Professional Documents
Culture Documents
A Novel Technique To Correct Kyphosis in Cervical Posterior Longitudinal Ligament
Uploaded by
bosnia agusOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Novel Technique To Correct Kyphosis in Cervical Posterior Longitudinal Ligament
Uploaded by
bosnia agusCopyright:
Available Formats
TECHNICAL NOTE
J Neurosurg Spine 26:325–330, 2017
A novel technique to correct kyphosis in cervical
myelopathy due to continuous-type ossification of the
posterior longitudinal ligament
Dong-Ho Lee, MD, PhD, Youn-Suk Joo, MD, Chang Ju Hwang, MD, PhD,
Choon Sung Lee, MD, PhD, and Jae Hwan Cho, MD
Department of Orthopedic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
OBJECTIVE Although posterior decompressive surgery is widely used to treat patients with cervical myelopathy and
multilevel ossification of the posterior longitudinal ligament (OPLL), a poor outcome is anticipated if the sagittal alignment
is kyphotic (or K-line negative). Accordingly, it is mandatory to perform anterior decompression and fusion in patients
with cervical kyphosis. However, it can be difficult to perform anterior surgery because of the high risk of complications.
This present report proposes a novel “greenstick fracture technique” to change the K-line from negative to positive in
patients with cervical myelopathy, OPLL, and kyphotic deformity.
METHODS Four patients with cervical myelopathy, continuous-type OPLL, and kyphotic sagittal alignment (who were
K-line negative) were indicated for surgery. Posterior laminectomy and lateral mass screw insertions using a posterior
approach were performed, followed by anterior surgery. Multilevel discectomy and thinning of the OPLL mass by bur
drilling was performed, then an intentional greenstick fracture at each disc level was made to convert the cervical K-line
from negative to positive. Finally, posterior instrumentation using a rod was carried out to maintain cervical lordosis.
RESULTS MRI showed complete decompression of the cord by posterior migration in all cases, which had been caused
by cervical lordosis. Restoration of neurological defects was confirmed at the 1-year follow-up assessment. No specific
complications were identified that were associated with this technique.
CONCLUSIONS A greenstick fracture technique may be effective and safe when applied to patients with cervical my-
elopathy, continuous-type OPLL, and kyphotic deformity (K-line negative). However, further studies with more cases will
be required to reveal its generalizability and safety.
https://thejns.org/doi/abs/10.3171/2016.8.SPINE16542
KEY WORDS cervical myelopathy; kyphosis; K-line; anterior surgery; surgical technique
C
ervicalmyelopathy is a common disease that is decompressive surgery was performed in patients with a
associated with hand clumsiness, gait disturbance, kyphotic cervical spine.17,19,20 Therefore, adequate correc-
and/or weakness of the limbs. The mainstay of tion of the cervical sagittal alignment by an anterior ap-
treatment for cervical myelopathy has involved surgery proach is considered to be important in cases of multilevel
because conservative management may only be applicable cervical cord compression with kyphotic deformity.20 To
to mild stenosis and has not generally been considered to restore cervical lordosis, anterior support achieved by in-
be effective in moderate to severe stenosis.14,16,18 However, tervertebral cage insertion may be effective.
many surgical options exist, including anterior decom- However, an anterior approach can be associated with
pression and fusion, posterior laminoplasty, posterior lam- many problems if the cervical myelopathy is caused by
inectomy and fusion, and/or combined surgery.12,21 Levels continuous-type ossification of the posterior longitudinal
of compression and the maintenance of cervical lordosis ligament (OPLL). A risk of CSF leakage, longer operative
have been considered to be two important parameters duration, and/or technical difficulties has been reported
for the selection of appropriate procedures.5,11 In patients to represent a challenge in patients with multilevel OPLL
with multilevel cord compression with a lordotic cervical undergoing anterior decompression. Accordingly, we sug-
spine, a posterior approach may be effective. However, gest herein a novel approach, the “greenstick fracture tech-
poor clinical outcomes have been reported when posterior nique,” that is relatively easy, safe, and clinically effective
ABBREVIATIONS HRQOL = health-related quality of life; JOA = Japanese Orthopaedic Association; NDI = neck disability index; OPLL = ossification of the posterior longi-
tudinal ligament; VAS = visual analog scale.
SUBMITTED May 10, 2016. ACCEPTED August 8, 2016.
INCLUDE WHEN CITING Published online October 28, 2016; DOI: 10.3171/2016.8.SPINE16542.
©AANS, 2017 J Neurosurg Spine Volume 26 • March 2017 325
Unauthenticated | Downloaded 12/30/21 03:05 PM UTC
D. H. Lee et al.
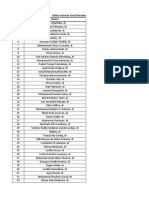
TABLE 1. Baseline characteristics of the 4 patients with cervical myelopathy and continuous-type OPLL
Case Age Symptom Nurick JOA C2–7 Lordosis* Levels of Follow-Up
No. (yrs), Sex Onset (mos) Major Symptoms Grade Score Neutral Flexion Extension OPLL Period
1 68, M 24–36 Hand clumsiness, arm pain 1 13 4 −14 20 C3–4, C5–6 1yr 6 mos
2 55, M 4 Hand clumsiness 1 14 4 −14 15 C4–7 1 yr
3 68, M 120 Gait disturbance, hand clumsiness 2 11 −3 −18 0 C2–5 1 yr
4 62, F 24 Hand clumsiness, arm pain 1 14 −1 −26 3 C2–6 1 yr
The preoperative K-line was negative in all cases.
* A negative value indicates kyphosis.
for restoring cervical lordosis. We aimed in this study to in Fig. 2. On the same day, posterior rod insertion with a
establish a new technique for the treatment of patients compression maneuver between screws was conducted to
with cervical myelopathy that results from multilevel maintain cervical lordosis. After the second stage of sur-
OPLL and kyphosis. gery, patients were cared for in the intensive care unit for
1 day to monitor airway function and to assess whether it
Methods was compromised.
Patient Population
Patients with cervical myelopathy, continuous-type Results
OPLL, and kyphotic sagittal alignment (who were K-line All 4 patients exhibited improvement of both subjec-
negative) were indicated for surgery. A total of 4 patients tive symptoms and clinical scores. Arm pain VAS scores
were retrospectively reviewed in this study. All patients decreased (from 6 to 0, from 3 to 0, from 5 to 3, and from
exhibited cervical myelopathy–related symptoms upon 8 to 5) and JOA scores improved (from 13 to 16, from 14
cord compression with continuous-type OPLL and sagit- to 17, from 11 to 13, and from 14 to 17) in the postopera-
tal kyphotic alignment. A visual analog scale (VAS) was tive 1-year period. HRQOL also showed overall improve-
used to measure neck pain and arm pain. A neck disabil- ment in all patients (Table 2). In 1 patient (Case 1), C-5
ity index (NDI) and Japanese Orthopaedic Association nerve palsy was observed after the first stage of surgery.
(JOA) score were used to assess the degree of disability. Additional total foraminotomy was performed on the left
Health-related quality of life (HRQOL) was measured us- C4–5 level and bilateral C5–6 level at the second stage of
ing SF-36 scores. All patients were followed-up for 1 year the operation. However, deltoid power in this patient fully
postoperatively. Basic patient demographic data, symp- recovered by 1 month postoperatively. Otherwise, no spe-
toms, and radiological characteristics are summarized in cific complications were identified. The mean operative
Table 1. All cases exhibited cord compression by multi- time was 128.5 and 265.0 minutes in the first and second
level OPLL and the loss of cervical lordosis. Among the 4 stages of the operation, respectively. The mean estimated
patients, 2 (Cases 3 and 4) did not show cervical lordosis blood loss was 200 and 350 ml in the first and second
in the extension position. An example (Case 1) is shown in stages of the operation, respectively. None of the patients
Fig. 1. This study was approved by the institutional review received a blood transfusion.
board of our institution, which waived the requirement for Radiological parameters regarding cervical sagittal
informed consent due to the retrospective nature of the alignment improved postoperatively. C2–7 lordosis was
study. restored in the 4 patients from 4° to 27°, from 4° to 18°,
from −3° to 23°, and from −1° to 26°. Postoperative lat-
Surgical Technique eral radiographs revealed cervical lordosis that was K-line
In general, posterior surgery was initially performed. positive in all cases and postoperative MRI showed no
Then, anterior and posterior surgeries were planned 1 week compressive lesions. Examples (Cases 3 and 4) are shown
later. Using a posterior midline approach, a total laminec- in Figs. 3 and 4.
tomy was performed from C-3 to C-6. An additional par-
tial laminectomy (undercutting) was performed in C-2 or
C-7. Then, lateral mass screws were inserted from C-3 to Discussion
C-6 and laminar and pedicle screws were inserted in C-2 Cervical myelopathy resulting from OPLL is a com-
and C-7, respectively. At 1 week after the initial posterior mon condition that can lead to cervical cord compression
surgery, anterior surgery was performed. Using a Smith- and requires surgical decompression.1,3 Although the se-
Robinson approach, the C3–7 disc space was exposed. At lection of an anterior or posterior approach has been the
each disc level, thinning of the OPLL mass was achieved subject of debate, multilevel cord compression by OPLL
by bur drilling following discectomy. Without attempt- and preoperative lordotic sagittal alignment are conditions
ing complete excision of the OPLL mass, an incomplete that favor a posterior approach.11 However, many studies
fracture was created in the shallow OPLL mass with a have shown that poor clinical and radiological outcomes
laminar spreader. A lordotic allocage was then inserted at may occur if posterior laminoplasty or laminectomy is
each disc level to restore cervical lordosis. This procedure, performed in patients with cervical kyphosis.4,19,20 Thus,
termed the “greenstick fracture technique,” is illustrated it is predicted that favorable outcomes should be expected
326 J Neurosurg Spine Volume 26 • March 2017
Unauthenticated | Downloaded 12/30/21 03:05 PM UTC
Greenstick fracture technique to correct kyphosis
FIG. 1. Case 1. Images obtained in a 68-year-old man who exhibited clumsiness in both hands as well as pain with numbness
in both hands for 2–3 years. A: Preoperative plain lateral radiographs showing that an OPLL mass (dashed line) touched the
K-line. B: Flexion and extension lateral radiographs. C: A lateral reconstructed CT image showing an OPLL mass. D: A double-
layer sign (arrow) shown on an axial CT scan.
FIG. 2. Illustration of the mechanism underlying the greenstick fracture technique. A: Huge OPLL mass (gray area) with a
kyphotic deformity that was K-line negative. B: Thinning of the OPLL mass at each disc level. C: A greenstick fracture with an
interbody cage results in restoration of cervical lordosis (K-line positive). Figure is available in color online only.
J Neurosurg Spine Volume 26 • March 2017 327
Unauthenticated | Downloaded 12/30/21 03:05 PM UTC
D. H. Lee et al.
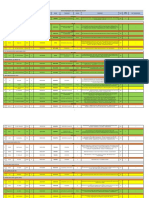
TABLE 2. Pre- and postoperative HRQOL scores be a reliable indicator that may predict outcomes follow-
Case NDI SF-36 PCS SF-36 MCS ing posterior surgery in patients with cervical myelopathy
and OPLL.7 The K-line is the line that connects the mid-
No. Preop Postop Preop Postop Preop Postop
point of the vertebral canal at the levels of C-2 and C-7 on
1 13 11 33.8 45.2 47 49.9 the lateral radiograph.7 It has been suggested that a suf-
2 0 4 41.4 57.7 48 52.9 ficient posterior shift of the cord will not be obtained af-
3 17 7 18.2 27.4 40.5 54.6 ter posterior decompressive surgery in the K-line negative
group.7 Accordingly, if the protruding OPLL mass touches
4 5 17 37.6 39.1 40.6 44.1
the K-line (K-line negative), even with a lordotic cervical
MCS = mental component summary; PCS = physical component summary. spine, patient outcomes following posterior laminoplasty
will not be favorable because cord compression can re-
main. However, the K-line itself represents a modifiable
when cervical lordosis is maintained because it can permit parameter. Thus, we proposed to change the K-line itself
a backward shift of the cord.4 However, the cutoff value in our present study by restoring cervical lordosis.
of kyphosis for a favorable outcome is also the subject of To convert cases from K-line negative to positive, an
debate. According to one study, a good outcome may be anterior approach is recommended in cases with mul-
anticipated when posterior laminoplasty is performed if tilevel OPLL. Anterior decompression with fusion has
the degree of kyphosis is less than 10°.20 been associated with improved postoperative neurological
In this context, the K-line concept has been proposed to function when used for patients with multilevel cervical
FIG. 3. Case 3. Images from a 68-year-old man who exhibited hand clumsiness and slowly progressive gait disturbance for 10
years. A: Preoperative lateral radiograph showing that the patient was K-line negative. Dashed line indicates the OPLL mass.
B: Dynamic lateral radiographs showing an inability to extend the neck. C: A huge continuous OPLL mass (arrows) shown on a
sagittal CT reconstruction image. D: Severe cord compression revealed on a sagittal T2-weighted MR image. E: A postoperative
lateral radiograph showing that this patient was K-line positive. F: Sagittal CT reconstruction image showing the remaining thin
OPLL mass (arrows). G: A well-decompressed state was revealed by sagittal MRI.
328 J Neurosurg Spine Volume 26 • March 2017
Unauthenticated | Downloaded 12/30/21 03:05 PM UTC
Greenstick fracture technique to correct kyphosis
compressive myelopathy.9,12 However, for anterior surgery OPLL and preoperative kyphotic alignment.15 However,
in patients with OPLL, it has been reported that this ap- this technique was associated with many complications,
proach is technically demanding and associated with a such as nonunion, graft trouble, and a difficult learning
higher incidence of operation-related complications.1,9 curve.6,10 These disadvantages can be overcome by our
These complications included the risk of a dural tear or novel technique, which does not require corpectomy or
CSF leakage, which was difficult to repair in anterior cer- complete anterior decompression; thus, it is technically
vical surgery.2,13 The incidence of dural tear and CSF leak- easier than the conventional floating technique. Further-
age has been reported to be 13.7-fold greater in patients more, a 2-stage operation also has advantages because
with OPLL compared with patients affected by other longer operative time itself can be a risk factor for peri-
conditions.8 It has also been reported that CSF leakage operative complications, and some procedures such as ad-
frequently occurs when a double-layer sign can be identi- ditional foraminotomy can be added in the second stage
fied by a CT scan, which also occurred in our cases (Fig. of the operation if arm pain persists or neurological deficit
1D).22 Thus, aggressive attempts to remove a whole OPLL such as C-5 nerve palsy develops. However, this technique
mass may increase the risk of a dural tear, which could has been performed in only 4 patients, so its generalizabil-
hinder the delicate surgical process and lead to second- ity is questionable. Furthermore, possible complications
ary complications, such as infections or wound problems. related to long operative time and deformity correction
Our greenstick fracture technique has been developed to should be considered, although fortunately they were not
convert the K-line by restoring cervical lordosis without found in these cases.
the risk of a dural tear or CSF leakage. Previously, an To summarize, a greenstick fracture technique repre-
anterior floating method combined with corpectomy has sents a relatively easy and safe procedure that can be used
been used, which may be suitable for cases with massive in patients with cervical myelopathy, continuous-type
FIG. 4. Case 4. Images obtained in a 62-year-old woman who exhibited hand clumsiness and right-sided arm pain for 2 years.
A: Preoperative lateral radiograph showing an OPLL mass (dashed line) and kyphotic deformity that was K-line negative. B: Dy-
namic lateral radiographs showing an inability to extend the neck. C: Continuous-type OPLL mass at the C2–6 level shown on a
sagittal CT reconstruction image. D: Postoperative lateral radiograph showing the lordotic alignment, K-line positive. E: Sagittal
CT reconstruction image demonstrating the remaining thin OPLL mass (arrows).
J Neurosurg Spine Volume 26 • March 2017 329
Unauthenticated | Downloaded 12/30/21 03:05 PM UTC
D. H. Lee et al.
OPLL, and kyphotic alignment. Both complete decom- 15. Sakai K, Okawa A, Takahashi M, Arai Y, Kawabata S, Eno-
pression of the cord and restoration of cervical lordosis can moto M, et al: Five-year follow-up evaluation of surgical
be achieved using this technique. However, further studies treatment for cervical myelopathy caused by ossification of
the posterior longitudinal ligament: a prospective compara-
with more cases will be required to reveal its generaliz- tive study of anterior decompression and fusion with floating
ability and safety. method versus laminoplasty. Spine (Phila Pa 1976) 37:367–
376, 2012
References 16. Sampath P, Bendebba M, Davis JD, Ducker TB: Outcome of
patients treated for cervical myelopathy. A prospective, mul-
1. An HS, Al-Shihabi L, Kurd M: Surgical treatment for ossifi- ticenter study with independent clinical review. Spine (Phila
cation of the posterior longitudinal ligament in the cervical Pa 1976) 25:670–676, 2000
spine. J Am Acad Orthop Surg 22:420–429, 2014 17. Shamji MF, Ames CP, Smith JS, Rhee JM, Chapman JR,
2. Cardoso MJ, Koski TR, Ganju A, Liu JC: Approach-related Fehlings MG: Myelopathy and spinal deformity: relevance of
complications after decompression for cervical ossification spinal alignment in planning surgical intervention for degen-
of the posterior longitudinal ligament. Neurosurg Focus erative cervical myelopathy. Spine (Phila Pa 1976) 38 (22
30(3):E12, 2011 Suppl 1):S147–S148, 2013
3. Choi BW, Song KJ, Chang H: Ossification of the posterior 18. Shimomura T, Sumi M, Nishida K, Maeno K, Tadokoro K,
longitudinal ligament: a review of literature. Asian Spine J Miyamoto H, et al: Prognostic factors for deterioration of
5:267–276, 2011 patients with cervical spondylotic myelopathy after nonsurgi-
4. Denaro V, Longo UG, Berton A, Salvatore G, Denaro L: cal treatment. Spine (Phila Pa 1976) 32:2474–2479, 2007
Favourable outcome of posterior decompression and stabi- 19. Suda K, Abumi K, Ito M, Shono Y, Kaneda K, Fujiya M: Lo-
lization in lordosis for cervical spondylotic myelopathy: the cal kyphosis reduces surgical outcomes of expansive open-
spinal cord “back shift” concept. Eur Spine J 24 (Suppl door laminoplasty for cervical spondylotic myelopathy. Spine
7):826–831, 2015 (Phila Pa 1976) 28:1258–1262, 2003
5. Emery SE: Anterior approaches for cervical spondylotic 20. Uchida K, Nakajima H, Sato R, Yayama T, Mwaka ES, Ko-
myelopathy: which? when? how? Eur Spine J 24 (Suppl bayashi S, et al: Cervical spondylotic myelopathy associated
2):150–159, 2015 with kyphosis or sagittal sigmoid alignment: outcome after
6. Emery SE, Bohlman HH, Bolesta MJ, Jones PK: Anterior anterior or posterior decompression. J Neurosurg Spine
cervical decompression and arthrodesis for the treatment 11:521–528, 2009
of cervical spondylotic myelopathy. Two to seventeen-year 21. Woods BI, Hohl J, Lee J, Donaldson W III, Kang J: Lamino-
follow-up. J Bone Joint Surg Am 80:941–951, 1998 plasty versus laminectomy and fusion for multilevel cervical
7. Fujiyoshi T, Yamazaki M, Kawabe J, Endo T, Furuya T, Koda spondylotic myelopathy. Clin Orthop Relat Res 469:688–
M, et al: A new concept for making decisions regarding the 695, 2011
surgical approach for cervical ossification of the posterior 22. Yang H, Yang L, Chen D, Wang X, Lu X, Yuan W: Implica-
longitudinal ligament: the K-line. Spine (Phila Pa 1976) tions of different patterns of “double-layer sign” in cervical
33:E990–E993, 2008 ossification of the posterior longitudinal ligament. Eur Spine
8. Hannallah D, Lee J, Khan M, Donaldson WF, Kang JD: J 24:1631–1639, 2015
Cerebrospinal fluid leaks following cervical spine surgery. J
Bone Joint Surg Am 90:1101–1105, 2008
9. Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y,
Yonenobu K, et al: Surgical strategy for cervical myelopathy
due to ossification of the posterior longitudinal ligament: Part
2: Advantages of anterior decompression and fusion over Disclosures
laminoplasty. Spine (Phila Pa 1976) 32:654–660, 2007 The authors report no conflict of interest concerning the materi-
10. Kumar GS, Rajshekhar V: Acute graft extrusion following als or methods used in this study or the findings specified in this
central corpectomy in patients with cervical spondylotic my- paper.
elopathy and ossified posterior longitudinal ligament. J Clin
Neurosci 16:373–377, 2009
11. Lawrence BD, Shamji MF, Traynelis VC, Yoon ST, Rhee JM,
Author Contributions
Chapman JR, et al: Surgical management of degenerative Conception and design: Cho, DH Lee. Acquisition of data: Joo.
cervical myelopathy: a consensus statement. Spine (Phila Pa Analysis and interpretation of data: Joo. Drafting the article: Cho.
1976) 38 (22 Suppl 1):S171–S172, 2013 Critically revising the article: Cho, DH Lee, Hwang, CS Lee.
12. Liu X, Wang H, Zhou Z, Jin A: Anterior decompression and Reviewed submitted version of manuscript: DH Lee, CS Lee.
fusion versus posterior laminoplasty for multilevel cervical Approved the final version of the manuscript on behalf of all
compressive myelopathy. Orthopedics 37:e117–e122, 2014 authors: Cho. Statistical analysis: Joo. Administrative/technical/
13. Mazur M, Jost GF, Schmidt MH, Bisson EF: Management material support: DH Lee, Hwang, CS Lee. Study supervision:
of cerebrospinal fluid leaks after anterior decompression for Hwang, CS Lee.
ossification of the posterior longitudinal ligament: a review of
the literature. Neurosurg Focus 30(3):E13, 2011 Correspondence
14. Rhee JM, Shamji MF, Erwin WM, Bransford RJ, Yoon ST, Jae Hwan Cho, Department of Orthopedic Surgery, Asan Medi-
Smith JS, et al: Nonoperative management of cervical my- cal Center, University of Ulsan College of Medicine, 388-1,
elopathy: a systematic review. Spine (Phila Pa 1976) 38 (22 PungNap-2-dong, SongPa-gu, Seoul, Korea. email: spinecjh@
Suppl 1):S55–S67, 2013 gmail.com.
330 J Neurosurg Spine Volume 26 • March 2017
Unauthenticated | Downloaded 12/30/21 03:05 PM UTC
You might also like
- Disorders of the Patellofemoral Joint: Diagnosis and ManagementFrom EverandDisorders of the Patellofemoral Joint: Diagnosis and ManagementNo ratings yet
- Surgical Outcomes of Posterior Spinal Fusion Alone Using Cervical Pedicle ScrewDocument26 pagesSurgical Outcomes of Posterior Spinal Fusion Alone Using Cervical Pedicle ScrewprototyposNo ratings yet
- Spinal Tumor Surgery: A Case-Based ApproachFrom EverandSpinal Tumor Surgery: A Case-Based ApproachDaniel M. SciubbaNo ratings yet
- Supine Cervical Traction After Anterior Cervical Diskectomy and FusionDocument4 pagesSupine Cervical Traction After Anterior Cervical Diskectomy and FusionOscar NgNo ratings yet
- Endoscopic Procedures on the SpineFrom EverandEndoscopic Procedures on the SpineJin-Sung KimNo ratings yet
- Ventral Correction of Postsurgical Cervical KyphosisDocument7 pagesVentral Correction of Postsurgical Cervical Kyphosis박진영No ratings yet
- Blizzard 2016Document9 pagesBlizzard 2016febyan yohanesNo ratings yet
- Surgical Technique: Vertebral Column Resection (VCR) For Severe Pediatric and Adult Spinal DeformityDocument23 pagesSurgical Technique: Vertebral Column Resection (VCR) For Severe Pediatric and Adult Spinal DeformityPeter Paul PascualNo ratings yet
- mcrae2015Document8 pagesmcrae2015Ananth BalakrishnanNo ratings yet
- Surgical Outcome of Scoliosis in Marfan Syndrome: A Case Series ReportDocument6 pagesSurgical Outcome of Scoliosis in Marfan Syndrome: A Case Series ReportMachfud SidiqNo ratings yet
- 11 - 2015 - Outcome Acetabuloplastia y Osteotomia VarizantesDocument8 pages11 - 2015 - Outcome Acetabuloplastia y Osteotomia VarizantesDaniel Alejandro Sini RiosNo ratings yet
- Laminoplasty Versus Laminectomy With Posterior Spinal Fusion For Multilevel Cervical Spondylotic MyelopathyDocument10 pagesLaminoplasty Versus Laminectomy With Posterior Spinal Fusion For Multilevel Cervical Spondylotic Myelopathyfebyan yohanesNo ratings yet
- Wolff 2019Document7 pagesWolff 2019Christopher BermeoNo ratings yet
- Scapular Winging TreatmentDocument10 pagesScapular Winging TreatmentludimilaGNo ratings yet
- Transforaminal Lumbar Interbody Fusion (TLIF) : Assessment of Clinical and Radiological OutcomeDocument6 pagesTransforaminal Lumbar Interbody Fusion (TLIF) : Assessment of Clinical and Radiological OutcomeJosh JoshiNo ratings yet
- J Neurosurg Spine Article p535Document6 pagesJ Neurosurg Spine Article p535wilsonwqaNo ratings yet
- Woods 2010Document8 pagesWoods 2010febyan yohanesNo ratings yet
- Open Capsular Shift For Multi Directional Shoulder InstabilityDocument4 pagesOpen Capsular Shift For Multi Directional Shoulder InstabilityWaqas HaleemNo ratings yet
- SEGUIMIENTO A 5 AÑOS PTGH REVERSADocument7 pagesSEGUIMIENTO A 5 AÑOS PTGH REVERSAmarcelogascon.oNo ratings yet
- Primary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesDocument10 pagesPrimary Total Shoulder Arthroplasty Performed Entirely Thru The Rotator Interval - Technique and Minimum Two-Year OutcomesmotohumeresNo ratings yet
- Case Report Proximal Adding On WANDocument19 pagesCase Report Proximal Adding On WANNugroho Tri WibowoNo ratings yet
- Girdle Stone Procedure in Bilateral Rheumatoid Hip: A Case ReportDocument2 pagesGirdle Stone Procedure in Bilateral Rheumatoid Hip: A Case Reportumer ilyasNo ratings yet
- Journal Neurosurgery SpineDocument3 pagesJournal Neurosurgery SpineWidi Nugraha HadianNo ratings yet
- Conunterclock WiseDocument5 pagesConunterclock WiseEduardo HernándezNo ratings yet
- Fingertip Injury 19Document5 pagesFingertip Injury 19Mukhamad Arif MunandarNo ratings yet
- 2022 Progress OpllDocument14 pages2022 Progress Opll정광익No ratings yet
- Allograft Medial Patellofemoral LigamentDocument11 pagesAllograft Medial Patellofemoral Ligamenttyoinfantil.hegcNo ratings yet
- Surgical Treatment of Tuberculous SpondylodiscitisDocument7 pagesSurgical Treatment of Tuberculous SpondylodiscitisindraNo ratings yet
- 2013 4 Spine12876Document9 pages2013 4 Spine12876Rendy SusantoNo ratings yet
- Fsurg 08 662720Document6 pagesFsurg 08 662720Deborah SalinasNo ratings yet
- Sun 2015Document5 pagesSun 2015febyan yohanesNo ratings yet
- What's New in Spine Surgery: Specialty UpdateDocument11 pagesWhat's New in Spine Surgery: Specialty UpdatePoliceNo ratings yet
- Sebastian Ruetten, MD, PHD, Martin Komp, MD, PHD, and Georgios Godolias, MD, ProfDocument9 pagesSebastian Ruetten, MD, PHD, Martin Komp, MD, PHD, and Georgios Godolias, MD, ProfKaustubh KeskarNo ratings yet
- Use of Allograft in Skeletally Immature Patients For Calcaneal Neck Lengthening OsteotomyDocument5 pagesUse of Allograft in Skeletally Immature Patients For Calcaneal Neck Lengthening OsteotomyMonem ShakeerNo ratings yet
- Paper 03-02-2012 PDFDocument6 pagesPaper 03-02-2012 PDFfalmvenNo ratings yet
- (Journal of Neurosurgery - Spine) The Lateral Extracavitary Approach To The Thoracolumbar Spine - A Case Series and Systematic ReviewDocument10 pages(Journal of Neurosurgery - Spine) The Lateral Extracavitary Approach To The Thoracolumbar Spine - A Case Series and Systematic Reviewkarine cim assençoNo ratings yet
- Treatment of Medial Epicondyle Fracture Without Associated Elbow Dislocation in Older Children and AdolescentsDocument7 pagesTreatment of Medial Epicondyle Fracture Without Associated Elbow Dislocation in Older Children and AdolescentsRahma HanifaNo ratings yet
- 2005 Jpo Distraction For Bayne Type 4Document5 pages2005 Jpo Distraction For Bayne Type 4MeetJainNo ratings yet
- Magnesium AbstractDocument1 pageMagnesium Abstracthkw8g5snyxNo ratings yet
- Evaluation of Percutaneous Kirschner Wire Fixation and Early Wrist Joint Exercises in The Management of Displaced Unstable Colles' FracturesDocument10 pagesEvaluation of Percutaneous Kirschner Wire Fixation and Early Wrist Joint Exercises in The Management of Displaced Unstable Colles' FracturesnaluphmickeyNo ratings yet
- Surgical Management of Cervical Ossified Posterior Longitudinal LigamentDocument13 pagesSurgical Management of Cervical Ossified Posterior Longitudinal Ligamentinfobusiness2010No ratings yet
- Revision Surgeries For Adult Spinal DeformityDocument12 pagesRevision Surgeries For Adult Spinal Deformitymetasoniko81No ratings yet
- Raccourcissement Cubitus - Acta Ortho BelgicaDocument6 pagesRaccourcissement Cubitus - Acta Ortho BelgicaLedouxNo ratings yet
- Du 2013Document9 pagesDu 2013febyan yohanesNo ratings yet
- Reparación Artroscopia EscafolunarDocument10 pagesReparación Artroscopia EscafolunarCristina Alvarez BautistaNo ratings yet
- A Modified Boytchev Procedure For Recurrent Anterior Dislocation of The Shoulder Khaled M Mostafa and Kamal El-GafaryDocument9 pagesA Modified Boytchev Procedure For Recurrent Anterior Dislocation of The Shoulder Khaled M Mostafa and Kamal El-GafaryDebangshu KumarNo ratings yet
- MRE2Document6 pagesMRE2Rafael Galan GalanNo ratings yet
- Sten Quist 2016Document5 pagesSten Quist 2016Fernanda AhumadaNo ratings yet
- Percutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsDocument7 pagesPercutaneous Endoscopic Decompression Via Transforaminal Approach For Lumbar Lateral Recess Stenosis in Geriatric PatientsAmina GoharyNo ratings yet
- Examination AAOS 2009 SpineDocument56 pagesExamination AAOS 2009 SpineJulieta PereyraNo ratings yet
- Chung2019 PDFDocument7 pagesChung2019 PDFUmer HussainNo ratings yet
- Kalkaneal OsteotomiDocument11 pagesKalkaneal Osteotomitravma777No ratings yet
- Jurnal tht7Document5 pagesJurnal tht7Tri RominiNo ratings yet
- Artrosis glenohumeral despues de artroscopia Bankart repair a long-term follow-up of 13 yearsDocument6 pagesArtrosis glenohumeral despues de artroscopia Bankart repair a long-term follow-up of 13 yearsmarcelogascon.oNo ratings yet
- Jurnal SkoliosisDocument9 pagesJurnal SkoliosisLidya SiahaanNo ratings yet
- Surgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsDocument8 pagesSurgical Treatment of Chronic Elbow Dislocation Allowing For Early Range of Motion: Operative Technique and Clinical ResultsLuis Carlos HernandezNo ratings yet
- Challenging Because Elderly Patients Are Usually Associated With Severe Cardiovascular ComorbiditiesDocument2 pagesChallenging Because Elderly Patients Are Usually Associated With Severe Cardiovascular ComorbiditiesSamuel Hananiel RoryNo ratings yet
- Tratamento Pós-Operatório Devido À Doença de Peyronie 2Document1 pageTratamento Pós-Operatório Devido À Doença de Peyronie 2vacextensor10No ratings yet
- Wang JL Qiw Liu Yj: Author InformationDocument11 pagesWang JL Qiw Liu Yj: Author InformationVladFelecanNo ratings yet
- MainDocument5 pagesMainRoxa777No ratings yet
- Neurosurgery Report: Head Injury and Cervical Fracture CasesDocument49 pagesNeurosurgery Report: Head Injury and Cervical Fracture Casesbosnia agusNo ratings yet
- Daftar Alamat Email Residen + NPM NC 2020Document4 pagesDaftar Alamat Email Residen + NPM NC 2020bosnia agusNo ratings yet
- Posterior Surgical Approach For Thoracic Burst Fracture And Spinal Cord InjuryDocument11 pagesPosterior Surgical Approach For Thoracic Burst Fracture And Spinal Cord Injurybosnia agusNo ratings yet
- Sinking Skin Flap Syndrome Following Decompressive Craniectomy For Acute Subdural Hemorrhage FinalDocument7 pagesSinking Skin Flap Syndrome Following Decompressive Craniectomy For Acute Subdural Hemorrhage Finalbosnia agusNo ratings yet
- DAFTAR PASIEN BEDAH SARAFDocument2 pagesDAFTAR PASIEN BEDAH SARAFbosnia agusNo ratings yet
- Pasien Poli Kamis, 08 Desember 2022Document1 pagePasien Poli Kamis, 08 Desember 2022bosnia agusNo ratings yet
- Anterior Odontoid Screw FixationDocument22 pagesAnterior Odontoid Screw Fixationbosnia agusNo ratings yet
- Fibrin Clot Formation and Lysis: Basic Mechanisms: Seminars in Thrombosis and Hemostasis February 2000Document15 pagesFibrin Clot Formation and Lysis: Basic Mechanisms: Seminars in Thrombosis and Hemostasis February 2000bosnia agusNo ratings yet
- BN NRDocument51 pagesBN NRbosnia agusNo ratings yet
- ISMT12 - Day 192 - Fardhian - Lateral Retroperitoneal Approach To The Lumbar SpineDocument28 pagesISMT12 - Day 192 - Fardhian - Lateral Retroperitoneal Approach To The Lumbar Spinebosnia agusNo ratings yet
- ISMT12 - Day 169 - Sheila - Spinal MeningitisDocument14 pagesISMT12 - Day 169 - Sheila - Spinal Meningitisbosnia agusNo ratings yet
- Sacral FractureDocument21 pagesSacral Fracturebosnia agusNo ratings yet
- Tumors of SpineDocument13 pagesTumors of Spinebosnia agusNo ratings yet
- Vascular pathologies of the spinal cordDocument22 pagesVascular pathologies of the spinal cordbosnia agusNo ratings yet
- STROBE Checklist Cross-SectionalDocument2 pagesSTROBE Checklist Cross-SectionalAmalia Riska G100% (1)
- ISMT12 - Day 112 - Fardhian - Physical and Neurologic ExaminationDocument26 pagesISMT12 - Day 112 - Fardhian - Physical and Neurologic Examinationbosnia agusNo ratings yet
- Update Pasien NC 05 Maret 2021 Untuk KonsulenDocument1 pageUpdate Pasien NC 05 Maret 2021 Untuk Konsulenbosnia agusNo ratings yet
- ISMT12 - Day 176 - Sheila - Diseases of Gray MatterDocument16 pagesISMT12 - Day 176 - Sheila - Diseases of Gray Matterbosnia agusNo ratings yet
- ISMT12 - Day 112 - Sheila - Case Infection Acute Communicating Hydrocephalus Due To Tuberculous MeningitisDocument29 pagesISMT12 - Day 112 - Sheila - Case Infection Acute Communicating Hydrocephalus Due To Tuberculous Meningitisbosnia agusNo ratings yet
- Laporan Intensif 25 April 2021Document21 pagesLaporan Intensif 25 April 2021bosnia agusNo ratings yet
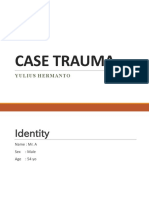
- Case Trauma: Yulius HermantoDocument17 pagesCase Trauma: Yulius Hermantobosnia agusNo ratings yet
- Update Pasien NC 30 Maret 2021 Per DPJPDocument2 pagesUpdate Pasien NC 30 Maret 2021 Per DPJPbosnia agusNo ratings yet
- Update Pasien NC 25 April 2021 Untuk KonsulenDocument2 pagesUpdate Pasien NC 25 April 2021 Untuk Konsulenbosnia agusNo ratings yet
- Update Pasien Bedah Saraf 25 April 2021Document2 pagesUpdate Pasien Bedah Saraf 25 April 2021bosnia agusNo ratings yet
- Siegel 2017Document8 pagesSiegel 2017bosnia agusNo ratings yet
- List Laptop Kisaran 7 JutaDocument5 pagesList Laptop Kisaran 7 Jutabosnia agusNo ratings yet
- Update Pasien NC 25 April 2021 Untuk KonsulenDocument2 pagesUpdate Pasien NC 25 April 2021 Untuk Konsulenbosnia agusNo ratings yet
- Spinal Shock: By: DR Ismah, Ortho DepartmentDocument16 pagesSpinal Shock: By: DR Ismah, Ortho Departmentbosnia agusNo ratings yet
- Spinal Shock.Document12 pagesSpinal Shock.bosnia agusNo ratings yet
- Treatment of Colonic Diverticular Disease: Role of Surgery: Controversies in GastroenterologyDocument5 pagesTreatment of Colonic Diverticular Disease: Role of Surgery: Controversies in GastroenterologyGianfranco MuntoniNo ratings yet
- Case Presentation Hernia 1 PDFDocument21 pagesCase Presentation Hernia 1 PDFMvs ramuNo ratings yet
- Total Mesorectal Excision (Tme)Document19 pagesTotal Mesorectal Excision (Tme)Mehtab JameelNo ratings yet
- Malaysia Health CareDocument4 pagesMalaysia Health Careaffandy96585No ratings yet
- Sudaria Ivy G. AnswerKeysDocument25 pagesSudaria Ivy G. AnswerKeysDeinielle Magdangal RomeroNo ratings yet
- Implant SystemsDocument103 pagesImplant SystemsBharathi GudapatiNo ratings yet
- KPJ Annual ReportDocument168 pagesKPJ Annual ReportRs AndaluciaNo ratings yet
- Custom Nasal Septum Prosthesis Using 3D PrintingDocument4 pagesCustom Nasal Septum Prosthesis Using 3D PrintingSahana RangarajanNo ratings yet
- From Concept To Market: Surgical Robot Development: Tamás Haidegger, Imre J. RudasDocument39 pagesFrom Concept To Market: Surgical Robot Development: Tamás Haidegger, Imre J. Rudas1325907No ratings yet
- Motivational EssayDocument1 pageMotivational EssayAtifa WardakNo ratings yet
- Registration of Medical Devices OnlineDocument4 pagesRegistration of Medical Devices OnlineGens GeorgeNo ratings yet
- Urodynamic Testing ReportDocument25 pagesUrodynamic Testing Reportzharah180% (1)
- Form 6 Revised 2022Document2 pagesForm 6 Revised 2022Angelo AlcantaraNo ratings yet
- DR Profile All Department Part 2Document50 pagesDR Profile All Department Part 2joynal abedeenNo ratings yet
- Appendicitis: Diseases and Conditions: AppendicitisDocument6 pagesAppendicitis: Diseases and Conditions: AppendicitisWen RodsaNo ratings yet
- The Five-Step Rhinoplasty Dead Space Closure TechniqueDocument2 pagesThe Five-Step Rhinoplasty Dead Space Closure TechniqueAdRiaNa JuLIetH LoZaDa PaTiÑoNo ratings yet
- Kaldenbach Carina Articol EPI Engleza PDFDocument9 pagesKaldenbach Carina Articol EPI Engleza PDFFlorin UngureanuNo ratings yet
- Guidelines For Referral To Restorative Specialst MOHDocument10 pagesGuidelines For Referral To Restorative Specialst MOHadi satriaNo ratings yet
- Dr. Cereno and Zafe vs. CA-2Document6 pagesDr. Cereno and Zafe vs. CA-2John Lyonell PagulayanNo ratings yet
- 24 Anorectal ConditionsDocument55 pages24 Anorectal ConditionsRaisa CleizeraNo ratings yet
- Main - Microblading Consent FormDocument2 pagesMain - Microblading Consent FormAnnee bellaNo ratings yet
- Jurnal Problem Foot ChildrenDocument5 pagesJurnal Problem Foot ChildrenAbu Bakar SiddiqNo ratings yet
- Ijspt 2022 17 3 33151Document13 pagesIjspt 2022 17 3 33151AV Niken AstutiNo ratings yet
- Total Abdominal Hysterectomy TechniqueDocument9 pagesTotal Abdominal Hysterectomy TechniqueVikram DevNo ratings yet
- Corneoscleral T&S - PrinciplesDocument10 pagesCorneoscleral T&S - PrinciplesMuhammad SyamilNo ratings yet
- Pontics in Fixed Partial DentureDocument63 pagesPontics in Fixed Partial DentureKashish ManghaniNo ratings yet
- Iris Suture Set Hattenbach EDocument2 pagesIris Suture Set Hattenbach Eophtho india incNo ratings yet
- Imaging in The Post-Partum Period: Clinical Challenges, Normal Findings, and Common Imaging PitfallsDocument13 pagesImaging in The Post-Partum Period: Clinical Challenges, Normal Findings, and Common Imaging PitfallsBesse Darmita Yuana PutriNo ratings yet
- D D I 6130.03 M S A, E, I M SDocument49 pagesD D I 6130.03 M S A, E, I M Snour abdallaNo ratings yet
- Preemptive Quadratus Lumborum Laparoscopic BariatricDocument8 pagesPreemptive Quadratus Lumborum Laparoscopic BariatricEmmanuel FortalezaNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)