side-lying position is not recommended for sleep. It SIDS on siblings, this is not the primary goal for the
is recommended that babies be dressed in sleepers second visit. However, the nurse must be flexible in
and that cribs are free of blankets, pillows, bumper case problems involving this area arise. Typically,
pads, and stuffed animals. Co-bedding with parents parents are unable to deal with decisions such
is not recommended as parents may roll on the as having other children during the second visit
child. because they are grieving for the child that they
lost. This topic may be discussed later in the course
CN: Safety and infection control;
of care.
CL: Create
CN: Psychosocial adaptation;
37. 1. The highest incidence of SIDS occurs in CL: Synthesize
infants between ages 2 and 4 months. About 90%
of SIDS occurs before the age of 6 months. Apnea
lasting longer than 20 seconds has also been
Billings_Part 2_Chap 2_Test 2.indd 208 8/7/2010 9:58:54 AM
The Child with Respiratory Health Problems 209
The Client Who Requires compressions are indicated only for respiratory
Immediate Care and arrests where the heart rate remains above 60. The
AED/defibrillator should be used as soon as it is
Cardiopulmonary Resuscitation ready, but rescuers should not discontinue compres-
sions until the device is ready for use. The ratio for
41. 2-person CPR in adults is 30:2.
2. Assess the airway. CN: Physiological adaptation;
CL: Synthesize
1. Administer activated charcoal. 45. 3. To maintain the best perfusion, it is
recommended that compressions be given at a rate
3. Reassure the mother. of 100 per minute in a 30 compression to 2 breath
ratio for one rescuer CPR. Children still are more
likely to have had a respiratory arrest than a cardiac
6. Perform a physical exam. arrest and are more likely to respond to opening the
airway and rescue breaths. Therefore, it is recom-
5. Obtain a history of the incident. mended that unless the collapse was witnessed, a
sole rescuer should attempt 5 cycles of CPR before
4. Check serum acetaminophen levels. leaving to call for help. Using 2-3 fingers for chest
compressions is recommended for infant CPR only.
Immediate care of the child who has ingested acet- Abdominal thrusts are no longer recommended for
aminophen is to ensure airway, breathing, and circu- unconscious victims.
lation. Next, the nurse should administer activated CN: Physiological adaptation;
charcoal. Acetylcysteine (Mucomyst) may also be CL: Evaluate
used as an antidote. When the child is stable, the
nurse should reassure the mother. Next, the nurse 46. 3. With CPR, effectiveness of external chest
should perform a physical exam to assess the child compressions is indicated by palpable peripheral
for other health problems, and then obtain fur- pulses, the disappearance of mottling and cyanosis,
ther information about how the child obtained the the return of pupils to normal size, and warm, dry
aspirin. The serum acetaminophen level should be skin. To determine whether the victim of cardio-
obtained 4 hours after ingestion. pulmonary arrest has resumed spontaneous breath-
ing and circulation, chest compressions must be
CN: Safety and infection control; stopped for 5 seconds at the end of the first minute
CL: Synthesize and every few minutes thereafter.
42. 1. When breathlessness is determined, the CN: Physiological adaptation;
priority nursing action is to clear the airway. This CL: Evaluate
action alone may reestablish spontaneous respira-
tion. If the client does not begin breathing, mouth- 47. 2. The nurse should use mechanical force–
to-mouth resuscitation is initiated. Oxygen therapy back slaps and chest thrusts–in an attempt to
would not be initiated at this time, because the child dislodge the object. Blind finger sweeps are not
is not breathing. Also, administering oxygen therapy appropriate in infants and children because the
would interfere with providing mouth-to-mouth foreign body may be pushed back into the airway.
resuscitation. Chest compressions are begun only Subdiaphragmatic abdominal thrusts are not used
after the client is determined to be pulseless. for infants age 1 year or younger because of the risk
of injury to abdominal organs. If the object is not
CN: Physiological adaptation; visible when opening the mouth, time is wasted
CL: Synthesize in looking for it. Action is required to dislodge the
43. 1. Rescue breaths should be delivered slowly object as quickly as possible.
at a volume that makes the chest rise and fall. For a CN: Reduction of risk potential;
5-year-old child, the rate is 10 breaths per minute. If CL: Apply
the nurse is also administering chest compressions,
the rate is 2 breaths for every 15 compressions. 48. 1. To deliver back slaps, the nurse should
place the infant face down, straddled over the
CN: Physiological adaptation; CL: Apply nurse’s arm, with the head lower than the trunk and
44. 3. CPR is done on children for heart rate the head supported. This position, together with the
of less 60 with signs of poor perfusion. Rescu- back slaps, facilitates dislodgment and removal of
ers should use a 15:2 compression to ventilation a foreign object and minimizes aspiration if vomit-
ratio for 2-rescuer CPR for a child. Breaths without ing occurs. Placing the infant with the head up and
raised above the trunk would not aid in dislodging
Billings_Part 2_Chap 2_Test 2.indd 209 8/7/2010 9:58:54 AM
210 The Nursing Care of Children
and removing the foreign object. In addition, this Any attempt to restrain the child, draw blood, insert
position places the infant at risk for aspiration an I.V., or examine her throat could result in total
should vomiting occur. Placing the head to one side airway obstruction.
may minimize the risk of aspiration. However, it
CN: Physiological adaptation;
would not help with removal of an object that is
CL: Synthesize
dislodged by the back slaps. Placing the infant with
the head parallel to the nurse and supported at the 53. 1. The toddler is exhibiting cold symptoms.
buttocks is more appropriate for burping the infant. A hoarse cough may be part of the upper respiratory
tract infection. The best suggestion is to have the
CN: Physiological adaptation; CL: Apply
father offer the child additional fluids at frequent
49. 3. The nurse should first obtain an Ambu intervals to help keep secretions loose and mem-
bag and assist with CPR by giving breaths at a rate branes moist. There is no evidence presented to sug-
of 2 breaths per 15 compressions. The PA is using gest that the child needs to be brought to the clinic
correct technique by using 2 to 3 fingers on the chest immediately. Although having the father count the
to administer chest compressions; The heel of both child’s respiratory rate may provide some additional
hands is used for older children and adolescents; information, it may lead the father to suspect that
the thumbs are used for premature infants. The com- something is seriously wrong, possibly leading to
pression to breath rate in 2- person CPR is 15 to 2. undue anxiety. A hot air vaporizer is not recom-
mended. However, a cool mist vaporizer would
CN: Management of care; CL: Apply
cause vasoconstriction of the respiratory passages,
50. 2. Back slaps are delivered rapidly and force- making it easier for the child to breathe and loosen-
fully with the heel of the hand between the infant’s ing secretions.
shoulder blades. Slowly delivered back slaps are
CN: Physiological adaptation;
less likely to dislodge the object. Using the heel of
CL: Synthesize
the hand allows more force to be applied than when
using the palm or the whole hand, increasing the 54. 2. The nurse may be having difficulty calming
likelihood of loosening the object. The fingertips the child because the child is experiencing increas-
would be used to deliver chest compressions to an ing respiratory distress. The normal respiratory rate
infant younger than 1 year of age. for a 21-month-old is 25 to 30 breaths/minute. The
child’s respiratory rate is 48 breaths/minute. There-
CN: Physiological adaptation; CL: Apply
fore the physician needs to be notified immediately.
51. 4. Crying indicates that the airway obstruc- Typically, acetaminophen is not given to a child
tion has been relieved. No additional thrusts are unless the temperature is 101° F (38.6° C) or higher.
needed. However, the child needs to be observed Letting the toddler cry is inappropriate with croup
closely for complications, including respiratory because crying increases respiratory distress. Offer-
distress. Tapping or shaking the shoulders is used ing fluids every few minutes to a toddler experienc-
initially to determine unresponsiveness in some- ing increasing respiratory distress would do little, if
one who appears unconscious. Delivering chest or anything, to calm the child. Also, the child would
back slaps could jeopardize the child’s now-patent have difficulty coordinating breathing and swallow-
airway. Because the obstruction has been relieved, ing, possibly increasing the risk of aspiration.
there is no need to sweep the child’s mouth. Addi-
CN: Physiological adaptation;
tionally, blind finger sweeps are contraindicated
CL: Synthesize
because the object may be pushed further back, pos-
sibly causing a complete airway obstruction.
CN: Physiological adaptation; The Client with Bronchiolitis
CL: Synthesize or Pharyngitis
55. 1, 2, 4. Viral pharyngitis is treated with
The Client with Croup symptomatic, supportive therapy. Treatment
includes use of a cool mist vaporizer, feeding a soft
52. 4. This child is in severe respiratory distress or liquid diet, and administration of acetaminophen
with the potential for complete airway obstruction. for comfort. Viral infections do not respond to anti-
The nurse should refrain from disturbing the child biotic administration. The child does not need to be
at this time to avoid irritating the epiglottis and on secretion precautions because viral pharyngitis is
causing it to completely obstruct the child’s airway. not contagious.
The child may be intubated or undergo a tracheot-
omy. However, initially, the child should be kept as CN: Psychosocial adaptation;
calm as possible with as little disruption as possible. CL: Synthesize
Billings_Part 2_Chap 2_Test 2.indd 210 8/7/2010 9:58:55 AM
The Child with Respiratory Health Problems 211
56. 3. In an infant with these symptoms, the first statement that she hopes she doesn’t get a cold from
action by the nurse would be to obtain an oxygen her child does not indicate understanding of what to
saturation reading to determine how well the infant do after discharge. For most parents, listening to the
is oxygenating, which is valuable information for child’s chest would not be helpful because the par-
an infant with trouble breathing. Because the father ents would not know what they were listening for.
probably can provide no other information, check- Rather, watching for an increased respiratory rate,
ing the heart rate would be the second action done fever, or evidence of poor eating or drinking would
by the nurse. Then the nurse would obtain the be more helpful in alerting the parent to potential
infant’s weight. illness.
CN: Reduction of risk potential; CN: Physiological adaptation;
CL: Synthesize CL: Evaluate
57. 3. Based on the assessment findings of 60. 4. The child is in respiratory distress
increased respiratory rate, retractions, and wheez- and is sitting in a position to relieve the airway
ing, this infant needs further evaluation, which obstruction; the nurse should provide a humidi-
could be obtained in an emergency department. fied environment with a croup tent with cool mist
Without a definitive diagnosis, administering a to facilitate breathing and liquefy secretions. The
nebulizer treatment would be outside the nurse’s child should remain sitting to facilitate breathing;
scope of practice unless there was an order for such the nurse should allow the child to determine the
a treatment. Sending the infant for a radiograph may most comfortable position. After the child is breath-
not be in the nurse’s scope of practice. The findings ing normally, the nurse can offer fluids; the physi-
need to be reported to a physician who can then cian also may order intravenous fluids. The nurse
determine whether or not a chest radiograph is war- can call the rapid response team if the respiratory
ranted. The infant is exhibiting signs and symptoms distress is not relieved by using a croup tent or other
of respiratory distress and is too ill to send out with vital signs changes indicate further distress.
just instructions on cold care for the mother. CN: Reduction of risk potential;
CN: Physiological adaptation; CL: Synthesize
CL: Synthesize
58. 1, 6. An infant with bronchiolitis will have Managing Care Quality and Safety
increased respirations and will tire more quickly,
so it is best and easiest for the infant to take fluids
more often in smaller amounts. The parents also
61. 3. RSV may be spread though both direct
and indirect contact. While contact and standard
would be instructed to watch for signs of increased
precautions should be employed, a measure to
difficulty breathing, which signal possible complica-
further decrease the risk of nosocomial infections
tions. Healthy infants and even those with bronchi-
is to avoid assigning the same nurse caring for an
olitis should sleep in the supine position. Calling
RSV client to a client at risk for infection. Children
the clinic for an episode of vomiting would not be
2 years of age and younger are most at risk for RSV,
necessary. However, the parents would be instructed
especially if they have other chronic problems such
to call if the infant cannot keep down any fluids for
as a heart defect. From an infection control perspec-
a period of more than 4 hours. Parents would not
tive, pairing 2 clients with RSV is ideal. RSV infec-
need to record how much the infant drinks. Chest
tions are unlikely to pose a serious problem in older
physiotherapy is not indicated because it does not
children.
help and further irritates the infant.
CN: Safety and infection control;
CN: Basic care and comfort; CL: Create
CL: Synthesize
59. 4. Handwashing is the best way to prevent 62. 4. Restarting an I.V. for 1 dose of a medica-
respiratory illnesses and the spread of disease. Bron-
tion may not be in the infant’s best interest when
chiolitis, a viral infection primarily affecting the
the medication can be given in an alternate form.
bronchioles, causes swelling and mucus accumula-
The prescriber should be contacted to determine
tion of the lumina and subsequent hyperinflation of
I.M. or P.O. options. Rocephin may be given I.M.,
the lung with air trapping. It is transmitted primar-
but changing the route of a medication administra-
ily by direct contact with respiratory secretions as
tion requires an order. Failing to complete an entire
a result of eye-to-hand or nose-to-hand contact or
course of antibiotics contributes to the emergence
from contaminated fomites. Therefore, handwash-
of antibiotic resistance and would rarely be the best
ing minimizes the risk for transmission. Taking
option.
the child’s temperature is not appropriate in most
cases. As long as the child is getting better, taking CN: Management of care; CL: Synthesize
the temperature will not be helpful. The mother’s
Billings_Part 2_Chap 2_Test 2.indd 211 8/7/2010 9:58:55 AM
212 The Nursing Care of Children
63. 2. Client safety is enhanced when the 64. 3, 4. To ensure client safety in obtaining
emphasis on medication errors is to determine the telephone orders, the order must be received by a
root cause. All errors should be reported so systems registered nurse. The nurse should write the order,
can identify patterns which contribute to errors. read the order back to the physician, and receive
Here, the similar names probably contributed to the confirmation from the physician that the order is
error. The nurse who commits the error knows all correct. It is not necessary to ask the unit clerk to
the relevant information and is in the best position listen to the order, to require the physician to come
to report it. While the physician should be notified, to the hospital to write the order on the chart, or to
it is a nursing responsibility to report errors not a have the nursing supervisor cosign the telephone
physician choice. Relating mistakes to a nurse’s order.
position focuses on personal blame.
CN: Safety and infection control;
CN: Safety and infection control; CL: Synthesize
CL: Synthesize
Billings_Part 2_Chap 2_Test 2.indd 212 8/7/2010 9:58:56 AM
You might also like
- Clinical Management Review 2023-2024: Volume 2: USMLE Step 3 and COMLEX-USA Level 3From EverandClinical Management Review 2023-2024: Volume 2: USMLE Step 3 and COMLEX-USA Level 3No ratings yet
- USMLE Step 3 Lecture Notes 2021-2022: Pediatrics, Obstetrics/Gynecology, Surgery, Epidemiology/Biostatistics, Patient SafetyFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Pediatrics, Obstetrics/Gynecology, Surgery, Epidemiology/Biostatistics, Patient SafetyRating: 5 out of 5 stars5/5 (2)
- Lippincott's PEDIATRIC7 ANSWERSDocument11 pagesLippincott's PEDIATRIC7 ANSWERSNursyNurseNo ratings yet
- MCQs in Pediatrics Review of Nelson Textbook of Pediatrics (PDFDrive)Document642 pagesMCQs in Pediatrics Review of Nelson Textbook of Pediatrics (PDFDrive)GrInDoVe9097No ratings yet
- Downloadfile 2Document8 pagesDownloadfile 2Michael SilvaNo ratings yet
- Nursing Care of Children Principles and Practice 4Th Edition James Test Bank Full Chapter PDFDocument32 pagesNursing Care of Children Principles and Practice 4Th Edition James Test Bank Full Chapter PDFhelgasophie7478k0100% (8)
- FUNDA Part 1 RatioDocument6 pagesFUNDA Part 1 RatioJo Hn VengzNo ratings yet
- MCQ NelsonDocument433 pagesMCQ NelsonShashank MisraNo ratings yet
- Nelson 20th MCQDocument593 pagesNelson 20th MCQcharlesy T89% (19)
- NCLEX Saunders Chapter 48 Infectious and Communicable DiseasesDocument1 pageNCLEX Saunders Chapter 48 Infectious and Communicable DiseasesMaynard Pabunan LlapitanNo ratings yet
- Vocabulary QuestionsDocument63 pagesVocabulary Questionsyouti100% (1)
- CHN 2 SET A (Key Answers)Document7 pagesCHN 2 SET A (Key Answers)Marie Ordonia de Pona100% (1)
- Valoración PreanestesicaDocument5 pagesValoración PreanestesicaSebastian Hdez BolañosNo ratings yet
- Mind'S Nest Review Center - SuperstesDocument10 pagesMind'S Nest Review Center - SuperstesEsarpy (Nana)100% (1)
- Office of The Infection Control Committee: Allied Care Experts (Ace) Medical Center - PaterosDocument5 pagesOffice of The Infection Control Committee: Allied Care Experts (Ace) Medical Center - PaterosCris GalendezNo ratings yet
- RationalizationDocument3 pagesRationalizationSophia Gella FredilesNo ratings yet
- Answers, Rationales, and Test Taking Strategies: The Client With CryptorchidismDocument8 pagesAnswers, Rationales, and Test Taking Strategies: The Client With CryptorchidismNursyNurseNo ratings yet
- 2012 Nursing Care of Children Principles and Practice 4e Test BankDocument11 pages2012 Nursing Care of Children Principles and Practice 4e Test Bankjamierodriguez050512992b51No ratings yet
- Lippincott's PEDIATRIC1 ANSWERSDocument9 pagesLippincott's PEDIATRIC1 ANSWERSNursyNurseNo ratings yet
- Chapter 41: The Child With An Infectious Disease Test Bank: Multiple ChoiceDocument10 pagesChapter 41: The Child With An Infectious Disease Test Bank: Multiple ChoiceNurse UtopiaNo ratings yet
- Chapter 35: Eye Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument5 pagesChapter 35: Eye Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Pediatric Nursing Flashcards2 - QuizletDocument50 pagesPediatric Nursing Flashcards2 - QuizletNursyNurseNo ratings yet
- Comprehensive Review PNLEDocument16 pagesComprehensive Review PNLEUserrrrrbista100% (3)
- Review Questionnaire MTRNALDocument13 pagesReview Questionnaire MTRNALKevin Vincent AquinoNo ratings yet
- PosttestDocument6 pagesPosttestBelleNo ratings yet
- Unit 1 QuizDocument4 pagesUnit 1 QuizAmanda KamienNo ratings yet
- Morepedsfinal 2Document39 pagesMorepedsfinal 2b7vm7nhvqmNo ratings yet
- Paediatrics Workbook - Nuc304: SUMMER 2021Document10 pagesPaediatrics Workbook - Nuc304: SUMMER 2021Rawan KhateebNo ratings yet
- Infectious DiseasesDocument4 pagesInfectious DiseasesRichevin DenzoNo ratings yet
- Pediatric Test DrillDocument5 pagesPediatric Test DrillDwayne GriffenNo ratings yet
- ATI ChildDocument9 pagesATI Childianshirow834No ratings yet
- Care of The NewbornDocument3 pagesCare of The NewbornJohn Wendell BuñagNo ratings yet
- Sandra John - Case Scenario On Normal NewbornDocument9 pagesSandra John - Case Scenario On Normal NewbornsandraNo ratings yet
- NLE Practice Exam With AnswersDocument43 pagesNLE Practice Exam With AnswersSuzette Rae TateNo ratings yet
- Chapter 30: Health Assessment and Physical Examination: Test BankDocument23 pagesChapter 30: Health Assessment and Physical Examination: Test BankNurse UtopiaNo ratings yet
- Strategies For Ensuring Healthcare Systems Preparedness and Optimizing N95 SuppliesDocument29 pagesStrategies For Ensuring Healthcare Systems Preparedness and Optimizing N95 SuppliesKmz QwzNo ratings yet
- Comprehensive Exam 1Document19 pagesComprehensive Exam 1karenkaren09100% (1)
- Health Promotion and MaintenanceDocument36 pagesHealth Promotion and MaintenanceJay-Dee Evangelista PacionNo ratings yet
- Full Download Test Bank For Foundations of Maternal Newborn and Womens Health Nursing 7th Edition by Murray PDF Full ChapterDocument32 pagesFull Download Test Bank For Foundations of Maternal Newborn and Womens Health Nursing 7th Edition by Murray PDF Full Chaptergodly.ypsiloid.h6ms2100% (16)
- Test Bank For Foundations of Maternal Newborn and Womens Health Nursing 7th Edition by MurrayDocument36 pagesTest Bank For Foundations of Maternal Newborn and Womens Health Nursing 7th Edition by Murraysolutive.zamboowtmcu100% (43)
- Practice Questions 1-9 (FINAL)Document38 pagesPractice Questions 1-9 (FINAL)Riz Austria RN0% (1)
- NCLEX Practice Exam For Pediatric Nursing 1: Start StartDocument9 pagesNCLEX Practice Exam For Pediatric Nursing 1: Start StartLot RositNo ratings yet
- MATERNALDocument26 pagesMATERNALadisdjkfbNo ratings yet
- NP4 Nov 2022Document12 pagesNP4 Nov 2022cacaass100% (1)
- Chapter 29: The Child With A Genitourinary Condition Leifer: Introduction To Maternity and Pediatric Nursing, 8th EditionDocument6 pagesChapter 29: The Child With A Genitourinary Condition Leifer: Introduction To Maternity and Pediatric Nursing, 8th Editionterri heimNo ratings yet
- Pedia Old eDocument11 pagesPedia Old eDivynne MadeloNo ratings yet
- A Study To Assess The Knowledge Regarding Newborn Danger Signs Among Staff Nurses in Selected Hospital in Kanpur, Uttar Pradesh With A View To Develop An Information BookletDocument7 pagesA Study To Assess The Knowledge Regarding Newborn Danger Signs Among Staff Nurses in Selected Hospital in Kanpur, Uttar Pradesh With A View To Develop An Information BookletEditor IJTSRDNo ratings yet
- BMJ 25-09Document14 pagesBMJ 25-09Kiran ShahNo ratings yet
- Test Bank For Foundations of Maternal Newborn and Womens Health Nursing 7th Edition by MurrayDocument6 pagesTest Bank For Foundations of Maternal Newborn and Womens Health Nursing 7th Edition by Murrayfarahflorav1lkiNo ratings yet
- Full Test BankDocument1 pageFull Test Bankjwjimmy20No ratings yet
- Quizzes SubsDocument36 pagesQuizzes SubsApril Mae Agomo-oNo ratings yet
- Child Evolve ExamDocument37 pagesChild Evolve Examfriendofnurse100% (14)
- NUR 145 - SAS 16-18 Activity For THF GroupDocument10 pagesNUR 145 - SAS 16-18 Activity For THF Groupella retizaNo ratings yet
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 59Document12 pagesMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 59sarasjunkNo ratings yet
- Diagnostic Exam Funda ReviewDocument13 pagesDiagnostic Exam Funda Reviewmark OrpillaNo ratings yet
- Chickenpox Case StudyDocument12 pagesChickenpox Case Studywan yuen kiNo ratings yet
- NCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!From EverandNCLEX: Pharmacology for Nurses: 100 Practice Questions with Rationales to help you Pass the NCLEX!Rating: 5 out of 5 stars5/5 (4)
- The Prospective Mother, a Handbook for Women During PregnancyFrom EverandThe Prospective Mother, a Handbook for Women During PregnancyNo ratings yet
- NICU Journal: A Parent's JourneyFrom EverandNICU Journal: A Parent's JourneyNo ratings yet
- Telephone Assessment in Primary Care: A practical guide to effective consultation and triageFrom EverandTelephone Assessment in Primary Care: A practical guide to effective consultation and triageNo ratings yet
- Nursing Care Plan #1 Mental HealthDocument13 pagesNursing Care Plan #1 Mental HealthNursyNurseNo ratings yet
- 3 Chapter 29 Practice Questions CardioDocument17 pages3 Chapter 29 Practice Questions CardioNursyNurseNo ratings yet
- Mental Status Assessment#2Document5 pagesMental Status Assessment#2NursyNurseNo ratings yet
- Online Connect Verbatim Report (Sample)Document5 pagesOnline Connect Verbatim Report (Sample)NursyNurseNo ratings yet
- Verbatim 1Document10 pagesVerbatim 1NursyNurseNo ratings yet
- Dosage Titration PresentationDocument17 pagesDosage Titration PresentationNursyNurseNo ratings yet
- Skin Pediatric NotesDocument8 pagesSkin Pediatric NotesNursyNurseNo ratings yet
- Antidiuretic Hormone: Manifestations of Dehydration-ElderlyDocument15 pagesAntidiuretic Hormone: Manifestations of Dehydration-ElderlyNursyNurseNo ratings yet
- 3 Communicable Diseases NotesDocument3 pages3 Communicable Diseases NotesNursyNurseNo ratings yet
- Dosage Calculation Review Part 2 - Medication DosagesDocument2 pagesDosage Calculation Review Part 2 - Medication DosagesNursyNurseNo ratings yet
- Dosage Calculation Review Part 1 - ConversionsDocument4 pagesDosage Calculation Review Part 1 - ConversionsNursyNurseNo ratings yet
- Dosage Calculation Review Part 3 - Flow Rate CalculationsDocument3 pagesDosage Calculation Review Part 3 - Flow Rate CalculationsNursyNurseNo ratings yet
- Pedi Math Packet 2016-2017-1Document26 pagesPedi Math Packet 2016-2017-1NursyNurseNo ratings yet
- Dosage by Weight Exercises and AnswersDocument3 pagesDosage by Weight Exercises and AnswersNursyNurseNo ratings yet
- Procedure Checklist Chapter 26, Skill 26-04: Obtaining A Wound CultureDocument1 pageProcedure Checklist Chapter 26, Skill 26-04: Obtaining A Wound CultureNursyNurseNo ratings yet
- Procedure Checklist Chapter 38, Skill 38-01: Administering IV Medication Via PRN Lock or IV LineDocument2 pagesProcedure Checklist Chapter 38, Skill 38-01: Administering IV Medication Via PRN Lock or IV LineNursyNurseNo ratings yet
- Procedure Checklist Chapter 34, Skill 34-02: Performing VenipunctureDocument3 pagesProcedure Checklist Chapter 34, Skill 34-02: Performing VenipunctureNursyNurseNo ratings yet
- Exam 1 Slides APDocument13 pagesExam 1 Slides APNursyNurseNo ratings yet
- BNS Exam 4 CH 31 Book Review Questions, Questions Taken From Key Points, and Within Book - Details - Kahoot!Document32 pagesBNS Exam 4 CH 31 Book Review Questions, Questions Taken From Key Points, and Within Book - Details - Kahoot!NursyNurseNo ratings yet
- Procedure Checklist Chapter 37, Skill 37-01: Reconstituting and Withdrawing Medication From A VialDocument2 pagesProcedure Checklist Chapter 37, Skill 37-01: Reconstituting and Withdrawing Medication From A VialNursyNurseNo ratings yet
- BNS Insulins & Other Meds We Covered - Details - Kahoot!Document22 pagesBNS Insulins & Other Meds We Covered - Details - Kahoot!NursyNurseNo ratings yet
- Important Slides Nutrition ch5Document18 pagesImportant Slides Nutrition ch5NursyNurseNo ratings yet
- Common Subcutaneous Medications Check Off - Details - Kahoot!Document9 pagesCommon Subcutaneous Medications Check Off - Details - Kahoot!NursyNurseNo ratings yet
- BNS Exam 4 2021 - Details - Kahoot!Document6 pagesBNS Exam 4 2021 - Details - Kahoot!NursyNurseNo ratings yet
- DVT And/or PE Treatment Dosage For Tinzaparin (Innohep®)Document1 pageDVT And/or PE Treatment Dosage For Tinzaparin (Innohep®)Kok Hui DiongNo ratings yet
- Psychology Major Total Credits: 40: Academic Advisement CenterDocument2 pagesPsychology Major Total Credits: 40: Academic Advisement CenterCNo ratings yet
- Kuang Yeu Medical Model FrontierDocument48 pagesKuang Yeu Medical Model FrontierSeyed Mohammad Hossein EmamiNo ratings yet
- Oil and Gas: Safety Passport (Ogsp)Document10 pagesOil and Gas: Safety Passport (Ogsp)kerolcarroll100% (1)
- Appendix 1 Ins GCP 4 Procedure Reporting GCP Inspections Requested CHMP GCP Inspection Report - enDocument31 pagesAppendix 1 Ins GCP 4 Procedure Reporting GCP Inspections Requested CHMP GCP Inspection Report - enAbhijeetNo ratings yet
- Body Piercing and Tattoos: A Survey On Young Adults ' Knowledge of The Risks and Practices in Body ArtDocument8 pagesBody Piercing and Tattoos: A Survey On Young Adults ' Knowledge of The Risks and Practices in Body ArtIliana StrahilovaNo ratings yet
- Components of WellnessDocument3 pagesComponents of WellnessMuhammad Abdul AzimNo ratings yet
- Senior Thesis 2022Document19 pagesSenior Thesis 2022api-608954316No ratings yet
- Well Test Knowledge InternationalDocument13 pagesWell Test Knowledge InternationalTheNourEldenNo ratings yet
- May 15, 2023 - AssignmentDocument6 pagesMay 15, 2023 - AssignmentMARY FORTUNE MAE RAMONESNo ratings yet
- Edmonton Police AssociationDocument3 pagesEdmonton Police AssociationEmily MertzNo ratings yet
- Exploring The Factors Affecting Teacher's Effectiveness in Higher Education: An Empirical Analysis of District Gujranwala, PakistanDocument17 pagesExploring The Factors Affecting Teacher's Effectiveness in Higher Education: An Empirical Analysis of District Gujranwala, PakistanSirajudinNo ratings yet
- CPR 2Document3 pagesCPR 2Baebee Lou100% (1)
- Journal of Interventional Medicine: Yanli Wang, Guohao Huang, Tian Jiang, Xinwei HanDocument5 pagesJournal of Interventional Medicine: Yanli Wang, Guohao Huang, Tian Jiang, Xinwei HanDzulRizkaNo ratings yet
- Simple Keys To Small Business Success: Marriage Licenses Marriage Licenses Marriage LicensesDocument1 pageSimple Keys To Small Business Success: Marriage Licenses Marriage Licenses Marriage LicensesSabrina BatesNo ratings yet
- Basic Personality InventoryDocument8 pagesBasic Personality InventoryElisa Mae Oranza Gura100% (1)
- Why Use KYKO Personality TestDocument1 pageWhy Use KYKO Personality TestBernard Ah Thau TanNo ratings yet
- (PEDIA) 2.04 Pediatric Neurologic Exam - Dr. Rivera PDFDocument15 pages(PEDIA) 2.04 Pediatric Neurologic Exam - Dr. Rivera PDFJudith Dianne IgnacioNo ratings yet
- The Self-Concept Revisited: or A Theory of A TheoryDocument13 pagesThe Self-Concept Revisited: or A Theory of A TheoryShams JhugrooNo ratings yet
- Anti-Coagulant (Vte in Obstetrics) - Madam LiewDocument10 pagesAnti-Coagulant (Vte in Obstetrics) - Madam LiewNana YunusNo ratings yet
- Must/Mustn't/Have To/don't Have ToDocument1 pageMust/Mustn't/Have To/don't Have ToKaren VelandiaNo ratings yet
- Syllabus Small Bowel ObstructionDocument4 pagesSyllabus Small Bowel ObstructionHARVEY SELIM0% (1)
- Ranny Armainis-21033112-Exercise Week 8 Bahasa InggrisDocument3 pagesRanny Armainis-21033112-Exercise Week 8 Bahasa InggrisRanny ArmainisNo ratings yet
- GanglionDocument10 pagesGanglionJunben DelacruzNo ratings yet
- Self ch2 p2Document18 pagesSelf ch2 p2akypc9No ratings yet
- Q A6 - Allocated QuestionsDocument3 pagesQ A6 - Allocated QuestionsadishsewlallNo ratings yet
- Contemporary Behavior TherapyDocument1 pageContemporary Behavior TherapyEv PresentacionNo ratings yet
- Behaviorism 2Document13 pagesBehaviorism 2genegeneNo ratings yet
- Part Time Vs Full Time Wear of Twin Block - Parekh2019Document8 pagesPart Time Vs Full Time Wear of Twin Block - Parekh2019rohitNo ratings yet
- Psychophysiological Methods in NeuroscienceDocument17 pagesPsychophysiological Methods in NeuroscienceKariela EstherNo ratings yet